Abstract
Removable partial dentures (RPDs) offer a broad range of aesthetics and restorative functions for partially edentulous patients. This systematic review examines patients' satisfaction rates and the factors that influence RPD satisfaction.
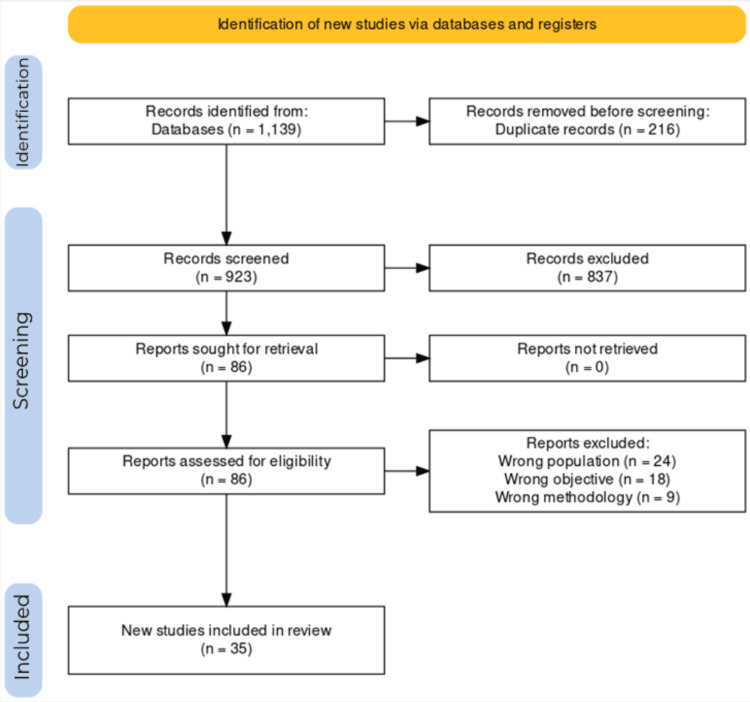
This systematic review was conducted according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and the Cochrane Handbook for Systematic Reviews. A systematic literature search was done on PubMed, Scopus, and Google Scholar using preset inclusion criteria.
A total of 923 non-duplicate articles were screened, and 35 were included in this review. Among the included studies, RPDs generally exhibited high satisfaction rates, with reported rates ranging between 50% and 81%. Several factors influenced satisfaction. Age played a major role, with older adults expressing higher satisfaction. Gender differences were also noted, especially in appearance satisfaction where women were more satisfied with RPDs than men. Prior experience with RPDs correlated positively with overall satisfaction. The number and location of missing teeth, as well as the type of RPD (metal vs. flexible), significantly influenced satisfaction levels. Flexible dentures were more satisfactory than metal RPDs. Attachments, such as magnetic attachments and implants, increased satisfaction. Patient complaints, encompassing pain, aesthetics, and cleanliness, were identified as common sources of dissatisfaction.
The results underscore the significance of customizing RPD treatment to individual needs, considering factors that influence RPD satisfaction. Recognizing the importance of influential factors such as age, gender RPD experience, etc., for clinicians seeking to optimize patient outcomes in RPD therapy is crucial.
Keywords: outcomes, satisfaction rate, patient satisfaction, satisfaction, aesthetics, chewing ability, partial edentulous, removable denture, partial denture, removable partial denture
Introduction and background
A removable partial denture (RPD) is designed for partially edentulous patients in need of teeth replacement for either functional or aesthetic purposes [1]. This option is suitable when a fixed partial denture (bridge) is not feasible due to factors such as insufficient supporting teeth (distal abutments) or financial constraints. There are three types of RPDs: cast metal partial denture, flexible partial denture, and acrylic partial denture (flipper tooth). RPDs are supported by the surrounding tissues and remaining teeth [2]. They are equipped with clasps made of cobalt-chrome, titanium metal, or plastic, which securely attach to the existing teeth, thereby enhancing the stability and retention of the RPD [3-4].
RPDs offer a broad spectrum of restorative functions. These include maintaining or enhancing speech clarity, improving masticatory efficiency, stabilizing dental relationships, and achieving the desired aesthetics [1,5-8]. Despite these benefits, RPDs pose a challenge of dissatisfaction for several patients. The biggest concern is usually the aesthetic aspect, which impacts both appearance and interpersonal communication [9-10]. Patient dissatisfaction with RPDs also stems from concerns about potential local damage to remaining teeth, such as risks of caries, periodontal disease, plaque accumulation, oral candidiasis, and denture stomatitis [2,4,11-14].
Due to the potential dissatisfaction associated with RPDs, one key focus during their design should be to ensure a patient’s satisfaction. In literature, satisfaction with RPDs is reported to be influenced by various factors, including the unique characteristics of each patient, their attitude toward RPD, prior experiences with removable dentures, the level of encouragement received for denture use, and the specific design and fabrication process of the RPD [3,15,16]. This review aims to improve knowledge of the factors influencing satisfaction with RPDs. Its primary objective is to assess the satisfaction rates among patients using RPDs. Additionally, the review investigates the various factors that contribute to satisfaction levels with RPDs.
Review
Protocol
This systematic review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) recommendations [17] and the Cochrane Handbook for Systematic Reviews. This study utilizes data collected from published clinical studies. Its design does not require any form of approval from an ethics committee.
Outcomes
The participants included all patients wearing RPDs, and the intervention focused on those who underwent rehabilitation with RPDs. Comparison or lack thereof was not a matter of concern as the review sought to understand the subjective experiences of patients utilizing RPDs. The primary outcome of studies was the patient-reported outcome measure of patient satisfaction evaluated after RPD therapy. A population, intervention, control, and outcome (PICO) were used to formulate a primary outcome question: What is the satisfaction rate among patients wearing RPDs? Patient satisfaction is the sense of well-being that patients feel following prosthetic therapy.
Inclusion and exclusion criteria
The articles included in this study were carefully selected to fulfill the study's purpose and address the following research question: "What is the prevalence of satisfaction in patients wearing RPDs? The inclusion and exclusion criteria were meticulously established and adhered to to achieve this objective. The review included clinical trials and observational studies evaluating patient-reported satisfaction outcomes associated with RPDs. Articles from studies with no available data, prosthetic rehabilitations other than RPDs, clinical report cases, case series, and reviews of all kinds were excluded from the study. Similarly, studies that did not assess RPD in terms of satisfaction or with fewer than 20 participants were excluded from the review. The cap for the number of participants was not considered for randomized controlled trials. Also, there is no time limit, all the articles published up to 2023 were included. No specific language was selected; all articles meeting the inclusion criteria were accepted, irrespective of the original language in which the articles were written.
Search strategy and databases
Three databases (MEDLINE/PubMed, Scopus, and Google Scholar) were electronically searched to identify all the relevant studies for articles published up to 2023 with no date language limitations. A supplemental manual search was performed on reference lists of included articles. The following keywords combined with Boolean operators and Medical Subject Headings (MeSH) were used in PubMed and modified for Scopus and Google Scholar (["removable partial denture" OR "partial denture" OR "removable denture" OR "partial edentulous" OR Retention OR "Chewing ability" OR Aesthetics OR "Buccal clasps") AND (satisfaction OR "patient satisfaction" OR "satisfaction rate" OR "patient experience" OR "quality of life" OR PROMs) AND ("dental patients" OR "denture wearers" OR "partial edentulism" OR edentulism) AND ("prosthodontic outcomes" OR "quality of life" OR "outcomes"]).
Selection procedure and data extraction
Reviewers performed a methodical analysis of all study titles, abstracts, and full text. Any disagreements were resolved by discussion to find a consensus during study selection and data extraction. The selection of studies at the database level was performed in the following steps. First, the retrieved articles were imported into a reference management software program (Zotero; Corporation for Digital Scholarship, Vienna, VA), and duplicates were subsequently removed. The remaining studies were then imported into Rayyan (Rayyan Systems, Inc.) where title and abstract screening was performed. The third step involved reading the full text of the selected studies and applying the inclusion and exclusion criteria. Studies not meeting the inclusion criteria were excluded, and the reasons for exclusion were recorded. Data extraction and synthesis were performed including collecting the following data: author and year of publication, study design, number and age of participants, type of denture, follow-up period, satisfaction variables considered, and the main results.
Results
Search Results
A bibliographic search of PubMed and Scopus databases identified 1,139 relevant articles where 216 articles were duplicates. A manual search was done on Google Scholar, where the first 10 pages were considered. The first stage of screening resulted in excluding 837 articles based on title and/or abstract screening. After title and abstract screening, 86 articles remained and were read in full. Fifty-one articles were eliminated based on the inclusion and exclusion criteria; the reasons for exclusion are included in the PRISMA flowchart (Figure 1). Thirty-five articles were finally included that had a clear assessment of the satisfaction of patients with RPDs.
Figure 1. PRISMA flowchart.
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Results of data extraction
The data extraction results are shown in the study descriptor table (Table 1).
Table 1. Study descriptor table.
VAS, visual analog scale; PMMA, polymethyl methacrylate; FPD, fixed partial denture; RPD, removable partial denture; OHRQoL, oral health-related quality of life; TR-RPD, thermoplastic resin-removable partial denture; MC-RPD, conventional metal clasp-retained removable partial denture; IARPD, implant-assisted removable partial denture; MI, mini implant; SD, standard deviation; CD, complete denture
| Author and year | Study design | Sample size | Age range/mean | Gender distribution | Denture | Comparison | Classification | Outcome measures | Outcomes (primary or secondary) | Findings | Country of origin |
| Yoshimoto et al. (2021) [18] | Retrospective cross-sectional | 132 | 71.0 ± 9.0 | 55 men | RPD | - | Kennedy classification II (over 40%) | VAS, Gummy Jelly, and food acceptance status | Masticatory satisfaction | Masticatory satisfaction among RPD wearers was not significantly associated with gender, age, denture wearing jaw, Kennedy classification, and occlusal support. Mean masticatory satisfaction score (VAS) = 75.3 across all participants. | Japan |
| Aljabri et al. (2017) [19] | Retrospective study | 60 | 51.18 ± 13.06 | 30 men | RPD (PMMA-based, nylon-based, and chrome cobalt alloys) | - | Satisfaction Questionnaire | Patient satisfaction | 35% were very satisfied, 21.7% were satisfied, and 23.3% were nearly satisfied. | Saudi Arabia | |
| Fueki et al. (2018) [20] | Randomized cross-over trial | 24 | 67.3 | 36.0% men | TR-RPDs, MC-RPDs | - | - | VAS, Likert Scale | Satisfaction, denture-related parameters | TR-RPDs hold an advantage over MC-RPDs in terms of oral appearance and can offer greater satisfaction than MC-RPDs in partially dentate arches with at least an occluding pair in the posterior region. The mean (±SD) overall satisfaction scores were 87.3 (±15.5) and 81.0 (±17.4) for TR-RPDs and MC-RPDs, respectively. | Japan |
| Shala et al. (2016) [21] | Retrospective study | 63 | 61.4 ± 9.6 | 36 men | RPDs, RPDs with attachment | - | Kennedy class I (34), IA [11], II [10] | Satisfaction Questionnaire | Patient satisfaction | 73.6% of patients were wearing RPD for the first time and were finally satisfied. According to the denture support of RPDs, clasp-retained quadrangular RPDs were 100% effective, followed by triangular dental support at 81% and linear dental support at 47.7%. | Kosovo |
| Akinyamoju et al. (2017) [22] | Quasi-experimental study | 30 | 33.8 ± 10.01 | - | flexible design, acrylic | - | - | VAS, questionnaire | Appearance, ease of cleaning, ability to speak, comfort while eating, and overall satisfaction | Subjects were more satisfied with the flexible RPD than the acrylic resin RPD. 21 (70.0%) participants were more satisfied with the flexible dentures, 6 (20.0%) with acrylic dentures, while 3 (10.0%) were equally satisfied with both types of dentures (P = 0.04). | Nigeria |
| Bilhan et al. (2012) [23] | Retrospective study | 99 | 63.26 ± 9.6 | 44 men | RPD | VAS | Patient satisfaction with several data about the dentures such as denture age, type of denture, centric relation, and vertical dimension | Loss of retention, ulcerations, and high vertical dimension caused patient dissatisfaction. Additionally, dentures with wrong-centric relations caused the need for the addition of artificial teeth. | Turkey | ||
| Negoro et al. (2021) [24] | Prospective study | 27 | 70.8 (7.1/48-83) | 11 men | IARPDs (short implants with magnetic attachments) | - | Kennedy Class I [21] and Class II [9] | VAS | Genera satisfaction, patient denture assessment and OHRQoL | The PDA, general patient satisfaction, and OHRQoL were improved by IARPD with a short implant using a magnetic attachment | Japan |
| Al Jaghsi et al. (2020) [25] | Multi-center randomized clinical trial | 76 | 43-83 | 29 men | Double-crown-retained, clasp-retained, attachment-retained | Satisfaction Questionnaire | General satisfaction, RPD retention, stability, support, eating, speaking, and aesthetics | Strategic MIs improved the satisfaction of patients with RPDs during the medium-term follow-up period. An earlier improvement in the satisfaction of patients with RPDs was seen after immediate loading of the MIs as compared with delayed loading. | Germany | ||
| Koyama et al. (2009) [26] | Retrospective study | 67 | 66.0-9.5 | 18 | RPD | - | - | Satisfaction Questionnaire | Satisfaction outcomes | The continued utilization of RPDs is related to factors such as the patient’s age, location of the edentulous area, number of occluding pairs of teeth, and number of occlusal rests, satisfaction, including pain while using RPDs, the color of the artificial teeth, and tooth shape and setup. | Japan |
| Frank et al. (1998) [27] | Population-based study | 58.6 ± 10.9 | 49.8% women | RPD (Mandibular) | - | - | Satisfaction Questionnaire | Satisfaction outcomes | A majority of survey respondents treated with a mandibular RPD in private dental practice were satisfied with the prosthesis, but a substantial amount of dissatisfaction existed. Dissatisfaction was related to age, health, prior experience with a prosthesis, and the type of opposing dentition. | United States | |
| Celebić and Knezović-Zlatarić (2003) [28] | Retrospective study | 268 | 63 (67 CD) | 35 men (RPD), 57 men (CD), 99 women (CD) | RPD (retained clasps) | CD (156) | - | Analog scale | Satisfaction | CD wearers were significantly more satisfied than RPD wearers with speech, chewing and retention of maxillary denture, while RPD wearers were significantly more satisfied with the retention and the comfort of wearing mandibular denture (P < 0.05). | Croatia |
| Zlatarić and Celebić (2008) [29] | Multiple regression analysis | 103 | 63 | 35 men | RPD | Kennedy Class I | Analogue scale | General patient satisfaction and patient satisfaction with aesthetics, retention, speech, chewing, and comfort | Aesthetics, chewing, and speech had significant effects on the patient’s general satisfaction with dentures. | Croatia | |
| Jensen et al. (2016) [30] | Retrospective study | 21 | - | - | ISRPD | Kennedy class I | VAS | Satisfaction outcomes | The patients scored 8.4 (SD 2.1) on general satisfaction on a 0–10 numeric scale meaning highly satisfied | The Netherlands | |
| Waas et al. (1994) [31] | Cross-sectional study | 320 | 55-75 | - | RPD (acrylic resin [>50%], distal extension [60%]) | - | - | Questionnaire | Satisfaction with the functioning of the dentition, chewing, aesthetics, speech and comfort | No differences in satisfaction were found between subjects with a metal frame prosthesis and an acrylic denture, nor between tooth-bounded and distal extension prostheses. The conclusion can be drawn that the indication for an RPD. should be limited in elderly people unless the RPD increases the number of the occlusal units | The Netherlands |
| Frank et al. (2000) [3] | Retrospective study | 82 | - | - | RPD | - | - | Questionnaire | Clinical acceptability and satisfaction | The standards appear to be unrelated to patient satisfaction. The most important standards are rest form, base extension, and stress distribution. | United States |
| Threeburuth et al. (2008) [32] | Randomized clinical trial | 30 | 64.1 ± 5.56 | 10 men | RPD (immediate-load mini implants, conventional-size implants) | - | Kennedy Class I | VAS | Comfort, retention, and chewing performance | Overall patient satisfaction with implant retained RPDs was significantly higher than with conventional RPDs in both groups (P < .05). Immediate-load mini dental implants can be used to retain mandibular Kennedy class I RPDs successfully if high primary stability is achieved. | Thailand |
| Alqutaibi (2020) [33] | Randomized crossover trial | 10 | 58.7 ± 9.3 | 3 men | RPD (conventional for three months followed by attachment retained for three months) | - | - | VAS | Satisfaction outcomes; cleaning, comfort, aesthetics, stability, mastication, oral condition, and general satisfaction | Higher short-term satisfaction rates in patients with ARRPDs than with the conventional clasp-retained RPDs. The superior aesthetics of ARRPDs are recognized. | Saudi Arabia |
| Kapur et al. (1991) [34] | Retrospective study | 228 | - | - | RPD (115) | FPD (113) | Kennedy Classes I and II | Satisfaction Questionnaire | Satisfaction, chewing, comfort, and safety | Both groups perceived improvement in chewing ability, comfort, and ease of chewing, eating enjoyment, and feeling secure with prostheses. Results support the superiority of the FPD in terms of patient satisfaction, but not enough to favor this type of prosthesis over the RPD without consideration of other pertinent factors. | United States |
| Zlatarić et al. (2003) [16] | Retrospective study | 205 | 38-89 | 80 men | RPD (123 maxillary, 138 mandibular) | - | Kennedy Class I (57.4%) and Class II (28.8%) | Satisfaction Questionnaire | Patient satisfaction | Majority of the patients treated with RPDs were satisfied with the prosthesis. Dissatisfaction was related to mastication, aesthetics, number of missing teeth, and maintenance of oral hygiene. | Croatia |
| Wakabayashi et al. (1998) [35] | Retrospective study | 66 | 61.2 | 24 men | RPD (50 maxillary, 44 mandibular) | - | - | VAS | aesthetics, pain, comfort, stability, ability to speak, chew, and general satisfaction | Female rated lower satisfaction with the comfort of their dentures, Younger patients expressed less satisfaction with the aesthetics than the older patients. The period of wearing dentures correlated with psychological measures of pain, comfort, and general satisfaction. No correlation between general satisfaction with dentures and retention. | Japan |
| Cosme et al. (2006) [36] | Retrospective study | 50 | 36-76 | 11 men | RPD | - | Kennedy Class I [20] | Satisfaction Questionnaire | Patient satisfaction | More than 50% of patients classified their RPDs as excellent regarding retention, mastication, aesthetics, comfort, and hygiene. In the professional evaluation, retention and stability were considered excellent in more than 66% of cases, and hygiene of teeth and prostheses was considered good in 52% and 46%, respectively. | Brazil |
| Al Omiri et al. (2013) [37] | Retrospective study | 68 | 53.2 ± 11.8 | 38 men | RPD [36] | CD [32] | - | Dental Impact on Daily Living Questionnaire | Patient satisfaction | Patients’ satisfaction with oral condition improved following using removable prosthetic rehabilitation with RPD having better impacts than CD. Psychological profiles might play a role and explain prosthetic impacts on daily living and patients’ satisfaction with prostheses | Saudi Arabia |
| Alageel et al. (2019) [38] | Retrospective study | 75 | - | - | RPD (retention) | - | - | McGill Denture Satisfaction Instrument | Patient satisfaction (retention) | RPD retention predicted from the number and position of clasps and missing teeth might help to determine patient satisfaction. In addition, patient satisfaction with RPDs was influenced by the arch type, the presence of a distal extension base, and the number of clasps | Canada |
| Hundan and Madan (2012) [39] | Retrospective study | 30 | 25-45 | - | RPD (flexible and conventional) | - | Kennedy Class II | Satisfaction Questionnaire | Aesthetics, and oral soft tissue tolerance | Statistically significant results were obtained in favor of flexible RPDs, in the parameters of ‘aesthetics’ and ‘overall patient satisfaction’. | India |
| Hartog et al. (2014) [40] | Prospective study | 153 | 38.3 ± 14.7 | 45.7% men | RPD (implant-supported, acrylic resin tissue-supported) | - | - | VAS, Satisfaction Questionnaire | Satisfaction (comfort, function, and aesthetics) | Patient satisfaction with a single-tooth implant in the aesthetic zone is high. Compared with an RPD that patients wore before implant treatment, patient satisfaction improved significantly after implant treatment in terms of function, comfort, and aesthetics | The Netherlands |
| Zlatarić et al. (2000) [41] | Retrospective study | 165 | 38-87 | 59 men | RPD | - | - | Satisfaction Questionnaire | Comfort, function, aesthetics, and general satisfaction | Women were more satisfied with chewing with lower partial dentures than men. Patients with more missing teeth gave lower grades for the comfort of wearing dentures. Patients of higher education gave lower grades for aesthetics. Dissatisfaction was related to mastication, aesthetics, the number of missing teeth, and the ability to speak. | Croatia |
| Khan et al. (2017) [42] | Cross-sectional study | 80 | 57.4 ± 13.1 | - | RPD | - | - | Satisfaction Questionnaire | Patient satisfaction (eating, smiling, emotional, contact with family) | Post-treatment, 76.3% indicated good oral health and satisfaction with no significant differences between the three Kennedy groups. | South Africa |
| Hakestam et al. (1997) [43] | Clinical follow-up study | 42 | - | - | RPD | FPD | - | Satisfaction Questionnaire, California Dental Association (CDA) quality assessment system | Patient satisfaction | The RPDs had a somewhat higher share of nonacceptable appliances according to the CDA criteria. There was an association between the CDA categories and patient satisfaction. | Sweden |
| Almohsen and Mahmoud (2021) [44] | Randomized cross-sectional study | 60 | 52.25 ± 1.8 | 60 men | RPD | - | - | Satisfaction Questionnaire | Satisfaction in chewing, speech, appearance, taste, pain, digestion, and psychological measurements | Most patients were satisfied with their properly fabricated RPDs in almost all seven categories. No significant differences in satisfaction were found regarding the type of the arch, age, and time after delivering the denture | Saudi Arabia |
| Sadek and Elawady (2019) [45] | Randomized Controlled Trial | 42 | - | - | RPD (Thermo press, conventional Vitallium) | - | Kennedy Class II | VAS | Satisfaction | Patient satisfaction and abutment survival were better with Thermo press RPD than conventional Vitallium RPD or Vitallium RPD with a surveyed bridge restoring the modification area. Although a nonstatistically significant difference was found in the survival rate of abutments between groups, a clinically important result was revealed as no abutment failures were reported in the Thermo press group. | Saudi Arabia |
| Persic et al. (2015) [46] | Cross-sectional study | 150 | 61-84 | 72 men | Maxillary RPD (c_RPD (88), PA-RPD (62)) | - | - | Orofacial Esthetic Scale, CFQ | Aesthetics, chewing function | Treatment outcomes were better in the PA-RPD group than the CRPDs. Women showed greater concern for the treatment outcomes; their rates were significantly better than in male patients in the PA-RPD group; however, when their satisfaction was lower, their rates were significantly worse than in male patients (in the C-RPD group). | Switzerland |
| Bortolini et al. (2010) [47] | Cross-sectional study | 32 | - | - | RPD (implant-retained) | - | - | Satisfaction Questionnaire | Patient satisfaction | Implant-retained RPDs are a reliable intermediate solution that can reduce biological and economic costs while maintaining implant treatment benefits and the ease of RPD procedures. | Italy |
| Wismeijer et al. (2011) [48] | Prospective study | 48 | - | - | RPD (Implant-assisted mandibular bilateral distal extension) | - | - | VAS | Patient satisfaction | There were significantly improved parameters of overall satisfaction, stability, chewing and appearance after three years (P < 0.05). There were also improvements in stability, chewing, and overall satisfaction. Speech also improved, but not significantly. Ball abutments (retentive anchors) on the distal implants, as opposed to healing caps, improved patient satisfaction for stability, chewing, and overall satisfaction. | New Zealand |
| Wolfart et al. (2016) [49] | Prospective clinical study | 30 | 64 ± 6 | 8 men, 9 female (RPDP) | RPD | - | - | VAS | Chewing satisfaction | All patients, were very satisfied after therapy concerning the ability to speak, chew, and stability of their prosthesis. Patients with a strongly reduced dentition and edentulous patients benefit from strategically placed implants under the existing removable dentures. | Germany |
| Manzon et al. (2019) [50] | Retrospective study | 120 | 73 | - | VALPLAST-RPD (Polyamide VALPLAST), CoCr-RPD (cobalt chromium alloy), and PMMA-RPD (heat polymerized) | - | - | Satisfaction Questionnaire | Patient satisfaction, including aesthetic, functional, and clinical outcomes | VALPLAST-RPD was the most satisfactory aesthetically. Patients with PMMA-RPD claimed a higher level of encumbrance (P < 0.001) and increased speech difficulties (P = 0.002). Each RPD material utilized may present advantages and disadvantages in an elderly population. | Italy |
Study characteristics: a summary
Five of the included studies were randomized clinical studies [20,32-33,44-45]. Four of the included studies were prospective clinical studies [24,40,49], and one included study was a population-based study [27]. The rest of the included articles were retrospective studies or clinical follow-up studies. Only 10 of the included studies had a sample population of more than 100 patients, with a total of 1,844 patients [16,18,28-29,31,34,40-41,46,50]. Two of the included studies compared RPDs with complete dentures (CDs) [28,37], and two studies compared RPDs with fixed partial dentures (FPDs) [34,43].
General satisfaction
The results from various studies examining satisfaction with RPDs reveal a high rate of satisfaction among patients. Studies reported an overall above-average rate of satisfaction among patients. Aljabri et al. reported 80% satisfaction [19], Shala et al. reported 73.6% satisfaction among first-timers [21], Waas et al. reported 81% satisfaction [31], Zlataric et al. reported 60% satisfaction [41], and Cosme et al. reported more than 50% being satisfied [36]. Other studies similarly reported high levels of general satisfaction among patients wearing RPDs [3,16,27,37,38].
The satisfaction scales that were used vary among articles. All the articles used questionnaires that were completed by the patients in different stages of the treatment. Some articles designed their questionnaires, and other articles used established tools that were already available to assess the satisfaction rates. The most used satisfaction scale was the visual analog scale (VAS), which is a famous scale consisting of a 10 cm horizontal line with two descriptors at the beginning and the end representing the maximum and minimum satisfaction rates. Also scales like the dental impact on daily life (DIDL), McGill Denture Satisfaction Instrument, oral health-related quality of life (OHRQoL) measures, and Chewing Function Quality (CFQ), the Orofacial Esthetic Scale (OES-CRO) were used.
Factors influencing RPD satisfaction
Gender
Frank et al. and Zlataric et al. found no significant difference in the level of satisfaction between men and women [19,27,16,41]. Yoshimoto et al. studied masticatory satisfaction among patients wearing RPD [18]. The authors established that masticatory satisfaction was not associated with gender. Akinyamoju et al. found a gender difference in the satisfaction of the subjects regarding the appearance of the dentures [22]. Females gave a higher mean rank score in terms of satisfaction with the appearance of acrylic partial dentures compared to men. This was also the case for flexible partial dentures. Al Omiri et al. found that females were less satisfied with appearance [37]. Akinyamoju et al. reported that women exhibited a higher mean satisfaction for overall comfort with eating in comparison to men [22]. Wakabayashi et al. reported significantly lower satisfaction among women regarding comfort [35].
Zlataric et al. reported that men were less satisfied with mandibular RPD in terms of mastication as compared to women [16,41]. Persic et al. found that gender alone did not have a significant impact. However, when combined with the factor of RPD retention type, it yielded significant effects. Female patients reacted more intensely than male patients for both RPD groups [46]. Khan et al. reported that, despite women being the majority, most complaints regarding different impacts came from men [42].
Age
Frank et al. reported that older adults were more satisfied with their RPDs except for subjects with opposing RPDs [27]. The authors reported that people younger than 60 expressed more dissatisfaction compared to those above 60. Waas et al. reported that older subjects with an RPD were in general less satisfied and reported more problems than subjects without RPDs [31]. Aljabri et al. found no significant difference in satisfaction rates between patients aged above and below 50 years [29]. Almohsen and Mahmoud found no significant difference in all criteria between patients above 50 and below 50 in all criteria except regarding digestion and taste where older patients were more satisfied [44]. Al Omiri et al. found no significant relationship between age and satisfaction [37].
Akinyamoju et al. found that subjects aged 36-45 years (36.7%) were more satisfied with the appearance of acrylic dentures [22]. Koyama et al. established a statistically significant correlation between age and satisfaction [26]. Wakayabashi et al. found that younger patients were less satisfied with the aesthetics of their dentures compared with older adults [35].
Social Classes
Akinyamoju et al. found that subjects in the lower class were more satisfied with the appearance of the acrylic denture (P = 0.61). Other studies have reported an insignificant influence of socioeconomic status on RPD satisfaction [22].
Experience With RPD
Frank et al. reported that patients who had experience with previous RPDs were more satisfied than the patients with their first-ever RPDs [3,27]. Zlataric et al. found no difference in satisfaction between patients with their first-ever RPDs and those who had previous experience [16,41]. Wakayabashi et al. established that the more experience patients had with their RPDs, the more they were satisfied with their ability to speak [35]. They also reported that patients who visited the clinic shortly after undergoing RPD therapy reported more problems with comfort and pain and were unhappy compared to long-term users. Almohsen and Mahmoud found no significant difference in time of use (less or more than 12 months) and level of satisfaction except in the psychological aspect [44].
Missing Teeth and Classification
Zlatarić et al. reported that patients with many missing teeth in the lower jaw (group 3, more than 10 missing) were less satisfied with comfort in comparison with patients with fewer missing teeth [41]. Zlatarić et al. established that patients with a greater number of missing teeth in the mandible had more uncomfortable RPDs in comparison with the patients with fewer missing teeth [16]. Alageel et al. found that a larger proportion of patients were satisfied with maxillary RPDs compared to mandibular RPDs. Additionally, patients with five missing teeth were more satisfied compared to those with six or more missing teeth [38].
Wakayabashi et al. reported that Kennedy Class IV patients had lower satisfaction with aesthetics compared to Kennedy Classes I and II patients. They also found that patients expressed dissatisfaction with aesthetics in dentures that involved anterior teeth [35]. Almohsen and Mahmoud reported that Kennedy Class III patients had a higher satisfaction rate regarding speech. Kennedy Class III and those with modifications had higher satisfaction regarding digestion and taste [44].
Types of RPD
Aljabri et al. and Akinyamoju et al. found a significant difference in patient satisfaction for metal and flexible RPDs [19,22]. This was about appearance, speech, and comfort while eating. Akinyamoju et al. reported that more subjects were satisfied with flexible dentures in terms of aesthetics, speech, and comfort [22]. Hundan and Madan found flexible dentures superior over casted ones regarding overall satisfaction [39]. Fueki et al. found that thermoplastic resin-removable partial dentures (TR-RPDs) had higher overall satisfaction scores compared to conventional metal clasp-retained removable partial dentures (MC-RPDs) [20]. Satisfaction was a result of appearance, comfort, speech, food impaction, ease of cleaning, denture stability, and mucosal pain. Alqutaibi reported a higher satisfaction rate with ARRPDs compared with conventional RPDs [33]. This was regarding ease of cleaning, speech, comfort, aesthetics, masticatory ability, and stability. Sadek et al. found thermo press RPD with more overall satisfaction compared to conventional RPDs [45]. It had increased retention and adaptation to underlying tissues. Manzon et al. determined that VALPLAST RPD was the most satisfactory for the elderly in terms of aesthetics [50]. PMMA RPD (polyamide) was, however, more suitable for this population considering their decreased masticatory force and softer diets compared to younger populations.
Attachments
Shala et al. reported higher levels of satisfaction for RPDs with attachment compared with RPD with clasps [21]. Alageel et al. reported that patients were more satisfied with supported RPDs than those with distal extension bases [38]. This was in terms of oral condition, mastication, appearance, and retention. Also, RPDs with more than three clasps had higher satisfaction compared with those with two or fewer. Patients were highly satisfied with chewing ability, retention, and aesthetics. Negoro et al. reported on implant-assisted removable partial dentures (IARPDs) with a magnetic attachment, which scored significantly better overall patient satisfaction compared to IARPD with a healing cap [24].
Hartog et al. reported significant improvement in satisfaction with aesthetics, function, and comfort for patients who received implant treatment [40]. Bortolini et al. reported increased patient satisfaction with the combined use of implants and conventional RPDs [47]. Wismeijer et al. studied mandibular implant-assisted RPD and reported improved overall satisfaction, chewing, and stability [48]. Wolfart et al. established that strategic placement of implants resulted in improved masticatory satisfaction when placed under RPD [49].
Complaints
Aljabri et al. reported complaints from 26.7% of the participants regarding pain during eating and speech problems [19]. Koyama et al. found a statistically significant correlation between patient satisfaction and pain, color of denture, and tooth shape [26]. Frank et al. reported that dissatisfaction mainly stemmed from chewing, mouth cleanliness, speech, appearance, and RPD cleanliness [27]. Wakabayashi et al. reported less complaints from patients regarding pain [35].
Comparison
Celebić and Knezović-Zlatarić reported that CD wearers were significantly more satisfied than RPD wearers in terms of chewing, speech, and retention [28]. RPD wearers were more satisfied in terms of retention and comfort. There was no difference regarding general satisfaction. Al Omiri et al. reported greater satisfaction for patients with partial dentures compared to CDs [37]. Kapur et al. found FPDs superior in terms of patient satisfaction; however, RPD was superior when other pertinent factors were considered [34]. Hakestam et al. used a quality assessment scale and found that high-quality assessment scores were associated with more satisfaction; RPDs compared to FPDs had less desirable quality factors [43].
Summary of results
This systematic review examined overall satisfaction with RPDs and explored how factors such as gender, age, social class, experience with RPDs, number and classification of missing teeth, types of RPDs, and attachments influenced patient satisfaction. The overall results suggested high satisfaction rates [3,19,21,31,36-38,41-42]. The reported satisfaction rates were 80% [19,21], 81% [31], 60% [41], and >50% [36]. Age was found to impact satisfaction, with older adults generally expressing higher levels of satisfaction. Gender differences were also observed, particularly in the context of appearance satisfaction [22,35]. Prior RPD experience correlated positively with satisfaction [15,27,41], and the number and location of missing teeth influenced satisfaction [15,38,41]. The type of RPD significantly affected satisfaction, with notable differences between metal and flexible RPDs [19-20,22]. Attachments, such as magnetic attachments and implants, increased satisfaction [21,40]. Patient complaints varied, with pain, aesthetics, and cleanliness being common sources of dissatisfaction [19,26,41]. These findings show the need for a personalized approach in RPD treatment to optimize patient satisfaction and OHRQoL.
Discussion
RPDs are a prevalent and adaptable prosthodontics treatment modality, addressing the problems of partial edentulism and resulting in the restoration of oral function and aesthetics among different populations. Prostheses are commonly used by patients with several missing teeth but retain some natural dentition. They are designed to enhance mastication, preserve the remaining teeth, and restore the integrity of the oral cavity. The success of the use of RPDs extends beyond the technicalities of their design and fabrication to include aspects of oral health quality of life and patient satisfaction. The use of RPDs should feel as natural as possible for patients, and examining the narratives of patients who wear them is critical in understanding areas for improvement. Patient satisfaction is a complex construct that assesses individual subjective experiences, perceptions, and contentment with oral health-related outcomes. Several factors contribute to patient satisfaction with RPDs, including fit and comfort, aesthetics and appearance, functional performance, psychosocial effect, and prior experience and expectations.
This study established that the majority of the patients are satisfied with their RPDs [3,16,19,21,27,31,36-38,41-42], with most reviewed studies reporting an above-average general satisfaction. Several factors contribute to the lack of patient satisfaction in the use of RPDs, and all this relates to the age of the patient, retention of RPD, poor denture fit, and adaptive capacity. Ill-fitting dentures can lead to discomfort, pain, and compromised functionality. Dentures that enhance, rather than hinder, mastication and speech functions contribute to an overall positive experience among patients. Psychosocial issues such as self-esteem, confidence, and the ability to engage socially are influenced by the denture's impact on oral function and aesthetics. Patients' prior experiences with dental prosthetics and their expectations regarding RPD outcomes play a role in shaping satisfaction. Aligning patient expectations with realistic outcomes is pivotal for achieving high levels of satisfaction.
Age emerged as a noteworthy factor influencing RPD satisfaction. Frank et al. noted that older adults generally expressed higher satisfaction, with dissatisfaction more prevalent among individuals under 60, especially in cases of opposing RPDs [27]. However, Waas et al. reported that older subjects were less satisfied [31]. Other studies, such as those by Almohsen and Mahmoud and Akinyamoju et al., found no consistent correlation between age and satisfaction [44,22]. The nuanced relationship between age and satisfaction underscores the need for a personalized approach to address the diverse preferences of different age groups.
The influence of gender on RPD satisfaction appeared to vary across different aspects. Studies by Frank et al., Aljabri et al., and Zlatarić et al. found no substantial difference in overall satisfaction between men and women [27,19,41,16]. However, disparities arise when specific elements are considered. Akinyamoju et al. observed that women exhibited higher satisfaction with the appearance of both acrylic and flexible partial dentures [22]. Conversely, Wakabayashi et al. reported lower satisfaction among women regarding comfort [35]. These findings suggest that gender-related factors can play a role in specific facets of RPD satisfaction.
Experience with RPDs emerged as a consistent predictor of satisfaction. Patients with prior RPD experience, as reported by Frank et al. and Zlatarić et al., tended to express higher satisfaction than those with their first-ever RPDs [27,16,41]. Long-term users, as highlighted by Wakayabashi et al., demonstrated increased satisfaction, particularly in terms of speech [35]. The positive correlation between experience and satisfaction emphasizes the importance of patient adaptation and acclimatization over time.
The number and location of missing teeth seemed to play a crucial role in RPD satisfaction. Zlatarić et al. observed that patients with more missing teeth, especially in the mandible, reported lower satisfaction, highlighting the importance of denture stability and comfort [16,41]. The classification of RPDs, such as Kennedy Class, also influences satisfaction, with Kennedy Class IV patients expressing lower satisfaction with aesthetics, as noted by Wakayabashi et al. [35].
The type of RPD significantly affected satisfaction rates. Studies by Aljabri et al. and Akinyamoju et al. revealed notable differences in satisfaction between metal and flexible RPDs, particularly in appearance, speech, and comfort while eating [19,22]. Fueki et al. reported higher overall satisfaction with thermoplastic resin RPDs compared to metal-cast RPDs, citing factors such as appearance, comfort, and stability [20].
The use of attachments, such as magnetic attachments and implants, significantly impacted satisfaction. Shala et al. found higher satisfaction for RPDs with attachments compared to those with clasps [21]. Hartog et al. reported improved satisfaction with aesthetics, function, and comfort for patients who received implant treatment, suggesting a positive correlation between implant-assisted RPDs and overall satisfaction [40].
The satisfaction rates of patients using RPDs are shown to be influenced by several factors. These findings highlight the importance of individualized approaches in RPD treatment, considering the diverse preferences and needs of patients across different demographic and clinical contexts. Further research is needed to better understand the complexities of these factors and how they affect RPD satisfaction.
The heterogeneity in the scales used to evaluate patient satisfaction was observed as a limitation, hindering meta-analysis. Further studies are needed to standardize the tools assessing patient satisfaction and correlate them with other factors. Additionally, further work is needed to evaluate the interactions between the different variables affecting patient satisfaction. This would enable a better understanding of the most important factors in satisfaction and their interactions.
Conclusions
In conclusion, this systematic review provides valuable insights into the satisfaction of patients with RPDs and the factors influencing their experiences. The overall findings indicate a high level of satisfaction among RPD wearers, with reported satisfaction rates ranging from 50% to 81% across various studies. The study characteristics, including the diverse methodologies employed, contribute to a comprehensive understanding of the factors influencing satisfaction.
Age emerged as a notable factor affecting RPD satisfaction, with older adults generally expressing higher levels of satisfaction, particularly when not dealing with opposing RPDs. Gender differences played a role in specific aspects of satisfaction, such as appearance, with women tending to exhibit higher satisfaction in this regard. Experience with RPDs consistently correlated with higher satisfaction, emphasizing the importance of patient adaptation and acclimatization over time.
The number and location of missing teeth, as well as the classification of RPDs, demonstrated significant impacts on satisfaction. Patients with more missing teeth, especially in the mandible, reported lower satisfaction, highlighting the importance of denture stability and comfort. The type of RPD, whether metal or flexible, significantly influenced satisfaction rates, with thermoplastic resin RPDs often being associated with higher overall satisfaction.
The use of attachments, such as magnetic attachments and implants, emerged as a critical factor positively impacting satisfaction. RPDs with attachments, as well as implant-assisted RPDs, were associated with higher levels of overall satisfaction, suggesting the potential benefits of incorporating advanced prosthodontic techniques.
Complaints from patients, including issues related to pain, aesthetics, and cleanliness, underscore the need for continued improvement in RPD design and fabrication. These findings collectively emphasize the importance of individualized approaches in RPD treatment, considering the diverse preferences and needs of patients across different demographic and clinical contexts.
In conclusion, while the overall satisfaction with RPDs is encouraging, further research is warranted to delve deeper into the complexities of these factors and their interplay to optimize patient satisfaction and OHRQoL in RPD wearers.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Mohammed Awawdeh, Abdualrhman H. Alharbi, Turki S. Alasiri, Naif Ibrahim Alrashidi, Sultan A. Alnafisah, Meshari B. Alotaibi
Acquisition, analysis, or interpretation of data: Mohammed Awawdeh, Abdualrhman H. Alharbi, Turki S. Alasiri, Naif Ibrahim Alrashidi, Sultan A. Alnafisah, Meshari B. Alotaibi
Drafting of the manuscript: Mohammed Awawdeh, Abdualrhman H. Alharbi, Turki S. Alasiri, Naif Ibrahim Alrashidi, Sultan A. Alnafisah, Meshari B. Alotaibi
Critical review of the manuscript for important intellectual content: Mohammed Awawdeh, Abdualrhman H. Alharbi, Turki S. Alasiri, Naif Ibrahim Alrashidi, Sultan A. Alnafisah, Meshari B. Alotaibi
Supervision: Mohammed Awawdeh, Abdualrhman H. Alharbi, Turki S. Alasiri, Naif Ibrahim Alrashidi, Sultan A. Alnafisah, Meshari B. Alotaibi
References
- 1.Carr AB, Brown DT. McCracken’s removable partial prosthodontics (13th Edition) St. Louis, MO: Elsevier; 2015. McCracken’s Removable Partial Prosthodontics, 13th ed. [Google Scholar]
- 2.Treatment protocol for denture stomatitis, prior to anatomical molding. Milton Rocha Gusmão J, Pereira RP. Gerodontology. 2013;30:232–235. doi: 10.1111/j.1741-2358.2012.00661.x. [DOI] [PubMed] [Google Scholar]
- 3.Relationship between the standards of removable partial denture construction, clinical acceptability, and patient satisfaction. Frank RP, Brudvik JS, Leroux B, et al. https://doi.org/10.1016/s0022-3913(00)70008-4. J Prosthet Dent. 2000;83:521–527. doi: 10.1016/s0022-3913(00)70008-4. [DOI] [PubMed] [Google Scholar]
- 4.Oral health status of patients 5-6 years after placement of cobalt-chromium removable partial dentures. Yeung AL, Lo EC, Chow TW, Clark RK. https://doi.org/10.1046/j.1365-2842.2000.00512.x. J Oral Rehabil. 2000;27:183–189. doi: 10.1046/j.1365-2842.2000.00512.x. [DOI] [PubMed] [Google Scholar]
- 5.Stewart’s clinical removable partial prosthodontics, 4th ed. Hsu C-J. J Prosthodont. 2009;18:711. [Google Scholar]
- 6.Prosthetic status: the formation of a schedule. Hoad-Reddick G, Grant AA. J Prosthet Den. 1988;1:105–110. doi: 10.1016/0022-3913(88)90118-7. [DOI] [PubMed] [Google Scholar]
- 7.Effect of implant support on distal extension removable partial dentures: in vitro assessment. Ohkubo C, Kurihara D, Shimpo H, Suzuki Y, Kokubo Y, Hosoi T. https://doi.org/10.1111/j.1365-2842.2006.01641.x. J Oral Rehabil. 2007;34:52–56. doi: 10.1111/j.1365-2842.2006.01641.x. [DOI] [PubMed] [Google Scholar]
- 8.Consumer satisfaction. Reifel NM, Rana H, Marcus M. https://doi.org/10.1177/08959374970110021101. Adv Dent Res. 1997;11:281–290. doi: 10.1177/08959374970110021101. [DOI] [PubMed] [Google Scholar]
- 9.Evaluation of stain removal and inhibition properties of eight denture cleansers: an in vitro study. Al-Huraishi H, Moran J, Jagger R, MacDonald E. Gerodontology. 2013;30:10–17. doi: 10.1111/j.1741-2358.2011.00522.x. [DOI] [PubMed] [Google Scholar]
- 10.Comparative stain removal properties of four commercially available denture cleaning products: an in vitro study. Alam M, Jagger R, Vowles R, Moran J. Int J Dent Hyg. 2011;9:37–42. doi: 10.1111/j.1601-5037.2009.00432.x. [DOI] [PubMed] [Google Scholar]
- 11.Periodontal findings in patients 10 years after insertion of removable partial dentures. Kern M, Wagner B. https://doi.org/10.1111/j.1365-2842.2001.00788.x. J Oral Rehabil. 2001;11:991–997. doi: 10.1046/j.1365-2842.2001.00788.x. [DOI] [PubMed] [Google Scholar]
- 12.Oral candidiasis: pathogenesis, clinical presentation, diagnosis and treatment strategies. Lalla RV, Patton LL, Dongari-Bagtzoglou A. https://pubmed.ncbi.nlm.nih.gov/23705242. J Calif Dent Assoc. 2013;41:263–268. [PubMed] [Google Scholar]
- 13.Periodontal status of teeth in contact with denture in removable partial denture wearers. Yusof Z, Isa Z. J Oral Rehabil. 1994;21:77–86. doi: 10.1111/j.1365-2842.1994.tb01126.x. [DOI] [PubMed] [Google Scholar]
- 14.Effect of acrylic removable partial denture in caries prevalence among diabetic and non-diabetic patients. Ambikathanaya UK, Swamy KR, Gujjari AK, Tejaswi S, Shetty S, Ravi MB. https://doi.org/10.4103/jpbs.jpbs_126_22. J Pharm Bioallied Sci. 2022;14:0–22. doi: 10.4103/jpbs.jpbs_126_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shape optimization for additive manufacturing of removable partial dentures-a new paradigm for prosthetic CAD/CAM. Chen J, Ahmad R, Suenaga H, Li W, Sasaki K, Swain M, Li Q. https://doi.org/10.1371/journal.pone.0132552. PLoS One. 2015;10:0. doi: 10.1371/journal.pone.0132552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.A survey of treatment outcomes with removable partial dentures. Knezović Zlatarić D, Celebić A, Valentić-Peruzović M, Jerolimov V, Pandurić J. J Oral Rehabil. 2003;30:847–854. doi: 10.1046/j.1365-2842.2003.01039.x. [DOI] [PubMed] [Google Scholar]
- 17.The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Page MJ, McKenzie JE, Bossuyt PM, et al. BMJ. 2021;372:0. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Factors affecting masticatory satisfaction in patients with removable partial dentures. Yoshimoto T, Hasegawa Y, Salazar S, Kikuchi S, Hori K, Ono T. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18126620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Removable partial dentures: Patient satisfaction and complaints in Makkah City, KSA. Aljabri MK, Ibrahim TO, Sharka RM. J Taibah Univ Med Sci. 2017;12:561–564. doi: 10.1016/j.jtumed.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patient satisfaction and preference with thermoplastic resin removable partial dentures: a randomised cross-over trial. Fueki K, Yoshida-Kohno E, Inamochi Y, Wakabayashi N. https://doi.org/10.1016/j.jpor.2019.05.003. J Prosthodont Res. 2020;64:20–25. doi: 10.1016/j.jpor.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 21.Patient’s satisfaction with removable partial dentures: a retrospective case series. Shala KS, Dula LJ, Pustina-Krasniqi T, Bicaj T, Ahmedi EF, Lila-Krasniqi Z, Tmava-Dragusha A. Open Dent J. 2016;10:656–663. doi: 10.2174/1874210601610010656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Comparison of patient satisfaction with acrylic and flexible partial dentures. Akinyamoju CA, Ogunrinde TJ, Taiwo JO, Dosumu OO. https://doi.org/10.4103/npmj.npmj_54_17 . Niger Postgrad Med J. 2017;24:143–149. doi: 10.4103/npmj.npmj_54_17. [DOI] [PubMed] [Google Scholar]
- 23.Complication rates and patient satisfaction with removable dentures. Bilhan H, Erdogan O, Ergin S, Celik M, Ates G, Geckili O. https://doi.org/10.4047/jap.2012.4.2.109. J Adv Prosthodont. 2012;4:109–115. doi: 10.4047/jap.2012.4.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patient-reported outcomes of implant-assisted removable partial dentures with magnetic attachments using short implants: a prospective study. Negoro M, Kanazawa M, Sato D, et al. https://doi.org/10.2186/jpr.jpr_d_20_00221. J Prosthodont Res. 2021;65:554–558. doi: 10.2186/jpr.JPR_D_20_00221. [DOI] [PubMed] [Google Scholar]
- 25.Immediate versus delayed loading of strategic mini-implants under existing removable partial dentures: patient satisfaction in a multi-center randomized clinical trial. Al Jaghsi A, Heinemann F, Biffar R, Mundt T. https://doi.org/10.1007/s00784-020-03360-y. Clin Oral Investig. 2021;25:255–264. doi: 10.1007/s00784-020-03360-y. [DOI] [PubMed] [Google Scholar]
- 26.Evaluation of factors affecting the continuing use and patient satisfaction with removable partial dentures over 5 years. Koyama S, Sasaki K, Yokoyama M, Sasaki T, Hanawa S. https://doi.org/10.1016/j.jpor.2009.11.007. J Prosthodont Res. 2010;54:97–101. doi: 10.1016/j.jpor.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 27.Treatment outcomes with mandibular removable partial dentures: a population-based study of patient satisfaction. Frank RP, Milgrom P, Leroux BG, et al. J Prosthet Dent. 1998;80:36–45. doi: 10.1016/s0022-3913(98)70089-7. [DOI] [PubMed] [Google Scholar]
- 28.A comparison of patient’s satisfaction between complete and partial removable denture wearers. Celebić A, Knezović-Zlatarić D. J Dent. 2003;7:445–451. doi: 10.1016/s0300-5712(03)00094-0. [DOI] [PubMed] [Google Scholar]
- 29.Factors related to patients’ general satisfaction with removable partial dentures: a stepwise multiple regression analysis. Zlatarić DK, Celebić A. https://www.quintpub.com/journals/ijp/abstract.php?iss2_id=257&article_id=3149&article=16&title=Short. Int J Prosthodont. 2008;21:86–88. [PubMed] [Google Scholar]
- 30.Implant-supported mandibular removable partial dentures; patient-based outcome measures in relation to implant position. Jensen C, Raghoebar GM, Kerdijk W, Meijer HJ, Cune MS. https://doi.org/10.1016/j.jdent.2016.10.008. J Dent. 2016;55:92–98. doi: 10.1016/j.jdent.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 31.Relationship between wearing a removable partial denture and satisfaction in the elderly. Van Waas M, Meeuwissen J, Meuwissen R, Käyser A, Kalk W, Van 't Hof M. Community Dent Oral Epidemiol. 1994;22:315–318. doi: 10.1111/j.1600-0528.1994.tb02059.x. [DOI] [PubMed] [Google Scholar]
- 32.Comparison of immediate-load mini dental implants and conventional-size dental implants to retain mandibular Kennedy class I removable partial dentures: a randomized clinical trial. Threeburuth W, Aunmeungtong W, Khongkhunthian P. https://doi.org/10.1111/cid.12646. Clin Implant Dent Relat Res. 2018;20:785–792. doi: 10.1111/cid.12646. [DOI] [PubMed] [Google Scholar]
- 33.A within-subject comparison of the conventional clasp-retained with attachment-retained removable partial dentures. Alqutaibi AY. https://doi.org/10.1016/j.jtumed.2020.05.005. J Taibah Univ Med Sci. 2020;15:305–311. doi: 10.1016/j.jtumed.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Veterans administration cooperative dental implant study—comparisons between fixed partial dentures supported by blade-vent implants and removable partial dentures Part IV: comparisons of patient satisfaction between two treatment modalities. Kapur KK. https://doi.org/10.1016/0022-3913(91)90516-y. J Prosthet Dent. 1991;66:517–529. doi: 10.1016/0022-3913(91)90516-y. [DOI] [PubMed] [Google Scholar]
- 35.The influence of some demographic and clinical variables on psychosomatic traits of patients requesting replacement removable partial dentures. Wakabayashi N, Yatabe M, Ai M, Sato M, Nakamura K. J Oral Rehabil. 1998;25:507–512. doi: 10.1046/j.1365-2842.1998.00264.x. [DOI] [PubMed] [Google Scholar]
- 36.Functional evaluation of oral rehabilitation with removable partial dentures after five years. Cosme DC, Baldisserotto SM, Fernandes Ede L, Rivaldo EG, Rosing CK, Shinkai RS. J Appl Oral Sci. 2006;14:111–116. doi: 10.1590/S1678-77572006000200009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Relationship between impacts of removable prosthodontic rehabilitation on daily living, satisfaction and personality profiles. Al-Omiri MK, Sghaireen MG, Al-Qudah AA, Hammad OA, Lynch CD, Lynch E. https://doi.org/10.1016/j.jdent.2013.12.010. J Dent. 2014;42:366–372. doi: 10.1016/j.jdent.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 38.Evaluation of the design-driven prediction of removable partial denture retention. Alageel O, Ashraf N, Bessadet M, Nicolas E, Tamimi F. https://doi.org/10.1016/j.prosdent.2019.10.005. J Prosthet Dent. 2020;124:357–364. doi: 10.1016/j.prosdent.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 39.Comparative clinical evaluation of removable partial dentures made of two different materials in Kennedy Applegate class II partially edentulous situation. Hundal M, Madan R. https://doi.org/10.1016/j.mjafi.2012.08.020. Med J Armed Forces India. 2015;71:0–12. doi: 10.1016/j.mjafi.2012.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patient satisfaction with single-tooth implant therapy in the esthetic zone. Hartog L, Meijer HJ, Santing HJ, Vissink A, Raghoebar GM. https://doi.org/10.11607/ijp.3672. Int J Prosthodont. 2014;27:226–228. doi: 10.11607/ijp.3672. [DOI] [PubMed] [Google Scholar]
- 41.The satisfaction with the removable partial denture therapy in the Croatian adult population. Zlatarić DK, Celebić A, Valentić-Peruzović M, Celić R, Filipović-Zore I, Baucić M. https://pubmed.ncbi.nlm.nih.gov/11216416/ Coll Antropol. 2000;24:485–494. [PubMed] [Google Scholar]
- 42.Impact of removable partial dental prostheses on the oral health-related quality of life of a South African cohort with varied distributions of missing posterior teeth. Khan S, Chikte U, Omar R. https://doi.org/10.1111/jopr.12692. J Prosthodont. 2019;28:0–9. doi: 10.1111/jopr.12692. [DOI] [PubMed] [Google Scholar]
- 43.Does the quality of advanced prosthetic dentistry determine patient satisfaction? Hakestam U, Karlsson T, Söderfeldt B, Rydén O, Glantz PO. https://doi.org/10.3109/00016359709059201. Acta Odontol Scand. 1997;55:365–371. doi: 10.3109/00016359709059201. [DOI] [PubMed] [Google Scholar]
- 44.Patients satisfaction with removable partial dentures in Qassim Region, Saudi Arabia. Almohsen O, Mahmoud M. https://doi.org/10.24911/ijmdc.51-1613946608 Int J Med. 2021;5:1066–1071. [Google Scholar]
- 45.Impact of removable partial denture type on patient satisfaction and abutment survival rate-RCT. Sadek SA, Elawady D. https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/31666857/ Open Access Maced J Med Sci. 2019;7:2513–2519. doi: 10.3889/oamjms.2019.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Influence of different prosthodontic rehabilitation options on oral health-related quality of life, orofacial esthetics and chewing function based on patient-reported outcomes. Peršić S, Čelebić A. https://doi.org/10.1007/s11136-014-0817-2. Qual Life Res. 2015;24:919–926. doi: 10.1007/s11136-014-0817-2. [DOI] [PubMed] [Google Scholar]
- 47.Implant-retained removable partial dentures: an 8-year retrospective study. Bortolini S, Natali A, Franchi M, Coggiola A, Consolo U. https://doi.org/10.1111/j.1532-849x.2011.00700.x. J Prosthodont. 2011;20:168–172. doi: 10.1111/j.1532-849X.2011.00700.x. [DOI] [PubMed] [Google Scholar]
- 48.Multicentre prospective evaluation of implant-assisted mandibular bilateral distal extension removable partial dentures: patient satisfaction. Wismeijer D, Tawse-Smith A, Payne AG. https://doi.org/10.1111/j.1600-0501.2011.02367.x. Clin Oral Implants Res. 2013;24:20–27. doi: 10.1111/j.1600-0501.2011.02367.x. [DOI] [PubMed] [Google Scholar]
- 49.Implant placement under existing removable dental prostheses and its effect on masticatory performance. Wolfart S, Wolf K, Brunzel S, Wolfart M, Caliebe A, Kern M. https://doi.org/10.1007/s00784-016-1746-y. Clin Oral Investig. 2016;20:2447–2455. doi: 10.1007/s00784-016-1746-y. [DOI] [PubMed] [Google Scholar]
- 50.Patient and clinical evaluation of traditional metal and polyamide removable partial dentures in an elderly cohort. Manzon L, Fratto G, Poli O, Infusino E. https://doi.org/10.1111/jopr.13102. J Prosthodont. 2019;28:868–875. doi: 10.1111/jopr.13102. [DOI] [PubMed] [Google Scholar]