Abstract
Objective
To determine inpatient healthcare utilization in an incident cohort of patients with systemic lupus erythematosus (SLE) compared to the general population.
Methods
This was a population-based cohort study in the upper Midwest, USA. We included patients fulfilling the European League Against Rheumatism/American College of Rheumatology SLE classification criteria between 1995–2018. They were 1:1 age-, sex-, county-matched with individuals without SLE. All hospital admissions and emergency department (ED) visits were electronically retrieved for 1995–2020. Rates for hospital admission, length of stay, readmission, ED visits, and discharge destination were compared between groups.
Results
341 patients with SLE and 341 comparators without SLE were included (mean age of 48.6 years at diagnosis, 79.2% female). Rates of hospitalization for patients with SLE and comparators were 29.8 and 9.9 per 100 person-years, respectively. These differences were present across sexes and age groups. Hospitalization rates were higher in patients with SLE after diagnosis and remained higher than comparators for the first 15 years of the disease. Patients with SLE were more likely than comparators to visit the emergency department (HR 2.71, 95% CI 2.05–3.59). Readmission rates (32% vs. 21%, p=0.017) were higher in patients with SLE. Length of stay and discharge destination were similar between both groups.
Conclusion
Patients with SLE were more likely to be hospitalized and to visit the emergency department than individuals without SLE, highlighting important inpatient care needs. Increased hospitalization rates were observed in both males and females and all age groups.
Key Indexing Terms: Systemic lupus erythematosus, hospitalization, healthcare utilization, epidemiology, incidence
BACKGROUND
Systemic lupus erythematosus (SLE) is an autoimmune disease which can affect multiple organ systems: skin, kidneys, joints, blood cells, serosal membranes, central nervous system, and others [1]. Women of childbearing age are more commonly affected [2]. In the United States, the prevalence of SLE is estimated to be 72.8/100,000 [2], and although mortality has decreased throughout the last decades [3, 4] morbidity is still very concerning [5].
SLE manifestations, its comorbidities, and complications due to immunosuppressive treatment can lead to emergency department (ED) visits or hospital admissions. Prior studies reported an incidence rate of 40 hospitalizations per 100 patient-years [6] and patients with SLE are mainly hospitalized due to SLE flares, infections, and cardiac diseases [7–9]. Readmissions represented 6 to 17% of all hospitalizations among patients with SLE [10, 11].
Nonetheless, as of today, no contemporary assessment thoroughly describes inpatient healthcare utilization, from ED to discharge of patients with SLE. Furthermore, methodological obstacles to the interpretation of previous studies include the use of diagnostic codes in administrative databases with their inherent risk of misclassification, short follow-up periods, the utilization of outdated data and lapsed classification criteria. Likewise, ED visits and reasons for hospitalization were described but not quantified in comparison to individuals without SLE.
The purpose of this study was to perform a contemporary and comprehensive assessment of inpatient healthcare utilization in a population-based cohort of patients with SLE, followed over more than twenty-five years.
METHODS
Study design
The Lupus Midwest Network (LUMEN💡) is a population-based registry of a 27-county region in southeastern Minnesota and southwestern Wisconsin nested in the Rochester Epidemiology Project (REP), a record-linkage system. The REP allows ready access to the medical records from health care providers for the local population, including the Mayo Clinic and its health system, the Olmsted Medical Center and their affiliated hospitals, local nursing homes, etc. The demographics, distribution of morbidity, and death rates in the REP region are like those in the upper Midwest [12]. The characteristics and strengths of the REP, as well as its generalizability, have been described elsewhere [13–15]. Any identified subjects who did not provide consent for use of their medical records for research purposes were excluded from the study — approximately 2% of the REP population [15]. The study was approved by the institutional review boards of the Mayo Clinic and Olmsted Medical Center.
Study population
Potential SLE cases were identified through two different strategies: 1) through International Classification of Diseases 9 (ICD-9) and ICD-10 codes for SLE, cutaneous lupus erythematosus, and other associated diseases and 2) through laboratory measures associated with SLE (anti-nuclear antibodies (>1:80), low complement, anti-double stranded DNA, anti-Sm, lupus anticoagulant anticardiolipin (IgG, IgM and IgA) and anti-beta 2 glycoprotein 1 (IgG, IgM and IgA) antibodies (see Table 1, Supplemental Digital Content, for the complete list of codes). Then individual chart reviews were performed, and data were abstracted by extensively trained reviewers. Demographic characteristics and clinical and laboratory data included in the classification criteria were abstracted from the electronic medical records. Patients meeting the 2019 European League Against Rheumatism/American College of Rheumatology (EULAR/ACR) classification criteria for SLE [16] and living in one of the 27 counties prior to the earliest date of criteria fulfillment were considered incident and included in the cohort. We used the EULAR/ACR criteria since it performs better at identifying patients in population-based studies [17].
Table 1.
Hospitalization rates (per 100 person-years) of 341 patients with systemic lupus erythematosus (SLE) and 341 comparators without SLE in the 27-county area, 1995–2020.
| Patients with SLE | Comparators without SLE | |||||||
|---|---|---|---|---|---|---|---|---|
| Parameter | Value | Hospitalizations (N) | Follow-up (py) | Rate* | Hospitalizations (N) | Follow-up (py) | Rate* | Rate ratio (95% CI) |
| Overall | 719 | 2409.2 | 29.8 | 199 | 2004.1 | 9.9 | 3.00 (2.57–3.52) | |
| Age, years | 0–19 | 16 | 50.1 | 32.0 | 1 | 36.8 | 2.7 | 8.10 (2.29–113.92) |
| 20–49 | 327 | 1179.4 | 27.7 | 57 | 889.7 | 6.4 | 4.30 (3.29–5.78) | |
| 50–64 | 173 | 664.3 | 26.0 | 30 | 523.9 | 5.8 | 4.49 (3.13–6.79) | |
| 65+ | 203 | 515.4 | 39.4 | 111 | 553.7 | 20.0 | 1.96 (1.56–2.48) | |
| Sex, n | Female | 557 | 1969.0 | 28.3 | 135 | 1651.4 | 8.2 | 3.45 (2.87–4.19) |
| Male | 162 | 440.2 | 36.8 | 64 | 352.7 | 18.1 | 2.02 (1.53–2.72) | |
| Race/Ethnicity, n | Non-Hispanic White | 509 | 1917.5 | 26.6 | 173 | 1824.7 | 9.5 | 2.80 (2.36–3.33) |
| All other | 210 | 491.7 | 42.7 | 26 | 179.4 | 14.5 | 2.95 (1.96–4.43) | |
| Duration of disease, years | 0–5 | 465 | 1377.7 | 33.8 | 136 | 1401.9 | 9.7 | 3.47 (2.88–4.22) |
| 5–10 | 156 | 617.2 | 25.3 | 46 | 367.2 | 12.5 | 2.00 (1.46–2.82) | |
| 10–15 | 79 | 258.6 | 30.5 | 10 | 120.2 | 8.3 | 3.52 (1.98–7.38) | |
| 15+ | 19 | 155.6 | 12.2 | 7 | 114.8 | 6.1 | 1.92 (0.88–4.97) | |
| County, n | Olmsted | 445 | 1499.5 | 29.7 | 112 | 1166.1 | 9.6 | 3.08 (2.52–3.81) |
| 26 Counties | 274 | 909.7 | 30.1 | 87 | 838.0 | 10.4 | 2.89 (2.29–3.71) | |
Abbreviations: CI= confidence interval; py= person-years; SLE= systemic lupus erythematosus.
per 100 person-years.
The hospitalization data was electronically available since 1995 in the REP, thus all patients who fulfilled the criteria from January 1, 1995 in Olmsted County or from 2010 in the other 26 counties until December 31, 2018 were included.
Patients with SLE were matched (1:1) on age, sex, and county of residence at the date of SLE classification to comparators without SLE from the same underlying population. Both groups were followed until December 31, 2020, emigration out of the geographical area, or death.
Data collection
A retrospective review of charts provided data on demographic, clinical, and serological characteristics of the patients. All hospitalizations and emergency department visits from January 1, 1995 in Olmsted County and from January 1, 2010 in the other 26 counties to December 31, 2020 were obtained. Data on Charlson comorbidity index [18], primary discharge diagnosis, length of stay and destination upon discharge, after ED visit and hospital admission were electronically retrieved. Primary discharge diagnoses were manually classified into 18 mutually exclusive categories based on the Clinical Classifications Software (CCS) for ICD-9 Clinical Modification (ICD-9-CM) and ICD-10-CM from the Healthcare Cost and Utilization Project [19]. SLE flares and diseases related to SLE involvement (e.g., pericarditis, auto-immune hemolysis, glomerulonephritis, fever of unknown origin) were considered as a standalone category. Infections of any system were included in ‘infectious diseases’; likewise, all solid or hematological cancer were classified in ‘neoplasms’. Readmission was defined as a distinct new admission within 30 days after the discharge of a previous distinct hospitalization. Discharge destination was manually reviewed and classified in four categories: home, rehabilitation/skilled nursing facility, death, and unknown.
Statistical analyses
Descriptive statistics (means, standard deviations [SD], medians, interquartile ranges [IQR], counts, and percentages) were used to summarize the characteristics of patients with SLE and comparators. Chi-square and rank-sum tests were performed to compare the baseline characteristics between patients with SLE and comparators. Hospitalization rates of cases and comparators were estimated using person-year (py) methods and compared using Poisson regression models. Generalized additive models with smoothing splines, using a quasi-Poisson distribution to account for overdispersion, were utilized to examine trends over time to allow for nonlinear effects. Given the differences in follow-up between Olmsted County residents and the rest of the counties, we performed a sensitivity analysis comparing the hospitalizations among patients with and without SLE living in Olmsted County and those living in the other counties. The readmission ratio was calculated with the number of readmissions (as numerator) and number of subsequent hospitalizations (as denominator). Comparisons between cohorts for readmissions, discharge destination, hospitalizations after ED visits, and length of stay were analyzed using generalized linear models adjusted for age and sex using a binomial distribution for binary outcomes and gaussian distributions for continuous outcomes, with random intercepts to account for multiple hospitalizations per patient. Cox proportional hazards models were used to calculate hazard ratios (HR) with 95% confidence intervals for time to first hospitalization and first ED visit after SLE diagnosis, adjusting for age, sex, and calendar year. We assessed the cumulative incidence of first hospitalization and first ED visit adjusting for the competing risk of death. A p-value < 0.05 was considered statistically significant. Analyses were performed using SAS version 9.4 (SAS Institute) and R 3.2.3 (R Foundation for Statistical Computing).
RESULTS
341 incident patients with SLE and as many comparators without SLE were included. Women represented 79.2%, and the mean age at diagnosis was 48.6 years. Representative of this geographical area, the majority of patients were non-Hispanic White (78.9% among SLE, 89.4% among non-SLE). The length of follow-up was 7.1 years for patients with SLE and 5.9 years for those without SLE, the main clinical manifestations of SLE are depicted in Supplemental Digital Content (see table 2 and 3 for more details).
Hospitalization rates and proportion of patients hospitalized
There were 719 hospitalizations among patients with SLE during 2409 person-years (py) of follow-up (hospitalization rate: 29.84/100 py), while among comparators without SLE there were 199 hospitalizations in 2004 person-years (hospitalization rate: 9.93/100 py). Patients with SLE had 3 times more hospitalizations than comparators without SLE (Rate ratio [RR] 3.0, 95% CI 2.57–3.52; Table 1). 54.5% of patients with SLE were hospitalized at least once vs. 25.5% of individuals without SLE (p<0.001).
Patients with SLE had significantly higher hospitalization rates compared to those without SLE in every age group. Whilst hospitalization rates were 8 times higher in SLE than non-SLE among patients younger than 20 years old (RR 8.1, 95% CI 2.29–113.92), hospitalization rates were four times higher in SLE compared to non-SLE among patients from 20 to 49 years old and from 50 to 64 years old (RR 4.3, 95% CI 3.29–5.78 and RR 4.49, 95% CI 3.13–6.79, respectively), and remained twice as high in those aged 65 years and older (RR 1.96, 95% CI 1.56–2.48). The hospitalization rate among men with SLE was twice as high compared to men without SLE (RR 2.02, 95% CI 1.53–2.72), and three times higher among women with SLE compared with women without SLE (RR 3.45, 95% CI 2.87–4.19). While hospitalization rates were higher for non-Whites than non-Hispanic Whites in both cohorts, the rate ratios for hospitalizations among patients with SLE compared with those without SLE were similar (RR 2.80, 95% CI 2.36–3.33 among non-Hispanic Whites and RR 2.95, 95% CI 1.96–4.43 among other race/ethnicity). In the sensitivity analysis, the rates of hospitalizations were similar among those living in Olmsted County and those living in the other 26 counties.
When looking at the duration of disease, patients with SLE had significantly higher hospitalization rates than comparators without SLE during the first 15 years after SLE diagnosis/index date for comparators. As depicted in Figure 1, hospitalization rates were at the highest in patients with SLE immediately after diagnosis and gradually reached the same rates of hospitalization as comparators around 20 years after diagnosis (SLE p for trend <0.001).By five years after diagnosis, more than half of the patients with SLE were hospitalized at least once, compared to 20% of the comparators (Figure 2).
Figure 1.
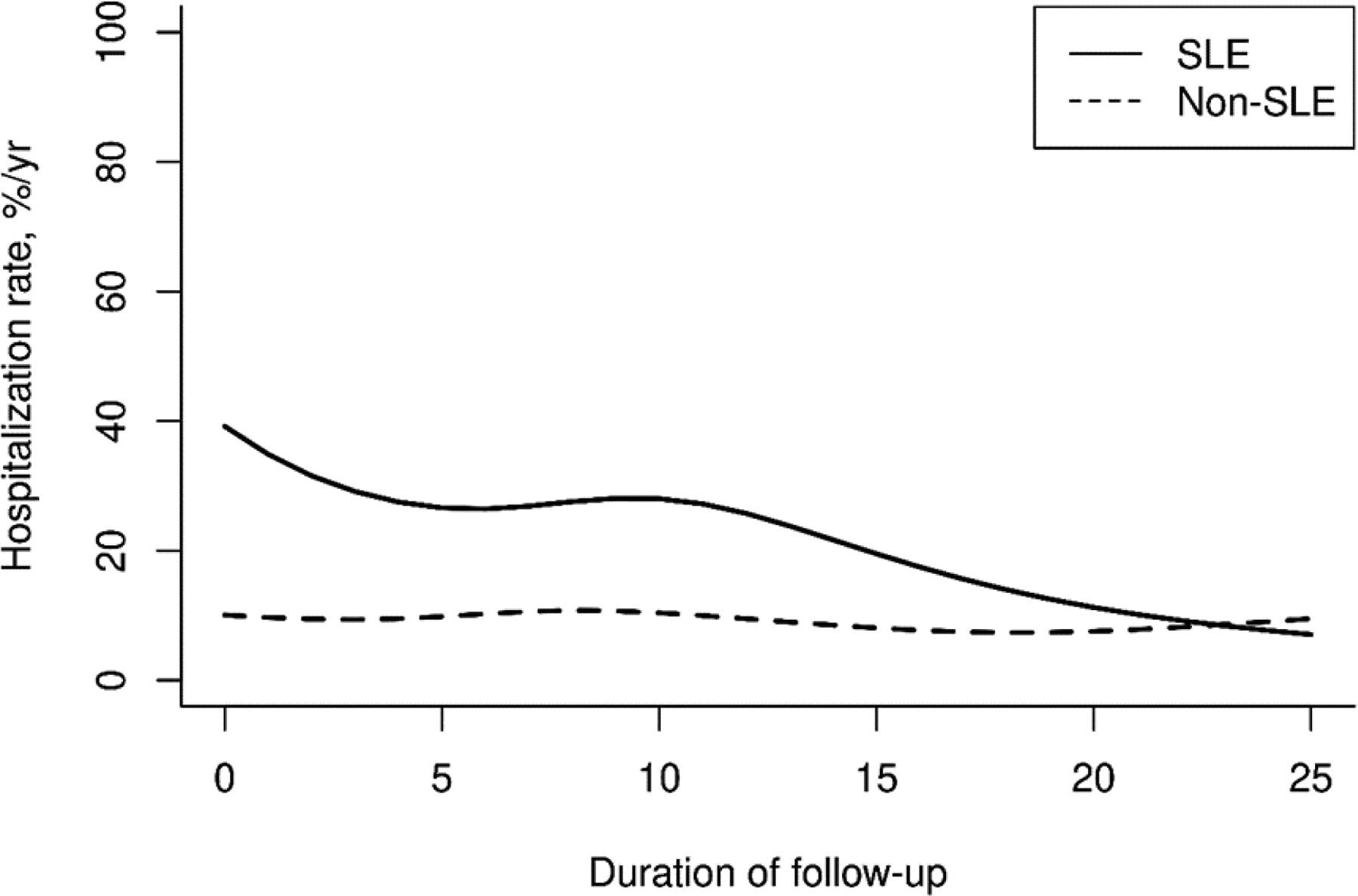
Age-, sex- and calendar year-adjusted hospitalization rate among patients with systemic lupus erythematosus (SLE) and control patients without SLE after diagnosis. Trends over duration of follow-up were statistically significant in patients without SLE (p<0.0001) but not in patients without SLE (p=0.58), based on Poisson regression, adjusted for age, sex, and calendar year.
Figure 2.
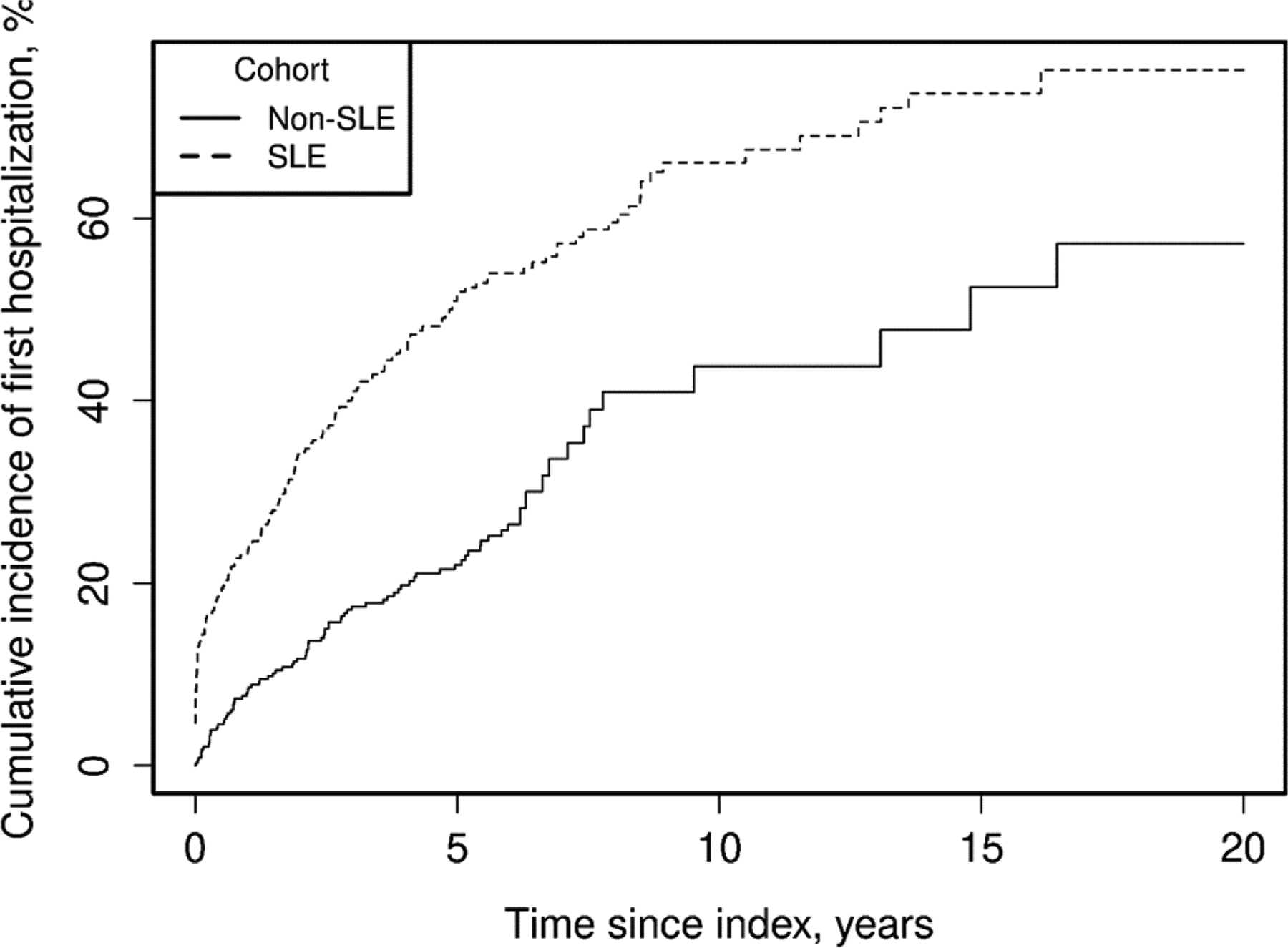
Cumulative incidence of time to first hospitalization comparing patients with SLE vs. without SLE adjusted for competing risk of death. Hazard Ratio 2.43 (95% Confidence Interval 1.88–3.16, p<0.001).
Although hospitalization mean length of stay among patients with SLE tended to be longer than in non-SLE group (6.1 vs 4.9 days), this difference did not reach statistical significance (p=0.056). Median length of stay was 3 days within both cohorts.
Reasons for hospitalization
The three most frequent causes of hospitalizations in patients with SLE were infections (n=177, 24.6% of all SLE hospitalizations, rate of hospitalization: 7.3/100 py), diseases of the circulatory system (n=109, 15.2%, rate of hospitalization: 4.5/100 py) and hospitalizations due to SLE flares (n=88, 12.2%, rate of hospitalization: 3.7/100 py; Table 2). Compared to individuals without SLE, the rates of hospitalizations were higher in 11 of the 18 discharge diagnosis categories, in particular for respiratory-related diseases (RR 5.82, 95% CI 2.5–20.04), diseases of the blood and the blood-forming organs (RR 5.27, 95% CI 1.35–74.73), renal diseases (RR 4.53, 95% CI 1.90–15.74), and infectious diseases (RR 3.84, 95% CI 2.76–5.56). The two main reasons for hospitalization among non-SLE comparators were infectious and circulatory system diseases.
Table 2.
Rates of hospitalization among patients with systemic lupus erythematosus (SLE) and comparators without SLE according to categorized primary discharge diagnoses in the 27-county area, 1995–2020.
| Patients with SLE* | Comparators without SLE† | ||||
|---|---|---|---|---|---|
| Diagnosis | Hospitalizations (N) | Rate‡ | Hospitalizations (N) | Rate‡ | Rate ratio (95% CI) |
| SLE flares | 88 | 3.7 | 0 | - | - |
| Diseases of the respiratory system | 31 | 1.3 | 4 | 0.2 | 5.82 (2.50–20.04) |
| Diseases of the blood and blood-forming organs | 9 | 0.4 | 1 | 0.05 | 5.27 (1.35–74.73) |
| Renal diseases | 24 | 1.0 | 4 | 0.2 | 4.53 (1.90–15.74) |
| Infectious and parasitic diseases | 177 | 7.3 | 38 | 1.9 | 3.84 (2.76–5.56) |
| Diseases of the circulatory system | 109 | 4.5 | 35 | 1.8 | 2.57 (1.79–3.83) |
| Diseases of the digestive system | 58 | 2.4 | 18 | 0.9 | 2.63 (1.61–4.63) |
| Diseases of the nervous system and sense organs | 31 | 1.3 | 10 | 0.5 | 2.50 (1.31–5.44) |
| Diseases of the skin and the subcutaneous tissue | 7 | 0.3 | 2 | 0.1 | 2.50 (0.70–16.07) |
| Urinary tract diseases, located after the kidney | 4 | 0.2 | 1 | 0.05 | 2.50 (0.49–36.18) |
| Metal illness, self-harm attempts, and alcohol abuse | 39 | 1.6 | 13 | 0.6 | 2.43 (1.36–4.78) |
| Nutritional and metabolic diseases | 29 | 1.2 | 10 | 0.5 | 2.34 (1.21–5.11) |
| Bone fractures, contusions, orthopedic operations, and orthopedic diseases due to implants | 16 | 0.7 | 7 | 0.4 | 1.83 (0.81–4.80) |
| Degenerative and other diseases of the musculoskeletal system | 34 | 1.4 | 14 | 0.7 | 1.98 (1.10–3.84) |
| Poisoning and medicine abuse without intentional self-harm | 5 | 0.2 | 2 | 0.1 | 1.83 (0.45–12.02) |
| Neoplasms and chemotherapies | 15 | 0.6 | 10 | 0.5 | 1.23 (0.57–2.83) |
| Complications of pregnancy; childbirth, and puerperium; diseases due to female genital system | 36 | 1.5 | 28 | 1.4 | 1.07 (0.66–1.77) |
| Other cause of hospitalization | 7 | 0.3 | 2 | 0.1 | 2.50 (0.70–16.07) |
Abbreviations: CI= confidence interval, SLE= systemic lupus erythematosus.
719 hospitalizations. Length of follow-up of 2,409 person-years.
199 hospitalizations. Length of follow-up of 2,004 person-years.
Rates are reported per 100 person-years.
Emergency department visits
Patients with SLE experienced 3,369 ED visits during follow-up and those without SLE experienced 1,552 ED visits during follow-up. By 10 years after SLE incidence/index date, the probability of 1 or more ED visits in the SLE group was 55% (95% CI 49%–63%) compared to 34% (95% CI 27%–49%) in the non-SLE group. Patients with SLE were 2.7-times as likely to visit the ED at least once than those without SLE (HR 2.71, 95% CI 2.05–3.59, p<0.001; Figure 3).
Figure 3.
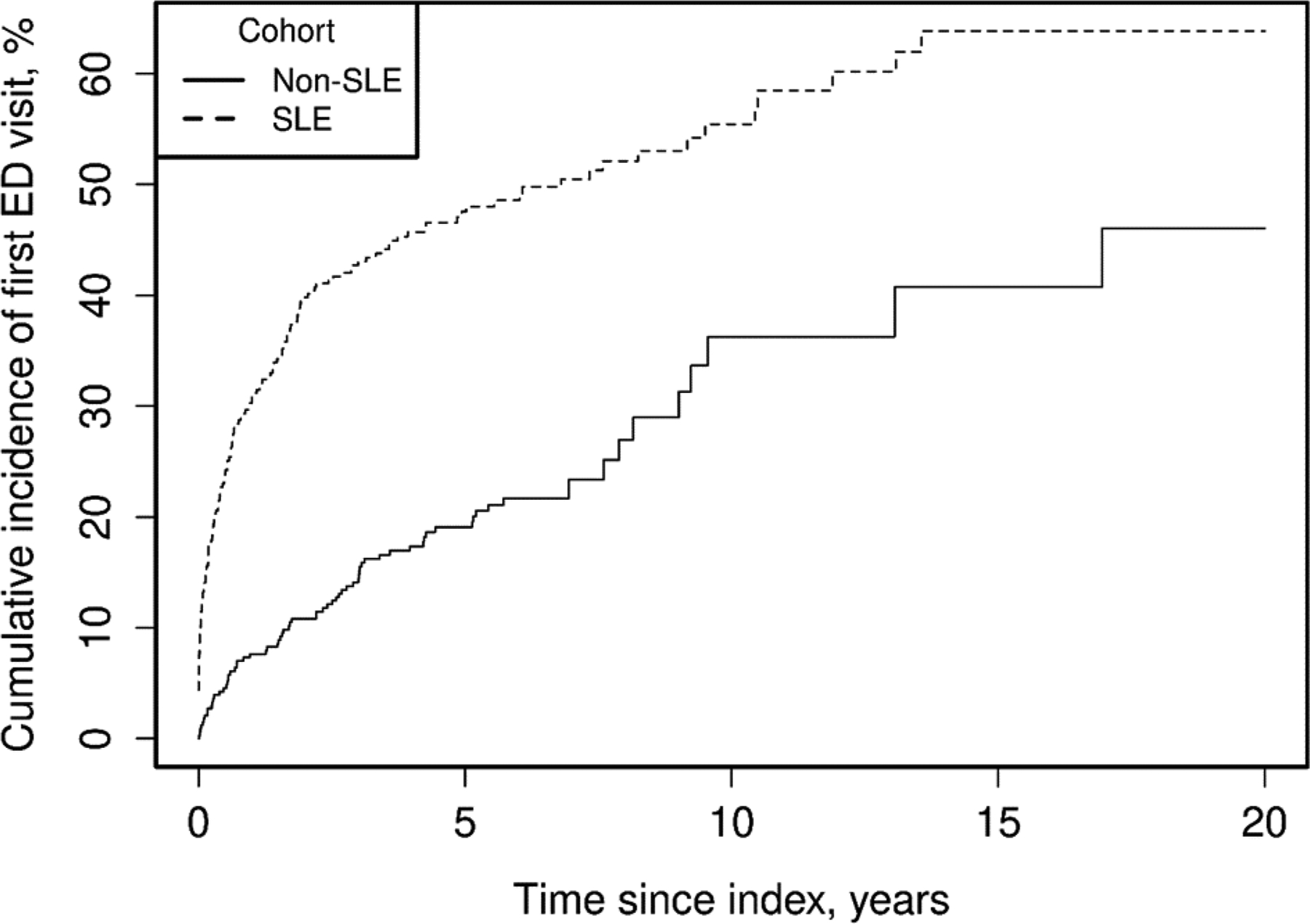
Cumulative incidence of first emergency department (ED) visits comparing patients with systemic lupus erythematosus (SLE) vs. individuals without SLE adjusted for competing risk of death. By 10 years after index date, the percentage of patients with 1 or more ED visits in the group with SLE was 55% (95% CI 49–63%) compared to 34% (95% CI 27–49%) in the group without SLE. Hazard Ratio 2.71 (95% Confidence Interval 2.05–3.39, p<0.001).
Following the patients with SLE ED visits, 13.4% (n=451/3369) of ED visits resulted in hospitalization. Patients with SLE were 2.5 times as likely to be hospitalized after an ED visit than comparators (age- and sex-adjusted odd ratio [OR] 2.50, 95% CI 1.76–3.57, p<0.001).
Transition of care after discharge
Patients with SLE were discharged to rehabilitation or a skilled nursing facility after 13.6% of hospitalizations. They did not have an increased risk to be discharged to these facilities than comparators (OR 1.19, 95% CI 0.63–2.24). Among hospitalizations of patients with SLE, 2.6% ended in death compared to 1.5% among comparators (OR 2.88, 95% CI 0.79–10.57).
Readmission ratios
Among all the hospitalizations of patients with SLE, 533 admissions occurred as a second or more hospitalization event, compared to 112 among comparators without SLE. Of these subsequent hospitalizations, 32% were readmissions within the 30 days (170/533 subsequent hospitalizations) in the group with SLE vs. 21% (23/112 subsequent hospitalizations) in the comparators without SLE (p=0.017).
DISCUSSION
This study demonstrated that patients with SLE had overall a 2 to 3-fold increased risk of hospitalization compared to the general population. This increased rate of hospitalization was found for both sexes, all ages, and both non-Hispanic White patients and for those of other race/ethnicity. Although the length of stay was longer for SLE patients, it did not reach statistical significance. Hospitalizations of patients with SLE were mainly due to infections, cardiovascular diseases, and SLE flares. Patients with SLE had a 2.7-fold increased risk of ED visits; and after visiting the ED, they were twice as likely to be hospitalized than comparators. Readmissions also occurred more frequently in patients with SLE.
In a previous study, the annual rate of hospitalization based on a Taiwanese nationwide cohort was 0.4 admission per patient, which is equivalent to 40 admissions per 100 py [6]. Our current study revealed a lower result, 29 admissions per 100py. It is difficult to compare these studies given the differences in the methods, the health systems, and their populations. In addition, Asian populations have been reported to have more severe SLE, which might be the driver of this discrepancy [20]. Regarding the increased risk of hospitalization, a study based on a Medicaid cohort and using billing code-based retrievals for SLE diagnosis and hospitalizations found that patients with SLE were 2.6 times as likely to be hospitalized than comparators [21], which is consistent with our findings.
Our findings also revealed that more than half of patients with SLE experienced at least one hospitalization after ten years of follow-up, confirming results from previous large cohorts [8, 21–23]. Nevertheless, two US studies of ICD code-based populations presented proportions of hospitalized patients with SLE as low as 22% and 26% [24, 25], respectively. Unlike our findings, these differences of proportions may be explained first by misascertainment of the diagnosis, also it is not clear if these studies included newly diagnosed or prevalent SLE patients. As our data shows, hospitalizations in SLE are more frequent in the early-years of the disease, thus a prevalent cohort would have lower hospitalizations. Finally, the aforementioned studies have shorter follow-up.
The risk of hospitalization among patients with SLE was at the highest directly after diagnosis, remained elevated during fifteen years after diagnosis, and then tended to be comparable to the risk among the general population. This decrease of the likelihood of hospitalization may be explained with the aging of comparators, implying an increase in the health care needs of the general population, on the other hand, it is possible that more patients with SLE eventually entered remission. It is also possible that we are observing a survivor effect and those with more severe disease (and thus driving hospitalizations) died within the first 15 years of the disease. A large study gathering patients from an insurance database and diagnosed according to various definitions of SLE observed the highest rates of hospital admission mainly in the 3 years of follow-up after diagnosis, tapering afterwards [26].
The current study showed a median length of stay of 3 days for hospitalized patients with SLE. While this result is consistent with other recent works [7, 27], others found a longer duration, from 6 to 10.9 days, in countries with comprehensive public healthcare systems [6, 8–10, 28, 29]. Our study took place in the United States, which has a pluralistic healthcare system and has been reported to have a shorter length of stay compared to most of the Organization for Economic Co-operation and Development (OECD) countries [30].
Our findings extend previous work, describing how patients with SLE are mainly hospitalized due to SLE flares, infections, or cardiovascular diseases [7–9]. These studies showed that SLE activity represented 15% of hospitalizations in a Danish cohort [8] and almost 24% of the first admissions of SLE patients from an academic health network based in Toronto [9]. Infections were the primary diagnosis of hospitalization in a study that used the National Inpatient Sample database from the US [7], they represented 19% in the Canadian study [9] and 21% in the Danish cohort [8]. Cardiovascular diseases were responsible for around 7% [7] to 10.5% [8] of hospitalizations. However, a Korean cohort using a non-mutually exclusive classification described that SLE flares represented 71% of all hospitalizations and less than 1% of the hospitalizations were related to cardiovascular system disease [23]. Surprisingly, we also highlighted that patients with SLE were hospitalized due to respiratory-related diseases, at a rate 6 times higher than comparators. Though it is important to consider that pleuro-pulmonary involvement is frequent in SLE and contributes to long-term sequelae (like pulmonary arterial hypertension, interstitial lung disease) [31], these results were unanticipated as all serositis, infections, pulmonary embolism, and neoplasms were manually excluded from the respiratory diseases category and respectively classified as SLE flares, infectious diseases, vascular diseases, and diseases related to neoplasm. In the current classification, the diagnoses remaining among respiratory-related diseases were acute and chronic respiratory failures, hypoxia, chronic obstructive pulmonary disease and its exacerbations, as well as pleural effusion not related to SLE.
To our knowledge, this is the first study that reported the transition of care after hospitalization in SLE. We found that patients with SLE were not more frequently discharged to skilled nurse facilities or inpatient rehabilitation compared to non-SLE individuals of the same age and sex.
Our study revealed that the majority of patients with SLE visited the ED at least once during the follow-up, significantly more than the comparators. ED utilization in patients with SLE has been previously described in multiple studies. A couple of reports described similar results to ours, with 40% to 46% of patients with SLE experiencing ED visits [24, 25]. Only one claim-based study during a follow-up period of 39 months presented a higher proportion, as high as 78.5% of patients with SLE [21]. As this cohort was retrieved from a Medicaid database, it encompasses mainly individuals with low-income, which represents a population with higher risk to visit the ED than the general population [32, 33]. Our findings showed that 13% of ED visits among patients with SLE were followed by hospital admission, with a risk to be hospitalized 2.5-fold more than comparators without SLE. A Mexican single-center study reported that 37.2% of the 180 patients with SLE visiting ED were then hospitalized [34]. However, that study reported only one ED visit per patient, did not report repeated visits, explaining the difference with our results.
We found that of hospitalizations among patients with SLE, 32% resulted in readmission, defined as subsequent hospitalization in the 30 days after a distinct discharge from hospital. Other studies have described lower readmission rates, 6% to 17% [10, 11]. However, those prior studies calculated readmissions among all hospitalizations as denominator, while we excluded the first hospitalization of each patient from the denominator.
Strengths of our study include a population-based cohort with matched comparators from the same population. With data collected until December 2020, our results are representative of the current status of healthcare utilization in SLE. Our study depicts a thorough and comprehensive picture of the inpatient course of patients with SLE, from the ED visit to hospital admission, discharge, and readmissions. This study was performed using the latest SLE classification criteria [16], manually ascertained, which decreases misclassification bias. Finally, the manual reviewing of every hospitalization diagnosis allowed the minimization of misclassification inherent to billing codes. Manual review allowed the use of a diagnosis classification based on the Clinical Classifications Software (CCS), key to classify SLE flares and diseases related to SLE involvement as a standalone category.
Our study is not without limitations. First, the upper Midwest of the USA is predominantly non-Hispanic White. SLE is a disease with higher prevalence in Black Americans, American Indians, Asian Americans, and Hispanic people [2, 35], and our findings may not be generalizable to areas with higher proportion of minorities. Second, given that the data is limited to the 27-County area, there is a potential underestimation of hospitalizations if patients were hospitalized outside the REP area. Thirdly, although causes of hospitalizations are usually multifactorial, it was necessary for the purpose of this study to be unambiguous while classifying reasons of hospitalization. Thus, we chose to limit reasons of hospitalization to the primary diagnosis at discharge, though admissions could involve several organs or systems.
In conclusion, patients with SLE have a higher risk of hospitalization than individuals without SLE. Risk of first hospitalization is increased by 2.5-fold and risk of hospitalization is significantly elevated for both sexes, all ages and races, and for the first 15 years of SLE evolution after diagnosis. Patients with SLE are by 2.7-fold more likely to encounter a first ED visit than the general population and are more likely to be hospitalized following an ED visit. Readmissions also occur more frequently. Studies that attempt to clarify factors leading to hospitalization in patients with SLE and identify interventions to decrease hospitalizations may help inform efforts to decrease inpatient healthcare utilization among patients with SLE.
Supplementary Material
PRACTICAL CLINICAL MESSAGES.
Patients with SLE are 2–3 times more likely to visit the emergency department and be hospitalized than the general population.
The three most frequent causes of hospitalization were infections, cardiovascular disease and SLE flares. The in-hospital mortality and discharge sites were similar between patients with SLE and comparators.
The increased risk of hospitalization in patients with SLE, persists during the first 15 years of the disease and after 15 years is similar to the general population.
Inpatient healthcare utilization for SLE remains elevated in 2020. Interventions can decrease preventable hospitalizations.
Acknowledgments:
To Barb Abbott & Maria Mendoza.
Funding Information:
The Lupus Midwest Network (LUMEN) project is supported by the Centers for Disease Control and Prevention of the U.S. Department of Health and Human Services (HHS) under Grant number U01 DP006491 as part of a financial assistance award totaling $1,750,000 with 100 percent funded by CDC/HHS.
This study used the resources of the Rochester Epidemiology Project (REP) medical records-linkage system, which is supported by the National Institute on Aging (NIA; AG 058738), by the Mayo Clinic Research Committee, and by fees paid annually by REP users. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC or the National Institutes of Health.
Alí Duarte-García is supported by the Rheumatology Research Foundation Scientist Development Award and the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery.
Footnotes
Competing Interests: None declared.
REFERENCES
- 1.Tsokos GC. Systemic lupus erythematosus. N Engl J Med. 2011;365(22):2110–21. [DOI] [PubMed] [Google Scholar]
- 2.Izmirly PM, Parton H, Wang L, McCune WJ, Lim SS, Drenkard C, et al. Prevalence of systemic lupus erythematosus in the United States: estimates from a meta-analysis of the Centers for Disease Control and Prevention National Lupus Registries. Arthritis Rheumatol. 2021;73(6):991–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yen EY, Shaheen M, Woo JMP, Mercer N, Li N, McCurdy DK, et al. 46-year trends in systemic lupus erythematosus mortality in the United States, 1968 to 2013: a nationwide population-based study. Ann Intern Med. 2017;167(11):777–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barber MRW, Drenkard C, Falasinnu T, Hoi A, Mak A, Kow NY, et al. Global epidemiology of systemic lupus erythematosus. Nat Rev Rheumatol. 2021;17(9):515–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuo CF, Chou IJ, Rees F, Grainge MJ, Lanyon P, Davenport G, et al. Temporal relationships between systemic lupus erythematosus and comorbidities. Rheumatology (Oxford). 2019;58(5):840–8. [DOI] [PubMed] [Google Scholar]
- 6.Chiu YM, Lai CH. Nationwide population-based epidemiologic study of systemic lupus erythematosus in Taiwan. Lupus. 2010;19(10):1250–5. [DOI] [PubMed] [Google Scholar]
- 7.Dhital R, Pandey RK, Poudel DR, Oladunjoye O, Paudel P, Karmacharya P. All-cause hospitalizations and mortality in systemic lupus erythematosus in the US: results from a national inpatient database. Rheumatol Int. 2020;40(3):393–7. [DOI] [PubMed] [Google Scholar]
- 8.Busch RW, Kay SD, Voss A. Hospitalizations among Danish SLE patients: a prospective study on incidence, causes of admission and risk factors in a population-based cohort. Lupus. 2018;27(1):165–71. [DOI] [PubMed] [Google Scholar]
- 9.Gu K, Gladman DD, Su J, Urowitz MB. Hospitalizations in patients with systemic lupus erythematosus in an academic health science center. J Rheumatol. 2017;44(8):1173–8. [DOI] [PubMed] [Google Scholar]
- 10.Rosa GPD, Ortega MF, Teixeira A, Espinosa G, Cervera R. Causes and factors related to hospitalizations in patients with systemic lupus erythematosus: analysis of a 20-year period (1995–2015) from a single referral centre in Catalonia. Lupus. 2019;28(9):1158–66. [DOI] [PubMed] [Google Scholar]
- 11.Yazdany J, Marafino BJ, Dean ML, Bardach NS, Duseja R, Ward MM, et al. Thirty-day hospital readmissions in systemic lupus erythematosus: predictors and hospital- and state-level variation. Arthritis Rheumatol. 2014;66(10):2828–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiology Project. Am J Epidemiol. 2011;173(9):1059–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rocca WA, Grossardt BR, Brue SM, Bock-Goodner CM, Chamberlain AM, Wilson PM, et al. Data resource profile: Expansion of the Rochester Epidemiology Project medical records-linkage system (E-REP). Int J Epidemiol. 2018;47(2):368–j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Pankratz JJ, Brue SM, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41(6):1614–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R, et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 2019;71(9):1400–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duarte-Garcia A, Hocaoglu M, Osei-Onomah SA, Dabit JY, Giblon RE, Helmick CG, et al. Population-based incidence and time to classification of systemic lupus erythematosus by three different classification criteria. Rheumatology (Oxford). 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. [DOI] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality R, MD. Clinical Classifications Software Refined (CCSR). Healthcare Cost and Utilization Project (HCUP). 2021. Available at: www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp. Accessed January, 2022. [Google Scholar]
- 20.Hoi A Asian lupus in a multi-ethnic society: what can be learnt? Int J Rheum Dis. 2015;18(2):113–6. [DOI] [PubMed] [Google Scholar]
- 21.Kan HJ, Song X, Johnson BH, Bechtel B, O’Sullivan D, Molta CT. Healthcare utilization and costs of systemic lupus erythematosus in Medicaid. Biomed Res Int. 2013;2013:808391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liang H, Pan HF, Tao JH, Ye DQ. Causes and factors associated with frequent hospitalization in Chinese patients with systemic lupus erythematosus: an ambispective cohort study. Med Sci Monit. 2019;25:8061–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JW, Park DJ, Kang JH, Choi SE, Yim YR, Kim JE, et al. The rate of and risk factors for frequent hospitalization in systemic lupus erythematosus: results from the Korean lupus network registry. Lupus. 2016;25(13):1412–9. [DOI] [PubMed] [Google Scholar]
- 24.Yelin E, Trupin L, Katz P, Criswell LA, Yazdany J, Gillis J, et al. Impact of health maintenance organizations and fee-for-service on health care utilization among people with systemic lupus erythematosus. Arthritis Rheum. 2007;57(3):508–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garris C, Jhingran P, Bass D, Engel-Nitz NM, Riedel A, Dennis G. Healthcare utilization and cost of systemic lupus erythematosus in a US managed care health plan. J Med Econ. 2013;16(5):667–77. [DOI] [PubMed] [Google Scholar]
- 26.Hanly JG, Thompson K, Skedgel C. Utilization of ambulatory physician encounters, emergency room visits, and hospitalizations by systemic lupus erythematosus patients: a 13-year population health study. Arthritis Care Res (Hoboken). 2016;68(8):1128–34. [DOI] [PubMed] [Google Scholar]
- 27.Levy O, Markov A, Drob Y, Maslakov I, Tishler M, Amit-Vazina M. All-cause hospitalizations in systemic lupus erythematosus from a single medical center in Israel. Rheumatol Int. 2018;38(10):1841–6. [DOI] [PubMed] [Google Scholar]
- 28.Lee J, Dhillon N, Pope J. All-cause hospitalizations in systemic lupus erythematosus from a large Canadian referral centre. Rheumatology (Oxford). 2013;52(5):905–9. [DOI] [PubMed] [Google Scholar]
- 29.Piga M, Casula L, Perra D, Sanna S, Floris A, Antonelli A, et al. Population-based analysis of hospitalizations in a West-European region revealed major changes in hospital utilization for patients with systemic lupus erythematosus over the period 2001–2012. Lupus. 2016;25(1):28–37. [DOI] [PubMed] [Google Scholar]
- 30.OECD. Health at a Glance 2019. 2019. Available at: https://www.oecd-ilibrary.org/content/publication/4dd50c09-en.
- 31.Hannah JR, D’Cruz DP. Pulmonary complications of systemic lupus erythematosus. Semin Respir Crit Care Med. 2019;40(2):227–34. [DOI] [PubMed] [Google Scholar]
- 32.Carlson LC, Kim J, Samuels-Kalow ME, Yun BJ, Terry DF, Weilburg JB, et al. Comparing neighborhood-based indices of socioeconomic risk factors and potentially preventable emergency department utilization. Am J Emerg Med. 2021;44:213–9. [DOI] [PubMed] [Google Scholar]
- 33.Trends in the utilization of emergency department services, 2009–2018. U.S. Department of Health and Human Services ; Office of the Assistant Secretary for Planning and Evaluation; 2021. Available at: https://aspe.hhs.gov/reports/trends-utilization-emergency-department-services-2009-2018. Accessed January, 2022. [Google Scholar]
- 34.Rojas-Serrano J, Cardiel MH. Lupus patients in an emergency unit. Causes of consultation, hospitalization and outcome. A cohort study. Lupus. 2000;9(8):601–6. [DOI] [PubMed] [Google Scholar]
- 35.Rees F, Doherty M, Grainge M, Davenport G, Lanyon P, Zhang W. The incidence and prevalence of systemic lupus erythematosus in the UK, 1999–2012. Ann Rheum Dis. 2016;75(1):136–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


