Summary:
Although research and innovation is a key within the field of plastic and reconstructive surgery, the impact of team structure, interpersonal dynamics, and/or standardized infrastructure on scholarly output has been infrequently studied. In this work, we present the formation and implementation of a novel plastic surgery research program that aims to unite previously disparate clinical and translational research efforts at our institution to facilitate critical inquiry. From July 2022 to June 2023, our department launched a pilot research program based on three pillars: (1) formalization of a research curriculum (monthly research meetings for agenda setting and discussion for project honing, formal research leadership for meeting facilitation and workflow regulation), (2) development of a centralized database to compile ongoing research (Google Drive repository to house all ongoing research documents, facilitate real-time editing, and provide resources/templates for assisting in the research process), and (3) bolstering of a core research identity built on mentorship and collaboration (more frequent interactions to shift previously siloed faculty-student mentorship into a robust milieu of intercollaboration). During the first year, we saw an increased number of publications and presentations, as well as robust participation and contribution from faculty, residents, and medical students. Future directions will focus on addressing resource limitation, such as project idea availability and funding, to sustain the success and growth of this novel research infrastructure.
Takeaways
Question: What is the effect of implementing a centralized research program on collaboration, research identity, and scholarly output on a plastic surgery department at an academic institution?
Findings: During the first year of implementation of a centralized research program, our department saw an increased number of publications and presentations, as well as robust participation and contribution from faculty, residents, and medical students.
Meaning: Centralization of research efforts within an academic plastic surgery department can increase scholarly output and solidify a cohesive research identity by optimizing its existing infrastructure.
INTRODUCTION
Central to the identity of plastic and reconstructive surgery (PRS) is an emphasis on research and innovation, whereby critical inquiry confers opportunity for advancement in patient care and operative technique. The previous decade saw a 72% increase in plastic surgery publications in 2021 compared with 2015, in part due to increases in time and availability during the COVID-19 pandemic.1 As such, research productivity has become a key factor in the evaluation of curriculum vitae quality. At the medical student level, applicants to integrated PRS programs frequently demonstrate the highest average numbers of publications, conference abstracts, and research experiences among graduating medical students, often pursuing dedicated research years.2 This is of particular importance, as previously used metrics, such as STEP 1 scores, are no longer used to differentiate among applicants. Moreover, PRS programs are ranked with research productivity as a central parameter.3 For residents, program reputation and affiliated medical school research rankings are associated with greater research output during integrated PRS training, demonstrating the need for institutional support in facilitating critical inquiry.4
Despite the focus on research productivity within PRS, the impact of team structure, interpersonal dynamics, and/or standardized infrastructure on scholarly output is infrequently studied. The implementation of a three-tiered hierarchy system, in which several levels of research coordinators managed research workflow within the division of plastic and reconstructive surgery at Mount Sinai, found greater efficiency and improvement in scholarly output.5 Moreover, in an attempt to provide early PRS and research exposure to medical students, the Hansjorg-Wyss department of plastic surgery at New York University developed a formalized plastic surgery research program for first-year medical students in 2013 that, over time, demonstrated productive involvement in plastic surgery research and majority admittance into integrated PRS programs for participating students.6 These few, yet significant, examples showcase the benefit of implementing structured research programs at multiple levels of participating medical personnel.
The value of implementing formalized research frameworks is further evidenced by the need to overcome rate limiting constraints on scholarly output. From 2012 to 2016, a decline in annual National Institutes of Health funding was associated with fewer PRS publications originating from academic institutions.7 Therefore, siloed approaches to research may further divide available resources, whereby centralization and cross-collaboration afford unique opportunities to perform investigation with high level of evidence. We present the formation and implementation of a novel PRS research program within the division of plastic and reconstructive surgery at The Warren Alpert Medical School of Brown University. This program aimed to unite previously disparate clinical and translational research efforts at our institution through the development of a cohesive infrastructure to facilitate critical inquiry at the medical student, research fellow, resident physician, and attending level.
FORMATION OF A CENTRALIZED RESEARCH PROGRAM
Overall Organizational Structure
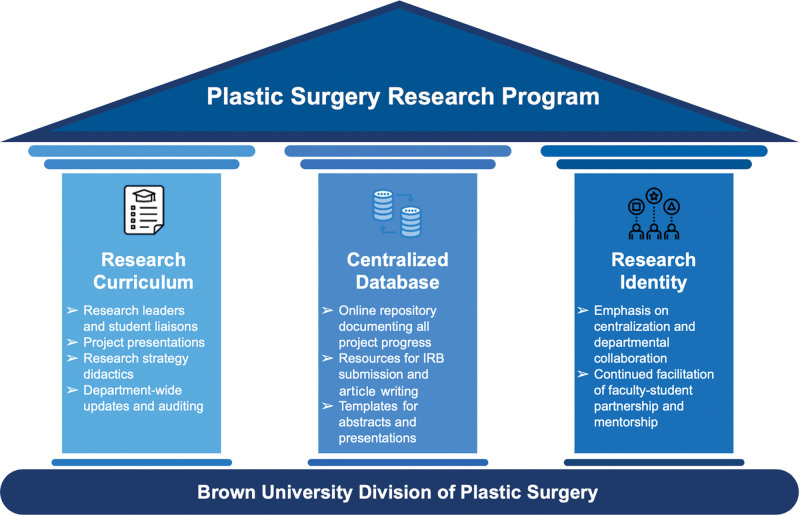
The Brown University plastic surgery research program (BU-PSRP) is founded on three central pillars: (1) formalization of a research curriculum within the integrated plastic surgery residency program, (2) development of a centralized document or database to compile ongoing research efforts, and (3) formation of a core research identity, with reliable mentorship from faculty and senior residents (Fig. 1).
Fig. 1.
BU-PSRP was founded on three pillars: a research curriculum that manages project progress through meetings, didactics, audits; a centralized database of all projects; and a core research identity centered around collaboration and fruitful mentorship.
Research Curriculum
Research Meetings
The utility of routinely scheduled research meetings is well known, serving as a conduit for intradepartmental discussions on scholarly investigation and consistent agenda setting. We endeavor to host monthly research meetings outside clinical hours (every second Wednesday at 5:00 pm) to present and discuss ongoing projects or new study ideas, interpret and dissect findings, and assign team-member roles. Research meetings are planned to last for 1 hour, with auditing of ongoing studies among attendees followed by structured discussion (5-minute presentations followed by peer feedback and goal setting) centered on one to two active projects. To avoid exceeding the allotted time interval, pending discussion is tabled for the subsequent meeting, with minutes actively recorded to ensure continuity. For weeks where ongoing research projects are not presented, discussion is centered on research strategies, including grant writing, study construct, or innovation. The meeting schedule is determined in advance and sent to interested parties at the beginning of the academic year. The agenda for the next meeting is discussed among leadership at the conclusion of each research meeting, with reminders sent periodically before the next meeting.
Department-wide research meetings are held quarterly during conference hours, with brief updates regarding the state of research at Brown University Plastic Surgery, followed by formalized presentations for completed projects with accompanying critique. These meetings are timed in accordance with local and national meetings to showcase ongoing research efforts.
Research Leadership
Reliable leadership is paramount to ensuring success of a research infrastructure. As such, we developed a novel resident role, entitled research chair, to serve as a point-person to guide monthly research meetings and oversee the program. Ancillary responsibilities include coordinating dates for department-wide research meetings with administrative chief residents, securing and distributing funding for meeting-related expenses, and communicating publication/presentation milestones to the department.
Incumbent in their responsibilities, annual research fellows assist the research chair in the timely auditing of active research projects and management of the centralized repository. Minutes are taken during each monthly meeting and published within the compendium. In addition, research fellows maintain communication with the leadership of The Warren Alpert Medical School Plastic Surgery Interest Group to actively recruit interested medical students.
Auditing Mechanism
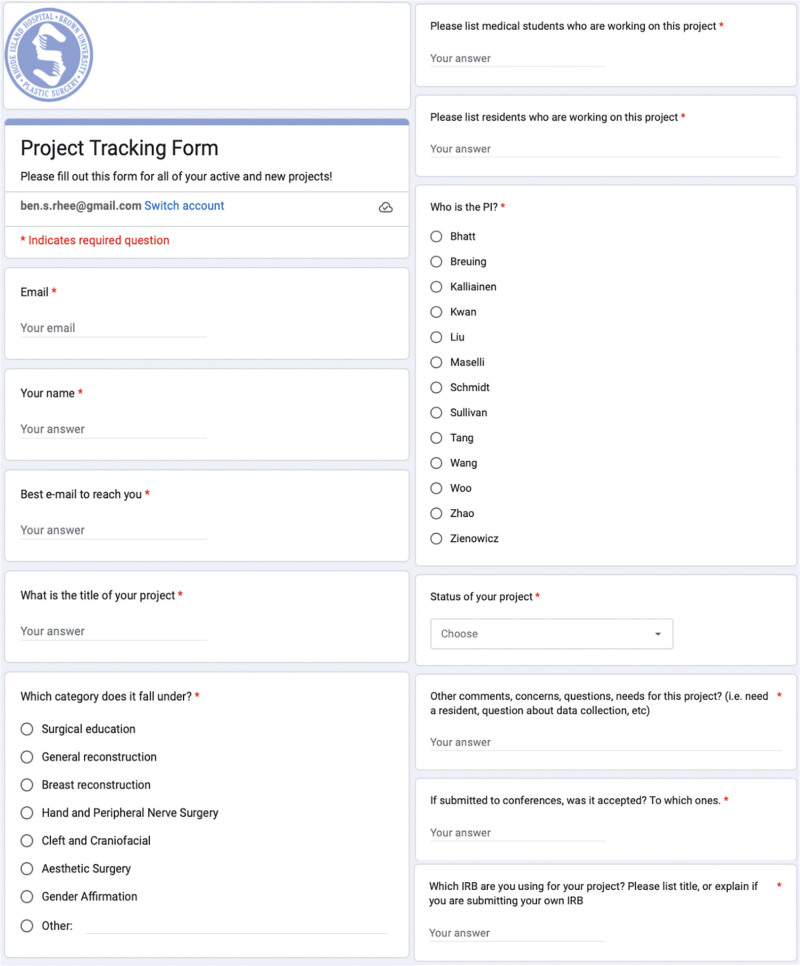
Interested parties are included in a Google Team list-serv. Schedule updates, meeting agendas, and publication milestones are routinely sent to members. Once added to the list-serv, interested parties receive read-only access to the research compendium. A project tracking form (Fig. 2) is sent to capture newly initiated studies. The results of the survey are automatically populated into the active projects spreadsheet on the compendium. It is the responsibility of the research fellows, as overseen by the research chair, to regularly audit and populate this spreadsheet.
Fig. 2.
The project tracking form is filled out for all newly initiated studies or active projects with newly added team members. It allows for real-time updates and automatic population of project entries in the compendium’s “active projects” spreadsheet.
Centralized Database
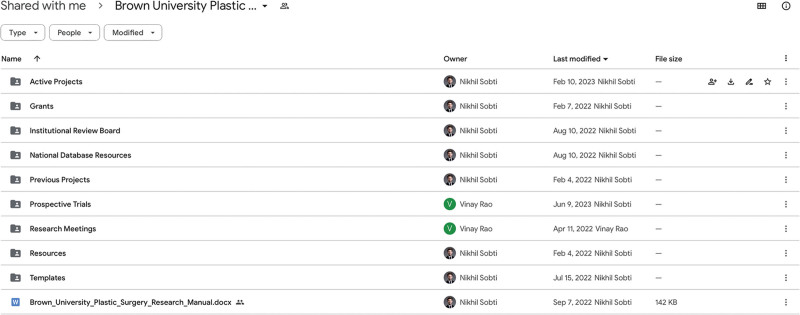
The research compendium (Fig. 3) was constructed to centralize documents pertaining to active and previous projects performed within the PRS department. Our vision was to develop a division-wide Google Drive repository for members to actively edit documents in real time to better facilitate progression of projects, while indexing previous drafts to record the history of research efforts. The compendium is divided into the following subfolders: (1) active projects, (2) grants, (3) institutional review board (IRB), (4) previous projects, (5) research meetings, (6) resources, and (7) templates. To note, those interested in participating in clinical research are given access to the compendium in a read-only capacity. If directly involved in a new/active project, a folder is made in the active projects subfolder, and participating team members are given edit privileges. Documents such as databases, article drafts, abstract drafts, and journal submissions are uploaded to project folders. Of note, protected health information is not stored on the research compendium, instead on secured REDCAP databases.
Fig. 3.
The research compendium is a Google Drive repository that compiles all projects within the department into one online location, seeking to better facilitate progression and completion of projects while documenting the history of research efforts and project drafts. It is divided into subfolders, as shown in the main page of the drive.
Active projects: These are divided into sections through folders based on subspecialty, including aesthetic surgery, breast reconstruction, cleft and craniofacial surgery, general reconstruction, hand and peripheral nerve surgery, and surgical education. In addition, this subfolder contains the active projects spreadsheet detailing ongoing studies, their stage of completion, and team members.
Grants: These include active and previously submitted grants, categorized by funding source. By using previously submitted grant submissions as a reference, we hope to provide a sufficient framework for future proposals.
IRB: This database involves active and previously submitted IRB documents. These files are often used as templates for future IRB submissions to expedite proposal construction. In addition, the availability of IRB documents serves to clarify those topics that are already approved for investigation, thereby limiting duplication of efforts when submitting new proposals.
Previous projects: These involve a compilation of projects successfully completed and published by the Brown University plastic surgery group, stratified by date. The previous projects spreadsheet has to be updated periodically, as studies become published online.
Research meetings: These include documents pertaining to research meetings, including minutes, presentations, and schedules.
Resources: These contain materials pertaining to study design, statistical analysis, software suites, grant writing, and presentation development.
Templates: Templates and examples of presentations, articles, abstracts, posters, and cover letters to obviate confusion regarding formatting and, more importantly, ensure consistency among submissions from Brown University plastic surgery.
Core Research Identity and Sustained Mentorship
Before the launch of the BU-PSRP, there was already a robust culture of mentorship between faculty/residents and medical students; however, these instances were often siloed and left little opportunity for cross-collaboration among faculty–student partnerships. The centralization of research efforts contributes to an environment in which multidimensional mentorship/collaboration can be achieved. By actively participating in scheduled research meetings, faculty members have more direct and sustained interaction with resident physicians and medical students. The centralized database allows members of the research program to more comprehensively grasp the department’s research landscape and connect with faculty/senior residents on projects that resonate with their particular interests. More frequent interactions and pairings between residents and medical students facilitates a cohesive learning environment, where faculty and senior residents would advise more junior trainees on clinical research execution. In sum, collaboration remains incumbent, and milestone successes are shared across and sustained by all members.
RESULTS AND LESSONS LEARNED
Results of the Inaugural Year
The BU-PSRP experienced its pilot launch and first full iteration between July 1, 2022 and July 1, 2023. During this period, 12 research meetings (of 12 anticipated, 100% compliance) were held, with an average overall attendance of 15–23 per meeting (two to five attendings, three to six residents, 10–12 medical students). An estimated 74 total members were registered within the list-serv, and 87 active projects were documented throughout the year. Table 1 summarizes the distribution of the projects when stratified by subspecialty and production stage. The top three subspecialties represented by the projects were cleft and craniofacial surgery (23), hand and peripheral nerve surgery (15), and surgical education (13). In terms of production stage, at the conclusion of the first iteration of BU-PSRP, five projects were in the conception/IRB submission stage, six were in the data collection stage, 30 in writing, and 22 under review for publication. Twenty-four resulted in article publication, representing a 27.6% conversion rate from conception to article publication in 1 year. With regard to the publications, the average number of medical students per publication was 1.6; residents, 2.1; and attendings, 1.0, increased from the previous year with the exception of attendings (medical students 1.1, residents 1.3, and attendings 2.0, respectively). In addition, the first iteration of the BU-PSRP saw increases in the number of poster and oral presentations given at local and national conferences (12 posters versus 11 posters in previous year; 20 oral presentations versus 14 oral presentations).
Table 1.
Distribution of Projects during the First Year of BU-PSRP by Subspecialty and Production Stage
| Subspecialty | Frequency (%), n = 87 |
Production Stage | Frequency (%), n = 87 |
|---|---|---|---|
| Aesthetics | 2 (2.3) | Conception | 2 (2.3) |
| Body contouring | 6 (6.9) | IRB submission | 2 (2.3) |
| Breast | 6 (6.9) | Data collection | 6 (6.9) |
| Cleft and craniofacial surgery | 23 (26.4) | Writing | 30 (34.5) |
| Gender affirmation | 1 (1.1) | Under review for publication | 22 (25.3) |
| General reconstruction | 7 (8.0) | Accepted/published |
25 (28.7) |
| Hand and peripheral nerve surgery | 15 (17.2) | ||
| Neuroplastic surgery | 11 (12.6) | ||
| Surgical education | 13 (14.9) | ||
| Surgical innovation: three-dimensional printing | 3 (3.4) |
Key Takeaways
The impact of our centralized infrastructure on research productivity may take several years to adequately ascertain. However, salient increases in output were appreciated during the first year of implementation, namely a 9.1%, 9.1%, and 42.9% increase in the volume of publications, poster presentations, and oral presentations, respectively. The rapid rise in the number of abstracts accepted may be attributed to improved throughput, where idea generation, study design, data collection, and statistical analyses are performed more efficiently. The apparent lag in rate of change for publications is likely a result of prolonged peer review and revision times. It has been reported that the median turnaround time for plastic surgery articles from submission to acceptance is 4.6 months (IQR 3–6.8 months).8 As such, the benefit of the BU-PSRP on publication output is more likely to be reflected in future iterations. In addition, the relative increase in the number of oral presentations versus poster presentations suggests an improvement in the quality of research being performed and critical refinement, made possible by regular auditing and discussion at research forums.
In terms of authorship, the average number of medical students per article publication increased from 1.1 to 1.6 during the BU-PSRP pilot year. This statistic highlights the central goal of involving junior trainees in the research landscape and increasing collaboration across the previous silos of relatively one-to-one partnerships with faculty and residents. Compared with the year prior, the level of interest in plastic surgery among students at The Warren Alpert Medical School of Brown University has remained constant, as evidenced by stable levels of membership within the Plastic Surgery Interest Group. Thus, the rise in average number of student authors per publication highlights our increasing ability to include more student trainees into meaningful opportunities within the novel infrastructure. Of note, the average number of student authors for articles under review for publication is 2.0. This reflects the rise in student involvement even within the first year of BU-PSRP because manuscripts under review would in general come from projects that started after those for which a publication had already resulted within the first iteration of the program.
The implementation and management of the BU-PSRP was greatly aided by the efforts of the annual student research fellows. As stated previously, dedicated researchers assist with agenda setting, detailing project development, and allocating roles to medical students across various project arms. As senior medical students, they served as a crucial bridge between junior trainees and senior members of the department. They were also instrumental in delegating medical students (and often residents) to available projects that most closely aligned with interest and comfort level.
Importantly, the formation of a structured research program allowed for a transition in focus from primarily case reports and retrospective series to prospective clinical trials. By the end of the pilot year, eight clinical trials had been initiated (increased from one the year prior), all in various stages ranging from study design to patient enrollment. This trend may be attributed to the discussion and troubleshooting opportunities afforded by the monthly meetings. The combination of invested faculty members and residents allowed for a productive forum to hone grant responses and collectively anticipate roadblocks pertaining to trial approval and implementation. In addition, formation of a core research identity facilitated interdepartmental collaboration, namely a multidisciplinary neuroplastic surgery team, where attendings and residents from the neurosurgery department participated in several of the monthly research meetings to map out a comprehensive study design and eventual grant submission for large-scale trials.
Despite the success of the inaugural year of the BU-PSRP, there exist salient limitations that inform future iterations. For instance, by the midpoint of the pilot year, availability of vetted research project ideas became a key limiting factor. The majority of novel ideas had already been formulated at the beginning of the cycle, and subsequent monthly meetings focused primarily on discussing and troubleshooting those projects. Thus, little time was available to construct new study ideas during the year. This limitation primarily impacts medical students; as mentioned earlier, integrated plastic surgery applicants carry the highest average numbers of research items among their medical school cohort. In addition to quality, a robust quantity of research projects with available opportunities is crucial for the development of student research experience and competitiveness for plastic surgery residency positions. To address this limitation, we propose a quarterly idea summit among senior residents and faculty. These meetings would focus on project idea generation, with each participant formulating a number of project ideas to be introduced at general meetings during the year.
Resource limitation, namely personnel and funding, represented another barrier during the pilot year. With rapid increases in the number of active projects, we noticed appreciable strain on attending and resident bandwidth, where competing clinical responsibilities slowed turnaround time in the research process. As such, there is a salient need for additional research staff. Moreover, the amount of departmental research funding remained constant throughout the year. In addition to supply cost, the transition toward open access publication, where article processing fees are charged to submitting authors, there exists a need for robust research funding. Applying for external funding can provide a viable solution for such resource limitation. In fact, a study on academic productivity of academic plastic surgeons found positive correlations between Plastic Surgery Foundation, American Association of Plastic Surgeons, and National Institute of Health grants and scholastic output of plastic surgeons receiving these types of funding.9 Furthermore, an increasing number of plastic surgeons have been receiving federal funding over the last several years, with many having previously been awarded Plastic Surgery Foundation grants. Therefore, investments into research infrastructure further improve productivity and may beget further industry or federal funding.
Future Directions
In addition to the aforementioned limitations, the reach and effectiveness of the BU-PSRP can be further augmented in the coming years. Research fellows remain instrumental in the continued success of our centralized approach. To appropriately compensate for their efforts, formalization of a research fellowship with annual stipends should be considered in future iterations. In fact, Carney et al demonstrated that clinical research output increased significantly after the incorporation of a formalized research fellowship between 2000 and 2015 at their institution.10 As such, departmental budgeting should be considered to facilitate funding of this position. Moreover, the implementation of a research day should be explored, where alumni of the program are invited to share research from their respective departments and reconnect with their home training program. This collaboration allows for a greater variety of research ideas by more researchers with diverse scholarly experiences, and also opens up the opportunity to facilitate partnerships among more plastic surgery departments.
CONCLUSIONS
The Brown University Plastic Surgery Research Program was launched in July 2022 within the division of plastic and reconstructive surgery at The Warren Alpert Medical School of Brown University to increase scholarly output; facilitate greater collaboration between faculty and junior trainees; and encourage a cohesive, centralized research identity within the department. During the first year, we saw an increased number of publications and presentations, as well as robust participation and contribution from faculty, residents, and medical students. Future directions will focus on addressing resource limitation, such as project idea availability and funding, in addition to incorporating new initiatives (ie, formalized research fellow stipends) to sustain the success and growth of this novel research infrastructure.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online 6 February 2024.
Disclosure statements are at the end of this article, following the correspondence information.
Drs. Sobti and Rhee contributed equally to this work.
REFERENCES
- 1.Karamitros G, Goulas S. Human capital and productivity in plastic surgery research across nations. Aesthetic Plast Surg. 2023;47:1644–1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schultz KP, Shih L, Davis MJ, et al. Integrated plastic surgery applicant review: important factors and selection criteria. Plast Reconstr Surg Glob Open. 2020;8:e2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seu MY, Esmaeeli S, Wiegmann AL, et al. Nationwide bibliometric analysis of integrated plastic surgery program directors. Plast Reconstr Surg Glob Open. 2023;11:e4711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siniakowicz C, Cadwell JB, Maisner RS, et al. Research productivity of integrated plastic surgery residents: does reputation matter? J Surg Res. 2022;276:298–304. [DOI] [PubMed] [Google Scholar]
- 5.Ibelli TJ, Akhavan AA, Margulies I, et al. Creation of a novel plastic surgery research program framework: a single division’s experience. Paper presented at: Annual Meeting of the American Council of Academic Plastic Surgeons; February 26, 2023; New Orleans, La. [Google Scholar]
- 6.Alfonso AR, Berman ZP, Diep GK, et al. Evolution of a plastic surgery summer research program: lessons learned from programmatic evaluation and quality enhancement. Plast Reconstr Surg Glob Open. 2023;11:e4785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chi D, Curiel D, Bucknor A, et al. Institutional collaboration in plastic surgery research: a solution to resource limitations. Plast Reconstr Surg Glob Open. 2018;6:e1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asaad M, Rajesh A, Banuelos J, et al. Time from submission to publication in plastic surgery journals: The story of accepted manuscripts. J Plast Reconstr Aesthet Surg. 2020;73:383–390. [DOI] [PubMed] [Google Scholar]
- 9.Ruan QZ, Cohen JB, Baek Y, et al. Identifying sources of funding that contribute to scholastic productivity in academic plastic surgeons. Ann Plast Surg. 2018;80:S214–S218. [DOI] [PubMed] [Google Scholar]
- 10.Carney MJ, Weissler JM, Koltz PF, et al. Academic productivity, knowledge, and education in plastic surgery: the benefit of the clinical research fellow. Plast Reconstr Surg. 2017;140:842–849. [DOI] [PubMed] [Google Scholar]