Abstract
Background
Folic acid supplementation is recommended for reducing the risk of birth defects. We aimed to assess the protective association of periconception folic acid supplements with birth defects in real-world setting.
Methods
This prospective, population-based cohort study utilized national preconception registered data of married Chinese couples planning a pregnancy within 6 months between 2010 and 2012 in Mainland China. Participated women are freely provided folic acid starting 3 months before conception till 3 months after conception. Birth defects were self-reported at 42 days postpartumn followup. R software (v4.0.2) was applied for statistical analyses.
Results
Complete data of 567,547 couples with pregnancy outcomes and folic acid supplementation were extracted for final analysis. A total of 74.7% women were with folic acid supplementation, and 599 birth defects were self-reported. The odd of birth defects was lower among women taking folic acid compared to their counterparts not taking (0.102% vs 0.116%, P < 0.001). In the multiple logistic regression analyses, the odd of birth defects was lower among couples with maternal folic acid supplementation (OR = 0.78, 95%CI: 0.66–0.95, P = 0.011), especially decreased odd of neural tube defects (NTDs) (OR = 0.56, 95%CI: 0.39–0.82, P = 0.003). This association was confirmed by 1:4 and 1:10 case control analysis. Odds of birth defects were significantly lower among women with folic acid supplementation more than 3 months before pregnancy (P < 0.001), and moreover, the odds of cleft (P = 0.007) and NTDs (P = 0.007) were of notable decrease.
Conclusion
This retrospective case cohort study provides programmatic evidence for public health strategy-making to for reducing the risk of NTDs and clefts.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-024-06283-8.
Keywords: Folic acid supplementation; Birth defects; Neural tubal defects; Clefts, congenital heart disease; China
Introduction
Periconception folic acid supplementation is a primary prevention intervention for reducing the risk of birth defects especially neural tube defects (NTDs) [1]. Early randomized controlled studies (RCTs) and cohort studies provided consistent beneficial evidence, which initiated from Hungarian randomized clinical trial in 1984, to cohort studies between 1984 and 1996 [2, 3]. Moreover, the US Preventive Service Task Force (USPSTF) recommended all women planning a pregnancy taking a daily dosage of 0.4–0.8 mg folic acid in 2009 [4–6]. However, the benefits of folic acid supplementation as a primary care are required to be informed.
In current postfortification era, there lacks new prospective studies to evaluate the benefits of folic acid supplement among women with pregnancy intention as a public health intervention [7]. Moreover, subsequent observational, case-control studies have not shown a protective association with birth defects such as NTDs [8]. These inconsistent protective association may be attenuated by greater controls for potential sources of bias, misclassification or recall bias. The potential for recall bias or difference by timing or duration of therapy, may attenuate the measured association. Despite of some known confounding including maternal age, education, smoking and alcohol consumption, other possible paternal factors should also be taken into consideration such as smoking and alcohol drinking. Additionally, placebo-controlled randomized trials that eliminate folic acid is challenging for the ethical consideration. Consequently, qualified prospective studies are scared to demonstrate a protective association of folic acid supplement among women with pregnancy intention as a real-world maternal health care.
Early randomized clinical and cohort studies provided consistent evidence of its benefit, but potentially offered greater controls for potential sources of bias, and ethical considerations for precluding placebo-controlled randomized trials that eliminate folic acid. Consequently, in the postfortification era, subsequent observational, case-control studies did not show a protective association with birth defects such as NTDs [8]. The potential for recall bias or difference by timing or duration of therapy, may attenuate the measured association. Additionally, despite of some known maternal confounding including age, education, occupation, smoking and alcohol consumption, these paternal factors should also be taken into consideration.
The Chinese government has launched the National Free Preconception Health Examination Project (NFPHEP) in 2010, in which, women planning a pregnancy within 6 months are freely provided take a daily 0.4 mg supplement of periconception folic acid. In this nation-wide public health care project, the timing and duration of folic acid supplementation, and pregnancy outcomes are followup. Nearly 74.7% women planning a pregnancy took folic acid supplemental before pregnancy [9, 10], and thus, this prospective cohort study provided an optimal opportunity for assessing the protective association of periconception folic acid supplements with NTDs, together with other birth defects, including clefts, congenital heart disease, limb anomalies, digestive tract anomalies, gastroschisis as well.
Materials and methods
Study design and participants
This prospective, population-based cohort study utilized NFPHEP database, which collected from couples intending to conceive within 6 months, covering 220 counties or districts across 31 provinces and province-level municipalities in mainland China during 2010–2012 [9, 10]. Married couples planning a pregnancy were freely provided with a preconception education and advocacy program on reproductive health by local family planning service agencies or maternal and children’s care service centers. Couples planning a pregnancy within 6 months with the wife’s age between 20 and 49 years, were included. Those women with incomplete information regarding folic acid supplementation or pregnancy outcomes, were excluded from the final analysis. This study followed the Strengthening and Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Data collection
Specialized community healthcare staff inquired about the pregnancy intention of married couples residing in their community and provided them with preconception health examinations. Trained health care personnel conducted a face-to-face interview and medical examination. Enrolled women are freely provided 0.4 mg/d supplement of folic acid starting 3 months before conception till 3 months after conception. Their medical examination and follow-up data are uploaded and stored in the NFPHEP medical service information system. Detailed design, organization, and implementation of this project are described elsewhere [9, 10].
Variables
The information of folic acid supplementation, socio-demographic and clinical information, including maternal and paternal age, education, occupation, residence status, exposure to harmful substances (smoking, toxic substances, noise, cats and dogs), maternal adverse pregnancy history (previous spontaneous abortion, fetal death, stillbirth, and preterm birth), wives with birth defects, were collected using standard questionnaires, and were extracted for analysis.
Information about maternal folic acid supplementation (taking/no taking), including its timing (≥3 months before conception, < 3 months before conception, after conception and no taking), was collected. The definitions of exposure to smoking, toxic substances, noise, cats and dogs, were categorized as yes and no. Passive smoking and alcohol consumption status was categorized as no, occasionally and often. The amount of alcohol consumed was not recorded, as Chinese people habitually consume alcohol from different containers and therefore the exact amount of alcohol ingested is difficult to record.
Outcomes and measurements
The primary outcome was the incidence of birth defects. Birth defects were reported by parents or medical staff at 42 days postpartumn followup. Secondary outcomes were the top six types of birth defects, including congenital heart disease, limb anomalies (including syndactyly, polydactyly and congenital club foot), clefts (including cleft lip and cleft palate), digestive tract anomalies (including duodenal atresia, esophageal atresia stenosis, anorectal atresia, intestinal atresia, congenital diaphragmatic hernia, congenital megacolon and congenital intestinal obstruction), gastroschisis and neural tube defects (including spina bifida, anencephaly, congenital hydrocephalus, encephalocoele, hemicardiac malformation, cerebral haemangioma and brain dysplasia). Other types of birth defects were not included for subgroup analysis.
Statistical analysis
We used numbers and proportions to describe the participants’ socio-demographic and clinical characteristics. Differences in baseline characteristics between with and without birth defects groups were examined using the χ2 test. To minimize bias, multiple logistic regression analysis and case-control analysis were conducted. Associated featured confounders including maternal and paternal age, education, occupation and residence, were adjusted. Matching was based upon maternal age, education, province, alcohol consumption and smoking behavior, and paternal alcohol consumption and smoking behavior (Table S1). Odds ratio (ORs) were adjusted by 31 associated featured confounders, and maternal and paternal age, education, occupation and residence. Statistical analyses were performed using R software (version 4.0.2; https://www.r-project.org). Two-sided P-values < 0.05 were considered statistically significant.
Results
Enrollment of participants
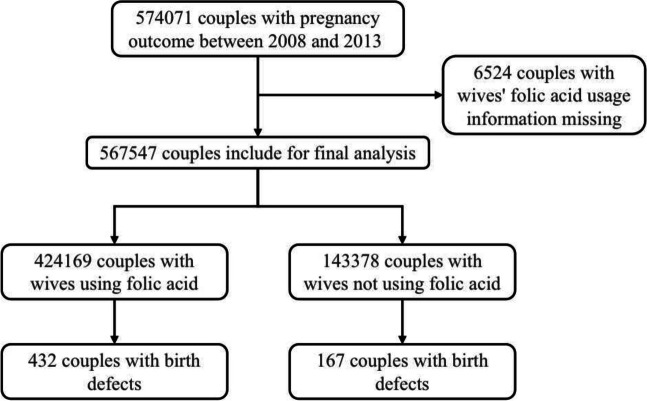
During the enrollment of the national preconception care project between 2010 and 2012, a total of 574,071 married couples intending to conceive with pregnancy outcomes were enrolled. Complete data of 567,547 couples with folic acid supplementation were extracted for final analysis, and data were missed in 6524 (1.1%) couples (Fig. 1). Baseline parameters between included and excluded couples were compared (Table S1).
Fig. 1.
Enrollment of the participating couples
Notably high portion of folic acid fortification among married women was observed (Table 1). In total, 424,169 (74.7%) were classified with folic acid supplementation (212,740 (37.5%) ≥3 months before conception, 83,765 (14.8%) < 3 months before conception, 127,232 (22.4%) after conception), and 143,378 (25.3%) with no folic acid intaking. Baseline parameters between couples with and without birth defects were compared (Table 1). Maternal adverse pregnancy history, anemia, using contraception, previous adverse pregnancy history, maternal and paternal exposure to passive smoking/toxic substances/noise/dogs and cats, vaginal bleeding/influenza/using drugs in early pregnancy were more frequent among couples with birth defects (P < 0.05).
Table 1.
General parameters of total participated couples and case-controlled couples
| Total couples | Case-controlled couples (1:4) | Case-controlled couples (1:10) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| No birth defects | Birth defects | P value | No birth defects | Birth defects | P value | No birth defects | Birth defects | P value | |
| (N = 566,948) | (N = 599) | (N = 2396) | (N = 599) | (N = 5990) | (N = 599) | ||||
| Maternal age (years) | 0.094 | 0.706 | 0.833 | ||||||
| 20–24 | 139,837 (24.66) | 142 (23.71) | 540 (22.54) | 142 (23.71) | 1354 (22.60) | 142 (23.71) | |||
| 25–29 | 282,041 (49.75) | 300 (50.08) | 1170 (48.83) | 300 (50.08) | 2930 (48.91) | 300 (50.08) | |||
| 30–34 | 107,784 (19.01) | 101 (16.86) | 528 (22.04) | 101 (16.86) | 1307 (21.82) | 101 (16.86) | |||
| 35–39 | 28,824 (5.08) | 46 (7.68) | 131 (5.47) | 46 (7.68) | 310 (5.18) | 46 (7.68) | |||
| ≥ 40 | 8462 (1.49) | 10 (1.67) | 27 (1.13) | 10 (1.67) | 89 (1.49) | 10 (1.67) | |||
| Paternal age (years) | 0.101 | 0.962 | 0.993 | ||||||
| 20–24 | 44,522 (7.85) | 50 (8.35) | 166 (6.93) | 50 (8.35) | 392 (6.54) | 50 (8.35) | |||
| 25–29 | 283,375 (49.98) | 276 (46.08) | 1151 (48.04) | 276 (46.08) | 2892 (48.28) | 276 (46.08) | |||
| 30–34 | 161,582 (28.50) | 179 (29.88) | 711 (29.67) | 179 (29.88) | 1794 (29.95) | 179 (29.88) | |||
| 35–39 | 56,112 (9.90) | 66 (11.02) | 274 (11.44) | 66 (11.02) | 663 (11.07) | 66 (11.02) | |||
| ≥ 40 | 21,357 (3.77) | 28 (4.67) | 94 (3.92) | 28 (4.67) | 249 (4.16) | 28 (4.67) | |||
| Maternal education | / | / | |||||||
| Illiteracy | 1178 (0.21) | 1 (0.17) | 1.000 | 8 (0.33) | 1 (0.17) | 0.698 | 20 (0.33) | 1 (0.17) | 0.716 |
| Primary school | 24,503 (4.32) | 32 (5.34) | 0.226 | 127 (5.30) | 32 (5.34) | 1.000 | 318 (5.31) | 32 (5.34) | 0.924 |
| Secondary school | 368,259 (64.95) | 390 (65.11) | 0.966 | 1555 (64.90) | 390 (65.11) | 0.962 | 3893 (64.99) | 390 (65.11) | 0.964 |
| High school | 113,230 (19.97) | 106 (17.70) | 0.168 | 418 (17.45) | 106 (17.70) | 0.904 | 1043 (17.41) | 106 (17.70) | 0.865 |
| College or undergraduate | 58,952 (10.40) | 70 (11.69) | 0.315 | 283 (11.81) | 70 (11.69) | 1.000 | 701 (11.70) | 70 (11.69) | 1.000 |
| Postgraduate or above | 826 (0.15) | 0 (0.00) | 1.000 | 5 (0.21) | 0 (0.00) | 0.590 | 15 (0.25) | 0 (0.00) | 0.389 |
| Paternal education | / | / | / | ||||||
| Illiteracy | 558 (0.10) | 1 (0.17) | 0.446 | 8 (0.33) | 1 (0.17) | 0.698 | 14 (0.23) | 1 (0.17) | 1.000 |
| Primary school | 21,330 (3.76) | 28 (4.67) | 0.236 | 125 (5.22) | 28 (4.67) | 0.678 | 281 (4.69) | 28 (4.67) | 1.000 |
| Secondary school | 356,604 (62.90) | 383 (63.94) | 0.612 | 1495 (62.40) | 383 (63.94) | 0.509 | 3761 (62.79) | 383 (63.94) | 0.595 |
| High school | 122,920 (21.68) | 109 (18.20) | 0.042 | 465 (19.41) | 109 (18.20) | 0.524 | 1179 (19.68) | 109 (18.20) | 0.418 |
| College or undergraduate | 64,271 (11.34) | 77 (12.85) | 0.246 | 298 (12.44) | 77 (12.85) | 0.783 | 741 (12.37) | 77 (12.85) | 0.745 |
| Postgraduate or above | 1265 (0.22) | 1 (0.17) | 1.000 | 5 (0.21) | 1 (0.17) | 1.000 | 14 (0.23) | 1 (0.17) | 1.000 |
| Maternal occupation | / | / | / | ||||||
| Farmers | 432,297 (76.25) | 444 (74.12) | 0.230 | 1765 (73.66) | 444 (74.12) | 0.836 | 4444 (74.19) | 444 (74.12) | 0.961 |
| Workers | 56,391 (9.95) | 54 (9.02) | 0.494 | 242 (10.10) | 54 (9.02) | 0.445 | 615 (10.27) | 54 (9.02) | 0.357 |
| Service officer | 22,107 (3.90) | 24 (4.01) | 0.833 | 102 (4.26) | 24 (4.01) | 0.909 | 226 (3.77) | 24 (4.01) | 0.737 |
| Business | 11,154 (1.97) | 13 (2.17) | 0.658 | 46 (1.92) | 13 (2.17) | 0.742 | 108 (1.80) | 13 (2.17) | 0.522 |
| Housewife | 12,188 (2.15) | 16 (2.67) | 0.395 | 60 (2.50) | 16 (2.67) | 0.773 | 139 (2.32) | 16 (2.67) | 0.571 |
| Teachers/officials | 21,487 (3.79) | 31 (5.18) | 0.085 | 121 (5.05) | 31 (5.18) | 0.917 | 304 (5.08) | 31 (5.18) | 0.922 |
| Others | 11,324 (2.00) | 17 (2.84) | 0.142 | 60 (2.50) | 17 (2.84) | 0.665 | 154 (2.57) | 17 (2.84) | 0.685 |
| Paternal occupation | / | / | / | ||||||
| Farmers | 420,794 (74.22) | 425 (70.95) | 0.068 | 1719 (71.74) | 425 (70.95) | 0.723 | 4325 (72.2) | 425 (70.95) | 0.535 |
| Workers | 71,968 (12.69) | 77 (12.85) | 0.902 | 312 (13.02) | 77 (12.85) | 0.946 | 772 (12.89) | 77 (12.85) | 1.000 |
| Service officer | 19,821 (3.50) | 19 (3.17) | 0.823 | 97 (4.05) | 19 (3.17) | 0.346 | 217 (3.62) | 19 (3.17) | 0.645 |
| Business | 19,509 (3.44) | 22 (3.67) | 0.736 | 87 (3.63) | 22 (3.67) | 1.000 | 212 (3.54) | 22 (3.67) | 0.817 |
| Househusband | 778 (0.14) | 0 (0.00) | 1.000 | 6 (0.25) | 0 (0.00) | 0.606 | 13 (0.22) | 0 (0.00) | 0.623 |
| Teachers/officials | 20,316 (3.58) | 35 (5.84) | 0.006 | 98 (4.09) | 35 (5.84) | 0.075 | 259 (4.32) | 35 (5.84) | 0.096 |
| Others | 13,762 (2.43) | 21 (3.51) | 0.108 | 77 (3.21) | 21 (3.51) | 0.701 | 192 (3.21) | 21 (3.51) | 0.716 |
| Maternal residence status | 0.931 | 0.522 | 0.665 | ||||||
| Rural | 533,260 (94.06) | 563 (93.99) | 2232 (93.16) | 563 (93.99) | 5594 (93.39) | 563 (93.99) | |||
| Urban | 33,688 (5.94) | 36 (6.01) | 164 (6.84) | 36 (6.01) | 396 (6.61) | 36 (6.01) | |||
| Paternal residence status | 0.180 | 1.000 | 1.000 | ||||||
| Rural | 525,830 (92.75) | 547 (91.32) | 2186 (91.24) | 547 (91.32) | 5471 (91.34) | 547 (91.32) | |||
| Urban | 41,118 (7.25) | 52 (8.68) | 210 (8.76) | 52 (8.68) | 519 (8.66) | 52 (8.68) | |||
| Maternal adverse pregnancy history | 6.46e-5 | 0.469 | 0.631 | ||||||
| Yes | 15,244 (2.69) | 34 (5.68) | 119 (4.97) | 34 (5.68) | 312 (5.21) | 34 (5.68) | |||
| No | 551,704 (97.31) | 565 (94.32) | 2277 (95.03) | 565 (94.32) | 5678 (94.79) | 565 (94.32) | |||
| Wives with birth defects | 0.001 | 1.000 | 1.000 | ||||||
| Yes | 1070 (0.19) | 6 (1.00) | 27 (1.13) | 6 (1.00) | 69 (1.15) | 6 (1.00) | |||
| No | 565,878 (99.81) | 593 (99.00) | 2369 (98.87) | 593 (99.00) | 5921 (98.85) | 593 (99.00) | |||
| Maternal passive smoking | / | / | / | ||||||
| No | 474,858 (83.76) | 461 (76.96) | 1.83e-5 | 1833 (76.5) | 461 (76.96) | 0.829 | 4575 (76.38) | 461 (76.96) | 0.801 |
| Occasionally | 81,755 (14.42) | 117 (19.53) | 5.85e-4 | 482 (20.12) | 117 (19.53) | 0.775 | 1199 (20.02) | 117 (19.53) | 0.830 |
| Often | 10,335 (1.82) | 21 (3.51) | 0.005 | 81 (3.38) | 21 (3.51) | 0.900 | 216 (3.61) | 21 (3.51) | 1.000 |
| Maternal exposed to toxic substances | 5.96e-4 | 0.467 | 1.000 | ||||||
| Yes | 36,581 (6.45) | 61 (10.18) | 272 (11.35) | 61 (10.18) | 616 (10.28) | 61 (10.18) | |||
| No | 530,367 (93.55) | 538 (89.82) | 2124 (88.65) | 538 (89.82) | 5374 (89.72) | 538 (89.82) | |||
| Maternal exposed to noise | 5.76e-4 | 1.000 | 1.000 | ||||||
| Yes | 6952 (1.23) | 18 (3.01) | 74 (3.09) | 18 (3.01) | 188 (3.14) | 18 (3.01) | |||
| No | 559,996 (98.77) | 581 (96.99) | 2322 (96.91) | 581 (96.99) | 5802 (96.86) | 581 (96.99) | |||
| Maternal exposure to cats and dogs | 1.63e-4 | 0.640 | 0.745 | ||||||
| Yes | 10,964 (1.93) | 26 (4.34) | 93 (3.88) | 26 (4.34) | 244 (4.07) | 26 (4.34) | |||
| No | 555,984 (98.07) | 573 (95.66) | 2303 (96.12) | 573 (95.66) | 5746 (95.93) | 573 (95.66) | |||
| Paternal smoking | 3.04e-5 | 0.888 | 0.860 | ||||||
| Yes | 167,938 (29.62) | 225 (37.56) | 908 (37.90) | 225 (37.56) | 2275 (37.98) | 225 (37.56) | |||
| No | 399,010 (70.38) | 374 (62.44) | 1488 (62.10) | 374 (62.44) | 3715 (62.02) | 374 (62.44) | |||
| Paternal passive smoking | / | / | / | ||||||
| No | 401,575 (70.83) | 375 (62.6) | 1.51e-5 | 1487 (62.06) | 375 (62.6) | 0.814 | 3711 (61.95) | 375 (62.6) | 0.791 |
| Occasionally | 148,097 (26.12) | 192 (32.05) | 0.001 | 781 (32.6) | 192 (32.05) | 0.845 | 1926 (32.15) | 192 (32.05) | 1.000 |
| Often | 17,276 (3.05) | 32 (5.34) | 0.003 | 128 (5.34) | 32 (5.34) | 1.000 | 353 (5.89) | 32 (5.34) | 0.648 |
| Paternal alcohol consumption | / | / | / | ||||||
| No | 392,995 (69.32) | 356 (59.43) | 3.14e-7 | 1439 (60.06) | 356 (59.43) | 0.780 | 3549 (59.25) | 356 (59.43) | 0.965 |
| Occasionally | 166,814 (29.42) | 233 (38.90) | 7.38e-7 | 918 (38.31) | 233 (38.9) | 0.814 | 2340 (39.07) | 233 (38.9) | 0.965 |
| Often | 7139 (1.26) | 10 (1.67) | 0.355 | 39 (1.63) | 10 (1.67) | 1.0 | 101 (1.69) | 10 (1.67) | 1.0 |
| Paternal exposed to toxic substances | 5.0e-7 | 0.734 | 0.900 | ||||||
| Yes | 42,266 (7.46) | 80 (13.36) | 308 (12.85) | 80 (13.36) | 789 (13.17) | 80 (13.36) | |||
| No | 524,682 (92.54) | 519 (86.64) | 2088 (87.15) | 519 (86.64) | 5201 (86.83) | 519 (86.64) | |||
| Maternal folic acid supplementation | 0.145 | 0.039 | 0.024 | ||||||
| Taking | 423,737 (74.74) | 432 (72.12) | 1827 (76.25) | 432 (72.12) | 4573 (76.34) | 432 (72.12) | |||
| No taking | 143,211 (25.26) | 167 (27.88) | 569 (23.75) | 167 (27.88) | 1417 (23.66) | 167 (27.88) | |||
| Folic acid timing | |||||||||
| ≥ 3 months before conception | 212,740 (37.52) | 163 (27.21) | 1.18e-7 | 852 (35.56) | 163 (27.21) | 1.11e-4 | 2116 (35.33) | 163 (27.21) | 5.92e-5 |
| < 3 months before conception | 83,765 (14.77) | 97 (16.19) | 0.327 | 426 (17.78) | 97 (16.19) | 0.400 | 1066 (17.8) | 97 (16.19) | 0.400 |
| After conception | 127,232 (22.44) | 172 (28.71) | 3.40e-4 | 549 (22.91) | 172 (28.71) | 0.003 | 1391 (23.22) | 172 (28.71) | 0.003 |
| No taking | 143,211 (25.26) | 167 (27.88) | 0.145 | 569 (23.75) | 167 (27.88) | 0.039 | 1417 (23.66) | 167 (27.88) | 0.024 |
Data were presented as mean (standard deviation)
Matching was based upon maternal age, educational level, province, alcohol consumption and smoking behavior, and paternal alcohol consumption and smoking behavior
Association of folic acid supplementation with reduced odds of birth defects
A total of 599 birth defects were self-reported. Rate of birth defects was statistically discordant: it was lower among women taking folic acid compared to their counterparts not taking (0.102% vs 0.116%, P < 0.001) (Table 2). In the multiple logistic regression analyses, the odds of birth defects was lower among couples with maternal folic acid supplementation (OR = 0.78, 95%CI: 0.66–0.95, P = 0.011), especially that odds of NTDs (OR = 0.55, 95%CI: 0.39–0.82, P = 0.003). This association was confirmed by 1:4 and 1:10 case control analysis.
Table 2.
Risk odds of birth defects related with maternal folic acid supplementation and based on different folic acid timing
| FA/NFA | Total couples | Case-controlled couples (1:4) | Case-controlled couples (1:10) | ||||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | ||
| Folic acid supplementation* | |||||||
| Total birth defects | 432/167 | 0.78 (0.66,0.95) | 0.011 | 0.81 (0.66,0.99) | 0.044 | 0.81 (0.67,0.98) | 0.033 |
| Congenital heart disease | 110/41 | 0.80 (0.55,1.16) | 0.237 | 0.88 (0.59,1.33) | 0.551 | 0.83 (0.57,1.22) | 0.342 |
| Limb anomalies | 37/15 | 0.95 (0.50,1.80) | 0.874 | 0.95 (0.46,1.96) | 0.882 | 0.84 (0.44,1.58) | 0.584 |
| Clefts | 73/33 | 0.72 (0.47,1.11) | 0.136 | 0.66 (0.41,1.04) | 0.075 | 0.69 (0.44,1.06) | 0.086 |
| Digestive tract anomalies | 32/12 | 0.69 (0.36,1.32) | 0.265 | 1.08 (0.53,2.23) | 0.827 | 0.93 (0.46,1.88) | 0.844 |
| Neural tube defects | 82/42 | 0.56 (0.39,0.82) | 0.003 | 0.56 (0.37,0.86) | 0.008 | 0.63 (0.42,0.93) | 0.019 |
| Gastroschisis | 64/19 | 1.03 (0.61,1.75) | 0.915 | 1.02 (0.57,1.83) | 0.953 | 0.96 (0.56,1.66) | 0.878 |
| Folic acid supplementation ≥ 3 months before pregnancy | |||||||
| Total birth defects | 163/167 | 0.60 (0.48,0.75) | < 0.001 | 0.63 (0.49,0.80) | < 0.001 | 0.66 (0.53,0.83) | < 0.001 |
| Congenital heart disease | 42/41 | 0.63 (0.41,0.97) | 0.036 | 0.73 (0.45,1.18) | 0.197 | 0.73 (0.46,1.14) | 0.167 |
| Limb anomalies | 12/15 | 0.51 (0.24,1.12) | 0.093 | 0.69 (0.28,1.70) | 0.415 | 0.61 (0.27,1.35) | 0.220 |
| Clefts | 22/33 | 0.47 (0.27,0.82) | 0.007 | 0.45 (0.25,0.82) | 0.008 | 0.46 (0.26,0.80) | 0.006 |
| Digestive tract anomalies | 13/12 | 0.62 (0.27,1.40) | 0.251 | 0.90 (0.38,2.09) | 0.798 | 0.80 (0.35,1.83) | 0.597 |
| Neural tube defects | 38/42 | 0.55 (0.36,0.85) | 0.007 | 0.51 (0.31,0.85) | 0.009 | 0.61 (0.38,0.96) | 0.034 |
| Gastroschisis | 30/19 | 0.97 (0.54,1.73) | 0.913 | 0.99 (0.51,1.91) | 0.966 | 0.94 (0.81,1.73) | 0.833 |
| Folic acid supplementation < 3 months before pregnancy | |||||||
| Total birth defects | 97/167 | 0.82 (0.64,1.06) | 0.134 | 0.89 (0.67,1.18) | 0.407 | 0.85 (0.65,1.11) | 0.337 |
| Congenital heart disease | 24/41 | 0.65 (0.39,1.11) | 0.115 | 0.88 (0.50,1.55) | 0.652 | 0.76 (0.45,1.30) | 0.321 |
| Limb anomalies | 10/15 | 0.94 (0.41,2.18) | 0.888 | 0.98 (0.38,2.52) | 0.961 | 0.97 (0.42,2.23) | 0.934 |
| Clefts | 19/33 | 0.82 (0.46,1.48) | 0.515 | 0.87 (0.45,1.67) | 0.668 | 0.83 (0.46,1.50) | 0.532 |
| Digestive tract anomalies | 8/12 | 0.84 (0.32,2.21) | 0.720 | 1.21 (0.46,3.21) | 0.701 | 1.09 (0.42,2.79) | 0.865 |
| Neural tube defects | 16/42 | 0.43 (0.23,0.81) | 0.008 | 0.56 (0.30,1.06) | 0.076 | 0.58 (0.32,1.06) | 0.075 |
| Gastroschisis | 97/167 | 0.75 (0.34,1.62) | 0.463 | 1.13 (0.51,2.50) | 0.755 | 1.04 (0.49,2.18) | 0.924 |
| Folic acid supplementation after pregnancy | |||||||
| Total birth defects | 172/167 | 1.02 (0.82,1.27) | 0.870 | 1.06 (0.83,1.35) | 0.671 | 1.02 (0.82,1.29) | 0.838 |
| Congenital heart disease | 44/41 | 0.90 (0.58,1.39) | 0.637 | 1.16 (0.71,1.91) | 0.552 | 1.03 (0.66,1.63) | 0.884 |
| Limb anomalies | 15/15 | 1.02 (0.50,2.11) | 0.949 | 1.18 (0.51,2.71) | 0.670 | 1.05 (0.50,2.24) | 0.893 |
| Clefts | 32/33 | 0.97 (0.59,1.61) | 0.909 | 0.84 (0.48,1.46) | 0.531 | 0.93 (0.55,1.56) | 0.782 |
| Digestive tract anomalies | 11/12 | 0.92 (0.39,2.17) | 0.854 | 1.32 (0.53,3.28) | 0.546 | 1.02 (0.43,2.39) | 0.967 |
| Neural tube defects | 28/42 | 0.62 (0.38,1.01) | 0.055 | 0.64 (0.37,1.10) | 0.105 | 0.69 (0.42,1.15) | 0.151 |
| Gastroschisis | 21/19 | 1.04 (0.55,1.96) | 0.910 | 1.00 (0.50,2.00) | 0.992 | 0.95 (0.49,1.83) | 0.870 |
*:including folic acid supplementation ≥3 months before pregnancy, < 3 months before pregnancy and after pregnancy
FA/NFA folic acid usage / non folic acid usage. OR odd ratio, CI confidence interval
Matching was based upon maternal age, educational level, province, alcohol consumption and smoking behavior, and paternal alcohol consumption and smoking behavior
ORs were adjusted by maternal and paternal age, education, occupation and residence
Effect of folic acid supplementation timing and dosage on reducing the odds of birth defects
Regarding folic acid timing, among women who took folic acid supplements ≥3 months months before conception, < 3 months before conception, after conception, and those who did not take the supplements, odds of birth defects were significantly lower among women with folic acid supplementation ≥3 months before pregnancy (OR = 0.60, 95%CI: 0.48–0.75, P < 0.001), together with lower odds of clefts (OR = 0.47, 95%CI: 0.27–0.82, P = 0.007) and NTDs (OR = 0.55, 95%CI: 0.36–0.85, P = 0.007), which was consistent in 1:4 and 1:10 case-control analysis (Table 2).
In addition, the effect of folic acid supplementation on birth defects were confirmed by comparing women who took before conception with those who didn’t take folic acid (OR = 0.68, 95%CI: 0.56–0.83, P < 0.001), while this effect was not statistically significant between women who took after conception with those who didn’t take folic acid (P > 0.05).
In addition, the odds of clefts was significantly decreased among couples with maternal folic acid supplementation before conception (OR = 0.59, 95%CI: 0.36–0.95, P = 0.029) and this odd was of no difference when comparing women who took after conception with those who didn’t take folic acid (P > 0.05) (Table S2).
Comment
Principle findings
In the postfortification era, the benefits of preconceptional folic acid supplementation on reducing the odds of birth defects require comprehensive consideration before implementation. This study is one of the first prospective cohorts providing essential, real-world evidence that, preconceptional folic acid supplementation of 0.4 mg/d dosage is protective for reducing the odds of offspring’s birth defects. With the great maternal health investment from Chinese government, periconceptional folic acid intake has achieved a high coverage among women with pregnancy intention [9]. Our findings are important for continuous efforts for promoting this public health policy for reducing the risk of some birth defects such as NTDs and clefts.
Results
In this large programmatic evaluation of periconception folic acid supplementation strategy, the comparative effectiveness on reducing the risk of birth defect was estimated in 574,071 married couples in Mainland China. We found that wives who in-took folic acid before conception had lower odds of cleft and NTDs. Folic acid supplementation might substantially decrease the risk of some types of common birth defects, especially with regular and full-term supplementation at least 3 months before conception and in the early 3 months of pregnancy.
Clinical implications
Our findings support periconception folic acid supplementation as an essential component of preconception care and indicate that folic acid might be beneficial for reducing the odds of NTDs and cleft, which is in agreement with evidence from previous randomized trials and cohorts [11–16]. These findings might be useful for maternal health care considering implementation of folic acid supplementation to reduce the risk of birth defects. Further studies are required to elucidate whether folic acid supplements be used consistently over the periods demarcated and whether our women be asked to take the supplements throughout pregnancy or only up to a certain point.
Research implications
Second, we found that folic acid supplementation of 0.4 mg/d dosage before pregnancy appeared to be protective for reducing the risks of offspring’s birth defects including clefts and NTDs. Due to concerns about potential adverse effects, this lower dosage is commonly recommended in many countries including high-income countries, which was much lower than in the previous RCTs for NTDs [2, 3]. However, the key question should be addressed is the efficacy of this low dosage has not been well tested in previous randomized or cohort studies [17, 18]. Therefore, our study provided real-world evidence for evaluating the efficacy of the 0.4 mg/d dosage.
Strengths and limitations
The main strength of this study is the use of data from the Chinese nation-wide preconception care database, characterized by high folic acid supplementation rate, adjusted associated maternal and paternal parameters, and matched known possible interfering factors, gave the power to detect subtle effect of folic acid supplementation. First, our dataset is reliable since it is based on prospective enrollment and nationwide coverage, with more than 85% coverage of couples intending to conceive and less than 10% missing data rate. Second, our study sample is vigorous, which has enrolled more than 2 million couples spanning 220 rural areas across all 31 provinces in mainland China. Third, this Chinese preconception health care strategy providing free folic acid supplementation seems feasible and well-implemented, assuring nearly 75% folic acid supplementation rate, compared to approximately 30–50% reported in the United States and some European countries [19], which was relatively lower than that in this study. Fourth, our protective association of folic acid supplementation with reducing birth defects was analyzed by conditional logistic regression and case-control analysis to minimize bias. A total of 31 associated featured items, together with some recognized confounders (including maternal and paternal age, education, occupation and residence), were adjusted.
Our study had some limitations. First, a definite causal relationship cannot be inferred from the cohort design, and a well-designed randomized study to evaluate folic acid fortification on reducing the risk of birth defects is difficult due to ethical considerations. Nevertheless, this prospective cohort seems more feasible, and the database used in the present study is ideal for analyzing their association. Second, there was a possible recall bias of the dosage and duration of folic acid supplementation and the prevalence of birth defects may be underestimated, considering that these pregnancy related information was based on questionnaires. To account for confounding effect, conditional logistic regression analysis featured with associated factors was simultaneously conducted to minimize bias. Third,
Our outcomes of birth defects were based on self-report at 42 days, which could lead to substantial misclassification as well as missing some birth defects. We have conducted 1:4 and 1:10 case-control analysis were simultaneously conducted to minimize bias, and the results of reduced risk association were confirmed.
Conclusions
In summary, given the priority of periconception folic acid supplementation, our study provides programmatic evidence for public health strategy-making to improve offspring’s birth outcomes and life quality.
Supplementary Information
Acknowledgements
We thank the health workers in the 220 counties of the 31 provinces for their strong collaboration and great efforts made as part of the National Free Preconception Health Examination Project. The authors have no conflicts of interest to declare.
Conflict of interest
The authors have no conflicts of interest to disclose. All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
Financial disclosure
No financial disclosures were reported by the authors of this paper.
Abbreviations
- NPHCP
the National preconception health care project
- NTDs
Neural tube defects
- ORs
Odds ratio
- RCT
Randomized controlled study
- STROBE
the Strengthening and reporting of observational studies in epidemiology
- USPSTF
the US preventive service task force
Authors’ contributions
QZ, JC and XL have designed the work. QZ, GD, JC and XL acquired, analyzed and interpreted the data. QZ, JC and XL have drafted the work. HS, YZ and SZ administrated and provided technical and material support for the project. QZ, JC and XL have substantively revised the work. All the authors have approved the submitted version, and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work.
Funding
This study was funded by Chinese Association of Maternal and Child Health Studies (AMCHS-2014-4) in the design and conduct of the study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Database reported in this publication was supported by Chinese government, a national nonprofit project which benefit rural reproductive aged population.
Availability of data and materials
The datasets during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This project was approved by the Chinese Association of Maternal and Child Health Studies (IRB-201001), and written informed consent was obtained from each participant before enrollment. For those participated couples who were illiterate, their finger print was taken for the informed consent.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Footnotes
Jingqi Chen and Xiaotian Li are co-corresponding authors. These corresponding author had full access to all the data in the study and had final responsibility for the decision to submit.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Qiongjie Zhou and Guiying Dong contributed equally to this work.
Contributor Information
Jingqi Chen, Email: jingqichen@fudan.edu.cn.
Xiaotian Li, Email: xiaotianli555@163.com.
References
- 1.Wolff T, Witkop CT, Miller T, Syed SB, U.S. Preventive Services Task Force Folic acid supplementation for the prevention of neural tube defects: an update of the evidence for the U.S. preventive services task force. Ann Intern Med. 2009;150(9):632–639. doi: 10.7326/0003-4819-150-9-200905050-00010. [DOI] [PubMed] [Google Scholar]
- 2.Mills JL, Rhoads GG, Simpson JL, et al. National Institute of Child Health and Human Development neural tube defects study group. The absence of a relation between the periconceptional use of vitamins and neural-tube defects. N Engl J Med. 1989;321(7):430–435. doi: 10.1056/NEJM198908173210704. [DOI] [PubMed] [Google Scholar]
- 3.Czeizel AE, Dudás I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med. 1992;327(26):1832–1835. doi: 10.1056/NEJM199212243272602. [DOI] [PubMed] [Google Scholar]
- 4.Milunsky A, Jick H, Jick SS, et al. Multivitamin/folic acid supplementation in early pregnancy reduces the prevalence of neural tube defects. JAMA. 1989;262(20):2847–2852. doi: 10.1001/jama.1989.03430200091032. [DOI] [PubMed] [Google Scholar]
- 5.Williams J, Mai CT, Mulinare J, et al. Centers for Disease Control and Prevention. Updated estimates of neural tube defects prevented by mandatory folic acid fortification—United States, 1995-2011. MMWR Morb Mortal Wkly Rep. 2015;64(1):1–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Harris RP, Helfand M, Woolf SH, et al. Methods work group, third US preventive services task force. Current methods of the US preventive services task force: a review of the process. Am J Prev Med. 2001;20(3):21–35. doi: 10.1016/S0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 7.Mosley BS, Cleves MA, Siega-Riz AM, et al. National birth defects prevention study. Neural tube defects and maternal folate intake among pregnancies conceived after folic acid fortification in the United States. Am J Epidemiol. 2009;169(1):9–17. doi: 10.1093/aje/kwn331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viswanathan M, Treiman KA, Kish-Doto J, et al. Folic acid supplementation for the prevention of neural tube defects: an updated evidence report and systematic review for the US preventive services task force. JAMA. 2017;317(2):190–203. doi: 10.1001/jama.2016.19193. [DOI] [PubMed] [Google Scholar]
- 9.Zhou Q, Zhang S, Wang Q, et al. China's community-based strategy of universal preconception care in rural areas at a population level using a novel risk classification system for stratifying couples´ preconception health status. BMC Health Serv Res. 2016;16(1):689. doi: 10.1186/s12913-016-1930-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou QJ, Acharya G, Zhang SK, et al. A new perspective on universal preconception care in China. Acta Obstet Gynecol Scand. 2016;95(4):377–381. doi: 10.1111/aogs.12865. [DOI] [PubMed] [Google Scholar]
- 11.Kancherla V, Botto LD, Rowe LA, et al. Preventing birth defects, saving lives, and promoting health equity: an urgent call to action for universal mandatory food fortification with folic acid. Lancet Glob Health. 2022;10(7):e1053–e1057. doi: 10.1016/S2214-109X(22)00213-3. [DOI] [PubMed] [Google Scholar]
- 12.Czeizel AE, Dudás I, Métneki J. Pregnancy outcomes in a randomised controlled trial of periconceptional multivitamin supplementation: final report. Arch Gynecol Obstet. 1994;255(3):131–139. doi: 10.1007/BF02390940. [DOI] [PubMed] [Google Scholar]
- 13.Czeizel AE, Métneki J, Dudás I. The higher rate of multiple births after periconceptional multivitamin supplementation: an analysis of causes. Acta Genet Med Gemellol. 1994;43(3–4):175–184. doi: 10.1017/s0001566000001938. [DOI] [PubMed] [Google Scholar]
- 14.Czeizel AE. Controlled studies of multivitamin supplementation on pregnancy outcomes. Ann N Y Acad Sci. 1993;678:266–275. doi: 10.1111/j.1749-6632.1993.tb26128.x. [DOI] [PubMed] [Google Scholar]
- 15.Czeizel AE, Dobó M, Vargha P. Hungarian cohort-controlled trial of periconceptional multivitamin supplementation shows a reduction in certain congenital abnormalities. Birth Defects Res A Clin Mol Teratol. 2004;70(11):853–861. doi: 10.1002/bdra.20086. [DOI] [PubMed] [Google Scholar]
- 16.Czeizel AE. Reduction of urinary tract and cardiovascular defects by periconceptional multivitamin supplementation. Am J Med Genet. 1996;62(2):179–183. doi: 10.1002/(SICI)1096-8628(19960315)62:2<179::AID-AJMG12>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 17.Moore LL, Bradlee ML, Singer MR, Rothman KJ, Milunsky A. Folate intake and the risk of neural tube defects: an estimation of dose-response. Epidemiology. 2003;14(2):200–205. doi: 10.1097/01.EDE.0000040253.12446.B2. [DOI] [PubMed] [Google Scholar]
- 18.Wolff T, Witkop CT, Miller T, Syed SB. Folic acid supplementation for the prevention of neural tube defects: an update of the evidence for the US preventive services task force. Rockville, MD: Agency for Healthcare Research and Quality; 2009. [PubMed] [Google Scholar]
- 19.Tinker SC, Cogswell ME, Devine O, Berry RJ. Folic acid intake among U.S. women aged 15-44 years, National Health and nutrition examination survey, 2003-2006. Am J Prev Med. 2010;38(5):534–542. doi: 10.1016/j.amepre.2010.01.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets during the current study are available from the corresponding author on reasonable request.