Key Points
Question
In patients with a history of gout, are higher levels of serum urate associated with a higher incidence of subsequent gout flares?
Findings
In this retrospective population-based study of 3613 patients with gout with a mean follow-up of 8.3 years, higher urate levels at baseline were associated with higher rates of recurrent gout. Overall, 95% of gout flares occurred in people with serum urate greater than or equal to 6 mg/dL and 98% occurred in people with serum urate greater than or equal to 5 mg/dL.
Meaning
Among patients with a history of gout, these findings support using a baseline serum urate value to assess risk of subsequent gout flares.
Abstract
Importance
Approximately 12 million adults in the US have a history of gout, but whether serum urate levels can help predict recurrence is unclear.
Objective
To assess associations of a single serum urate measurement with subsequent risk of acute gout flares and subsequent risk of hospitalizations for gout among patients in the UK with a history of gout.
Design, Setting, and Participants
This retrospective study included patients with a history of gout identified from the UK between 2006 and 2010 who were followed up through Primary Care Linked Data medical record linkage until 2017 and through the Hospital Episode Statistics database until 2020.
Exposures
Serum urate levels at enrollment.
Main Outcome and Measure
Rate of recurrent acute gout, ascertained by hospitalization, outpatient, and prescription/procedure records, and adjusted rate ratios using negative binomial regressions.
Results
Among 3613 patients with gout (mean age, 60 years; 3104 [86%] men), 1773 gout flares occurred over a mean follow-up of 8.3 years. Of these, 1679 acute gout flares (95%) occurred in people with baseline serum urate greater than or equal to 6 mg/dL and 1731 (98%) occurred in people with baseline serum urate greater than or equal to 5 mg/dL. Rates of acute gout flares per 1000 person-years were 10.6 for participants with baseline urate levels less than 6 mg/dL, 40.1 for levels of 6.0 to 6.9 mg/dL, 82.0 for levels of 7.0 to 7.9 mg/dL, 101.3 for levels of 8.0 to 8.9 mg/dL, 125.3 for urate levels of 9.0 to 9.9 mg/dL, and 132.8 for levels greater than or equal to 10 mg/dL. Rate ratio of flares were 1.0, 3.37, 6.93, 8.67, 10.81, and 11.42, respectively, over 10 years (1.61 [1.54-1.68] per mg/dL). Rates of hospitalization per 1000 person-years during follow-up were 0.18 for those with baseline serum urate less than 6 mg/dL, 0.97 for serum urate of 6.0 to 6.9 mg/dL, 1.8 for serum urate of 7.0 to 7.9 mg/dL, 2.2 for serum urate of 8.0 to 8.9 mg/dL, 6.7 for serum urate of 9.0 to 9.9 mg/dL, and 9.7 for serum urate greater than or equal to 10 mg/dL. Rate ratios of hospitalization for gout, adjusting for age, sex, and race were 1.0, 4.70, 8.94, 10.37, 33.92, and 45.29, respectively (1.87 [1.57-2.23] per mg/dL).
Conclusions and Relevance
In this retrospective study of patients with a history of gout, serum urate levels at baseline were associated with the risk of subsequent gout flares and rates of hospitalization for recurrent gout. These findings support using a baseline serum urate level to assess risk of recurrent gout over nearly 10 years of follow-up.
This retrospective study of patients with gout examines whether serum urate levels are associated with subsequent risk of gout flares and hospitalization for gout.
Introduction
Gout affects more than 12 million adults in the US.1 Acute gout is typically episodic and associated with severe pain,2 reduced quality of life, and a transient increase in major cardiovascular3 and venous thrombotic events.4 Acute gout is caused by accumulation of monosodium urate crystallization in the joints,2,5,6 typically due to chronic hyperuricemia, with serum urate levels exceeding the saturation point of approximately 6.8 mg/dL for monosodium urate crystallization in the body.2,5,6 Among people without a history of gout, population-based studies reported graded associations between baseline serum urate levels above the saturation point and the risk of gout even after 10 or more years following the initial serum urate measurement.7,8,9 However, associations between serum urate levels and the risk of recurrent gout among patients with a history of gout are unclear.
In this retrospective study of patients with a history of gout treated in primary care, associations of baseline serum urate levels with subsequent episodes of acute gout and acute gout requiring hospitalization were evaluated.
Methods
Source Population
The source population was the UK Biobank, a cohort of more than 500 000 adults aged 40 to 69 years recruited between 2006 to 2010 through the UK National Health Service.10,11 Participants provided blood samples and attended a baseline visit during which information was collected on sociodemographic data, health behaviors, medical conditions, medications, and height and weight. These data were linked to hospital inpatient and death records (available for all participants) and primary care data (available for 45% of the entire UK Biobank cohort). Hospitalization linkage and vital statistics data were available through March 2020, whereas primary care data were available from the UK Biobank through September 2017. The UK Biobank obtained ethical approval from the North West–Haydock Research Ethics Committee (16/NW/0274) and all participants provided written informed consent, including for linkage to their health-related records.
Study Population
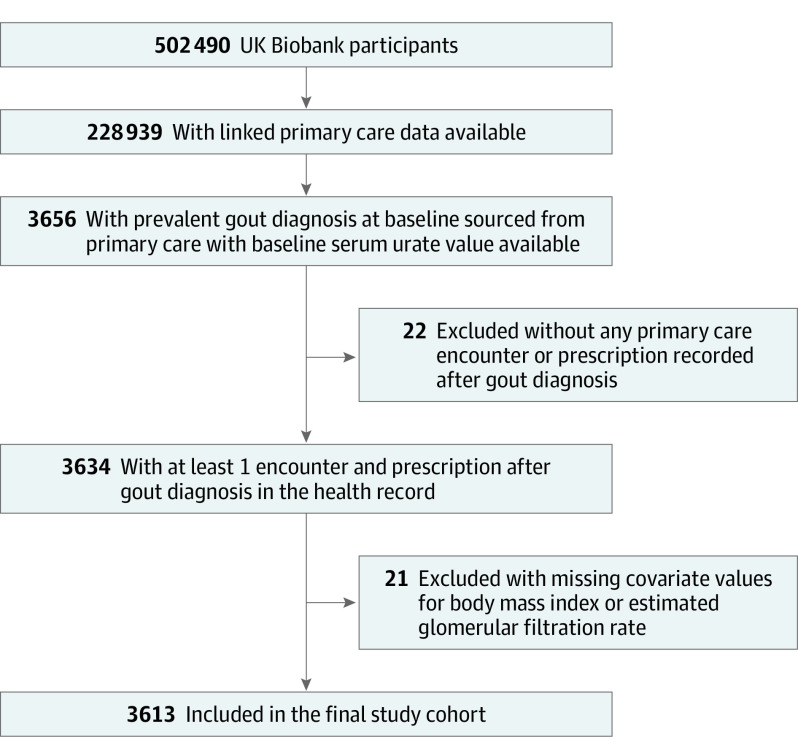
The study population consisted of all UK Biobank participants with a history of gout at baseline,12 defined as having a diagnosis of gout recorded in the primary care data before the enrollment date, and whose individual primary care clinical diagnoses and prescription data were linked to other UK Biobank data. Therefore, analyses were restricted to the 45% of UK Biobank participants who were linked to primary care data.13 Baseline characteristics of UK Biobank participants with and without primary care data linkage were similar (eTable 1 in Supplement 1). Eligible patients had at least 1 primary care encounter and prescription medication record after gout diagnosis and nonmissing serum urate data at baseline (Figure 1).
Figure 1. Cohort Development in Study of Recurrent Flares Among Patients With History of Gout.
Ascertainment of Exposure: Serum Urate Measurement
Blood samples were collected from participants as part of their baseline assessment visit and shipped to the UK Biobank central processing site for processing and storage in an automated freezer at −80 °C within 24 hours. Serum urate was measured from each participant’s baseline blood sample using an enzymatic assay on a Beckman Coulter AU5800 platform.14
Ascertainment of End Points: Recurrent Gout Flares
Based on recent studies conducted in the UK Clinical Practice Research Datalink3,4 and UK Biobank,12 recurrent flares were defined as hospitalization with gout (International Statistical Classification of Diseases, Tenth Revision [ICD-10] M10) as the primary discharge diagnosis; diagnosis of a new acute gout episode in primary care records; or diagnosis of gout in primary care records and prescription issued on the same day for corticosteroids, colchicine, or nonsteroidal anti-inflammatory drugs or a pertinent procedure (eTable 2 in Supplement 1). Hospitalizations for gout based on ICD codes have been validated, and specificity and positive predictive value were 100%.15 Gout visit and flare drug prescription/procedure had a positive predictive value of 95% for a gout flare in a prior study.16 Episodes of acute gout that occurred within 30 days of a previous flare encounter were considered part of the same episode and excluded.17
Ascertainment of Covariates
Covariates were ascertained at the UK Biobank baseline assessment and through linked medical records and included age, sex, self-reported race (fixed categories of Black, Asian, White, multiple, or other), body mass index (BMI), smoking status, alcohol intake,18 coffee intake, red meat intake, fish intake, poultry intake,19 diuretic20 and urate-lowering therapy21 use, diabetes,17 cardiovascular disease,17 hypertension,17 and chronic kidney disease17 (eMethods in Supplement 1). These factors affect serum urate levels and may be confounders of the associations studied here. Race and ethnicity were included because previous studies reported higher rates of gout in Black and Asian individuals compared with White individuals.1
Statistical Analysis
We conducted cohort analyses to examine associations between categories of baseline serum urate levels and rates of recurrent gout flares during the subsequent 1, 2, 5, and 10 years. We computed person-time of follow-up from the baseline examination to the earliest date of either death or end of the study period, whichever occurred first (September 20, 2017, when counting flares captured from the inpatient and outpatient data). Based on population studies for incident gout risk among individuals without gout at baseline,7,8,9 serum urate levels were categorized as less than 6.0 mg/dL, 6.0 to 6.9 mg/dL, 7.0 to 7.9 mg/dL, 8.0 to 8.9 mg/dL, 9.0 to 9.9 mg/dL, and greater than or equal to 10.0 mg/dL, with a level of less than 6.0 mg/dL serving as the reference group (ie, American College of Rheumatology and European Alliance of Associations for Rheumatology threshold22,23), as well as continuously (per mg/dL and per SD). In a secondary analysis, we examined serum urate categories with levels less than 5.0 mg/dL as the reference group, consistent with the British Society of Rheumatology’s target serum urate level.24 We separately examined the association between baseline urate levels and gout flares requiring hospitalizations (using gout as the primary discharge diagnosis), for which hospital inpatient data were obtained through March 5, 2020. Negative binomial regression was used to account for the recurrent flare event counts during follow-up in our primary analysis, exponentiating the coefficients to generate rate ratios (RRs) and 95% CIs overall and by subgroups defined by sex, race, age group, chronic kidney disease status, and diuretic and urate-lowering therapy use. We additionally used Poisson regression to assess recurrent flare counts, with robust variance to account for potential overdispersion.
RRs were adjusted for age, sex, and race.2,6 Additional analyses were performed that additionally adjusted for BMI; smoking status; consumption of alcohol, coffee, red meat, fish, and poultry; diuretic and urate-lowering therapy use; and presence of diabetes, cardiovascular disease, hypertension, and chronic kidney disease. We evaluated potential subgroup effects and interactions with age, sex, race, chronic kidney disease status, diuretic use, and urate-lowering therapy use by testing significance of the interaction terms (between each dichotomous covariate and continuous serum urate) added to our final models. All P values were 2-sided. All statistical analyses were conducted using R version 4.2.2 (R Foundation).
Results
A total of 3613 people from the UK Biobank database who had a history of gout and underwent a serum urate measurement between April 28, 2007, and September 29, 2010, were included (after excluding those with missing covariate values for BMI and estimated glomerular filtration rate [n = 21]) (Figure 1). Among the participants, 3104 (86%) were men and the mean age was 60 years. The mean (SD) serum urate level was 6.87 (1.63) mg/dL at baseline (Table). Male sex, higher BMI, greater alcohol consumption, smoking, greater red meat intake, diuretic use, and chronic kidney disease were associated with higher serum urate categories, whereas older age and use of urate-lowering therapy were associated with lower serum urate level categories (Table).
Table. Baseline Characteristics of the Study Population With Prevalent Gouta.
| Characteristic | Serum urate level, No. (%) | Trend P valueb | Total (N = 3613) | |||||
|---|---|---|---|---|---|---|---|---|
| <6 mg/dL (n = 1057) |
6 to 7 mg/dL (n = 781) | 7 to 8 mg/dL (n = 872) | 8 to 9 mg/dL (n = 609) | 9 to 10 mg/dL (n = 212) | ≥10 mg/dL (n = 82) | |||
| Women | 315 (29.8) | 70 (9.0) | 56 (6.4) | 40 (7.2) | 21 (7.8) | 7 (7.8) | <.001 | 509 (14.1) |
| Men | 742 (70.2) | 711 (91.0) | 816 (93.6) | 569 (93.4) | 191 (90.1) | 75 (91.5) | 3104 (85.9) | |
| Age, mean (SD), y | 60.5 (6.5) | 60.8 (6.4) | 60.4 (6.8) | 59.6 (7.2) | 58.6 (7.8) | 59.0 (7.8) | <.001 | 60.2 (6.8) |
| Race | .70 | |||||||
| Asian | 22 (2.1) | 19 (2.4) | 19 (2.2) | 14 (2.3) | 4 (1.9) | 2 (2.4) | 80 (2.2) | |
| Black | 6 (0.6) | 8 (1.0) | 7 (0.8) | 8 (1.3) | 1 (0.5) | 2 (2.4) | 32 (0.9) | |
| White | 1018 (96.3) | 745 (95.4) | 837 (96.0) | 579 (95.1) | 204 (96.2) | 78 (95.1) | 3461 (99.1) | |
| Multiplec | 4 (0.4) | 5 (0.6) | 3 (0.3) | 2 (0.3) | 1 (0.5) | 0 | 15 (0.4) | |
| Otherd | 5 (0.5) | 4 (0.5) | 3 (0.3) | 3 (0.5) | 1 (0.5) | 0 | 16 (0.4) | |
| Serum urate level, mean (SD), mg/dL | 4.9 (0.8) | 6.6 (0.3) | 7.5 (0.3) | 8.4 (0.3) | 9.4 (0.3) | 10.7 (0.7) | <.001 | 6.9 (1.6) |
| BMI, mean (SD) | 29.4 (4.9) | 29.4 (5.0) | 29.9 (4.3) | 30.5 (4.8) | 31.4 (5.7) | 32.2 (6.0) | <.001 | 30.0 (4.9) |
| Alcohol consumption | <.001 | |||||||
| Daily | 269 (25.4) | 254 (32.5) | 293 (33.6) | 222 (36.5) | 75 (35.4) | 24 (29.3) | 1137 (31.5) | |
| Never | 88 (8.3) | 57 (7.3) | 40 (4.6) | 30 (4.9) | 12 (5.7) | 6 (7.3) | 233 (6.4) | |
| Smoking status | ||||||||
| Never | 480 (45.4) | 333 (42.6) | 375 (43.0) | 243 (39.9) | 89 (42.0) | 32 (39.0) | 1552 (43.0) | |
| Former | 486 (46.0) | 371 (47.5) | 423 (48.5) | 318 (52.2) | 94 (44.3) | 39 (47.6) | .02 | 1731 (47.9) |
| Current | 88 (8.3) | 75 (9.6) | 66 (7.6) | 48 (7.9) | 24 (11.3) | 9 (8.6) | 310 (8.6) | |
| Coffee intake, cups/d | .10 | |||||||
| 0 | 247 (23.4) | 153 (19.6) | 208 (23.9) | 151 (24.8) | 63 (29.7) | 16 (19.5) | 838 (23.2) | |
| 1-2 | 433 (41.0) | 315 (40.3) | 355 (40.7) | 250 (41.1) | 78 (36.8) | 27 (32.9) | 1458 (40.4) | |
| 3-5 | 246 (23.3) | 192 (24.6) | 196 (22.5) | 130 (21.3) | 38 (17.9) | 20 (24.4) | 822 (22.8) | |
| >5 | 53 (5.0) | 53 (6.8) | 37 (4.2) | 25 (4.1) | 12 (5.7) | 6 (7.3) | 186 (5.1) | |
| Red meat intake, mean (SD), servings/wk | 3.9 (2.5) | 4.4 (2.7) | 4.2 (2.3) | 4.4 (2.6) | 4.9 (3.6) | 4.2 (2.5) | <.001 | 4.3 (2.5) |
| Poultry intake, mean (SD), servings/wk | 1.9 (1.2) | 2.0 (1.2) | 2.0 (1.3) | 2.0 (1.3) | 2.1 (1.5) | 1.7 (1.2) | .22 | 2.0 (1.2) |
| Fish intake, mean (SD), servings/wk | 2.3 (1.7) | 2.4 (1.6) | 2.4 (2.0) | 2.2 (1.9) | 2.6 (1.9) | 2.3 (1.7) | .54 | 2.3 (1.7) |
| Diuretic use at baseline | 110 (10.4) | 79 (10.1) | 100 (11.5) | 84 (13.8) | 35 (16.5) | 26 (12.0) | <.001 | 434 (12.0) |
| Urate-lowering therapy use at baseline | 455 (43.0) | 164 (21.0) | 74 (8.5) | 37 (6.1) | 11 (5.2) | 8 (9.8) | <.001 | 749 (20.7) |
| Hypertension | 340 (32.2) | 228 (29.2) | 255 (29.2) | 188 (30.9) | 68 (32.1) | 33 (40.2) | .41 | 1112 (30.8) |
| Cardiovascular disease | 140 (13.2) | 86 (11.0) | 97 (11.1) | 83 (13.6) | 37 (17.5) | 14 (17.1) | .17 | 457 (12.6) |
| Diabetes | 167 (15.8) | 110 (14.1) | 84 (9.6) | 77 (12.6) | 24 (11.3) | 18 (22.0) | .08 | 480 (13.3) |
| Chronic kidney disease stage ≥3e | 54 (5.1) | 30 (3.8) | 37 (4.2) | 50 (8.2) | 34 (16.0) | 28 (34.1) | <.001 | 233 (6.4) |
Serum urate levels were measured from blood samples taken at the baseline assessment, at the same time that data were collected on anthropometrics and self-reported dietary intake, lifestyle factors, and current medication use.
P values are for the trend across the 6 categories of serum urate level and were calculated using linear regression (for continuous variables), logistic regression (for dichotomous variables), and ordinal logistic regression (for categorical variables).
Self-selected by participants, with further response options including “White and Black Caribbean,” “White and Black African,” “White and Asian,” and “Any other mixed background.”
Self-selected by participants, with no further response options available.
Glomerular filtration rate <60 mL/min.
Over a mean follow-up of 8.3 years, 1773 new episodes of gout were treated in primary care or required hospitalizations. Of the 3613 participants, 72% had 0 acute gout episodes, 16% had 1 acute gout episode, 6% had 2 acute gout episodes, and 5% had at least 3 acute gout episodes. Overall, 1679 of 1773 acute gout episodes (95% [95% CI, 94%-96%]) occurred in those with baseline serum urate greater than or equal to 6 mg/dL and 1731 of 1773 (98% [95% CI, 97%-98%]) occurred in those with baseline serum urate greater than or equal to 5 mg/dL (Figure 2; eTable 3 in Supplement 1).
Figure 2. Rate and Rate Ratio (RR) for Recurrent Gout Flares According to Serum Urate Level and Follow-Up From Baseline.
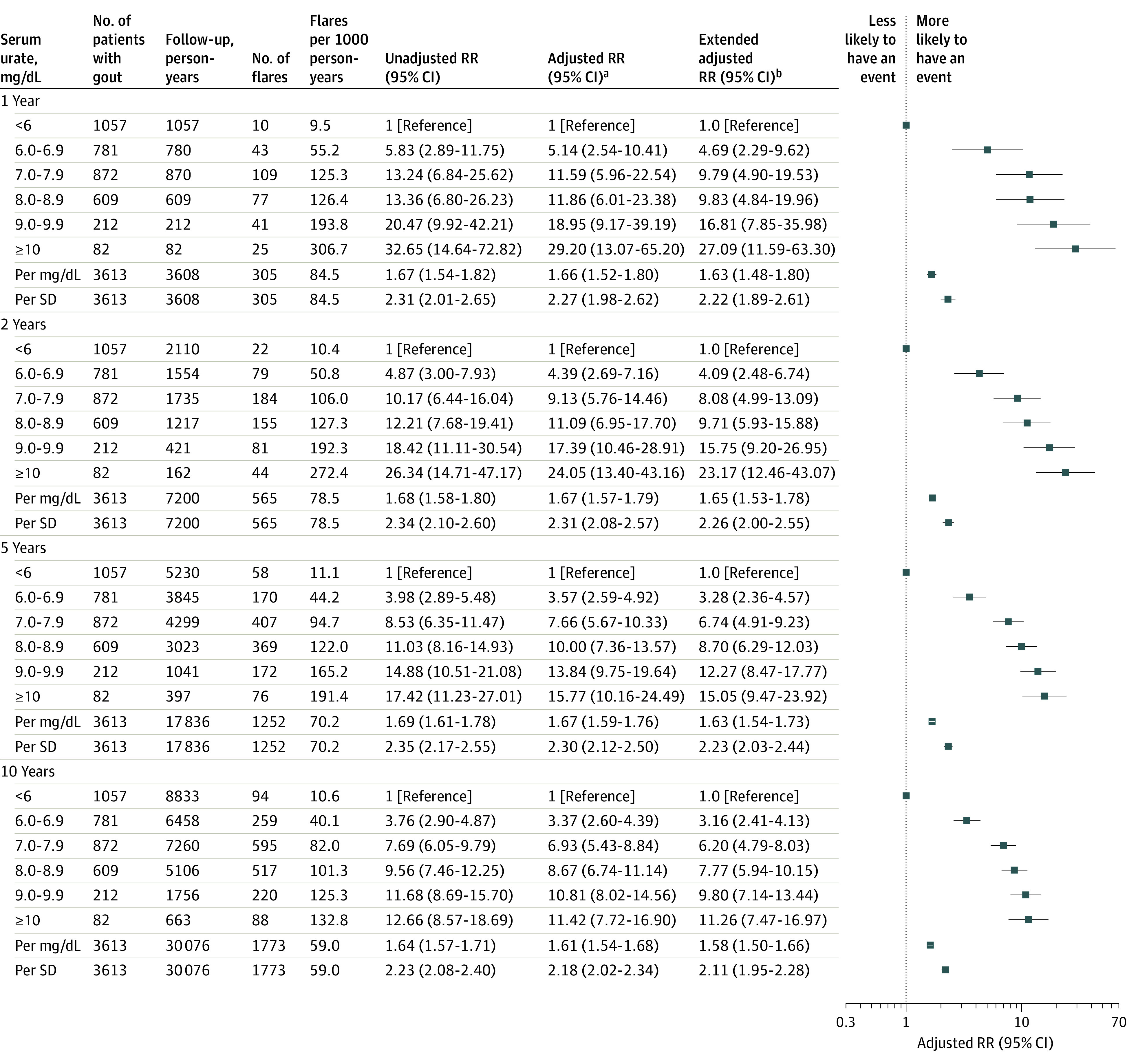
aAdjusted for age, sex, and race.
bAdjusted for variables included in the primary model (age, sex, race) plus body mass index (continuous), smoking status, alcohol intake, coffee intake, red meat, fish, and poultry intake, current use of diuretic medications and urate-lowering therapy, and prevalent diabetes, cardiovascular disease, hypertension, and chronic kidney disease.
Serum urate levels were associated with recurrent acute gout in a graded manner. Rates of acute gout flares per 1000 person-years (with RRs adjusted for age, sex, and race) were 10.6 for participants with baseline urate levels less than 6 mg/dL (adjusted RR, 1.0), 40.1 for levels of 6.0 to 6.9 mg/dL (adjusted RR, 3.37 [95% CI, 2.60-4.39]), 82.0 for levels of 7.0 to 7.9 mg/dL (adjusted RR, 6.93 [95% CI, 5.43-8.84]), 101.3 for levels of 8.0 to 8.9 mg/dL (adjusted RR, 8.67 [95% CI, 6.74-11.14]), 125.3 for levels of 9.0 to 9.9 mg/dL (adjusted RR, 10.81 [95% CI, j8.02-14.56]), and 132.8 for levels greater than or equal to 10 mg/dL (adjusted RR, 11.42 [95% CI, 7.72-16.90]) (P for trend <.001) (Figure 2).
After further adjustment for BMI; smoking status; consumption of alcohol, coffee, red meat, fish, and poultry; diuretic and urate-lowering therapy use; and diabetes, cardiovascular disease, hypertension, and chronic kidney disease, corresponding RRs were 1.0, 3.16, 6.20, 7.77, 9.80, and 11.26 (95% CI, 7.47-16.97), respectively (P for trend <.001) (Figure 2). Each 1-mg/dL increase in serum urate was associated with a 61% increase in recurrent flare rate (RR, 1.61 [95% CI, 1.54-1.68]) and each increase by 1 SD was associated with a 118% increase in recurrent flare rate (RR, 2.18 [95% CI, 2.02-2.34]). Corresponding RRs in the fully adjusted model were 1.58 (95% CI, 1.50-1.66) per mg/dL and 2.11 (95% CI, 1.95-2.28) per SD (Figure 2).
During the first year of follow-up, corresponding rates per 1000 person-years were 9.5 for serum urate less than 6 mg/dL (adjusted RR, 1.0), 55.2 for serum urate of 6.0 to 6.9 mg/dL (adjusted RR, 5.14 [95% CI, 2.54-10.41]), 125.3 for serum urate of 7.0 to 7.9 mg/dL (adjusted RR, 11.59 [95% CI, 5.96-22.54]), 126.4 for serum urate of 8.0 to 8.9 mg/dL (adjusted RR, 11.86 [95% CI, 6.01-23.38]), 193.8 for serum urate of 9.0 to 9.9 mg/dL (adjusted RR, 18.95 [95% CI, 9.17-39.19]), and 306.7 for serum urate greater than or equal to 10 mg/dL (adjusted RR, 29.20 [95% CI, 13.07-65.20]). Continuously, the RR adjusting for age, sex, and race were 1.66 (95% CI, 1.52 to 1.80) per mg/dL and 2.27 (95% CI, 1.98 to 2.62) per SD (Figure 2). Associations were similar when RRs and 95% CIs were estimated using Poisson regression and robust variances (eTable 4 in Supplement 1). Associations between baseline serum urate level and flare rate remained similar among subsets defined by sex, race, presence of chronic kidney disease, diuretic use, and urate-lowering therapy use (P for interaction between mean serum urate change and each covariate >.22) (Figure 3).
Figure 3. Rate and Rate Ratio (RR) for Recurrent Gout Flares per mg/dL and SD of Serum Urate Over 10 Years.
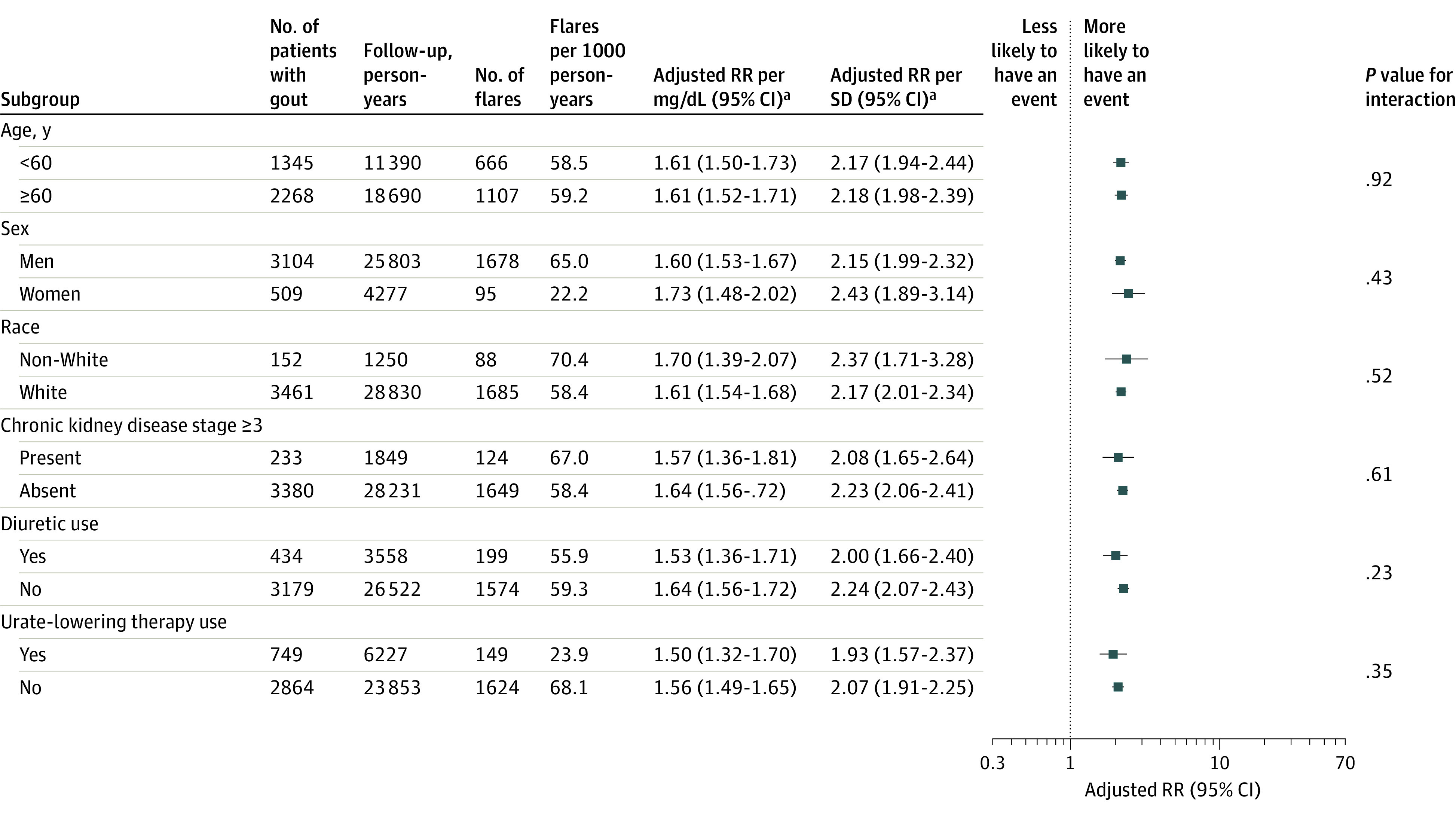
aAdjusted for age, sex, and race.
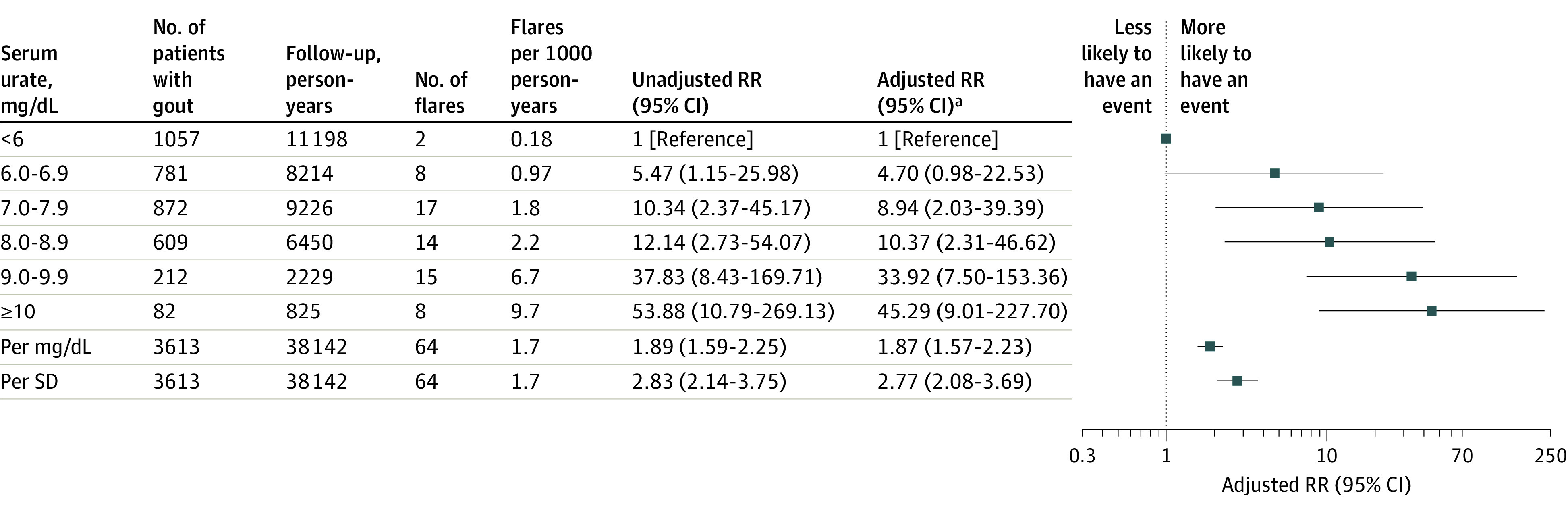
Sixty-four hospitalizations with gout as the primary discharge diagnosis were documented, with 62 (97% [95% CI, 93%-100%) occurring in those with baseline serum urate greater than or equal to 6 mg/dL and all 64 (95% CI, 94%-100%) occurring in those with baseline serum urate greater than or equal to 5 mg/dL (Figure 4; eTable 5 in Supplement 1). Rates of hospitalization for gout (and RRs adjusted for age, sex, and race) per 1000 person-years were 0.18 for those with serum urate less than 6.0 mg/dL (adjusted RR, 1.0), 0.97 for those with rerum urate of 6.0 to 6.9 mg/dL (adjusted RR, 4.70 [95% CI, 0.98-22.53]), 1.8 for those with serum urate of 7.0 to 7.9 (adjusted RR, 8.94 [95% CI, 2.03-39.39]), 2.2 for those with serum urate of 8.0 to 8.9 (adjusted RR, 10.37 [95% CI, 2.31-46.62]), 6.7 for those with serum urate of 9.0 to 9.9 (adjusted RR, 33.92 [95% CI, 7.50-153-36]), and 9.7 for those with serum urate greater than or equal to 10 mg/dL (adjusted RR, 45.29 [95% CI, 9.01-227.70]) (Figure 4). These results corresponded to an 87% increase in gout-primary hospitalization rates per 1-mg/dL increase in serum urate (RR, 1.87 [95% CI, 1.57 to 2.23]) and a 177% increase in gout-primary hospitalization rates per SD (RR, 2.77 [95% CI, 2.08 to 3.69]).
Figure 4. Rate and Rate Ratios (RR) for Recurrent Gout Flares Requiring Hospitalization.
Discussion
In this population-based cohort study of 3613 patients with history of gout who were followed up in primary care for a mean of 8.3 years, 95% of new gout flares occurred in people with baseline serum urate levels of at least 6 mg/dL (ie, US and European therapeutic target threshold22,23) and 98% occurred in those with levels of at least 5 mg/dL (ie, British Society of Rheumatology target threshold24). Overall, 97% of new gout flares resulting in hospitalizations occurred in those with sodium urate of at least 6 mg/dL and 100% of new gout flares resulting in hospitalizations occurred in those with serum urate of at least 5 mg/dL. The associations with gout flares remained after adjusting for sex, race, chronic kidney disease status, diuretic use, and urate-lowering therapy use. Overall, a single serum urate level measure was strongly associated with the risk of recurrent gout flares in this study, with nearly all acute gout flares occurring in people with baseline serum urate greater than 5 mg/dL or 6 mg/dL.
Uric acid, with a pKa of 5.8, is a mild acid and primarily exists as urate, its ionized form, under physiological pH conditions.2 As urate concentration increases above the saturation point of approximately 6.8 mg/dL25,26 in physiologic fluids, supersaturation and monosodium urate crystal formation occur, which is a necessary step in the pathogenesis of gout flares.2,5,6 The solubility of urate in joint fluids may be influenced by other factors in the joint, such as temperature, pH level, concentration of cations, level of articular dehydration, and the presence of nucleating agents.2,27,28,29
In this study, there was no significant effect modification by baseline urate-lowering therapy use, suggesting that higher serum urate levels were associated with higher risk of gout flares in a similar manner between people using urate-lowering therapy and those not using urate-lowering therapy. Urate-lowering therapy did not significantly alter the association of serum urate with risk of an acute gout flare. The observed associations did not change meaningfully with additional statistical adjustment for BMI; smoking status; consumption of alcohol, coffee, red meat, fish, and poultry; diuretic and urate-lowering therapy use; and diabetes, cardiovascular disease, hypertension, and chronic kidney disease.
Strengths of this study include the prospective data collection, the length of follow-up, and the ascertainment of flares from primary hospitalizations for gout and from outpatient diagnoses, including those specifically for acute gout. The study design included measurement of serum urate at a baseline point related to participation in the UK Biobank and should have avoided detection of lower serum urate levels during acute flares, when serum urate levels are known to drop.30,31,32,33
Limitations
This study has several limitations. First, UK Biobank participants typically have a better socioeconomic status and are healthier than the UK general population.11 Second, acute gout flares that were not treated by medical personnel could not be measured. Therefore, these data may underestimate the number of acute gout flares in the cohort. Third, some patients might have had a plan for acute gout flares that prevented the need to seek medical attention and lower serum urate levels from active management. Fourth, certain subgroups, such as certain racial groups, were relatively small in size. Fifth, in this observational data set, residual and unmeasured confounding may exist. Sixth, 55% of the UK Biobank did not have primary care record data available and could not be included in this study.
Conclusions
In this retrospective study of patients with history of gout, serum urate levels at baseline were associated with the risk of subsequent gout flares and with rates of hospitalization for recurrent gout. These findings support using a baseline serum urate to assess risk of recurrent gout over nearly 10 years of follow-up.
Educational Objective: To identify the key insights or developments described in this article.
-
This study examined the association between serum urate levels and recurrent episodes of gout in a mostly older male population in the UK. What percentage of recurrent episodes of gout occurred in those with elevated urate levels?
Almost 50% of acute gout episodes occurred in participants with baseline serum urate ≥6 mg/dL.
Ninety-five percent of acute gout episodes occurred in participants with baseline serum urate ≥6 mg/dL.
Although serum urate levels were associated with recurrent acute gout in a graded manner, the majority of episodes of acute gout occurred in participants with unremarkable baseline urate levels.
-
How were baseline serum urate levels and hospitalization for gout associated?
Hospitalizations with gout were rare and no participants were hospitalized with a primary discharge diagnosis of gout.
Rates of hospitalization for gout were not associated with baseline serum urate levels.
Althpugh infrequent, hospitalizations for gout occurred only in participants with serum urate ≥5 mg/dL.
-
How did other risk factors modify the value of a serum urate level in predicting the risk of recurrent gout?
Adjustment for the use of urate-lowering therapies eliminated the association between recurrent gout flares and serum urate levels.
In association with elevated serum urate levels, all risk factors demonstrated synergistically increased probability of recurrent gout flares.
Observed associations between serum urate and gout flares were stable regardless of statistical adjustment for body mass index, smoking, consumption of red meat, and other risk factors.
eMethods. Assessment of Covariates
eReferences
eTable 1. Baseline Characteristics of the UK Biobank Participants with and without Linked Primary Care Data Available
eTable 2. Diagnostic Codes for Gout in Primary Care Records
eTable 3. Rate and Rate Ratio (RR) for Recurrent Gout Flares According to Serum Urate Level and Follow-Up Time from Baseline, Reference <5 mg/dL
eTable 4. Rate and Rate Ratio (RR) for Recurrent Gout Flares According to Serum Urate Level from Baseline Over 10 Years’ Follow-Up, Reference <6 mg/dL, Generated Using Poisson Regression Models with Robust Variance
eTable 5. Rate and Rate Ratios (RR) for Recurrent Gout Flares Requiring Hospitalization, Reference <5 mg/dL
Data sharing statement
References
- 1.Yokose C, McCormick N, Lu N, et al. Trends in prevalence of gout among US Asian adults, 2011-2018. JAMA Netw Open. 2023;6(4):e239501. doi: 10.1001/jamanetworkopen.2023.9501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi HK, Mount DB, Reginato AM; American College of Physicians; American Physiological Society . Pathogenesis of gout. Ann Intern Med. 2005;143(7):499-516. doi: 10.7326/0003-4819-143-7-200510040-00009 [DOI] [PubMed] [Google Scholar]
- 3.Cipolletta E, Tata LJ, Nakafero G, Avery AJ, Mamas MA, Abhishek A. Association between gout flare and subsequent cardiovascular events among patients with gout. JAMA. 2022;328(5):440-450. doi: 10.1001/jama.2022.11390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cipolletta E, Tata LJ, Nakafero G, Avery AJ, Mamas MA, Abhishek A. Risk of venous thromboembolism with gout flares. Arthritis Rheumatol. 2023;75(9):1638-1647. doi: 10.1002/art.42480 [DOI] [PubMed] [Google Scholar]
- 5.Dalbeth N, Choi HK, Joosten LAB, et al. Gout. Nat Rev Dis Primers. 2019;5(1):69. doi: 10.1038/s41572-019-0115-y [DOI] [PubMed] [Google Scholar]
- 6.Choi HK. Gout and other crystal-associated arthropathies. In: Loscalzo JFA, Kasper D, Hauser S, Longo D, Jameson J, eds. Harrison’s Principles of Internal Medicine. 21st ed. McGraw Hill; 2022. [Google Scholar]
- 7.Campion EW, Glynn RJ, DeLabry LO. Asymptomatic hyperuricemia: risks and consequences in the Normative Aging Study. Am J Med. 1987;82(3):421-426. doi: 10.1016/0002-9343(87)90441-4 [DOI] [PubMed] [Google Scholar]
- 8.Bhole V, de Vera M, Rahman MM, Krishnan E, Choi H. Epidemiology of gout in women: fifty-two-year follow-up of a prospective cohort. Arthritis Rheum. 2010;62(4):1069-1076. doi: 10.1002/art.27338 [DOI] [PubMed] [Google Scholar]
- 9.Dalbeth N, Phipps-Green A, Frampton C, Neogi T, Taylor WJ, Merriman TR. Relationship between serum urate concentration and clinically evident incident gout: an individual participant data analysis. Ann Rheum Dis. 2018;77(7):1048-1052. doi: 10.1136/annrheumdis-2017-212288 [DOI] [PubMed] [Google Scholar]
- 10.Caleyachetty R, Littlejohns T, Lacey B, et al. United Kingdom Biobank (UK Biobank): JACC Focus Seminar 6/8. J Am Coll Cardiol. 2021;78(1):56-65. doi: 10.1016/j.jacc.2021.03.342 [DOI] [PubMed] [Google Scholar]
- 11.Fry A, Littlejohns TJ, Sudlow C, et al. Comparison of sociodemographic and health-related characteristics of UK biobank participants with those of the general population. Am J Epidemiol. 2017;186(9):1026-1034. doi: 10.1093/aje/kwx246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joshi AD, McCormick N, Yokose C, et al. Prediagnostic glycoprotein acetyl levels and incident and recurrent flare risk accounting for serum urate levels: a population-based, prospective study and mendelian randomization analysis. Arthritis Rheumatol. 2023;75(9):1648-1657. doi: 10.1002/art.42523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Primary Care Linked Data: Version 1.0. UK Biobank; 2019. Accessed January 2, 2024. https://biobank.ctsu.ox.ac.uk/crystal/refer.cgi?id=591
- 14.Companion Document to Accompany Serum Biomarker Data. UK Biobank; 2019. Accessed January 2, 2024. https://biobank.ctsu.ox.ac.uk/crystal/ukb/docs/serum_biochemistry.pdf
- 15.Singh JA. Veterans Affairs databases are accurate for gout-related health care utilization: a validation study. Arthritis Res Ther. 2013;15(6):R224. doi: 10.1186/ar4425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zheng C, Rashid N, Wu YL, et al. Using natural language processing and machine learning to identify gout flares from electronic clinical notes. Arthritis Care Res (Hoboken). 2014;66(11):1740-1748. doi: 10.1002/acr.22324 [DOI] [PubMed] [Google Scholar]
- 17.Rothenbacher D, Primatesta P, Ferreira A, Cea-Soriano L, Rodríguez LA. Frequency and risk factors of gout flares in a large population-based cohort of incident gout. Rheumatology (Oxford). 2011;50(5):973-981. doi: 10.1093/rheumatology/keq363 [DOI] [PubMed] [Google Scholar]
- 18.Neogi T, Chen C, Niu J, Chaisson C, Hunter DJ, Zhang Y. Alcohol quantity and type on risk of recurrent gout attacks: an internet-based case-crossover study. Am J Med. 2014;127(4):311-318. doi: 10.1016/j.amjmed.2013.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y, Chen C, Choi H, et al. Purine-rich foods intake and recurrent gout attacks. Ann Rheum Dis. 2012;71(9):1448-1453. doi: 10.1136/annrheumdis-2011-201215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hunter DJ, York M, Chaisson CE, Woods R, Niu J, Zhang Y. Recent diuretic use and the risk of recurrent gout attacks: the online case-crossover gout study. J Rheumatol. 2006;33(7):1341-1345. [PubMed] [Google Scholar]
- 21.Zhang Y, Neogi T, Chen C, Chaisson C, Hunter DJ, Choi HK. Cherry consumption and decreased risk of recurrent gout attacks. Arthritis Rheum. 2012;64(12):4004-4011. doi: 10.1002/art.34677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.FitzGerald JD, Dalbeth N, Mikuls T, et al. 2020 American College of Rheumatology Guideline for the Management of Gout. Arthritis Care Res (Hoboken). 2020;72(6):744-760. doi: 10.1002/acr.24180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richette P, Doherty M, Pascual E, et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis. 2017;76(1):29-42. doi: 10.1136/annrheumdis-2016-209707 [DOI] [PubMed] [Google Scholar]
- 24.Hui M, Carr A, Cameron S, et al. ; British Society for Rheumatology Standards, Audit and Guidelines Working Group . The British Society for Rheumatology Guideline for the Management of Gout. Rheumatology (Oxford). 2017;56(7):1246. doi: 10.1093/rheumatology/kex250 [DOI] [PubMed] [Google Scholar]
- 25.Loeb JN. The influence of temperature on the solubility of monosodium urate. Arthritis Rheum. 1972;15(2):189-192. doi: 10.1002/art.1780150209 [DOI] [PubMed] [Google Scholar]
- 26.Seegmiller JE. The acute attack of gouty arthritis. Arthritis Rheum. 1965;8(5):714-725. doi: 10.1002/art.1780080431 [DOI] [PubMed] [Google Scholar]
- 27.Burt HM, Dutt YC. Growth of monosodium urate monohydrate crystals: effect of cartilage and synovial fluid components on in vitro growth rates. Ann Rheum Dis. 1986;45(10):858-864. doi: 10.1136/ard.45.10.858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McGill NW, Dieppe PA. The role of serum and synovial fluid components in the promotion of urate crystal formation. J Rheumatol. 1991;18(7):1042-1045. [PubMed] [Google Scholar]
- 29.Fam AG, Stein J, Rubenstein J. Gouty arthritis in nodal osteoarthritis. J Rheumatol. 1996;23(4):684-689. [PubMed] [Google Scholar]
- 30.Halpern R, Fuldeore MJ, Mody RR, Patel PA, Mikuls TR. The effect of serum urate on gout flares and their associated costs: an administrative claims analysis. J Clin Rheumatol. 2009;15(1):3-7. doi: 10.1097/RHU.0b013e3181945d2c [DOI] [PubMed] [Google Scholar]
- 31.Wu EQ, Patel PA, Mody RR, et al. Frequency, risk, and cost of gout-related episodes among the elderly: does serum uric acid level matter? J Rheumatol. 2009;36(5):1032-1040. doi: 10.3899/jrheum.080487 [DOI] [PubMed] [Google Scholar]
- 32.Urano W, Yamanaka H, Tsutani H, et al. The inflammatory process in the mechanism of decreased serum uric acid concentrations during acute gouty arthritis. J Rheumatol. 2002;29(9):1950-1953. [PubMed] [Google Scholar]
- 33.Schlesinger N, Norquist JM, Watson DJ. Serum urate during acute gout. J Rheumatol. 2009;36(6):1287-1289. doi: 10.3899/jrheum.080938 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Assessment of Covariates
eReferences
eTable 1. Baseline Characteristics of the UK Biobank Participants with and without Linked Primary Care Data Available
eTable 2. Diagnostic Codes for Gout in Primary Care Records
eTable 3. Rate and Rate Ratio (RR) for Recurrent Gout Flares According to Serum Urate Level and Follow-Up Time from Baseline, Reference <5 mg/dL
eTable 4. Rate and Rate Ratio (RR) for Recurrent Gout Flares According to Serum Urate Level from Baseline Over 10 Years’ Follow-Up, Reference <6 mg/dL, Generated Using Poisson Regression Models with Robust Variance
eTable 5. Rate and Rate Ratios (RR) for Recurrent Gout Flares Requiring Hospitalization, Reference <5 mg/dL
Data sharing statement