Abstract
Purpose of Review
Irreparable subscapularis tears, especially in younger patients with higher functional demands, present a challenging entity. Pectoralis major and latissimus dorsi tendon transfers are commonly considered for surgical management of this pathology, yet no consensus exists regarding the superior option. The purpose of this article is to review the most current tendon transfer techniques for irreparable subscapularis tears.
Recent Findings
For decades, transfer of the pectoralis major has been considered the gold standard technique for irreparable subscapularis tears. This transfer was found to reduce pain and improve functional outcome scores, yet range of motion and force of internal rotation were not maintained in long-term follow-up studies. The latissimus dorsi tendon transfer for the same indications has demonstrated biomechanical superiority in recent cadaveric studies with promising short-term results clinically.
Summary
Both pectoralis major and latissimus dorsi tendon transfers improve outcomes of patients with irreparable subscapularis tears. Future comparative studies are still needed to determine superiority amongst techniques.
Keywords: Irreparable subscapularis tendon tears, Latissimus dorsi transfer, Pectoralis major transfer, Tendon transfer
Introduction
The glenohumeral joint is a complex anatomic structure, stabilized by a large network of ligaments, tendons, and other connective tissue elements, conferring the greatest mobility of any major joint in the human body [1]. The inherent bony stability of the shoulder is poor with a significant mismatch in size existing between the humeral head and glenoid. Adequate force coupling of rotator cuff musculature actively compresses the humeral head into the cavity of the glenoid and provides dynamic stabilization while ranging about the glenohumeral center of rotation [2]. However, whether caused by acute trauma or chronic degeneration, rotator cuff pathology that disrupts this force coupling creates debilitating deficits in joint kinematics, leading to pain, weakness, loss of motion, degenerative changes, and potentially requiring surgical intervention [3, 4].
Rotator cuff tear (RTC) is the primary reason for shoulder surgery in middle-aged and older adults, varying in tear size and muscle atrophy, with up to 30% of all RCTs being classified as irreparable [5, 6]. Depending on the extent of the RCT, various joint-preserving procedures allow repair or reconstruction of these irreparable tears, given the articular cartilage of the glenohumeral joint is preserved [7••]. Recent anatomic and biomechanical advancements in treatment of posterosuperior RCT insufficiency with muscle tendon transfer have further encouraged further exploration of unique tendon transfers in addressing anterosuperior RCT insufficiency [8–10].
Regarding anterosuperior RC insufficiency, a deficient subscapularis disrupts force coupling in the transverse plane of the GH joint, often manifesting as pain and functional deficit including loss of internal rotation strength and eventually anterior instability [11]. Additionally, the presence of a coexistent supraspinatus tear may introduce vertical imbalance, causing anterosuperior migration of the humeral head [12]. Isolated subscapularis tendon tears are uncommon, with a reported incidence of 3–10%, and very few tendon transfers have been described to address irreparable subscapularis tears including transfers of the pectoralis major, pectoralis minor, and latissimus dorsi [12–15]. To date, each procedure appears to improve outcomes, yet further comparative studies are still needed to determine relative indications for each.
Subscapularis
Anatomy
The subscapularis is the largest, most powerful rotator cuff muscle, originating from the ventral surface of the scapular body, providing approximately 50% of the rotator cuff force [16]. The tendinous portion of its insertion, comprising the superior two thirds of the muscle, inserts variably onto the lesser tuberosity and bicipital groove. The muscular portion of its insertion, comprising the inferior third, inserts onto the lesser tuberosity and anterior aspect of the humeral metaphysis [17]. The subscapularis is innervated by the upper and lower subscapularis nerves, and differences in activation during shoulder movement may suggest functional independence between superior and inferior portions of the muscle [18].
Biomechanics
The subscapularis confers both active and passive stability at the GH joint. The primary role of the subscapularis is internal rotation. Secondarily, superior fibers assist predominately in abduction while inferior fibers assist in adduction [19]. Considering its role in dynamic stabilization through balanced force coupling, the subscapularis resist the infraspinatus in the axial plane and the shearing forces of the deltoid in the coronal plane with tensioning of the inferior fibers [20]. Passively, the subscapularis provides an anterior buttressing effect, resisting dislocation anteriorly [21].
Injury Pattern
Subscapularis tears may be degenerative in nature or secondary to acute trauma, increasing in prevalence as individuals age [22]. Combined subscapularis and supraspinatus tears are more common than isolated subscapularis tendon tears, commonly attributed to increased stress at the subscapularis tendon insertion as opposed to subcoracoid impingement [23, 24]. As for acute rupture, the subscapularis is most vulnerable during eccentric loading with hyperextension and abduction of the arm; partial tears commonly involve the undersurface of the tendon, extending medially without involvement of superficial fibers, and full-thickness tears commonly occur at the tendinous insertion [11]. Subscapularis tears have also been associated with anterior GH dislocation [25].
Non-operative vs. Operative Considerations
Non-operative management of subscapularis tendon tears, including activity modification, analgesics, anti-inflammatories, corticosteroid injections, and physical therapy, is similar to that involving standard posterosuperior rotator cuff pathology. Previously mentioned conservative measures are useful in improving range of motion, strengthening, and reducing pain in low-demand, elderly patients or those unfit for surgery because of comorbid conditions [3]. Older, less active patients with chronic degenerative tears commonly trial non-operative management, yet failure of these therapy modalities is an indication for surgery.
Indications for surgical intervention in subscapularis tendon tears essentially parallel that of any rotator cuff repair. As the risk of tear progression persists with non-operative therapies, there is a general consensus that acute RCTs, including the subscapularis, should be intervened upon more urgently to prevent further retraction and atrophy [26].
Irreparable Tears
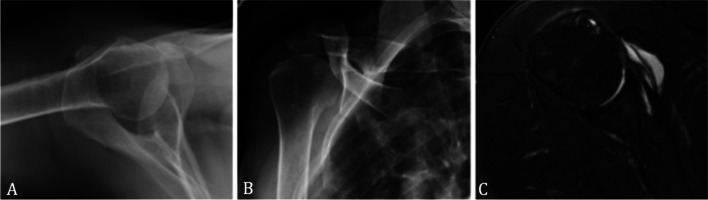
Irreparable rotator cuff tears cannot be repaired primarily because of excessive tendinous retraction and muscular atrophy. Although no rigid guidelines exist, poor outcomes including increased risk of postoperative retearing have been associated with length and width of the tear exceeding 40 mm [27], severe fatty infiltration (Goutallier stage 3 or 4) [28], and a narrowed acromiohumeral interval [29] (Fig. 1C). Currently, salvage options for irreparable isolated subscapularis tendon tears are anterior capsular reconstruction [30], tendon transfer [7••], and reverse shoulder arthroplasty [31].
Fig. 1.
X-ray and MRI findings of tendon transfer candidates. A Concentric glenohumeral joint without evidence of static decentering. B Grashey AP of the shoulder, without degenerative glenohumeral findings. C Axial T2-weighted MRI demonstrating a retracted, torn subscapularis
Tendon Transfer
Relative Indications
Tendon transfer may be utilized as a salvage procedure in irreparable subscapularis tears with minimal glenohumeral arthritis. Comparatively, anterior capsular reconstruction affords restoration of anteroinferior stability at the expense of range of motion, and reverse shoulder arthroplasty is reserved for older patients with shoulder instability and osteoarthritis. The ideal candidate for tendon transfer is a young patient whose primary complaint is weakness without glenohumeral arthropathy (Fig. 1A, B). The goal of the procedure is restoration of balanced force coupling about the GH joint to restore joint kinematics [5], effectively relieving pain, restoring range of motion, and enhancing shoulder function.
Pectoralis Major
The pectoralis major (PM) is found at the anterior superior chest, allowing adduction, flexion, and internal rotation of the humerus. Both clavicular and sternal origins converge to a common insertion site on the anterior humerus, just lateral to the bicipital groove [32]. Different variations of the PM transfer have been described, particularly, transferring the tendon superficial or deep to the conjoint tendon. Biomechanical studies have shown that transferring the tendon deep to the coracoid restores glenohumeral kinematics more effectively, as the line of action more closely mimics that of the subscapularis [33]. However, transfer deep to the conjoint requires dissection of the musculocutaneous nerve and the transferred muscle theoretically could impinge or stretch this nerve. Despite this concern of the nerve proximity, postoperative palsy following tendon transfer deep to the conjoint is reportedly rare [34]. In the absence of anterior instability or static anterior subluxation, PM tendon transfer has extensively demonstrated its efficacy in alleviating pain and improving subjective measures of function in patients with isolated, irreparable subscapularis tears [11, 35••]. An important consideration with any tendon transfer is the deficits seen when the donor tendon is no longer in its native orientation. Transfer of the entire pectoralis major would be expected to result in loss of flexion and adduction strength, and thus, for this reason, and the size constraint of rerouting the tendon between the musculocutaneous nerve, the conjoint tendon and the coracoid, typically only a portion (e.g., the superior half) of the tendon is used [36].
Pectoralis Minor
The pectoralis minor (PMi) is found at the anterior superior chest, originating from ribs three through five and inserting onto the medial aspect of the coracoid process [37]. It provides shoulder stability by downwardly depressing, internally rotating and anteriorly tilting the scapula, but in modern, screen-based society, it is frequently tight and, indeed, release of this tendon has shown no noted functional deficits [38]. Tendinous transfer of its insertion onto the lesser tuberosity, specifically in tears of the upper two-thirds of the subscapularis tendon with a concomitant supraspinatus tear, is anatomically feasible with improvements in shoulder function and pain relief [13]. The PMi is a smaller muscle than the PM and has a shorter tendon. However, the PMi line of pull is close to the subscapularis and early results show feasibility with arthroscopic and open techniques [13, 39]. Transferring the tendon deep to the coracoid, as with PM tendon transfer, is safe with respect to its proximity to the brachial plexus and musculocutaneous nerve, yet significant questions persist as available studies have excluded patient with anterior instability or static anterior subluxation of the GH joint. Additionally, increases in strength following PMi tendon transfer have demonstrated stagnancy, with no appreciable increases in strength over time, potentially explained by over distention of the muscle fibers upon transfer to a more lateral insertion [40••]. As for the significant reduction in pain following PMi transfer, this has been attributed to its passive tenodesis effect, referring to the restoration of anterior to posterior force coupling at the GH joint [13].
Latissimus Dorsi
The latissimus dorsi (LD) is a powerful thoracohumeral muscle with a broad origin, including the inferior angle of the scapula, the 9th to 12th ribs, the spinous process of the 7th to 12th thoracic vertebrae, the thoracolumbar fascia, and the posterior one-third of the iliac crest, that inserts onto the lesser tuberosity. This allows for extension, adduction, and internal rotation of the humerus. Utilizing the latissimus dorsi for tendon transfers around the shoulder is well studied, and in the case of irreparable subscapularis tear, particularly synergistic effects potentially exist given each muscle is innervated by the posterior chord of the brachial plexus. Surgical technique for transferring the LD tendon anteriorly to the lesser tuberosity has evolved, now performed open, arthroscopically assisted, and entirely arthroscopically. The LD has been a “workhorse” flap for free tissue transfer after the advent of microvascular surgery, and an extensive literature in this field shows minimal deficits in the majority of patients even with complete harvest of the LD, though highly athletic patients can perceive the loss [41, 42, 43••].
Comparative Studies
Biomechanics
With various, well described, tendon transfer techniques addressing irreparable subscapularis tendon tears, the most optimal transfer is still to be delineated. Biomechanically, PM transfer has provided consistent improvements in pain, yet functional limitations exist with reductions in internal rotation power over time [44]. LD transfer has been more recently adopted in hopes of a more biomechanically advantaged transfer, as the LD line of action more closely mimics that of the subscapularis [8].
In 2022, Kontaxis et al. provided insight into the biomechanical function of pectoralis major, pectoralis minor, and latissimus dorsi tendon transfers to the lesser tuberosity. This study demonstrated that LD transfer most closely mimics internal rotation moment arms generated by the subscapularis at the expense of some adduction strength at the shoulder. Interestingly so, PM transfer was found to reduce internal rotation by roughly 30° regardless of the degree of abduction. While internally rotating the humeral head, the attachment site and origin of the PM and PMi align, leading to anterior translation of the humeral head rather than internal rotation torque. However, the LD maintains its normal distance from the center of the humeral head, allowing for a constant internal rotation moment arm throughout its contraction. This was posited to potentially explain poor functional outcomes in patients with instability or anterior subluxation of the humeral head after PM tendon transfer. For this reason, it was also suggested that LD transfer might provide the greatest functional improvement, particularly in internal rotation, of patients with irreparable subscapularis tendon tears [45••].
Outcomes
Although PM and LD tendon transfers have produced good clinical outcomes, the existing body of literature has remained fairly devoid of comparative studies to appropriately assess which is superior. In 2022, Luo et al. sought to provide consensus to this discussion by performing a systematic review comparing outcomes following PM and LD tendon transfer for irreparable subscapularis tendon tears. In total, 12 studies were included for analysis, capturing 269 shoulders treated with tendon transfer, 184 by PM tendon transfer and 85 by LD tendon transfer. In both PM and LD groups, patients improved postoperatively with respect to Constant Murley Score (CMS), the primary outcome of the study, along with secondary outcomes (VAS, SSV, ROM, bell-press test, and lift-off test) with low rates of complications and failure. When compared, LD tendon transfer showed greater improvements in CMS, abduction, forward flexion, external rotation, and bell-press test [46••]. However, there were several limitations to this systematic review, including limited availability of studies addressing LD tendon transfer in anterosuperior rotator cuff tears as well as limited mean follow-up (17.4 months) compared to the PM group (66.9 month). However, most complications were found to have occurred within 12 months postoperatively, and clinical outcomes peaking within 12 months as well. Lastly, the majority of the studies included were considered level 4 evidence, meaning high-quality comparative evidence was insufficient, and future, randomized control trials are still needed to reach a more definitive consensus.
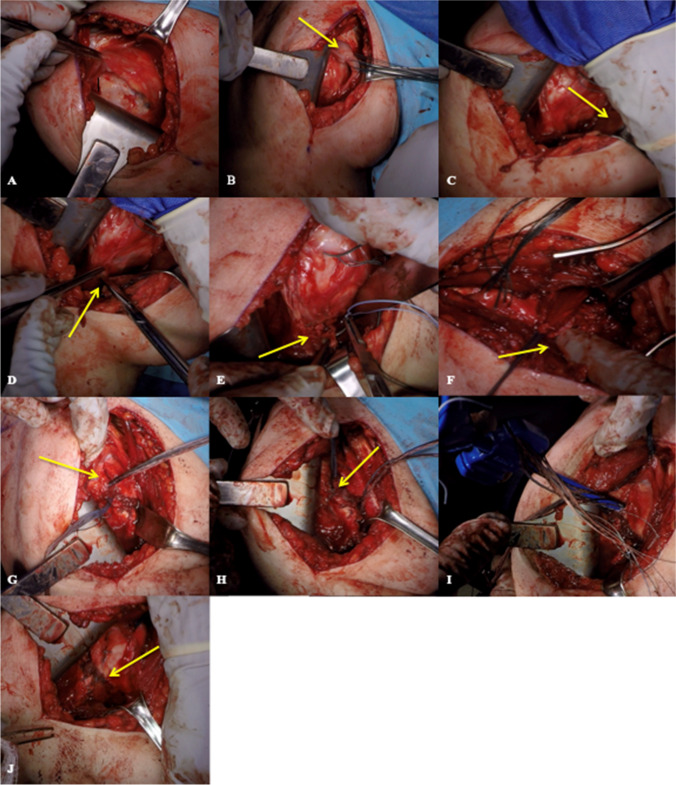
Author’s Preference
In our practice, we favor an anterior, open approach for LD tendon transfer in the setting of irreparable subscapularis tears. Patients are positioned in a beach chair position, under general anesthesia with an interscalene block, and a standard deltopectoral approach is utilized. The lesser tuberosity is exposed (Fig. 2A), and an attempt to mobilize and repair any remaining subscapularis tendon is made (Fig. 2B). The proximal quarter to third of the PM tendon is then detached, providing access to then dissect distally along the latissimus dorsi tendon insertion, separating it from the teres major (Fig. 2D). The LD tendon is detached from its humeral insertion, and with traction applied through sutures, is mobilized (Fig. 2E). The LD muscle is released using limited dissection with Metzenbaum scissors to avoid adjacent neurovascular structures and then bluntly with finger dissection, permitting further excursion of the tendon (Fig. 2F). Once sufficient tendon excursion is achieved, the LD tendon is transferred to the lesser tuberosity. The tendon should be mobilized enough to suture the leading edge of the broad tendon to the anterior cable of the supraspinatus. Additional fixation is achieved with a double row, trans-osseous equivalent repair of the tendon to the lesser tuberosity (Fig. 2G, H, I).
Fig. 2.
Open, anterior LD tendon transfer. A Exposure to the bare lesser tuberosity. B Torn subscapularis retrieved and elevated to accommodate tendon transfer. C Pectoralis retracted away from LD tendon. D LD tendon carefully dissected away from teres major. E Traction sutures placed LD tendon. F Gentle digital mobilization achieves adequate excursion to transfer LD tendon to lesser tuberosity. G Triple-loaded all tape suture placed at inferior aspect of lesser tuberosity. H Traction suture through LD tendon tied into native supraspinatus anterior cable. I Triple-loaded all tape sutures passed through 5.5-mm SwiveLock anchor, placed superior to lesser tuberosity, providing broad footprint reduction. J Remnant subscapularis sutured over the LD tendon, providing additional biologic support
To avoid complications, relevant nerve anatomy must be respected. The radial nerve lies on the anterior aspect of the latissimus dorsi tendon, approximately 1.5 to 5 cm medial to the insertion with the greatest distance in abduction and external rotation, thus dissection should proceed bluntly if more than a few cm from the tendon insertion and in this position [47•]. Furthermore, the teres major, immediately posterior and often adherent to the LD, must be dissected free from the LD. The two have very different morphology with the LD flat and tendinous and the teres major a fleshy muscle with a very short tendon. Leaving the teres intact (and repairing any PM taken down in the approach) is important as preserving adductors and internal rotators is relevant—especially as many of these patients may need reverse total shoulder later in life. Lastly, if the teres major is left intact, it protects the axillary nerve [48].
Clinical Reflection
Isolated, irreparable subscapularis tears are relatively rare, and because of this, technical complexities should be minimized [12]. Proponents of arthroscopic assistance in LD transfer suggest arthroscopic evaluation of the glenohumeral joint permits optimal partial repair of any remaining rotator cuff and more precise detachment of the LD tendon from the teres major [7••]. In addition, incorporation of a separate axillary incision permitting extensive release of adhesion allows maximal excursion of the LD tendon prior to transfer; however, careful consideration of the tendon’s anatomic relationship to the axillary nerve must be nuanced as the tendon is transferred from the axillary incision to the lesser tuberosity. In our experience, the anterior, open approach to LD tendon transfer introduces the least technical complexity, accomplishing the goals of restoring balanced force coupling and increasing function. In fact, we posit that extensive lysis of adhesions utilizing a separate axillary incision could potentially produce redundancy anteriorly, allowing undesirable anterior translation of the humeral head secondary to an imbalance force couple in the transverse plane.
Conclusion
Transfer of the pectoralis major has been considered the transfer of choice for irreparable subscapularis tears for decades, with established long-term follow-up supporting its efficacy in reducing pain and function, yet improvements in range of motion and internal rotation were not maintained over time. Because of this degradation in functional improvement, transfer of the latissimus dorsi tendon has certainly become an attractive option. Recent cadaveric biomechanical studies have demonstrated its efficacy in maintaining an internally rotating moment arm at the glenohumeral joint and promising short-term clinical results with respect to improvements in pain and functional shoulder scores. Open, arthroscopic, and combined techniques for latissimus dorsi tendon transfer are described, and we believe that the open, anterior approach alone affords optimal clinical outcomes to patients, minimizing technical complexity and risk of injury to major anatomical structures.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of these authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Huegel J, Williams AA, Soslowsky LJ. Rotator cuff biology and biomechanics: a review of normal and pathological conditions. Curr Rheumatol Rep. 2015;17(1):476. doi: 10.1007/s11926-014-0476-x. [DOI] [PubMed] [Google Scholar]
- 2.Abboud JA, Soslowsky LJ. Interplay of the static and dynamic restraints in glenohumeral instability. Clin Orthop Relat Res. 2002;400:48–57. doi: 10.1097/00003086-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Oh JH, Jun BJ, McGarry MH, Lee TQ. Does a critical rotator cuff tear stage exist?: a biomechanical study of rotator cuff tear progression in human cadaver shoulders. J Bone Joint Surg Am. 2011;93(22):2100–2109. doi: 10.2106/jbjs.J.00032. [DOI] [PubMed] [Google Scholar]
- 4.Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589–604. doi: 10.1016/j.csm.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Warner JJ. Management of massive irreparable rotator cuff tears: the role of tendon transfer. Instr Course Lect. 2001;50:63–71. [PubMed] [Google Scholar]
- 6.Neri BR, Chan KW, Kwon YW. Management of massive and irreparable rotator cuff tears. J Shoulder Elbow Surg. 2009;18(5):808–818. doi: 10.1016/j.jse.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 7.Burnier M, Lafosse T. Pectoralis major and anterior latissimus dorsi transfer for subscapularis tears. Curr Rev Musculoskelet Med. 2020;13(6):725–733. doi: 10.1007/s12178-020-09674-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mun SW, Kim JY, Yi SH, Baek CH. Latissimus dorsi transfer for irreparable subscapularis tendon tears. J Shoulder Elbow Surg. 2018;27(6):1057–1064. doi: 10.1016/j.jse.2017.11.022. [DOI] [PubMed] [Google Scholar]
- 9.Elhassan BT, Wagner ER, Bishop AT. Feasibility of contralateral trapezius transfer to restore shoulder external rotation: part I. J Shoulder Elbow Surg. 2012;21(10):1363–1369. doi: 10.1016/j.jse.2011.10.031. [DOI] [PubMed] [Google Scholar]
- 10.Li X, Cusano A, Eichinger J. Eden-Hybinette and pectoralis major transfer for recurrent shoulder instability due to failed Latarjet and chronic subscapularis rupture. Orthopedics. 2017;40(1):e182–e187. doi: 10.3928/01477447-20161006-02. [DOI] [PubMed] [Google Scholar]
- 11.Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br Vol. 1991;73(3):389–94. doi: 10.1302/0301-620x.73b3.1670434. [DOI] [PubMed] [Google Scholar]
- 12.Resch H, Povacz P, Ritter E, Matschi W. Transfer of the pectoralis major muscle for the treatment of irreparable rupture of the subscapularis tendon. J Bone Joint Surg Am. 2000;82(3):372–382. doi: 10.2106/00004623-200003000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Paladini P, Campi F, Merolla G, Pellegrini A, Porcellini G. Pectoralis minor tendon transfer for irreparable anterosuperior cuff tears. J Shoulder Elbow Surg. 2013;22(6):e1–5. doi: 10.1016/j.jse.2012.12.030. [DOI] [PubMed] [Google Scholar]
- 14.Kany J, Guinand R, Croutzet P, Valenti P, Werthel JD, Grimberg J. Arthroscopic-assisted latissimus dorsi transfer for subscapularis deficiency. Eur J Orthop Surg Traumatol. 2016;26(3):329–334. doi: 10.1007/s00590-016-1753-3. [DOI] [PubMed] [Google Scholar]
- 15.Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89(6):1184–1193. doi: 10.2106/jbjs.F.00007. [DOI] [PubMed] [Google Scholar]
- 16.Keating JF, Waterworth P, Shaw-Dunn J, Crossan J. The relative strengths of the rotator cuff muscles. A cadaver study. J Bone Joint Surg Br Vol. 1993;75(1):137–40. doi: 10.1302/0301-620x.75b1.8421011. [DOI] [PubMed] [Google Scholar]
- 17.Morag Y, Jamadar DA, Miller B, Dong Q, Jacobson JA. The subscapularis: anatomy, injury, and imaging. Skeletal Radiol. 2011;40(3):255–269. doi: 10.1007/s00256-009-0845-0. [DOI] [PubMed] [Google Scholar]
- 18.Kadaba MP, Cole A, Wootten ME, McCann P, Reid M, Mulford G, et al. Intramuscular wire electromyography of the subscapularis. J Orthop Res. 1992;10(3):394–397. doi: 10.1002/jor.1100100312. [DOI] [PubMed] [Google Scholar]
- 19.Kato K. Innervation of the scapular muscles and its morphological significance in man. Anat Anz. 1989;168(2):155–168. [PubMed] [Google Scholar]
- 20.Aluisio FV, Osbahr DC, Speer KP. Analysis of rotator cuff muscles in adult human cadaveric specimens. Am J Orthop (Belle Mead NJ) 2003;32(3):124–129. [PubMed] [Google Scholar]
- 21.Symeonides PP. The significance of the subscapularis muscle in the pathogenesis of recurrent anterior dislocation of the shoulder. J Bone Joint Surg Br Vol. 1972;54(3):476–83. doi: 10.1302/0301-620X.54B3.476. [DOI] [PubMed] [Google Scholar]
- 22.Deutsch A, Altchek DW, Veltri DM, Potter HG, Warren RF. Traumatic tears of the subscapularis tendon. Clinical diagnosis, magnetic resonance imaging findings, and operative treatment. Am J Sports Med. 1997;25(1):13–22. doi: 10.1177/036354659702500104. [DOI] [PubMed] [Google Scholar]
- 23.MacMahon PJ, Taylor DH, Duke D, Brennan DD, O'Brien J, Eustace SJ. Contribution of full-thickness supraspinatus tendon tears to acquired subcoracoid impingement. Clin Radiol. 2007;62(6):556–563. doi: 10.1016/j.crad.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 24.Bergin D, Parker L, Zoga A, Morrison W. Abnormalities on MRI of the subscapularis tendon in the presence of a full-thickness supraspinatus tendon tear. AJR Am J Roentgenol. 2006;186(2):454–459. doi: 10.2214/ajr.04.1723. [DOI] [PubMed] [Google Scholar]
- 25.Neviaser RJ, Neviaser TJ. Recurrent instability of the shoulder after age 40. J Shoulder Elbow Surg. 1995;4(6):416–418. doi: 10.1016/s1058-2746(05)80032-1. [DOI] [PubMed] [Google Scholar]
- 26.Goldberg DB, Tamate TM, Hasegawa M, Kane TJKT, You JS, Crawford SN. Literature review of subscapularis tear, associated injuries, and the available treatment options. Hawai’i J Health Soc Welfare. 2022;81(3 Suppl 1):2–7. [PMC free article] [PubMed] [Google Scholar]
- 27.Sugihara T, Nakagawa T, Tsuchiya M, Ishizuki M. Prediction of primary reparability of massive tears of the rotator cuff on preoperative magnetic resonance imaging. J Shoulder Elbow Surg. 2003;12(3):222–225. doi: 10.1016/s1058-2746(02)86888-4. [DOI] [PubMed] [Google Scholar]
- 28.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. doi: 10.1097/00003086-199407000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Nové-Josserand L, Edwards TB, O'Connor DP, Walch G. The acromiohumeral and coracohumeral intervals are abnormal in rotator cuff tears with muscular fatty degeneration. Clin Orthop Relat Res. 2005;433:90–96. doi: 10.1097/01.blo.0000151441.05180.0e. [DOI] [PubMed] [Google Scholar]
- 30.Komperda KW, Adamson GJ, Itami Y, McGarry MH, Kantor A, Lin CC, et al. Anterior capsule reconstruction versus pectoralis major transfer for irreparable subscapularis tears involving the anterior capsule: a comparative biomechanical cadaveric study. Arthroscopy. 2019;35(11):3002–3008. doi: 10.1016/j.arthro.2019.05.046. [DOI] [PubMed] [Google Scholar]
- 31.Edwards TB, Williams MD, Labriola JE, Elkousy HA, Gartsman GM, O'Connor DP. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18(6):892–896. doi: 10.1016/j.jse.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 32.Chiavaras MM, Jacobson JA, Smith J, Dahm DL. Pectoralis major tears: anatomy, classification, and diagnosis with ultrasound and MR imaging. Skeletal Radiol. 2015;44(2):157–164. doi: 10.1007/s00256-014-1990-7. [DOI] [PubMed] [Google Scholar]
- 33.Konrad GG, Sudkamp NP, Kreuz PC, Jolly JT, McMahon PJ, Debski RE. Pectoralis major tendon transfers above or underneath the conjoint tendon in subscapularis-deficient shoulders. An in vitro biomechanical analysis. J Bone Joint Surg Am Vol. 2007;89(11):2477–84. doi: 10.2106/jbjs.F.00811. [DOI] [PubMed] [Google Scholar]
- 34.Shin JJ, Saccomanno MF, Cole BJ, Romeo AA, Nicholson GP, Verma NN. Pectoralis major transfer for treatment of irreparable subscapularis tear: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):1951–1960. doi: 10.1007/s00167-014-3229-5. [DOI] [PubMed] [Google Scholar]
- 35.Ernstbrunner L, Wieser K, Catanzaro S, Agten CA, Fornaciari P, Bauer DE, et al. Long-term outcomes of pectoralis major transfer for the treatment of irreparable subscapularis tears: results after a mean follow-up of 20 years. J Bone Joint Surg Am. 2019;101(23):2091–2100. doi: 10.2106/jbjs.19.00172. [DOI] [PubMed] [Google Scholar]
- 36.Jennings GJ, Keereweer S, Buijze GA, De Beer J, DuToit D. Transfer of segmentally split pectoralis major for the treatment of irreparable rupture of the subscapularis tendon. J Shoulder Elbow Surg. 2007;16(6):837–842. doi: 10.1016/j.jse.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 37.Burley HEK, Haładaj R, Olewnik Ł, Georgiev GP, Iwanaga J, Tubbs RS. The clinical anatomy of variations of the pectoralis minor. Surg Radiol Anat: SRA. 2021;43(5):645–651. doi: 10.1007/s00276-021-02703-y. [DOI] [PubMed] [Google Scholar]
- 38.Servasier L, Jeudy J, Raimbeau G, Bigorre N. Arthroscopic release of the pectoralis minor tendon as an adjunct to acromioplasty in the treatment of subacromial syndrome associated with scapular dyskinesia. Orthop Traumatol Surg Res: OTSR. 2022;108(2):103211. doi: 10.1016/j.otsr.2022.103211. [DOI] [PubMed] [Google Scholar]
- 39.Yamakado K. Arthroscopic-assisted pectoralis minor transfer for irreparable anterosuperior massive rotator cuff tear. Arthrosc Tech. 2018;7(3):e193–e198. doi: 10.1016/j.eats.2017.08.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sánchez Carbonel JF, Hinz M, Lozano C, Kleim BD, Imhoff AB, Siebenlist S. Pectoralis major and pectoralis minor transfer for irreparable subscapularis tendon tears. Oper Orthop Traumatol. 2022;34(1):45–54. doi: 10.1007/s00064-021-00760-5. [DOI] [PubMed] [Google Scholar]
- 41.Lee KT, Mun GH. A systematic review of functional donor-site morbidity after latissimus dorsi muscle transfer. Plast Reconstr Surg. 2014;134(2):303–314. doi: 10.1097/prs.0000000000000365. [DOI] [PubMed] [Google Scholar]
- 42.Koh CE, Morrison WA. Functional impairment after latissimus dorsi flap. ANZ J Surg. 2009;79(1–2):42–47. doi: 10.1111/j.1445-2197.2008.04797.x. [DOI] [PubMed] [Google Scholar]
- 43.Elhassan BT, Wagner ER, Kany J. Latissimus dorsi transfer for irreparable subscapularis tear. J Shoulder Elbow Surg. 2020;29(10):2128–2134. doi: 10.1016/j.jse.2020.02.019. [DOI] [PubMed] [Google Scholar]
- 44.Elhassan B, Ozbaydar M, Massimini D, Diller D, Higgins L, Warner JJ. Transfer of pectoralis major for the treatment of irreparable tears of subscapularis: does it work? J Bone Joint Surg Br Vol. 2008;90(8):1059–1065. doi: 10.1302/0301-620x.90b8.20659. [DOI] [PubMed] [Google Scholar]
- 45.Kontaxis A, Lawton CD, Sinatro A, Bachner E, Lamplot JD, Dines DM, et al. Biomechanical analysis of latissimus dorsi, pectoralis major, and pectoralis minor transfers in subscapularis-deficient shoulders. J Shoulder Elbow Surg. 2022;31(2):420–427. doi: 10.1016/j.jse.2021.08.022. [DOI] [PubMed] [Google Scholar]
- 46.Luo Z, Lin J, Sun Y, Zhu K, Wang C, Chen J. Outcome comparison of latissimus dorsi transfer and pectoralis major transfer for irreparable subscapularis tendon tear: a systematic review. Am J Sports Med. 2022;50(7):2032–2041. doi: 10.1177/03635465211018216. [DOI] [PubMed] [Google Scholar]
- 47.Gates S, Sager B, Collett G, Chhabra A, Khazzam M. Surgically relevant anatomy of the axillary and radial nerves in relation to the latissimus dorsi tendon in variable shoulder positions: a cadaveric study. Should Elb. 2020;12(1):24–30. doi: 10.1177/1758573218825476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Elhassan BT. Feasibility of latissimus and teres major transfer to reconstruct irreparable subscapularis tendon tear: an anatomic study. J Shoulder Elbow Surg. 2015;24(4):e102–e103. doi: 10.1016/j.jse.2014.12.035. [DOI] [PubMed] [Google Scholar]