Abstract
Varicella zoster virus (VZV) infection may cause large or medium vessel vasculitis, including granulomatous arteritis of the nervous system and central nervous system vasculitis. However, small vessel vasculitis, such as cutaneous leukocytoclastic vasculitis (LCV) associated with localized cutaneous VZV infection, herpes zoster, is uncommon. Herein, we present the case of a 75- year-old man with segmental leukocytoclastic vasculitis associated with herpes zoster on the leg. To the best of our knowledge, there are four cases of segmental leukocytoclastic vasculitis in herpes zoster reported in the English literature; we compared our case with these previous reports. Our review of five patients suggests that most patients were immunosuppressed. We also found that the leg is susceptible to LCV associated with herpes zoster. Anti-viral treatment was effective for LCV as well as herpes zoster. Prior reports have proposed etiologies inducing LCV; for example, immune complexes are mediated by vessel wall damage. In support of this, histopathology in our case showed a C3-positive reaction with the small vessel walls in the dermis in direct immunofluorescence. Although the mechanism of LCV associated with herpes zoster remains unclear, we should consider LCV while diagnosing and treating patients with herpes zoster, especially immunosuppressed patients.
Key words: herpes zoster, Varicella zoster virus, leukocytoclastic vasculitis, immunosuppression, amenamevir
Introduction
Varicella zoster virus (VZV) infection may cause large or medium vessel vasculitis including granulomatous arteritis of the nervous system and central nervous system vasculitis.1-3 However, small vessel vasculitis such as cutaneous leukocytoclastic vasculitis (LCV) associated with localized cutaneous VZV infection, herpes zoster, is uncommon.1,2 Herein, we present a rare case of segmental leukocytoclastic vasculitis associated with herpes zoster of the leg. To the best of our knowledge, there are four reports of segmental leukocytoclastic vasculitis in patients with herpes zoster in the English literature; we compared our case with these previous cases.
Case Report
A 75-year-old man presented with painful purpura and blisters on his right lower leg. He had a history of focal glomerulosclerosis, hypertension, steroid-induced diabetes, and myocardial infarction. He had been taking prednisone 20 mg and cyclosporine 75 mg once daily for focal glomerulosclerosis. He had pain in his leg two weeks previously without any skin lesions. The pain in his leg worsened, and palpable purpura and some blisters appeared in a linear distribution on his lower right leg (Figure 1a). A skin biopsy of his lower right leg was performed, which revealed intraepidermal bulla with ballooning degeneration and acantholysis, and perivascular dense infiltration of neutrophils accompanied by some leukocytoclasia and hemorrhage in the dermis that was consistent with leukocytoclastic vasculitis and viral infection (Figure 1b and c). Direct immunofluorescence demonstrated a C3-positive reaction with small vessel walls in the dermis (Figure 1d). Leukocytoclastic vasculitis associated with herpes zoster was confirmed, and the patient was treated with a one-week course of amenamevir, following which the purpura resolved and all blisters scabbed over.
Discussion and Conclusions
Herpes zoster is caused by reactivation of VZV, which is latent in ganglionic neurons along the entire neuraxis. Immunosuppression is a risk factor for VZV reactivation.2,4 VZV infection in immunosuppressed patients can have atypical manifestations, such as painless lesions, absence of vesicles, erythematous lesions, and vasculitis.1-4 To the best of our knowledge, four cases of segmental LCV associated with herpes zoster have been reported (Table 1). Our review of these cases revealed that most patients were immunosuppressed. All patients were male with an average age of 66.6 years. We also found that the leg is susceptible to LCV associated with herpes zoster. Anti-viral treatment was effective for LCV as well as herpes zoster. Based on these observations, we speculate that the risk factors for LCV associated with herpes zoster may include immunosuppression, male sex, and older age, with the lower limbs most likely to be affected (Table 1). The etiology of LCV may include immune complex deposition mediated by vessel wall damage or stimulated autoreactive immune cells elicited by molecular mimicry.1 Another possibility is that direct VZV infection of the endothelium may cause thickened intima and vascular remodeling.2,4 In addition, it has been reported that IgA vasculitis, an acute LCV with strong abdominal symptoms, may result from VZV infection based on the observation that VZV envelope glycoprotein antigens were found in both cutaneous and gastrointestinal lesions.5 However, the mechanism of VZV reactivation causing cutaneous vasculitis remains unclear. Taken together, these findings suggest that clinicians should be alert to the possibility of LCV in patients with herpes zoster, especially in immunosuppressed patients.
Table 1.
Clinical findings of published cases and the present patient.
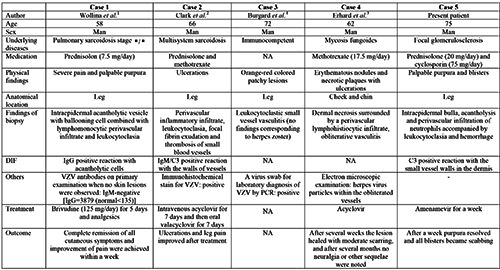
DIF, direct immunofluorescence; VZV, varicella zoster virus; PCR, polymerase chain reaction; NA, not applicable; Ig, immunoglobulin.
Figure 1.
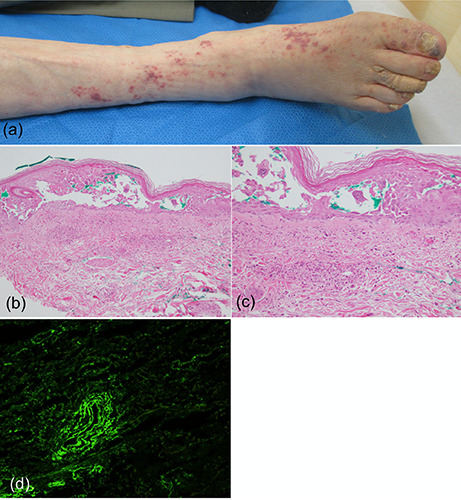
Clinical and histopathological features of the patient. a) Painful purpura and blisters on the lower right leg; b and c) histopathological analysis showing intraepidermal acantholytic bulla with ballooning degeneration and perivascular infiltration of neutrophils accompanied by leukocytoclasia and erythrocyte extravasation (hematoxylin and eosin staining, original magnification ×100; b and B) original magnification ×200; d) direct immunofluorescence showing a C3-positive reaction with small vessel walls in the dermis.
References
- 1.Wollina U, Schonlebe J. Segmental leukocytoclastic vasculitis in herpes zoster. Int J Dermatol 2012;51:1351-2. [DOI] [PubMed] [Google Scholar]
- 2.Clark AK, Dhossche J, Korcheva VB, et al. Herpes zoster presenting as unilateral vasculitis. Dermatol Online J 2018;24. [PubMed] [Google Scholar]
- 3.Erhard H, Runger TM, Kreienkamp M, et al. Atypical varicella- zoster virus infection in an immunocompromised patient: result of a virus-induced vasculitis. J Am Acad Dermatol 1995;32: 908-11. [DOI] [PubMed] [Google Scholar]
- 4.Burgard B, Smola S, Vogt T, et al. Small Vessel Vasculitis in Herpes Zoster-Discussion of Current Aspects of Varicella Zoster Virus Vasculopathy. Am J Dermatopathol 2018;40:602-4. [DOI] [PubMed] [Google Scholar]
- 5.Ushigome Y, Yamazaki Y, Shiohara T. IgA vasculitis with severe gastrointestinal symptoms may be an unusual manifestation of varicella zoster virus reactivation. Br J Dermatol 2017;176:1103-5. [DOI] [PubMed] [Google Scholar]


