Abstract
Objective:
Alcohol-related problems (e.g., physical, interpersonal, intrapersonal, impulse control, social responsibility) can have an impact on posttraumatic stress disorder (PTSD) symptoms during treatment. Evidence-based online self-help tools exist to target alcohol use and related problems and co-occurring PTSD symptoms. It is unknown to what degree individuals with varying alcohol-related problems respond differently to web-based interventions for hazardous alcohol use and PTSD. The current study evaluated specific alcohol-related problems as potential moderators of PTSD symptom changes during the VetChange online intervention while controlling for average daily alcohol use, gender, race, and age.
Method:
We conducted a secondary analysis of a randomized controlled trial that included 600 post-9/11 veterans (518 men and 82 women). Mixed-effects regression models of alcohol-related problems on PTSD severity scores over time were performed separately in an initial intervention group (IIG; n = 404) and a delayed intervention group (DIG; n = 196) that was used as a comparison condition.
Results:
Interpersonal problems emerged as a moderator of PTSD symptom changes in IIG such that veterans endorsing greater interpersonal problems demonstrated larger reductions in PTSD symptoms throughout VetChange. There were no significant moderation effects in DIG. Non-White veterans reported significantly higher PTSD symptoms during VetChange. Post hoc analyses indicated that veterans with higher interpersonal problems were more likely to engage in online intervention content focused on identifying high-risk drinking situations and coping with symptoms.
Conclusions:
Findings imply that veterans reporting alcohol-related interpersonal problems may benefit the most from, and be more motivated to use, online interventions for hazardous alcohol use and PTSD symptoms.
Hazardous drinking (i.e., consuming alcohol above recommended guidelines, Dawson et al., 2005; U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2010) and posttraumatic stress disorder (PTSD) frequently co-occur, with 55%–68% of veterans with probable PTSD also meeting criteria for alcohol use disorder (AUD; Dworkin et al., 2018), and 63% of veterans with hazardous drinking being diagnosed with PTSD (Seal et al., 2011). Research supports a functional link between AUD and PTSD (Simons et al., 2018; Straus et al., 2018; van Dam et al., 2012) insofar as symptoms from both disorders may mutually maintain and exacerbate each other (Mahoney et al., 2020; Simpson et al., 2014). The physical effects of heavy drinking can worsen inter- and intrapersonal symptoms of PTSD (e.g., social isolation, irritability), which can lead to cyclical increases in alcohol use to cope with mounting difficulties (Simpson et al., 2014; Straus et al., 2018).
Although veterans with comorbid AUD and PTSD are more likely to use mental health services compared to veterans with either diagnosis alone (Blanco et al., 2013), they often do not fully engage in or frequently drop out of treatment (e.g., Roberts et al., 2015; Szafranski et al., 2017). Concurrent interventions targeting co-occurring AUD and PTSD have been developed to improve treatment outcomes (Back et al., 2019; Simpson et al., 2021). However, veterans may not receive concurrent treatment for many reasons, including stigma, scheduling conflicts, or transportation (Burnett-Zeigler et al., 2011; Hoge et al., 2004). Web-based interventions designed to alleviate co-occurring AUD and PTSD symptoms may address these barriers by expanding treatment reach and access to care (Brief et al., 2011; McLean et al., 2010).
VetChange, an online modular intervention, was developed to target co-occurring hazardous alcohol use and PTSD symptoms in post-9/11 veterans (Brief et al., 2011, 2013). A randomized clinical trial (RCT) found that participants who completed this intervention reported substantial reductions in alcohol use, alcohol-related problems (based on a combined total score), and PTSD symptoms (Brief et al., 2013). Subsequent moderator analyses showed larger improvements in alcohol use and related problems over time among those with greater PTSD severity (Brief et al., 2018). However, the extent to which specific alcohol-related problems moderate changes in PTSD symptoms during VetChange remains an unknown but important factor to investigate in identifying person-level moderators of treatment response. Thus, the present study extends previous research on VetChange by determining who may benefit most from this online intervention based on reports of different alcohol-related problems measured at baseline.
Research supports the longitudinal linkage of PTSD symptoms and alcohol consumption and related problems over time among post-9/11 veterans (Mahoney et al., 2020; Simons et al., 2018). Miller et al. (1995) suggested that alcohol-related problems can include physical health consequences (e.g., sleeping problems, sickness), interpersonal difficulties (e.g., loss of friendship or intimate relationship), intrapersonal stress (e.g., feeling bad or guilty), impulsivity (e.g., risk-taking behaviors), or conflicts in personal relationships (e.g., work/school problems). In Iraq and Afghanistan veterans, alcohol-related problems are positively associated with PTSD symptoms beyond alcohol consumption, which may be explained by PTSD severity and alcohol-related problems exacerbating each other via intrapersonal dysregulation, impulsivity, and externalizing behaviors (Gaher et al., 2014; Hahn et al., 2015). Although evidence appears to support a robust relation between alcohol-related problems and PTSD symptoms, no study to date, to our knowledge, has directly tested the moderating effect of specific alcohol-related problems on PTSD symptom changes in individuals using a web-based intervention targeting hazardous alcohol use and PTSD. This area is important for further exploration to provide a more nuanced understanding of individual treatment responses and treatment efficacy for co-occurring disorders.
Alcohol-related problems have been implicated in treatment utilization with researchers suggesting that inter- and intrapersonal problems contribute to motivation for therapy (Conner et al., 2022). Thus, specific alcohol-related problems may be associated with motivation to engage in an online self-help intervention for hazardous drinking and PTSD symptoms. This relation is crucial to understand for designing effective web-based interventions because these interventions can only be responsive to users’ needs and preferences to the extent that they become known. The clear clinical implication is that the efficacy of evidence-based self-help interventions can be improved if we are able to better match intervention content with the needs of those who may benefit from them (Kraemer et al., 2006). Knowing whether specific alcohol-related problems moderate PTSD symptom change should help to elucidate this mechanism.
Our study aims to address a gap in the literature by evaluating specific alcohol-related problems as potential moderators of PTSD symptom changes during use of a web-based intervention. Using data from an existing RCT of VetChange (Brief et al., 2013), we compared the moderating effects of alcohol-related problems on changes in PTSD severity scores over time in an initial intervention group (IIG) while they had access to VetChange and a delayed intervention group (DIG) comparison condition before they received access to VetChange. Given that the present study examines changes in PTSD severity only over the first 8 weeks before DIG received access to VetChange, we hypothesized that specific alcohol-related problems would moderate PTSD symptoms in the IIG but not DIG group because those in DIG did not receive the intervention. We predicted that moderation effects would indicate that participants with higher levels of specific alcohol-related problems at baseline would show greater PTSD symptom reductions during VetChange. Because of alcohol-related problems not being pre-specified as a moderator of PTSD severity in the VetChange research protocol (Brief et al., 2011), we conducted analyses in an exploratory manner that used initial multilevel models to identify which specific alcohol-related problems robustly related to changes in PTSD severity and then those identified variables were tested as potential moderators in final models.
Method
Participants
This study is a secondary analysis of data from an RCT (Brief et al., 2013) that evaluated the efficacy of a web-based intervention for hazardous drinking and co-occurring PTSD symptoms. All procedures were approved separately by the institutional review boards of a medical center and university. The parent trial's inclusion criteria were (a) being a veteran of the Afghanistan and/or Iraq wars, (b) age 18 years or older, (c) having an Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 1992; Bradley et al., 2003) score in the at-risk drinking range (5–25 for women, 8–25 for men; veterans were excluded if their score was greater than 25), (d) currently drinking alcohol above daily (<3/4 per day for women/men) or weekly (<7/14 per week for women/men) recommendations (Dawson et al., 2005; U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2010) as measured by the Quick Drink Screen (QDS; Sobell et al., 2003), and (e) willing to share email address for contact purposes.
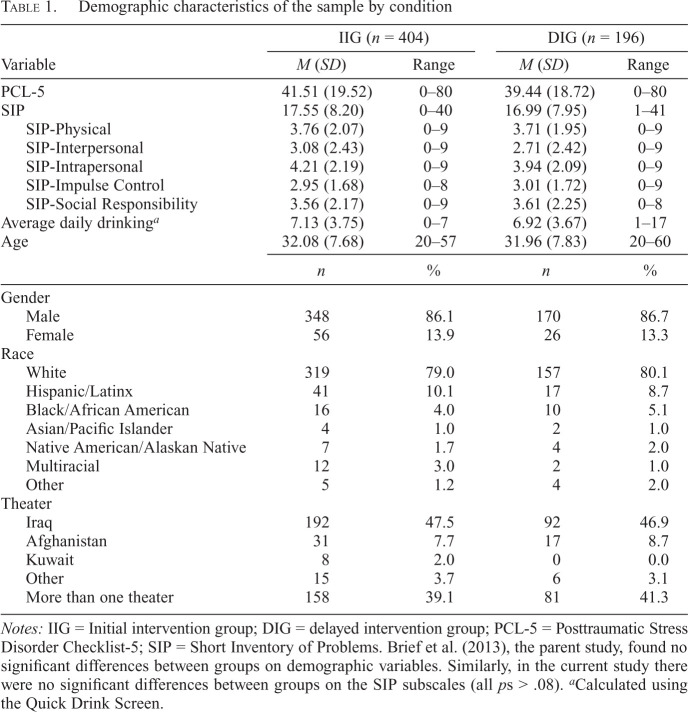
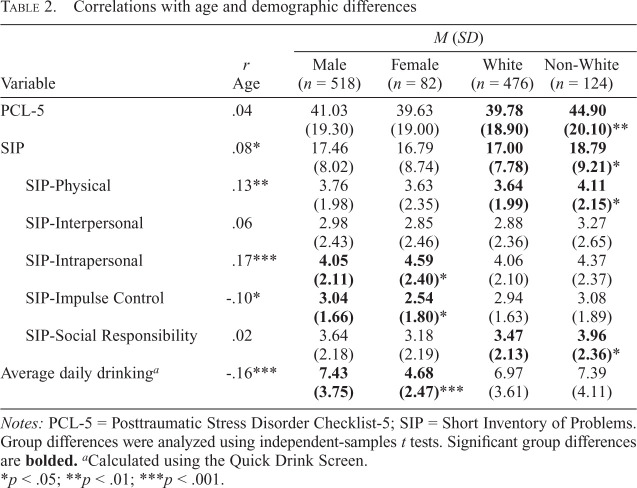
The parent trial's total sample was 600 veterans. Although PTSD severity and diagnosis were not specific inclusion criteria, 386 (64.30%) participants scored at or above the established cutoff of 33 on the PTSD Checklist-5 (PCL-5) for clinically significant PTSD symptoms indicative of probable PTSD (Bovin et al., 2016). Veterans with probable PTSD (M = 19.38, SD = 8.04) compared to those without (M = 13.74, SD = 6.92) reported significantly greater alcohol-related problems at baseline, t(598) = -8.64, p < .001, Cohen's d = -0.74. Table 1 presents the sample characteristics and Table 2 displays the study variables’ correlations with age and demographic differences in these variables.
Table 1.
Demographic characteristics of the sample by condition
| Variable | IIG (n = 404) | DIG (n = 196) | ||
|---|---|---|---|---|
| M (SD) | Range | M (SD) | Range | |
| PCL-5 | 41.51 (19.52) | 0–80 | 39.44 (18.72) | 0–80 |
| SIP | 17.55 (8.20) | 0–40 | 16.99 (7.95) | 1–41 |
| SIP-Physical | 3.76 (2.07) | 0–9 | 3.71 (1.95) | 0–9 |
| SIP-Interpersonal | 3.08 (2.43) | 0–9 | 2.71 (2.42) | 0–9 |
| SIP-Intrapersonal | 4.21 (2.19) | 0–9 | 3.94 (2.09) | 0–9 |
| SIP-Impulse Control | 2.95 (1.68) | 0–8 | 3.01 (1.72) | 0–9 |
| SIP-Social Responsibility | 3.56 (2.17) | 0–9 | 3.61 (2.25) | 0–8 |
| Average daily drinkinga | 7.13 (3.75) | 0–7 | 6.92 (3.67) | 1–17 |
| Age | 32.08 (7.68) | 20–57 | 31.96 (7.83) | 20–60 |
| n | % | n | % | |
|---|---|---|---|---|
| Gender | ||||
| Male | 348 | 86.1 | 170 | 86.7 |
| Female | 56 | 13.9 | 26 | 13.3 |
| Race | ||||
| White | 319 | 79.0 | 157 | 80.1 |
| Hispanic/Latinx | 41 | 10.1 | 17 | 8.7 |
| Black/African American | 16 | 4.0 | 10 | 5.1 |
| Asian/Pacific Islander | 4 | 1.0 | 2 | 1.0 |
| Native American/Alaskan Native | 7 | 1.7 | 4 | 2.0 |
| Multiracial | 12 | 3.0 | 2 | 1.0 |
| Other | 5 | 1.2 | 4 | 2.0 |
| Theater | ||||
| Iraq | 192 | 47.5 | 92 | 46.9 |
| Afghanistan | 31 | 7.7 | 17 | 8.7 |
| Kuwait | 8 | 2.0 | 0 | 0.0 |
| Other | 15 | 3.7 | 6 | 3.1 |
| More than one theater | 158 | 39.1 | 81 | 41.3 |
Notes: IIG = Initial intervention group; DIG = delayed intervention group; PCL-5 = Posttraumatic Stress Disorder Checklist-5; SIP = Short Inventory of Problems. Brief et al. (2013), the parent study, found no significant differences between groups on demographic variables. Similarly, in the current study there were no significant differences between groups on the SIP subscales (all ps > .08).
Calculated using the Quick Drink Screen.
Table 2.
Correlations with age and demographic differences
| Variable | M (SD) | ||||
|---|---|---|---|---|---|
| r | Male | Female | White | Non-White | |
| Age | (n = 518) | (n = 82) | (n = 476) | (n = 124) | |
| PCL-5 | .04 | 41.03 | 39.63 | 39.78 | 44.90 |
| (19.30) | (19.00) | (18.90) | (20.10) ** | ||
| SIP | .08* | 17.46 | 16.79 | 17.00 | 18.79 |
| (8.02) | (8.74) | (7.78) | (9.21) * | ||
| SIP-Physical | .13** | 3.76 | 3.63 | 3.64 | 4.11 |
| (1.98) | (2.35) | (1.99) | (2.15) * | ||
| SIP-Interpersonal | .06 | 2.98 | 2.85 | 2.88 | 3.27 |
| (2.43) | (2.46) | (2.36) | (2.65) | ||
| SIP-Intrapersonal | .17*** | 4.05 | 4.59 | 4.06 | 4.37 |
| (2.11) | (2.40) * | (2.10) | (2.37) | ||
| SIP-Impulse Control | -.10* | 3.04 | 2.54 | 2.94 | 3.08 |
| (1.66) | (1.80) * | (1.63) | (1.89) | ||
| SIP-Social Responsibility | .02 | 3.64 | 3.18 | 3.47 | 3.96 |
| (2.18) | (2.19) | (2.13) | (2.36) * | ||
| Average daily drinkinga | -.16*** | 7.43 | 4.68 | 6.97 | 7.39 |
| (3.75) | (2.47) *** | (3.61) | (4.11) | ||
Notes: PCL-5 = Posttraumatic Stress Disorder Checklist-5; SIP = Short Inventory of Problems. Group differences were analyzed using independent-samples t tests. Significant group differences are bolded.
Calculated using the Quick Drink Screen.
p < .05;
p < .01;
p < .001.
Intervention
VetChange is an evidence-based web intervention designed to address hazardous alcohol use and PTSD symptoms for veterans of the Afghanistan and Iraq wars. VetChange is informed by principles of motivation, feedback, and coping that can decrease hazardous drinking and improve PTSD symptoms (e.g., Litz et al., 2004; Miller et al., 2013; Pedersen et al., 2017). Participants were allowed to select any treatment module after completing Module 1, which involves an initial assessment designed to provide personalized feedback on alcohol use severity, alcohol-related problems, comparisons with population-based norms and guidelines for safe drinking, and PTSD symptoms. Module 2 focuses on motivation to change via exercises for decreasing ambivalence, increasing commitment to change, and assessing readiness to change. Module 3 empowers users to decide on a drinking goal (i.e., moderation or abstinence) and outline a plan to achieve this goal. Module 4 guides users to identify high-risk situations for drinking, and then Module 5 helps them cope with internal (i.e., feelings or moods) highrisk drinking situations. In Modules 6 and 7, users choose to learn skills for stress management, anger management, and/or sleep hygiene based on the initial PTSD assessment (i.e., veterans endorsing difficulties with sleep are directed to the sleep hygiene module). Module 8 provides psychoeducation on social support and guides users to create a social support plan. Participants were allowed 8 weeks to complete all modules in the RCT.
Procedure
Study procedures were reported in Brief et al. (2011, 2013). Online informed consent was obtained for all participants. Veterans were recruited using social media ads. Once deemed eligible and enrolled, participants were randomized to either IIG (n = 404), which received the intervention, or DIG (n = 196), which waited 8 weeks to be able to access the intervention. DIG was used as a comparison condition. Data from baseline and post-intervention (i.e., the first 8 weeks of the study before DIG received access to VetChange) were analyzed in the present study. Participants were remunerated with a $20 Amazon gift card for each assessment they completed.
Measures
PTSD Checklist-5. The 20-item PCL-5 (Weathers et al., 2013) is a self-report measure of PTSD symptom severity with strong validity and reliability (e.g., Blevins et al., 2015; Bovin et al., 2016; Wortmann et al., 2016). Participants rate their symptoms over the past month in response to a stressful life event from 0 (not at all) to 4 (extremely). The internal consistencies of the PCL-5 at baseline (Cronbach's α = .96) and post-intervention (Cronbach's α = .97) were excellent.
Short Inventory of Problems. The 15-item Short Inventory of Problems (SIP; Miller et al., 1995) is a self-report measure of alcohol-related problems. Participants rate specific problems based on the frequency at which they occurred over the past 3 months using a scale ranging from 0 (never) to 3 (daily or almost daily). The SIP consists of five subscales, each reflecting a discrete consequence of alcohol use: physical (“Because of my drinking, I have not eaten properly”), interpersonal (“My family has been hurt by my drinking”), intrapersonal (“I have been unhappy because of my drinking”), impulse control (“I have taken foolish risks when I have been drinking”), and social responsibility (“I have failed to do what is expected of me because of my drinking”). The SIP total and subscales exhibit good internal consistency (e.g., Hirchak et al., 2022), reliability (e.g., Bender et al., 2007), and validity (e.g., Allensworth-Davies et al., 2012). Research supports the SIP's five-factor structure (e.g., Kiluk et al., 2013; Marra et al., 2014). The internal consistencies of the SIP subscales ranged from sufficient (Impulse Control, Cronbach's α = .63) to acceptable (Impulse Control, Cronbach's α = .78) at baseline.
Quick Drink Screen. The four-item QDS (Sobell et al., 2003) is a self-report screener that quantifies alcohol use over the past 30 days. We used items 1 (average number of drinking days per week) and 2 (average number of standard drinks per drinking day) to calculate average daily drinking at baseline (i.e., summing these two items and then diving by 7). The QDS is an efficient, reliable, and valid measure of alcohol use (e.g., Letourneau et al., 2017; Roy et al., 2008). The internal consistency of the QDS at baseline (Cronbach's α = .596) was borderline likely because of the scale being only a four-item questionnaire.
Data analytic plan
We analyzed data and generated plots in R using the nlme (Pinheiro et al., 2020), lme4 (Bates et al., 2011), and sjPlot packages (Lüdecke, 2019). For all models, repeated measures (Level 1, specified as fixed effects) were nested within person (Level 2) and we included a random effect for the participant ID. We estimated models using restricted maximum likelihood and omitted missing data listwise. We decided to test models separately between the IIG and DIG conditions, from baseline to post-intervention (i.e., the first 8 weeks of the study before DIG received access to VetChange). That is, we were initially interested in evaluating whether the changes that occurred among veterans in the IIG condition were moderated by baseline SIP scores. However, realizing that any observed change in PTSD could also be attributable to other factors (e.g., regression to the mean), we subsequently evaluated outcomes among veterans in the DIG condition, before they received the intervention, as an inferential control.
We used a data-driven approach in which mixed-effects regression models were used to predict PCL-5 scores from baseline to post-intervention. We first tested an initial model to determine which SIP subscales at baseline meaningfully related to PCL-5 scores in IIG while accounting for all other SIP subscales. This model included Time (baseline = 1 and post-intervention = 2) as a Level-1 predictor and all baseline SIP subscales as Level-2 predictors. We tested the same model again except with interaction terms between Time and the SIP subscales with statistically significant main effects in the prior model included as Level-2 predictors, to evaluate potential moderation effects. Interaction terms that significantly predicted PCL-5 scores were then graphed to determine the direction of moderating effects in IIG. Subsequently, we conducted the same set of mixed-effects regression models in DIG to rule out regression to the mean. In other words, if a significant Time × SIP subscale interaction is observed in IIG but not in DIG, then we are able to rule out that PTSD severity did not merely change because of the passage of time with no intervention but rather as a function of the SIP subscale. Average daily drinking, gender, race, and age were controlled for in all models as Level-2 covariates. Race was dichotomized to White (n = 476) and non-White (i.e., Hispanic/Latinx, Black/African American, Asian/Pacific Islander, Native American/Alaskan Native, multiracial, other; n = 124) in analyses to retain power to detect group differences.
We also performed post hoc analyses to help clarify intervention usage patterns that might account for observed trends in our primary analyses. We conducted binomial logistic regressions separately for each module to test whether participants high on identified moderators (i.e., SIP subscales at baseline) were more likely to complete specific VetChange modules. The SIP subscale at baseline was the independent variable and module completion (completed module = 1, did not complete module = 2) was the dependent variable in these analyses.
Results
Table 3 presents results from the final mixed-effects regression models predicting PCL-5 scores in IIG and DIG. In IIG, the initial model including Time, all SIP subscales, average daily drinking, gender, race, and age revealed that SIP-Interpersonal was the only subscale significantly associated with PCL-5 scores, b = 1.79, SE = 0.48, t(394) = 3.73, p < .001. Therefore, the Time × SIP-Interpersonal interaction was added to the model and re-analyzed (Table 3). This final model demonstrated that the Time × SIP-Interpersonal interaction significantly predicted PCL-5 scores (p < .001). Also, the main effects of SIP-Interpersonal (p < .001) and race (non-White; p = .003) were significant predictors in this model.
Table 3.
Final mixed-effects regression models predicting PCL-5 scores
| Variable | b | SE | df | t |
|---|---|---|---|---|
| IIG (N = 404) | ||||
| Intercept | 22.85 | 5.29 | 394 | 4.32** |
| SIP-Physical | 0.27 | 0.56 | 394 | 0.48 |
| SIP-Intrapersonal | 0.80 | 0.58 | 394 | 1.36 |
| SIP-Impulse Control | 1.22 | 0.65 | 394 | 1.89 |
| SIP-Social Responsibility | 0.35 | 0.54 | 394 | 0.65 |
| Time | 3.18 | 1.71 | 193 | -1.86 |
| SIP-Interpersonal | 3.79 | 0.72 | 394 | 5.24** |
| Average daily drinkinga | 0.02 | 0.25 | 394 | 0.09 |
| Gender (female) | -2.65 | 2.71 | 394 | -0.98 |
| Race (non-White) | 6.52 | 2.20 | 394 | 2.96* |
| Age | 0.15 | 0.12 | 394 | 1.21 |
| Time × SIP-Interpersonal | -1.58 | 0.43 | 193 | -3.68** |
| Random intercept SD = 14.74 (Residual SD = 10.78) | ||||
| DIG (N = 196) | ||||
| Intercept | 21.11 | 7.61 | 186 | 2.77* |
| SIP-Physical | 0.11 | 0.76 | 186 | 0.14 |
| SIP-Interpersonal | 0.18 | 0.67 | 186 | 0.27 |
| SIP-Social Responsibility | 0.33 | 0.70 | 186 | 0.47 |
| Time | 0.12 | 2.67 | 117 | 0.05 |
| SIP-Intrapersonal | 1.59 | 1.16 | 186 | 1.37 |
| SIP-Impulse Control | 4.83 | 1.27 | 186 | 3.80** |
| Average daily drinkinga | -0.26 | 0.35 | 186 | -0.76 |
| Gender (female) | -1.07 | 3.82 | 186 | -0.28 |
| Race (non-White) | 2.84 | 3.09 | 186 | 0.92 |
| Age | -0.02 | 0.16 | 186 | -0.11 |
| Time × SIP-Intrapersonal | 0.36 | 0.63 | 117 | 0.57 |
| Time × SIP-Impulse Control | -1.38 | 0.77 | 117 | -1.79 |
| Random intercept SD = 14.95 (Residual SD = 8.78) |
Notes: PCL-5 = Posttraumatic Stress Disorder Checklist-5; IIG = initial intervention group; SIP = Short Inventory of Problems; DIG = delayed intervention group.
Calculated using the Quick Drink Screen.
p < .01;
p < .001.
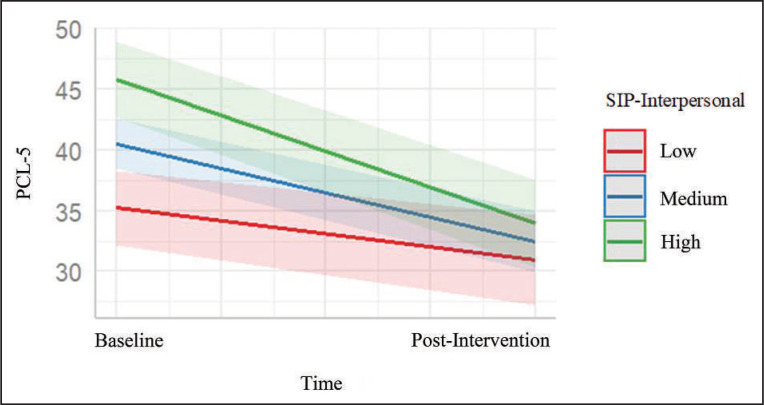
We then plotted the Time × SIP-Interpersonal interaction to inspect moderating effects at low (1 SD below the mean), medium (mean), and high (1 SD above the mean) levels of baseline SIP-Interpersonal (Figure 1). Participants in IIG endorsing high SIP-Interpersonal scores demonstrated significantly greater PTSD symptoms at baseline compared with those reporting low and medium SIP-Interpersonal scores. However, participants with high SIP-Interpersonal scores at baseline exhibited greater reductions on the PCL-5 throughout VetChange relative to those endorsing low and medium SIP-Interpersonal scores. As a result, all participants exhibited similar levels of PTSD symptoms at post-intervention regardless of their baseline SIP-Interpersonal score.
Figure 1.
Moderating effect of SIP-Interpersonal on PCL-5 scores throughout VetChange. Participants endorsing high SIP-Interpersonal scores demonstrated significantly greater posttraumatic stress disorder (PTSD) symptoms at baseline compared with those reporting low and medium SIP-Interpersonal scores. However, participants with high SIP-Interpersonal scores at baseline exhibited greater reductions on the PCL-5 throughout VetChange relative to those endorsing low and medium SIP-Interpersonal scores. As a result, all participants exhibited similar levels of PTSD symptoms at post-intervention regardless of their baseline SIP-Interpersonal score. SIP = Short Inventory of Problems; PCL-5 = Posttraumatic Stress Disorder Checklist-5.
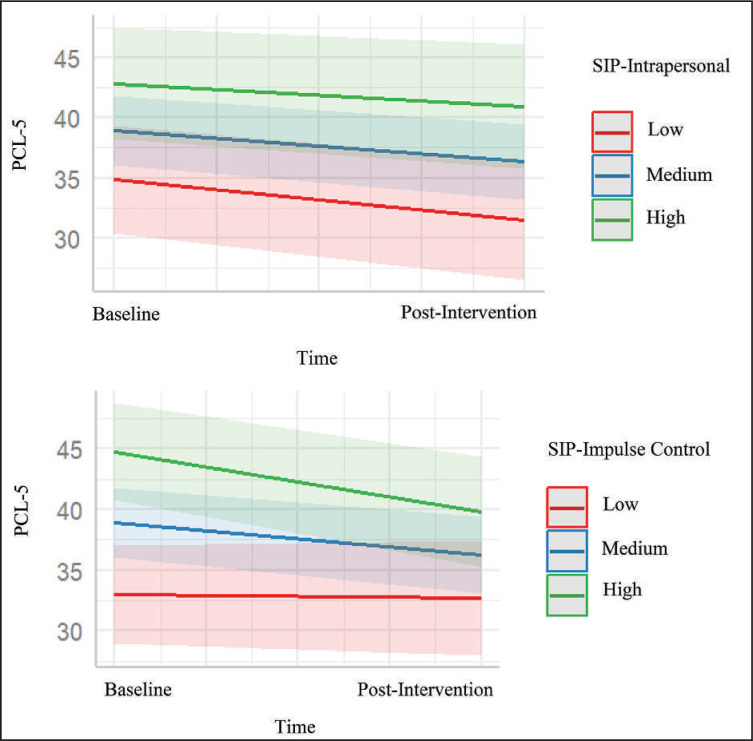
In DIG, the initial mixed-effects regression model including Time, all SIP subscales, average daily drinking, gender, race, and age revealed that SIP-Intrapersonal, b = 2.01, SE = 0.86, t(186) = 2.35, p = .02, and SIP-Impulse Control, b = 3.11, SE = 0.84, t(186) = 3.72, p < .001, were significant predictors of PCL-5 scores. Accordingly, the Time × SIP-Intrapersonal and Time × SIP-Impulse Control interactions were added to the model and re-analyzed (Table 3). Both interactions were not significant predictors of PCL-5 scores. To provide a point of comparison to the moderating effect of SIP-Interpersonal on PCL-5 scores in IIG, we plotted these nonsignificant interactions in the same manner as the significant interaction observed in IIG for SIP-Interpersonal (Figure 2). Only the main effect of SIP-Impulse Control was a significant predictor (p < .001) in the final DIG model. In sum, none of the SIP subscales moderated PCL-5 changes in DIG before they received access to VetChange.
Figure 2.
Nonsignificant interaction effects on PCL-5 scores in DIG. These plots depict the nonsignificant effects of Time × SIP-Intrapersonal and Time × SIP-Impulse Control on PCL-5 scores in the DIG comparison condition before they received access to the VetChange intervention. The plots are provided as a point of comparison to the moderating effect of SIP-Interpersonal on PCL-5 scores observed in IIG while they had access to VetChange. Given that no significant interaction (i.e., moderation) effects were present in DIG, we were able to determine that the moderating effect of SIP-Interpersonal that occurred in IIG was not due to the passage of time (i.e., regression to the mean). PCL-5 = Posttraumatic Stress Disorder Checklist-5; DIG = delayed intervention group; SIP = Short Inventory of Problems; IIG = initial intervention group.
We conducted a series of post hoc binomial logistic regression analyses to supplement findings and refine interpretations. Given that SIP-Interpersonal was the only moderator of PCL-5 scores, these logistic regressions tested if participants high on this subscale at baseline were more likely to complete specific modules within the VetChange intervention (Table 4). Regressions revealed that those with higher baseline SIP-Interpersonal scores were more likely to complete Module 4 (identify high-risk situations for drinking; p = .027) and Module 6 (manage stress, anger, or sleep; p = .031).
Table 4.
Logistic regression analyses with SIP-Interpersonal predicting module completion
| Module | SIP-Interpersonal | ||
|---|---|---|---|
| Est. | SE | z | |
| Module 1: Personalized feedback on alcohol use | 0.04 | 0.07 | 0.63 |
| Module 2: Motivation enhancement | 0.06 | 0.04 | 1.30 |
| Module 3: Make a plan for a drinking goal | 0.04 | 0.04 | 1.04 |
| Module 4: Identify high-risk situations for drinking | 0.09 | 0.04 | 2.22* |
| Module 5: Cope with an internal high-risk situation for drinking | 0.06 | 0.04 | 1.43 |
| Module 6: Manage stress, anger, or sleep | 0.09 | 0.04 | 2.15* |
| Module 7: Manage stress, anger, or sleep | 0.07 | 0.04 | 1.71 |
| Module 8: Develop a social support plan | 0.08 | 0.04 | 1.84 |
Notes: SIP = Short Inventory of Problems; est. = estimate.
p < .05.
Discussion
We found support for interpersonal alcohol-related problems as a moderator of PTSD symptom scores during the use of VetChange, such that veterans endorsing greater interpersonal problems demonstrated larger reductions in PTSD symptoms over time. Importantly, we did not observe the same moderating effect in the DIG comparison condition before they received access to the intervention, implying that the PTSD severity of those who received VetChange was related to the level of interpersonal problems they reported at baseline rather than the passage of time (i.e., regression to the mean). Moreover, the moderating effect of interpersonal problems was observed even when controlling statistically for average daily drinking, gender, race, and age, and preliminary analyses indicated that, for the most part, demographic variables likely did not influence interpersonal problems (i.e., not correlated with age, no gender or race differences).
However, the IIG model did demonstrate that non-White veterans reported significantly higher average PTSD symptoms compared with White veterans. Although Brief et al. (2018) found that veterans with higher levels of PTSD at baseline responded well to VetChange, future research should still consider whether content modifications may be needed to be maximally responsive to veterans of color. It is also worth noting that greater impulse control problems exhibited the only significant main effect regarding PTSD symptoms in the final model for DIG. Because there was no active intervention in DIG, this result indicates that higher alcohol-related impulsivity scores were associated with higher mean PTSD scores over time (e.g., Kearns et al., 2022; Morris et al., 2020).
Co-occurring AUD and PTSD is associated with inter-personal difficulties marked by lower social connectedness and psychosocial resources (Norman et al., 2018; Straus et al., 2019). Considering the functional link between AUD and PTSD (Simons et al., 2018; Straus et al., 2018; van Dam et al., 2012), improving interpersonal alcohol-related problems may have a therapeutic effect on PTSD symptoms. Our results documented that post-9/11 veterans with high levels of alcohol-related interpersonal problems exhibited greater improvements in PTSD symptoms during VetChange relative to those with medium and low levels of interpersonal problems, resulting in comparable PTSD symptom scores across levels of interpersonal problems at post-intervention. Thus, VetChange may be particularly well suited for post-9/11 veterans experiencing high levels of interpersonal problems in the context of comorbid hazardous drinking and PTSD symptoms.
Although we measured interpersonal problems related to drinking at baseline and did not examine change in this variable, it may be that helping veterans identify these problems could increase motivation to seek and engage in treatment. Schreiner and colleagues (2021) found that interpersonal/social benefits (e.g., repairing relationships) was a top reason for changing alcohol use among veterans. Similarly, post- 9/11 veterans reporting above-average alcohol-related inter-personal problems may also recognize interpersonal benefits as an important reason for behavior change and participating in treatment. Thus, modifying VetChange to guide veterans to identify interpersonal reasons for change may increase engagement in the intervention and enhance the potency of its content, which can bolster improvements in hazardous drinking and co-occurring PTSD symptoms.
Brief motivation-based strategies during initial therapy phases, such as motivational interviewing (Miller & Rollnick, 2013), that build awareness of interpersonal problems, explore how they are related to functioning, and elucidate their connections with symptoms may be a vital first step to bolster treatment engagement and response (Conner et al., 2022; Dupree et al., 2016). Given that co-occurring AUD and PTSD negatively affects therapy outcomes (e.g., Roberts et al., 2015; Szafranski et al., 2017), incorporating motivation-enhancement techniques targeting interpersonal problems could be a central component for strengthening adherence to web-based interventions, especially if individuals are completing these treatments on their own without regular guidance or monitoring from a therapist (Harper et al., 2022; Meis et al., 2019).
In addition, post hoc analyses revealed that participants with greater interpersonal problems were more likely to complete Module 4 (identify high-risk situations for drinking) and Module 6 (manage stress, anger, or sleep) in VetChange. Highlighting or augmenting these modules within VetChange may be most germane to veterans reporting greater interpersonal problems. Engagement with these modules may have contributed to reductions in PTSD symptoms during the intervention (e.g., Litz et al., 2004; Miller et al., 2013; Pedersen et al., 2017). These strategies may constitute mechanisms of change through which PTSD symptoms improved in veterans with greater interpersonal problems (e.g., Badour et al., 2012; Magill et al., 2020). Future studies may benefit from testing the ability to identify high-risk drinking situations and coping skills enhancement as mechanisms of web-based interventions for populations experiencing interpersonal difficulties in the context of PTSD and/or AUD. Surprisingly, veterans with greater interpersonal problems were not more likely to engage in the module for social support (Module 8), which could imply that initial coping is needed and seen by veterans as a helpful prerequisite to seeking additional social support. Thus, investigating multiple skills as a sequential process of change in symptoms during online modular treatments is particularly imperative (Brose et al., 2023; Lee et al., 2021).
Our study has several limitations. Although we used well-validated and reliable questionnaires, these measures can be susceptible to bias and context effects, especially with demand characteristics in an RCT design. Next, 35.70% of the sample did not meet the cutoff for probable PTSD and thus findings may not be fully generalizable to individuals diagnosed with PTSD. Furthermore, the sample mostly consisted of White men from post-9/11 conflicts, which may not generalize to veterans who are more diverse in terms of race and/or gender. Future studies may also benefit from having a larger sample in the comparison condition. Finally, the parent trial (Brief et al., 2013) demonstrated high rates of attrition, which may have limited the statistical power of analyses.
In summary, these data indicate that higher levels of alcohol-related interpersonal problems were associated with more pronounced PTSD improvements during VetChange in models accounting for average daily drinking, race, gender, and age, which was not replicated in the comparison condition that did have access to VetChange. Veterans with greater interpersonal problems were also more likely to engage in online intervention content targeting the identification of high-risk drinking situations and management of stress, anger, or sleep. Further research is needed to assess functional associations between interpersonal problems, treatment engagement and motivation, and PTSD symptom change during use of online self-help tools—an important resource to expand intervention reach to veterans with hazardous drinking and PTSD symptoms (Enggasser et al., 2021). Lastly, we did not find evidence to suggest that greater alcohol-related problems were associated with poorer outcomes, which is encouraging for veterans experiencing severe problems related to alcohol use.
Footnotes
Potential conflicts have been disclosed and we do not believe they have material impact on the study's execution, interpretation of findings, and/or publication of results. This work was supported by National Institute on Alcohol Abuse and Alcoholism Grant RC1AA019248, 2009 and by the Office of Academic Affiliations, Department of Veterans Affairs.
References
- Allensworth-Davies D., Cheng D. M., Smith P. C., Samet J. H., Saitz R. The Short Inventory of Problems–Modified for Drug Use (SIP-DU): Validity in a primary care sample. American Journal on Addictions. 2012;21(3):257–262. doi: 10.1111/j.1521-0391.2012.00223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor T. F., de la Fuente J. R., Saunders J., Grant M. AUDIT. The Alcohol Use Disorders Identification Test. Guidelines for use in primary health care. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- Badour C. L., Blonigen D. M., Boden M. T., Feldner M. T., Bonn-Miller M. O. A longitudinal test of the bi-directional relations between avoidance coping and PTSD severity during and after PTSD treatment. Behaviour Research and Therapy. 2012;50(10):610–616. doi: 10.1016/j.brat.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back S. E., Killeen T., Badour C. L., Flanagan J. C., Allan N. P., Ana E. S., Lozano B., Korte K. J., Foa E. B., Brady K. T. Concurrent treatment of substance use disorders and PTSD using prolonged exposure: A randomized clinical trial in military veterans. Addictive Behaviors. 2019;90:369–377. doi: 10.1016/j.addbeh.2018.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates D., Maechler M., Bolker B.Lme4: Linear Mixed-Effects Models Using S4 Classes. R package version 0.999375-38. 2011. http://CRAN.R-project.org/package=lme4
- Bender R. E., Griffin M. L., Gallop R. J., Weiss R. D. Assessing negative consequences in patients with substance use and bipolar disorders: Psychometric properties of the short inventory of problems (SIP) American Journal on Addictions. 2007;16(6):503–509. doi: 10.1080/10550490701641058. [DOI] [PubMed] [Google Scholar]
- Blanco C., Xu Y., Brady K., Pérez-Fuentes G., Okuda M., Wang S. Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: Results from National Epidemiological Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2013;132(3):630–638. doi: 10.1016/j.drugalcdep.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins C. A., Weathers F. W., Davis M. T., Witte T. K., Domino J. L. The posttraumatic stress disorder checklist for DSM 5 (PCL 5): Development and initial psychometric evaluation. Journal of Traumatic Stress. 2015;28(6):489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Bovin M. J., Marx B. P., Weathers F. W., Gallagher M. W., Rodriguez P., Schnurr P. P., Keane T. M. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment. 2016;28(11):1379–1391. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Bradley K. A., Bush K. R., Epler A. J., Dobie D. J., Davis T. M., Sporleder J. L., Maynard C., Burman M. L., Kivlahan D. R. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): Validation in a female Veterans Affairs patient population. Archives of Internal Medicine. 2003;163(7):821–829. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Brief D. J., Rubin A., Enggasser J. L., Roy M., Keane T. M. Web-based intervention for returning veterans with symptoms of posttraumatic stress disorder and risky alcohol use. Journal of Contemporary Psychotherapy. 2011;41(4):237–246. doi: 10.1007/s10879-011-9173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brief D. J., Rubin A., Keane T. M., Enggasser J. L., Roy M., Helmuth E., Hermos J., Lachowicz M., Rybin D., Rosenbloom D. Web intervention for OEF/OIF veterans with problem drinking and PTSD symptoms: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2013;81(5):890–900. doi: 10.1037/a0033697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brief D. J., Solhan M., Rybin D., Enggasser J. L., Rubin A., Roy M., Helmuth E., Schreiner A., Heilman M., Vittorio L., Rosenbloom D., Keane T. M. Web-based alcohol intervention for veterans: PTSD, combat exposure, and alcohol outcomes. Psychological Trauma: Theory, Research, Practice, and Policy. 2018;10(2):154–162. doi: 10.1037/tra0000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brose A., Heinrich M., Bohn J., Kampisiou C., Zagorscak P., Knaevelsrud C. Sequencing effects of behavioral activation and cognitive restructuring in an Internet-based intervention for depressed adults are negligible: Results from a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2023;91(3):122–138. doi: 10.1037/ccp0000789. [DOI] [PubMed] [Google Scholar]
- Burnett-Zeigler I., Ilgen M., Valenstein M., Zivin K., Gorman L., Blow A., Duffy S., Chermack S. Prevalence and correlates of alcohol misuse among returning Afghanistan and Iraq veterans. Addictive Behaviors. 2011;36(8):801–806. doi: 10.1016/j.addbeh.2010.12.032. [DOI] [PubMed] [Google Scholar]
- Conner K. R., Abar B., Aldalur A., Chiang A., Hutchison M., Maisto S. A., Stecker T. Alcohol-related consequences and the intention to seek care in treatment naïve women and men with severe alcohol use disorder. Addictive Behaviors. 2022;131:107337. doi: 10.1016/j.addbeh.2022.107337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D. A., Grant B. F., Li T. K. Quantifying the risks associated with exceeding recommended drinking limits. Alcoholism: Clinical and Experimental Research. 2005;29(5):902–908. doi: 10.1097/01.ALC.0000164544.45746.A7. [DOI] [PubMed] [Google Scholar]
- Dupree C. H., Magill M., Apodaca T. R. The pros and cons of drinking: A qualitative analysis of young adult drinking discussions within motivational interviewing. Addiction Research and Theory. 2016;24(1):40–47. doi: 10.3109/16066359.2015.1060966. [DOI] [Google Scholar]
- Dworkin E. R., Bergman H. E., Walton T. O., Walker D. D., Kaysen D. L. Co-occurring post-traumatic stress disorder and alcohol use disorder in U.S. military and veteran populations. Alcohol Research: Current Reviews. 2018;39(2):161–169. [PMC free article] [PubMed] [Google Scholar]
- Enggasser J. L., Livingston N. A., Ameral V., Brief D. J., Rubin A., Helmuth E., Roy M., Solhan M., Litwack S., Rosenbloom D., Keane T. M. Public implementation of a web-based program for veterans with risky alcohol use and PTSD: A RE-AIM evaluation of VetChange. Journal of Substance Abuse Treatment. 2021;122:108242. doi: 10.1016/j.jsat.2020.108242. [DOI] [PubMed] [Google Scholar]
- Gaher R. M., Simons J. S., Hahn A. M., Hofman N. L., Hansen J., Buchkoski J. An experience sampling study of PTSD and alcohol-related problems. Psychology of Addictive Behaviors. 2014;28(4):1013–1025. doi: 10.1037/a0037257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn A. M., Tirabassi C. K., Simons R. M., Simons J. S. Military sexual trauma, combat exposure, and negative urgency as independent predictors of PTSD and subsequent alcohol problems among OEF/OIF veterans. Psychological Services. 2015;12(4):378–383. doi: 10.1037/ser0000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper K. L., Thompson-Hollands J., Keane T. M., Marx B. P. Mental health treatment utilization and relationship functioning among male and female OEF/OIF veterans. Psychological Services. 2022;19(3):597–603. doi: 10.1037/ser0000548. [DOI] [PubMed] [Google Scholar]
- Hirchak K. A., Tonigan J. S., Hernandez-Vallant A., Herron J., Cloud V., Venner K. L. The validity of the Short Inventory of Problems and drinking intensity among urban American Indian adults. Substance Use & Misuse. 2021;56(4):501–509. doi: 10.1080/10826084.2021.1883656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge C. W., Castro C. A., Messer S. C., McGurk D., Cotting D. I., Koffman R. L. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Kearns N. T., Gunn R. L., Stevens A. K., Berey B. L., Metrik J. Longitudinal associations between impulsivity and alcohol and cannabis use frequency, quantity, and problems among military veterans. Psychology of Addictive Behaviors. 2022;36(7):762–774. doi: 10.1037/adb0000825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiluk B. D., Dreifuss J. A., Weiss R. D., Morgenstern J., Carroll K. M. The Short Inventory of Problems–revised (SIP-R): Psychometric properties within a large, diverse sample of substance use disorder treatment seekers. Psychology of Addictive Behaviors. 2013;27(1):307–314. doi: 10.1037/a0028445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer H. C., Frank E., Kupfer D. J. Moderators of treatment outcomes: Clinical, research, and policy importance. JAMA. 2006;296(10):1286–1289. doi: 10.1001/jama.296.10.1286. [DOI] [PubMed] [Google Scholar]
- Lee D. J., Marx B. P., Thompson-Hollands J., Gallagher M. W., Resick P. A., Sloan D. M. The temporal sequence of change in PTSD symptoms and hypothesized mediators in Cognitive Processing Therapy and Written Exposure Therapy for PTSD. Behaviour Research and Therapy. 2021;144:103918. doi: 10.1016/j.brat.2021.103918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letourneau B., Sobell L. C., Sobell M. B., Agrawal S., Gioia C. J. Two brief measures of alcohol use produce different results: AUDIT C and quick drinking screen. Alcoholism: Clinical and Experimental Research. 2017;41(5):1035–1043. doi: 10.1111/acer.13364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litz B. T., Williams L., Wang J., Bryant R., Engel C. C., Jr. A therapist-assisted internet self-help program for traumatic stress. Professional Psychology, Research and Practice. 2004;35(6):628–634. doi: 10.1037/0735-7028.35.6.628. [DOI] [Google Scholar]
- Lüdecke D.sjPlot: Data visualization for statistics in social science. R package version 2.7.0. 2019. https://cran.r-project.org/package=sjPlot
- Magill M., Tonigan J. S., Kiluk B., Ray L., Walthers J., Carroll K. The search for mechanisms of cognitive behavioral therapy for alcohol or other drug use disorders: A systematic review. Behaviour Research and Therapy. 2020;131:103648. doi: 10.1016/j.brat.2020.103648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney C. T., Livingston N. A., Wong M. M., Rosen R. C., Marx B. P., Keane T. M. Parallel process modeling of posttraumatic stress disorder symptoms and alcohol use severity in returning veterans. Psychology of Addictive Behaviors. 2020;34(5):569–578. doi: 10.1037/adb0000569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marra L. B., Field C. A., Caetano R., von Sternberg K. Construct validity of the Short Inventory of Problems among Spanish speaking Hispanics. Addictive Behaviors. 2014;39(1):205–210. doi: 10.1016/j.addbeh.2013.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean C. P., Schlenger W. E., Litz B. T. Internet use in the aftermath of trauma. IOS Press; 2010. Using the internet to deliver treatments for PTSD; pp. 231–242. [Google Scholar]
- Meis L. A., Noorbaloochi S., Hagel Campbell E. M., Erbes C. R., Polusny M. A., Velasquez T. L., Bangerter A., Cutting A., Eftekhari A., Rosen C. S., Tuerk P. W., Burmeister L. B., Spoont M. R. Sticking it out in trauma-focused treatment for PTSD: It takes a village. Journal of Consulting and Clinical Psychology. 2019;87(3):246–256. doi: 10.1037/ccp0000386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M. B., Leffingwell T., Claborn K., Meier E., Walters S., Neighbors C. Personalized feedback interventions for college alcohol misuse: An update of Walters & Neighbors (2005) Psychology of Addictive Behaviors. 2013;27(4):909–920. doi: 10.1037/a0031174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W. R., Rollnick S. Motivational interviewing: Helping people change. 3rd ed. Guilford Press; 2013. [Google Scholar]
- Miller W. R., Tonigan J. S., Longabaugh R. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse. Washington, DC: U.S. Government Printing Office; 1995. [Google Scholar]
- Morris V. L., Huffman L. G., Naish K. R., Holshausen K., Oshri A., McKinnon M., Amlung M. Impulsivity as a mediating factor in the association between posttraumatic stress disorder symptoms and substance use. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(6):659–668. doi: 10.1037/tra0000588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman S. B., Haller M., Hamblen J. L., Southwick S. M., Pietrzak R. H. The burden of co-occurring alcohol use disorder and PTSD in U.S. military veterans: Comorbidities, functioning, and suicidality. Psychology of Addictive Behaviors. 2018;32(2):224–229. doi: 10.1037/adb0000348. [DOI] [PubMed] [Google Scholar]
- Pedersen E. R., Parast L., Marshall G. N., Schell T. L., Neighbors C. A randomized controlled trial of a web-based, personalized normative feedback alcohol intervention for young-adult veterans. Journal of Consulting and Clinical Psychology. 2017;85(5):459–470. doi: 10.1037/ccp0000187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro J., Bates D., DebRoy S., Sarkar D., R Core Team Nlme: Linear and Nonlinear Mixed Effects Models. R package version 3.1-145. 2020. https://CRAN.R-project.org/package=nlme
- Roberts N. P., Roberts P. A., Jones N., Bisson J. I. Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical Psychology Review. 2015;38:25–38. doi: 10.1016/j.cpr.2015.02.007. [DOI] [PubMed] [Google Scholar]
- Roberts N. P., Roberts P. A., Jones N., Bisson J. I. Cochrane Database of Systematic Reviews; 2016. Psychological therapies for post-traumatic stress disorder and comorbid substance use disorder. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy M., Dum M., Sobell L. C., Sobell M. B., Simco E. R., Manor H., Palmerio R. Comparison of the quick drinking screen and the alcohol timeline followback with outpatient alcohol abusers. Substance Use & Misuse. 2008;43(14):2116–2123. doi: 10.1080/10826080802347586. [DOI] [PubMed] [Google Scholar]
- Schreiner A. M., Livingston N. A., Heilman M., Lynch T., Vittorio L., Brief D. J., Rubin A., Enggasser J. L., Roy M., Solhan M., Helmuth E., Rosenbloom D., Keane T. M. Understanding motives for and against hazardous drinking and change among returning veterans. Psychological Services. 2021;18(4):523–532. doi: 10.1037/ser0000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons J. S., Simons R. M., Keith J. A., Grimm K. J., Stoltenberg S. F., O’Brien C., Andal K. PTSD symptoms and alcohol-related problems among veterans: Temporal associations and vulnerability. Journal of Abnormal Psychology. 2018;127(8):733–750. doi: 10.1037/abn0000376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson T. L., Goldberg S. B., Louden D. K. N., Blakey S. M., Hawn S. E., Lott A., Browne K. C., Lehavot K., Jaysen D. Efficacy and acceptability of interventions for co-occurring PTSD and SUD: A meta-analysis. Journal of Anxiety Disorders. 2021;84:102490. doi: 10.1016/j.janxdis.2021.102490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson T. L., Stappenbeck C. A., Luterek J. A., Lehavot K., Kaysen D. L. Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology. 2014;123(1):237–247. doi: 10.1037/a0035193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell L. C., Agrawal S., Sobell M. B., Leo G. I., Young L. J., Cunningham J. A., Simco E. R. Comparison of a quick drinking screen with the timeline followback for individuals with alcohol problems. Journal of Studies on Alcohol. 2003;64(6):858–861. doi: 10.15288/jsa.2003.64.858. [DOI] [PubMed] [Google Scholar]
- Straus E., Haller M., Lyons R. C., Norman S. B. Functional and psychiatric correlates of comorbid post-traumatic stress disorder and alcohol use disorder. Alcohol Research: Current Reviews. 2018;39(2):121–129. [PMC free article] [PubMed] [Google Scholar]
- Straus E., Norman S. B., Haller M., Southwick S. M., Hamblen J. L., Pietrzak R. H. Differences in protective factors among U.S. Veterans with posttraumatic stress disorder, alcohol use disorder, and their comorbidity: Results from the National Health and Resilience in Veterans Study. Drug and Alcohol Dependence. 2019;194:6–12. doi: 10.1016/j.drugalcdep.2018.09.011. [DOI] [PubMed] [Google Scholar]
- Szafranski D. D., Snead A., Allan N. P., Gros D. F., Killeen T., Flanagan J., Pericot-Valverde I., Back S. E. Integrated, exposure-based treatment for PTSD and comorbid substance use disorders: Predictors of treatment dropout. Addictive Behaviors. 2017;73:30–35. doi: 10.1016/j.addbeh.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, & the U.S. Department of Agriculture. Dietary guidelines for Americans. 7th ed. Washington, DC: U.S. Government Printing Office; 2010. pp. 30–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dam D., Vedel E., Ehring T., Emmelkamp P. M. Psychological treatments for concurrent posttraumatic stress disorder and substance use disorder: A systematic review. Clinical Psychology Review. 2012;32(3):202–214. doi: 10.1016/j.cpr.2012.01.004. [DOI] [PubMed] [Google Scholar]
- Weathers F. W., Litz B. T., Keane T. M., Palmieri P. A., Marx B. P., Schnurr P. P. The PTSD Checklist for DSM-5 (PCL-5) Scale available from the National Center for PTSD; 2013. www.ptsd.va.gov [Google Scholar]
- Wortmann J. H., Jordan A. H., Weathers F. W., Resick P. A., Dondanville K. A., Hall-Clark B., Foa E. B., Young-McCaughan S., Yarvis J. S., Hembree E. A., Mintz J., Peterson A. L., Litz B. T. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment. 2016;28(11):1392–1403. doi: 10.1037/pas0000260. [DOI] [PubMed] [Google Scholar]