Abstract
Identifying sub-groups of the population with different reasons for uncontrolled blood pressure (BP) can inform where to direct interventions to increase hypertension control. We determined characteristics associated with not being aware of having hypertension and being aware but not treated with antihypertensive medication among US adults with uncontrolled BP using the 2015–2018 National Health and Nutrition Examination Surveys (n=2,282). Among US adults with uncontrolled BP, systolic BP ≥140 mmHg or diastolic BP ≥90 mmHg, 38.0% were not aware they had hypertension, 15.6% were aware but not treated and 46.4% were aware and treated with antihypertensive medication. After multivariable adjustment, US adults who were 18–39 versus ≥70 years old were more likely (PR: 1.49 [95% CI: 1.11–1.99]) and those who had a healthcare visit in the past year were less likely (PR: 0.61 [95%CI: 0.48–0.77]) to be unaware they had hypertension. Among US adults with uncontrolled BP who were aware they had hypertension, those 18–39, 40–49, 50–59 and 60–69 versus ≥70 years old were more likely to not be treated versus being treated with antihypertensive medication. Not being treated with antihypertensive medication versus being treated and having uncontrolled BP was less common among those with versus without a usual source of healthcare (PR: 0.69 [95%CI: 0.51–0.94]) and who reported having versus not having a healthcare visit in past year (PR: 0.46 [95%CI: 0.35–0.61]). In conclusion, to increase BP control, interventions should be directed towards populations in which hypertension awareness is low and uncontrolled BP is common despite antihypertensive medication use.
Keywords: Uncontrolled blood pressure, awareness, hypertension, treatment, high blood pressure, blood pressure control
Summary
Data from this study emphasize the need for interventions to increase the use of adequate antihypertensive medication regimens including single pill combinations, especially among older adults, non-Hispanic Blacks and Hispanics and those without a usual source of healthcare.
According to data from the National Health and Nutrition Examination Survey (NHANES) 2017–2018, 56.3% of US adults with hypertension have uncontrolled blood pressure (BP), defined by systolic BP (SBP) ≥ 140 mm Hg or diastolic BP (DBP) ≥ 90 mm Hg.1 In October 2020, the US Surgeon General published a Call to Action to Control Hypertension that emphasized improving the awareness and treatment of hypertension, with the goal of making hypertension control a national public health priority.2, 3 Increasing the proportion of US adults with controlled BP can be achieved by increasing hypertension awareness, use of antihypertensive medication among those who are aware they have hypertension, and up titration of treatment among individuals taking antihypertensive medication with uncontrolled BP.
Identifying the reasons underlying uncontrolled BP, overall and in population subgroups, has implications for determining strategies that should be implemented to increase hypertension control. The purpose of the current study was to identify sociodemographic characteristics, healthcare access factors, and cardiovascular disease (CVD) risk factors among US adults with uncontrolled BP that are associated with being unaware versus aware of hypertension and not treated versus treated with antihypertensive medication. In a secondary analysis, we determined trends in the proportion of US adults with uncontrolled BP who were unaware they had hypertension, were aware they had hypertension but were not treated, and were treated with antihypertensive medication but had uncontrolled BP. To accomplish these goals, we analyzed data from the US NHANES 1999–2002 to 2015–2018.
Methods
Detailed methods and protocols for NHANES are provided elsewhere.4 All data used in the current analysis are publicly available through the National Center for Health Statistics (NCHS) and can be accessed at https://wwwn.cdc.gov/nchs/nhanes/default.aspx. The data analysis was conducted using STATA V16 (Stata Corporation, College Station, TX). All analytical scripts are available on request. Since 1999–2000, NHANES has been conducted in two-year cycles. For each two-year cycle, a stratified, multistage, probability sampling method was employed to select participants for enrollment. We pooled data for two-year NHANES cycles into 4-year groups to provide stable statistical estimates. The analysis was restricted to adults aged 18 years or older (Figure S1; n= 56,367). Participants who self-reported being pregnant or had a positive pregnancy test (n= 1,588) and those who did not have at least one valid SBP and DBP measurement (n= 2,772) or were missing information on antihypertensive medication use (n= 246) were excluded. Additionally, participants who had controlled BP, defined by SBP < 140 mm Hg and DBP < 90 mm Hg (n= 41,403) were excluded. A total of 10,358 participants (n=2,282 in NHANES 2015–2018) were included in the analyses. Written informed consent was obtained from each participant. The analysis of anonymous NHANES data were considered exempt from human subjects protection review by the Institutional Review Board of the University of Alabama at Birmingham.
Data collection
Data were collected during an in-home interview and a study visit conducted at a mobile examination center. Standardized questionnaires were used to assess sociodemographic characteristics, healthcare access and CVD risk factors. Sociodemographic characteristics included participants’ age, sex, race/ethnicity, marital status, education, annual household income and employment status. Healthcare access variables included type of health insurance, having a usual source of healthcare and having a healthcare visit in the past year. CVD risk factors included obesity, smoking status, diabetes, chronic kidney disease (CKD) and history of CVD. Smoking status and history of CVD, defined by prior diagnosis of myocardial infarction, coronary heart disease, stroke or heart failure, were self-reported. Height and weight were measured and blood and urine samples were collected during the study examination. Obesity was defined as a body mass index ≥30 kg/m2. Diabetes was defined by a fasting plasma glucose ≥126 mg/dL (≥200 mg/dL for those who were not fasting), glycated hemoglobin ≥6.5%, or a self-reported diagnosis of diabetes with self-reported use of insulin or oral glucose lowering medication. CKD was defined as an estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73m2 using the CKD-Epidemiology Collaboration equation5 or a urinary albumin-to-creatinine ratio >30 mg/g.
Blood pressure measurements
The same protocol was followed to measure SBP and DBP in all NHANES cycles. Trained physicians measured SBP and DBP three times using a mercury sphygmomanometer after participants had been seated and rested for five minutes. The mean of all available measurements was used to define SBP and DBP. Quality control included re-certification of physicians every three months with retraining if needed. All physicians participated in annual retraining. Uncontrolled BP was defined as SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg.
Outcomes
Participants with uncontrolled BP were categorized as not being aware they had hypertension, being aware but not treated with antihypertensive medication, and being aware and treated with antihypertensive medication. During the in-home interview, participants responding ‘no’ to the question “Have you ever been told by a doctor or other health professional that you had hypertension, also called high BP?” were categorized as being unaware that they had hypertension. Among those who were aware they had hypertension, not being treated was defined by answering no to either of the follow-up questions, which were asked in a sequence “Because of your high BP, have you ever been told to take prescribed medication?” and then “Are you now taking prescribed medicine?” Aware and treated was defined as taking antihypertensive medication.
Statistical analysis
Using data from 2015–2018, characteristics of US adults with uncontrolled BP were summarized as percentages for categorical variables and means with standard errors for continuous variables and presented overall and for those in each of the uncontrolled BP categories: unaware of having hypertension, aware but not treated with antihypertensive medication, and treated with antihypertensive medication. The estimated number and age-adjusted proportion of US adults in each of the uncontrolled BP categories were calculated overall and in sub-groups defined by sociodemographic characteristics, healthcare access, and CVD risk factors. Age adjustment was performed using direct standardization with the standard being US adults with uncontrolled BP in 2015–2018 (18 to 39 years [11.4%]; 40 to 49 years [12.0%], 50 to 59 years [24.0%]; 60 to 69 years [22.7%]; ≥ 70 years [29.9%]).
For the primary analysis, Poisson regression with robust variance estimation was used to estimate multivariable-adjusted prevalence ratios (PR) and 95% confidence intervals (CI) for the sociodemographic characteristics, healthcare access factors and CVD risk factors associated with each of the uncontrolled BP categories. Models were adjusted for the sociodemographic characteristics and healthcare access variables. In addition to models for overall population, analysis was also stratified by age, <60 and ≥60 years of age, based on the median of the age distribution of US adults with hypertension. The reasons for uncontrolled BP may be different for adults with apparent treatment resistant hypertension (aTRH) as compared to the general population.6 Therefore, in a sensitivity analysis, we repeated the multivariable-adjusted regression models after excluding 324 participants with uncontrolled BP while taking 3 or more classes of antihypertensive medication.
In a secondary analysis, the proportion of US adults with uncontrolled BP who were unaware, aware but not treated with antihypertensive medication, and treated with antihypertensive medication were estimated for 1999–2002, 2003–2006, 2007–2010, 2011–2014, and 2015–2018. These proportions were calculated for the overall population and for US adults <60 and ≥ 60 years of age, separately.
NHANES sampling weights were used in all calculations to obtain nationally representative estimates of the non-institutionalized US population. A two-tailed p-value <0.05 was used to define statistical significance.
Results
Among US adults with uncontrolled BP, 15.6 million (38.0%) were unaware they had hypertension, 6.4 million (15.6%) were aware but not treated with antihypertensive medication and 19.1 million (46.4%) were taking antihypertensive medication (Table S1). Among US adults who were aware they had hypertension, 7.3% reported having never been told to take antihypertensive medication. Among the remaining 92.7% who reported having been told to take antihypertensive medication, 19.2% were not currently taking antihypertensive medication. Among US adults with uncontrolled BP, 30.0% were ≥70 years old and 49.1% were female (Table 1).
Table 1:
Characteristics of US adults with uncontrolled blood pressure, overall and by hypertension awareness and antihypertensive medication use, NHANES 2015–2018.
| Aware | ||||
|---|---|---|---|---|
| Characteristics | Overall | Unaware | Not treated with antihypertensive medication | Treated with antihypertensive medication |
| (n=2,282) | (n=794) | (n=316) | (n=1,172) | |
| Sociodemographic factors | ||||
| Age group in years, % | ||||
| 18 to 39 | 11.4 | 15.9 | 19.2 | 5.0 |
| 40 to 49 | 12.0 | 15.2 | 17.7 | 7.5 |
| 50 to 59 | 24.0 | 25.1 | 35.0 | 19.4 |
| 60 to 69 | 22.7 | 20.7 | 17.6 | 25.9 |
| ≥70 | 30.0 | 23.0 | 10.5 | 42.1 |
| Female, % | 49.1 | 45.1 | 37.3 | 56.4 |
| Race/ethnicity*, % | ||||
| Non-Hispanic White | 62.8 | 63.5 | 63.2 | 62.1 |
| Non-Hispanic Black | 15.6 | 12.4 | 15.5 | 18.3 |
| Hispanic | 12.5 | 14.9 | 11.5 | 10.9 |
| Non-Hispanic Asian | 5.3 | 5.7 | 4.3 | 5.3 |
| Marital status | ||||
| Never married | 10.5 | 12.7 | 11.3 | 7.9 |
| Married/Living with partner | 60.6 | 62.2 | 63.8 | 58.2 |
| Divorced/Separated/Widowed | 29.1 | 25.1 | 24.9 | 33.9 |
| Education level, % | ||||
| <High school | 16.0 | 13.9 | 17.3 | 17.3 |
| High school/ some college | 59.7 | 56.1 | 58.2 | 63.1 |
| College graduate or above | 24.3 | 29.9 | 24.5 | 19.6 |
| Annual household income, % | ||||
| <$20,000 | 18.9 | 16.5 | 16.7 | 21.6 |
| $20,000 to <$45,000 | 27.0 | 23.2 | 27.2 | 30.0 |
| $45,000 to <$75,000 | 20.2 | 20.0 | 15.6 | 21.8 |
| ≥$75,000 | 33.9 | 40.3 | 40.5 | 26.6 |
| Employed | 47.5 | 56.9 | 61.2 | 35.1 |
| Blood pressure | ||||
| SBP, mm Hg, mean | 152 (0.5) | 148 (0.7) | 153 (1.2) | 154 (0.5) |
| DBP, mm Hg, mean | 80 (0.8) | 82 (0.8) | 86 (1.0) | 76 (0.9) |
| Healthcare access | ||||
| Health insurance, % | ||||
| None | 11.6 | 11.6 | 21.9 | 8.1 |
| Private | 55.3 | 62.0 | 47.8 | 52.4 |
| Government | 33.1 | 26.4 | 30.3 | 39.5 |
| Usual healthcare facility, % | 87.2 | 81.7 | 74.4 | 95.9 |
| Had healthcare visit in past year, % | 87.3 | 78.6 | 77.6 | 97.8 |
| CVD risk factors | ||||
| Obese, % | 48.3 | 41.1 | 54.5 | 52.1 |
| Current smoker, % | 16.8 | 15.4 | 25.1 | 15.1 |
| Diabetes, % | 20.9 | 11.7 | 14.5 | 30.6 |
| Chronic kidney disease, % | 32.0 | 19.5 | 34.0 | 41.6 |
| History of CVD, % | 13.9 | 5.7 | 9.9 | 22.0 |
Numbers in table denote column percent or mean (standard error).
NHANES: National Health And Nutrition Examination Surveys; SBP: systolic blood pressure; DBP: diastolic blood pressure; CVD: Cardiovascular disease.
Uncontrolled blood pressure defined by systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg.
The percentages for race/ethnicity do not add up to 100% as US adults in racial/ethnic groups other than Non-Hispanic White, Black or Asian or Hispanics are not presented in the table due to the small sample size.
Primary analysis – Factors associated with uncontrolled BP
Sociodemographic characteristics and healthcare access
Among US adults with uncontrolled BP, younger adults were more likely to be unaware of their hypertension status (Table 2). The age-adjusted proportion of US adults with uncontrolled BP who were unaware of their hypertension status was higher for those with an annual household income ≥ $75,000 and who were employed, and lower for non-Hispanic Blacks versus non-Hispanic Whites and Asians and Hispanics, divorced/separated/widowed versus never married or married/living with a partner, those with less than a high school education or a high school education/some college versus college graduates, with no health insurance or government health insurance versus private health insurance, those with versus without a usual healthcare facility and a healthcare visit in the past year. Among US adults with uncontrolled BP, older adults were less likely to be aware and not treated with antihypertensive medication. The age-adjusted proportion of US adults with uncontrolled BP not treated with antihypertensive medication was lower among those who were unemployed, had private insurance, a usual source of healthcare and who reported a healthcare visit in the past year. The proportion of US adults who were treated with antihypertensive medication and had uncontrolled BP was lower at younger age. The age-adjusted proportion of US adults who were treated with antihypertensive medication was lower among non-Hispanic Whites versus other race-ethnic groups, among those who were employed or did not have a usual source of healthcare or who reported not having a healthcare visit in past year.
Table 2:
Age-adjusted percentage of US adults with uncontrolled blood pressure who were unaware they had hypertension, were aware and not treated, and treated with antihypertensive medication by sociodemographic and healthcare access factors, NHANES 2015–2018.
| Aware | |||
|---|---|---|---|
| Characteristics | Unaware% (95% CI) | Not treated with antihypertensive medication% (95% CI) | Treated with antihypertensive medication% (95% CI) |
| Sociodemographic factors | |||
| Age group in years | |||
| 18 to 39 | 53.0 (45.0–60.9) | 26.4 (19.9–34.1) | 20.6 (14.2–28.8) |
| 40 to 49 | 48.2 (38.5–57.9) | 22.9 (16.9–30.3) | 28.9 (21.4–37.9) |
| 50 to 59 | 39.7 (32.2–47.8) | 22.7 (16.8–29.9) | 37.5 (30.3–45.3) |
| 60 to 69 | 34.7 (26.3–44.3) | 12.1 (8.1–17.8) | 53.1 (43.4–62.6) |
| ≥70 | 29.2 (25.2–33.6) | 5.5 (3.7–8.0) | 65.3 (60.0–70.3) |
| Sex | |||
| Female | 37.2 (32.5–42.1) | 12.9 (10.4–15.9) | 49.9 (45.2–54.6) |
| Male | 39.0 (34.8–43.3) | 17.1 (13.8–20.9) | 43.9 (40.4–47.5) |
| Race/ethnicity | |||
| Non-Hispanic White | 39.7 (34.6–45.0) | 17.0 (13.8–20.8) | 43.4 (39.5–47.3) |
| Non-Hispanic Black | 28.5 (24.9–32.5) | 13.8 (11.8–16.2) | 57.6 (53.7–61.4) |
| Hispanic | 42.1 (37.9–44.8) | 12.5 (9.4–16.3) | 45.5 (41.4–49.5) |
| Non-Hispanic Asian | 37.5 (30.7–44.8) | 15.5 (9.5–24.4) | 47.0 (41.0–53.0) |
| Marital status | |||
| Never married | 37.0 (28.7–46.1) | 14.6 (9.5–21.9) | 48.4 (37.8–59.2) |
| Married/Living with partner | 38.8 (34.0–43.9) | 16.0 (13.4–19.1) | 45.2 (41.4–49.0) |
| Divorced/Separated/Widowed | 34.4 (29.0–40.2) | 16.3 (11.7–22.1) | 49.3 (42.9–55.8) |
| Education level | |||
| <High school | 33.9 (29.6–38.5) | 17.9 (13.1–24.0) | 48.2 (43.5–52.8) |
| High-school/some college | 35.4 (30.7–40.5) | 15.0 (12.9–17.5) | 49.5 (45.7–53.4) |
| College graduate | 46.7 (39.3–54.3) | 15.9 (10.9–22.5) | 37.4 (32.0–43.1) |
| Annual household income | |||
| <$20,000 | 34.2 (27.0–42.2) | 15.7 (12.0–20.3) | 50.1 (43.2–57.0) |
| $20,000 to <$45,000 | 33.9 (30.1–38.0) | 17.1 (13.8–20.8) | 49.0 (44.9–53.2) |
| $45,000 to <$75,000 | 37.7 (31.1–44.9) | 11.7 (8.2–16.6) | 50.5 (43.1–57.9) |
| ≥$75,000 | 42.2 (34.8–50.0) | 16.5 (12.9–20.9) | 41.2 (35.6–47.1) |
| Employed | |||
| No | 43.1 (37.4–49.0) | 38.8 (32.2–45.8) | 64.9 (60.0–69.5) |
| Yes | 56.9 (51.0–62.6) | 61.2 (54.2–67.8) | 35.1 (30.5–40.0) |
| Healthcare access | |||
| Insurance type | |||
| None | 33.7 (24.3–44.6) | 24.1 (17.1–32.7) | 42.2 (31.1–54.2) |
| Private | 42.7 (37.5–48.0) | 13.3 (10.6–16.5) | 44.0 (39.4–48.8) |
| Government | 31.3 (26.8–36.3) | 16.4 (13.8–19.2) | 52.3 (48.1–56.5) |
| Usual health care facility | |||
| No | 51.1 (41.9–60.6) | 24.5 (19.7–30.0) | 24.2 (16.8–33.5) |
| Yes | 36.3 (32.6–40.2) | 13.9 (11.9–16.3) | 49.7 (46.3–53.1) |
| Had health care visit in past year | |||
| No | 60.2 (49.2–70.3) | 21.1 (16.2–27.0) | 18.6 (11.9–28.0) |
| Yes | 34.8 (30.9–39.0) | 14.5 (12.4–16.9) | 50.7 (47.3–54.0) |
NHANES: National Health and Nutrition Examination Survey; CI: confidence interval.
Uncontrolled blood pressure defined by systolic blood pressure ≥140 or diastolic blood pressure ≥90 mm Hg.
After multivariable adjustment, US adults 18–39 years of age were more likely to be unaware they had hypertension compared to US adults ≥70 years of age (PR: 1.49 [95%CI: 1.11–1.99]; Table 3 left column). College graduates were more likely than those with less than a high school education to be unaware they had hypertension (PR: 1.37 [95%CI: 1.03–1.83]). Those who had versus did not have a healthcare visit in the past year were less likely to be unaware they had hypertension (PR: 0.61 [95%CI: 0.48–0.77]).
Table 3:
Association of sociodemographic and healthcare access factors with lack of hypertension awareness and not treated with antihypertensive medication among US adults with uncontrolled blood pressure, NHANES 2015–2018.
| Characteristics | Hypertension awareness Unaware versus aware | Not treated versus treated with antihypertensive medication |
|---|---|---|
| Prevalence ratio* (95% CI) | Prevalence ratio* (95% CI) | |
| Sociodemographic factors | ||
| Age group in years | ||
| 18 to 39 | 1.49 (1.11–1.99) | 5.72 (3.23–10.13) |
| 40 to 49 | 1.34 (0.93–1.92) | 5.56 (2.69–11.49) |
| 50 to 59 | 1.21 (0.81–1.81) | 4.92 (2.56–9.45) |
| 60 to 69 | 1.19 (0.83–1.73) | 2.64 (1.17–5.98) |
| ≥70 | 1 (ref) | 1 (ref) |
| Sex | ||
| Female | 1 (ref) | 1 (ref) |
| Male | 0.98 (0.81–1.19) | 1.12 (0.80–1.57) |
| Race/ethnicity | ||
| Non-Hispanic White | 1 (ref) | 1 (ref) |
| Non-Hispanic Black | 0.79 (0.63–1.00) | 0.70 (0.54–0.91) |
| Hispanic | 1.10 (0.90–1.34) | 0.72 (0.54–0.96) |
| Non-Hispanic Asian | 0.98 (0.75–1.29) | 0.84 (0.63–1.13) |
| Marital status | ||
| Never married | 1 (ref) | 1 (ref) |
| Married/Living with partner | 0.85 (70–1.02) | 0.87 (0.65–1.16) |
| Divorced/Separated/Widowed | 0.81 (0.63–1.04) | 1.00 (0.65–1.53) |
| Education level | ||
| <High school | 1 (ref) | 1 (ref) |
| High-school/ some college | 1.07 (0.82–1.39) | 0.89 (0.63–1.26) |
| College graduate | 1.37 (1.03–1.83) | 1.15 (0.68–1.93) |
| Annual household income | ||
| <$20,000 | 1 (ref) | 1 (ref) |
| $20,000 to <$45,000 | 0.89 (0.68–1.16) | 1.17 (0.83–1.64) |
| $45,000 to <$75,000 | 0.95 (0.68–1.34) | 0.92 (0.60–1.40) |
| ≥$75,000 | 1.01 (0.74–1.39) | 1.39 (0.96–2.02) |
| Employed | ||
| No | 1 (ref) | 1 (ref) |
| Yes | 1.05 (0.79–1.39) | 0.91 (0.67–1.24) |
| Healthcare access | ||
| Insurance type | ||
| None | 1 (ref) | 1 (ref) |
| Private | 1.27 (0.87–1.85) | 0.84 (0.60–1.17) |
| Government | 1.00 (0.69–1.44) | 0.94 (0.68–1.31) |
| Usual healthcare facility | ||
| No | 1 (ref) | 1 (ref) |
| Yes | 0.88 (0.71–1.10) | 0.69 (0.51–0.94) |
| Had health care visit in past year | ||
| No | 1 (ref) | 1 (ref) |
| Yes | 0.61 (0.48–0.77) | 0.46 (0.35–0.61) |
The bold font indicates statistically significant results with p value <0.05.
Prevalence ratios were estimated from models that included age, sex, race/ethnicity, marital status, education level, annual household income, employment status, insurance type, usual healthcare facility and having a healthcare visit in past year.
NHANES: National Health and Nutrition Examination Survey; CI: confidence interval.
Uncontrolled blood pressure was defined by systolic blood pressure ≥140 or diastolic blood pressure ≥90 mm Hg.
Among those who were aware they had hypertension, US adults who were 18–39, 40–49, 50–59 and 60–69 years of age as compared to those ≥70 years of age were more likely to not be treated versus treated with antihypertensive medication (PR: 5.72 [95%CI: 3.23–10.13], PR: 5.56 [95%CI: 2.69–11.49], PR: 4.92 [95% CI: 2.56–9.45] and PR: 2.64 [95%CI: 1.17–5.98], respectively; Table 3 right column). Also, not being treated versus being treated with antihypertensive medication was less common among non-Hispanic Black and Hispanic adults as compared to non-Hispanic White adults (PR: 0.70 [95%CI: 0.54–0.91] and PR: 0.72 [95%CI: 0.54–0.96], respectively), those with versus without a usual source of healthcare (PR: 0.69 [95%CI: 0.51–0.94]) and US adults who reported having versus not having a healthcare visit in past year (PR: 0.46 [95%CI: 0.35–0.61]).
Factors associated with being unaware of having hypertension and not being treated with antihypertensive medication for US adults < 60 years of age and ≥ 60 years of age, separately, are presented in Table S2 and after excluding those with aTRH are presented in Table S3.
CVD risk factors and uncontrolled BP
The age-adjusted proportion of US adults with uncontrolled BP who were unaware they had hypertension was lower for those who were obese, current smokers, and had diabetes, CKD and a history of CVD (Table 4). After multivariable adjustment, US adults who were obese (PR: 0.69 [95%CI: 0.55–0.86]), had diabetes (PR: 0.56 [95%CI: 0.42–0.76]), CKD (PR: 0.59 [95%CI: 0.46–0.75]), and a history of CVD (PR: 0.41 [95%CI: 0.27–0.62]) had a lower likelihood of being unaware versus aware that they had hypertension (Table 5). Among US adults who were aware they had hypertension, there was no evidence that any of the CVD risk factors were associated with not being treated as compared to being treated with antihypertensive medication. Factors associated with being unaware of having hypertension and not being treated with antihypertensive medication among those with uncontrolled BP are presented by age in Table S4 and after excluding participants with aTRH are presented in Table S5.
Table 4:
Age-adjusted percentage of US adults with uncontrolled blood pressure who were unaware they had hypertension, were aware and not treated, and treated with antihypertensive medication by cardiovascular disease risk factors, NHANES 2015–2018.
| Aware | |||
|---|---|---|---|
| Characteristics | Unaware% (95% CI) | Not treated with antihypertensive medication% (95% CI) | Treated with antihypertensive medication% (95% CI) |
| Cardiovascular disease risk factors | |||
| Obesity | |||
| No | 45.0 (39.9–50.3) | 15.5 (11.7–20.6) | 39.4 (34.9–44.1) |
| Yes | 30.0 (25.3–35.1) | 15.8 (12.0–20.5) | 54.2 (50.1–58.3) |
| Current smoker | |||
| No | 39.4 (35.9–43.1) | 14.7 (12.5–17.3) | 45.8 (43.4–48.2) |
| Yes | 32.4 (25.3–40.4) | 19.8 (15.1–25.5) | 47.9 (40.7–55.1) |
| Diabetes | |||
| No | 41.9 (37.4–46.5) | 16.4 (13.9–19.2) | 41.7 (38.3–45.2) |
| Yes | 23.9 (19.5–29.0) | 12.2 (8.2–17.8) | 63.8 (58.6–68.8) |
| Chronic kidney disease | |||
| No | 44.1 (40.1–48.1) | 12.6 (11.4–16.1) | 42.3 (39.3–45.4) |
| Yes | 25.4 (20.3–31.2) | 21.5 (16.7–27.3) | 53.1 (46.6–59.5) |
| History of cardiovascular disease | |||
| No | 40.9 (36.9–45.0) | 15.6 (13.6–17.8) | 43.5 (40.2–46.8) |
| Yes | 14.2 (9.8–20.1) | 12.7 (7.3–21.3) | 73.1 (65.0–79.8) |
NHANES: National Health and Nutrition Examination Survey; CI: confidence interval.
Uncontrolled blood pressure was defined by systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg.
Table 5:
Association of cardiovascular disease risk factors with lack of hypertension awareness and not treated with antihypertensive medication among US adults with uncontrolled blood pressure, NHANES 2015–2018.
| Hypertension awareness, Unaware versus aware | Not treated versus treated with antihypertensive medication | |
|---|---|---|
| Prevalence ratio* (95% CI) | Prevalence ratio* (95% CI) | |
| Cardiovascular disease risk factors | ||
| Obesity | ||
| No | 1 (ref) | 1 (ref) |
| Yes | 0.69 (0.55–0.86) | 0.88 (0.59–1.32) |
| Current smoker | ||
| No | 1 (ref) | 1 (ref) |
| Yes | 0.89 (0.70–1.13) | 1.12 (0.78–1.61) |
| Diabetes | ||
| No | 1 (ref) | 1 (ref) |
| Yes | 0.56 (0.42–0.76) | 0.62 (0.37–1.07) |
| Chronic kidney disease | ||
| No | 1 (ref) | 1 (ref) |
| Yes | 0.59 (0.46–0.75) | 1.23 (0.91–1.67) |
| History of cardiovascular disease | ||
| No | 1 (ref) | 1 (ref) |
| Yes | 0.41 (0.27–0.62) | 0.78 (0.45–1.37) |
The bold font indicates statistically significant results with p value <0.05.
Prevalence ratios adjusted for age, sex, race/ethnicity, marital status, education level, annual household income, employment status, insurance type, usual healthcare facility and having a healthcare visit in past year.
NHANES: National Health and Nutrition Examination Survey; CI: confidence interval.
Uncontrolled blood pressure defined by systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg.
Secondary analysis - Trends in reasons for uncontrolled BP
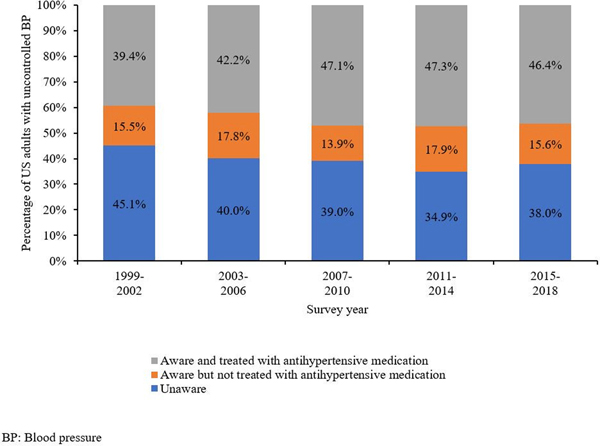
Between 1999–2002 and 2015–2018, the proportion of US adults with uncontrolled BP who were unaware they had hypertension decreased while the proportion who were aware and treated with antihypertensive medication increased (Figure 1). The proportion of US adults <60 years of age with uncontrolled BP who were unaware they had hypertension, not treated and treated with antihypertensive medication was within 5% in 1999–2002 and 2015–2018 (Figure S2, top panel). Between 1999–2002 and 2015–2018, the proportion of US adults ≥ 60 years of age with uncontrolled BP who were treated with antihypertensive medication increased from 48.7% to 60.1% while the proportion unaware they had hypertension decreased from 41.0% to 31.6% (Figure S2, bottom panel).
Figure 1: Trends in reasons for uncontrolled blood pressure among US adults from 1999 to 2018.
Unawareness to hypertension was defined by answering no to the question “Have you ever been told by a doctor or other health professional that you had hypertension, also called high blood pressure?” Not treated with antihypertensive medication was defined by answering no to either of the questions “Because of your high blood pressure/hypertension, have you ever been told to take prescribed medicine?” or “Are you now taking prescribed medicine?” Treated with antihypertensive medication was defined as taking antihypertensive medication with uncontrolled blood pressure.
Discussion
In the current study, younger adults were more likely to be unaware they had hypertension while those who had a healthcare visit in the past year and with obesity, diabetes, CKD, and a history of CVD were less likely to be unaware they had hypertension. Among those who were aware they had hypertension, not being treated versus being treated with antihypertensive medication but having uncontrolled BP was more common among younger adults and less common among non-Hispanic blacks and Hispanics as compared to non-Hispanic whites, and those with a usual source of healthcare and who reported having a healthcare visit in past year.
Almost 50% of US adults with uncontrolled BP were aware they had hypertension and were treated with antihypertensive medication. Additionally, the proportion of US adults ≥ 60 years of age who were treated with antihypertensive medication but had uncontrolled BP increased between 1999–2002 and 2015–2018. Uncontrolled BP among US adults treated with antihypertensive medication could be attributed to the regimen prescribed upon treatment initiation, lack of clinically-appropriate medication titration, and low medication adherence.7–9 BP control can be achieved more quickly with the use of dual- or triple antihypertensive combination therapies.10–13 Additionally, single pill combinations have been shown to be associated with better medication adherence and achieving BP control compared with multiple pill therapy.14 However, analyses have estimated that only 13.5% of US adults ≥ 65 years of age with Medicare health insurance initiate antihypertensive medication with single pill combinations.15 Once antihypertensive medication has been initiated, lack of healthcare access may result in not having follow-up visits where antihypertensive medication can be titrated.9, 16, 17 Among US adults with Medicare health insurance, 32% had low antihypertensive medication adherence in the year following treatment initiation.15 The high proportion of US adults treated with antihypertensive medication and having uncontrolled BP emphasizes the need for initiatives to increase prescribing of medication regimens that have been demonstrated to lower BP sufficiently and improve access to care so that BP levels and medication adherence can be monitored.
Being unaware of having hypertension was the second most common reason for uncontrolled BP among US adults. The United States Preventive Services Task Force recommends screening for high BP in all adults, 18 years of age and older.18 The recommended screening interval is every 3 to 5 years for those 18–39 years of age without increased hypertension risk and annual screening for those 40 years and older or younger adults who have an increased risk for hypertension including Black adults, those with overweight/obesity and with elevated BP.18 Additionally, young adults are less likely to have health insurance and a usual source of care, each of which may contribute to missed opportunities for hypertension screening.19–21 Moreover, many young adults do not perceive themselves at risk for hypertension and CVD.21, 22 Although hypertension awareness was more common among US adults with versus without obesity, diabetes, CKD or history of CVD, a majority of US adults with uncontrolled BP do not have these conditions.23 These data emphasize the need for population-wide hypertension screening to increase hypertension awareness.
Not being treated with antihypertensive medication also contributed to uncontrolled BP among US adults who reported being aware they had hypertension. Individuals may choose to not initiate antihypertensive medication due to a perception of low risk for CVD or lack access to a pharmacy.7, 24–26 Also, prior studies have reported a high percentage of patients discontinue antihypertensive medication.24, 27 The current study highlights the need to better understand why patients who are aware they have hypertension are not taking antihypertensive medication and develop approaches to increase evidence-based treatment recommendations.
In the current study, the proportion of younger adults who were unaware they had hypertension did not change substantially over past two decades. Although most young adults have a low 10-year risk for CVD, long-standing uncontrolled BP increases their lifetime risk for CVD.28 Data from the current study emphasize the need for interventions aimed at hypertension screening and increased antihypertensive medication use among young and middle-aged adults. Also, a high proportion of non-Hispanic Blacks and Hispanics were treated with antihypertensive medication but had uncontrolled BP. In a prior analysis of US adults taking antihypertensive medication, non-Hispanic Blacks and Hispanics were less likely than non-Hispanic whites to have controlled BP.1 Prior studies have reported that Black adults require more classes of antihypertensive medication to achieve BP control compared with white adults.10, 29 Interventions to appropriately titrate antihypertensive medications among non-Hispanic Blacks and Hispanics has the potential to reduce disparities in BP control in the US.
Strategies to improve hypertension awareness and appropriate antihypertensive treatment among US adults are needed. May Measurement Month, a global awareness campaign that was initiated by the International Society of Hypertension, has been successful in identifying thousands of adults with untreated and inadequately treated hypertension.30 In addition, ensuring patients are given their BP levels both orally and written, as recommended in the 2017 ACC/AHA BP guideline can help with increasing hypertension awareness.31 Also, use of single pill combinations for treatment initiation can result in fewer dose adjustments and improve adherence.11, 14 Programs like Kaiser Permanente Northern California Hypertension Program have demonstrated that BP control can be achieved for a high proportion of adults following such evidence-based strategies.32 However, further research is needed on how to implement these programs in a broader range of settings.
Among US adults with uncontrolled BP, the proportion that were aware they had hypertension and that were treated with antihypertensive medication was similar in the current study and in a previous report from NHANES 2003–2010.33 The 2020 Call to Action to Control Hypertension by the US Surgeon General provides a roadmap for achieving BP control and reducing the risk for future CVD events.3 The Call to Action includes the evidence-based strategies that are aligned with recommendations by the 2017 ACC/AHA BP guideline to increase BP control including enhancing electronic health record systems to improve workflow, providing decision support tools, implementing treatment protocols, using integrated care teams with community partnerships, providing clinicians feedback on their performance, and promoting shared patient-provider management with self-measured BP monitoring.3, 34 Changes at the local, state and national levels are discussed in the Call to Action to support lifestyle behaviors and health systems in making modifications to facilitate BP control.
The current study has several strengths. NHANES provides nationally representative estimates for the non-institutionalized US population and the results of this analysis have broad generalizability. Each NHANES cycle included a large sample size and BP was measured following a standardized protocol. Despite these strengths, this study has several limitations. Data on hypertension awareness and antihypertensive medication use for this analysis were self-reported. However, the results were similar after excluding adults with aTRH defined using pill bottle review to identify antihypertensive medication classes. Also, data were not collected on medication dose, frequency, medication adherence, side effects and insurance reimbursement for medications. BP was assessed at a single time point and some people with uncontrolled BP may have had controlled BP if assessed at a second visit. Finally, the response rate for NHANES has declined from 1999–2002 through 2015–2018, however, the effect of this on the current study’s results is unclear.
Perspectives
The majority of US adults with uncontrolled BP were not aware they had hypertension or were aware and treated with antihypertensive medication. To increase BP control, interventions to increase hypertension awareness should be directed towards younger adults, those without a healthcare visit in the past year and without CVD risk factors. Interventions are also needed to increase BP control among US adults already taking antihypertensive medication, potentially through greater use of single pill combinations, especially among older adults, non-Hispanic Black and Hispanic adults, and those without a usual source of healthcare.
Supplementary Material
Novelty and Significance.
What is new?
The US Surgeon General’s Call to Action to Control Hypertension emphasizes that awareness and control of high BP are a public health priority.
Understanding the reasons for uncontrolled BP has implications for determining which strategies should be implemented to increase hypertension control.
What is relevant?
Most US adults with uncontrolled BP were either not aware they had hypertension, or were treated with antihypertensive medication but had uncontrolled BP.
Older adults were more likely to be treated with antihypertensive medication but have uncontrolled BP.
Younger adults (<70 years) were more likely, while those who had a healthcare visit in the past year were less likely, to be unaware they had hypertension.
Among those who were aware they had hypertension, not being treated with antihypertensive medication versus treated but having uncontrolled BP was more common among younger adults and less common among those with a usual source of healthcare and who reported having a healthcare visit in past year.
Funding
Kathryn Foti is supported by National Institutes of Health/National Heart, Lung, and Blood Institute (NIH/NHLBI) grant T32 HL007024. Shakia Hardy is supported by NIH/NHLBI grant R01 HL139716.
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of interest disclosures
Dr. Muntner receives research support and consulting fees from Amgen Inc. Dr. Oparil reports research grants from NIH/NHLBI, Bayer, George Medicines Pty Limited, and Idorsia Pharmaceuticals, ad hoc lecture honoraria from Ascension, personal fees from Preventric Diagnostics, Inc. as Chief Medical Officer and from Cincor Pharma Inc. as Scientific Advisory Board Member, and receiving annual stipend as Editor-in-Chief for Current Hypertension Reports (Springer Science Business Media LLC), all outside of the submitted work. No other disclosures were reported.
References
- 1.Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA. 2020;324:1190–1200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adams JM, Wright JS. A national commitment to improve the care of patients with hypertension in the US. JAMA. 2020;324(18):1825–1826 [DOI] [PubMed] [Google Scholar]
- 3.The surgeon general’s call to action to control hypertension. Center for Disease Control and Prevention. 2020;2020 [Google Scholar]
- 4.US centers for disease control and prevention. National Health and Nutrition Examination Survey.2020 [Google Scholar]
- 5.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, Ckd EPI. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarwar MS, Islam MS, Al Baker SM, Hasnat A. Resistant hypertension: Underlying causes and treatment. Drug research. 2013;63:217–223 [DOI] [PubMed] [Google Scholar]
- 7.Williams B, Shaw A, Durrant R, Crinson I, Pagliari C, de Lusignan S. Patient perspectives on multiple medications versus combined pills: A qualitative study. QJM: An International Journal of Medicine. 2005;98:885–893 [DOI] [PubMed] [Google Scholar]
- 8.Elliott WJ. What factors contribute to the inadequate control of elevated blood pressure? The Journal of Clinical Hypertension. 2008;10:20–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khatib R, Schwalm J-D, Yusuf S, Haynes RB, McKee M, Khan M, Nieuwlaat R. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: A systematic review and meta-analysis of qualitative and quantitative studies. PLoS One. 2014;9:e84238-e84238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cushman WC, Ford CE, Einhorn PT, Wright JT Jr., Preston RA, Davis BR, Basile JN, Whelton PK, Weiss RJ, Bastien A, Courtney DL, Hamilton BP, Kirchner K, Louis GT, Retta TM, Vidt DG. Blood pressure control by drug group in the Antihypertensive and Lipid-Lowering Treatment to prevent Heart Attack Trial (ALLHAT). Journal of clinical hypertension (Greenwich, Conn.). 2008;10:751–760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salam A, Atkins ER, Hsu B, Webster R, Patel A, Rodgers A. Efficacy and safety of triple versus dual combination blood pressure-lowering drug therapy: A systematic review and meta-analysis of randomized controlled trials. Journal of hypertension. 2019;37:1567–1573 [DOI] [PubMed] [Google Scholar]
- 12.Bellows BK, Ruiz-Negrón N, Bibbins-Domingo K, King JB, Pletcher MJ, Moran AE, Fontil V. Clinic-based strategies to reach United States Million Hearts 2022 blood pressure control goals. Circulation. Cardiovascular quality and outcomes. 2019;12:e005624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.An J, Luong T, Qian L, Wei R, Liu R, Muntner P, Brettler J, Jaffe MG, Moran AE, Reynolds K. Treatment patterns and blood pressure control with initiation of combination versus monotherapy antihypertensive regimens. Hypertension. 2021;77:103–113 [DOI] [PubMed] [Google Scholar]
- 14.Tsioufis K, Kreutz R, Sykara G, van Vugt J, Hassan T. Impact of single-pill combination therapy on adherence, blood pressure control, and clinical outcomes: A rapid evidence assessment of recent literature. Journal of hypertension. 2020;38:1016–1028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tajeu GS, Kent ST, Kronish IM, Huang L, Krousel-Wood M, Bress AP, Shimbo D, Muntner P. Trends in antihypertensive medication discontinuation and low adherence among medicare beneficiaries initiating treatment from 2007 to 2012. Hypertension. 2016;68:565–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coleman MT, Lott JA, Sharma S. Use of continuous quality improvement to identify barriers in the management of hypertension. American journal of medical quality : the official journal of the American College of Medical Quality. 2000;15:72–77 [DOI] [PubMed] [Google Scholar]
- 17.Schafheutle EI, Hassell K, Noyce PR, Weiss MC. Access to medicines: Cost as an influence on the views and behaviour of patients. Health & social care in the community. 2002;10:187–195 [DOI] [PubMed] [Google Scholar]
- 18.Liu K, Colangelo LA, Daviglus ML, Goff DC, Pletcher M, Schreiner PJ, Sibley CT, Burke GL, Post WS, Michos ED, Lloyd-Jones DM. Can antihypertensive treatment restore the risk of cardiovascular disease to ideal levels?: The coronary artery risk development in young adults (CARDIA) study and the multi-ethnic study of atherosclerosis (MESA). Journal of the American Heart Association. 2015;4:e002275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fortuna RJ, Robbins BW, Mani N, Halterman JS. Dependence on emergency care among young adults in the United States. J Gen Intern Med. 2010;25:663–669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Derington CG, King JB, Herrick JS, Shimbo D, Kronish IM, Saseen JJ, Muntner P, Moran AE, Bress AP. Trends in antihypertensive medication monotherapy and combination use among US adults, National Health and Nutrition Examination Survey 2005–2016. Hypertension. 2020;75:973–981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luquis RR, Kensinger WS. Perceptions of health care and access to preventive services among young adults. Journal of community health. 2017;42:1204–1212 [DOI] [PubMed] [Google Scholar]
- 22.Gooding HC, McGinty S, Richmond TK, Gillman MW, Field AE. Hypertension awareness and control among young adults in the national longitudinal study of adolescent health. J Gen Intern Med. 2014;29:1098–1104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States, 1999 to 2012: Progress toward Healthy People 2020 goals. Circulation. 2014;130:1692–1699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clifford S, Barber N, Horne R. Understanding different beliefs held by adherers, unintentional nonadherers, and intentional nonadherers: Application of the necessity-concerns framework. Journal of psychosomatic research. 2008;64:41–46 [DOI] [PubMed] [Google Scholar]
- 25.Robins LS, Jackson JE, Green BB, Korngiebel D, Force RW, Baldwin LM. Barriers and facilitators to evidence-based blood pressure control in community practice. Journal of the American Board of Family Medicine : JABFM. 2013;26:539–557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amstislavski P, Matthews A, Sheffield S, Maroko AR, Weedon J. Medication deserts: Survey of neighborhood disparities in availability of prescription medications. International journal of health geographics. 2012;11:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hugtenburg JG, Timmers L, Elders PJ, Vervloet M, van Dijk L. Definitions, variants, and causes of nonadherence with medication: A challenge for tailored interventions. Patient preference and adherence. 2013;7:675–682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reges O, Ning H, Wilkins JT, Wu CO, Tian X, Domanski MJ, Lloyd-Jones DM, Allen NB. Association of Cumulative Systolic Blood Pressure With Long-Term Risk of Cardiovascular Disease and Healthy Longevity: Findings From the Lifetime Risk Pooling Project Cohorts. Hypertension. 2021;77(2):347–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rao S, Segar MW, Bress AP, Arora P, Vongpatanasin W, Agusala V, Essien UR, Correa A, Morris AA, de Lemos JA, Pandey A. Association of Genetic West African Ancestry, Blood Pressure Response to Therapy, and Cardiovascular Risk Among Self-Reported Black Individuals in the Systolic Blood Pressure Reduction Intervention Trial (SPRINT). JAMA cardiology. 2020;6(4):388–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beaney T, Burrell LM, Castillo RR, Charchar FJ, Cro S, Damasceno A, Kruger R, Nilsson PM, Prabhakaran D, Ramirez AJ, Schlaich MP, Schutte AE, Tomaszewski M, Touyz R, Wang J-G, Weber MA, Poulter NR, Investigators tM. May measurement month 2018: A pragmatic global screening campaign to raise awareness of blood pressure by the international society of hypertension. European Heart Journal. 2019;40:2006–2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT, Jr., Whelton PK. Potential us population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137:109–118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310:699–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vital signs: Awareness and treatment of uncontrolled hypertension among adults--United States, 2003–2010. MMWR. Morbidity and mortality weekly report. 2012;61:703–709 [PubMed] [Google Scholar]
- 34.Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.