Abstract
The long-term effects of SARS-CoV-2 infection represent a relevant global health problem. Long COVID (LC) is defined as a complex of signs and symptoms developed during or after SARS-CoV-2 infection and lasting > 12 weeks. In common variable immunodeficiency (CVID) patients, we previously reported higher risk of hospitalization and death during SARS-CoV-2 infection, as well as prolonged swab positivity and frequent reinfections. The aim of the present study was to assess the risk of LC in an Italian cohort of CVID patients. We used a translated version of the survey proposed by Centers for Disease Control and Prevention (CDC) to collect data on LC. In the enrolled cohort of 175 CVID patients, we found a high prevalence of LC (65.7%). The most frequent LC symptoms were fatigue (75.7%), arthralgia/myalgia (48.7%), and dyspnea (41.7%). The majority of patients (60%) experienced prolonged symptoms, for at least 6 months after infection. In a multivariate analysis, the presence of complicated phenotype (OR 2.44, 95% CI 1.88–5.03; p = 0.015), obesity (OR 11.17, 95% CI 1.37–90.95; p = 0.024), and female sex (OR 2.06, 95% CI 1.09–3.89; p = 0.024) significantly correlated with the development of LC. In conclusion, in this multicenter observational cohort study, we demonstrated that CVID patients present an increased prevalence of LC when compared to the general population. Improved awareness on the risk of LC in CVID patients could optimize management of this new and alarming complication of SARS-CoV-2 infection.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10875-024-01656-2.
Keywords: Long COVID, common variable immunodeficiency, SARS-CoV-2, COVID-19, complicated phenotype, chronic lung disease, obesity
Introduction
COVID-19 affected more than 770 million people (772,166,517 people at last update) worldwide since February 2020 and resulted in millions of hospitalizations and more than 6.9 million deaths (6,987,831 deaths at last update), representing a global health emergency (https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports, last access December 22nd 2023) [1]. The long-term effects of SARS-CoV-2 infection in the COVID-19 disease survivors have been less explored than the acute phase of infection, but it represents a relevant global health problem involving millions of people worldwide with social and economic repercussions [2]. Post-acute sequelae of various infections in the general population have been extensively reported in literature, in particular after Epstein-Barr virus, Giardia lamblia, and other coronavirus infections (SARS-CoV and Middle East respiratory syndrome-CoV) [3–5]. According to the World Health Organization (WHO), long COVID (LC), also known as post-acute sequelae of COVID-19 (PASC), or post COVID-19 condition is defined as the presence of signs and symptoms developed during or after COVID-19 and continuing for more than 12 weeks, not explained by an alternative diagnosis [6].
Since different definitions of LC are available and different study designs were used, it is difficult to estimate the real prevalence of this condition worldwide. According to the WHO, 10 to 20% of adults infected with SARS-CoV-2 eventually develop LC (https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition; last access December 22, 2023) [7]. The most recent data from the Center for Disease Control and Prevention (CDC) on the US population report that LC affects 11% of adults previously infected with SARS-CoV-2 [8]. Epidemiological data on LC in the Italian population are not available. LC symptoms include fatigue, cough, dyspnea, chest pain, palpitation, headache, anosmia, dysgeusia, musculoskeletal symptoms like myalgias and arthralgias, brain fog, and other cognitive disorders. Moreover, neuropsychiatric dysfunctions, such as depression, anxiety, and sleep disturbance, have been described [9], as well as gastrointestinal (diarrhea, nausea), renal (hematuria, oliguria), endocrine alterations (amenorrhea), and dermatological manifestation (cutaneous rash) [10]. LC symptoms generally affect daily activity with an important negative effect on health-related quality of life (HRQoL) [11]. A meta-analysis showed that female sex is a risk factor for the development of LC [12]. In the general population, older age (> 65 years old), obesity and cardiovascular comorbidities, and chronic obstructive pulmonary disease (COPD) and asthma were found to be risk factors for LC [10, 13, 14]. A severe course of SARS-CoV-2 infection and the duration of hospitalization were linked to a higher odds of LC, while vaccination was protective [15–18]. Of note, patients with LC show an impaired formation of anti-SARS-CoV-2 neutralizing antibodies and anti-Spike protein and lower levels of IgG3 antibodies [19, 20].
Inborn errors of immunity (IEIs) are a group of heterogeneous disorders resulting in increased susceptibility to infections, development of autoimmune conditions, and increased risk of malignancy [21]. Higher hospitalization and mortality due to COVID-19 have been reported in this group of patients when compared to the general population in different studies [22–24].
Within IEIs, common variable immunodeficiency (CVID) is the most frequent symptomatic disorder in adults [25]. Despite the higher susceptibility to infections, studies focusing on their post-acute sequelae in CVID are lacking. Besides a higher risk of hospitalization and death during SARS-CoV-2 infection, these patients experienced prolonged course of COVID-19 and a higher rate of reinfection [26, 27].
Thus, these patients could be prone to develop LC, taking into account a potential impaired antibody response and a high prevalence of pre-existing lung damage. However, to date, no study addresses LC in patients with primary antibody deficiencies. We performed a retrospective observational cohort study with the aim to determine the prevalence of LC in an Italian multicentric cohort of CVID patients. Secondly, we tried to define general and specific risk factors for the development of LC.
Methods
We performed a multicentric retrospective observational cohort study including a cohort of consecutive patients with a CVID diagnosis established according to the European Society for Immunodeficiencies (ESID) criteria [28]. The population was selected from four Italian referral centers for primary immune deficiencies of Rome, Naples, Padua, and Cagliari. The study period lasted from March 1, 2020, to June 1, 2023. The inclusion criteria were diagnosis of CVID, age ≥ 18 years, a documented SARS-CoV-2 infection, and a follow-up ≥ 6 months after infection. SARS-CoV-2 positivity was assessed by approved tests (PCR molecular test and rapid antigen test with determination of cut off index). Genotype assessment of SARS-CoV-2 variant on nasopharyngeal swabs was not systematically conducted. The infection strain was attributed mostly on the basis of the date of the positive test, according to the epidemiological data available for National Health Authorities of Italy [29, 30]. The duration of SARS-CoV-2 infection was recorded as the days from the first positive swab to the first negative one. Reinfection was defined as the record of a new positive SARS-CoV-2 test > 90 days after the resolution of the first infection. Data about sex, age, body mass index (BMI), CVID clinical phenotype, comorbidities, ongoing therapies, COVID-19 disease severity, vaccination status, and SARS-CoV-2-specific treatments, such as antiviral therapy or monoclonal antibodies (mAbs), were collected. Considering BMI values, the population was divided into underweight (BMI < 18.5), normal weight (BMI from 18.5 to 24.9), overweight (BMI from 25.0 to 29.9), and obese (BMI ≥ 30.0). BMI presented is the habitual value, preceding SARS-CoV-2; data was assessed also after infection, and no variations were found in our cohort. Comorbidities recorded included obesity, arterial hypertension, previous cardiovascular events, chronic arterial disease, diabetes mellitus, chronic kidney disease (CKD), and malignancy. The SARS-CoV-2 infection’s complications reported were hospitalization, pulmonary thromboembolism (PTE), and bacterial superinfections. Chronic lung disease was considered in the presence of any pre-existing chronic pulmonary involvement, in particular bronchiectasis and/or granulomatous lymphocytic interstitial lung disease (GLILD) and/or end-stage lung disease (ESLD) and/or asthma and/or COPD. ESLD was defined as chronic oxygen-dependent respiratory failure. Chronic immunosuppressive treatment was considered in the presence of chronic administration of steroids and/or disease-modifying antirheumatic drugs (DMARD) and/or mAbs for immunosuppressive purposes. The CVID cohort was classified into two different clinical phenotypes according to Chapel’s criteria: “infection only” and “complicated’’ [31]. All patients enrolled in the study were on IgG replacement therapy (IgRT), and IgG trough level (IgG TL) was included in the laboratory data collection. COVID-19 severity was defined according to WHO classification [32]. Due to the small sample size, moderate and severe COVID-19 disease were merged in a single group (moderate-severe patients), including also intensive care unit (ICU) admission. Data about thoracic computed tomography were not available for the entire cohort, so not included in the study. All vaccinated patients received a mRNA vaccine, namely, BNT162b2. The dates of the first positive and the first negative SARS-CoV-2 test were recorded to evaluate the duration of the RT-PCR positivity.
According to WHO definition, LC was defined as “Signs and symptoms that develop during or after SARS-CoV-2 infection and continue for more than 12 weeks and are not explained by an alternative diagnosis” [33]. The survey proposed by CDC was used to collect data on LC [34]. Figure S1 shows the Italian translated version of CDC long COVID survey. The symptoms evaluated in the survey were fatigue, mental fog, difficulty breathing/shortness of breath, joint/muscle pain, palpitations, chest pain, dizziness, changes in the menstrual cycle (for female patients), difficulty in tasting and smelling, and inability to exercise. After obtaining informed consent, the questionnaire was offered to patients by trained health professionals, during an outpatient or a telematic visit. The LC questionnaire data collection took place from October 1, 2022, to June 1, 2023. The study was approved by the Local Ethical Committee and was performed in accordance with the most recent version of the Declaration of Helsinki.
Statistical Analysis
Patient characteristics were summarized using medians, standard deviations, interquartile ranges (IQR), and percentages as appropriate. Chi-squared tests of independence or Fisher’s exact tests were used for categorical data as appropriate. Mann–Whitney U was used for unpaired continuous data. Binomial logistic regression models were fitted to calculate odds ratios (OR) with 95% confidence intervals (95% CI). To confirm the finding, multivariable logistic regression analysis was performed considering age, sex, SARS-CoV-2 infection course, and considerable CVID features. Statistical significance was considered as a p value < 0.05. All the analyses were performed using Jamovi version 2.3.28.0.
Results
A total of 224 CVID patients who experienced SARS-CoV-2 infection were enrolled in this study from March 1, 2020, to June 1, 2023. Since eight patients died during SARS-CoV-2 infection or in the next few months and two patients were lost at follow-up, the CDC LC survey was offered to 215 patients with 175 responders (81% of the total cohort). The median interval of time of follow-up since SARS-CoV-2 infection to the date of completion of the CDC survey was of 13 (IQR 11–16) months. The sex and age distribution of responders and general cohort were similar. Of note, 115/175 patients (65.7%) presented at least one symptom of LC (LC cohort). Patients without evidence of LC symptoms were included in the non-LC cohort.
Long COVID Features
In the LC cohort, 74 patients (64.3%) were females with a median age of 51 years (IQR 44.0–59.5). CVID clinical phenotype was complicated in 58 patients (50.4%) whereas 53 patients (46.1%) suffered from chronic lung disease and 44 (38.3%) showed bronchiectasis, 18 (15.7%) GLILD, and 2 (1.7%) met the criteria for ESLD. In addition, 35 patients (30.4%) presented, in their history, at least one episode of autoimmune cytopenia, in particular 32 (27.8%) immune thrombocytopenia (ITP) and five patients (4.3%) autoimmune hemolytic anemia (AIHA), two patients suffering of both conditions. CVID-related enteropathy was present in 16 patients (14.3%) of our LC cohort, while systemic autoimmune disease in nine patients (8.0%). Data about demographic features of the study population are summarized in Table 1. In the LC cohort, 83 patients (72.2%) got infected during the Omicron period and the median duration of infection was 18 days (IQR 11.0–23.5). At first infection, 31 patients (27%) were unvaccinated, while 59 patients (51.3%) were vaccinated with 3 doses and 17 (14.8%) with 4 doses. The COVID-19 severity was mild in 104 patients (90.4%), while 12 (9.6%) presented a moderate-severe infection that required hospitalization, and two patients (1.7%) required ICU admission. The complications reported during SARS-CoV-2 infection were PTE in one patient (0.9%) and bacterial superinfections in six patients (5.2%). Data about SARS-CoV-2 course of infection are summarized in Table 2.
Table 1.
Demographics, CVID-related features, and comorbidities of LC and non-LC cohort
| Survey responders (n = 175) (n (%)) | LC (115 (65.7)) | Non-LC (60 (34.2)) | p | OR (95% CI) |
|---|---|---|---|---|
| Demographics | ||||
| Median age (IQR) | 51 (44–59.5) | 48.5 (33–62.8) | 0.273 | 1.01 (0.99–1.03) |
| Sex (F) (%) | 74 (64.3) | 28 (46.7) | 0.024 | 2.06 (1.09–3.89) |
| Median BMI (IQR) | 23.5 (21.2–27) | 23.6(21–25.7) | 0.137 | 1.09 (1.01–1.19) |
| BMI underweight (%) | 5 (4.4) | 10 (17.2) | 0.008 | 0.22 (0.07–0.68) |
| BMI normal range (%) | 65 (57.0) | 28 (48.3) | 0.207 | 1.50 (0.80–2.84) |
| BMI overweight (%) | 30 (26.3) | 19 (32.8) | 0.514 | 0.79 (0.40–1.59) |
| BMI obesity (%) | 13 (11.4) | 1 (1.7) | 0.028 | 7.34 (0.93–57.5) |
| CVID clinical phenotype | ||||
| Complicated phenotype (%) | 58 (50.4) | 18 (30) | 0.010 | 2.37 (1.22–4.60) |
| Autoimmune cytopenia (%) | 35 (30.4) | 7 (11.7) | 0.002 | 3.94 (1.55–10.00) |
| ITP (%) | 32 (27.8) | 6 (10) | 0.007 | 3.47 (1.36–8.85) |
| AIHA (%) | 5 (4.3) | 3 (5) | 0.845 | 0.86 (0.20–3.74) |
| Enteropathy (%) | 16 (14.3) | 15 (25.4) | 0.072 | 0.49 (0.22–1.08) |
| Immunosuppressive therapy (%) | 12 (10.4) | 3 (5) | 0.233 | 2.21 (0.60–8.17) |
| Laboratory features | ||||
| Median lymphocyte count (IQR) | 1470 (1170–2060) | 1545 (1167–2205) | 0.939 | 1.00 (0.99–1.00) |
| Patients with IgA < 7 (%) | 56 (41.1) | 26 (44.8) | 0.594 | 0.84 (0.45–1.60) |
| IgG TL (IQR) | 708 (554–854) | 719 (543–859) | 0.939 | 1.00 (0.99–1.00) |
| Respiratory involvement | ||||
| Chronic lung disease (%) | 53 (46.1) | 21 (35.0) | 0.160 | 1.59 (0.83–3.03) |
| GLILD (%) | 18 (15.7) | 6 (10) | 0.302 | 1.67 (0.63–4.46) |
| Bronchiectasis (%) | 44 (38.3) | 18 (30) | 0.278 | 1.45 (0.74–2.82) |
| ESLD (%) | 2 (1.7) | 0 (0) | 0.547 | 2.67 (0.26–56.4) |
| Comorbidities | ||||
| Obesity (%) | 13 (11.4) | 1 (1.7) | 0.028 | 7.34 (0.93–57.5) |
| Hypertension (%) | 28 (24.3) | 13 (21.7) | 0.691 | 1.16 (0.55–2.46) |
| Diabetes mellitus (%) | 10 (8.7) | 3 (5) | 0.376 | 1.81 (0.48–6.84) |
| Cardiovascular events (%) | 6 (5.2) | 3 (5) | 0.951 | 1.05 (0.25–4.34) |
| Arterial disease (%) | 9 (7.8) | 5 (8.3) | 0.907 | 0.93 (0.30–2.92) |
| CKD (%) | 3 (2.6) | 3 (5) | 0.409 | 0.51 (0.10–2.60) |
| Cancers (%) | 16 (13.9) | 12 (20) | 0.297 | 0.65 (0.28–1.47) |
Statistically significant results in bold
Table 2.
SARS-CoV-2 course of infection of LC and non-LC cohorts
| Survey responders (n = 175) | LC (n = 115) | Non-LC (n = 60) | p | OR (95% CI) |
|---|---|---|---|---|
| Unvaccinated (%) | 31 (27) | 12 (21.7) | 0.303 | 1.50 (0.69–3.27) |
| Vaccination status 3 doses (%) | 59 (51.3) | 31 (51.7) | 0.325 | 0.70 (0.35–1.42) |
| Vaccination status 4 doses (%) | 17 (14.8) | 12 (20) | 0.380 | 0.69 (0.31–1.57) |
| Median days of infection (IQR) | 18 (11–23.5) | 13 (8–22) | 0.029 | 1.02 (0.99–1.05) |
| Wuhan + alpha | 25 (21.7) | 8 (13.3) | 0.181 | 1.81 (0.76–4.29) |
| Delta | 7 (6.1) | 3 (5) | 0.769 | 1.23 (0.31–4.94) |
| Omicron (%) | 83 (72.2) | 50 (83.3) | 0.104 | 0.52 (0.23–1.15) |
| Antiviral (%) | 37 (32.2) | 17 (28.3) | 0.602 | 1.20 (0.60–2.38) |
| mAb (%) | 46 (40) | 19 (31.7) | 0.280 | 1.44 (0.74–2.78) |
| Antiviral + mAb (%) | 78 (67.8) | 36 (60.0) | 0.303 | 1.41 (0.73–2.69) |
| Mild (%) | 104 (90.4) | 59 (98.3) | 0.050 | 0.16 (0.02–1.27) |
| Moderate-severe (%) | 12 (9.6) | 1 (1.7) | 0.050 | 6.24 (0.79–49.51) |
| Reinfections (%) | 26 (22.6) | 11 (18.3) | 0.510 | 1.30 (0.59–2.86) |
| ICU (%) | 2 (1.7) | 1 (1.6) | 0.972 | 1.04 (0.93–11.8) |
| Complication during COVID-19 | ||||
| Hospitalization (%) | 12 (9.6) | 1 (1.7) | 0.050 | 6.24 (0.79–49.51) |
| PTE (%) | 1 (0.9) | 0 | 1.000 | 1.59 (0.64–39.5) |
| Bacterial superinfection (%) | 6 (5.2) | 1 (1.7) | 0.255 | 3.25 (0.38–27.6) |
Statistically significant results in bold
Comparison of Long COVID Cohort Versus Non-long COVID Cohort
In our study, we found significant associations of LC with female sex (OR 2.06, 95% CI 1.09–3.89; p = 0.024), clinical complicated phenotype (OR 2.37, 95% CI 1.22–4.60; p = 0.010), and clinical history of autoimmune cytopenia (OR 3.94, 95% CI 1.55–10.00; p = 0.002). Data are shown in Table 1. Obesity (BMI ≥ 30.0) was significantly more represented in the LC cohort, but with a wide OR and 95% CI (OR 7.34, 95% CI 0.93–57.5; p = 0.028). On the other hand, hospitalization tends to be related to the development of LC (OR 6.24, 95% CI 0.79–49.5; p = 0.050), whereas mild disease seems to be a protective factor (OR 0.16, 95% CI 0.02–1.27; p = 0.050), albeit none of the associations reached statistical significance. Complete data are presented in Table 2.
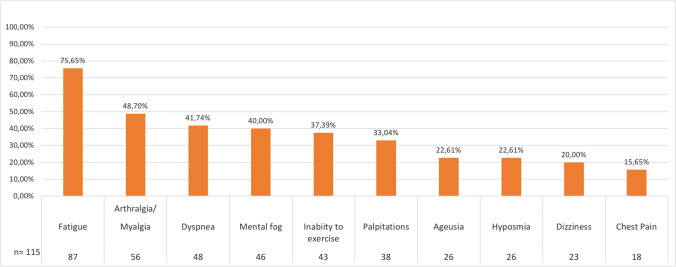
The most frequent symptoms reported in the LC survey were fatigue in 87 patients (75.7%), arthralgia/myalgia in 56 patients (48.7%), and dyspnea in 48 patients (41.7%). Of note, 89 patients (77.39%) had at least three symptoms and 66 patients (57.4%) had more than three symptoms of LC. Interestingly, the LC symptoms lasted more than 6 months in 69 patients (60%) and 59 patients (51.3%) declared persistence of symptoms at the moment of the present survey. Symptoms of LC in our cohort are summarized in Fig. 1. We then explored the possible correlation of single LC symptoms and LC duration with CVID-related features and SARS-CoV-2 course of infection. We found significant results regarding fatigue, dyspnea, and symptoms lasting more than 6 months. Complete data are resumed in Supplementary Table S1. Fatigue was significantly related to complicated phenotype (OR 2.35, 95% CI 1.10–5.02; p = 0.027), autoimmune cytopenia (OR 2.74, 95% CI 1.31–5.74; p = 0.007), and ITP (OR 2.70, 95% CI 1.26–5.79; p = 0.009). Interestingly, vaccination with four doses had a protective effect on the development of fatigue (OR 0.39, 95% CI 0.17–0.92; p = 0.028). Not surprisingly, dyspnea correlated with chronic lung disease (OR 2.39, 95% CI 1.21–4.71; p = 0.011), GLILD (OR 3.92, 95% CI 1.61–9.51; p = 0.002), and bronchiectasis (OR 2.34, 95% CI 1.18–4.63; p = 0.013). Moreover, the presence of dyspnea correlated with female sex (OR 2.41, 95% CI 1.17–4.98; p = 0.016), complicated phenotype (OR 2.60, 95% CI 1.31–5.14; p = 0.005), and a moderate-severe infection course (OR 6.15, 95% CI 1.76–21.51; p = 0.004). Prolonged symptoms, lasting more than 6 months, were related to female sex (OR 2.45, 95% CI 1.29–4.67; p = 0.006) and moderate-severe course of infection (OR 5.02, 95% CI 1.31–19.25; p = 0.019). We then repeated the analysis considering only the Omicron wave. Results are summarized in Supplementary Table S2. Of note, neither vaccination status nor SARS-CoV-2-specific treatments impacted on the LC development in the Omicron period. On the other hand, autoimmune cytopenia persisted to significantly correlate to LC development (OR 4.15, 95% CI 1.34–12.87; p = 0.014). Univariate analysis for LC adjusted for sex and age was performed in order to better define significant data. Significant variable were female sex (OR 2.00, 95% CI 1.05–3.80; p = 0.034), obesity (OR 8.83, 95% CI 1.02–70.80; p = 0.040), BMI underweight (OR 0.17, 95% CI 0.05–0.56; p = 0.003), and complicated phenotype (OR 2.28, 95% CI 1.17–4.46; p = 0.016), autoimmune cytopenia (OR 3.67, 95% CI 1.32–10.16; p = 0.012), and in particular ITP (OR 3.28, 95% CI 1.27–8.44; p = 0.014). Infection during the Omicron period was instead associated with a lower risk of LC development (OR 0.40, 95% CI 0.17–0.92; p = 0.032). Interestingly, in a multivariate analysis considering sex, age, complicated phenotype, hospitalization, chronic lung disease, days of duration of the SARS-CoV-2 infection, obesity (BMI ≥ 30.0), and Omicron period, only complicated phenotype (OR 2.44, 95% CI 1.88–5.03; p = 0.015), obesity (OR 11.17, 95% CI 1.37–90.95; p = 0.024), and female sex (OR 2.46, 95% CI 1.20–5.07; p = 0.014) significantly correlated with the development of LC. For completed data, see Table 3.
Fig. 1.
Long COVID symptoms with number and percentage of patients considering the LC-CVID cohort in our population (n = 115)
Table 3.
Multivariate analysis: CVID variables/SARS-CoV-2 infection features and LC
| Survey responders (n = 175) | p | OR (95% CI) |
|---|---|---|
| Sex (F) | 0.014 | 2.46 (1.96–5.07) |
| Complicated phenotype | 0.015 | 2.45 (1.20–5.03) |
| Obesity (BMI > 30.0) | 0.024 | 11.17 (1.37–9.95) |
| Age | 0.418 | 1.01 (0.98–1.04) |
| Hospitalized | 0.211 | 4.10 (0.45–36.71) |
| Omicron | 0.191 | 0.53 (0.21–1.37) |
| Median days of infection | 0.930 | 0.99 (0.96–1.03) |
| Chronic lung disease | 0.715 | 1.41 (0.56–2.31) |
Statistically significant results in bold
Discussion
In our CVID cohort, we found a high prevalence of LC, particularly in those patients with a complicated phenotype. LC is emerging as a frequent complication of SARS-CoV-2 infection; however, research on the topic is still limited. LC has an important impact on HRQoL of patients who survived the acute phase of the infection. Multiple chronic diseases, such as arterial hypertension, diabetes, obesity, COPD, and asthma, lead to an increased risk of severe COVID-19 and may contribute to the development of LC during the phase of recovery [10, 13, 14]. Indeed, a severe course of SARS-CoV-2 infection with need of hospitalization has been reported to increase the risk of LC [15–17]. In patients with IEIs, there is an increased risk of severe and fatal COVID-19 disease when compared to the general population [22–24]. More specifically, CVID patients have specific risk factors that expose them to a severe and prolonged course of SARS-CoV-2 infection and a high rate of reinfection [26, 27]. Chronic lung disease, a complicated clinical phenotype, and chronic immunosuppressive treatment were found to be associated with an increased risk of COVID-19-related hospitalization and death [22, 26, 27]. The CVID cohort analyzed in the present study reflects the epidemiology of CVID cohorts described in literature, presenting a younger median age than the general population and an increased incidence of respiratory involvement, autoimmune complications, and malignancy [35]. Also, the higher number of patients infected during the Omicron wave reflects the spreading of the infection in the general population, likely related to higher transmission capacity of the strain and to the reduction in vigilance after vaccination and reduction of disease severity.
To our knowledge, this is the first multicentric retrospective observational cohort study to assess the prevalence and the specific features of LC in patients with CVID. In our CVID cohort, prevalence of LC seems to be higher than in the general population (65.7% of the cohort who responded to the survey vs 11% reported in the general adult US population or 10–20% reported by the WHO) (https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition; last access December 22, 2023) [7, 8].
Pathogenesis of LC is mostly unknown, and data about pathophysiological mechanisms are limited. Impaired vaccine response, with defective neutralizing antibody production, has been implied in the development of LC in the general population [19]. A reduced formation of neutralizing antibodies can be present in CVID patients, and we could speculate that this incomplete response may, at least in part, explain the increased prevalence of LC in our CVID patients compared to the general population, even if serological data were not available in our cohort [36].
In our CVID cohort, females were found to have an increased risk of developing LC (64.3% of the LC-cohort). This result is in line with available data in the general population [12]. Less severe acute COVID-19 disease in females has been linked to estrogen functions, downregulation of ACE-2 expression, and higher expression of type I IFN [37]. However, an altered regulation of type I IFN may lead to overactivation of the immune system, predisposing females to higher risk of LC symptoms after recovery of infection [38].
Regarding SARS-CoV-2 infection features, a severe course requiring hospitalization leads to an increased probability of prolonged symptoms and LC, especially in vulnerable individuals [16, 17]. In our cohort, hospitalization during infection tends to have an impact on LC development, even if not reaching statistical significance. In a previous study, we demonstrated that complicated phenotype is a risk factor for hospitalization in CVID patients during SARS-CoV-2 infection [26]. In the present study, LC correlates with complicated phenotype in CVID patients. Apart from obesity, different from the general population, cardiovascular comorbidities and chronic lung disease seem not to impact LC development in our CVID cohort [16]. Of note, Hajjar et al. in 2017 suggested that higher BMI is generally related to the presence of fatigue in primary antibody deficiency (PAD) patients [39]. On the other hand, in our cohort, BMI underweight was significantly more prevalent in the non-LC group. To our knowledge, data about the relation between underweight and LC are not present in literature, while nutritional deficiencies have been related to risk of hospitalization, death, and LC sequelae in patients with severe COVID-19 [40]. Underweight is a multifactorial condition that might be influenced by nutritional status and enteropathy in CVID patients. However, we did not find any difference in enteropathy between LC and non-LC subgroups, and data about nutritional status were not available. Further studies including a multidimensional evaluation of nutritional status could be useful to better characterize the relation to LC development.
Due to the younger age of CVID patients, cardiovascular events are not frequent complications in our cohort, probably explaining the absence of correlation. Moreover, in our CVID cohort, chronic lung disease did not influence LC prevalence. Conversely, the item of dyspnea in the LC survey, defined as new-onset dyspnea after SARS-CoV-2 infection, was significantly related to a pre-existing chronic lung involvement.
In the multivariate analysis, considering age, chronic lung disease, SARS-CoV-2 infection features such as severity, duration of infection, and Omicron period, only female sex, obesity, and complicated phenotype were significantly linked to LC in our CVID cohort. Although pathogenesis of LC is still mostly unclear, immunological dysfunction with persistence of chronic inflammation seems to be involved [5]. The persistence of high levels of IFN I and IFN III and proinflammatory cytokines, such as CXCL9, CXCL10, and IL-8, after COVID-19 recovery has been related to the development of LC [38]. Interestingly, a similar cytokine dysregulation has been described in CVID patients with a complicated phenotype and autoimmune cytopenia [41].
The impact of autoimmune disease on LC development is controversial. Despite the known role of COVID-19 as a trigger of chronic inflammation and immune dysregulation in predisposed individuals, the role of pre-existing immune dysregulation on LC risk is debated [42]. Inflammatory rheumatic diseases have been associated with LC development in different cohorts, suggesting that chronic inflammation of systemic immune-rheumatic diseases impact on post-acute sequelae of COVID-19 [43]. However, patients with inflammatory rheumatic diseases experience chronic symptoms such as myalgia, arthralgia, and fatigue that in part overlap with LC. For this reason, the observed difference in these patients when compared with healthy controls could in part be explained by clinical manifestations in the context of underlying rheumatic diseases [44].
Post-acute sequelae of other infectious diseases have been explored in non-CVID patients, in which chronic complications of infections often occur as persistent organ specific symptoms such as inflammatory bowel disease-like presentation after Giardia lamblia infection [4] or as chronic fatigue syndrome after EBV or Middle East respiratory syndrome (MERS) infection [45]. Symptoms of LC could in part overlap with chronic fatigue syndrome; however, post-acute sequelae of COVID-19 can be accompanied by rheumatological symptoms, dizziness, loss of smell and taste, palpitations, and due to the multisystem nature of this condition. CVID patients are predisposed to several infections with the risk of recurrence and chronic evolution. However, apart from EBV-related lymphomas, studies focusing on post-acute sequelae of infections in CVID are lacking [46, 47].
Dyspnea, fatigue, and arthralgia/myalgia were the most frequent LC reported symptoms in our CVID cohort, and 57.4% of our patients had more than three LC symptoms. Dyspnea and fatigue are known complications that worsen the quality of life of patients with chronic conditions and primary immunodeficiencies [39, 48]. Discrimination of long COVID symptoms in the context of chronic diseases and vulnerable individuals may be challenging. In our cohort, dyspnea was not surprisingly correlated with the presence of a chronic lung disease. However, the CDC survey specifically explored new-onset symptoms after COVID-19. In our cohort, we did not register lung function worsening but just an increase of the reported subjective symptom “dyspnea.” We can speculate that SARS-CoV-2 perturbed the respiratory balance, especially in fragile individuals with pre-existent pulmonary diseases. Moving to fatigue, apart from autoimmunity, in our cohort, this symptom did not correlate with female sex, obesity, and bronchiectasis; as previously reported to be strongly correlated with this specific symptom in CVID patients before the pandemic [39], this might support a more LC-related than CVID-related explanation of fatigue in our patients. Finally, despite dyspnea and fatigue could be potentially influenced by pre-existing comorbidities, arthralgia and myalgia are not CVID-specific features.
Unfortunately, a specific pre-COVID evaluation of all the symptoms possibly confounding with LC was not available in the described CVID cohort. However, data collected before the pandemic in our and in other CVID cohorts report a prevalence of tiredness, weakness, arthralgia lower than 25%, and a prevalence of fatigue around 30%, which is much less than what found in our LC cohort [39, 49]. This further supports the LC-related etiology of the symptoms reported in our study.
Due to the heterogeneity of symptoms, lack of defined pathophysiological mechanisms, and non-standardized diagnostic criteria, a specific treatment for LC is not defined. However, prompt individuation of LC risk factor in vulnerable patients could optimize follow-up and future management, also considering physical therapy, psychological support, and rehabilitation [50, 51].
We are aware that this study has some limitations. First of all, the relatively small sample size and the not standardized LC diagnosis could have an impact on the selection of the LC cohort in the study. Second, the use of patient-reported outcomes and the possible overlap of LC symptoms with CVID-related symptoms could represent a bias, as for other chronic diseases. We also did not systematically evaluate serological response to SARS-CoV-2 infection and vaccination, and cytokine profile of our CVID patients was not available. Moreover, the retrospective design of the study could also have generated a temporal bias, because of the lapse of time from the SARS-CoV-2 infection and the administration of LC survey. However, the majority of patients experienced prolonged symptoms lasting more than 6 months from the infection and often still present when answering the survey. Moreover, our CVID patients are familiar with CVID-QoL and other QoL-related questionnaires investigating symptoms such as weakness/tiredness, dyspnea, and myalgia. For this reason, when asked through the CDC tool to specifically focus on new-onset symptoms, we believe that they have been able to discriminate them from those previously present in daily life and that the LC-related patient reported outcome is reasonably trustable. To our knowledge, this is the first multicentric observational cohort study trying to assess the role of CVID features on the risk of developing LC. We administered a CDC survey to measure LC symptoms, and our CVID cohort reflects the epidemiology of infection and disease-related complications reported in literature for such a rare disease. Our findings are partly in line with those coming from the healthy population and fragile patients [15, 17].
In conclusion, we demonstrated that CVID patients present an increased prevalence of LC than the general population. In CVID, factors associated with LC are female sex and obesity, like in the healthy controls. In addition, the complicated phenotype, a specific feature of the CVID immune-dysregulated substrate, is associated with LC. An improvement in awareness on the risk of LC condition in CVID patients could optimize the management of a new and alarming complication of SARS-CoV-2 in fragile patients, even if further studies are needed to confirm the findings.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank patients and their families and Jeffrey Modell Foundation and FoRiBiCa ETS for their support. We also acknowledge ERN RITA; Rome, Treviso, Naples and Rotterdam are ERN RITA Referral Centers.
Abbreviations
- IEI
Inborn errors of immunity
- CVID
Common variable immunodeficiency
- LC
Long COVID
- PASC
Post-acute sequelae of COVID-19
- WHO
World Health Organization
- CDC
Centers for Disease Control and Prevention
- ESLD
End-stage lung disease
- GLILD
Granulomatous lymphocytic interstitial lung disease
- ITP
Immune thrombocytopenia
- AIHA
Autoimmune hemolytic anemia
- COPD
Chronic obstructive pulmonary disease
- BMI
Body mass index
- mAbs
Monoclonal antibodies
- ICU
Intensive care unit
- HRQoL
Health-related quality of life
- IgG-TL
IgG trough level
- CKD
Chronic kidney disease
Author Contribution
AV, RFG, CMD, HB, and PB analyzed the data and wrote the manuscript proof; DF, FC, CM, GC, and GGa were responsible for study design and prepared the manuscript; CMD, GGi, CP, and APeGL contributed to data collection and cared for patients and manuscript revision; GS, VASHD, and MR critically reviewed the text. All co-authors review the final version of the manuscript.
Funding
Open access funding provided by Università degli Studi di Padova within the CRUI-CARE Agreement.
Availability of Data and Material
Data is available upon reasonable request to the corresponding author.
Declarations
Ethics Approval
The study has been approved by the Ethical Committee of the Sapienza University of Rome (CE 5834, n.052/2020 and CE 4604, n.316/2016).
Consent to Participate
Informed consent was waived by the Institutional Review Board due to the observational nature of the study and anonymization before analysis.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Annalisa Villa, Cinzia Milito, Francesco Cinetto and Davide Firinu contributed equally to this work.
Change history
11/1/2024
The original version of this paper was updated due to incorrect structuring of the given and family names of Renato Finco Gambier
References
- 1.Coronavirus disease (COVID-19) situation reports [Internet]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed 22 Dec 2023.
- 2.Faghy MA, Owen R, Thomas C, Yates J, Ferraro FV, Skipper L, et al. Is long COVID the next global health crisis? J Glob Health. 2022;12:03067. 10.7189/jogh.12.03067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruiz-Pablos M, Paiva B, Montero-Mateo R, Garcia N, Zabaleta A. Epstein-Barr virus and the origin of myalgic encephalomyelitis or chronic fatigue syndrome. Front Immunol. 2021;12. 10.3389/fimmu.2021.656797. [DOI] [PMC free article] [PubMed]
- 4.Hanevik K, Wensaas K-A, Rortveit G, Eide GE, Mørch K, Langeland N. Irritable bowel syndrome and chronic fatigue 6 years after giardia infection: a controlled prospective cohort study. Clin Infect Dis Off Publ Infect Dis Soc Am. 2014;59:1394–400. 10.1093/cid/ciu629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masood M, Chodisetti S, BaHammam A. Long COVID: the long-term consequences of COVID-19 and the proposed pathophysiological mechanisms. J Nat Sci Med. 2023;6(1):3–11. 10.4103/jnsm.jnsm_133_22. [Google Scholar]
- 6.Post COVID-19 condition [Internet]. Available from: https://www.who.int/teams/health-care-readiness/post-covid-19-condition. Accessed 22 Dec 2023.
- 7.Post COVID-19 condition (long COVID) [Internet]. Available from: https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition. Accessed 22 Dec 2023
- 8.Ford ND. Long COVID and significant activity limitation among adults, by age — United States, June 1–13, 2022, to June 7–19, 2023. MMWR Morb Mortal Wkly Rep [Internet]. 2023;72. Available from: https://www.cdc.gov/mmwr/volumes/72/wr/mm7232a3.htm. Accessed 22 Dec 2023 [DOI] [PMC free article] [PubMed]
- 9.Alghamdi HY, Alrashed AM, Jawhari AM, Abdel-Moneim AS. Neuropsychiatric symptoms in post-COVID-19 long haulers. Acta Neuropsychiatr. 2022;34:318–29. 10.1017/neu.2022.13. [DOI] [PubMed] [Google Scholar]
- 10.Subramanian A, Nirantharakumar K, Hughes S, Myles P, Williams T, Gokhale KM, et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med. 2022;28:1706–14. 10.1038/s41591-022-01909-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malik P, Patel K, Pinto C, Jaiswal R, Tirupathi R, Pillai S, et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-a systematic review and meta-analysis. J Med Virol. 2022;94:253–62. 10.1002/jmv.27309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review. J Infect Dis. 2022;226:1593–607. 10.1093/infdis/jiac136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luo J, Zhang J, Tang HT, Wong HK, Lyu A, Cheung CH, et al. Prevalence and risk factors of long COVID 6–12 months after infection with the Omicron variant among nonhospitalized patients in Hong Kong. J Med Virol. 2023;95: e28862. 10.1002/jmv.28862. [DOI] [PubMed] [Google Scholar]
- 14.Jassat W, Mudara C, Vika C, Welch R, Arendse T, Dryden M, et al. A cohort study of post-COVID-19 condition across the Beta, Delta, and Omicron waves in South Africa: 6-month follow-up of hospitalized and nonhospitalized participants. Int J Infect Dis. 2023;128:102–11. 10.1016/j.ijid.2022.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Daugherty SE, Guo Y, Heath K, Dasmariñas MC, Jubilo KG, Samranvedhya J, et al. Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ. 2021;373: n1098. 10.1136/bmj.n1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fernández-de-Las-Peñas C, Pellicer-Valero OJ, Navarro-Pardo E, Palacios-Ceña D, Florencio LL, Guijarro C, et al. Symptoms experienced at the acute phase of SARS-CoV-2 infection as risk factor of long-term post-COVID symptoms: the LONG-COVID-EXP-CM multicenter study. Int J Infect Dis. 2022;116:241–4. 10.1016/j.ijid.2022.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cristillo V, Pilotto A, Cotti Piccinelli S, Bonzi G, Canale A, Gipponi S, et al. Premorbid vulnerability and disease severity impact on long-COVID cognitive impairment. Aging Clin Exp Res. 2022;34:257–60. 10.1007/s40520-021-02042-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao P, Liu J, Liu M. Effect of COVID-19 vaccines on reducing the risk of long COVID in the real world: a systematic review and meta-analysis. Int J Environ Res Public Health. 2022;19:12422. 10.3390/ijerph191912422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.García-Abellán J, Fernández M, Padilla S, García JA, Agulló V, Lozano V, et al. Immunologic phenotype of patients with long-COVID syndrome of 1-year duration. Front Immunol. 2022;13: 920627. 10.3389/fimmu.2022.920627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cervia C, Zurbuchen Y, Taeschler P, Ballouz T, Menges D, Hasler S, et al. Immunoglobulin signature predicts risk of post-acute COVID-19 syndrome. Nat Commun. 2022;13:446. 10.1038/s41467-021-27797-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seidel MG, Kindle G, Gathmann B, Quinti I, Buckland M, van Montfrans J, et al. The European Society for Immunodeficiencies (ESID) registry working definitions for the clinical diagnosis of inborn errors of immunity. J Allergy Clin Immunol Pract. 2019;7:1763–70. 10.1016/j.jaip.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Tangye SG, COVID Human Genetic Effort consortium. Impact of SARS-CoV-2 infection and COVID-19 on patients with inborn errors of immunity. J Allergy Clin Immunol. 2023;151:818–31. 10.1016/j.jaci.2022.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giardino G, Milito C, Lougaris V, Punziano A, Carrabba M, Cinetto F, et al. The impact of SARS-CoV-2 infection in patients with inborn errors of immunity: the experience of the Italian Primary Immunodeficiencies Network (IPINet). J Clin Immunol. 2022;42:935–46. 10.1007/s10875-022-01264-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shields AM, Burns SO, Savic S, Richter AG, UK PIN COVID-19 Consortium. COVID-19 in patients with primary and secondary immunodeficiency: the United Kingdom experience. J Allergy Clin Immunol. 2021;147:870-875.e1. 10.1016/j.jaci.2020.12.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bousfiha A, Moundir A, Tangye SG, Picard C, Jeddane L, Al-Herz W, et al. The 2022 update of IUIS phenotypical classification for human inborn errors of immunity. J Clin Immunol. 2022;42:1508–20. 10.1007/s10875-022-01352-z. [DOI] [PubMed] [Google Scholar]
- 26.Milito C, Firinu D, Bez P, Villa A, Punziano A, Lagnese G, et al. A beacon in the dark: COVID-19 course in CVID patients from two European countries: different approaches, similar outcomes. Front Immunol. 2023;14:1093385. 10.3389/fimmu.2023.1093385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Milito C, Lougaris V, Giardino G, Punziano A, Vultaggio A, Carrabba M, et al. Clinical outcome, incidence, and SARS-CoV-2 infection-fatality rates in Italian patients with inborn errors of immunity. J Allergy Clin Immunol Pract. 2021;9:2904-2906.e2. 10.1016/j.jaip.2021.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.ESID - European Society for Immunodeficiencies [Internet]. Available from: https://esid.org/Working-Parties/Registry-Working-Party/. Accessed 22 Dec 2023
- 29.Sanità E-IS di. EpiCentro [Internet]. Available from: https://www.epicentro.iss.it/. Accessed 22 Dec 2023
- 30.Bergna A, Lai A, Ventura CD, et al. Genomic epidemiology of the main SARS-CoV-2 variants circulating in Italy in 2020 and 2022 period. Authorea Preprints; 2023. 10.22541/au.168931270.03874429/v1.
- 31.Chapel H, Lucas M, Patel S, Lee M, Cunningham-Rundles C, Resnick E, et al. Confirmation and improvement of criteria for clinical phenotyping in common variable immunodeficiency disorders in replicate cohorts. J Allergy Clin Immunol. 2012;130:1197-1198.e9. 10.1016/j.jaci.2012.05.046. [DOI] [PubMed] [Google Scholar]
- 32.WHO Working Group on the Clinical Characterisation and Management of COVID-19 infection. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis. 2020;20(8):e192–7. 10.1016/S1473-3099(20)30483-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV, WHO Clinical Case Definition Working Group on Post-COVID-19 Condition. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022;22(4):e102–7. 10.1016/S1473-3099(21)00703-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Long COVID - household pulse survey - COVID-19 [Internet]. Available from: https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm. Accessed 22 Dec 2023
- 35.Yazdani R, Habibi S, Sharifi L, Azizi G, Abolhassani H, Olbrich P, et al. Common variable immunodeficiency: epidemiology, pathogenesis, clinical manifestations, diagnosis, classification, and management. J Investig Allergol Clin Immunol. 2020;30:14–34. 10.18176/jiaci.0388. [DOI] [PubMed] [Google Scholar]
- 36.Durkee-Shock JR, Keller MD. Immunizing the imperfect immune system: coronavirus disease 2019 vaccination in patients with inborn errors of immunity. Ann Allergy Asthma Immunol. 2022;129(5):562-571.e1. 10.1016/j.anai.2022.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang C, Ramasamy A, Verduzco-Gutierrez M, Brode WM, Melamed E. Acute and post-acute sequelae of SARS-CoV-2 infection: a review of risk factors and social determinants. Virol J. 2023;20:124. 10.1186/s12985-023-02061-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Phetsouphanh C, Darley DR, Wilson DB, Howe A, Munier CML, Patel SK, et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol. 2022;23:210–6. 10.1038/s41590-021-01113-x. [DOI] [PubMed] [Google Scholar]
- 39.Hajjar J, Guffey D, Minard CG, Orange JS. Increased incidence of fatigue in patients with primary immunodeficiency disorders: prevalence and associations within the US Immunodeficiency Network Registry. J Clin Immunol. 2017;37:153–65. 10.1007/s10875-016-0367-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu JY, Liu MY, Hung KC, Hsu WH, Tsai YW, Liu TH, et al. Nutritional deficiency anemia and post-acute sequelae in patients with severe acute respiratory syndrome coronavirus 2 infection: a six-month retrospective cohort analysis of 30 892 patients. J Med Virol. 2023;95(11): e29246. 10.1002/jmv.29246. [DOI] [PubMed] [Google Scholar]
- 41.de Lollo C, de MoraesVasconcelos D, da Silva Oliveira LM, Domingues R, de Carvalho GC, da Silva Duarte AJ, et al. Chemokine, cytokine and type I interferon production induced by Toll-like receptor activation in common variable immune deficiency. Clin Immunol Orlando Fla. 2016;169:121–7. 10.1016/j.clim.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 42.Tang K-T, Hsu B-C, Chen D-Y. Autoimmune and rheumatic manifestations associated with COVID-19 in adults: an updated systematic review. Front Immunol. 2021;12: 645013. 10.3389/fimmu.2021.645013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leon L, Perez-Sancristobal I, Madrid A, Lopez-Pedraza L, Colomer JI, Lerma S, et al. Persistent post-discharge symptoms after COVID-19 in rheumatic and musculoskeletal diseases. Rheumatol Adv Pract. 2022;6:rkac008. 10.1093/rap/rkac008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boekel L, Atiqi S, Leeuw M, Hooijberg F, Besten YR, Wartena R, et al. Post-COVID condition in patients with inflammatory rheumatic diseases: a prospective cohort study in the Netherlands. Lancet Rheumatol. 2023;5:e375–85. 10.1016/S2665-9913(23)00127-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ahn SH, Kim JL, Kim JR, Lee SH, Yim HW, Jeong H, et al. Association between chronic fatigue syndrome and suicidality among survivors of Middle East respiratory syndrome over a 2-year follow-up period. J Psychiatr Res. 2021;137:1–6. 10.1016/j.jpsychires.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rivalta B, Amodio D, Milito C, Chiriaco M, Di Cesare S, Giancotta C, et al. Case report: ebv chronic infection and lymphoproliferation in four APDS patients: the challenge of proper characterization, therapy, and follow-up. Front Pediatr. 2021;27(9): 703853. 10.3389/fped.2021.703853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Allain V, Grandin V, Meignin V, Bertinchamp R, Boutboul D, Fieschi C, Galicier L, et al. Lymphoma as an exclusion criteria for CVID diagnosis revisited. J Clin Immunol. 2023;43(1):181–91. 10.1007/s10875-022-01368-5. [DOI] [PubMed] [Google Scholar]
- 48.von Spee-Mayer C, Echternach C, Agarwal P, Gutenberger S, Soetedjo V, Goldacker S, et al. Abatacept use is associated with steroid dose reduction and improvement in fatigue and CD4-dysregulation in CVID patients with interstitial lung disease. J Allergy Clin Immunol Pract. 2021;9:760-770.e10. 10.1016/j.jaip.2020.10.028. [DOI] [PubMed] [Google Scholar]
- 49.Pulvirenti F, Cinetto F, Milito C, Bonanni L, Pesce AM, Leodori G, et al. Health-related quality of life in common variable immunodeficiency Italian patients switched to remote assistance during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8(6):1894-1899.e2. 10.1016/j.jaip.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oronsky B, Larson C, Hammond TC, Oronsky A, Kesari S, Lybeck M, et al. A review of persistent post-COVID syndrome (PPCS). Clin Rev Allergy Immunol. 2023;64:66–74. 10.1007/s12016-021-08848-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fugazzaro S, Contri A, Esseroukh O, Kaleci S, Croci S, Massari M, et al. Rehabilitation interventions for post-acute COVID-19 syndrome: a systematic review. Int J Environ Res Public Health. 2022;19:5185. 10.3390/ijerph19095185. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is available upon reasonable request to the corresponding author.