Highlights
-
•
Over 1 billion persons worldwide are impacted by neurologic disability.
-
•
Brain health initiatives and programs are a means to potentially reduce neurologic disability and cost and include a process that spans the life course.
-
•
Brain health initiatives and programs are gaining traction across the globe through action plans patterned after those of the world health organization and regional neurologic societies.
-
•
A stepwise approach of intersectoral collaboration may prove valuable for achieving global brain health.
Keywords: Brain health, Neurologic disability, Dementia, Cognitive impairment, Stroke, World health organization
Abstract
Brain health initiatives and programs are gaining traction worldwide. Some are clinically based, others research based, and some are a combination of clinical and research action plans. Achievement of global brain health is a challenging endeavor with prerequisites including but not limited to multidisciplinary and multisectoral approaches, strengthening of neurologic policies at local and regional levels, global advocacy, leadership and collaboration amongst stakeholders, development of technical and guidance documents, and strengthening and interpretation of the relevant evidence. Over 1 billion persons worldwide are impacted by neurologic disorders, and brain health initiatives are needed to curb the human suffering and cost of these disorders. We provide a brief review of select brain health initiatives and programs and offer possible steps to achieve brain health globally.
1. Introduction
Brain health initiatives are gaining traction and recognition across the globe [1]. Some such programs are clinically based and designed to evaluate, prevent, treat, and assist in the recovery of brain disorders or are veiled under an umbrella of prevention of cognitive impairment. Others are policy-based or are folded into pathways to promote overall healthy aging or may conjoin the many comprehensive facets of brain health [2], [3], [4], [5]. In addition, brain health units are designed to promote optimal brain development, cognitive health, and wellbeing and prevent and manage brain conditions across the life course [1]. To achieve the aims of global brain health, substantial multidisciplinary and multisectoral approaches are necessary. Also, there must be a strengthening of neurologic policies at local and regional levels, global advocacy, leadership, and collaboration amongst stakeholders, development of guideline and technical documents, and generation and synthesis of relevant evidence [1]. The strategies to accomplish brain health are broad and include making brain disorders a priority, providing effective, timely and responsive care and prevention; having an intersectoral program for brain health promotion and prevention; and establishing ongoing research and information exchange.
In July 2023 the importance of brain health was trumpeted to the world at “World Brain Day”; a celebration acknowledging a growing recognition of the importance of brain health [6]. The main aims of “World Brain Day” were to promote awareness and education about brain disorders that affect persons throughout the world and emphasize brain health and the disabling consequences of an unhealthy brain. A theme of “World Brain Day” was to ‘leave no one behind’ by creating policies and programs to break down barriers associated with stigma, discrimination, and lack of access to professional care and rehabilitation associated with brain disorders. The program was supported by a global cast of organizations centered around the World Federation of Neurology in partnership with regional players such as the American Academy of Neurology, African Academy of Neurology, and others [6]. Additional themes included prevention of brain disabilities, awareness that global brain health can reduce brain disorders and disability, and recognition that universal access to care is essential. Also, education may reduce disparities in brain health, and advocacy for brain health is a human right [6]. In fact, for persons with brain disorders and disability, death may occur 20 years earlier than in those without brain disabilities, and the likelihood of developing chronic conditions such as depression, diabetes mellitus, obesity and stroke is 2 times higher [6].
The “World Brain Day” promotion for brain health is but one example of brain health coming of age and gaining traction at regional and more global levels. As formal brain health programs have begun to take form and gain momentum, we now briefly review select programs and conclude with possible steps needed to successfully achieve brain health regionally and globally.
2. Search strategy
There was no formal electronic search for relevant articles. The authors utilized relevant articles available in their personal archives.
3. Types and contents of regional and global brain health initiatives
3.1. Interconnected determinants of brain health and rethinking the academic medical center model and workforce
Before we explore specific brain health initiatives and programs, it is worthwhile to consider the overarching and interconnected determinants of brain health. For example, 5 such main determinants may be thought of as influencing brain structure and function. These include healthy environments, safety and security, learning and social connections, access to quality services, and physical health [7]. As such, a main goal is to empower and meaningfully engage communities to achieve optimal brain health in these interconnected spheres of influence [8].
In addition, one needs to consider rethinking and reimagining the academic medical center model, a major driver of health and healthcare, and the workforce deployed to deliver healthcare. Traditional academic medicine has been anchored to a model of ‘bench-to-bedside’ whereby ivory tower academic health centers serve as a physical hub that houses scientific research, medical training and direct patient care [9]. In the process, the community that the academic medical center serves and community engagement activities may have largely been left behind. Research has shown shortcomings of the traditional academic medical model as exemplified during the COVID-19 pandemic, by shortcomings in non-communicable disease detection and management, and health care disparities that are not being adequately addressed in the model. This has led to a call for improvement in communication and engagement with the community, broader collaboration in such areas as social, behavioral and environmental sciences, and better integration with public health systems to reduce fragmentation of health care and improve health care delivery [9].
Simply put, there is a need for the convergence of sciences and synergistic actions whereby a diverse group of scientists and other key workers from different but related disciplines join together and break down silos to solve healthcare challenges [10]. In step with this rationale, the Institute of Medicine emphasized the importance of social, behavioral, and environmental factors on health outcomes at the population level [11,12]. Furthermore, there is now a call for going beyond the model of ‘bench-to-bedside’ to an academic medical center model of ‘bench-to-bedside-to-population-to society’ [9].
To achieve a new academic medical model, there may be a need for a “physician-public health” practitioner. Such individuals would be trained to build community and related partnerships, have a population health orientation, be rooted in the principles of health equity, and able to act as teachers and scientific interpreters to provide technical assistance (e.g., best practices, grant writing), develop new prototypes of health care delivery, and disseminate effective practice guidance [13]. Onboarding academic medical centers to a reimagined and rethought way of doing business and modifying the workforce to be more engaged in the community, promises to advance brain health and other healthcare areas as academic medicine remains a major force driving change in medicine and medical practice.
3.2. Specific brain health initiatives and programs
3.2.1. International brain health initiatives and programs
The International Brain Initiative (IBI) was established to coordinate global brain research efforts [14,15]. IBI facilitates communication, exchange of ideas and information, and identification of common goals among 7 other brain research initiatives (Australian Brain Alliance, Canadian Brain Research Strategy, China Brain Project, EU Human Brain Project, Japan Brain/MINDS Project, Korea Brain Institute, and US Brain Initiative). A major focus of IBI is to explore brain and nervous system circuitry and comprehensive brain functions.
STRiDE was a 7-country (India, Jamaica, Mexico, Brazil, Kenya, Indonesia, and South Africa) initiative designed to carry out research targeting gaps in the provision of care of progressive cognitive impairment [16,17]. Work products have included development of research and training agendas for various countries, building research capacitance, development of a toolkit for awareness of cognitive impairment, situational analysis of such care, treatment and support, and recommendations for national dementia plans.
The Davos Alzheimer's Collaborative (DAC) is organized as a global multi-stakeholder partnership to mobilize the world against Alzheimer's disease by advancing research, prevention, and patient care [18]. DAC offers a clinical trial-ready system for the development and testing of new therapies for the prevention and treatment of cognitive impairment. Health care systems ranging from those in low to high resource settings may qualify to join the collaborative. A goal is to build an international cohort of 1 million persons with Alzheimer's disease. Early accomplishments include the establishment of 12 cohorts from Africa, Asia, and South America linked together and polygenic risk scores from ∼100,000 participants with Alzheimer's disease. In addition, the DAC clinical trial platform has begun to build sites, and international health care systems are being recruited to study blood biomarkers and technology-enabled methods in clinical practice. Furthermore, DAC is attempting to provide the FINGER multidomain intervention brain health initiative to interested health care systems and a learning laboratory to share innovative practices among health systems and national health ministries. DAC is led by the World Economic Forum and the Global CEO Initiative on Alzheimer's Disease (CEOi).
The European Academy of Neurology (EAN) launched a Brain Health Strategy referred to as “one brain, one life, one approach,” and several European countries such as Norway, Poland and Germany developed national plans consistent with the EAN and WHO recommendations for brain health [7,19,20]. The WHO approach provides a single source document for understanding the optimization of brain health [7]. The main pillars of the EAN and WHO recommendations include shared components such as support for integrated, people-centered approaches to care, fostering of research in prevention, determinants, and assessments of brain health, promotion of education of the public, students and health care workers, and raising awareness of neurological disorders impacting brain health. Also, there is emphasis on brain health according to a life-course approach. The latter approach has been advocated by other key organizations such as the American Academy of Neurology [21].
Finally, the G7 countries plus the Republic of Korea provide 11 potential international policy targets for a practical framework for planning for brain health: dementia risk reduction, early diagnosis, awareness, support for caregivers, safe environments, high quality care services, research and innovation in the field, and other targets [22]. Such policy targets are important to consider as the world has entered the Decade of the Brain epoch (2021–2030) and highly populous countries such as China with large numbers of older persons, are searching for means to effectively utilize the intellectual and vocational capacitance of the older population as they shift from disease-centered care to population-based health [5].
3.2.2. National and local brain health initiatives and programs: an example from the United States
In the United States, the Centers for Disease Control and Prevention (CDC&P) and Alzheimer's Association (AA) established the 3rd in a series of Healthy Brain Initiative Road Maps for 2018–2023 to advance cognitive health in relation to public health [23]. This healthy brain initiative provides guidance in relation to how state and local public health agencies, and their partners, can promote cognitive health, address cognitive impairment for persons living in the community, and support the needs of caregivers. Specifically, the guidance provides 25 actions across 4 public health domains (education and empowerment, development of policies and mobilization of partnerships, development of a competent workforce, and programmatic monitoring and evaluation) [23]. Furthermore, the following key components are discussed: risk identification and reduction, diagnosis, education and training, caregiver issues, and evidence of impact of disease. This iteration of the Road Map adds to the 21 actions already present in the 2nd iteration for 2013–2018 [23]. Highlights of the component actions across the 4 domains are listed in Table 1.
Table 1.
Highlights of alzheimer's association and centers for disease control and prevention healthy brain initiative road map (2018–2023) [23].
| Education and Empowerment |
|---|
| *Educate the public about brain health and cognitive aging and the benefits of early detection and diagnosis |
| *Promote communication about brain health and cognitive decline risks to promote healthy outcomes and well-being across the life span |
| *Promote communication about the important role of caregivers and their well-being |
| *Promote prevention of abuse, neglect and exploitation of cognitively impaired persons |
| *Provide information and tools for patients with cognitive impairment and caregivers to allow them to respond to challenges during the course of illness |
| *Strengthen knowledge about care planning across the continuum of cognitively impairing illnesses |
| *Improve access to interventions and services for patients with cognitively impairing illnesses and caregivers |
| Policies and Partnerships |
|---|
| *Promote effective interventions and best practices for brain health |
| *Assure availability of the best possible science and training for the workforce |
| *Support education of policy markers about brain health and its many facets |
| *Support inclusion of healthcare quality measures and assessments |
| *Encourage public and private partnerships to engage in and promote services and policies in the community |
| *Promote public health plans that direct emergency preparedness and emergency response for persons with dementia and their caregivers |
| Competent Workforce |
|---|
| *Educate the workforce by provision of reliable information and application of the information to those they serve |
| *Assure that educational messaging underscores the essential role of caregivers |
| *Educate the workforce with the best information on cognitive impairment and caregiving |
| *Foster continuing education of all relevant aspects of cognitive impairment and caregiving |
| *Strengthen competencies by provision of interpersonal training about cognitive impairment |
| *Educate the workforce about treatment of co-morbidities, brain injury risks, and behavioral health needs |
| Monitoring and Evaluation |
|---|
| *Implement the Behavioral Risk Factor Surveillance System optional modules on Cognitive Decline and Caregiving |
| *Support national data collection for dementia and caregiving |
| *Use surveillance data to inform development of the public health program and caregiving |
| *Assess program impact and effectiveness through evaluation of training and caregiving support programs |
| *Evaluate gaps between workforce capacitance and demand for services |
4. Proposal for a brain health programmatic model at an academic medical center
Thus far, we have discussed the components of various brain health initiatives and programs. Some focus primarily on clinical care, others on research, and some integrate both clinical care and research. In relation to brain health global or regional reach, there is a continuum ranging from large multi-region or global collaborations to more local or regional ones. In a complementary piece in this special issue of Cerebral Circulation, Cognition and Behavior by Saks and colleagues, a description of 24 brain health initiatives and programs at international and national levels relating to vascular contributions to cognitive decline is provided.
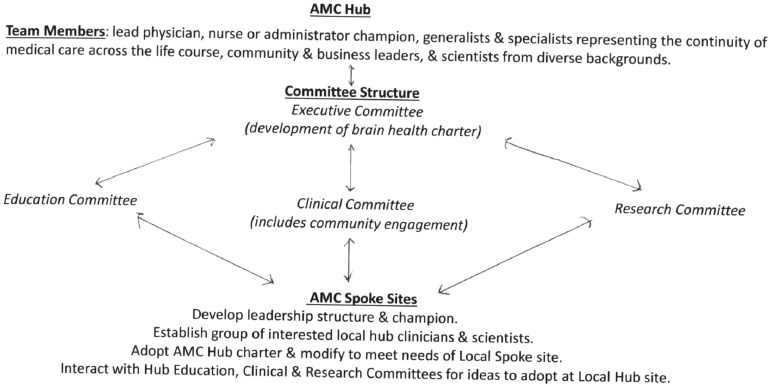
Because academic medical centers are a main driver of medicine and medical care, we provide an academic medical center brain health programmatic model for consideration. To be effective a brain health initiative or program will need to be continuous across the lifespan; seek multidisciplinary partnerships and representation; have a nucleus or hub with the capacitance to connect outlying component members; establish meaningful community engagement; in its full-blown form develop innovative research, clinical and education programs; and establish a leadership structure predicated on representation of transdisciplinary partnerships and inclusive of community representation. The aforementioned key components of an academic medical center brain health initiative or program are discussed below. Depending on the scope of a brain health initiative or program, the components may be functionally considered as a complete or partial package. Thus, depending on the scope of the initiative or program component parts may be used or modified as single units to fit the circumstances or included in the total package. Cognitive medicine, an emerging field, provides a platform as a step towards a brain health programmatic model [24]. The Fig. 1 provides a summary of the proposed components of the academic medical center model for brain health.
Fig. 1.
Academic medical center (AMC) model for brain health.
In the context of our discussion thus far, an “initiative” denotes a new action or plan to solve a problem, whereas a “program” denotes instructions that are implemented to achieve a specific result. In common application, the terms are often used interchangeably as there is overlap between the definitions.
4.1. Continuity across the life course, multidisciplinary partnerships and representation
Brain health spans the life continuum from pre-utero, fetal and childhood development through the early, middle, and later adulthood periods. Given the long reach of brain health at the academic medical center level, there is a need to bring together a broad transdisciplinary team including engagement by the academic medical center, sponsor medical school, and multiple departments or component divisions (e.g., neonatology, pediatrics, obstetrics/gynecology, adolescent medicine, primary care, internal and family medicine). Certain specialties such as neurology, psychiatry, geriatrics, ophthalmology, and otolaryngology and traditionally inpatient-based practitioners such as those in neurosurgery, intensive care, nursing, social work and rehabilitation may prove to have important roles in such an initiative or program. Furthermore, designation of champion administrative and lead physician or nurse representatives to serve as leads or co-leads of the initiative or program are needed. Establishment of partnerships amongst the diverse multidisciplinary team leaders and members is important to the success of the overall initiative or program.
4.2. Hub-Spoke structure
Academic medical centers are frequently affiliated with remote sites in a hub-spoke relationship. In such cases, for such a brain health initiative or program to be successful, a governance structure is required including but not necessarily limited to a charter to define aims, goals, objectives, leadership and committee structure, and a description of the scope of the clinical, research, and education/teaching efforts. The hub site is traditionally responsible for developing the charter and driving forward the philosophical approach and functional operating procedures in collaboration with the spoke sites whereby programs within the hub can be rolled out to the spoke sites or modified by the spoke sites to fit their needs.
4.3. Meaningful community engagement
An important component of a brain health academic medical model is how the center interacts with the community. The academic medical center must serve its community in an effective manner. Therefore, representatives from the broader community should be sought as members of the committee leadership structure and charged with providing recommendations on ways that the brain health initiative or program may better serve the broader community and its underrepresented constituents. In addition, business leaders should be sought to join the committee structure to provide further linkage to the community at large. Such a process will help to begin movement of brain health education, clinical, and research programs into the community that the academic medical center serves.
4.4. Leadership structure: executive, education, clinical and research committees
The basic leadership structure should include an executive committee with a chair, vice chair, members at large, and key committees with chairs such as those representing the following standing committee areas: education, and clinical and research activities. An education committee, for example, could include representatives from the medical school, nursing school and allied health science schools who have expertise in curriculum development, teaching, and brain health and are responsible for development of education programs at the medical school, academic medical center, and community levels. A major focus will be on education of trainees and the overall work force with an emphasis on but not limited to medical students, resident physicians, nursing students and staff, allied health students and professionals, and the community. A clinical committee composed of department members with expertise in clinical medicine and brain health (e.g., neurologists, geriatricians, primary care specialists, psychiatrists, physiatrists) will be responsible for the establishment of transdisciplinary clinical programs for the overall initiative. Finally, a research committee composed of bench and clinical researchers with an interest in brain health research will be charged with development of priorities for transdisciplinary research efforts.
The components discussed in 4.1, 4.2, 4.3, 4.4 above represent a foundation from which to build upon for an academic medical center model of a brain health initiative or program. The discussion is by no means exhaustive but rather forms a nidus of a skeleton of support from which to build on. Furthermore, as a modular system of educational, clinical, and research components, it offers the potential to modify individual components and use them separately or in total based on the individual needs and circumstances of a specific academic medical center.
5. What will it take to advance and achieve global brain health?
The establishment of global brain health is a noble cause which has appeal to community members, researchers, clinicians, and others. The idea of protecting the brain from injury serves as a stepping stone to healthier, longer life for potentially many in the community [7]. Whereas the cost-effectiveness of such initiatives or programs has not been definitively proven, as shared in this discussion and that by Saks et al. in this issue of Cerebral Circulation, Cognition, and Behavior, the movement to achieve brain health is gaining substantial momentum. National brain health strategies and dementia and dementia prevention plans have begun to promulgate across the globe. Furthermore, action plans for optimizing brain health across the life span are now available [7,23]. Although cost-effectiveness issues remain uncertain, it has been argued that savings of scale could occur by an approach that conjoins prevention of stroke, heart disease and dementia, as these conditions share similar risks [10,25].
Whereas the cause is noble, there are challenges to attaining global brain health. A reality of attempting to achieve global brain health is that communities in different regions are starting from disparate positions in relation to availability of governmental healthcare funding, services and favorable public health policies. Low-and-middle income countries, for example, may suffer from lack of access to care and preventive services in comparison to higher income countries. This potentially leaves behind some worldwide regions where the burden of neurologic disability is highest, unless the hierarchy of need changes whereby those governments focus healthcare resources in this area. Another challenge is the need to consider brain health across the entire life course. Such an approach requires more vigilance and potential cost as compared to a focused approach in one epoch in life. It is apparent that cardiovascular risks, for example, come into play as early as midlife (or even before) in relation to their potentially ravaging effects on brain structure and function and thus, are not just problems of older persons [26]. In addition, achievement of a global aim such as brain health requires participation of all countries and regions. Despite ongoing momentum and the many advances in the brain health domain, it is unclear if all countries or regions are willing to cooperate with one another. Because world economies and livelihood needs have become more and more interconnected, the interconnectedness may drive key determinants of brain health such as physical, mental, environmental and socioeconomic factors in either a positive or negative direction. As such, a lack of cooperation between countries could have a major negative impact on the world food supply and food security, and environmental or other key factors that lead to adverse brain health outcomes [27].
Forward movement of brain health initiatives and programs has not been easy. A pertinent example is the slow progress made by the WHO and national governments in relation to achieving key targets of the Global Action Plan on the public health response to cognitively impairing illnesses [28]. The Global Action Plan was designed with 7 key actions in mind (Table 2) [28,29]. To date and over a 6-year period, however, only about a quarter of the nation members have achieved the goal of establishing a National Dementia Plan (NDP) (54 new plans are needed by 2025 to reach the WHO target) [29]. In addition, it is estimated that 75 % of persons with cognitive impairment remain undiagnosed and 85 % are not receiving post-diagnostic care. In response to the disappointing results, Alzheimer's Disease International (ADI) has called for the following actions: 1. an extension of the Global Action Plan timeline; 2. for governments to accelerate efforts to establish NDPs; 3. consideration of integration of dementia plans into other policies such as those for healthy aging (e.g., brain health); 4. although comprehensive policy may not be achievable by some countries, any good faith efforts are encouraged; 5. ADI invites direct collaboration between ADI and governments to enhance the likelihood of reaching the goal; 6. health systems need to prepare for and strengthen themselves to take on the onslaught of cognitive impairment; 7. hurdles and costs for caregivers must be addressed; 8. research harmonization and data collection are needed including investment by governments; and 9. health system resilience building is needed to prepare for the next pandemic [29].
Table 2.
| 1. | Dementia is a public health priority |
| 2. | Dementia awareness and friendliness |
| 3. | Risk reduction of dementia |
| 4. | Diagnosis, treatment, care and support of patient |
| 5. | Support for caregivers of patients |
| 6. | Establishment of information systems |
| 7. | Dementia research and innovation efforts |
Key take-away messages from the ADI Global Action Plan report 2023 are that caregivers need to be supported (e.g., allowance for time off work when indicated for caregiver services), public health awareness through education for risk reduction is important, and however small the steps governments need to begin to tackle cognitive impairment to meet the challenges of families, communities, and health systems [28,29]. With the recent breakthroughs in disease-modifying therapy monoclonal antibodies for removal of beta-amyloid plaques from the brain, it has become apparent that national health systems are not well prepared to deliver the drugs to but a fraction of persons who might be eligible [30]. In addition, challenges of equitable access, greater access to necessary diagnostic testing (e.g., serial MRI brain studies, PET scans and other diagnostic tests such as biomarkers), availability of infrastructure and staff at infusion centers, and payment mechanisms for such therapies are just some of the hurdles that remain in play [30]. Furthermore, WHO has developed “best buys” which represent 4 key risks (tobacco use, harmful use of alcohol, and unhealthy diet and physical activity) as cost-effective public health interventions to prevent and control non-communicable diseases (e.g., diabetes mellitus, cardiovascular disease, cancer, chronic respiratory disease) [31]. Whereas risks for brain health are featured in the “best buys” listing, dementia or brain health have not made the non-communicable disease category list for “best buys” as of yet, potentially leaving questions of the importance of the focus of the latter neurologic issues in the minds of healthcare planners.
Achieving brain health at a global level is a formidable challenge. Although major advances have or are being made toward accomplishing the goal, we have a long way to go until we reach the point of global cooperation and support for brain health in high-, middle- and low-income countries. A disproportionate burden of neurologic disability resides in low-and middle-income countries who may be strapped for healthcare resources. Important lessons are being learned from the initial ADI Global Action Plan results and the many existent brain health initiatives as discussed in this piece and the one by Saks and colleagues in this issue of Cerebral Circulation Cognition and Behavior. We are at a point in time where an approach of seeking small victories or steps forward and honoring the adage that “perfection should not be the enemy of good” may help carry us closer to reaching the global goals of awareness, recognition, and knowledge of brain health. However, taking the next steps to more comprehensive brain health in practical terms may be more challenging as intersectoral and international cooperation will be needed.
Despite the many challenges, innovative brain health initiatives and programs are being developed and established. For example, in addition to the initiatives and programs already discussed in this piece, there is the “Brain Capital Grand Strategy” which includes 4 major components: brain capital, brain economy, brain capital index, and an investment plan [32]. The concept of brain capital originated in a global business and economic conference on addiction and mental health in 2011 [32]. Broadly, the concept takes into account the strengthening of the global economy by sustenance of productive capacity that stimulates investments in brain health research, education, prevention and care. The contention is that how a country uses its brain capital and well-being significantly impacts its economic competitiveness and prosperity [32]. Because the brain is best understood in terms of transdisciplinary thought, there needs to be a broad partnership between business and science. Furthermore, brain capital contributes to a brain economy, as new jobs demand cognitive, emotional and social skills, and such an approach places a premium on brain-based skills such as communication, networking, interpersonal skills and social perception [32]. Brain health is frequently overlooked, yet it is a central component for boosting economic resilience. Within a brain capital model is a brain capital index, a means of tracking, benchmarking and implementing the overall strategy. Finally, a brain capital investment plan supports such factors as value-based health care, government grant making, social impact investment, information technology, medical innovation, philanthropy, and other components [32].
Taken together, the brain capital model concept can be expanded to establish a grand plan by synergistically integrating 4 components: 1. Insights from human-, psychological-, social- and cognitive capital and neuroscience policy; 2. Components of a brain capital investment plan; 3. A holistic policy approach; and 4. A brain capital index [32]. Thus, a brain capital grand strategy includes integration of the pillars of brain capital, brain economy, brain capital index, and brain capital investments plan. Additional brain health initiatives aligned with a grand capital brain strategy including ones with brain capital investment plan themes are listed and briefly described in Table 3 [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42].
Table 3.
Brain health initiatives aligned with a grand capital brain strategy [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42].
| Brain Initiative: Description | |
|---|---|
| 1. | Weill Neurohub: a collaborative effort between University of California, San Francisco, Berkeley, and University of Washington to bring together neuroscientists and researchers working at the convergence of science (e.g., engineers, computer scientists, physics, chemistry, and mathematics, and industry) to speed the development of new treatments for neurological and psychiatric diseases [33]. |
| 2. | Healthy Brains Global Initiative: established with support of the World Health Organization, UNICEF, and the World Bank to create a sea change in the impact of mental health and related services; and breakthroughs and evidence-based interventions to improve health and well-being utilizing an outcomes-based model to support community-based approaches to improvement of mental health, life chances, and systems-level change [34]. |
| 3. | Behavioral Insight and Neuroscience Unit: a transdisciplinary group in Latin America that provides scientific knowledge about human behavior to design better public policies and improve people's quality of life. The unit connects evidence, social protection, and health policies with a focus on vulnerable life epochs such as childhood and older age [35]. |
| 4. | Social Impact Bonds (Pay-for-Success Financing): Social impact bonds (pay-for-success financing), are a novel means to improve social outcomes in high-risk communities. Private sector funds are used to implement proven interventions and services. Such funds are repaid by the public sector only when contractual targets for desired outcomes have been reached. Efforts may be placed on breaking down barriers related to social determinants of health (e.g., homelessness and lack of housing) or delivery of affordable high-quality training to optimize ‘brain skills’ [32,36]. |
| 5. | Brain Health Project: a research institute and member of the University of Texas at Dallas designed to deliver evidence-based scientific programs to better understand and address brain health and performance and empower persons about brain health. The initiative promotes longitudinal and interventional studies [37]. |
| 6. | Brain Health Living Labs: a model that is user-centric and operates in a clinical-academic setting to integrate up-to-date clinical care, research and innovation for brain health within a public-private-consumer partnership. The model allows for transdisciplinary approaches in a community setting [32,38]. |
| 7. | Alzheimer Drug Discovery Foundation: an organization which uses philanthropic support to accelerate the discovery of drugs to prevent, treat and cure Alzheimer's disease and related disorders and funds breakthrough research through academia and industry [39]. |
| 8. | Alzheimer's Disease Therapeutics ‘Megafund’: a public-private funding approach which creates a mega fund through sales of bonds to investors and ‘portfolio’ or multiple parallel research projects are carried out to increase the likelihood of reaching a breakthrough discovery [40]. |
| 9. | Global Brain Health Institute: founded by the University of California, San Francisco and Trinity College Dublin, the institute aims to improve brain health for populations across the world, especially those in vulnerable or underserved areas, by bringing together a mix of disciplines, professions, backgrounds, skills, perspectives, and approaches to develop new science-based solutions. A goal of the institute is to train a new generation of brain health leaders [41,42]. |
Neurological disorders are the leading causes of disability-adjusted life years lost worldwide [7,32]. Globally, there are more than 1 billion persons impacted by neurological disorders [32]. Brain disorders such as stroke, progressive cognitive impairment and others are or may be prevented. In addition, investment in the optimization of brain health promises to reduce neurological, mental and other related disorders, and thus, result in potentially lower healthcare costs, lower disability rates, promote higher productivity in society, and is associated with other benefits. As we have heard from the pundits, there is ‘no health without brain health’ and the brain is essential for allowing us to achieve a meaningful and purposeful life. Therefore, we must continue to press forward by ‘leaving no one behind’ and advocating for and practicing prevention and treatment of neurological disability [43]. We should embrace the pillars of the WHO action plan for life course brain health [7]. The main pillars are consistent with other such plan pillars [19,21,23] and include [7]: shared components such as support for integrated, people-centered approaches to care; fostering of research in prevention, determinants, and assessments of brain health; promotion of education of the public, students and health care workers; and raising awareness of neurological disorders impacting brain health. Also, emphasis is placed on the important role of and need for support of caregivers. In an action to improve brain health by building global synergies and transformations, the “neurological quadrangle” composed of 4 key pillars, surveillance, prevention, acute care and rehabilitation, is proposed as a framework to improve brain health and well-being across the life span [44].
If we do not embrace the advancement of brain health, where will it take us? The answer is on a road to more human peril, disability, loss of realization of human potential, and unfulfilled living. Stay tuned as new brain health initiatives, action plans, and platforms become available [45].
Submission declaration and verification
The article has not been published previously, is not under consideration for publication elsewhere, is approved by all authors who are responsible for the content, and will not be published elsewhere in the same form.
Declaration of generative AI in scientific publishing
The authors have not used AI and AI-assisted technologies in the writing process.
Authentication
This manuscript has not been created through the use of artificial intelligence systems.
Funding
This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Philip B. Gorelick: Conceptualization, Writing – original draft, Writing – review & editing. Atticus H. Hainsworth: Writing – review & editing. Anders Wallin: Writing – review & editing.
Declaration of competing interest
Readers are referred to the authors’ ICJME statement in relation to any potential conflicts of interest.
Acknowledgement
None.
References
- 1.Samarasekera U. Making brain health a global priority. Lancet Neurol. 2023;22:297–298. doi: 10.1016/S1474-4422(23)00085-6. [DOI] [PubMed] [Google Scholar]
- 2.Njamnshi A.K., Ngarka L., Njamnshi W.Y., et al. on behalf of the BRAIN-SCAN Congress 1.5 scientific committee and organizing secretariat. The brain research Africa initiative (BRAIN) Lancet Neurol. 2023;22:467–468. doi: 10.1016/S1474-4422(23)00164-3. [DOI] [PubMed] [Google Scholar]
- 3.Akinyemi O.R., Owolabi M.O., Okubadejo N., et al. On behalf of the African dementia consortium. Lancet Neurol. 2023;22:28–29. doi: 10.1016/S1474-4422(22)00475-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Latin America takes center stage in dementia prevention. Lancet Neurol. 2020;10:711. doi: 10.1016/S1474-4422(20)30260-X. [DOI] [PubMed] [Google Scholar]
- 5.Chen X., Giles J., Yao Y., et al. The path to healthy aging in China: a peking university-lancet commission. Lancet. 2022;400:1967–2006. doi: 10.1016/S0140-6736(22)01546-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World federation of neurology world brain day toolbox. https://drive.google.com/drive/folders/1jnbNoAmeA9Kv2SSRWNRCq_nb30xPTQok. (accessed online: June 11, 2023).
- 7.World Health Organization; Geneva: 2022. Optimizing Brain Health Across the Life Course: WHO Position Paper.https://creativecommons.org/licenses/by-nc-sa/3.0/igo/ License: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 8.Gorelick P.B. Community engagement: lessons learned from the AAASPS and SDBA. Stroke. 2022;53:654–662. doi: 10.1161/STROKEAHA.121.034554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dzau V.J., Laitner M.H., Balatbat C.A. Has traditional medicine had its day? The need to redefine academic medicine. Lancet. 2022;400:1481–1486. doi: 10.1016/S0140-6736(22)01603-8. [DOI] [PubMed] [Google Scholar]
- 10.Hachinski V., Donnan G.A., Gorelick P.B., et al. Stroke: working toward a prioritized world agenda. Stroke. 2010;41(6):1084–1099. doi: 10.1161/STROKEAHA.110.586156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Institute of Medicine . National Academies Press; Washington, DC: 2012. Primary Care and Public health: Exploring Integration to Improve Population Health. [PubMed] [Google Scholar]
- 12.Institute of Medicine . National Academies Press; Washington, DC: 2013. Toward Quality Measures For Population Health and Leading Health Indicators. [PubMed] [Google Scholar]
- 13.Bibbins-Domingo K., Fernandez A. Physician-public health practitioners—The missing academic medicine career track. JAMA Health Forum. 2022;3(3) doi: 10.1001/jamahealthforum.2022.0949. [DOI] [PubMed] [Google Scholar]
- 14.Quaglio G., Toia P., Moser E.L., et al. The International Brain Initiative: enabling collaborative science. Lancet Neurol. 2021;20:985–986. doi: 10.1016/S1474-4422(21)00389-6. [DOI] [PubMed] [Google Scholar]
- 15.Bjaalie J.G., Okabe S., Richards L.J. International brain initiative: an innovative framework for coordinated global brain research efforts. Neuron. 2020;105:212–216. doi: 10.1016/j.neuron.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Dementia care: beyond a diagnosis. Lancet Neurol. 2022;21:947. doi: 10.1016/S1474-4422(22)00402-1. [DOI] [PubMed] [Google Scholar]
- 17.STRiDE. https://www.alzint.org/what-we-do/research/stride/. (accessed online: January 28, 2024).
- 18.Davos Alzheimer's Collaborative. World Economic Forum announces major milestones in the global fight against Alzheimer's disease. https://www.davosalzheimerscollaborative.org/news. (accessed online: October 27, 2022).
- 19.Bassetti C.L.A., Endres M., Sander A., et al. The European academy of neurology brain health strategy: one brain, one life, one approach. Eur. J. Neurol. 2022;29:2559–2566. doi: 10.1111/ene.15391. [DOI] [PubMed] [Google Scholar]
- 20.Hachinski V. The new brain age. Neurology. 2022;99:468–472. doi: 10.1212/WNL.0000000000201059. [DOI] [PubMed] [Google Scholar]
- 21.Avitzur O., Rost N.S., Evans D.A. Neurologists have a plan for lifelong brain health. Neurology. 2022;99:925–926. doi: 10.1212/WNL.0000000000201339. [DOI] [PubMed] [Google Scholar]
- 22.Seong S.J., Kim B.N., Kim K.W. National dementia plans of group of seven countries and South Korea based on international recommendations. JAMA Netw. Open. 2022;5(11) doi: 10.1001/jamanetworkopen.2022.40027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alzheimer's Association and Centers for Disease Control and Prevention . Alzheimer's Association; Chicago, Illinois: 2018. Healthy Brain Initiative, State and Local Public Health Partnerships to Address Dementia: the 2018-2023 Road Map. [Google Scholar]
- 24.Wallin A., Kettunin P., Johansson P.M., et al. Cognitive medicine—A new approach in health care science. BMC Psychiatry. 2018;18:42. doi: 10.1186/s12888-018-1615-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hachinski V. The comprehensive, customized, cost-effective approach (CCCAP) to prevention of dementia. Alzheimer's Dement. 2022;18:1565–1568. doi: 10.1002/alz.12586. [DOI] [PubMed] [Google Scholar]
- 26.Mahinrad S., Sorond F., Gorelick P.B. The role of vascular risk factors in cognitive impairment and dementia and prospects for prevention. Clin. Geriatr. Med. 2022;39(1):123–134. doi: 10.1016/j.cger.2022.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Avan A., Hachinski V. The brain health learn and act group. Alzheimer's Dement. 2022;18:1396–1407. doi: 10.1002/alz.12478. [DOI] [PubMed] [Google Scholar]
- 28.Time to get serious about the global action plan on dementia. Lancet Neurol. 2023;22:643. doi: 10.1016/S1474-4422(23)00248-X. [DOI] [PubMed] [Google Scholar]
- 29.Benoist C., Weidner W., Barbarino P., et al. ADI; London: 2023. Alzheimer's Disease International (ADI): From Plan to Impact VI; pp. 4–65. pgs. [Google Scholar]
- 30.Belder C.R.S., Schott J.M., Fox N.C. Preparing for disease-modifying therapies in Alzheimer's disease. Lancet Neurol. 2023 doi: 10.1016/S1474-4422(23)00274-0. published online July 15, 2023. [DOI] [PubMed] [Google Scholar]
- 31.WHO Regional Office for the Eastern Mediterranean . WHO; Cairo, Egypt: 2018. NCD Best Buys and Other Effective Interventions. [Google Scholar]
- 32.Smith E., Diab A., Wilkerson B., et al. A brain capital grand strategy: toward economic reimagination. Mol. Psychiatry. 2021;26:3–22. doi: 10.1038/s41380-020-00918-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weill Neurohub. https://www.weillneurohub.org (accessed online: August 28, 2023).
- 34.Healthy Brains Global Initiative. https://www.hbgi.org/ (accessed online: January 28, 2024).
- 35.Fundacion INECO. Institute of neurosciences and public policies 2020. https://www.fundacionineco.org/en/institutos/institutodeneuroscienciasypoliticaspublica/ (accessed online: August 28, 2023).
- 36.Iovan S., Lantz P.M., Shapiro S. “Pay for success” projects: financing interventions that address social determinants of health in 20 countries. Am. J. Public Health. 2018;108:1473–1477. doi: 10.2105/AJPH.2018.304651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Center for BrainHealth. The BrainHealth Project. https://brainhealth.utdallas.edu/the-brainhealth-project/. Accessed: 8.28.23 2023..
- 38.Cleveland Clinic Brain Health Initiative. https://healthybrains.org (accessed online: August 28, 2023).
- 39.Alzheimer's Drug Discovery Foundation. https://www.alzdiscovery.org/about-addf. (accessed online: August 28, 2023).
- 40.Lo A.W., Ho C., Cummings J., Kosik K.S. Parallel discovery of Alzheimer's therapeutics. Sci. Transl. Med. 2014;6 doi: 10.1126/scitranslmed.3008228. 241cm245. [DOI] [PubMed] [Google Scholar]
- 41.Smith D. The next generation of leaders advocating for brain health. Lancet Neurol. 2018;17:29–30. doi: 10.1016/S1474-4422(17)30359-9. [DOI] [PubMed] [Google Scholar]
- 42.Global Brain Health Institute. https://www.gbhi.org/ (accessed online: January 28, 2024).
- 43.Grisold W., Dodick D.W., Guekht A., et al. The World federation of neurology world brain day 2023. Lancet Neurol. 2023;22:652. doi: 10.1016/S1474-4422(23)00240-5. [DOI] [PubMed] [Google Scholar]
- 44.Mayowa M.O., Leonardi M., Bassetti C., et al. Global synergistic actions to improve brain health for human development. Nat. Rev. 2023;19:371–383. doi: 10.1038/s41582-023-00808-z. (neurology) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rost N.S., Salinas J., Jordan J.T., et al. The brain health imperative in the 21st century—A call to action. Neurology. 2023;101:1–10. doi: 10.1212/WNL.0000000000207739. [DOI] [PMC free article] [PubMed] [Google Scholar]