Abstract
Objective:
To develop and implement an objective, reliable approach to surveillance for ventilator-associated events in adult patients.
Design:
The Centers for Disease Control and Prevention (CDC) convened a Ventilator-Associated Pneumonia (VAP) Surveillance Definition Working Group in September 2011. Working Group members included representatives of stakeholder societies and organizations and federal partners.
Main results:
The Working Group finalized a three-tier, adult surveillance definition algorithm for ventilator-associated events. The algorithm uses objective, readily available data elements and can identify a broad range of conditions and complications occurring in mechanically ventilated adult patients, including but not limited to VAP. The first tier definition, ventilator-associated condition (VAC), identifies patients with a period of sustained respiratory deterioration following a sustained period of stability or improvement on the ventilator, defined by changes in the daily minimum fraction of inspired oxygen or positive end-expiratory pressure. The second tier definition, infection-related ventilator-associated complication (IVAC), requires that patients with VAC also have an abnormal temperature or white blood cell count, and be started on a new antimicrobial agent. The third tier definitions, possible and probable VAP, require that patients with IVAC also have laboratory and/or microbiological evidence of respiratory infection.
Conclusions:
Ventilator-associated events surveillance was implemented in January 2013 in the CDC’s National Healthcare Safety Network. Modifications to improve surveillance may be made as additional data become available and users gain experience with the new definitions.
Keywords: ventilator-associated pneumonia, intensive care unit, epidemiology, public health, critical care, mechanical ventilation
In September 2011, the Centers for Disease Control and Prevention (CDC) convened a Ventilator-Associated Pneumonia (VAP) Surveillance Definition Working Group to organize a formal process for leaders and experts of key stakeholder organizations to discuss the challenges of VAP surveillance definitions and to propose new approaches to VAP surveillance in adult patients. The charges to the Working Group were to:
Critically review a draft, streamlined VAP surveillance definition developed for use in adult patients;
Suggest modifications to enhance the reliability and credibility of the surveillance definition within the critical care and infection prevention communities;
Propose a final adult surveillance definition algorithm, to be implemented in the CDC’s National Healthcare Safety Network (NHSN), taking into consideration the potential future use of the algorithm in public reporting, interfacility comparisons, and pay-for-reporting and pay-for-performance programs.
BACKGROUND AND RATIONALE FOR CHANGING THE APPROACH TO VAP SURVEILLANCE
For decades, the diagnosis of VAP has been a controversial topic. Definitions used in patient care, research studies, and public health disease surveillance have relied on combinations of subjective clinical signs and symptoms, radiographic evidence, and laboratory data. None of the various combinations of findings is sensitive or specific for VAP compared to a histopathological “gold standard (1–11)”. The lack of an easily applied, objective definition has had major implications for prevention and treatment research and operations. With investigators utilizing different definitions and end points, it is challenging to determine which interventions are truly effective in preventing and treating VAP. The lack of an objective and specific definition also has major repercussions for public health. As prevention and reporting of healthcare-associated infections (HAIs) are at the center of local, state, and national healthcare policy and prevention initiatives, there is an essential need for accurate, reliable outcome measurement. In particular, as facility-specific HAI rates are increasingly subject to public scrutiny through legislative public reporting mandates, as well as payment incentive programs such as the Centers for Medicare and Medicaid Services Hospital Inpatient Quality Reporting Program, it is clear that objective, reliable HAI and other healthcare-associated event measures are critical for ensuring that healthcare facilities are compared and reimbursed in a fair and equitable manner.
HISTORY OF CDC SURVEILLANCE FOR PNEUMONIA IN HEALTHCARE SETTINGS
Surveillance for nosocomial pneumonia began in the CDC’s National Nosocomial Infections Surveillance (NNIS) system in the 1970s (12). Participating in the NNIS system was a small group of medical centers that agreed to dedicate resources to HAI surveillance and prevention activities. NNIS system hospitals, whose identities were kept confidential, received training and used standardized methods to voluntarily report HAI data to the CDC. These data were used by the participating hospitals for their own internal quality improvement purposes and by the CDC to estimate the burden and national trends of HAIs. In 1999, in response to concerns that the NNIS pneumonia surveillance definitions lacked specificity, the CDC undertook a revision process that resulted in the pneumonia (PNEU) definitions. These were implemented in 2002 and continued to be used for VAP surveillance in the NNIS system’s successor surveillance system, the NHSN (13). These PNEU definitions include three different sets of criteria and rely on combinations of radiographic, clinical, and laboratory evidence, with radiographic and clinical evidence required in all cases. Patients who were on ventilators (for any amount of time) at onset of a PNEU event or within 48 hours of the event were classified as having VAP.
The PNEU definitions were initially welcomed by the healthcare epidemiology and infection prevention communities because of the perceived increase in specificity. Over the ensuing years, however, as demands on the time of infection preventionists grew, discontent with the PNEU definitions’ complexity also grew. Surveillance for VAP was generally regarded as being more time-consuming and burdensome than surveillance for other NHSN-defined HAIs. In addition, the advent of legislative mandates requiring public reporting of HAI rates in more than 26 states as of 2011, and inclusion of selected HAI measures in Centers for Medicare and Medicaid Services pay-for-reporting and pay-for-performance programs beginning in 2011, amplified concerns about the reliability of VAP surveillance using the PNEU definitions. The use of subjective definition elements (e.g., some clinical signs and symptoms) and technical definition elements (e.g., chest radiographs) meant that hospitals and even individuals within the same hospital could take very different, and not necessarily comparable, approaches to VAP surveillance (14). Through use of certain surveillance approaches (e.g., strict interpretation of clinical signs and symptoms and chest radiograph findings, requiring physician approval of cases), VAP rates could be lowered without actually making changes to improve patient care (15). Evidence began to demonstrate that patients who met the surveillance definition criteria frequently did not actually have VAP from a clinical perspective, and many patients with clinically diagnosed VAP did not meet the surveillance definition criteria (16–18). The PNEU definitions lacked clinical credibility.
Few states have enacted legislation mandating VAP public reporting (in 2012, only Pennsylvania, Oklahoma and Washington had such mandates), likely at least in part because of widespread concern regarding the complexity and credibility of the definitions. The same concern prevented the U.S. Department of Health and Human Services from including VAP in its initial Action Plan to Prevent Healthcare-Associated Infections (19). Furthermore, in 2008, the National Quality Forum (NQF), a national standards-setting organization focused on improving healthcare quality, convened a technical advisory panel to review and provide recommendations on VAP measures and their suitability for endorsement as national outcome measures for use by federal and state governments and other entities focused on large-scale improvements in HAI rates. In the NQF report, “National Voluntary Consensus Standards for the Reporting of Healthcare-Associated Infection Data,” published in March 2008, the NQF requested that the CDC “reconsider case definitions” for VAP (20).
INITIAL EFFORTS TO MODIFY VAP SURVEILLANCE IN THE NHSN
In response to concerns of the healthcare epidemiology, infection prevention, and critical care communities, and to the charge from the NQF, the CDC initiated efforts in early 2009 to revise its approach to VAP surveillance. Several guiding principles were considered in this process:
CDC healthcare-associated event surveillance definitions are not intended to be used in the clinical management of patients.
CDC healthcare-associated event surveillance definitions should be appropriate for use in every healthcare facility, regardless of the availability of specialized diagnostic testing, with minimal burden on infection prevention and other facility personnel.
This surveillance does not seek to recommend diagnostic testing or procedures by including selected criteria in its healthcare-associated event surveillance definitions. The surveillance definitions are updated periodically in an attempt to reflect changes in medical practice; they are not updated to drive changes in medical practice.
The CDC is not a regulatory agency, and does not have the authority or ability to require that facilities adhere to particular diagnostic testing standards to meet criteria in its healthcare-associated event surveillance definitions.
Input from subject matter experts initially indicated that the PNEU definitions should be revised to achieve even greater specificity, through the requirement of microbiological evidence of infection in addition to radiographic and clinical evidence. The NQF VAP Technical Advisory Panel also urged the CDC to consider “development of an outcome measure based on a definition that requires laboratory results (e.g., histopathological exams, semi-quantitative and quantitative cultures), clinical criteria, and radiology results consistent with VAP” (20, p. 16). The difficulties with introducing a requirement for microbiological evidence were four-fold: 1) ample evidence suggests that microbiological findings do not increase the accuracy of VAP diagnosis, compared to a histopathological “gold standard (2, 8, 10, 11)”; 2) lung biopsies are rarely obtained in critically ill and frequently unstable patients suspected of having VAP; 3) considerable debate and uncertainty remains regarding the optimal approach to sampling the lower respiratory tract in patients suspected of having VAP (21–25); and 4) significant variability exists in lower respiratory tract sampling practices, microbiology laboratory specimen processing, and reporting practices among intensive care units (ICUs) and healthcare facilities (26).
Similarly, although chest radiographs remain integral to the clinical diagnosis of pneumonia, including VAP, they pose specific challenges when utilized in a surveillance definition: 1) chest radiographic findings lack specificity for VAP (5, 6, 10); 2) interobserver variability in detecting pneumonia on chest radiographs is substantial (27); and 3) infection preventionists, who are the hospital personnel typically responsible for VAP surveillance, often lack the expertise to independently assess chest radiographs and reports for the presence of findings that meet the VAP definition criteria.
In 2009–2010, with the potential for public reporting, interfacility comparisons of VAP rates, and use of VAP in federal pay-for-reporting and pay-for-performance programs on the horizon, it was rapidly becoming apparent that reliability—the ability to ensure that the definition could be used in a standard way across all ICUs and healthcare facilities—was a critical consideration in making any modifications to the VAP surveillance approach. At the same time, it was unclear if any specific modifications to the VAP definitions would increase their accuracy in identifying patients with bona fide VAP. The lack of a widely accepted, objective approach to VAP diagnosis has been a fundamental challenge in efforts to improve surveillance. Other VAP definitions do exist, such as the Clinical Pulmonary Infection Score, the criteria of Johanson and colleagues, and the European VAP surveillance definitions, but they are no more reliable than the CDC PNEU definitions (28–30).
With this in mind, the CDC decided to focus its efforts on enhancing the reliability and usability of the VAP surveillance definitions, and began evaluating new definitions based on research done by Klompas and colleagues in the CDC Prevention Epicenters Program (31–33). The Epicenters work, which began as an effort to enhance the objectivity and usability of the PNEU/VAP definitions, evolved to focus more generally on potentially preventable complications of mechanical ventilation rather than VAP alone. This allows for a simpler and more objective approach to surveillance and encourages a broader view of prevention in mechanically ventilated patients. Epicenters investigators utilized a definition of “ventilator-associated complications,” based on sustained increases in the daily minimum fraction of inspired oxygen (Fio2) or positive end-expiratory pressure (PEEP) after ≥2 days of stable or decreasing daily minimum Fio2 or PEEP. In a retrospective study in which the ventilator-associated complications definition was applied to medical record data from approximately 600 patients, those who met the definition had longer durations of mechanical ventilation, length of ICU, and hospital stay, and increased mortality rates, compared to patients who did not meet the definition (32). Identification of cases using the ventilator-associated complications definition took significantly less time than using the PNEU/VAP definitions (32). Other evaluations conducted by the CDC Prevention Epicenters, the CDC, and other collaborators using similar objective definitions have supported these findings (34, 35).
VAP SURVEILLANCE DEFINITION WORKING GROUP PROCESS AND OUTCOME
The VAP Surveillance Definition Working Group was established to provide much-needed expert input and to work with CDC staff to finalize a new, more objective approach to surveillance in mechanically ventilated patients that would be suitable for use in public reporting, interfacility comparisons, and pay-for-performance programs. The leaders of the Critical Care Societies Collaborative (CCSC) reached out to member societies (the American Association of Critical-Care Nurses, the American College of Chest Physicians, the American Thoracic Society, and the Society of Critical Care Medicine) to identify representatives to participate in the Working Group. Leaders from the following organizations were also asked to identify representatives to participate: the American Association for Respiratory Care, the Association for Professionals in Infection Control and Epidemiology, the Council of State and Territorial Epidemiologists, the Healthcare Infection Control Practices Advisory Committee Surveillance Working Group, the Infectious Diseases Society of America, and the Society for Healthcare Epidemiology of America. The CDC’s federal partners, including the National Institutes of Health and the Department of Health and Human Services’ Office of Healthcare Quality (now part of the Office of Disease Prevention and Health Promotion), were also invited to participate. The list of representatives and federal participants appears in Table 1.
TABLE 1.
Ventilator-Associated Pneumonia Surveillance Definition Working Group Organizations, Representatives, and Federal Participants
| Organization | Representative(s) |
|---|---|
| American Association of Critical-Care Nurses | Suzanne Burns and Beth Hammer |
| American Association for Respiratory Care | Dean Hess |
| American College of Chest Physicians | Robert Balk and David Gutterman |
| American Thoracic Society | Nicholas Hill and Mitchell Levy |
| Association of Professionals in Infection Control and Epidemiology | Linda Greene |
| Council of State and Territorial Epidemiologists | Carole VanAntwerpen |
| Healthcare Infection Control Practices Advisory Committee Surveillance Working Group | Daniel Diekema |
| Infectious Diseases Society of America | Edward Septimus |
| Society for healthcare epidemiology of America | Michael Klompas |
| Society of Critical Care Medicine | Clifford Deutschman, Marin Kollef, and Pamela Lipsett |
| U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion | Don Wright |
| National Institutes of Health | David Henderson |
| Centers for Disease Control and Prevention, Division of Healthcare Quality Promotion | Scott Fridkin, Alice Guh, Shelley Magill, Teresa Horan, others |
The VAP Surveillance Definition Working Group kick-off meeting was held at the CDC main campus in Atlanta, Georgia, on September 19, 2011. During the meeting, members were given three examples of draft, objective definitions as a starting point for discussion. By the end of the meeting, the working group had developed a draft surveillance definition algorithm and had identified key issues for ongoing discussion. By January 2012 the Working Group had agreed on a final algorithm, identified research agenda topics, contributed to the development and submission of a new measure proposal to the NQF, and developed and implemented communication strategies for Working Group society members and other stakeholders. Working Group members also reviewed and provided feedback on the NHSN surveillance protocol, which became available for use on January 1, 2013 (http://www.cdc.gov/nhsn/acute-care-hospital/vae/index.html).
Ventilator-Associated Events Surveillance Definition Algorithm
The Working Group’s surveillance definition algorithm, which is referred to as the ventilator-associated events (VAE) surveillance definition algorithm, represents a purposeful departure from VAP toward more general, objective measures of conditions and complications occurring in patients on mechanical ventilation (Figure 1). The VAE surveillance definition algorithm uses a tiered approach, moving from measures of VAC, to IVAC, to possible and probable VAP.
Figure 1.
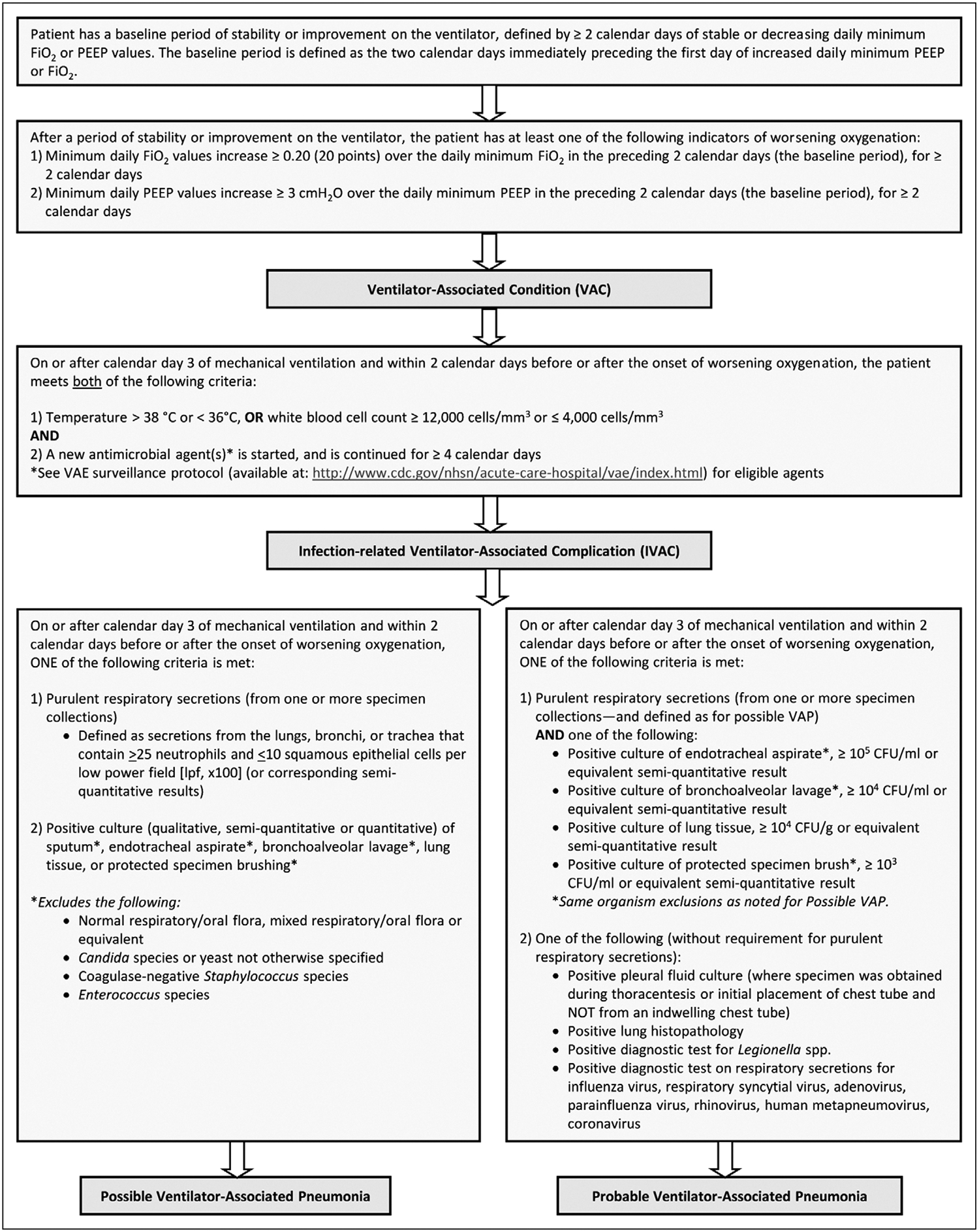
Ventilator-associated events surveillance definition algorithm*. *Available at: http://www.cdc.gov/nhsn/acute-care-hospital/vae/index.html. CFU = colony-forming units, Fio2 = fraction of inspired oxygen, PEEP = positive end-expiratory pressure, VAP = ventilator-associated pneumonia
The first tier of VAE surveillance, VAC, seeks to identify episodes of sustained respiratory deterioration, and will capture both infectious and non-infectious conditions and complications occurring in mechanically ventilated patients. VAC is defined by a sustained period of worsening oxygenation that immediately follows a baseline period of stability or improvement on the ventilator. To meet the VAC definition, a mechanically ventilated patient must have at least 2 calendar days of stable or decreasing daily minimum PEEP or Fio2, followed by at least 2 days of increased daily minimum PEEP or Fio2, where the increase in the daily minimum PEEP is ≥3 cm H2O greater than the daily minimum PEEP during the baseline period, or where the increase in the daily minimum Fio2 is ≥0.20 (or 20 percentage points in oxygen concentration) greater than the daily minimum Fio2 during the baseline period. For example, if a patient’s daily minimum Fio2 requirement on days 4 and 5 of mechanical ventilation is 0.40, then the patient’s daily minimum Fio2 requirement would need to be at least 0.60 on days 6 and 7 of mechanical ventilation for the VAC definition to be met. The decisions to set specific thresholds of 3 cm H20 and 0.20 (20 points) for the increases in PEEP and Fio2, respectively, and to define a sustained increase as an increase persisting for at least 2 calendar days were based on expert opinion of what criteria would likely identify clinically important events, while minimizing inadvertent inclusion of other types of events resulting in transient changes in oxygenation—such as surgery or performance of other procedures. Thresholds were also selected based upon published data indicating that increases of ≥2.5 cm H2O in PEEP or ≥0.15 (15 points) in Fio2 sustained for at least 2 days were associated with longer durations of mechanical ventilation, ICU and hospital stays, and increased mortality (32). Subsequently, additional data have been published that support the working group’s approach to VAC (35).
The second tier, IVAC, attempts to identify the subset of VACs that are potentially infection-related, as evidenced by an abnormal white blood cell count or temperature and the initiation of a new antimicrobial agent. IVAC will likely pin-point patients with pulmonary and extrapulmonary infections of sufficient severity to trigger respiratory deterioration. The Working Group recognized the low predictive value of an abnormal temperature or white blood cell count in ICU patients, and Klompas and colleagues have shown that the addition of fever or abnormal white blood cell count to the VAC definition does not substantially enhance the definition’s predictive value for death (35); nevertheless, these are objective and readily available signs that are frequently used at the bedside to assess for the presence of infection. The additional required criterion of the start of a new antimicrobial, where the new agent is continued for at least 4 days, may add specificity and clinical credibility to the IVAC definition, although data are needed to clarify this.
The third tier, possible and probable VAP, attempts to zero in on the subset of IVAC patients with respiratory infections as manifested by objective evidence of purulent respiratory secretions (where purulence is defined using quantitative or semiquantitative criteria for the number of neutrophils on Gram stain) and/or positive results of microbiological tests performed on respiratory tract specimens. The possible VAP definition is met by the presence of purulent secretions or a positive lower respiratory tract culture (showing any growth); the probable VAP definition requires purulent secretions in addition to a positive lower respiratory tract culture meeting certain quantitative or semi-quantitative thresholds of pathogen growth. Organisms that are not commonly regarded as true VAP pathogens are excluded from possible and probable VAP culture criteria (with the exception of lung tissue cultures): Candida spp., coagulase-negative staphylococci, and Enterococcus spp. The probable VAP definition can also be met with the presence of a positive pleural fluid culture, lung tissue with histopathologic evidence of infection, or positive diagnostics tests for Legionella or selected respiratory tract viruses, without the concomitant requirement for purulent secretions. Although data have shown that requiring purulent secretions or positive cultures in patients who have met a VAC definition actually diminishes the association between mortality and VAC (35), the Working Group felt that it was important to provide definitions within the VAE algorithm that more closely resemble VAP diagnostic criteria used at the bedside.
This tiered approach is believed to be the most appropriate approach in the current environment. It acknowledges the limitations in the ability to accurately identify VAP for surveillance purposes—simply labeling an event “VAP” does not make it so—and focuses instead on a more general measure of complications of mechanical ventilation. The approach may also reduce the likelihood of definition gaming or manipulation that could artificially lower event rates.
Two features of the VAE surveillance definition algorithm are of particular note. First, radiographic evidence of pneumonia is not included as a criterion in any tier of the algorithm, for the reasons outlined previously: lack of specificity, and the subjectivity inherent in facilities’ and individual providers’ practices in ordering, performing, interpreting, and reporting the results of chest radiographs. Second, only VAC and IVAC (and therefore the overall VAE rate—the rate of all events meeting at least the VAC definition—and the rate of all events meeting at least the IVAC definition) are intended to be possible candidates for future use in public reporting, interfacility comparisons, and pay-for-performance programs. The VAC and IVAC definitions use criteria based on data anticipated to be available from most mechanically ventilated patients and less subject to manipulation or gaming. By contrast, the third tier, possible and probable VAP, was developed to be used only in internal quality improvement. These VAP definitions include criteria based on documentation of purulent secretions and/or microbiological findings and are more in keeping with traditional clinical constructs of VAP. Because of the substantial variability in the ordering and collection of lower respiratory tract specimens, and in laboratory processing of specimens and reporting of results, the Working Group determined that it was not appropriate to include these data elements in the VAC and IVAC definitions.
An iterative process for refining the definitions must be ensured as experience using the definition algorithm accumulates in the coming years. Although there was clearly a need to establish a new surveillance approach in the NHSN, there is also an urgent need to advance the science of surveillance for VAP and other VAE. The VAE surveillance definition algorithm should be studied, validated, and improved in an ongoing manner. Evaluation and refinement of the definitions should be conducted in collaboration with members of the Working Group and other members of stakeholder communities and organizations. The Working Group is already discussing potential modifications based on user feedback received during the first 3 months of VAE surveillance.
CHALLENGES IN IMPLEMENTATION
Significant challenges remain. Because of the marked differences between the VAE and PNEU definitions, it is not possible for facilities to compare historical rates of VAP detected using the PNEU definitions with rates of VAP detected using the VAE Possible and Probable VAP definitions. The concept of VAE requires a shift in the approach to national surveillance and prevention in mechanically ventilated patients, and there are many unanswered questions. The ultimate goal of public health officials, medical investigators, and healthcare facility staff and providers is to improve the outcomes of patients who require mechanical ventilation—and the most important of these unanswered questions is whether events detected by the VAE surveillance definitions can be prevented using well-established, standard-of-care practices. A CDC Prevention Epicenters multicenter study to assess whether VAEs can be prevented by increasing the frequency of paired daily spontaneous awakening and breathing trials is underway, and more work evaluating the preventability of VAE will certainly be needed. The VAE definitions will detect a wide variety of conditions and complications in patients on mechanical ventilation; research has shown that most events detected by an objective VAC definition are VAP, acute respiratory distress syndrome, pulmonary edema, or atelectasis (32). Additional work is needed to determine the clinical correlates of other events in the VAE surveillance algorithm: IVAC and possible and probable VAP. Because of the broad range of conditions detected by the VAE definitions, and particularly the VAC definition, it is perhaps reasonable to anticipate that interventions designed to get patients off ventilators and breathing on their own earlier may reduce VAE rates. However, it is unclear whether the VAE algorithm will be useful in further evaluating the impact of interventions more specifically targeted to VAP prevention, such as regular oral care or continuous aspiration of subglottic secretions.
Another major limitation is the lack of a new approach to VAP surveillance in infants and children. The current VAE surveillance definition algorithm was developed for adult mechanically ventilated patients. Another working group, convened by the CDC in 2012 and composed of leaders and experts in pediatric and neonatal critical care, infectious diseases, infection prevention, and healthcare epidemiology, is considering whether VAE can be modified for use in younger patients.
Educating critical care providers and the healthcare epidemiology and infection prevention communities about the rationale for this new approach is essential. Helping healthcare facility personnel understand the VAE definitions and criteria and determine how to best organize their patient data to maximize the efficiency of surveillance is also important. Optimizing the operations of VAE surveillance in the ICU will require close working relationships among unit staff, particularly respiratory therapists and infection prevention personnel. Infection preventionists may not be familiar with ventilator-related data elements, such as Fio2 and PEEP, and so may benefit from the assistance of respiratory therapists and/or other ICU personnel in organizing data elements at the bedside or in the medical record. Other elements of the definitions (e.g., minimum and maximum daily temperatures, white blood cell counts, culture results) can be added to the ventilator data by appropriate personnel to allow for easier event identification. Additional guidance and tools to aid in implementing VAE surveillance, including worksheets and a web-based VAE calculator, are available on the NHSN website (http://www.cdc.gov/nhsn/acute-care-hospital/vae/index.html).
While most facilities may initiate manual VAE surveillance, the future aim is for this to be done electronically, in an automated fashion; getting to this point requires working closely with the medical information technology community and electronic health record vendors. Healthcare epidemiology, infection prevention, and critical care personnel in facilities with more advanced technologic capabilities and resources are encouraged to engage their information technology colleagues to innovate in this area and share their experiences with other healthcare facilities and the CDC.
Summary
Researchers estimate that hundreds of thousands of people require life-saving mechanical ventilation each year in the United States (36, 37). Due to complex critical illness, the frequent presence of multiple and significant comorbid conditions, and the invasive nature of mechanical ventilation, complications in these patients are common–but some are potentially avoidable. The VAP Surveillance Definition Working Group’s new approach to surveillance in mechanically ventilated adults acknowledges the current limitations in VAP diagnosis and the potential benefit in focusing surveillance on an objective, reliable, but more general measure of significant conditions and complications that result in sustained periods of worsening oxygenation. The Working Group’s consensus tiered approach was implemented by the CDC’s NHSN in January 2013. While much work remains, we believe this innovative approach to surveillance has significant potential to increase the validity of comparisons among healthcare facilities and, more importantly, to improve measurement and patient safety in the ICU.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, the American Association for Respiratory Care, the Association of Professionals in Infection Control and Epidemiology, the Council of State and Territorial Epidemiologists, or the Infectious Diseases Society of America.
The work described herein was supported by the Centers for Disease Control and Prevention (CDC).
Dr. Klompas received grant support from the Centers for Disease Control (CDC), U.S. Food and Drug Administration, and the Office of the National Co-ordinator for Health IT. Dr. Balk received grant support from the CDC and bioMérieux for participation in the EPIC CAP study (CDC) and the Procalcitonin in ICU antibiotic stewardship study (CDC and bioMérieux). Dr. Deutschman received grant support from the National Institute of General Medical Sciences. Dr. Diekema received grant support from Merck, Cerexa, bioMériuex, PurThread Technologies, and Pfizer.
Dr. Klompas received support for travel from the CDC, Society of Healthcare Epidemiologists of America, Association of Professionals in Infection Control, and the Duke University Infection Control Outreach Network. Dr. Balk received support for travel from the CDC and Critical Care Societies Collaborative. Dr. Burns received support for travel from the American Association of Critical-Care Nurses (AACN; meeting unrelated to this study). Drs. Deutschman and Lipsett received support for travel from the Society of Critical Care Medicine. Ms. Greene received support for travel from the Department of Health and Human Services/CDC.
Ms. Greene consults for INC. Dr. Hess consulted for Philips Respironics, ResMed, Pari, and Breathe. Ms. Greene lectured for Premier, Advanced Sterilization Products, and APIC. Dr. Burns lectured for AACN (annual national conference). Ms. Greene presented speeches for Covidien and Maquet. Dr. Septimus received an honorarium for a lecture. Dr. Klompas received support from the Society of Healthcare Epidemiologists of America for the development of educational presentations.
Ms. Greene is employed by the Rochester General Hospital. Dr. Lipsett has board membership with the Society of Critical Care Medicine. Dr. Deutschman received a stipend for his Presidency with the Society of Critical Care Medicine.
Dr. Deutschman received royalties from Elsevier for the textbook, Evidence-based Practice of Critical Care Medicine. Dr. Burns receives royalties from McGraw-Hill for books endorsed by AACN. Ms. Greene receives royalties from Up-To-Date, Jones and Bartlett, and McGraw-Hill.
Footnotes
The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Andrews CP, Coalson JJ, Smith JD, Johanson WG. Diagnosis of nosocomial bacterial pneumonia in acute, diffuse lung injury. Chest 1981;80:254–258. [DOI] [PubMed] [Google Scholar]
- 2.Kirtland SH, Corley DE, Winterbauer RH, et al. The diagnosis of ventilator-associated pneumonia: a comparison of histologic, microbiologic, and clinical criteria. Chest 1997;112:445–447. [DOI] [PubMed] [Google Scholar]
- 3.Klompas M. Does this patient have ventilator-associated pneumonia? JAMA 2007;297:1583–1593. [DOI] [PubMed] [Google Scholar]
- 4.Papazian L, Thomas P, Garbe L, et al. Bronchoscopic or blind sampling techniques for the diagnosis of ventilator-associated pneumonia. Am J Respir Crit Care Med 1995;152:1982–1991. [DOI] [PubMed] [Google Scholar]
- 5.Wunderink RG, Woldenberg LS, Zeiss J, et al. The radiologic diagnosis of autopsy-proven ventilator-associated pneumonia. Chest 1992;101:458–463. [DOI] [PubMed] [Google Scholar]
- 6.Fabregas N, Ewig S, Torres A, et al. Clinical diagnosis of ventilator associated pneumonia revisited: comparative validation using immediate post-mortem lung biopsies. Thorax 1999;54:867–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koenig SM, Truwit JD. Ventilator-associated pneumonia: diagnosis, treatment, and prevention. Clin Microbiol Rev 2006;19:637–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marquette CH, Copin M-C, Wallet F, et al. Diagnostic tests for pneumonia in ventilated patients: prospective evaluation of diagnostic accuracy using histology as a diagnostic gold standard. Am J Respir Crit Care Med 1995;151:1878–1888. [DOI] [PubMed] [Google Scholar]
- 9.Tejerina E, Esteban A, Fernandez-Segoviano P, et al. Accuracy of clinical definitions of ventilator-associated pneumonia: comparison with autopsy findings. J Crit Care 2010;25:62–68. [DOI] [PubMed] [Google Scholar]
- 10.Torres A, El-Ebiary M, Padro L, et al. Validation of different techniques for the diagnosis of ventilator-associated pneumonia: comparison with immediate postmortem pulmonary biopsy. Am J Respir Crit Care Med 1994;149:324–331. [DOI] [PubMed] [Google Scholar]
- 11.Torres A, Fabregas N, Ewig S, et al. Sampling methods for ventilator-associated pneumonia: validation using different histologic and microbiologic references. Crit Care Med 2000;28:2799–2804. [DOI] [PubMed] [Google Scholar]
- 12.Garner JS, Jarvis WR, Emori TG, et al. CDC definitions for nosocomial infections, 1988. Am J Infect Control 1988;16:128–140. [DOI] [PubMed] [Google Scholar]
- 13.Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 2008;36:309–332. [DOI] [PubMed] [Google Scholar]
- 14.Klompas M. Interobserver variability in ventilator-associated pneumonia surveillance. Am J Infect Control 2010;38:237–239. [DOI] [PubMed] [Google Scholar]
- 15.Klompas M. Eight initiatives that misleadingly lower ventilator-associated pneumonia rates. Am J Infect Control 2012;40:408–410. [DOI] [PubMed] [Google Scholar]
- 16.Skrupky LP, McConnell K, Dallas J, Kollef MH. A comparison of ventilator-associated pneumonia rates as identified according to the National Healthcare Safety Network and American College of Chest Physicians criteria. Crit Care Med 2012;40:281–284. [DOI] [PubMed] [Google Scholar]
- 17.Thomas BW, Maxwell RA, Dart BW, et al. Errors in administrative-reported ventilator-associated pneumonia rates: are never events really so? Am Surg 2011;77:998–1002. [PubMed] [Google Scholar]
- 18.Klompas M. Is a ventilator-associated pneumonia rate of zero really possible? Curr Opin Infect Dis 2012;25:176–182. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. National targets and metrics. Monitoring progress toward action plan goals: a midterm assessment. Available at: http://www.hhs.gov/ash/initiatives/hai/nationaltargets/index.html#table1. Accessed June 19, 2012
- 20.National Quality Forum. National voluntary consensus standards for the reporting of healthcare-associated infection data. Published March 2008. Available at: http://www.qualityforum.org/Publications/2008/03/National_Voluntary_Consensus_Standards_for_the_Reporting_of_Healthcare-Associated_Infection_Data.aspx. Accessed June 19, 2012.
- 21.Ruiz M, Torres A, Ewig S, et al. Noninvasive versus invasive microbial investigation in ventilator-associated pneumonia. Am J Respir Crit Care Med 2000;162:119–125. [DOI] [PubMed] [Google Scholar]
- 22.Fagon J-Y, Chastre J, Wolff M, et al. Invasive and non-invasive strategies for management of suspected ventilator-associated pneumonia. Ann Intern Med 2000;132:621–630. [DOI] [PubMed] [Google Scholar]
- 23.Canadian Critical Care Trials Group. A randomized trial of diagnostic techniques for ventilator-associated pneumonia. N Engl J Med 2006;355:2619–2630. [DOI] [PubMed] [Google Scholar]
- 24.Berton DC, Kalil AC, Cavalcanti M, Teixeira PJZ. Quantitative versus qualitative cultures of respiratory secretions for clinical outcomes in patients with ventilator-associated pneumonia. Cochrane Database Syst Rev 2012;1:CD006482. [DOI] [PubMed] [Google Scholar]
- 25.Heyland DK, Cook DJ, Marshall J, et al. The clinical utility of invasive diagnostic techniques in the setting of ventilator-associated pneumonia. Chest 1999;115:1076–1084. [DOI] [PubMed] [Google Scholar]
- 26.Morris AC, Kefala K, Simpson AJ, et al. Evaluation of the effect of diagnostic methodology on the reported incidence of ventilator-associated pneumonia. Thorax 2009;64:516–522. [DOI] [PubMed] [Google Scholar]
- 27.Young M, Marrie TJ. Interobserver variability in the interpretation of chest roentgenograms of patients with possible pneumonia. Arch Intern Med 1994;154:2729–2732. [DOI] [PubMed] [Google Scholar]
- 28.Pugin J, Auckenthaler R, Mili N, et al. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and non-bronchoscopic “blind” bronchoalveolar lavage. Am Rev Respir Dis 1991;143:1121–1129. [DOI] [PubMed] [Google Scholar]
- 29.Johanson WG, Pierce AK, Sanford JP, Thomas GD. Nosocomial respiratory infections with Gram-negative bacilli: the significance of colonization of the respiratory tract. Ann Intern Med 1972;77:701–706. [DOI] [PubMed] [Google Scholar]
- 30.HELICS-ICU working group. Surveillance of Nosocomial Infections in Intensive Care Units. Protocol, version 6.1. PH/EPI reports D/2004/2505/48. Brussels: Scientific Institute of Public Health; 2004. [Google Scholar]
- 31.Klompas M, Kleinman K, Platt R. Development of an algorithm for surveillance of ventilator-associated pneumonia with electronic data and comparison of algorithm results with clinician diagnoses. Infect Control Hosp Epidemiol 2008;29:31–37. [DOI] [PubMed] [Google Scholar]
- 32.Klompas M, Khan Y, Kleinman K, et al. Multicenter evaluation of a novel surveillance paradigm for complications of mechanical ventilation. PLoS One 2011;6:e18062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klompas M, Kleinman K, Khan Y, et al. Rapid and reproducible surveillance for ventilator-associated pneumonia. Clin Infect Dis 2012;54:370–377. [DOI] [PubMed] [Google Scholar]
- 34.Ricks PM, Klompas M, Viray M, et al. Assessment of a draft streamlined ventilator-associated pneumonia definition: data collection burden, agreement with current National Healthcare Safety Network pneumonia definitions, and clinical relevance [abstract 383]. Dallas, TX: 21st Annual Scientific Conference of the Society for Healthcare Epidemiology of America, April 1–4, 2011. [Google Scholar]
- 35.Klompas M, Magill S, Robicsek A, et al. Objective definitions for ventilator-associated pneumonia. Crit Care Med 2012;40:3154–3161. [DOI] [PubMed] [Google Scholar]
- 36.Behrendt CE. Acute respiratory failure in the United States: incidence and 31-day survival. Chest 2000;118:1100–1105. [DOI] [PubMed] [Google Scholar]
- 37.Kahn JM, Goss CH, Heagerty PJ, et al. Hospital volume and the outcomes of mechanical ventilation. N Engl J Med 2006; 355:41–50. [DOI] [PubMed] [Google Scholar]


