Abstract
Introduction and importance:
Acute appendicitis is a common surgical emergency marked by appendix inflammation, presenting as acute abdominal pain and typically treated with appendectomy. The authors report a rare case of disseminated appendicular lymphoma presenting as acute appendicitis. Acute appendicitis is a common surgical emergency.
Case presentation:
This case involved a 75-year-old male patient who underwent appendectomy, revealing an enlarged appendix with lymphomatous nodules.
Clinical discussion:
Lymphoma involvement in the appendix is extremely rare, and lymphomas presenting as acute appendicitis are even more exceptional. Imaging investigations, including ultrasound and CECT scan of the abdomen, are recommended to aid in diagnosis. On computed tomography, appendiceal lymphoma is characterized by markedly diffuse mural soft-tissue thickening with preserved vermiform morphology and occasional aneurysmal dilatation of the lumen.
Conclusion:
This case underscores the importance of considering unusual etiologies in atypical appendicitis presentations.
Keywords: Acute appendicitis, appendix, case reports, lymphoma
Introduction and importance
Highlights
Acute appendicitis is a common surgical emergency marked by appendix inflammation, presenting as acute abdominal pain.
Our case involved a 75-year-old male patient who underwent appendectomy, revealing an enlarged appendix with lymphomatous nodules.
The combination of surgery and chemotherapy is considered the best treatment for appendiceal lymphomas
Acute appendicitis is a common surgical emergency marked by appendix inflammation, presenting as acute abdominal pain and typically treated with appendectomy1 However, uncommon etiologies can often complicate the diagnosis. Lymphomas, malignancies originating from lymphocytes, rarely involve the appendix, and lymphomas presenting as acute appendicitis are rare, with limited cases reported in the medical literature2,3.
The rarity of lymphoma involvement in the appendix can lead to delayed or incorrect diagnosis, as lymphoma-related appendicitis may mimic typical appendicitis clinically. Understanding and recognizing these atypical presentations is crucial to ensure appropriate management and treatment.
This case report describes a 75-year-old male patient who presented with symptoms suggestive of acute appendicitis. The case has been reported in line with SCARE guidelines4.
Case presentation
A 75-year-old male came to our hospital with acute onset of continuous dull aching pain over right iliac fossa for 3 days associated with anorexia and nausea. He had fever (maximum temperature 101.6 F). He had not passed stool and flatus for 2 days. Patient also complained of loss of appetite, fatigability and unintentional weight loss of 8 kg in a period of 1 month.
A physical examination showed the patient to be ill-looking with significant lower abdominal tenderness, with more tenderness occurring in the right quadrant. Rebound tenderness was noted. He had pallor and a temperature of 101F.
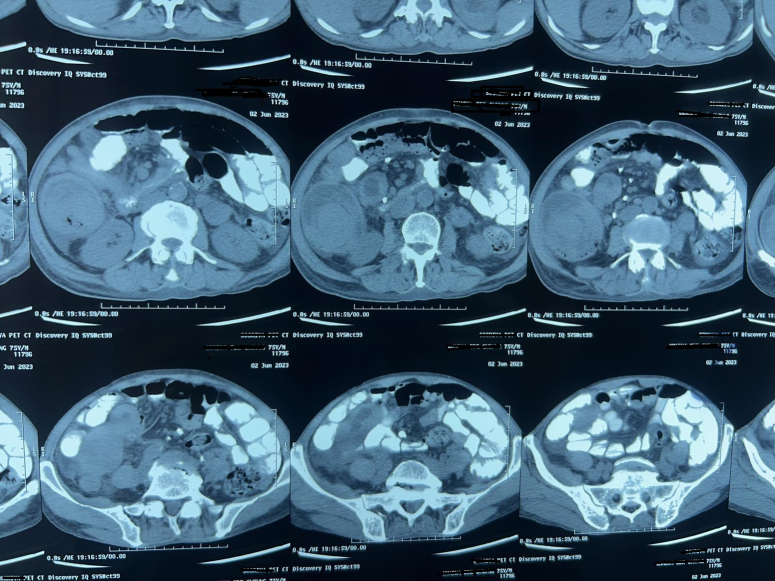
Following a lab examination, blood tests revealed an elevated white cell count of 16.9×109/l (range 4–11 ×109/l), with an associated N% of 71% (range 50–70%),with raised creatinine 145 mmol/l (range 59–104 mmol/l). However, abdominal ultrasonography revealed 8×4 cm hypodense mass in right iliac fossa and computed tomography (CT) enterograffin showed a well-defined oval shape heterogenous mass with probable solid cystic component [Figure 1].
Figure 1.
12×10 cm, Oval shaped well-defined heterogeneous mass with probable solid cystic component in right iliac fossa, no lymphadenopathy.
The patient was prepared for exploratory laparotomy and right limited hemicolectomy with ileocolostomy was performed with intraoperative findings of ~15×10 cm appendicular mass, hard in consistency and invading up to caecum, with thickening of caecum and terminal ileum [Figure 2], and minimal ascites and no enlarged lymph nodes were seen. Postoperative period was uneventful.
Figure 2.
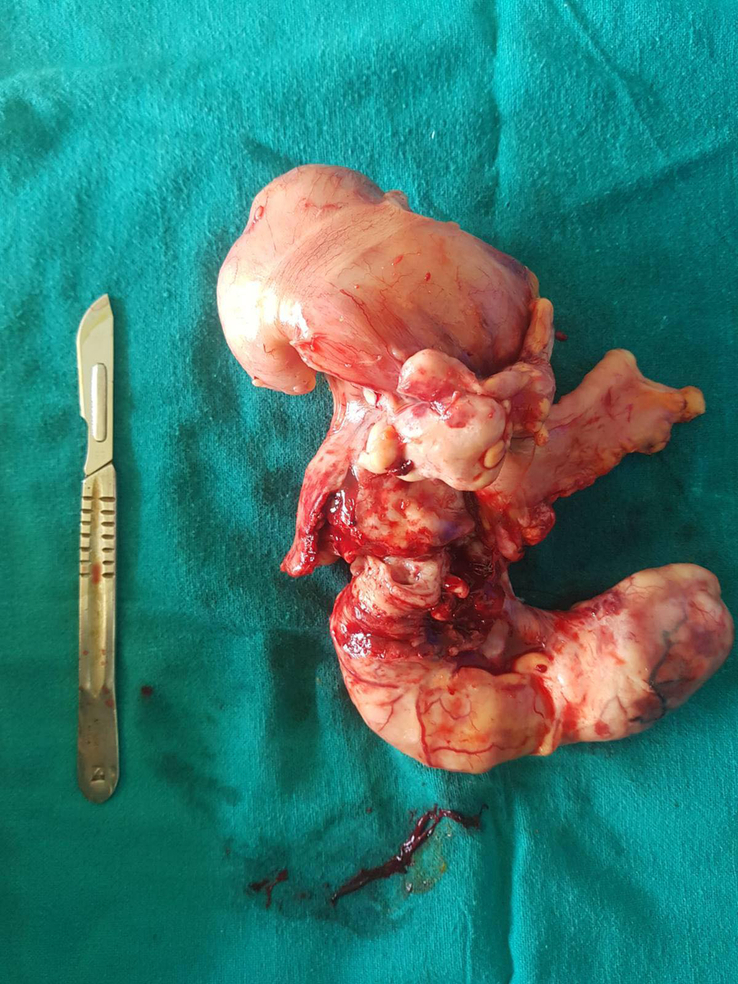
15×10 cm sized, grossly enlarged, inflamed appendix with hard consistency with invasion into caecum.
After 1 week, the final histologic examination revealed a non-Hodgkin lymphoma with IHC confirming it to be an extranodal marginal zone lymphoma with involvement of the ileum, caecum, appendix, and colon involving up to serosa [Figures 3–5]. IHC revealed that tumour cells were CD20, BCL2, and PAX5 positive. However CD3, CD5, CD10, CD23, CD30 BCL6 were negative.
Figure 3.
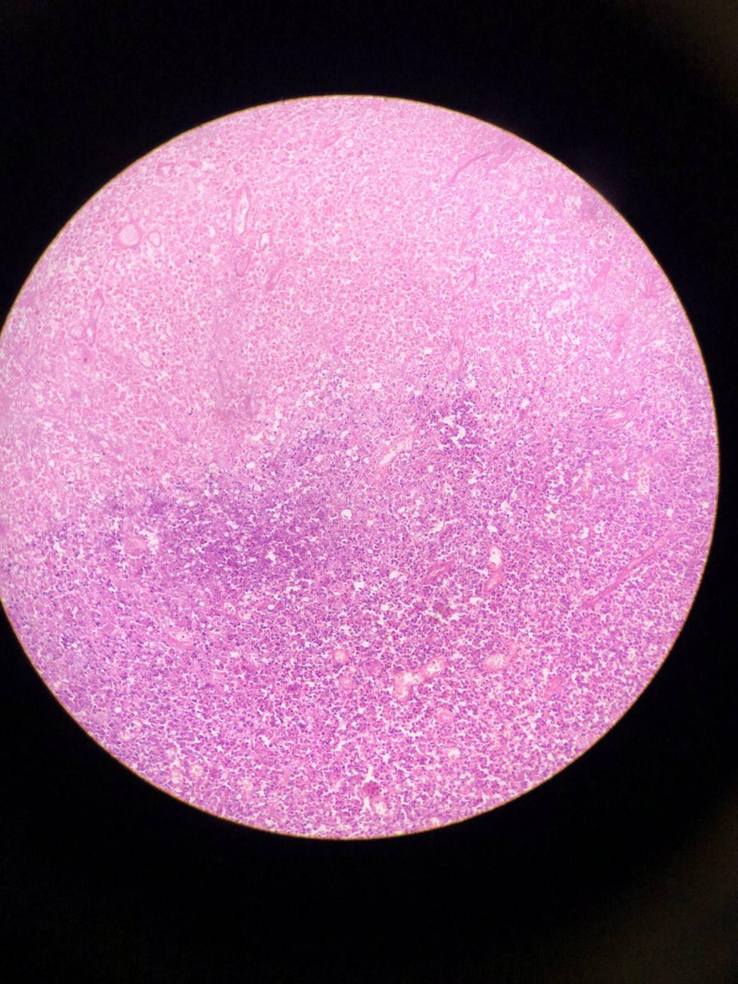
40× magnification: Section shows extensive areas of necrosis along with viable small lymphoid cells.
Figure 5.
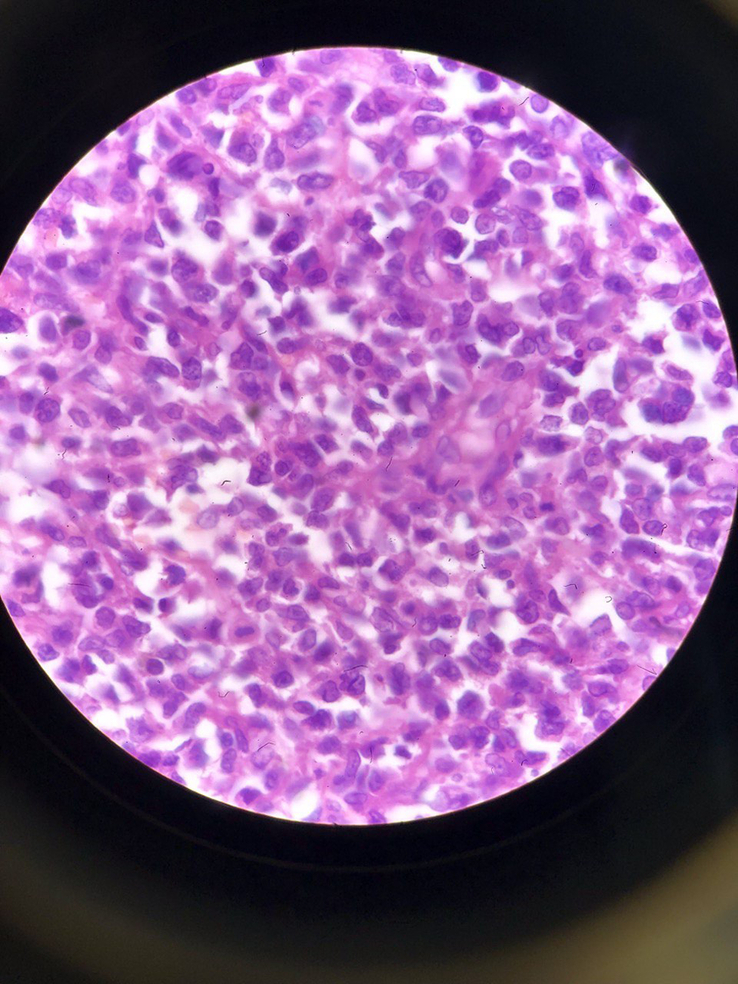
400× magnification: Cell show mild pleomorphism, scant cytoplasm, round nuclei and prominent nucleoli.
Figure 4.
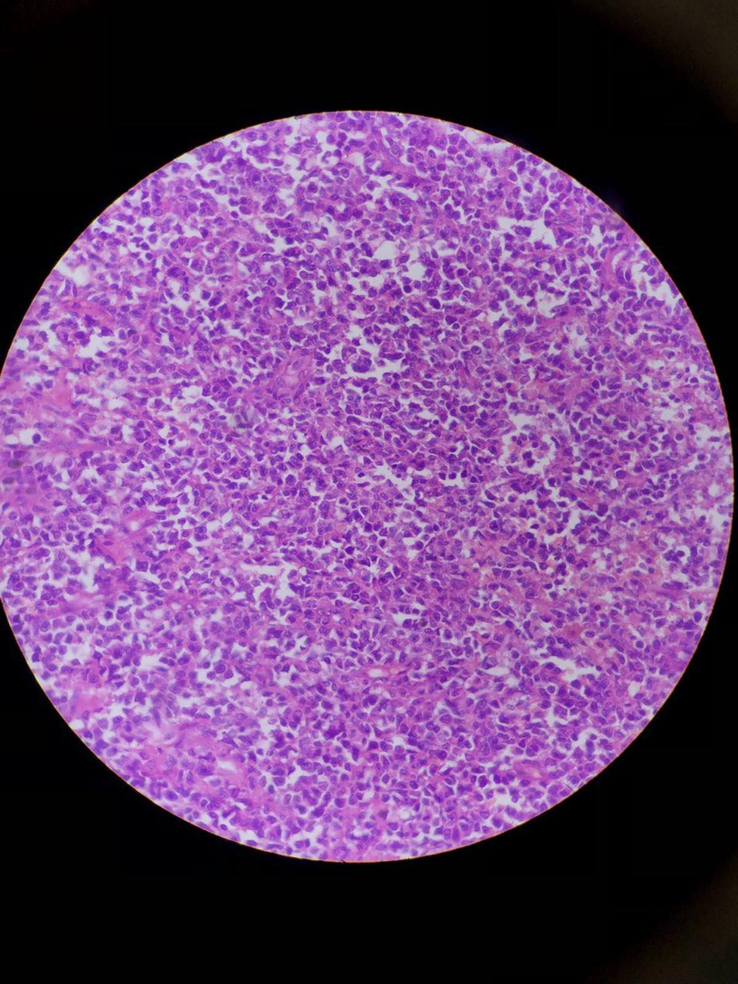
200× magnification showing monotonous population of lymphoid cells.
The patient was discharged after 8 days with an oncological referral as both proximal and distal margins were involved by tumour cells. Postoperative treatment with chemotherapy was carried out. Patient was planned for six cycles of CHOP Regimen and then ileocolostomy reversal after completion of chemotherapy was planned. On follow-up after 1 months, patient was gaining weight, nutritionally well-built and ileostomy was functioning with output 400–500 ml/24 h output 400–500 ml/24 h.
Clinical discussion
Cancers of the appendix, especially appendiceal lymphomas, belong to the rare category of primary gastrointestinal non-Hodgkin lymphomas, constituting less than 1% of non-Hodgkin lymphoma cases5. The incidence of gastrointestinal tract lymphoma, comprising 4–20% of non-Hodgkin’s lymphoma and 30–45% of extranodal cases, predominantly affects the stomach, small bowel, pharynx, and colon, with a median age at diagnosis of 55 years, and a male predominance2,5,6.
Acute appendicitis is the typical presentation, though other uncommon symptoms, such as gastrointestinal bleeding and intussusception, may occur. Appendiceal lymphomas are usually diagnosed intraoperatively and classified accordingly2,7.
Appendiceal neoplasms are more frequently observed in females during the sixth decade of life, although our case was an elderly male. While appendicular lymphoma may present as appendicitis, early-stage appendiceal lymphomas are commonly diagnosed incidentally during resection for suspected appendicitis2. Features of Acute appendicitis-like pain in the right lower quadrant is the most common clinical presentation. Advanced-stage appendiceal lymphomas may penetrate the visceral peritoneum and invade adjacent organs, leading to serious complications2,7,8.
Imaging investigations, including ultrasound and CECT scan of the abdomen, are recommended to aid in diagnosis. On CT, appendiceal lymphoma is characterized by markedly diffuse mural soft-tissue thickening with preserved vermiform morphology and occasional aneurysmal dilatation of the lumen. Coexisting abdominal lymphadenopathy is variably observed8. Preoperative diagnosis of appendiceal neoplasms is increasingly possible with the widespread use of CT, where diffuse enlargement of the appendix from lymphomatous infiltration is a diagnostic feature. PET/CT is crucial for lymphoma staging and assessment of therapeutic response7–9.
Histology confirms the diagnosis of appendiceal lymphomas. Optimal treatment strategies depend on the primary tumour’s histopathologic characteristics, TNM stage, and grade. The treatment guidelines for appendiceal lymphomas are not well defined, leading to controversies regarding the surgical approach (open vs. laparoscopic), adjuvant chemotherapy, and follow-up protocols2,5,10,11.
Colonoscopy is recommended before radical treatment to exclude synchronous colon cancer11. Patients with appendiceal lymphomas should undergo regular follow-up investigations to monitor recurrence and second malignancy risk, tumour markers, along with radiologic imaging (ultrasonography/CECT scan), are advised at 6-month intervals for 2 years post-appendectomy, followed by annual CT scans10–12. and tumour marker assessments for 5–10 years. Our patient was advised to have regular follow-ups with a CECT scan after 3 months, and then at every six-month intervals for 2 years, and then annually for 5 years.
Conclusion
Appendicular lymphoma is a rare but life-threatening condition, necessitating timely recognition and proper management to reduce its high morbidity and mortality rates. As it usually presents as acute appendicitis, clinicians should be vigilant, maintain a high level of suspicion, and consider histopathological examination of all appendectomy specimens. Although preoperative diagnosis is challenging, CT plays a pivotal role in aiding diagnosis, and PET/CT is necessary for staging lymphoma. In the literature, the combination of surgery and chemotherapy is considered the best treatment for appendiceal lymphomas.
Ethical approval
Nothing to declare.
Consent
Written informed consent was obtained from the patient for publication of this study and accompanying images.
Sources of funding
The authors declare that this study had no funding source.
Author contribution
D.R., P.J.L. and S.D.: study concept, data collection and surgical therapy for the patient. D.R. and O.P.B.: writing—original draft preparation. P.B. and B.P.K.: editing and writing. P.J.L.: senior author and manuscript reviewer. All the authors read and approved the final manuscript.
Conflicts of interest disclosure
No potential conflict of interest relevant to this article was reported.
Research registration unique identifying number (UIN)
Not applicable.
Guarantor
Dipesh Regmi accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Data availability statement
None.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgements
The authors thank all collaborators who provided excellent assistance during the study.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Dipesh Regmi, Email: dipeshregmi9@gmail.com.
Shishir Devkota, Email: devkotashishir53@gmail.com.
Om Prakash Bhatta, Email: meprakashom@gmail.com.
Prashant Bhetwal, Email: prashantbhetwal36@gmail.com.
Sushil Kumar Yadav, Email: skyadav136@iom.edu.np.
Pratik Baral, Email: pratikbaral16@gamil.com.
Bishnu Prasad Kandel, Email: drkandel@hotmail.com.
Paleswan Joshi Lakhey, Email: lakheypj@gmail.com.
References
- 1.Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg WJES 2020;15:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ayub A, Santana-Rodríguez N, Raad W, et al. Primary appendiceal lymphoma: clinical characteristics and outcomes of 116 patients. J Surg Res 2017;207:174–180. [DOI] [PubMed] [Google Scholar]
- 3.Fu TY, Wang JS, Tseng HH. Primary appendiceal lymphoma presenting as perforated acute appendicitis. J Chin Med Assoc JCMA 2004;67:629–632. [PubMed] [Google Scholar]
- 4.Sohrabi C, Mathew G, Maria N, et al. Collaborators . The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 2023;109:1136–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawkes EA, Wotherspoon A, Cunningham D. Diagnosis and management of rare gastrointestinal lymphomas. Leuk Lymphoma 2012;53:2341–2350. [DOI] [PubMed] [Google Scholar]
- 6.Dincel O, Göksu M, Türk BA, et al. Incidental findings in routine histopathological examination of appendectomy specimens; retrospective analysis of 1970 patients. Indian J Surg 2018;80:48–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guo J, Wu G, Chen X, et al. Primary appendiceal lymphoma presenting as suspected perforated acute appendicitis: clinical, sonography and CT findings with pathologic correlation. Int J Clin Exp Pathol 2014;7:7068–7071. [PMC free article] [PubMed] [Google Scholar]
- 8.Pickhardt PJ, Levy AD, Rohrmann CA, et al. Non-Hodgkin’s lymphoma of the appendix. Am J Roentgenol 2002;178:1123–1127. [DOI] [PubMed] [Google Scholar]
- 9.Bhasker AG, Kotecha JD, Pandey R, et al. Non-Hodgkin’s lymphoma of the appendix and distal ileum. A rare case report. J Minimal Access Surg 2021;17:548–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caristo G, Griseri G, Fornaro R, et al. Primary lymphoma of appendix presenting as acute appendicitis: a case report. Int J Surg Case Rep 2018;48:30–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoehn RS, Rieser CJ, Choudry MH, et al. Current management of appendiceal neoplasms. Am Soc Clin Oncol Educ Book 2021;41:1–15. [DOI] [PubMed] [Google Scholar]
- 12.Rossi A, Maloney Patel N. Appendiceal neoplasms—a practical guide. J Surg Oncol 2023;127:1300–1305. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
None.