Abstract
In a long-term care facility, whose residents have been diagnosed with Alzheimer’s disease or dementia, falls are a particularly prominent issue. Technology in health care has continued to evolve and play a larger role in how we care for our patients, even in preventing falls. However, overreliance on these types of technologies may have detrimental effects. In our facility, it was felt that staff reliance on position-change alarms was inappropriate due to the high rate of false alarms associated with these devices. We took a tiered approach to removing position-change alarms from our facility, monitoring the fall incidence rate for a period before, during, and after the elimination of these alarms. After discontinuing their use, we found a decrease in the rate of falls, and a decrease in the percentage of our residents who fell. Staff has easily adapted and reports a calmer, more pleasant environment.
Keywords: Alzheimer’s disease, dementia, falls, bed-exit alarms, fall prevention, long-term care facility
Introduction
There is no question that falls in health care facilities are a major issue that must be addressed due to the physical and economical consequences of such an event, in particular because the number of patients in long-term care who are at risk of falling is expected to continue to grow. 1 -3 As such, technology has continually evolved with the intention of preventing patient falls, and a great deal of research has been conducted to determine who is at the greatest risk of falling, in order to focus on who should receive such interventions. 4,5 While some studies indicate that persons with mild dementia are at less risk of experiencing a fall, 6 several others suggest that patients with dementia are at increased risk of falling. 7,8 Other reports indicate that while a typical acute care fall rate might be as high as 9.1 falls per 1000 patient days, long-term care facilities are expected to have a fall rate which is at least twice that which occurs in acute care. 9
The evolution of fall prevention has seen a number of interventions which are intuitive in nature; the use of restraints and bedside rails were used widely in the attempt to keep patients safe. However, these techniques have been shown repeatedly not to be nearly as effective as expected, 8,10,11 and have even been quite dangerous. There have been numerous reports of elderly patients becoming entrapped in side rails, some with fatal consequences. 12 Additionally, data continues to mount which supports the removal of restraints; patients who are free to move about have shown better functionality and a decreased incidence of falling. 13,14 In light of this information, it may not be as surprising that one of the most common interventions used in long-term care to prevent resident falls is not as effective as believed 15 and could actually be a hazard—the bed-exit, or position-change, alarm.
Bed-exit alarms are used to alert caregivers that a patient who should not leave bed unassisted is doing so. These alarms were designed with the intent of reducing falls and facilitating faster responses to persons who have already fallen. They may consist of pressure-sensor activated alarms, which are typically sensor pads placed under the sheets or mattress or can be built in to the bed; cords which can be clipped to a patient’s clothing; and position-sensitive alarms, such as a cuff to be worn on the patient’s leg. The rate of nuisance alarms and resistance to tampering varies with both the type and brand of alarm. 16 Additionally, pressure-sensor alarms are often placed on the chair of a sitting patient to monitor any attempts to stand and walk unassisted. Any number of combinations of these alarms may be used to address the specific behaviors of patients. 17 More recently, infrared beams, less intrusive devices, and more sensitive and specific integrated bed-exit systems are being developed. 9,18 -20
Alarms that monitor patient movement while they are in bed or seated are used almost ubiquitously in residential care homes and are Joint Commission of Accreditation of Healthcare Organizations (JCAHO) endorsed. 21 However, there is a lack of evidence to suggest that these alarms are actually effective, and trials evaluating their effectiveness have not shown a significant improvement in the incidence of falls in patients who were monitored using these alarms when compared to a control group. In fact, the authors specifically mentioned the rate of false alarms, which was reported as a barrier to their use. 18,22 While false alarms may be considered a nuisance, it has been postulated that they also impede clinical care, as caregivers become desensitized to alarms 23 -26 and eventually may begin to respond only to the alarms and not to the needs of the patient. 27
Methods
Setting
Retrospective review of clinic records and patient charts for this research was approved by the ProMedica Health System Institutional Review Board. The setting of this uncontrolled before and after study is a free-standing, 60-bed, not-for-profit residential care facility tailored specifically to meet the needs of individuals with Alzheimer’s disease or advanced dementia. Our facility is part of a health system comprised of 11 hospitals, one of which is located adjacent to our facility. We have a total of 55 staff members, consisting of 8 licensed practical nurses, 7 registered nurses, and 40 state-tested nursing assistants in order to maintain a high staff to patient ratio. All residents receive a community referral prior to admission and undergo onsite evaluation including fall risk assessment, level of care, brief interview for mental status (BIMS), and evaluation by a physical therapist or occupational therapist upon arrival.
Since the opening of the facility in 1994, bed-exit alarms have been utilized for patients who are identified as being at high risk of falling or have shown behaviors that would increase falls. Every attempt is made to individualize care to meet the needs of each resident; therefore, a combination of built-in bed alarms, bed alarm pads, tabs which clip to the resident, and chair alarm pads were used as necessary. Movement alarm devices were used in approximately 75% of the residents during the day, the night, or at all times. Furthermore, individual interventions are continually developed for each resident based on their specific needs to prevent falls, such as scheduled restroom visits every 2 hours during the night for residents experiencing nocturia. Moreover, our facility has never utilized chemical means, bedside rails, or restraints as prevention for falls.
Planning and Implementation
Little evidence to suggest that bed-exit alarms are actually effective in preventing falls exists, and nursing administration observed a loud and disruptive environment due to the alarms sounding frequently. It was the opinion of administration that the staff may have become too dependent on the alarms due to their rounding habits; staff waited to respond to an alarm rather than acting to prevent them. As such, nursing administration wished to eliminate the use of such alarms in the facility. We monitored the number and types of falls occurring in the presence of the movement alarm devices for 4 months prior to and following the elimination of the position-change alarms. It was anticipated that staff members may not be supportive of removing the movement alarms initially. As such, administration elected to introduce the goal during a staff meeting and allow the staff to process the information slowly.
The “Alarm-Free” goal was discussed in 3 separate staff meetings over the course of 7 months before phasing out the alarms. In these staff meetings, the director of nursing reviewed literature with staff and also used role playing in order to introduce new perspectives to staff members. Administration planned to retrain staff in maintaining safety and involved staff members by asking for feedback and constructive ideas on how to keep the residents safe upon removal of the alarms. Conscious efforts were made to maintain a positive and high-energy attitude during staff education in this period.
The final phase of planning before removing the alarms was to educate the families of all residents. This was absolutely critical in ensuring success of the intervention and was achieved via one-on-one discussion, family council, and newsletters.
We began gradually removing the alarms from the beds and chairs of residents in June 2010. This was accomplished by incorporating the goal and progress into an established daily meeting which has proven to be integral in keeping staff updated about patient status and current state of operations. During the implementation of the intervention, administration and nurses reviewed the patients who had movement monitoring devices and their assessed level of fall risk. This assessment included medications, vital signs, chronic illnesses, history of falls, behaviors, and acute illnesses and injuries. Patients with the lowest risk of falling were the first to have their alarms eliminated to allow staff to gradually adapt to the new level of care required for our residents and prevent anticipated effects of a steep learning curve to the process. The staff was retrained to implement a more integrated fall prevention plan upon elimination of the alarms; they were required to round more frequently and to chart in places where they could maintain a view of their residents, even if this meant sitting outside of a resident’s room if, for example, the resident was experiencing increased restroom requirements (due to gastrointestinal upset or urinary tract infection). The staff was also retrained in their communication with their coworkers in order to ensure that common areas were constantly supervised and that any patients requiring one-on-one attention could receive it without sacrificing another unit. Additionally, families of residents were asked to complete a detailed social history to better allow us to understand the resident as a whole person to better cater to their specific needs.
After successfully removing a patient’s monitoring device, the next patient with the lowest risk of falling was transitioned to reside free of alarms; patients with the highest fall risk were the last to have their alarms removed. A new patient was not necessarily chosen each day, and discussion about how well staff and residents were transitioning dictated the rate at which more patients’ alarms were removed. This process continued until the end of August 2010 such that the facility functioned without bed- and chair-exit alarms as of September 1, 2010.
For 4 months prior to implementation of the “alarm-free initiative,” administration collected information about the number of falls occurring each month, the number of residents involved in the reported incidents, the number of patients residing in the facility, the admission rate (turnover of residents), and the number of patients requiring antipsychotic medication. The type of fall which occurred was also recorded and was categorized as follows: fall during ambulation, self-reported, lowered to floor, almost fell, slid from chair, fell out of bed, stood unassisted, or fell during a lift. For the purposes of analysis, the falls which could not have been affected by the bed-exit and chair alarms were removed, including falls during ambulation, almost fell, self-reported, and lowered to floor. Importantly, the incidents which were recorded in the categories “almost fell” and “lowered to floor” are not classified as falls by JCAHO, 21 however, the data describing all incidents within our facility are reported herein (see Table 1 ). Administration collected the same information during the 3-month intervention period and during the 4-month postintervention period. Importantly, none of the direct care staff members were aware that the administration was collecting and monitoring fall data or that it would be analyzed to determine the effectiveness of the intervention.
Table 1.
Summary of Resident Census, Number of Falls, and Types of Falls During Observation Period for All Residents a
| Feb | March | April | May | June | July | Aug | Sept | Oct | Nov | Dec | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Census | 48 | 48 | 48 | 48 | 58 | 58 | 58 | 60 | 60 | 60 | 60 |
| Number of admissions | 3 | 2 | 2 | 4 | 9 | 3 | 1 | 2 | 2 | 1 | 1 |
| Type of fall | |||||||||||
| Slid from chair | 2 | 1 | 1 | 1 | |||||||
| Out of bed | 6 | 1 | 2 | 3 | 3 | 2 | 5 | 1 | 3 | ||
| Stood unassisted | 2 | 2 | 2 | 3 | 2 | 4 | 1 | 1 | 3 | ||
| Lift | |||||||||||
| Total | 8 | 3 | 5 | 6 | 6 | 4 | 10 | 1 | 2 | 3 | 3 |
| Residents involved | 6 | 3 | 4 | 5 | 5 | 4 | 7 | 1 | 3 | 3 | 3 |
| Other fallsa | |||||||||||
| Self-reported | 1 | 2 | 1 | ||||||||
| During ambulation | 3 | 2 | 1 | 6 | 1 | 3 | 2 | 1 | 2 | 1 | 6 |
| Lowered to floor | 1 | 1 | 4 | 3 | 3 | 2 | 1 | ||||
| Almost fall | 1 | 1 | 1 | 1 | 2 | ||||||
| Total | 4 | 3 | 1 | 8 | 2 | 7 | 5 | 6 | 4 | 4 | 9 |
a Not included in analysis.
Statistical Analysis
The R Project for Statistical Computing (version 2.12.2) was used in data analysis. Analysis of variance (ANOVA) tests with post hoc comparisons were run in an attempt to identify mean differences in the number of falls per 1000 patient days by intervention stage and the percentage of residents falling by intervention stage, and the percentage of residents using antipsychotic drugs by intervention stage. Tests were declared statistically significant for a 2-sided P value of <.05.
Results
A total of 48 patients resided at the facility during the preintervention phase of this study, which increased to 58 residents during the intervention period and increased again to 60 patients during the postintervention phase of the observed time. Only 31 of these patients were residents during the entirety of all of the periods observed during this research. In order to control for changes which could be due to the introduction of a new resident to an unfamiliar setting, we analyzed the data of these 31 residents separately. However, we do report the data for our entire population, as well as observations made using this data. Of our total population, 93% of the residents were female, the mean age was 84.4 years and the average length of stay was 2.2 years. Of the subset population, in which most of our analysis was focused, 87% of the residents were female, the mean age was 85.9 years, and 35.5% were prescribed antipsychotic medications (including risperidone, quetiapine, and olanzapine). All residents were diagnosed as having either Alzheimer’s disease or dementia; 90.3% had been diagnosed with one or more comorbid mental health condition, including Organic Brain Syndrome (OBS), psychosis, depression, anxiety, paranoid state, insomnia, mood disorder, and obsessive-compulsive disorder.
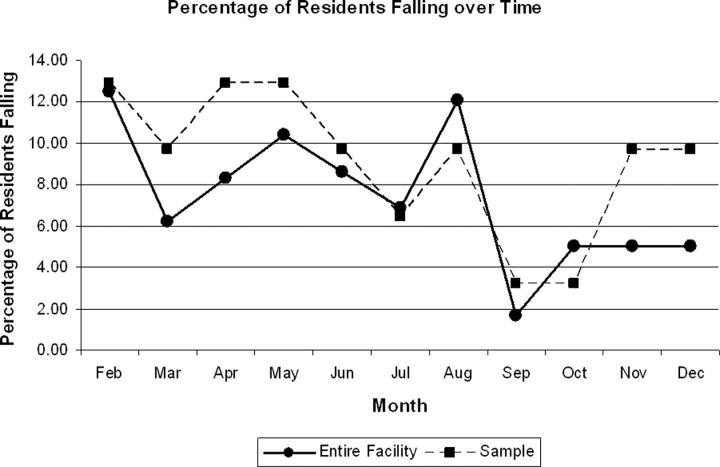
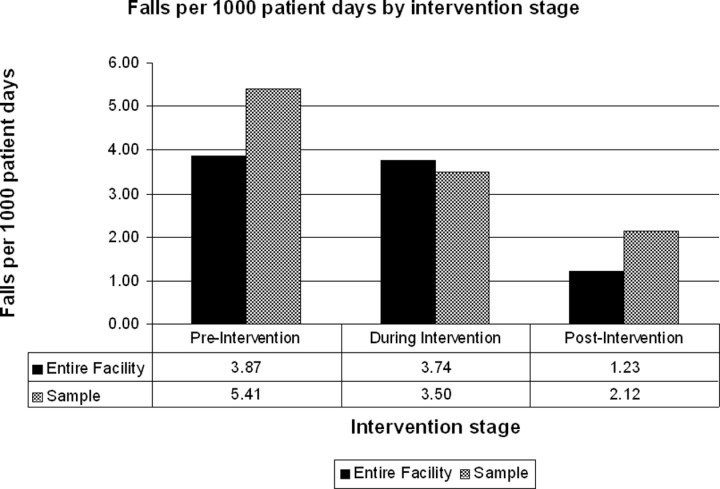
We collected information for 3720 patient days during the preintervention period, during which the incidence rate of falls was 5.41 falls per 1000 patient days. Some residents were involved in more than 1 fall, such that the mean percentage of residents involved in an incident was 12.09% ± 1.61% during the preintervention phase. Data collected during the intervention phase consisted of 2852 patient days, during which time 3.50 falls per 1000 patient days were observed. During the intervention period of the study, the mean percentage of residents who fell was 8.60% ± 1.86% (Figure 1 and Table 2 ). Finally, our postintervention phase monitored the incidence rate of falls over the course of 3782 patient days; the incidence rate of falls following the intervention fell to 2.12 falls per 1000 patient days and the percentage of residents involved in a fall was reduced to 6.45% ± 3.72% (Figure 1).
Figure 1.
Mean percentage of residents who fell as a function of time in both the entire population and the subpopulation. Results indicate the percentage of patients who fell during the observation period decreased over time, as the alarms were removed from the facility.
Table 2.
Summary of Number and Types of Falls of 31 Residents Included in Subset Analysis a
| Feb | March | April | May | June | July | Aug | Sept | Oct | Nov | Dec | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Type of fall | |||||||||||
| Slid from chair | 2 | 1 | 1 | 1 | |||||||
| Out of bed | 4 | 1 | 2 | 3 | 2 | 3 | 1 | 3 | |||
| Stood unassisted | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 3 | |||
| Lift total | 6 | 3 | 5 | 6 | 3 | 2 | 5 | 1 | 1 | 3 | 3 |
| Residents involved | 4 | 3 | 4 | 4 | 3 | 2 | 3 | 1 | 1 | 3 | 3 |
| Other falls b | |||||||||||
| Self-reported | 1 | ||||||||||
| During ambulation | 3 | 1 | 4 | 1 | 2 | 1 | 3 | 1 | |||
| Lowered to floor | 1 | 1 | 1 | 2 | 1 | 1 | |||||
| Almost fall | |||||||||||
| Total | 3 | 1 | 1 | 4 | 2 | 0 | 3 | 4 | 3 | 1 | 2 |
a Included those who resided within the facility during entirety of the observation period.
b Not included in the analysis.
Analysis of variance test results indicated no significant difference in the mean number of falls per 1000 patient days between the intervention stage and the pre- or postintervention stage. However, the mean number of falls prior to the removal of alarms (during the pre-intervention period) was significantly higher than the mean number of falls following the intervention (P = .03). Similarly, we observed no significant difference in the mean percentage of residents falling when comparing the intervention period to either the preintervention or postintervention periods. However, the mean percentage of residents who fell was significantly lower in the postintervention period when compared to the preintervention stage (P = .04). These results suggest that the removal of bed-exit and chair alarms was directly related to a decrease in the number of falls experienced by residents and the percentage of residents involved in those incidences.
We also report herein the number of falls that occurred in the facility within all of our residents, including those who joined during the period of observation. When considering the entire population, we still observed a decrease in the number of falls which occurred per 1000 patient days as a function of intervention stage (Table 3 ). Moreover, we also observed a decrease in the percentage of residents involved in those incidents as a function of time (Figure 2 ). We also analyzed data collected concerning the percentage of patients given antipsychotic medication during each intervention stage. Anecdotally, when considering the entire population of the facility during this time period, results of the mean percentage of residents using antipsychotic drugs by intervention stage indicated that the preintervention mean percentage (30.21%) was statistically different (P < .001) from the postintervention percentage mean (22.92%), but there were no differences between either the pre- or postintervention mean percentages of patients given antipsychotic medication when compared to the during intervention percentage mean (27.01%). However, when considering only those patients who were residents during the entire observation period, no significant differences were found in the use of antipsychotic medications. This suggests that our observation of the trend of antipsychotic use in the entire facility may have been an artifact of the admission of a greater number of patients who did not require this type of medication.
Table 3.
Analysis of Variance With Tukey Post Hoc Tests to Compare the Number of Falls per 1000 Patient Days Between Intervention Periods for the Entire Resident Population (n = 60) and Subpopulation (n = 31) a
| Entire Group | df 2, 8 | F 4.695 | P .04 | Sample | df 2, 8 | F 4.959 | P .04 |
|---|---|---|---|---|---|---|---|
| Mean Difference (I-J) | P | Mean Difference (I-J) | P | ||||
| Pre vs during | 0.13 | .99 | Pre vs during | 1.91 | .27 | ||
| During vs post | 2.24 | .09 | During vs post | 1.39 | .47 | ||
| Pre vs post | 2.64 | .05 | Pre vs post | 3.30 | .03 | ||
a Results indicate that significant differences (P ≤ 0.05) between the pre- and postintervention phases exist for the entire and subpopulation.
Figure 2.
Graphic representation of falls per 1000 patient days as a function of intervention stage. Depicted are the number of falls occurring in both the overall population and the longitudinal population (only those who resided in the facility during the entire observation period). Results show a trend for decreased number of falls as alarms were removed.
Discussion
The frequency of alarms in our facility was the driving force for our investigation because not only did we feel that staff may have become too dependent on the alarms for fall prevention, but the occurrence of these alarms was extremely disruptive to our residents, as well. In the climate of the “culture change” movement, it has become increasingly evident that attempting to create an environment which simulates a patient’s own home as closely as possible is quite promising. Research supports the removal of restraints and bedside rails, which would obviously never be used in the home. Likewise, an alarm which may sound during the night when the wearer simply changes sleeping position would not be acceptable for use in the home. Such disturbances in the middle of the night are likely to be perceived as a fire alarm or other similar emergency by a suddenly awakened, disoriented person. The result might be a reflexive response to flee, which could actually cause a fall that would not have occurred, as well as unnecessary stress. To our knowledge, no previous study has demonstrated the possible detrimental effects of position-change alarms in a long-term care facility.
The evidence presented here supports our hypothesis that bed-exit alarms do not contribute significantly to fall prevention, and they may even play an antagonistic role in this endeavor in a long-term care facility, particularly one whose residents have Alzheimer’s disease or dementia. Our data show that as we continued to remove the alarms from our patients, the incidence of falls in the facility decreased, which suggests that the frequency of the alarms sounding may have been related to the number of falls which occurred. It is important to consider the number of residents admitted to the facility during this time. It is understood that particularly in patients with Alzheimer’s or dementia, the first 24 hours after being admitted to a facility such as ours is the time in which the patient is at highest risk of falling. It is also important to consider that as our number of residents increased, even the actual number of falls decreased appreciably without statistical analysis. Prior to, and during the intervention period, we experienced an average of 6 falls per month, while the average number of falls after all alarms were removed was reduced to 3 falls per month. Though review of the raw data of our entire population seems to obviate our conclusions, it is important to consider only the population that resided in the facility during the entire observation period. It is possible that over time, more patients were admitted who had less risk of falling than those who were already residing within the facility, which would introduce bias to our study. Importantly, when we considered only those 31 residents who were present during all 3 stages of the intervention, we still observed a statistically significant reduction in the number of falls and the percentage of residents experiencing those falls. Of note, the number of falls recorded per 1000 patient days at all stages of the intervention (even preintervention) are remarkably lower than expected for a long-term care facility of this type.
Of particular interest were the results of observing the percentage of residents requiring antipsychotic medication as a function of the intervention. These results illustrate the possible bias that could be introduced by increasing the subject population in an uncontrolled fashion. Comparison of the percentage of all residents requiring antipsychotics suggests that the use of these medications decreased during the intervention. However, it became clear that these results did not translate to the subpopulation used for analysis; only 1 patient in this population discontinued antipsychotic medications during this research study. It is the opinion of the authors that the patients no longer being disrupted may positively affect their mental well-being. Enjoying a full night’s rest may change the affect of some residents, while it is also possible that due to the nature of these patients’ states of mind, the alarms may cause increased confusion and a great deal of anxiety. Further studies to investigate the effect of these alarms on patients’ medication needs and mental well-being are warranted.
Other positive results were observed by administration and staff after elimination of the bed-exit alarms, as well. The entire facility became a much quieter and calmer place for residents to live and for staff to work. The staff members began to become much more attuned to the needs of their patients once they ceased to rely on alarms. As there was no longer the need to respond to an alarm, when a patient did attempt to exit a bed or chair unassisted, the staff asked what the resident needed rather than telling them to sit back down. Anecdotally, the facility’s staff members have commented that the residents sleep better at night without the alarms, seem less agitated, and have exhibited fewer behaviors. Moreover, the staff members are no longer desensitized to the alarms, and now have become very proud of their facility and teammates for successfully removing them. Some staff members commented that they are no longer able to tolerate alarms in other facilities, and postintervention, they truly realize how disruptive the alarms were.
There are a number of limitations inherent in this research, particularly the fact that this study was a retrospective, uncontrolled before and after study. However, because this study was uncontrolled, the staff was unaware that the effects of eliminating the alarms were being monitored for research purposes, which may have resulted in less bias. One potential limitation of the study that could not be controlled was the fact that our study population changed over time as new residents were admitted to the facility. While we compensated for this by analyzing data pertaining only to the population that resided in the facility during the entire observation period, we could not account for other possible effects of admitting new patients during the study. It has been observed in our facility that a resident is at the greatest risk of falling within their first 24 hours of moving to the facility. Additionally, an increase in the number of residents changes the staff-to-patient ratio. Both of these factors could increase the burden on staff and indirectly affect the care they are able to provide the other residents, thus possibly affecting fall rates. The turnover rate in our facility also introduced a limitation to our study; longer observation periods would result in fewer residents being eligible for our subset of patients who were present throughout the entire study. Observing trends over longer periods of time is desirable but might include too few residents to gather meaningful conclusions.
So many factors affect fall rates that it is impossible to control for all of them, which is a major limitation of any study like ours. For example, our staff has noted that cold and flu season has been a time of increased falls in the facility, which could explain why the rate of falls peaked in November and December. Importantly, while we cannot control for all of the effects, it is still of value to appreciate the fact that these results, while perhaps not generalizable to all units within a health care facility, illustrate the real-world effects of bed-exit alarms in a long-term care facility which caters to patients with dementia or Alzheimer’s disease.
We do acknowledge and understand that bed-exit alarms alone are not meant to prevent falls and are to be used as only a component of an integrated plan to prevent falls in a health care facility. It has been our experience, however, that these alarms are disruptive and have not been effective as a component of our fall prevention endeavors. We did use alarms that sounded throughout the facility and appreciate that an alarm system which sends a signal directly to the nurses’ station or to a beeper worn by a nurse or other caregiver might be more effective. However, with our observation, we assert that these alarms may give a false sense of security and that patient care can be adjusted in a manner to better serve everyone involved.
Acknowledgement
The authors would like to thank the entire staff of the Goerlich Center for their participation in this endeavor. Without their continued support, the “Alarm Free” initiative would not have been so successful, and this research would not have been possible.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Lach HW. The costs and outcomes of falls: what’s a nursing administrator to do? Nurs Adm Q. 2010; 34(2): 147–155. [DOI] [PubMed] [Google Scholar]
- 2. Scott-Cawiezell J, Vogelsmeier A. Nursing home safety: a review of the literature. Annu Rev Nurs Res. 2006; 24: 179–215. [PubMed] [Google Scholar]
- 3. Pynoos J, Rose D, Rubenstein L, Choi IH, Sabata D. Evidence-based interventions in fall prevention. Home Health Care Serv Q. 2006; 25(1-2): 55–73. [DOI] [PubMed] [Google Scholar]
- 4. Johnson M, George A, Tran DT. Analysis of falls incidents: Nurse and patient preventive behaviours. Int J Nurs Pract. 2011; 17(1): 60–66. [DOI] [PubMed] [Google Scholar]
- 5. van Dijk PTM, Meulenberg OGRM, van de Sande HJ, Habbema JDF. Falls in Dementia Patients. Gerontologist. 1993; 33(2): 200–204. [DOI] [PubMed] [Google Scholar]
- 6. Harrison B, Booth D, Algase D. Studying fall risk factors among nursing home residents who fell. J Gerontol Nurs. 2001; 27(10): 26–34. [DOI] [PubMed] [Google Scholar]
- 7. Van Doorn C, Gruber-Baldini AL, Zimmerman S, et al. Dementia as a risk factor for falls and fall injuries among nursing home residents. J Am Geriatr Soc. 2003; 51(9): 1213–1218. [DOI] [PubMed] [Google Scholar]
- 8. Oliver D, Connelly JB, Victor CR, et al. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ. 2007; 334(7584): 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hilbe J, Schulc E, Linder B, Them C. Development and alarm threshold evaluation of a side rail integrated sensor technology for the prevention of falls. Int J Med Inform. 2010; 79(3): 173–180. [DOI] [PubMed] [Google Scholar]
- 10. Capezuti E, Maislin G, Strumpf N, Evans LK. Side rail use and bed-related fall outcomes among nursing home residents. J Am Geriatr Soc. 2002; 50(1): 90–96. [DOI] [PubMed] [Google Scholar]
- 11. Oliver D, Healey F, Haines TP. Preventing falls and fall-related injuries in hospitals. Clin Geriatr Med. 2010; 26(4): 645–692. [DOI] [PubMed] [Google Scholar]
- 12. Todd JF, Ruhl CE, Gross TP. Injury and death associated with hospital bed side-rails: reports to the US Food and Drug Administration from 1985 to 1995. Am J Public Health. 1997; 87(10): 1675–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Allen RS, Burgio LD, Fisher SE, Michael Hardin J, Shuster JL, Jr. Behavioral characteristics of agitated nursing home residents with dementia at the end of life. Gerontologist. 2005; 45(5): 661–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kwok T, Mok F, Chien WT, Tam E. Does access to bed-chair pressure sensors reduce physical restraint use in the rehabilitative care setting? J Clin Nurs. 2006; 15(5): 581–587. [DOI] [PubMed] [Google Scholar]
- 15. Williams J, Kaasalainen S, Hadjistavropoulos T, et al. A qualitative investigation of injurious falls in long-term care: perspectives of staff members. Disabil Rehabil. 2011; 33(5): 423–432. [DOI] [PubMed] [Google Scholar]
- 16. Bed exit alarms. Health Devices. 2004; 33(9): 305–330. [PubMed] [Google Scholar]
- 17. Bed-exit alarms. A component (but only a component) of fall prevention. Health Devices. 2004; 33(5): 157–168. [PubMed] [Google Scholar]
- 18. Capezuti E, Brush BL, Lane S, Rabinowitz HU, Secic M. Bed-exit alarm effectiveness. Arch Gerontol Geriatr. 2009; 49(1): 27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bruyneel M, Libert W, Ninane V. Detection of bed-exit events using a new wireless bed monitoring assistance. Int J Med Inform. 2011; 80(2): 127–132. [DOI] [PubMed] [Google Scholar]
- 20. Kelly KE, Phillips CL, Cain KC, Polissar NL, Kelly PB. Evaluation of a nonintrusive monitor to reduce falls in nursing home patients. J Am Med Dir Assoc. 2002; 3(6): 377–382. [DOI] [PubMed] [Google Scholar]
- 21. Fatal Falls: Lessons for the Future. Sentinel Event Alert. 2000; (14):1–3. [PubMed] [Google Scholar]
- 22. Tideiksaar R, Feiner CF, Maby J. Falls prevention: the efficacy of a bed alarm system in an acute-care setting. Mt Sinai J Med. 1993; 60(6): 522–527. [PubMed] [Google Scholar]
- 23. Block FE, Jr, Nuutinen L, Ballast B. Optimization of alarms: a study on alarm limits, alarm sounds, and false alarms, intended to reduce annoyance. J Clin Monit Comput. 1999; 15(2): 75–83. [DOI] [PubMed] [Google Scholar]
- 24. Edworthy J, Hellier E. Alarms and human behaviour: implications for medical alarms. Br J Anaesth. 2006; 97(1): 12–17. [DOI] [PubMed] [Google Scholar]
- 25. Garg R, Bhalotra AR, Goel N, Pruthi A, Bhadoria P, Anand R. Attitude of resident doctors towards intensive care units’ alarm settings. Indian J Anaesth. 2010; 54(6): 522–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. The hazards of alarm overload. Keeping excessive physiologic monitoring alarms from impeding care. Health Devices. 2007; 36(3): 73–83. [PubMed] [Google Scholar]
- 27. Rader J, Frank B, Brady C. Rethinking the Use of Position Change Alarms. Quality Partners of Rhode Island, The Quality Improvement Organization Support Center for Nursing Home Quality Improvement. 2007. [Google Scholar]