Abstract
Central line-associated bloodstream infections (CLABSIs) are common healthcare-associated infections in pediatrics. Children’s hospital CLABSI standardized infection ratios decreased when comparing 2016–2019 (−26%, 95% CI [−31%, −20%]), and increased from 2019 to 2022 (18%, 95% CI [9%, 26%]). Resilient pediatric CLABSI prevention initiatives are needed.
Keywords: central line-associated bloodstream infection, healthcare-associated infections, infection prevention
INTRODUCTION
On any given day, an estimated one in 31 (3%) hospitalized patients in the United States has a healthcare-associated infection (HAI) [1]. Central line-associated bloodstream infections (CLABSIs) are a common HAI; 27 021 CLABSIs were reported from 3710 hospitals to the National Healthcare Safety Network (NHSN) in 2021 [2]. Children and adolescents under the age of 18 experience HAIs in healthcare at similar rates as adults [1] and CLABSIs are the most common device-associated HAI event in hospitalized children [3]. A previous report found increased CLABSI standardized infection ratios (SIRs) in Quarter 2 2020, the beginning of the COVID-19 pandemic, including within pediatric wards [4]. We further analyzed CLABSI SIRs of children’s hospitals reporting to NHSN from 2016 to 2022 to inform the need for pediatric-specific prevention efforts.
METHODS
The National Healthcare Safety Network is a surveillance system for healthcare quality measurement and improvement with nearly 40 000 healthcare facilities reporting to NHSN annually; all healthcare facilities receiving payment from the Centers for Medicare & Medicaid Services (CMS) are required to report patient safety data to NHSN. In this analysis, we included all children’s hospitals’ central line days and CLABSI event data in NHSN from 2016 to 2022. This included all pediatric unit types from reporting hospitals defined by NHSN enrollment as a children’s hospital; pediatric wards within general adult hospitals were not included. All reporting pediatric inpatient unit types were included in the analysis. Annual SIRs were calculated by dividing the number of observed infections by the predicted infections determined from the risk adjusted model using national data during the 2015 baseline period [5]. The inclusion criteria used for this work differ from criteria used in the HAI Progress Reports; SIR estimates may not match exactly (https://www.cdc.gov/nhsn/datastat/progress-report.html). Analyses were not limited to continuous reporters (eg, facilities reporting in 2017 may not match facilities reporting in 2019). We calculated SIR percentiles for a subset of facilities with at least one predicted CLABSI per year. Calculated SIRs were compared using a mid-P exact test.
RESULTS
A total of 110 children’s hospitals reported 8 890 970 central line days during the study period. Facility counts, events, pooled SIRs, and percentile distribution of SIRs by year are shown in Table 1 and Figure 1. In 2022, 41% of central line days were reported from pediatric wards, followed by 32% from pediatric intensive care units and 26% from neonatal intensive care units (NICU); percentages were similar for all years. The overall SIR for children’s hospitals in 2016 was 0.924, 2019 was 0.687, and 2022 was 0.808. Comparing years 2016 and 2019, children’s hospitals’ SIRs decreased by 26% (95% CI [−31%, −20%], P-value < .001). For 2019 and 2022, SIRs increased by 18% (95% CI [9%, 26%], P-value < .001). Of reporting facilities, 63% of facilities reported all seven years, which accounted for 94% of central line days.
Table 1.
Annual Distribution of Pediatric Central Line-Associated Bloodstream Infection Standardized Infection Ratios for Children’s Hospitals for 2016–2022 Reported to the National Healthcare Safety Network
| Percentile—Facility Level SIRs** | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Year | Facility Count* | CLABSI Events | Central Line Days | Predicted Number of Events | Pooled SIR | 10th | 25th | 50th | 75th | 90th |
| 2016 | 79 | 1457 | 1 170 151 | 1576.72 | 0.924 | 0.396 | 0.654 | 0.948 | 1.149 | 1.364 |
| 2017 | 88 | 1403 | 1 256 554 | 1702.31 | 0.824 | 0.216 | 0.533 | 0.752 | 1.021 | 1.312 |
| 2018 | 97 | 1328 | 1 257 195 | 1709.11 | 0.777 | 0.339 | 0.540 | 0.707 | 1.026 | 1.206 |
| 2019 | 97 | 1208 | 1 297 981 | 1759.24 | 0.687 | 0.331 | 0.442 | 0.658 | 0.862 | 1.423 |
| 2020 | 93 | 1098 | 1 207 578 | 1644.25 | 0.668 | 0.269 | 0.470 | 0.644 | 0.832 | 1.241 |
| 2021 | 94 | 1272 | 1 311 354 | 1805.94 | 0.704 | 0.368 | 0.508 | 0.665 | 0.908 | 1.212 |
| 2022 | 100 | 1527 | 1 388 759 | 1890.00 | 0.808 | 0.395 | 0.614 | 0.801 | 1.018 | 1.442 |
Abbreviations: CLABSI, central line-associated bloodstream infection; SIR, standardized infection ratio.
All facilities with reported central line days were included in pooled SIR calculations.
Facilities with at least 1 predicted event were included in percentile calculations.
Figure 1.
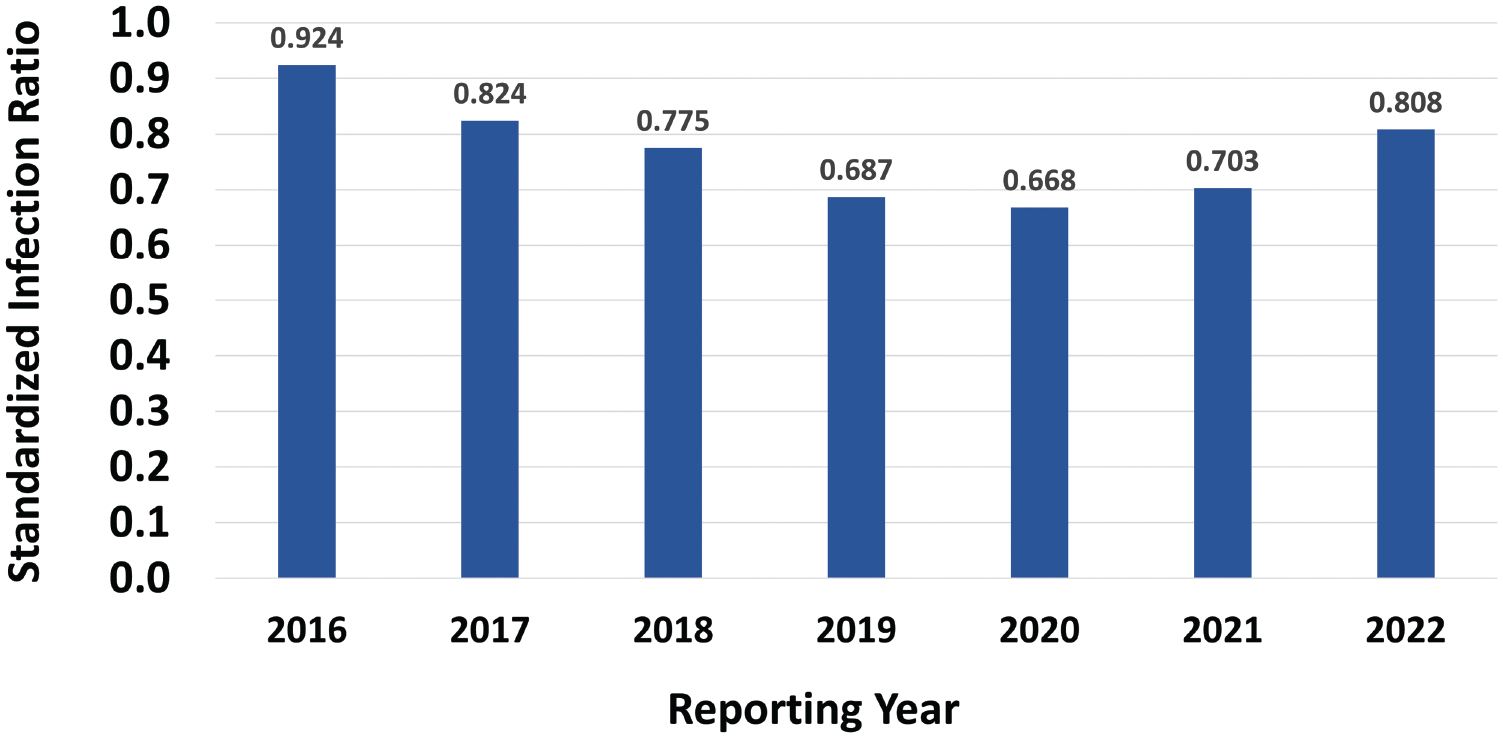
Graphical representation of the annual distribution of pediatric central line-associated bloodstream infection standardized infection ratios for children’s hospitals for 2016–2022 reported to the National Healthcare Safety Network.
DISCUSSION
Pediatric CLABSI SIRs reported from children’s hospitals for 2016–2022 year are <1 which suggests improvement from the 2015 NHSN baseline period. However, when comparing equal time frames, the pediatric CLABSI SIR decreased significantly from 2016 to 2019 but increased significantly from 2019 to 2022. The percentage of central line days did not vary significantly by unit type throughout the study period. Due to this observed increase in CLABSI SIRs, it is important to look at pediatric risk factors for CLABSI and how these may have changed over time.
Some CLABSI risk factors, like duration of central line use may not be unique to pediatric patients, however, other risk factors differ from adults including prematurity, size of the patient and size of central line, parenteral and lipid infusions for neonates [6], breakage of central venous catheters [7], and the presence of genetic syndromes [8]. Strategies to prevent CLABSIs were originally published in 2008 and later revised in 2014 and 2022 [9]. While pediatric-specific studies are included in the recommendations, they are not as well represented as adult studies which may limit evidence and applicability to pediatric settings.
Prevention efforts that reduce HAIs in adults may not have the same impact on pediatric patients and may require nuanced modifications, particularly in the NICU. A recent systematic review [10], along with a white paper from the Society for Healthcare Epidemiology of America [11], compiled evidence-based recommendations and expert opinion for CLABSI prevention in NICUs, however, the impact of these interventions on CLABSI rates will take time to become apparent and may be confounded by other concurrent healthcare system stressors. Tailoring infection prevention tools and bundles specific to pediatric settings may facilitate the implementation of recommended practices to ensure high compliance and a reduction in rates of HAIs.
A previous NHSN study noted a decrease in central line days and an increase in device utilization rates within pediatric medical-surgical wards (0.14–0.18) when comparing Q2 2019 (pre-COVID-19) to Q2 2020 among facilities that reported complete data in both quarters [4]. These data may suggest higher severity of disease, lower patient census in 2020 due to COVID-19 restrictions in children’s hospitals, or other differences in the patient population when comparing Q2 2019 to Q2 2020. Similarly, looking at all hospitals, not just pediatric facilities, there was an overall 28% increase in the CLABSI SIR during this period. While the reason for this CLABSI SIR increase is unclear, several factors may have contributed. Infection control and patient care practices might have changed during the pandemic due to COVID-19-specific infection prevention and control recommendations, the presence of staffing and supply shortages, and surges of patients requiring care [12]. The observed increase in pediatric CLABSI SIRs between 2019 and 2022 is likely multifactorial, influenced by more than the healthcare stressors of the COVID-19 pandemic, and will require additional investigations into changing acuity of patients and care locations within hospitals, among other considerations already stated.
There are several limitations to this study. Children’s hospitals occasionally care for non-pediatric patients (eg, age >18), a practice that was pronounced during COVID-19 surges. Patient demographics are not included in denominator data reported to NHSN so conclusions cannot be made on patient age, changing patient acuity, or other demographics year-to-year which may have influenced findings or patients’ necessity for central lines. This could be particularly important in 2020 and 2022 due to the COVID-19 pandemic and changes in patient care practices along with the dynamic ability of facilities to implement infection control bundles. Distribution of central line days by unit type are included in denominator data and adjusted for in SIR calculations.
With continued SARS-CoV-2 infections and surges of other respiratory illnesses leading to high rates of pediatric hospitalizations, HAIs will continue to pose significant danger to pediatric patients and may stall improvements made in prevention efforts like CLABSI reduction. Additional pediatric-specific studies and quality improvement initiatives should be developed to identify resilient infective prevention opportunities to mitigate the effect of healthcare stressors and reduce CLABSIs events within this vulnerable population.
Funding/Support:
No funding or support was received for this research.
Footnotes
Conflict of Interest Disclosures: The authors have no conflicts of interest relevant to this article to disclose.
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
REFERENCES
- 1.Magill SS, O’Leary E, Janelle SJ, et al. ; Emerging Infections Program Hospital Prevalence Survey Team. Emerging infections program hospital prevalence survey team. changes in prevalence of health care-associated infections in U.S. hospitals. N Engl J Med 2018; 379:1732–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Antibiotic Resistance and Patient Safety Portal—Central Line-Associated Bloodstream Infections. Accessed January 4, 2023. https://arpsp.cdc.gov/profile/nhsn/clabsi
- 3.Dudeck MA, Edwards JR, Allen-Bridson K, et al. National Healthcare Safety Network report, data summary for 2013, device-associated module. Am J Infect Control 2015; 43:206–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel PR, Weiner-Lastinger LM, Dudeck MA, et al. Impact of COVID-19 pandemic on central-line-associated bloodstream infections during the early months of 2020, National Healthcare Safety Network. Infect Control Hosp Epidemiol 2022; 43:790–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. The NHSN Standardized Infection Ratio (SIR). Available at: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/nhsn-sir-guide.pdf. Accessed 1 May 2023.
- 6.Brodie SB, Sands KE, Gray JE, et al. Occurrence of nosocomial bloodstream infections in six neonatal intensive care units. Pediatr Infect Dis J 2000; 19:56–65. [DOI] [PubMed] [Google Scholar]
- 7.Lundgren IS, Zhou C, Malone FR, McAfee NG, Gantt S, Zerr DM. Central venous catheter repair is associated with an increased risk of bacteremia and central line-associated bloodstream infection in pediatric patients. Pediatr Infect Dis J 2012; 31:337–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elward AM, Fraser VJ. Risk factors for nosocomial primary bloodstream infection in pediatric intensive care unit patients: a 2-year prospective cohort study. Infect Control Hosp Epidemiol 2006; 27:553–60. [DOI] [PubMed] [Google Scholar]
- 9.Buetti N, Marschall J, Drees M, et al. Strategies to prevent central line-associated bloodstream infections in acute-care hospitals: 2022 update. Infect Control Hosp Epidemiol 2022; 43:553–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Recommendations for Prevention and Control of Infections in Neonatal Intensive Care Unit Patients: Central Line-associated Blood Stream Infections. Published February 2022. Accessed December 5, 2022. https://www.cdc.gov/infectioncontrol/pdf/guidelines/nicu-clabsi-h.pdf
- 11.Muller M, Bryant KA, Espinosa C, et al. SHEA Neonatal Intensive Care Unit (NICU.White Paper Series: practical approaches for the prevention of central-line-associated bloodstream infections. Infect Control Hosp Epidemiol 2023; 44:550–64. [DOI] [PubMed] [Google Scholar]
- 12.McMullen KM, Smith BA, Rebmann T. Impact of SARS-CoV-2 on hospital acquired infection rates in the United States: predictions and early results. Am J Infect Control 2020; 48:1409–11. [DOI] [PMC free article] [PubMed] [Google Scholar]


