Abstract
Introduction and importance:
Essential thrombocythemia (ET) is a rare chronic myeloproliferative hematologic disorder, leading to an elevated platelet count. Two-thirds of patients are asymptomatic during their lifetime, while others may experience symptoms like redness, congestion, and erythromelalgia after long symptom-free intervals.
Case presentation:
The authors present a rare instance of a 55-year-old female who, despite receiving aspirin and losartan treatment, eventually developed digital gangrene. In further work-ups, she had an elevated platelet count and a positive JAK 2 mutation. Her platelet count was reduced throughout treatment with aspirin, hydroxyurea, and heparin, which was followed by the necrotic tip of her index finger being surgically debrided.
Clinical discussion:
Significant symptoms, such as severe acrocyanosis and even peripheral gangrene, can be treated with a single dose of aspirin. Daily aspirin consumption withstanding, this case developed the severe form of ET. In addition, while thrombocytosis predisposes patients to thrombotic complications in theory, there is little evidence to support a correlation between absolute platelet count and thrombosis.
Conclusion:
The initial symptom of ET could be such severe and uncommon that may develop arterial acral thrombosis despite previous daily low-dose aspirin consumption.
Keywords: acral thrombosis, case report, digital gangrene, essential thrombocythemia, thrombocytosis
Introduction
Highlights
Essential thrombocythemia (ET) is an uncommon chronic myeloproliferative hematologic disorder.
Two-thirds of patients are asymptomatic during their lifetime.
In ET, cerebrovascular and coronary events are more likely than peripheral thrombosis.
This case presented with digital gangrene as first manifestation of ET.
Essential thrombocythemia (ET) is a rare chronic myeloproliferative hematologic disorder characterized by abnormal megakaryocyte proliferation, which results in an elevated platelet count. ET is defined when there is persistent thrombocytosis above 600×109/l in the platelet count without of a known cause, according to clinical, histologic, and cytogenetic findings1.
Even though incidence varies depending on the community, two-thirds of patients are asymptomatic and only obtain medical care by chance when thrombocytosis is discovered during a routine blood cell count. ET manifests in a variety of ways, but its key clinical characteristics are the risk of bleeding and thrombotic events. Age over 60 and a history of prior thrombotic events are two critical risk factors for thrombosis in ET. Treatment with an antiplatelet dosage alone typically yields a significant improvement in most patients2.
We present a rare instance of a 55-year-old patient with ET who, despite receiving aspirin and losartan treatment, eventually developed digital gangrene. Her platelet count was reduced throughout therapy with aspirin, hydroxyurea, and heparin, which was followed by the necrotic tip of her index finger being surgically debrided. We also conducted a literature search in the PubMed database using ((((((Essential Thrombocythemia) OR (ET)) AND (Digital Gangrene)) OR (Limb Ischemia)) AND (Thrombocytosis)) AND (Thrombosis)) AND (Case Report) to gather information for the article. This work has been reported in line with the surgical case report (SCARE) 2023 criteria3.
Presentation of case
A 55-year-old woman presented to our hospital with a chief complaint of blackish discoloration of her right index finger that started 2 weeks ago. The patient claimed that following exposure to citric acid, she experienced itching, erythema, and pain initially, and then, the pain intensified, and the color changed to purple. She did not present any rheumatologic signs, including malar rash, eye or mouth dryness, genital aphthous, but recurrent oral aphthous ulcers. Moreover, she did not report any history of Raynaud’s phenomenon. Her past medical history was only significant for hypertension. There was no positive family, allergy, surgery or habitual history. She reported daily aspirin and losartan consumption. Physical examination showed a young lady, Pulse- 80 bpm, BP – 110/90 mmHg, temperature – 36.8°C, RR- 18 bpm. The right index finger had blackish discoloration but no ulceration (Fig. 1). It was tender to touch. Right upper extremity was colder than the other. Upper and lower limb pulses were palpable, symmetric, and normal. Ankle brachial indices were detected as normal. A Color Doppler study of her right upper limb was done, which showed normal arterial triphasic flow till the base of the second digit. No stricture or plaque was seen in the arteries. Eighter superficial or deep veins were open and compressible and had normal flow. True anteroposterior and lateral radiographs of second finger were performed to rule out the bone infraction. In physical examination, lymphadenopathy and organomegaly were not detected. Laboratory tests demonstrated serum chemistry, coagulation tests, and CRP within normal range. Complete blood counts revealed hemoglobin of 14 mg/dl, leukocyte count of 10.07×103/mm3 platelet count of 921×103/mm3, and mean corpuscular volume 101.2 fl. She was detected for a positive JAK 2 mutation. In order to differentiate ET and polycythemia vera, bone marrow aspiration and biopsy was done. Biopsy revealed myeloproliferative disease with adequate iron storage. As the diagnosis of ET was made, heparin (5000 units IV bolus, then continuous infusion of 1000 units/hr), aspirin (80 mg orally once a day), and hydroxyurea (500 mg orally twice daily) were administered immediately. Then, general surgeons of our hospital debrided the distal part of the second distal digit in the operating room (Fig. 2). Until the patient’s platelet count falls below 450 000, hydroxyurea and aspirin were prescribed. As the recurrence of thrombotic events is possible, the patient was suggested to be monitored and refer for follow-ups. Management of patient-centric factors (e.g. hypertension, cholesterol, and weight/diet) and preventive measures was done to reduce thrombotic risk. To get the patient back to normal range of platelet, follow-up CBC tests were done every 2 weeks at first, then every month, and finally every 2 months. In later follow-ups, she was symptom-free with no evidence of ischemia and necrotic tip of index had been got autoamputated (Fig. 3). The patient’s platelets are now within normal range, with a count of less than 450 000, after 6 months (Fig. 4).
Figure 1.
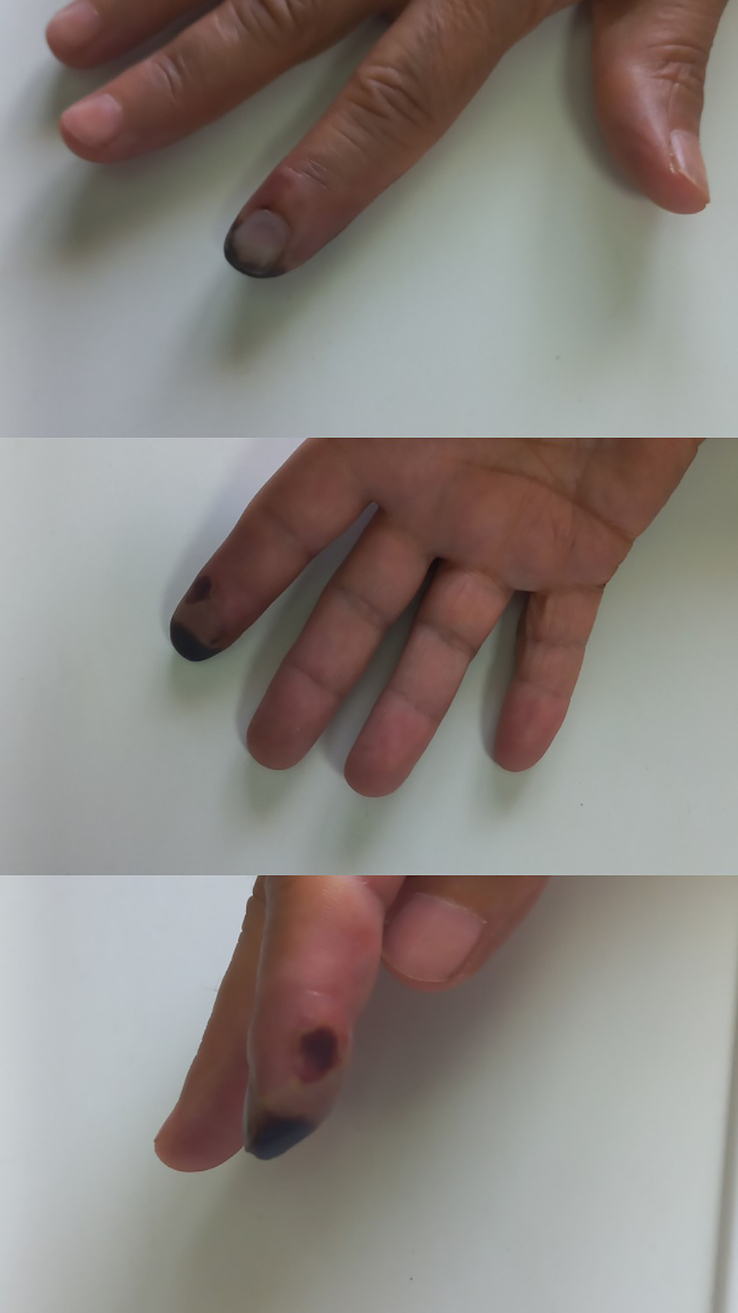
Gangrene of distal second digit.
Figure 2.

Debridement of the ischemic part in the operating room.
Figure 3.

Patient’s hand after auto-amputation of the necrotic distal second digit.
Figure 4.
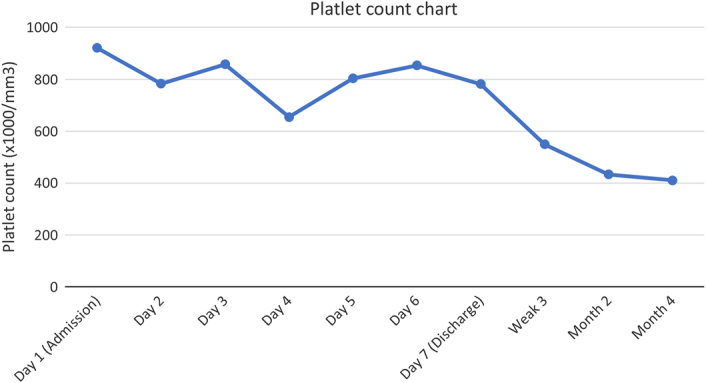
Platelet count drop following treatment.
Discussion
ET progresses slowly and is characterized by long symptom-free periods, which are interspersed by thrombotic or hemorrhagic occurrences1. It is diagnosed as thrombocytosis with megakaryocytic hyperplasia in the bone marrow that causes redness, congestion, and excruciating burning in the limbs4. While some significant symptoms, such as severe acrocyanosis and even peripheral gangrene, can be treated with a single dose of aspirin, the vast majority of patients will experience the ischemia phenomenon reversed, and their erythromelalgia resolve within 2 to 4 days5; nonetheless, the patent’s painful acral gangrene was not related to classic erythromelalgia, because her extremities were not warm and congested. The case presented above is atypical because her first manifestation of ET was arterial acral ischemia, despite receiving aspirin, and losartan treatment.
ET appears rare, although it has been described in all hematological texts6. Although thrombocytosis theoretically predisposes patients to thrombotic complications (e.g. deep vein thrombosis in the lower extremities, thrombosis of the mesenteric veins, and possible pulmonary embolism), little evidence supports a correlation between absolute platelet count and thrombosis, and only a few cases have been described7.
Thrombosis mainly takes place in veins rather than arteries7, on the contrary, ET leads to arterial events more than venous events. A study conducted on 12 456 ET cases with an ET diagnosis, showed that most common thrombotic events were ischemic stroke (42.5%), acute myocardial infarction (25.9%), and transient ischemic attack (24.8%). Peripheral arterial thrombosis consists 2.7% of all thrombotic events in ET patients. It also revealed that the median time from ET diagnosis to first thrombotic event was 10.1 months whereas first manifestation of this case was thrombosis8.
In asymptomatic patients, the decision to introduce cytoreductive therapy is controversial. Large prospective trials of ET are needed to investigate the cost-benefit profile in this situation. However, in complicated cases of thrombosis, treatment for the myeloproliferative disorder is indicated, and the decision to use long-term aspirin and, or anticoagulants must be made on an individual basis9. Harrison et al., conducted a study in which adult patients were randomly distributed into two groups: Group 1, patients treated with low-dose aspirin plus hydroxyurea, and Group 2, patients treated with aspirin plus anagrelide. Significantly more patients in the anagrelide group than in the hydroxyurea group reached the study endpoint. The authors concluded that hydroxyurea plus aspirin was superior to anagrelide plus aspirin for patients with ET to inhibit complications10. Similar studies conducted in this field support the importance of our findings. Papadonikolakis et al.11, reported a 34-year-old patient with ET who had developing digital gangrene, Raynaud’s syndrome, and was unresponsive to medication. In another study, Chen et al., mentioned a 34-year-old man presented with a 10-day history of right limb weakness and numbness. Despite not having therapy for 6 months prior to admission, he was diagnosed with ET in 2008. He had an increased platelet count. He had a satisfactory course of treatment after MRI revealed an acute watershed infarction. However, a headache and weakening in his left limb resulted in his readmission after 14 months. There was spontaneous subdural bleeding, as shown by a head computed tomography scan. He had a decompressive craniectomy and a subdural hematoma removed. One year after being discharged, his condition showed signs of improvement and stability. This instance implies that ET can both induce very diverse strokes and act as a risk factor for strokes12. Our report was unique as the patient was unaware of his illness and since, even with aspirin therapy, the patient’s initial sign of the disease was digital gangrene.
In this case, medical treatment of heparin (5000 units IV bolus, then continuous infusion of 1000 units/hr), aspirin (80 mg orally once a day), and hydroxyurea (500 mg orally twice daily) were started, and debridement of the distal part of second distal digit was performed. She did not develop any complication of ischemia in later follow-ups.
Conclusion
This case presented with digital gangrene as first manifestation of ET and made us aware that the initial symptoms of ET, an uncommon condition, could be acral arterial thrombosis, an uncommon cite. Moreover, even though aspirin is the main treatment for this disease, ET may lead to arterial acral thrombosis despite previous daily low-dose aspirin consumption.
Ethical approval
Ethical approval is not required as this article is a case report.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author contribution
All authors have same contribution.
Conflicts of interest disclosures
All authors have no conflict of interest to declare.
Research registration unique identifying number (UIN)
This article is a case report.
Guarantor
Maryam Rashidian is corresponding author and guarantor of this study.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgements
The authors acknowledge all medical professionals who collaborated in patient assessment, care, and appropriate interventions.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Amirhossein Mirhosseini, Email: Amir.mir85@gmail.com.
Ramin Bozorgmehr, Email: Raminchebozorgmehr@gmail.com.
Fatemeh Bastan, Email: Fatemehbastan79@Gmail.Com.
Maryam Rashidian, Email: maryamrashidian1378@gmail.com.
References
- 1.Sanchez S, Ewton A. Essential thrombocythemia: a review of diagnostic and pathologic features. Arch Pathol Lab Med 2006;130:1144–1150. [DOI] [PubMed] [Google Scholar]
- 2.Accurso V, Santoro M, Mancuso S, et al. The essential thrombocythemia in 2020: what we know and where we still have to dig deep. Clin Med Insights Blood Disord 2020;13:2634853520978210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sohrabi C, Mathew G, Maria N, et al. The scare 2023 guideline: updating consensus surgical case report (scare) guidelines. Int J Surg 2023;109:1136–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ashorobi D, Gohari P. Essential thrombocytosis. Statpearls. StatPearls Publishing Copyright ©; 2023. StatPearls Publishing LLC.; 2023. [PubMed] [Google Scholar]
- 5.Hussain S, Schwartz JM, Friedman SA, et al. Arterial thrombosis in essential thrombocythemia. Am Heart J 1978;96:31–36. [DOI] [PubMed] [Google Scholar]
- 6.Meier B, Burton JH. Myeloproliferative disorders. Hematol Oncol Clin North Am 2017;31:1029–1044. [DOI] [PubMed] [Google Scholar]
- 7.Lawrence PF, Bell RM, Dayton MT. Essentials of general surgery, Sixth ed. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2019. [Google Scholar]
- 8.Pemmaraju N, Gerds AT, Yu J, et al. Thrombotic events and mortality risk in patients with newly diagnosed polycythemia vera or essential thrombocythemia. Leukemia Res 2022;115:106809. [DOI] [PubMed] [Google Scholar]
- 9.Pearson TC. The risk of thrombosis in essential thrombocythemia and polycythemia vera. Semin Oncol 2002;29(3 suppl 10):16–21. [DOI] [PubMed] [Google Scholar]
- 10.Harrison CN, Campbell PJ, Buck G, et al. Hydroxyurea compared with anagrelide in high-risk essential thrombocythemia. N Engl J Med 2005;353:33–45. [DOI] [PubMed] [Google Scholar]
- 11.Papadonikolakis A, Chloros GD, Smith BP, et al. Digital ischemia due to essential thrombocythemia: a case report. J Hand Surg Am 2007;32:1053–1057. [DOI] [PubMed] [Google Scholar]
- 12.Chen X, Cao L, Feng H, et al. Successive development of ischemic stroke and hemorrhagic stroke in a patient with essential thrombocythemia: a case report. J Int Med Res 2021;49:300060520987718. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.


