Abstract
BACKGROUND
Postpartum depression (PPD) not only affects the psychological and physiological aspects of maternal health but can also affect neonatal growth and development. Partners who are in close contact with parturient women play a key role in communication and emotional support. This study explores the PPD support relationship with partners and its influencing factors, which is believed to establish psychological well-being and improve maternal partner support.
AIM
To explore the correlation between PPD and partner support during breastfeeding and its influencing factors.
METHODS
Convenience sampling was used to select lactating women (200 women) who underwent postpartum examinations at the Huzhou Maternity and Child Health Care Hospital from July 2022 to December 2022. A cross-sectional survey was conducted on the basic information (general information questionnaire), depression level [edinburgh postnatal depression scale (EPDS)], and partner support score [dyadic coping inventory (DCI)] of the selected subjects. Pearson’s correlation analysis was used to analyze the correlation between PPD and DCI in lactating women. Factors affecting PPD levels during lactation were analyzed using multiple linear regression.
RESULTS
The total average score of EPDS in 200 lactating women was (9.52 ± 1.53), and the total average score of DCI was (115.78 ± 14.90). Dividing the EPDS, the dimension scores were: emotional loss (1.91 ± 0.52), anxiety (3.84 ± 1.05), and depression (3.76 ± 0.96). Each dimension of the DCI was subdivided into: Pressure communication (26.79±6.71), mutual support (39.76 ± 9.63), negative support (24.97 ± 6.68), agent support (6.87 ± 1.92), and joint support (17.39 ± 4.19). Pearson’s correlation analysis demonstrated that the total mean score and individual dimension scores of EPDS during breastfeeding were inversely correlated with the total score of partner support, stress communication, mutual support, and co-support (P < 0.05). The total mean score of the EPDS and its dimensions were positively correlated with negative support (P < 0.05). Multiple linear regression analysis showed that the main factors affecting PPD during breastfeeding were marital harmony, newborn health, stress communication, mutual support, negative support, co-support, and the total score of partner support (P < 0.05).
CONCLUSION
PPD during breastfeeding was associated with marital harmony, newborn health, stress communication, mutual support, negative support, joint support, and the total DCI score.
Keywords: Lactation period, Puerpera, Postpartum depression, Partner support, Correlation
Core Tip: Lactating women face both physical and psychological pressures and are prone to postpartum depression (PPD), bipolar disorder, and other mental disorders. The partner is a close contact for the mother during this time, and their communication with the mother or behavioral decisions are crucial. Through this study, we found that during breastfeeding, mothers’ PPD, degree of marital harmony, newborn health situation, and partner support were associated.
INTRODUCTION
Given the implementation of China’s three-child policy, women's mental health status is of great significance to family and social development. Postpartum depression (PPD) is a common non-psychotic depression in women that persists for a certain period after childbirth. Studies have reported that the incidence of PPD in China is approximately 10.9%-18.6%[1,2]. In addition, there is evidence that PPD may impair infant development, increase children's distraction and antisocial or neurotic behaviors, and affect their cognition and play choices[3]. Moreover, by comparing the incidence of depression in women at 35-60 d and 18-30 mo postpartum, it was found that PPD continues to affect women's mental health[4]. As a unique physiological period for women, lactation is accompanied by changes in personal factors, such as role conversion, irregular work and rest, decreased resistance, and abnormal hormone secretion. In addition, there may be negative external factors such as a shift in the family’s attention, preference for the baby’s gender, a lack of understanding, and disrespect caused by differences in the perceptions of relatives and elders. Therefore, breastfeeding women are faced with both physical and psychological pressures and are prone to PPD, bipolar disorder, and other mental diseases[5,6]. For lactating women who lack the daily attention of relatives and friends as well as normal social interactions, the need for care from relatives and friends as well as social support, social trust, and partner support is critical.
As a close contact of lactating women, the partner's communication with the women and their behavioral decisions are crucial. Supportive coping is an effective way for partners to relieve individual stress through a series of measures, such as providing emotional support or helping solve problems after receiving specific stress signals[7]. Good partner support can not only help postpartum women physically but also provide psychological support, help them gain positive strength and a sense of hope about PPD, and prevent the deterioration of the marriage[8,9]. Currently, there are few studies on the factors influencing PPD among breastfeeding mothers in China, and the correlation between PPD and dyadic coping inventory (DCI) remains unclear. This study analyzed the correlation between PPD and DCI in women during lactation and explored the influencing factors to provide evidence for improving the mental health status of postpartum women.
MATERIALS AND METHODS
Object
Convenience sampling was used to select lactating women (200 women) who underwent postpartum examinations at the Huzhou Maternity and Child Health Care Hospital from July 2022 to December 2022. The inclusion criteria were as follows: Women who were: (1) Lactating; (2) between 18 and 40 years of age; (3) in a legal marriage or de facto marriage; and (4) willing to voluntarily participate in the investigation. The exclusion criteria were as follows: (1) Serious physical disease or disability, (2) accompanied by malignant tumors and mental abnormalities, and (3) dyslexia.
Methods
The relevant questionnaires were completed under the guidance of professional investigators trained in the hospital, who explained the purpose and significance of the study to the postpartum women and their families and informed them of the matters that needed attention. The questionnaire could only be issued with the consent of the postpartum woman and her family. The questionnaire was completed after on-site verification and retrieval.
Survey tool
(1) General information questionnaire: This included age, education level, planned pregnancy, parity, prenatal sleep, marital harmony, newborn health status, and mode of delivery; (2) The edinburgh postnatal depression scale (EPDS): This scale was developed by Cox et al[10] and translated into Chinese by Lee et al[11] at the Chinese University of Hong Kong. The scale includes three independent structural subscales (10 items in total): The affective deficit, anxiety, and depression subscales. Each item was scored on a scale of 0-3 points, with a total score of 0-30, which was proportional to depression; (3) DCI: The DCI compiled by Randall and Bodenmann[12] was used in this study. The questionnaire has five dimensions (35 items in total): Stress communication, negative coping, agent coping, mutual support, and joint support. All entries are self-assessed on a scale of 1-5, and the total score ranging from 35-175 for negative support responses is reversed. The score was proportional to partner-supportive coping.
Statistical analysis
The Chinese version of the Epi Data 3.1 was used for two-person input of the scale data. SPSS Statistics for Windows, version 26.0 (Armonk: NY, IBM Corp), was used to analyze the project data. Counting variables are expressed as [n (%)] and compared using the χ2 test. Continuous variables are reported as mean ± SD. Comparisons were performed using the t-test or one-way analysis of variance (ANOVA). This study employed multiple regression analysis to explore the factors influencing lactating women’s PPD score; inspection level α = 0.05. Statistical significance was set at P < 0.05, on behalf of the difference was statistically significant.
RESULTS
Single factor analysis of EPDS scores of women during lactation and EPDS scores of women with different characteristics
The total score of EPDS in 200 lactating women was (9.52 ± 1.53). Dividing the EPDS for all dimensions resulted in the following scores for emotional loss (1.91 ± 0.52), anxiety (3.84 ± 1.05), and depression (3.76 ± 0.96). The results are presented in Table 1. There were significant differences in PPD scores among those with different marital harmony and newborn health conditions (P < 0.05). The results are presented in Table 2.
Table 1.
Edinburgh postnatal depression scale scores during lactation
|
Item
|
Dimension score (points)
|
| Lack of emotion | 1.91 ± 0.52 |
| Anxiety | 3.84 ± 1.05 |
| Depression | 3.76 ± 0.96 |
| Total EPDS mean score | 9.52 ± 1.53 |
EPDS: Edinburgh postnatal depression scale.
Table 2.
Univariate analysis of edinburgh postnatal depression scale scores of parturients with different characteristics
|
Item
|
Number of cases
|
EPDS (scores)
|
t/F value
|
P value
|
| Age (yr) | -1.904 | 0.058 | ||
| ≤ 30 | 95 | 9.31 ± 1.36 | ||
| > 30 | 105 | 9.71 ± 1.65 | ||
| Education level (yr) | 0.246 | 0.864 | ||
| Junior high school and below | 41 | 9.63 ± 1.55 | ||
| Secondary school or high school | 72 | 9.51 ± 1.51 | ||
| Junior college | 62 | 9.40 ± 1.73 | ||
| Bachelor’s degree or above | 25 | 9.64 ± 1.53 | ||
| Plan a pregnancy | -1.170 | 0.243 | ||
| Yes | 129 | 9.43 ± 1.55 | ||
| No | 71 | 9.69 ± 1.49 | ||
| Number of births | ||||
| Primary birth | 118 | 9.38 ± 1.52 | -1.450 | 0.149 |
| Multiparous | 82 | 9.71 ± 1.53 | ||
| Prenatal sleep status | 1.030 | 0.380 | ||
| Good | 84 | 9.57 ± 1.63 | ||
| General | 48 | 9.21 ± 1.50 | ||
| Occasional insomnia | 46 | 9.61 ± 1.18 | ||
| Frequent insomnia | 22 | 9.82 ± 1.79 | ||
| Marriage harmony situation | -4.804 | < 0.001 | ||
| Harmonious | 126 | 9.14 ± 1.35 | ||
| Disharmonious | 74 | 10.16 ± 1.59 | ||
| Mode of delivery | 1.759 | 0.080 | ||
| Natural childbirth | 110 | 9.69 ± 1.49 | ||
| Cesarean section | 90 | 9.31 ± 1.56 | ||
| Neonatal health | -10.051 | < 0.001 | ||
| Healthy | 137 | 8.92 ± 1.25 | ||
| Unhealthy | 63 | 10.83 ± 1.24 |
EPDS: Edinburgh postnatal depression scale.
Maternal DCI score
The average DCI score of 200 lactating women was (115.78 ± 14.90). Each dimension of the DCI was separated into pressure communication (26.79 ± 6.71), mutual support (39.76 ± 9.63), negative support (24.97 ± 6.68), agent support (6.87 ± 1.92), and joint support (17.39 ± 4.19) scores. The results are presented in Table 3.
Table 3.
Dyadic coping inventory scores during lactation
|
Item
|
Dimension score (points)
|
| Stress communication | 26.79 ± 6.71 |
| Mutual support | 39.76 ± 9.63 |
| Negative support | 24.97 ± 6.68 |
| Agent support | 6.87 ± 1.92 |
| Joint support | 17.39 ± 4.19 |
| DCI total average | 115.78 ± 14.90 |
DCI: Dyadic coping inventory.
Correlation analysis of PPD and DCI during lactation
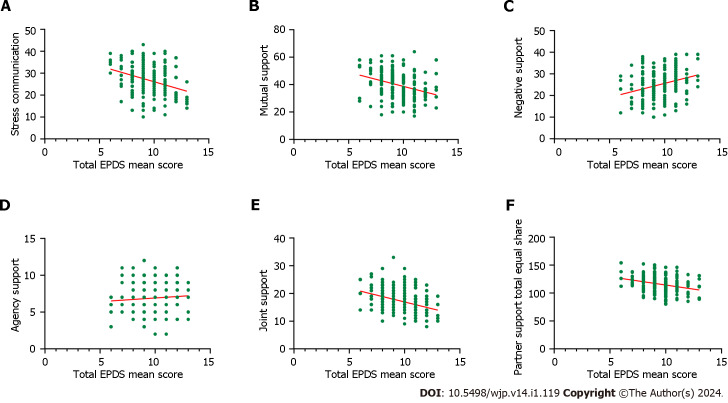
Pearson’s correlation analysis showed that the total average score of the EPDS and its dimensions during lactation were inversely proportional to the total scores of partner support, stress communication, mutual support, and common support of lactating women (P < 0.05). The total average score and each dimension of the EPDS were positively correlated with negative support (P < 0.05). The results are presented in Table 4. Among them, the relationship between the EPDS total mean score and each dimension and the total DCI mean score is shown in Figure 1.
Table 4.
Correlation between edinburgh postnatal depression scale and dyadic coping inventory during lactation
|
Dimensions
|
Lack of emotion
|
Anxiety
|
Depression
|
Total EPDS mean score
|
| Stress communication | -0.150a | -0.252c | -0.163a | -0.327c |
| Mutual support | -0.282c | -0.165a | -0.185b | -0.326c |
| Negative support | 0.178a | 0.157a | 0.205b | 0.298c |
| Agent support | -0.087 | 0.117 | 0.046 | 0.080 |
| Joint support | -0.238b | -0.158a | -0.301c | -0.357c |
| DCI total average | -0.248c | -0.172a | -0.167a | -0.308c |
P < 0.05.
P < 0.001.
P < 0.0001.
EPDS: Edinburgh postnatal depression scale; DCI: Dyadic coping inventory.
Figure 1.
The relationship between the total mean score of edinburgh postnatal depression scale and each dimension and total mean score of dyadic coping inventory. A: Edinburgh postnatal depression scale (EPDS) total split and pressure relationship; B: EPDS always divides relationships with mutual support; C: Relationship between total EPDS mean score and negative support; D: Relationship between EPDS general sharing and agency support; E: Relationship between total EPDS sharing and joint support; F: Relationship between the total mean EPDS score and the total mean dyadic coping inventory score. EPDS: Edinburgh postnatal depression scale.
Stepwise regression analysis of different characteristics and DCI on PPD during lactation
Multivariate linear regression analysis was undertaken with the total mean score of PPD as the dependent variable, and the characteristics of puerpera and each dimension and the total score of the DCI as the independent variables (Table 5). The selected variable α = 0.05, and the excluded variable α = 0.10 were used for multiple linear regression analysis, the results showed that the main factors affecting PPD in lactating women were marital harmony, newborn health, pressure communication, mutual support, negative support, common support, and the total average score of the DCI (P < 0.05). The results are presented in Table 6.
Table 5.
Variable assignment
|
Item
|
Assignment mode
|
| Age | ≤ 30 yr = 0, > 30 yr = 1 |
| Education level | Junior high school and below = 0, secondary school or high school = 1, junior college = 2, Bachelor’s degree or above = 3 |
| Plan a pregnancy | Yes = 0, no = 1 |
| Number of births | Primary birth = 0, produce = 1 |
| Prenatal sleep status | Good = 0, general = 1, occasional insomnia = 2, frequent insomnia = 3 |
| Marriage harmony situation | Harmonious = 0, disharmonious = 1 |
| Mode of delivery | Natural childbirth = 0, cesarean section = 1 |
| Neonatal health | Healthy = 0, unhealthy = 1 |
| Stress communication | - |
| Mutual support | - |
| Negative support | - |
| Agent support | - |
| Joint support | - |
| DCI total average | - |
DCI: Dyadic coping inventory.
Table 6.
Multiple stepwise regression analysis of postpartum depression during lactation by different characteristics and dyadic coping inventory.
|
Independent variable
|
Partial regression coefficient
|
Standard regression coefficient
|
t
|
P value
|
| Marital harmony | 0.903 | 0.190 | 4.765 | < 0.001 |
| Newborn health | 1.069 | 0.194 | 5.524 | < 0.001 |
| Stress communication | -0.129 | 0.032 | -4.074 | < 0.001 |
| Mutual support | -0.099 | 0.029 | -3.389 | 0.001 |
| Negative support | -0.061 | 0.030 | -2.015 | 0.045 |
| Joint support | -0.143 | 0.033 | -4.361 | < 0.001 |
| DCI total average | 0.085 | 0.029 | 4.765 | 0.004 |
R = 0.744, R2 = 0.553, after the adjustment R2 = 0.537, F = 33.957, P < 0.001. DCI: Dyadic coping inventory.
DISCUSSION
PPD refers to mothers with no previous history of mental disorders showing symptoms of depression, postpartum within six weeks of the first onset; depression, boredom, crying and emotional irritability are the main characteristics of PPD. Severe cases may manifest as hallucinations and even self-harm, harming the baby, and other violent episodes[13]. PPD is a common abnormal psychological behavior in gynecology that seriously endangers the physical and mental health of pregnant women and affects the growth and development of infants. The incidence of PPD is slightly different between countries, with a prevalence of more than 20% in Western countries and 10%-20% in China[14,15]. The total average score of EPDS in 200 lactating women in this study was (9.52 ± 1.53), indicating that the EPDS of lactating women were at a moderate level. This may have been affected by different PPD evaluation time points and different evaluation tools. In addition, PPD is related to other factors such as regional economic development, population structure, cultural background, and so on.
The total partner support score of 200 cases during lactation was (115.78 ± 14.90), and the partner support level for PPD during lactation was moderate. This indicated that women were more willing to face the illness with their partners. Regarding communication and mutual support pressure, the score was relatively high, showing that mothers with PPD tend to communicate and take the initiative to talk about their psychological problems to obtain their partner's support and understanding, when facing pressure. By encouraging and supporting each other, both parties can reduce psychological pressure and create a good spiritual environment[16,17]. Korotkin et al[18] believed that the expression of emotions in the process of patients seeking social support can significantly improve their psychological pressure of patients. Studies have found that a good family atmosphere can provide sufficient material and spiritual support, enhance patients' sense of self-esteem, and reduce pressure when they are ill[19]. These findings provide guidelines for interventions in PPD.
This study found that the total average score and each dimension of the postpartum EPDS were inversely related to the total score of partner support, pressure communication, mutual support, and common support, and positively related to negative support (P < 0.05), suggesting that good relationships with the partner can lower the mother’s bad mood. Eastwood[20] found that emotional support from a partner was closely associated with PPD and was an important indicator to measure partnerships. Razurel and Kaiser[21] noted that pregnant women had different expectations and requirements from family members. Partners can provide strong support for lactating women with depression in terms of their financial and psychological well-being as well as disease-related care, which can reduce their psychological burden, relieve patients' negative emotions, and greatly improve their quality of life[22,23].
The effect of influential factors of PPD are relatively complex. Multiple linear regression analysis results show that the influence degree of the factors in lactating mothers’ PPD include marital harmony, newborn health condition, communication, mutual support, negative pressure support, mutual support, and partner support total score (P < 0.05). According to existing literature, marital disharmony is also a risk factor for PPD[24,25]. Analysis suggests that the capacity of lactating parturients to bear psychological stress is weak, and marital disharmony can increase their psychological burden. Additionally, when newborn health is poor, pregnant women will not only find it difficult to accept, but also have a large psychological gap, and are therefore prone to serious negative mental well-being, thus inducing PPD[26,27]. Therefore, clinical attention should be paid to postpartum psychological changes and corresponding measures should be taken to reduce PPD as much as possible. Partners are the most important source of social support for patients and an important aspect that affects patients' perceptions of illness. Good partner support can be reflected in the care and understanding of patients' physical and mental well-being and is a positive and strong source of hope for patients[28]. The positive support and communication of partners can alleviate postpartum women’s negative emotions and improve the negative cognition of the patients. Contrastingly, negative support can increase a patients' negative awareness, and negative support and awareness promote each other[29].
CONCLUSION
In summary, PPD during lactation was associated with marital harmony, newborn health, stress communication, mutual support, negative support, co-support, and partner support. Hospitals and relevant departments should pay attention to the level of PPD in parturients, guide them to correctly recognize and understand the disease, carry out targeted individualized nursing interventions for patients and their partners, and improve the support level of their partners to improve the mental health of parturients with PPD.
ARTICLE HIGHLIGHTS
Research background
Postpartum depression (PPD) not only causes anxiety, lower self-image, self-guilt, and other conditions in lactating women but also has adverse effects on the health of the baby. PPD can appear in normal life circumstances and negative life events such as marital discord. Good partner support can not only help patients physically but also provide psychological support. Exploring the relationship between PPD and dyadic coping inventory (DCI) in lactating women and analyzing the related influencing factors of PPD are helpful for clinical interventions from related factors to prevent and alleviate the occurrence of PPD.
Research motivation
Negative partner support, marital disharmony, and unhealthy newborns were associated with PPD in lactating women.
Research objectives
By exploring the relationship between PPD and partner support and the factors affecting PPD in lactating women, it is helpful to provide a reference for the clinical construction of PPD intervention programs and partner support strategies.
Research methods
A general information questionnaire, edinburgh postnatal depression scale (EPDS) scale, and DCI scale were used to investigate the correlation between PPD and partner support during lactation, and to further analyze the factors affecting the level of PPD.
Research results
The total average score of EPDS of 200 women during lactation was (9.52 ± 1.53), and the total average score of partner support was (115.78 ± 14.90), both of which were at the medium level. The degree of marital harmony, neonatal health, stress communication, mutual support, negative support, common support, and total partner support score were factors influencing PPD in lactating women.
Research conclusions
Through research, we found that the poor psychological health of lactating women is significantly related to their partner support. By analyzing the influencing factors of women's PPD, providing timely psychological help and encouraging partners to provide maternal support and care will help to improve the PPD level of lactating women.
Research perspectives
Future research should establish a predictive model based on the factors influencing PPD in lactating women.
Footnotes
Institutional review board statement: The study was reviewed and approved by the Huzhou Maternity and Child Health Care Hospital (Zhejiang Province).
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: There are no conflicts of interest to report.
STROBE statement: The authors have read the STROBE Statement-checklist of items, and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: October 26, 2023
First decision: November 8, 2023
Article in press: December 5, 2023
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Santini A, Italy; Sonali S, United States S-Editor: Qu XL L-Editor: A P-Editor: Chen YX
Contributor Information
Ji-Ming Ruan, Department of Obstetrics and Gynecology, Huzhou Maternity and Child Health Care Hospital, Huzhou 313000, Zhejiang Province, China.
Ling-Juan Wu, Department of Obstetrics and Gynecology, Huzhou Maternity and Child Health Care Hospital, Huzhou 313000, Zhejiang Province, China. wulingjuan110@163.com.
Data sharing statement
Data used in this study were obtained from the corresponding author.
References
- 1.Liu X, Wang S, Wang G. Prevalence and Risk Factors of Postpartum Depression in Women: A Systematic Review and Meta-analysis. J Clin Nurs. 2022;31:2665–2677. doi: 10.1111/jocn.16121. [DOI] [PubMed] [Google Scholar]
- 2.Nisar A, Yin J, Waqas A, Bai X, Wang D, Rahman A, Li X. Prevalence of perinatal depression and its determinants in Mainland China: A systematic review and meta-analysis. J Affect Disord. 2020;277:1022–1037. doi: 10.1016/j.jad.2020.07.046. [DOI] [PubMed] [Google Scholar]
- 3.Grace SL, Evindar A, Stewart DE. The effect of postpartum depression on child cognitive development and behavior: a review and critical analysis of the literature. Arch Womens Ment Health. 2003;6:263–274. doi: 10.1007/s00737-003-0024-6. [DOI] [PubMed] [Google Scholar]
- 4.Gopalan P, Spada ML, Shenai N, Brockman I, Keil M, Livingston S, Moses-Kolko E, Nichols N, O'Toole K, Quinn B, Glance JB. Postpartum Depression-Identifying Risk and Access to Intervention. Curr Psychiatry Rep. 2022;24:889–896. doi: 10.1007/s11920-022-01392-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Silva CS, Lima MC, Sequeira-de-Andrade LAS, Oliveira JS, Monteiro JS, Lima NMS, Santos RMAB, Lira PIC. Association between postpartum depression and the practice of exclusive breastfeeding in the first three months of life. J Pediatr (Rio J) 2017;93:356–364. doi: 10.1016/j.jped.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Becker M, Weinberger T, Chandy A, Schmukler S. Depression During Pregnancy and Postpartum. Curr Psychiatry Rep. 2016;18:32. doi: 10.1007/s11920-016-0664-7. [DOI] [PubMed] [Google Scholar]
- 7.Varner S, Lloyd G, Ranby KW, Callan S, Robertson C, Lipkus IM. Illness uncertainty, partner support, and quality of life: A dyadic longitudinal investigation of couples facing prostate cancer. Psychooncology. 2019;28:2188–2194. doi: 10.1002/pon.5205. [DOI] [PubMed] [Google Scholar]
- 8.Hinnen C, Ranchor AV, Baas PC, Sanderman R, Hagedoorn M. Partner support and distress in women with breast cancer: The role of patients' awareness of support and level of mastery. Psychol Health. 2009;24:439–455. doi: 10.1080/08870440801919513. [DOI] [PubMed] [Google Scholar]
- 9.Gil N, Fisher A, Beeken RJ, Pini S, Miller N, Buck C, Lally P, Conway R. The role of partner support for health behaviours in people living with and beyond cancer: A qualitative study. Psychooncology. 2022;31:1997–2006. doi: 10.1002/pon.6032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 11.Lee DT, Yip SK, Chiu HF, Leung TY, Chan KP, Chau IO, Leung HC, Chung TK. Detecting postnatal depression in Chinese women. Validation of the Chinese version of the Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1998;172:433–437. doi: 10.1192/bjp.172.5.433. [DOI] [PubMed] [Google Scholar]
- 12.Randall AK, Bodenmann G. The role of stress on close relationships and marital satisfaction. Clin Psychol Rev. 2009;29:105–115. doi: 10.1016/j.cpr.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Pearlstein T, Howard M, Salisbury A, Zlotnick C. Postpartum depression. Am J Obstet Gynecol. 2009;200:357–364. doi: 10.1016/j.ajog.2008.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sockol LE, Epperson CN, Barber JP. Preventing postpartum depression: a meta-analytic review. Clin Psychol Rev. 2013;33:1205–1217. doi: 10.1016/j.cpr.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ceriani Cernadas JM. Postpartum depression: Risks and early detection. Arch Argent Pediatr. 2020;118:154–155. doi: 10.5546/aap.2020.eng.154. [DOI] [PubMed] [Google Scholar]
- 16.Kroska EB, Stowe ZN. Postpartum Depression: Identification and Treatment in the Clinic Setting. Obstet Gynecol Clin North Am. 2020;47:409–419. doi: 10.1016/j.ogc.2020.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Traa MJ, De Vries J, Bodenmann G, Den Oudsten BL. Dyadic coping and relationship functioning in couples coping with cancer: a systematic review. Br J Health Psychol. 2015;20:85–114. doi: 10.1111/bjhp.12094. [DOI] [PubMed] [Google Scholar]
- 18.Korotkin BD, Hoerger M, Voorhees S, Allen CO, Robinson WR, Duberstein PR. Social support in cancer: How do patients want us to help? J Psychosoc Oncol. 2019;37:699–712. doi: 10.1080/07347332.2019.1580331. [DOI] [PubMed] [Google Scholar]
- 19.Yamada A, Isumi A, Fujiwara T. Association between Lack of Social Support from Partner or Others and Postpartum Depression among Japanese Mothers: A Population-Based Cross-Sectional Study. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17124270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eastwood JG, Jalaludin BB, Kemp LA, Phung HN, Barnett BE. Relationship of postnatal depressive symptoms to infant temperament, maternal expectations, social support and other potential risk factors: findings from a large Australian cross-sectional study. BMC Pregnancy Childbirth. 2012;12:148. doi: 10.1186/1471-2393-12-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Razurel C, Kaiser B. The role of satisfaction with social support on the psychological health of primiparous mothers in the perinatal period. Women Health. 2015;55:167–186. doi: 10.1080/03630242.2014.979969. [DOI] [PubMed] [Google Scholar]
- 22.Pilkington P, Milne L, Cairns K, Whelan T. Enhancing reciprocal partner support to prevent perinatal depression and anxiety: a Delphi consensus study. BMC Psychiatry. 2016;16:23. doi: 10.1186/s12888-016-0721-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lal A, Bartle-Haring S. Relationship among differentiation of self, relationship satisfaction, partner support, and depression in patients with chronic lung disease and their partners. J Marital Fam Ther. 2011;37:169–181. doi: 10.1111/j.1752-0606.2009.00167.x. [DOI] [PubMed] [Google Scholar]
- 24.Qi W, Zhao F, Liu Y, Li Q, Hu J. Psychosocial risk factors for postpartum depression in Chinese women: a meta-analysis. BMC Pregnancy Childbirth. 2021;21:174. doi: 10.1186/s12884-021-03657-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shi P, Ren H, Li H, Dai Q. Maternal depression and suicide at immediate prenatal and early postpartum periods and psychosocial risk factors. Psychiatry Res. 2018;261:298–306. doi: 10.1016/j.psychres.2017.12.085. [DOI] [PubMed] [Google Scholar]
- 26.Slomian J, Honvo G, Emonts P, Reginster JY, Bruyère O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Womens Health (Lond) 2019;15:1745506519844044. doi: 10.1177/1745506519844044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McPeak KE, Sandrock D, Spector ND, Pattishall AE. Important determinants of newborn health: postpartum depression, teen parenting, and breast-feeding. Curr Opin Pediatr. 2015;27:138–144. doi: 10.1097/MOP.0000000000000185. [DOI] [PubMed] [Google Scholar]
- 28.Goldzweig G, Baider L, Andritsch E, Rottenberg Y. Hope and social support in elderly patients with cancer and their partners: an actor-partner interdependence model. Future Oncol. 2016;12:2801–2809. doi: 10.2217/fon-2016-0267. [DOI] [PubMed] [Google Scholar]
- 29.Desta M, Memiah P, Kassie B, Ketema DB, Amha H, Getaneh T, Sintayehu M. Postpartum depression and its association with intimate partner violence and inadequate social support in Ethiopia: a systematic review and meta-analysis. J Affect Disord. 2021;279:737–748. doi: 10.1016/j.jad.2020.11.053. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data used in this study were obtained from the corresponding author.