Abstract
Background
Post COVID-19 syndrome, also known as "Long COVID," is a complex and multifaceted condition that affects individuals who have recovered from SARS-CoV-2 infection. This systematic review and meta-analysis aim to comprehensively assess the global prevalence of depression, anxiety, and sleep disorder in individuals coping with Post COVID-19 syndrome.
Methods
A rigorous search of electronic databases was conducted to identify original studies until 24 January 2023. The inclusion criteria comprised studies employing previously validated assessment tools for depression, anxiety, and sleep disorders, reporting prevalence rates, and encompassing patients of all age groups and geographical regions for subgroup analysis Random effects model was utilized for the meta-analysis. Meta-regression analysis was done.
Results
The pooled prevalence of depression and anxiety among patients coping with Post COVID-19 syndrome was estimated to be 23% (95% CI: 20%—26%; I2 = 99.9%) based on data from 143 studies with 7,782,124 participants and 132 studies with 9,320,687 participants, respectively. The pooled prevalence of sleep disorder among these patients, derived from 27 studies with 15,362 participants, was estimated to be 45% (95% CI: 37%—53%; I2 = 98.7%). Subgroup analyses based on geographical regions and assessment scales revealed significant variations in prevalence rates. Meta-regression analysis showed significant correlations between the prevalence and total sample size of studies, the age of participants, and the percentage of male participants. Publication bias was assessed using Doi plot visualization and the Peters test, revealing a potential source of publication bias for depression (p = 0.0085) and sleep disorder (p = 0.02). However, no evidence of publication bias was found for anxiety (p = 0.11).
Conclusion
This systematic review and meta-analysis demonstrate a considerable burden of mental health issues, including depression, anxiety, and sleep disorders, among individuals recovering from COVID-19. The findings emphasize the need for comprehensive mental health support and tailored interventions for patients experiencing persistent symptoms after COVID-19 recovery.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-023-05481-6.
Keywords: Post COVID-19 syndrome, Long COVID, Depression, Anxiety, Sleep disorder, Prevalence, Systematic review, Meta-analysis
Introduction
The ongoing COVID-19 pandemic has precipitated a worldwide health catastrophe, impacting not only the physical health of those infected but also their emotional stability [1]. Post-COVID-19 syndrome, which pertains to the persistence of symptoms beyond the expected recovery period, has become a burgeoning concern and has been correlated with the emergence of mental health afflictions such as depression and anxiety [2]. According to the National Institute for Health and Care Excellence (NICE), "post-COVID-19 syndrome" (PCS) is a complex set of symptoms that emerge during or after a COVID-19 infection, lasting for a minimum of 12 weeks, and cannot be explained by alternative diagnoses. PCS often presents with various clusters of symptoms that can change over time and impact multiple systems in the body. These symptoms may overlap and may fluctuate in severity [3]. This development underscores the necessity of additional research into the correlation between post-COVID-19 syndrome and mental health, as well as the urgency of addressing the emotional needs of those affected by the virus.
Research has established that individuals with post-COVID-19 syndrome are more susceptible to depression and anxiety. Around 30 to 40% of individuals who have recovered from COVID-19 have been reported for experiencing symptoms such as anxiety, depression, sleep issues, and post-traumatic stress disorder, which is similar to what has been observed in survivors of other coronaviruses [4].
The exact mechanisms by which post-COVID-19 syndrome contributes to the development of depression and anxiety remain unclear. However, it is theorized that the physical and psychological stress caused by the illness may play a role. For instance, the extended nature of the illness and the uncertainty of its outcome can engender feelings of hopelessness and frustration. Post-COVID-19 syndrome often entails persistent physical symptoms such as fatigue, respiratory difficulties, and muscle and joint pain, which can severely impact quality of life and daily functioning [5]. Additionally, the social and economic ramifications of the pandemic may exacerbate these feelings, with many individuals facing job loss, financial insecurity, and social isolation [6]. On the other hand, mechanisms originated from the immune system might play a role. Dysregulations in the immune responses, thrombosis in cerebral microvasculature, neuroanatomical alterations, and adverse effects of drugs administered during the disease potentially predispose the patients to neuropsychiatric complications [7, 8].
Considering the high rates of mental disorders linked to post-COVID-19 syndrome, it is imperative to conduct further research to comprehend the mechanisms by which the illness may be contributing to these mental health conditions. This will facilitate healthcare providers in developing more effective interventions and treatments for those affected by post-COVID-19 syndrome.
The COVID-19 pandemic has inflicted a considerable toll on the mental health of individuals, particularly those affected by post-COVID-19 syndrome. Elucidating the unprecedented aspects of this issue provides healthcare providers with adequate knowledge to mitigate the negative impact of post-COVID-19 syndrome on mental health and enhance the quality of life for those affected by the illness. The strong association between post-COVID-19 syndrome and depression, anxiety, and sleep disturbances emphasizes the importance of further research on this subject and the necessity of evaluating the extent of this interplay. Therefore, we conducted a thorough systematic review and meta-analysis to address this issue by investigating the incidence of mental disorders among patients experiencing post-COVID-19 syndrome.
Methods
The present systematic review was conducted based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and guideline retrieved from the Cochrane Handbook for Systematic Reviews of Interventions [9, 10]. The protocol of this review was prospectively registered on PROSPERO with the following registration code: CRD42023413023.
Search strategy
We performed a comprehensive database search in PubMed, Scopus, Embase, and Web of science up to 24 January 2023, using the search string with the combination of following keywords: post-acute covid-19 syndrome, long covid-19 syndrome, COVID-19 survivors, COVID-19 sequelae, depression, anxiety, sleep, and prevalence (Supplementary File). No limitation was implemented on our search results.
Eligibility criteria
The inclusion criteria definition was: 1) Population: patients who were recovered from SARS-CoV-2 in their past medical history; 2) Assessment: previously validated measurements for depression, anxiety, and sleep scales; 3) Comparison: not applicable; 4) Outcome: reported the prevalence rate; 5) Type of Study: all types of original studies. There was no limitation on date and the language of the published report. Case report studies, review studies, meta-analyses, commentary studies, and letter to editor articles without any relevant data were excluded.
Screening and data extraction
Two-step screening were performed by our reviewers. Disagreements were resolved by the third reviewer (A.S.). Data were extracted on an Excel spreadsheet. The extracted data included Author, Year, Country, Population, Total patients, Assessment scales, Cut-offs, and depression, anxiety, and sleep disorders prevalence.
Quality assessment
Four reviewers independently evaluated the included studies using the Newcastle–Ottawa Quality Assessment [11]. The studies with 7 or more yeses are rated as “Good”, 5–6 as “Fair”, and with 4 or fewer as “Poor" quality report.
Synthesis
We conducted a meta-analysis using a proportion random effects model to estimate the prevalence of depression, anxiety, and sleep disorder. Given the diverse study populations and methods, we used a random effects model to summarize the prevalence, presenting proportions and 95% confidence intervals (95% CI). To assess heterogeneity, we utilized the Cochrane Q-test and I2 statistic, considering I2 values higher than 75% as high levels of heterogeneity. We evaluated publication bias using Doi plot visualization and Peters test [12, 13]. Conducting a subgroup analysis, we categorized studies based on their geographical region, and assessment measure used. Additionally, we examined the moderating effect of factors such as year of publication, sample size, age, and percentage of male participants through conducting a meta-regression analysis. All statistical analyses and graphical representations were performed using STATA, R (version 4.1.3) and the meta package (version 5.5) [14].
Results
Characteristics
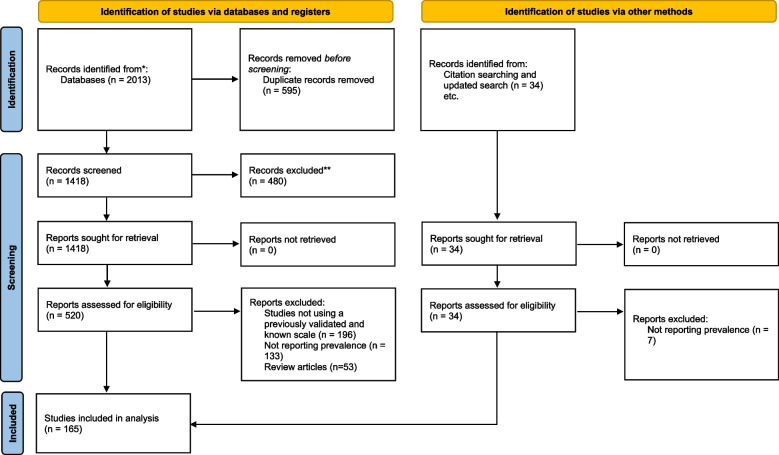
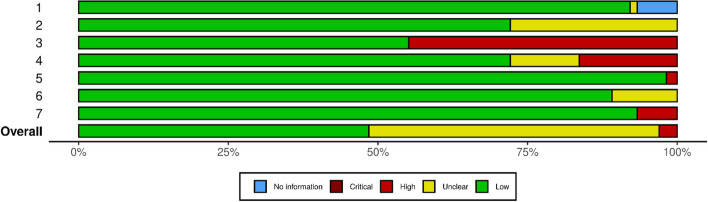
After examining a total of 2013 records, 165 studies with 9,923,461 total patients were included in our review [15–179] (Fig. 1). Eighty of the studies were designed in cohort [87–166], 71 cross-sectional [16–86], 7 case control [167–173], 4 survey study [174, 176–178], 1 randomized clinical trial [15] and 2 secondary analysis [175, 179]. Included studies were published between 2019–2023. The most common assessment scales used for depression diagnosis were BDI, DASS, HADS, PHQ, and for anxiety were GAD, HADS-A, and for sleep disorders were PSQI. We assessed the risk of bias for each study using the quality assessment checklist based on Newcastle–Ottawa Scale. Based on the results of our quality assessment, there were 81 studies with good, 79 with fair and 5 with poor methodological quality. Detailed characteristics of each study and its quality assessment are provided in Supplementary File (Fig. 2).
Fig. 1.
PRISMA flow diagram
Fig. 2.
Results of quality assessment
Prevalence of depression
Data from 143 studies with 7,782,124 participants reporting the relevant outcome were included. The pooled prevalence of depression among patients coping with Post COVID-19 syndrome was estimated to be 23% (95% CI: 20%—26%; I2 = 99.9%) (Supplementary Fig. 1). Subgroup analysis based on geographical regions and assessment scales showed a significant between-subgroup differences (Table 1).
Table 1.
Results of meta-analysis
| Outcome | No. of studies | Prevalence | [95% Confidence interval] | I2 |
|---|---|---|---|---|
| Depression | 142 | 23% | 20% - 26% | 99% |
| Anxiety | 131 | 23% | 20% - 26% | 99% |
| Sleep disorder | 27 | 45% | 37% - 53% | 98% |
Prevalence of anxiety
Data from 132 studies with 9,320,687 participants reporting the relevant outcome were included. The pooled prevalence of anxiety among patients coping with Post COVID-19 syndrome was estimated to be 23% (95% CI: 20%—26%; I2 = 99.9%) (Supplementary Fig. 2). Subgroup analysis based on geographical regions and assessment scales showed a significant between-subgroup differences (Table 1).
Prevalence of sleep disorder
Data from 27 studies with 15,362 participants reporting the relevant outcome were included. The pooled prevalence of sleep disorder among patients coping with Post COVID-19 syndrome was estimated to be 45% (95% CI: 37%—53%; I2 = 98.7%) (Supplementary Fig. 3). Subgroup analysis based on geographical regions and assessment scales showed a significant between-subgroup differences (Table 1).
Meta-regression analysis
A meta-regression analysis was performed to examine the potential moderating effects of factors such as year of publication, sample size, age, and percentage of male participants. The results of meta-regression showed significant correlation between the prevalence of 1) depression and total sample size and male percentage of the included studies; 2) anxiety and total sample size of the included studies; and 3) sleep disorder and age and male percentage of the included studies (Table 2).
Table 2.
Results of meta-regression
| Coefficient | Standard error | P >|z| | 95% CI | |
|---|---|---|---|---|
| Depression | ||||
| Year | -0.04 | 0.06 | 0.46 | -0.15 to 0.07 |
| Total | -1.36e-07 | 5.09e-08 | 0.008 | -2.35e-07 to -3.58e-08 |
| Age | -0.003 | 0.003 | 0.32 | -0.009 to 0.003 |
| Male (%) | -0.005 | 0.002 | 0.02 | |
| Anxiety | ||||
| Year | 0.02 | 0.06 | 0.77 | -0.10 to .014 |
| Total | -1.00e-07 | 5.08e-08 | 0.04 | -2.00e-07 to -6.40e-10 |
| Age | -0.001 | 0.003 | 0.66 | -0.008 to 0.005 |
| Male (%) | -0.0003 | 0.0009 | 0.72 | -0.002 to 0.001 |
| Sleep disorder | ||||
| Year | -0.19 | 0.13 | 0.14 | -0.46 to 0.06 |
| Total | -.00007 | .00005 | 0.17 | -0.00017 to 0.00003 |
| Age | 0.03 | 0.01 | 0.01 | 0.006 to 0.049 |
| Male (%) | -0.011 | 0.005 | 0.04 | -0.0229 to -0.0003 |
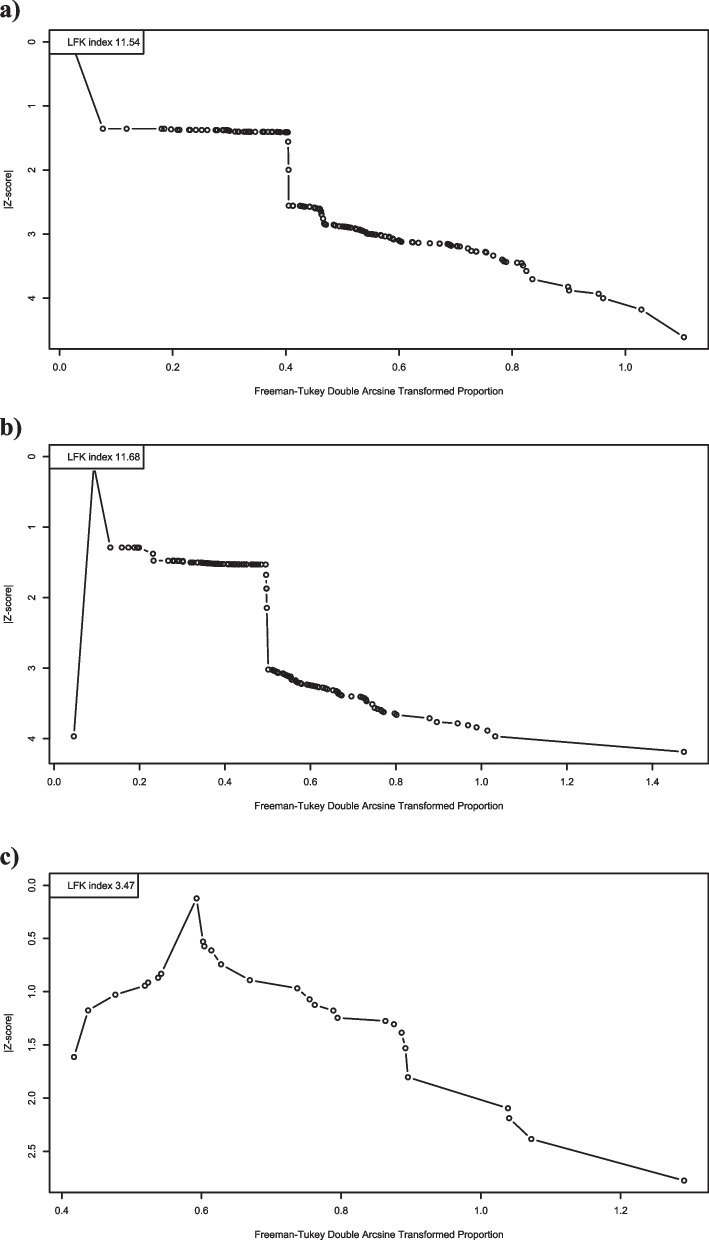
Publication bias
Publication bias was assessed using Doi plot visualization and Peters test. The results showed a significant source of possible publication bias based on peters test for depression (p = 0.0085) and sleep disorder (p = 0.02). There were no sources of publication bias for anxiety (p = 0.11). The Doi plots are presented in Fig. 3.
Fig. 3.
Doi plots for the prevalence of a) depression; b) anxiety; and c) sleep disorder
Discussion
To the best of our knowledge, this systematic review and meta-analysis represents the most comprehensive and wide-ranged investigation of depression, anxiety, and sleep disorders among long COVID patients. The primary objective of this study was to provide an updated and accurate evaluation of the prevalence rates of these mental health conditions by analyzing data from 66 studies. The findings from our study indicated that COVID-19 patients have a general prevalence of 23% for depression, 23% for anxiety, and 37% for sleep disturbances.
Assessing the prevalence of mental disorders such as depression, anxiety, and sleep disturbance among individuals with the post-COVID syndrome is crucial for comprehending the complete impact of the COVID-19 pandemic on mental health as it is an ongoing global health crisis. While much of the focus has been on physical symptoms and outcomes, there is a growing recognition of the impact that COVID-19 can have on mental health. This information is paramount for designing targeted interventions aimed at promoting the mental well-being of post-COVID syndrome patients and for identifying individuals who may be at greater risk of developing mental health conditions. Furthermore, evaluating the incidence of mental disorders can furnish valuable data for public health officials in their efforts to mitigate the overall effect of the pandemic on mental health. By evaluating and addressing the incidence of mental disorders among individuals with post-COVID syndrome, healthcare professionals can work towards improving patient outcomes and ensuring that those affected receive the necessary care and support to manage their symptoms and attain complete recovery. Understanding the prevalence and risk factors associated with these conditions is important for developing effective interventions and support for individuals affected by COVID-19, both in the short and long term.
The typical duration for recovery from COVID-19 ranges from 2 to 3 weeks, contingent upon the severity of the symptoms. However, there is still a lack of agreement regarding the appropriate definitions for scenarios in which COVID-19 symptoms persist beyond the acute phase of the infection [180]. The term "Long COVID" is commonly used to describe the condition of individuals who have recuperated from COVID-19, but exhibit persistent symptoms beyond the expected recovery period [181]. Previous research is increasingly providing evidence to suggest that a considerable percentage of individuals who have survived COVID-19 are prone to a variety of physical and psychological symptoms that persist or even emerge several months after the initial infection [182, 183]. Neuropsychiatric symptoms, such as depression, anxiety, post-traumatic stress disorder (PTSD), sleep disturbances, fatigue, and cognitive deficits, have been reported commonly within the studies investigating long COVID [184].
Initially, research was centered on analyzing the psychosocial reaction to the COVID-19 pandemic and the effects of various preventive measures, including lockdowns, school closures, and travel restrictions, on the mental health outcomes of the general population. However, recent studies have expanded this scope to include not only the effects of pandemic-related circumstances but also the impact of COVID-19 as a debilitating disease [185, 186].
Several risk factors have been identified for mental disorders related to long COVID. These risk factors can be classified into several categories, such as demographic factors, clinical factors, and environmental factors. Demographic factors that have been associated with an increased risk of mental disorders in "long COVID" patients include older age, female gender, socioeconomic status, and pre-existing mental health conditions [180, 187, 188]. Clinical factors, such as the severity of the initial COVID-19 infection [189, 190], medical comorbidities [191], hospital admission, and a greater load of symptoms both during the acute phase of the infection and after discharge have also been identified as risk factors for mental disorders [192]. Environmental factors, such as the death of family members due to COVID-19, social distancing, and quarantine, may also increase the risk of mental health problems among long COVID patients [193]. The factors that have been identified as playing a role in determining the extent of mental health problems can be employed to screen individuals who have contracted COVID-19. This screening can facilitate the provision of timely interventions to those who continue to experience post-COVID symptoms, particularly with respect to mental health.
The underlying mechanisms responsible for depression, anxiety, and sleep disturbances among long COVID patients is a complex and multifaceted process that is not yet fully understood. Previous studies on the pathophysiology of these conditions suggest that the viral infection can directly impact the central nervous system, leading to the development of psychiatric symptoms. This process is probably caused by the invasion of the virus into the CNS and the subsequent neuronal damages including demyelination and neurodegeneration [194, 195]. Furthermore, the high levels of proinflammatory cytokines during COVID-19 have been shown to cause an increase in neuroinflammatory response, which can lead to a disruption in neurotransmitter activity and the development of mood disorders such as depression and anxiety [196]. Additionally, the inflammatory response to COVID-19 can lead to oxidative stress and mitochondrial dysfunction, which can further exacerbate neuropsychiatric symptoms [197]. Another explanation is that ischemia caused by microvascular dysfunction and thrombosis could lead to the formation of several small cerebral infarctions, resulting in persistent neurological impairment [198].
The prevalence of mental health disorders among long COVID survivors emphasizes the need for community-level interventions to promote mental health and well-being. it is evident that the care of COVID-19 patients extends beyond hospital discharge, and interdisciplinary collaboration is necessary for comprehensive outpatient care to ensure that long COVID patients who require mental health support have access to appropriate services. Physicians and healthcare workers should inform patients, particularly those in high-risk groups, of the potential long-term effects of COVID-19 and encourage them to seek medical care for any developing conditions. Healthcare providers and public health officials must work collaboratively to reduce the stigma associated with mental health issues and promote access to mental health resources and support groups. This approach will ensure that individuals with long COVID receive the necessary care and support to effectively manage their mental health.
The current study possesses strengths that contribute to the robustness of our findings and their potential implications for the field. We employed a comprehensive search protocol that encompassed all the relevant studies related to our outcomes, which ensured that our analysis was comprehensive and not limited to specific regions or countries. Additionally, we included a diverse sample of participants with varied demographic characteristics in our analysis, which increases the generalizability of our findings.
The results of our studies should be interpreted in the context of some limitations. The results obtained from studies showed a high level of heterogeneity. Moreover, the included studies were observational, therefore a causal relationship could not be established based on these findings. Furthermore, most of the studies did not include an unexposed control group making it challenging to conclude that mental disorders are direct consequences of the disease rather than the socioeconomic impacts of the pandemic. One of the limitations is the inconsistency in the definition of the long COVID timeframe employed in the different studies included in our analysis. Moreover, the identification and diagnosis of mental health disorders examined in our study relied on questionnaires that varied between the included studies. While we have conducted a comprehensive analysis based on the existing evidence regarding the prevalence of the three primary psychiatric manifestations in individuals grappling with long COVID, it is essential to highlight a critical aspect. Studies should take into account the hospitalization rates of patients and continue to monitor these individuals to determine whether those with more severe disease are more likely to experience long COVID [199]. It is worth noting that this aspect has often been overlooked, primarily due to the predominantly cross-sectional nature of most studies on this subject. Therefore, there is a compelling need for future longitudinal studies with adequate follow-up to delve deeper into this specific topic and provide a more comprehensive understanding of the relationship between disease severity, hospitalization, and the occurrence of long COVID. syndrome Altogether, these limitations may affect the comparability of the findings from different studies and the accuracy of our findings.
In conclusion, our results revealed higher rates of mental health conditions among long COVID patients than in the general population. This information is critical for designing interventions aimed at promoting the mental well-being of post-COVID syndrome patients, identifying high-risk individuals, and mitigating the overall effect of the pandemic on mental health. Further research should focus on identifying the specific mechanisms responsible for the development of mental health conditions among long COVID patients, as well as evaluating the effectiveness of interventions aimed at promoting mental well-being. Additionally, community-level interventions are necessary to promote mental health and well-being among long COVID survivors.
Supplementary Information
Additional file 1: Supplementary Table 1. PRISMA 2020 checklist. Supplementary Table 2. Search strategies for online databases. Supplementary Table 3. Characteristics of the included studies. Supplementary Fig 1. Risk of bias assessment for each included study.
Acknowledgements
We would like to extend our thanks to the Clinical Research Development Unit of Imam Ali hospital, Karaj, Iran.
Author’ contributions
N.S, M.J, M.B: Project Administration, Data curation, Writing – Review & Editing A.S: Conceptualization, Validation, Resources, Methodology, Software, Formal analysis, Visualization, Writing – Original Draft M.T, O.S, P.F, A.E, O.R, AH.S, : Data curation, Writing- Original Draft H.S, M.H, F.SA, A.A, B.J, MR.M: Data curation.
Funding
This study did not receive funding, grant, or sponsorship from any individuals or organizations.
Availability of data and materials
All data has been presented in the manuscript.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Arman Shafiee, Email: armanshafieemd@gmail.com.
Mahmood Bakhtiyari, Email: mahmood.bakhtiyari@ymail.com.
References
- 1.Luo M, Guo L, Yu M, Jiang W, Wang HJPr HJPr. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–a systematic review and meta-analysis. Psychiatry Res. 2019;2020(291):113190. doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carfì A, Bernabei R, Landi FJJ. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Health NIf, Excellence C . COVID-19 Rapid Guideline: NICE. 2021. [PubMed] [Google Scholar]
- 4.Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garrigues E, Janvier P, Kherabi Y, Le Bot A, Hamon A, Gouze H, et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020;81(6):e4–e6. doi: 10.1016/j.jinf.2020.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whiteside DM, Basso MR, Naini SM, Porter J, Holker E, Waldron EJ, et al. Outcomes in post-acute sequelae of COVID-19 (PASC) at 6 months post-infection part 1: cognitive functioning. Clin Neuropsychol. 2022;36(4):806–828. doi: 10.1080/13854046.2022.2030412. [DOI] [PubMed] [Google Scholar]
- 7.Lee MH, Perl DP, Nair G, Li W, Maric D, Murray H, et al. Microvascular injury in the brains of patients with Covid-19. N Engl J Med. 2021;384(5):481–483. doi: 10.1056/NEJMc2033369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, Lange F, et al. Brain imaging before and after COVID-19 in UK Biobank. 2021:2021.06.11.21258690.
- 9.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10(10.1002):14651858. doi: 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14(1):45. doi: 10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295(6):676–680. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- 13.Hunter JP, Saratzis A, Sutton AJ, Boucher RH, Sayers RD, Bown MJ. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol. 2014;67(8):897–903. doi: 10.1016/j.jclinepi.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Harrer M, Cuijpers P, Furukawa T, Ebert D. Doing Meta-Analysis with R: A Hands-On Guide. 2021. [Google Scholar]
- 15.Vlake JH, van Bommel J, Wils EJ, Bienvenu J, Hellemons ME, Korevaar TI, et al. Intensive care unit-specific virtual reality for critically Ill patients with COVID-19: multicenter randomized controlled trial. J Med Internet Res. 2022;24(1):e32368. 10.2196/32368. [DOI] [PMC free article] [PubMed]
- 16.Ahmed GK, Khedr EM, Hamad DA, Meshref TS, Hashem MM, Aly MM. Long term impact of Covid-19 infection on sleep and mental health: a cross-sectional study. Psychiatry Res. 2021;305:114243. doi: 10.1016/j.psychres.2021.114243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ajmi S, Masmoudi R, Sallemi R, Feki I, Masmoudi J. Anxiety, depression and post-traumatic stress symptoms among COVID-19 survivors in Tunis. Eur Psychiatry. 2022;65:S527. doi: 10.1192/j.eurpsy.2022.1344. [DOI] [Google Scholar]
- 18.Akçay E, Çöp E, Dinç GS, Göker Z, Parlakay AÖ, Demirel BD, et al. Loneliness, internalizing symptoms, and inflammatory markers in adolescent COVID-19 survivors. Child Care Health Dev. 2022;48(6):1112–1121. doi: 10.1111/cch.13043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Albu S, Zozaya NR, Murillo N, Garciá-Molina A, Chacón CAF, Kumru H. What's going on following acute COVID-19? clinical characteristics of patients in an out-patient rehabilitation program. NeuroRehabilitation. 2021;48(4):469–480. doi: 10.3233/NRE-210025. [DOI] [PubMed] [Google Scholar]
- 20.Ali AM, Alkhamees AA, Hori H, Kim Y, Kunugi H. The depression anxiety stress scale 21: development and validation of the depression anxiety stress scale 8-item in psychiatric patients and the general public for easier mental health measurement in a post COVID-19 world. Int J Environ Res Public Health. 2021;18(19):10142. doi: 10.3390/ijerph181910142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anik AI, Ahmed T, Nandonik AJ, Parvez A, Das Pooja S, Kabir ZN. Evidence of mental health-related morbidities and its association with socio-economic status among previously hospitalized patients with symptoms of COVID-19 in Bangladesh. Front Public Health. 2023;11:1132136. doi: 10.3389/fpubh.2023.1132136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bahadur A, Mundhra R, Sharma S, Ajmani M, Zaman R, Chaturvedi J. Psychological distress and post-COVID sequelae in postpartum females after clinically stable COVID-19 infections: a single-center observational study from India. Int J Appl Basic Med Res. 2022;12(3):185–188. doi: 10.4103/ijabmr.ijabmr_173_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braga LW, Oliveira SB, Moreira AS, Pereira ME, Carneiro VS, Serio AS, et al. Neuropsychological manifestations of long COVID in hospitalized and non-hospitalized brazilian patients. NeuroRehabilitation. 2022;50(4):391–400. doi: 10.3233/NRE-228020. [DOI] [PubMed] [Google Scholar]
- 24.Bungenberg J, Humkamp K, Hohenfeld C, Rust MI, Ermis U, Dreher M, et al. Long COVID-19: objectifying most self-reported neurological symptoms. Ann Clin Transl Neurol. 2022;9(2):141–154. doi: 10.1002/acn3.51496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campo-Arias A, Pedrozo-Pupo JC, Herazo E. Post-traumatic Stress Risk among COVID-19 Survivors in Colombia. 2021. [Google Scholar]
- 26.Cansei N, Tetik BK, Demir GH, Kurt O, Evren B, Yiicel A. Assessment of psychological responses and related factors of discharged patients who have been hospitalized with covid-19. Psychiatr Danub. 2021;33(4):611–619. doi: 10.24869/psyd.2021.611. [DOI] [PubMed] [Google Scholar]
- 27.Dale LP, Cuffe SP, Kolacz J, Leon KG, Bossemeyer Biernacki N, Bhullar A, et al. Increased autonomic reactivity and mental health difficulties in COVID-19 survivors: implications for medical providers. Front Psychiatry. 2022;13:830926. doi: 10.3389/fpsyt.2022.830926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dankowski R, Sacharczuk W, Duszyńska D, Mikołajewska W, Szałek-Goralewska A, Łojko-Dankowska A, et al. Depression and anxiety in patients recently recovered from coronavirus disease (COVID-19) Neuropsychiatria i Neuropsychologia. 2021;16(1–2):11–16. doi: 10.5114/nan.2021.108028. [DOI] [Google Scholar]
- 29.Dar SA, Dar MM, Sheikh S, Haq I, Azad A, Mushtaq M, et al. Psychiatric comorbidities among COVID-19 survivors in North India: a cross-sectional study. J Educ Health Promot. 2021;10:309. doi: 10.4103/jehp.jehp_119_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dondaine T, Ruthmann F, Vuotto F, Carton L, Gelé P, Faure K, et al. Long-term cognitive impairments following COVID-19: a possible impact of hypoxia. J Neurol. 2022;269(8):3982–3989. doi: 10.1007/s00415-022-11077-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.El Hayek S, Kassir G, Zalzale H, Gonzalez-Diaz JM, Bizri M. Emerging psychiatric themes in post-COVID-19 patients on a psychiatry consultation-liaison service. Psychiatr Q. 2021;92(4):1785–1796. doi: 10.1007/s11126-021-09944-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Elmazny A, Magdy R, Hussein M, Elsebaie EH, Ali SH, Abdel Fattah AM, et al. Neuropsychiatric post-acute sequelae of COVID-19: prevalence, severity, and impact of vaccination. Eur Arch Psychiatry Clin Neurosci. 2023;273(6):1349–1358. doi: 10.1007/s00406-023-01557-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ezzelregal HG, Hassan AM, Mohamed RS, Ahmed NO. Post-COVID depression among a sample of egyptian patients and its associated factors. Egypt J Bronchol. 2021;15(1):7. doi: 10.1186/s43168-021-00086-7. [DOI] [Google Scholar]
- 34.Fernández-De-las-peñas C, Valera-Calero JA, Herrero-Montes M, Del-Valle-loarte P, Rodríguez-Rosado R, Ferrer-Pargada D, et al. The self-reported Leeds assessment of neuropathic symptoms and signs (S-LANSS) and PainDETECT questionnaires in COVID-19 survivors with post-COVID pain. Viruses. 2022;14(7):1486. doi: 10.3390/v14071486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferrando SJ, Dornbush R, Lynch S, Shahar S, Klepacz L, Karmen CL, et al. Neuropsychological, medical, and psychiatric findings after recovery from acute COVID-19: a cross-sectional study. J Acad Consult Liaison Psychiat. 2022;63(5):474–484. doi: 10.1016/j.jaclp.2022.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fu L, Fang Y, Luo D, Wang B, Xiao X, Hu Y, et al. Pre-hospital, in-hospital and post-hospital factors associated with sleep quality among COVID-19 survivors 6 months after hospital discharge: cross-sectional survey in five cities in China. BJPsych Open. 2021;7(6):e191. doi: 10.1192/bjo.2021.1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grover S, Sahoo S, Mishra E, Gill KS, Mehra A, Nehra R, et al. Fatigue, perceived stigma, self-reported cognitive deficits and psychological morbidity in patients recovered from COVID-19 infection. Asian J Psychiatr. 2021;64:102815. doi: 10.1016/j.ajp.2021.102815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hammerle MB, Sales DS, Pinheiro PG, Gouvea EG, de Almeida PIFM, de Araujo DC, et al. Cognitive complaints assessment and neuropsychiatric disorders after mild COVID-19 infection. Arch Clin Neuropsychol. 2023;38(2):196–204. doi: 10.1093/arclin/acac093. [DOI] [PubMed] [Google Scholar]
- 39.Harrison M, Briggs-Price S, Gerlis C, Gardiner N, Singh S, Daynes E. The interaction between fatigue and anxiety in people post hospitalisation with COVID-19. Physiotherapy (United Kingdom) 2022;114:e202–e203. [Google Scholar]
- 40.Hazumi M, Usuda K, Okazaki E, Kataoka M, Nishi D. Differences in the course of depression and anxiety after COVID-19 infection between recovered patients with and without a psychiatric history: a cross-sectional study. Int J Environ Res Public Health. 2022;19(18):11316. doi: 10.3390/ijerph191811316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Henneghan AM, Lewis KA, Gill E, Franco-Rocha OY, Vela RD, Medick S, et al. Describing cognitive function and psychosocial outcomes of COVID-19 survivors: a cross-sectional analysis. J Am Assoc Nurse Pract. 2021;34(3):499–508. doi: 10.1097/JXX.0000000000000647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang LQ, Xu XH, Zhang LJ, Zheng DW, Liu YT, Feng B, et al. Post-traumatic stress disorder symptoms and quality of life of COVID-19 survivors at 6-month follow-up: a cross-sectional observational study. Front Psych. 2022;12:10. doi: 10.3389/fpsyt.2021.782478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huarcaya-Victoria J, Barreto J, Aire L, Podestá A, Caqui M, Guija-Igreda R, et al. Mental health in COVID-2019 survivors from a general hospital in Peru: sociodemographic, clinical, and inflammatory variable associations. Int J Ment Health Addict. 2023;21(2):1264–1285. doi: 10.1007/s11469-021-00659-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Imran J, Nasa P, Alexander L, Upadhyay S, Alanduru V. Psychological distress among survivors of moderate-to-critical COVID-19 illness: a multicentric prospective cross-sectional study. Indian J Psychiatry. 2021;63(3):285–289. doi: 10.4103/psychiatry.IndianJPsychiatry_1074_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Islam MS, Ferdous MZ, Islam US, Mosaddek ASM, Potenza MN, Pardhan S. Treatment, persistent symptoms, and depression in people infected with covid-19 in Bangladesh. Int J Environ Res Public Health. 2021;18(4):1–16. doi: 10.3390/ijerph18041453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jafri MR, Zaheer A, Fatima S, Saleem T, Sohail A. Mental health status of COVID-19 survivors: a cross sectional study. Virol J. 2022;19(1):3. doi: 10.1186/s12985-021-01729-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kamran R, Tufail S, Raja HZ, Alvi RU, Shafique A, Saleem MN, et al. Post COVID-19 pandemic generalized anxiety status of health professional undergraduate students. Pak J Med Health Sci. 2022;16(12):144–146. [Google Scholar]
- 48.Khatun K, Farhana N. Assessment of level of depression and associated factors among COVID-19-recovered patients: a cross-sectional study. Microbiol Spectr. 2023;11(2):e0465122. doi: 10.1128/spectrum.04651-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Korkut S. Research of the coronavirus anxiety, post-traumatic stress, generalized anxiety disorder, quality of life, and stress coping styles in COVID-19 survivors. Psychol Rep. 2022;125(6):3069–3083. doi: 10.1177/00332941221129131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Larsson AC, Engwall M, Palstam A, Persson HC. Self-assessed aspects of health 3 months after COVID-19 hospitalization—A swedish cross-sectional study. Int J Environ Res Public Health. 2022;19(13):8020. doi: 10.3390/ijerph19138020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li Z, He J, Wang Y, Bai M, Zhang Y, Chen H, et al. A cross-sectional study on the mental health of patients with COVID-19 1 year after discharge in Huanggang, China. Eur Arch Psychiatry Clin Neurosci. 2022;273(2):301–310. doi: 10.1007/s00406-022-01484-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liyanage-Don N, Winawer M, Hamberger M, Agarwal S, Trainor A, Quispe K, et al. Prevalence and correlates of cognitive symptoms among patients recovering from COVID-19 illness. J Gen Intern Med. 2021;36(SUPPL 1):S24–S25. [Google Scholar]
- 53.Matsumoto K, Hamatani S, Shimizu E, Käll A, Andersson G. Impact of post-COVID conditions on mental health: a cross-sectional study in Japan and Sweden. BMC Psychiatry. 2022;22(1):237. doi: 10.1186/s12888-022-03874-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mazhari S, Sabahi A, Gilanipour H, Keshvardoost S. Agreement for diagnosis of depression and anxiety between self-assessment with e-questionnaire and psychiatric telephone interview among post-COVID-19 patients. J Educ Health Promot. 2022;11(1):6. doi: 10.4103/jehp.jehp_1519_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mendes Paranhos AC, Nazareth Dias ÁR, Da MachadoSilva LC, Vieira Hennemann Koury G, De Jesus Sousa E, Cerasi AJ, et al. Sociodemographic characteristics and comorbidities of patients with long COVID and persistent olfactory dysfunction. JAMA Netw Open. 2022;5(9):e2230637. doi: 10.1001/jamanetworkopen.2022.30637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Méndez R, Balanzá-Martínez V, Luperdi SC, Estrada I, Latorre A, González-Jiménez P, et al. Short-term neuropsychiatric outcomes and quality of life in COVID-19 survivors. J Intern Med. 2021;290(3):621–631. doi: 10.1111/joim.13262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Moy FM, Lim ERJ, Hairi NN, Bulgiba A. Depression and its associated factors among COVID-19 survivors in a middle income country. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Naik H, Shao S, Tran KC, Wong AW, Russell JA, Khor E, et al. Evaluating fatigue in patients recovering from COVID-19: validation of the fatigue severity scale and single item screening questions. Health Qual Life Outcomes. 2022;20(1):170. doi: 10.1186/s12955-022-02082-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pappa S, Barmparessou Z, Athanasiou N, Sakka E, Eleftheriou K, Patrinos S, et al. Depression, insomnia and post-traumatic stress disorder in COVID-19 survivors: role of gender and impact on quality of life. J Pers Med. 2022;12(3):486. doi: 10.3390/jpm12030486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pasin T, Dogruoz Karatekin B, Pasin O. Pain, anxiety, and quality of life of COVID-19 survivors with myofascial pain syndrome: a cross sectional study. Pain Manag Nurs. 2023;24(4):400–405. doi: 10.1016/j.pmn.2022.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pathak A, Pathak R, Gupta NR, Chopra P. Prevalence of psychiatric morbidity and their clinical correlates in patients post COVID-19: a cross-sectional study from rural northern India. J Clin Diagn Res. 2023;17(1):VC01–VC7. [Google Scholar]
- 62.Pistarini C, Fiabane E, Houdayer E, Vassallo C, Manera MR, Alemanno F. Cognitive and emotional disturbances due to COVID-19: an exploratory study in the rehabilitation setting. Front Neurol. 2021;12:643646. doi: 10.3389/fneur.2021.643646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pudlo R, Jaworska I, Szczegielniak A, Niedziela J, Kułaczkowska Z, Nowowiejska-Wiewióra A, et al. Prevalence of insomnia in the early post-COVID-19 recovery period. Int J Environ Res Public Health. 2022;19(21):14224. doi: 10.3390/ijerph192114224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Richter D, Schulze H, Charles James J, Siems N, Trampe N, Gold R, et al. Brainstem raphe hypoechogenicity is associated with depressive symptoms in long-COVID patients. Eur J Neurol. 2022;29:753. doi: 10.1007/s00415-022-11154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Richter D, Schulze H, James JC, Siems N, Trampe N, Gold R, et al. Hypoechogenicity of brainstem raphe in long-COVID syndrome–less common but independently associated with depressive symptoms: a cross-sectional study. J Neurol. 2022;269(9):4604–4610. doi: 10.1007/s00415-022-11154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Salehian R, Abdi M, Abedin MS, Maroufi A, Rahmani K. Posttraumatic stress symptoms, anxiety, and depression among COVID-19 survivors after discharge from hospital. Iran J Psychiatry Behav Sci. 2022;16(3).
- 67.Salimi Z, Najafi R, Khalesi A, Oskoei R, Moharreri F, Khaniki SH, et al. Evaluating the depression, anxiety, stress, and predictors of psychological morbidity among COVID-19 survivors in Mashhad, Iran. Iran J Psychiatry Behav Sci. 2021;15(2).
- 68.Schneider A, Huber L, Lohse J, Linde K, Greissel A, Sattel H, et al. Association between somatic symptom disorder and symptoms with daily life impairment after SARS-CoV-2 infection - results from a population-based cross-sectional study. J Psychosom Res. 2023;168:111230. doi: 10.1016/j.jpsychores.2023.111230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schulze H, Charles James J, Trampe N, Richter D, Pakeerathan T, Siems N, et al. Cross-sectional analysis of clinical aspects in patients with long-COVID and post-COVID syndrome. Front Neurol. 2022;13:979152. doi: 10.3389/fneur.2022.979152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shah A, Bhattad D. Immediate and short-term prevalence of depression in covid-19 patients and its correlation with continued symptoms experience. Indian J Psychiatry. 2022;64(3):301–306. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_840_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shukla AK, Atal S, Banerjee A, Jhaj R, Balakrishnan S, Chugh PK, et al. An observational multi-centric COVID-19 sequelae study among health care workers. Lancet Reg Health Southeast Asia. 2023;10:100129. doi: 10.1016/j.lansea.2022.100129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Singh RK, Pragya P, Singh S. Assessment of COVID-19-related new onset of depression and anxiety: a comparative cross-sectional study. Int J Pharmaceut Clin Res. 2021;13(4):166–174. [Google Scholar]
- 73.Speichert LJ, Schweda A, Witzke O, Konik M, Rohn H, Stettner M, et al. Fear of death during COVID-19 does not explain post-infection depression symptoms beyond reported symptoms during the infection in COVID-19 survivors. Int J Environ Res Public Health. 2022;19(21):13773. doi: 10.3390/ijerph192113773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Suresh A, Shivanna SS, Satyanarayana PT. Posttraumatic stress disorder among adolescent girls infected with COVID-19: a cross-sectional study. J Indian Assoc Child Adolesc Ment Health. 2022;18(1):82–91. [Google Scholar]
- 75.Swami MK, Mahal P, Arora IK, Mishra VC, Panda TK, Nebhinani N, et al. Psychiatric morbidity among patients attending the post-COVID clinic and its association with hematological inflammatory markers. Asian J Psychiatr. 2022;78:103293. doi: 10.1016/j.ajp.2022.103293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tabacof L, Tosto-Mancuso J, Wood J, Cortes M, Kontorovich A, McCarthy D, et al. Post-acute COVID-19 syndrome negatively impacts physical function, cognitive function, health-related quality of life, and participation. Am J Phys Med Rehabil. 2022;101(1):48–52. doi: 10.1097/PHM.0000000000001910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tanriverdi A, Savci S, Kahraman BO, Ozpelit E. Extrapulmonary features of post-COVID-19 patients: muscle function, physical activity, mood, and sleep quality. Ir J Med Sci. 2022;191(3):969–975. doi: 10.1007/s11845-021-02667-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tarantino S, Graziano S, Carducci C, Giampaolo R, Grimaldi Capitello T. Cognitive difficulties, psychological symptoms, and long lasting somatic complaints in adolescents with previous SARS-CoV-2 infection: a telehealth cross-sectional pilot study. Brain Sci. 2022;12(8):969. doi: 10.3390/brainsci12080969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tavares-Júnior JWL, Oliveira DN, da Silva JBS, Feitosa WLQ, Sousa AVM, Cunha LCV, et al. Long-covid cognitive impairment: cognitive assessment and apolipoprotein E (APOE) genotyping correlation in a brazilian cohort. Front Psychiatry. 2022;13:947583. doi: 10.3389/fpsyt.2022.947583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Titus AR, Mezuk B, Hirschtick JL, McKane P, Elliott MR, Fleischer NL. Patterns and predictors of depressive and anxiety symptoms within a population-based sample of adults diagnosed with COVID-19 in Michigan. Soc Psychiatry Psychiatr Epidemiol. 2023;58(7):1099–1108. doi: 10.1007/s00127-023-02453-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Torales J, González-Urbieta I, Barrios I, Waisman-Campos M, Terrazas-Landivar A, Viola L, et al. "Pandemic fatigue" in South America: a multi-center report from Argentina, Bolivia, Paraguay, Peru, and Uruguay. Brain Sci. 2023;13(3):444. doi: 10.3390/brainsci13030444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Vargas Ramirez LK, Rodriguez Corredor LK. Functional limitations, anxiety and depression post-COVID in Colombian adults. In: B58. Pulmonary Rehabilitation: New Horizons. American Thoracic Society; 2022. p. A3183.
- 83.Villalpando JMG, Forcelledo HA, Castillo JLB, Sastré AJ, Rojop IEJ, Hernández VO, et al. COVID-19, Long COVID Syndrome, and Mental Health Sequelae in a Mexican population. Int J Environ Res Public Health. 2022;19:6970. doi: 10.3390/ijerph19126970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Xiao X, Yang X, Zheng W, Wang B, Fu L, Luo D, et al. Depression, anxiety and post-traumatic growth among COVID-19 survivors six-month after discharge. Eur J Psychotraumatol. 2022;13(1):2055294. doi: 10.1080/20008198.2022.2055294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Xu F, Wang X, Yang Y, Zhang K, Shi Y, Xia L, et al. Depression and insomnia in COVID-19 survivors: a cross-sectional survey from chinese rehabilitation centers in Anhui province. Sleep Med. 2022;91:161–165. doi: 10.1016/j.sleep.2021.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yavuz Z, Tezcan S, Kumcu MK, Ölmez B, Yücesan C. Post-COVID-19 prolonged neurological symptoms and characteristics: a face-to-face survey study. Neurology Asia. 2022;27(4):899–908. doi: 10.54029/2022stz. [DOI] [Google Scholar]
- 87.Abramoff BA, Dillingham TR, Brown LA, Caldera F, Caldwell KM, McLarney M, et al. Psychological and cognitive functioning among patients receiving outpatient rehabilitation for post-COVID sequelae: an observational study. Arch Phys Med Rehabil. 2023;104(1):11–17. doi: 10.1016/j.apmr.2022.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Agergaard J, Ullahammer WM, Gunst JD, Østergaard L, Schiøttz-Christensen B. Characteristics of a danish post-COVID cohort referred for examination due to persistent symptoms six months after mild acute COVID-19. J Clin Med. 2022;11(24):7338. doi: 10.3390/jcm11247338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Albtoosh AS, Toubasi AA, Al Oweidat K, Hasuneh MM, Alshurafa AH, Alfaqheri DL, et al. New symptoms and prevalence of postacute COVID-19 syndrome among nonhospitalized COVID-19 survivors. Sci Rep. 2022;12(1):16921. doi: 10.1038/s41598-022-21289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Azevedo MN, Rodrigues EDS, Passos EAFV, Filho MAB, Barreto APA, Lima MCC, et al. Multimorbidity associated with anxiety symptomatology in post-COVID patients. Psychiatry Res. 2022;309:114427. doi: 10.1016/j.psychres.2022.114427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bai F, Tomasoni D, Falcinella C, Barbanotti D, Castoldi R, Mulè G, et al. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect. 2022;28(4):611.e9–e16. doi: 10.1016/j.cmi.2021.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Boesl F, Audebert H, Endres M, Pruss H, Franke C. A neurological outpatient Clinic for Patients with Post-COVID-19 syndrome - a report on the clinical presentations of the first 100 patients. Front Neurol. 2021;12:4. doi: 10.3389/fneur.2021.738405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Boiko DI, Skrypnikov AM, Shkodina AD, Hasan MM, Ashraf GM, Rahman MH. Circadian rhythm disorder and anxiety as mental health complications in post-COVID-19. Environ Sci Pollut Res Int. 2022;29(19):28062–28069. doi: 10.1007/s11356-021-18384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bonazza F, Luridiana Battistini C, Fior G, Bergamelli E, Wiedenmann F, D'Agostino A, et al. Recovering from COVID-19: psychological sequelae and post-traumatic growth six months after discharge. Eur J Psychotraumatol. 2022;13(1):2095133. doi: 10.1080/20008198.2022.2095133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Brown LA, Ballentine E, Zhu Y, McGinley EL, Pezzin L, Abramoff B. The unique contribution of depression to cognitive impairment in post-acute sequelae of SARS-CoV-2 infection. Brain Behav Immun Health. 2022;22:100460. doi: 10.1016/j.bbih.2022.100460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Casoni FM, Marelli S, Castelnuovo A, Mombelli S, Salsone M, Zucconi M, et al. Sleep quality in in a Covid-19 rehabilitation department. Neurol Sci. 2022;43:S521. [Google Scholar]
- 97.Chen AK, Wang X, McCluskey LP, Morgan JC, Switzer JA, Mehta R, et al. Neuropsychiatric sequelae of long COVID-19: pilot results from the COVID-19 neurological and molecular prospective cohort study in Georgia, USA. Brain Behav Immun Health. 2022;24:100491. doi: 10.1016/j.bbih.2022.100491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cheung J, Nordmeier K, Kelland S, Harrington M, Williman J, Storer M, et al. Symptom persistence and recovery among COVID-19 survivors during a limited outbreak in Canterbury, New Zealand: a prospective cohort study. Intern Med J. 2023;53(1):37–45. doi: 10.1111/imj.15930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Choudhry AA, Shahzeen F, Choudhry SA, Batool N, Murtaza F, Dilip A, et al. Impact of COVID-19 infection on quality of sleep. Cureus. 2021;13(9):e18182. doi: 10.7759/cureus.18182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Clemente I, Sinatti G, Cirella A, Santini SJ, Balsano C. Alteration of inflammatory parameters and psychological post-traumatic syndrome in long-COVID patients. Int J Environ Res Public Health. 2022;19(12):7103. doi: 10.3390/ijerph19127103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Clift AK, Ranger TA, Patone M, Coupland CAC, Hatch R, Thomas K, et al. Neuropsychiatric ramifications of severe COVID-19 and other severe acute respiratory infections. JAMA Psychiat. 2022;79(7):690–698. doi: 10.1001/jamapsychiatry.2022.1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cook P, Allde E, Griffith F, Khorasanee R, Luke C, Ridley B, et al. Could the emergency department facilitate the start of a holistic follow-up pathway for patients recovering from COVID-19? Ulster Med J. 2022;91(3):135–138. [PMC free article] [PubMed] [Google Scholar]
- 103.Dai S, Zhao B, Liu D, Zhou Y, Liu Y, Lan L, et al. Follow-up study of the cardiopulmonary and psychological outcomes of covid-19 survivors six months after discharge in Sichuan, China. Int J Gen Med. 2021;14:7207–7217. doi: 10.2147/IJGM.S337604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Damiano RF, Caruso MJG, Cincoto AV, de Almeida Rocca CC, de Pádua SA, Bacchi P, et al. Post-COVID-19 psychiatric and cognitive morbidity: preliminary findings from a brazilian cohort study. Gen Hosp Psychiatry. 2022;75:38–45. doi: 10.1016/j.genhosppsych.2022.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Eloy P, Tardivon C, Martin-Blondel G, Isnard M, Turnier PL, Marechal ML, et al. Severity of self-reported symptoms and psychological burden 6-months after hospital admission for COVID-19: a prospective cohort study. Int J Infect Dis. 2021;112:247–253. doi: 10.1016/j.ijid.2021.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Fernández-de-Las-Peñas C, Martín-Guerrero JD, Florencio LL, Navarro-Pardo E, Rodríguez-Jiménez J, Torres-Macho J, et al. Clustering analysis reveals different profiles associating long-term post-COVID symptoms, COVID-19 symptoms at hospital admission and previous medical co-morbidities in previously hospitalized COVID-19 survivors. Infection. 2023;51(1):61–69. doi: 10.1007/s15010-022-01822-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Fernández-De-las-peñas C, Martín-Guerrero JD, Pellicer-Valero ÓJ, Navarro-Pardo E, Gómez-Mayordomo V, Cuadrado ML, et al. Female sex is a risk factor associated with long-term post-COVID related-symptoms but not with COVID-19 symptoms: the LONG-COVID-EXP-CM multicenter study. J Clin Med. 2022;11(2):413. doi: 10.3390/jcm11020413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fischer A, Badier N, Zhang L, Elbéji A, Wilmes P, Oustric P, et al. Long COVID classification: findings from a clustering analysis in the predi-COVID cohort study. Int J Environ Res Public Health. 2022;19(23):16018. doi: 10.3390/ijerph192316018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Frontera JA, Sabadia S, Yang D, de Havenon A, Yaghi S, Lewis A, et al. Life stressors significantly impact long-term outcomes and post-acute symptoms 12-months after COVID-19 hospitalization. J Neurol Sci. 2022;443:11. doi: 10.1016/j.jns.2022.120487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ghosn J, Bachelet D, Livrozet M, Cervantes-Gonzalez M, Poissy J, Goehringer F, et al. Prevalence of post-acute coronavirus disease 2019 symptoms twelve months after hospitalization in participants retained in follow-up: analyses stratified by gender from a large prospective cohort. Clin Microbiol Infect. 2023;29(2):254.e7–e13. doi: 10.1016/j.cmi.2022.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gorelik Y, Dror A, Zayyad H, Wertheim O, Abu Jabal K, Nazzal S, et al. Associations between reported post-COVID-19 symptoms and subjective well-being, Israel, july 2021 - april 2022. Epidemiol Infect. 2023;151:e16. doi: 10.1017/S0950268822001996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gramaglia C, Gattoni E, Gambaro E, Bellan M, Balbo PE, Baricich A, et al. Anxiety, stress and depression in COVID-19 survivors from an italian cohort of hospitalized patients: results from a 1-year follow-up. Front Psychiatry. 2022;13:862651. doi: 10.3389/fpsyt.2022.862651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Guido CA, Lucidi F, Midulla F, Zicari AM, Bove E, Avenoso F, et al. Neurological and psychological effects of long COVID in a young population: a cross-sectional study. Front Neurol. 2022;13:925144. doi: 10.3389/fneur.2022.925144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Guo Y, Wang H, Xiao M, Guan X, Lei Y, Diao T, et al. Long-term outcomes of COVID-19 convalescents: An 18.5-month longitudinal study in Wuhan. Int J Infect Dis. 2023;127:85–92. doi: 10.1016/j.ijid.2022.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Haag K, Du Toit S, Skeen S, Roberts KS, Chideya Y, Notholi V, et al. Predictors of COVID-related changes in mental health in a south african sample of adolescents and young adults. Psychol Health Med. 2022;27:239–255. doi: 10.1080/13548506.2022.2108087. [DOI] [PubMed] [Google Scholar]
- 116.Hartung TJ, Neumann C, Bahmer T, Chaplinskaya-Sobol I, Endres M, Geritz J, et al. Fatigue and cognitive impairment after COVID-19: A prospective multicentre study. EClinicalMedicine. 2022;53:101651. doi: 10.1016/j.eclinm.2022.101651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Heesakkers H, van der Hoeven JG, Corsten S, Janssen I, Ewalds E, Burgers-Bonthuis D, et al. Mental health symptoms in family members of COVID-19 ICU survivors 3 and 12 months after ICU admission: a multicentre prospective cohort study. Intensive Care Med. 2022;48(3):322–331. doi: 10.1007/s00134-021-06615-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Houben-Wilke S, Goërtz YM, Delbressine JM, Vaes AW, Meys R, Machado FV, et al. The impact of long COVID-19 on mental health: observational 6-month follow-up study. JMIR Mental health. 2022;9(2):e33704. doi: 10.2196/33704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Huang X, Liu L, Eli B, Wang J, Chen Y, Liu Z. Mental health of COVID-19 survivors at 6 and 12 months postdiagnosis: a cohort study. Front Psychiatry. 2022;13:863698. doi: 10.3389/fpsyt.2022.863698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hüfner K, Tymoszuk P, Ausserhofer D, Sahanic S, Pizzini A, Rass V, et al. Who Is at Risk of Poor Mental Health Following Coronavirus Disease-19 Outpatient Management? Front Med. 2022;9:792881. doi: 10.3389/fmed.2022.792881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jung YH, Ha EH, Choe KW, Lee S, Jo DH, Lee WJ. Persistent symptoms after acute COVID-19 infection in omicron era. J Korean Med Sci. 2022;37(27):e213. doi: 10.3346/jkms.2022.37.e213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kalamara E, Pataka A, Boutou A, Panagiotidou E, Georgopoulou A, Ballas E, et al. Persistent Sleep Quality Deterioration among Post-COVID-19 Patients: Results from a 6-Month Follow-Up Study. J Pers Med. 2022;12(11):1909. doi: 10.3390/jpm12111909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kaur K, Patel VK, Kumar P, Vasavada DA, Nerli LM, Tiwari DS. A prospective study of major depressive disorder among COVID 19 survivors at a tertiary care hospital. Arch Ment Health. 2021;22(1):23–27. doi: 10.4103/AMH.AMH_72_20. [DOI] [Google Scholar]
- 124.Kaur P, Mudgal V, Rastogi P. Study of post covid psychiatric disorders in a tertiary care hospital. Indian J Psychiatry. 2023;65:S66–S67. [Google Scholar]
- 125.Lier J, Stoll K, Obrig H, Baum P, Deterding L, Bernsdorff N, et al. Neuropsychiatric phenotype of post COVID-19 syndrome in non-hospitalized patients. Front Neurol. 2022;13:988359. doi: 10.3389/fneur.2022.988359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Magnúsdóttir I, Lovik A, Unnarsdóttir AB, McCartney D, Ask H, Kõiv K, et al. Acute COVID-19 severity and mental health morbidity trajectories in patient populations of six nations: an observational study. Lancet Public Health. 2022;7(5):e406–e416. doi: 10.1016/S2468-2667(22)00042-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Maley JH, Sandsmark DK, Trainor A, Bass GD, Dabrowski CL, Magdamo BA, et al. Six-month impairment in cognition, mental health, and physical function following COVID-19-associated respiratory failure. Crit Care Explor. 2022;4(4):e0673. doi: 10.1097/CCE.0000000000000673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mantovani E, Mariotto S, Gabbiani D, Dorelli G, Bozzetti S, Federico A, et al. Chronic fatigue syndrome: an emerging sequela in COVID-19 survivors? J Neurovirol. 2021;27(4):631–637. doi: 10.1007/s13365-021-01002-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Marasco G, Cremon C, Barbaro MR, Cacciari G, Falangone F, Kagramanova A, et al. Post COVID-19 irritable bowel syndrome. Gut. 2022:gutjnl-2022-328483. 10.1136/gutjnl-2022-328483. Epub ahead of print. [DOI] [PubMed]
- 130.Mazza MG, Palladini M, De Lorenzo R, Bravi B, Poletti S, Furlan R, et al. One-year mental health outcomes in a cohort of COVID-19 survivors. J Psychiatr Res. 2022;145:118–124. doi: 10.1016/j.jpsychires.2021.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Mazza MG, Palladini M, De Lorenzo R, Magnaghi C, Poletti S, Furlan R, et al. Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: effect of inflammatory biomarkers at three-month follow-up. Brain Behav Immun. 2021;94:138–147. doi: 10.1016/j.bbi.2021.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mazza MG, Palladini M, Villa G, De Lorenzo R, Rovere Querini P, Benedetti F. Prevalence, trajectory over time, and risk factor of post-COVID-19 fatigue. J Psychiatr Res. 2022;155:112–119. doi: 10.1016/j.jpsychires.2022.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Mei Q, Wang F, Bryant A, Wei L, Yuan X, Li J. Mental health problems among COVID-19 survivors in Wuhan China. World Psychiatry. 2021;20(1):139–140. doi: 10.1002/wps.20829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Méndez R, Balanzá-Martínez V, Luperdi SC, Estrada I, Latorre A, González-Jiménez P, et al. Long-term neuropsychiatric outcomes in COVID-19 survivors: a 1-year longitudinal study. J Intern Med. 2022;291(2):247–251. doi: 10.1111/joim.13389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Menges D, Ballouz T, Anagnostopoulos A, Aschmann HE, Domenghino A, Fehr JS, et al. Burden of post-COVID-19 syndrome and implications for healthcare service planning: a population-based cohort study. PLoS One. 2021;16(7):e0254523. doi: 10.1371/journal.pone.0254523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Moura AEF, Oliveira DN, Torres DM, Tavares-Júnior JWL, Nóbrega PR, Braga-Neto P, et al. Central hypersomnia and chronic insomnia: expanding the spectrum of sleep disorders in long COVID syndrome - a prospective cohort study. BMC Neurol. 2022;22(1):417. doi: 10.1186/s12883-022-02940-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Müller K, Poppele I, Ottiger M, Zwingmann K, Berger I, Thomas A, et al. Impact of Rehabilitation on Physical and Neuropsychological Health of Patients Who Acquired COVID-19 in the Workplace. Int J Environ Res Public Health. 2023;20(2):1468. doi: 10.3390/ijerph20021468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Naidu SB, Shah AJ, Saigal A, Smith C, Brill SE, Goldring J, et al. The high mental health burden of "long covid" and its association with on-going physical and respiratory symptoms in all adults discharged from hospital. Eur Respir J. 2021;57(6):2004364. doi: 10.1183/13993003.04364-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Nehme M, Braillard O, Chappuis F, Courvoisier DS, Kaiser L, Soccal PM, et al. One-year persistent symptoms and functional impairment in SARS-CoV-2 positive and negative individuals. J Intern Med. 2022;292(1):103–115. doi: 10.1111/joim.13482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Niedziela JT, Głowacki J, Ochman M, Pudlo R, Adamczyk-Sowa M, Nowowiejska-Wiewióra A, et al. Post–COVID-19 complications in hospitalized and nonhospitalized patients: the Silesian database of COVID-19 complications (SILCOV-19) Pol Arch Int Med. 2022;132(6):16233. doi: 10.20452/pamw.16233. [DOI] [PubMed] [Google Scholar]
- 141.Noviello D, Costantino A, Muscatello A, Bandera A, Consonni D, Vecchi M, et al. Functional gastrointestinal and somatoform symptoms five months after SARS-CoV-2 infection: a controlled cohort study. Neurogastroenterol Motil. 2022;34(2):e14187. doi: 10.1111/nmo.14187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ocsovszky Z, Otohal J, Berényi B, Juhász V, Skoda R, Bokor L, et al. The associations of long-COVID symptoms, clinical characteristics and affective psychological constructs in a non-hospitalized cohort. Physiol Int. 2022;109(2):230–245. doi: 10.1556/2060.2022.00030. [DOI] [PubMed] [Google Scholar]
- 143.Park HY, Song IA, Lee SH, Sim MY, Oh HS, Song KH, et al. Prevalence of mental illness among COVID-19 survivors in South Korea: nationwide cohort. BJPsych open. 2021;7(6):e183. doi: 10.1192/bjo.2021.1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Patel N, Dahman B, Bajaj JS. Development of New Mental and Physical Health Sequelae among US Veterans after COVID-19. J Clin Med. 2022;11(12):3390. doi: 10.3390/jcm11123390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Pellitteri G, Surcinelli A, De Martino M, Fabris M, Janes F, Bax F, et al. Sleep alterations following COVID-19 are associated with both neuroinflammation and psychological disorders, although at different times. Front Neurol. 2022;13:929480. doi: 10.3389/fneur.2022.929480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Peluso MJ, Kelly JD, Lu S, Goldberg SA, Davidson MC, Mathur S, et al. Rapid implementation of a cohort for the study of post-acute sequelae of SARS-CoV-2 infection/COVID-19. medRxiv : the preprint server for health sciences. 2021.
- 147.Perrot JC, Segura M, Beranuy M, Gich I, Nadal MJ, Pintor A, et al. Comparison of post-COVID symptoms in patients with different severity profiles of the acute disease visited at a rehabilitation unit. PLoS One. 2022;17(9 Septamber):e0274520. doi: 10.1371/journal.pone.0274520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Rass V, Beer R, Schiefecker AJ, Lindner A, Kofler M, Ianosi BA, et al. Neurological outcomes 1 year after COVID-19 diagnosis: a prospective longitudinal cohort study. Eur J Neurol. 2022;29(6):1685–1696. doi: 10.1111/ene.15307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Rousseau AF, Minguet P, Colson C, Kellens I, Chaabane S, Delanaye P, et al. Post-intensive care syndrome after a critical COVID-19: cohort study from a Belgian follow-up clinic. Ann Intensive Care. 2021;11(1):118. doi: 10.1186/s13613-021-00910-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Santos CAD, Filho GGF, Alves MM, Macedo EYL, Pontes deAMG, Paula AP, et al. Maternal and Neonatal Outcomes Associated with Mild COVID-19 Infection in an Obstetric Cohort in Brazil. Am J Trop Med Hyg. 2022;107(5):1060–1065. doi: 10.4269/ajtmh.22-0421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Sathyamurthy P, Madhavan S, Pandurangan V. Prevalence, pattern and functional outcome of post COVID-19 syndrome in older adults. Cureus J Med Sci. 2021;13(8):22. doi: 10.7759/cureus.17189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Sayde GE, Stefanescu A, Hammer R. Interdisciplinary Treatment for Survivors of Critical Illness in the Era of COVID-19: Expanding the Post-Intensive Care Recovery Model and Impact on Psychiatric Outcomes. J Acad Consult Liaison Psychiatry. 2023;64(3):226–235. doi: 10.1016/j.jaclp.2023.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Staudt A, Jörres RA, Hinterberger T, Lehnen N, Loew T, Budweiser S. Associations of post-acute COVID syndrome with physiological and clinical measures 10 months after hospitalization in patients of the first wave. Eur J Intern Med. 2022;95:50–60. doi: 10.1016/j.ejim.2021.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Straudi S, Manfredini F, Baroni A, Milani G, Fregna G, Schincaglia N, et al. Construct Validity and Responsiveness of the COVID-19 Yorkshire Rehabilitation Scale (C19-YRS) in a Cohort of Italian Hospitalized COVID-19 Patients. Int J Environ Res Public Health. 2022;19(11):6696. doi: 10.3390/ijerph19116696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Taquet M, Dercon Q, Luciano S, Geddes JR, Husain M, Harrison PJ. Incidence, co-occurrence, and evolution of long-COVID features: A 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. 2021;18(9):e1003773. doi: 10.1371/journal.pmed.1003773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Targa A, Benítez I, Moncusí-Moix A, Vaca R, Gort-Paniello C, Minguez O, et al. Sleep and circadian rest-activity pattern of critical COVID-19 survivors in the long-term: a 6-month follow-up study. Sleep Med. 2022;100:S89–S90. doi: 10.1016/j.sleep.2022.05.250. [DOI] [Google Scholar]
- 157.Titze-de-Almeida R, da Cunha TR, dos Santos Silva LD, Ferreira CS, Silva CP, Ribeiro AP, et al. Persistent, new-onset symptoms and mental health complaints in Long COVID in a Brazilian cohort of non-hospitalized patients. BMC Infect Dis. 2022;22(1):133. doi: 10.1186/s12879-022-07065-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Tokumasu K, Honda H, Sunada N, Sakurada Y, Matsuda Y, Yamamoto K, et al. Clinical Characteristics of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Diagnosed in Patients with Long COVID. Medicina (Lithuania). 2022;58(7):850. doi: 10.3390/medicina58070850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.van Raaij BFM, Stöger JL, Hinnen C, Penfornis KM, de Jong CMM, Klok FA, et al. Fibrotic-like abnormalities notably prevalent one year after hospitalization with COVID-19. Respir Med Res. 2022;82:100973. doi: 10.1016/j.resmer.2022.100973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Vlake JH, Van Bommel J, Hellemons ME, Wils EJ, Bienvenu OJ, Schut AFC, et al. Psychologic distress and quality of life after ICU treatment for Coronavirus Disease 2019: a multicenter, observational cohort study. Crit Care Explor. 2021;3(8):e0497. 10.1097/CCE.0000000000000497. [DOI] [PMC free article] [PubMed]
- 161.Wang S, Quan L, Chavarro JE, Slopen N, Kubzansky LD, Koenen KC, et al. Associations of depression, anxiety, worry, perceived stress, and loneliness prior to infection with risk of post-COVID-19 conditions. JAMA Psychiat. 2022;79(11):1081–1091. doi: 10.1001/jamapsychiatry.2022.2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Wang Y, Xie J, Garcia C, Prieto-Alhambra D. Long-term mental health outcomes after SARS-CoV-2 infection: prospective cohort study. 2022. [Google Scholar]
- 163.Weidman K, LaFond E, Hoffman KL, Goyal P, Parkhurst CN, Derry-Vick H, et al. Post-intensive care unit syndrome in a cohort of COVID-19 survivors in New York City. Ann Am Thoracic Society. 2022;19(7):1158–1168. doi: 10.1513/AnnalsATS.202104-520OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Wiertz CMH, Hemmen B, Sep SJS, Van Santen S, Van Horn YY, Van Kuijk SMJ, et al. Life after COVID-19: the road from intensive care back to living - a prospective cohort study. BMJ Open. 2022;12(11):e062332. doi: 10.1136/bmjopen-2022-062332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Yang Q, Zhang M, Lai Y, Liu X, Liu F, Zang H, et al. COVID-19 could cause long term peripheral nerve demyelination and axonal loss: A One Year Prospective Cohort Study. 2022. [Google Scholar]
- 166.Zhu S, Gao Q, Yang L, Yang Y, Xia W, Cai X, et al. Prevalence and risk factors of disability and anxiety in a retrospective cohort of 432 survivors of coronavirus Disease-2019 (Covid-19) from China. PLoS One. 2020;15(12):e0243883. doi: 10.1371/journal.pone.0243883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Fernández-de-Las-Peñas C, Torres-Macho J, Elvira-Martínez CM, Molina-Trigueros LJ, Sebastián-Viana T, Hernández-Barrera V. Obesity is associated with a greater number of long-term post-COVID symptoms and poor sleep quality: a multicentre case-control study. Int J Clin Pract. 2021;75(12):e14917. doi: 10.1111/ijcp.14917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Fernández-de-las-Peñas C, Torres-Macho J, Velasco-Arribas M, Plaza-Canteli S, Arias-Navalón JA, Hernández-Barrera V, et al. Preexisting hypertension is associated with a greater number of long-term post-COVID symptoms and poor sleep quality: a case–control study. J Hum Hypertens. 2022;36(6):582–584. doi: 10.1038/s41371-022-00660-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Fu L, Wang B, Chan PSF, Luo D, Zheng W, Ju N, et al. Associations between COVID-19 related stigma and sleep quality among COVID-19 survivors six months after hospital discharge. Sleep Med. 2022;91:273–281. doi: 10.1016/j.sleep.2021.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Magdy R, Elmazny A, Soliman SH, Elsebaie EH, Ali SH, Fattah AMA, et al. Post-COVID-19 neuropsychiatric manifestations among COVID-19 survivors suffering from migraine: a case-control study. J Headache Pain. 2022;23(1):10. doi: 10.1186/s10194-022-01468-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Murga I, Aranburu L, Gargiulo PA, Gómez Esteban JC, Lafuente JV. Clinical Heterogeneity in ME/CFS. A Way to Understand Long-COVID19 Fatigue. Front Psychiatry. 2021;12:735784. doi: 10.3389/fpsyt.2021.735784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Schulz M, Mangiapane S, Scherer M, Karagiannidis C, Czihal T. Post-acute sequelae of SARS-CoV-2 infection-characterization of community-treated patients in a case-control study based on Nationwide claims data. Deutsches Arzteblatt Int. 2022;119(10):177–178. doi: 10.3238/arztebl.m2022.0134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Senara S, Salah H, Wahed WA, Yehia A. Frequency of fibromyalgia syndrome and anxiety post-corona virus disease-2019 (COVID-19) in patients attending the rheumatology clinic. Egypt Rheumatol. 2023;45(2):127–131. doi: 10.1016/j.ejr.2022.11.007. [DOI] [Google Scholar]
- 174.Badinlou F, Lundgren T, Jansson-Frojmark M. Mental health outcomes following COVID-19 infection: impacts of post-COVID impairments and fatigue on depression, anxiety, and insomnia - a web survey in Sweden. BMC Psychiatry. 2022;22(1):11. doi: 10.1186/s12888-022-04405-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Cacciatore M, Raggi A, Pilotto A, Cristillo V, Guastafierro E, Toppo C, et al. Neurological and Mental Health Symptoms Associated with Post-COVID-19 Disability in a Sample of Patients Discharged from a COVID-19 Ward: A Secondary Analysis. Int J Environ Res Public Health. 2022;19(7):4242. doi: 10.3390/ijerph19074242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Diem L, Fregolente-Gomes L, Warncke JD, Hammer H, Friedli C, Kamber N, et al. Fatigue in Post-COVID-19 Syndrome: Clinical Phenomenology, Comorbidities and Association With Initial Course of COVID-19. J Cent Nerv Syst Dis. 2022;14:11795735221102727. doi: 10.1177/11795735221102727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Diem L, Schwarzwald A, Friedli C, Hammer H, Gomes-Fregolente L, Warncke J, et al. Multidimensional phenotyping of the post-COVID-19 syndrome: a swiss survey study. CNS Neurosci Ther. 2022;28(12):1953–1963. doi: 10.1111/cns.13938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2019686. doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Leonardi M, Cacciatore M, Pilotto A, Cristillo V, Guastafierro E, Toppo C, et al. NEUROLOGICAL and mental health symptoms associated with post-COVID-19 disability in a sample of patients discharged from a COVID-19 ward: a secondary analysis. Neurol Sci. 2022;43:S324–S325. doi: 10.3390/ijerph19074242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nat Med. 2021;27(4):626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Fernández-de-Las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, Cuadrado ML, Florencio LLJIjoer health p. Defining post-COVID symptoms (post-acute COVID, long COVID, persistent post-COVID): an integrative classification. Int J Environ Res Public Health. 2021;18(5):2621. doi: 10.3390/ijerph18052621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re'em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021;38:101019. doi: 10.1016/j.eclinm.2021.101019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Carfì A, Bernabei R, Landi FJPsipaaC-J Gemelli against COVID-19 post-acute care study group. Scand J Work Environ Health. 2020;324(6):603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Schou TM, Joca S, Wegener G, Bay-Richter CJB. behavior,, immunity. Psychiatric and neuropsychiatric sequelae of COVID-19–A systematic review. Brain Behav Immun. 2021;97:328–348. doi: 10.1016/j.bbi.2021.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Arora T, Grey I, Östlundh L, Lam KBH, Omar OM, Arnone DJJohp. The prevalence of psychological consequences of COVID-19: A systematic review and meta-analysis of observational studies. J Health Psychol. 2022;27(4):805–824. doi: 10.1177/1359105320966639. [DOI] [PubMed] [Google Scholar]
- 186.Nochaiwong S, Ruengorn C, Thavorn K, Hutton B, Awiphan R, Phosuya C, et al. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci Rep. 2021;11(1):1–18. doi: 10.1038/s41598-021-89700-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Carvalho-Schneider C, Laurent E, Lemaignen A. Seguimiento de adultos con COVID-19 no crítico dos meses después del inicio de los síntomas. Infección Microbiol Clin. 2021;27(2):258–63. doi: 10.1016/j.cmi.2020.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Jacobs LG, Gourna Paleoudis E, Lesky-Di Bari D, Nyirenda T, Friedman T, Gupta A, et al. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. PLoS One. 2020;15(12):e0243882. doi: 10.1371/journal.pone.0243882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Liu D, Baumeister RF, Veilleux JC, Chen C, Liu W, Yue Y, et al. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan. China. 2020;292:113297. doi: 10.1016/j.psychres.2020.113297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Mannan A, Mehedi H, Chy N, Qayum MO, Akter F, Rob M, et al. A multi-centre, cross-sectional study on coronavirus disease 2019 in Bangladesh: clinical epidemiology and short-term outcomes in recovered individuals. New Microbes New Infect. 2021;40:100838. doi: 10.1016/j.nmni.2021.100838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Nie X-D, Wang Q, Wang M-N, Zhao S, Liu L, Zhu Y-L, et al. Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. Int J Psychiatry Clin Pract. 2021;25(2):109–114. doi: 10.1080/13651501.2020.1791345. [DOI] [PubMed] [Google Scholar]
- 193.Cai X, Hu X, Ekumi IO, Wang J, An Y, Li Z, et al. Psychological distress and its correlates among COVID-19 survivors during early convalescence across age groups. Am J Geriatr Psychiatry. 2020;28(10):1030–1039. doi: 10.1016/j.jagp.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Thye AY, Law JW, Tan LT, Pusparajah P, Ser HL, Thurairajasingam S, et al. Psychological Symptoms in COVID-19 Patients: Insights into Pathophysiology and Risk Factors of Long COVID-19. Biology. 2022;11(1):61. doi: 10.3390/biology11010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Kubota T, Kuroda N, Sone D. Neuropsychiatric aspects of long COVID: a comprehensive review. Psychiatry Clin Neurosci. 2023;77(2):84–93. doi: 10.1111/pcn.13508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Kappelmann N, Dantzer R, Khandaker GMJP. Interleukin-6 as potential mediator of long-term neuropsychiatric symptoms of COVID-19. Psychoneuroendocrinology. 2021;131:105295. doi: 10.1016/j.psyneuen.2021.105295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Boldrini M, Canoll PD, Klein RSJJp. How COVID-19 affects the brain. JAMA Psychiat. 2021;78(6):682–683. doi: 10.1001/jamapsychiatry.2021.0500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Research Accessibility Team (RAT) The microvascular hypothesis underlying neurologic manifestations of long COVID-19 and possible therapeutic strategies. Cardiovasc Endocrinol Metab. 2021;10(4):193–203. doi: 10.1097/XCE.0000000000000253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Zheng YB, Zeng N, Yuan K, Tian SS, Yang YB, Gao N, et al. Prevalence and risk factor for long COVID in children and adolescents: a meta-analysis and systematic review. J Infect Public Health. 2023;16(5):660–672. doi: 10.1016/j.jiph.2023.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Table 1. PRISMA 2020 checklist. Supplementary Table 2. Search strategies for online databases. Supplementary Table 3. Characteristics of the included studies. Supplementary Fig 1. Risk of bias assessment for each included study.
Data Availability Statement
All data has been presented in the manuscript.