Abstract
Introduction:
Students in the preclinical phase have adequate clinical exposure to normal physiological findings of clinical examinations performed in healthy peers but do not have exposure to pathological findings other than theoretical knowledge, which is challenging for students during the clinical phase of curricula in examining actual patients. Simulation based medical education (SBME) has recently emerged to address this gap. This study aimed to assess performance and confidence level of simulation based clinical examination of respiratory system in preclinical undergraduate medical students of a medical college.
Methods:
A comparative cross-sectional study was conducted in the Department of Human Physiology of Medical College. All second year medical students using purposive sampling were taken. Students were divided into three groups and subdivided into six subgroups and each subgroup carried out examination in either healthy subjects or both healthy subjects and manikin. Predesigned proforma was used for assessment of students and the clinical examination process was invigilated by certified physiologists.
Results:
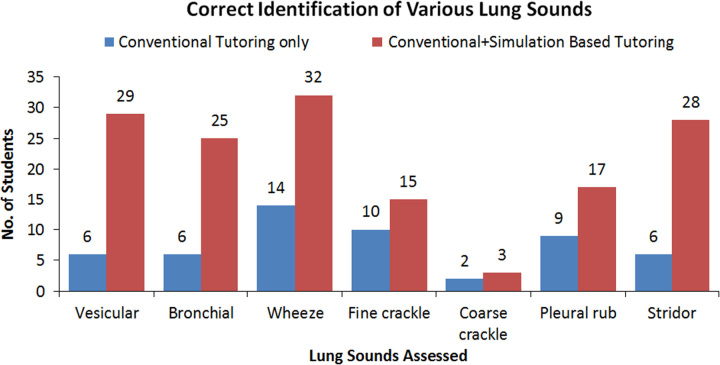
Students who received both simulation and conventional tutoring methods were able to accurately identify all lung sounds better as compared to those with conventional tutoring with the percentage difference being maximum in identifying vesicular (29 vs 6), stridor (28 vs 6), and bronchial (25 vs 6) breath sounds and least in identifying coarse crackles (3 vs 2). Majority (39 out of 41) of the students receiving SBME of respiratory system were satisfied with the simulation based practice and 34 of those students were even confident on clinical examination.
Conclusion:
SBME increases performance status and confidence level in medical students. A practical curriculum can be planned to incorporate simulation based clinical examination in preclinical medical students in practical sessions.
Keywords: clinical, confidence, performance, SBME, simulation, students
Introduction
Highlights
We aim to study the benefits of simulation based clinical examination in preclinical medical students.
Those students with simulation performed better in identifying both normal and abnormal breath sounds.
Simulation increases confidence and performance during clinical examination.
One of the fundamental clinical skills to be acquired by medical students is the ability to carry out various systemic examinations and differentiate between physiologic and pathologic findings. Integrating clinical skills during preclinical years can improve confidence, performance, and enables students to do better during clinical rotations1,2. In many developing countries, the exposure to clinical examination skills starts from their preclinical years enabling students to appreciate the physiological findings. Pathological findings are explained theoretically in these sessions. The success of these teaching methods is reliant on the student’s capacity to successfully engage with the material and create a mental image of the situation, which can be challenging for undergraduate medical students with limited clinical experience of actual patients3. When the students start their clinical rotation and come in contact with patients, they get exposed to the pathological findings. Although the best way to acquire clinical skills is at the patient’s bedside, it is limited by a relatively large student-to-patient ratio, the complexity of clinical presentations, the inconvenience of repeated physical examinations on patients with advanced diseases and the existence of sudden outbreaks of contagious diseases, like COVID-194. These limitations have added to the need of finding a means to supplement authentic clinical experience, which can be achieved with simulations of varying fidelity5–8.
Simulation-based medical education (SBME) with deliberate practice has surfaced to be superior than traditional clinical education in various countries9. Simulation provides facilitators with the ability to deliver training in a controlled, more standardized environment under a variety of conditions, including uncommon or high-risk scenarios and allows facilitators with better opportunity for feedback, evaluation of performance, and competency due to the objectively standard scenarios presented2,10,11. The manikins used in medical education have undergone significant advances in recent years, which can be programmed to reflect various physiological signs and to respond to procedures performed by the students, so when used appropriately, participant engagement, learning and reflection on practice are heightened3,6,12,13. Various country’s Medical Councils encourage and accredit simulation-based learning whenever possible14,15. The role of SBME in preclinical years for clinical examination of respiratory system in countries with low socio economic status like Nepal has not been widely studied. This study aimed to assess performance and confidence level of simulation based clinical examination of respiratory system in preclinical undergraduate medical students of a medical college in Kathmandu.
Methods
A comparative cross-sectional study was conducted in the Department of Human Physiology of a medical college. Tenth batch, second year MBBS students meeting inclusion criteria who agreed to participate in the study were included in the study. Absentees during the tutorial session of practical class regarding the respiratory system examination were excluded from the study. The conventional practical session carried out in our institution had 10–15 min of discussion on the theoretical aspect of respiratory system examination followed by demonstration of clinical examination of respiratory system by the faculty.
For study purposes, the students were broadly divided into three groups A, B, and C as per the practical session of the college and then each group was subdivided as A1, A2, B1, B2, C1, and C2. On day one of the practical session, students were briefed on the respiratory system examination. Then, the first subgroup (A1) carried out examination in a healthy subject and the second subgroup (A2) carried out examination in a healthy subject as well as in a manikin. To ensure that the peer subjected to examination during the practical was healthy, the faculty, who is a certified physiologist, examined him prior to the students and subject without any signs and symptoms of respiratory ailments were chosen. The manikin used was medium-fidelity manikin manufactured by Nasco Lifeform. Similar patterns were done for groups B and C. The healthy subject taken in each group was one of their peers in each subgroup. On the second day of practical’s, all students were evaluated on the preprogrammed manikin to identify various lung sounds.
Assessment was done using predesigned proforma where all the students with or without simulation were asked to identify normal and abnormal breath sounds in the preprogrammed manikin. This process was observed and scored by an invigilator, a certified clinical physiologist, who would present during the process to record the student’s performance. The proforma used for this assessment was designed by the research team based on their experience and rigorous study of the literature. The two physiologists who were involved in the assessment process were previously trained by the principal investigator. Following that, group with simulation study were additionally asked to fill out questionnaire forms prepared with the help of similar studies done previously for assessing performance and confidence level in identifying both normal and pathological breath sound11. Validation of the questionnaire was done in 20 students of the senior batch and the results were not incorporated into the results.
Approval from the Institution Review Committee (IRC) of our institution was obtained with Reg no 705 dated November 2022. Administrative approval was taken from the principal. Informed consent was taken from each participant. Anonymity of the participants was maintained. Data was collected between 18th and 27th January 2023. Data was entered and analyzed using MS-Excel 2010. Frequency and percentages were calculated for data analysis.
This article has been registered with UIN in the research registry and has been reported in line with the strengthening the reporting of cohort, cross-sectional and case–control studies in surgery (STROCSS) criteria16.
Results
A total of 80 students were included in the study as 20 students were either absent during the tutorial session or in the assessment phase of the study, and were therefore excluded. Of the 80 participants, 41 students were exposed to the simulation based practical session in addition to the conventional tutoring on respiratory system examination, while the remaining 39 students were only tutored with the conventional methods.
Students with simulation based practical sessions were able to identify various pathological breath sounds more accurately as compared to conventional methods only as shown by (Fig. 1). The number of participants correctly identifying various breath sounds in conventional tutoring with simulation students versus conventional tutoring only students were compared (Fig. 1). Vesicular breath sounds (29 vs 6), stridor (28 vs 6), and bronchial (25 vs 6) breath sounds were identified four times more; wheeze (31 vs 14) more than twice; and pleural rub (17 vs 9) almost twice more accurately by simulation with conventional tutoring group, as compared to conventional tutoring only students. Coarse crackles (3 vs 2) followed by fine crackles (15 vs 10) were the two lung sounds where the difference in identification was the least (Fig. 1).
Figure 1.
Distribution of correct responses for identification of the various lung sounds during assessment (N=80). (Conventional tutoring only N=39, simulation with conventional tutoring N=41).
All students with SBME exposure wished to integrate simulation based clinical examination as shown by (Table 1). One student did not find the facilitator conducting the simulation suitable to the way he/she learnt.
Table 1.
Satisfaction about simulation-based session (N=41)
| SN | Statement | SDA N | DA N | N N | A N | SA N |
|---|---|---|---|---|---|---|
| 1 | The integration of simulation with manikin for clinical skills teaching method was effective in achieving the learning objectives of the session | 0 | 0 | 0 | 20 | 21 |
| 2 | The integration of simulation with manikin for clinical skills teaching method was well organized in terms of scheduling and planning | 0 | 0 | 5 | 13 | 23 |
| 3 | The facilitators gave me clear instructions of what is expected from me during this session | 0 | 0 | 2 | 14 | 25 |
| 4 | The integration of simulation with manikin for clinical skills teaching method were motivating me to learn | 0 | 0 | 4 | 23 | 14 |
| Sufficient guidance was given to me by the facilitator before I performed on simulation | 0 | 0 | 0 | 25 | 16 | |
| 6 | The way my facilitators conducted the simulation was suitable to the way I learn | 0 | 1 | 1 | 11 | 28 |
| 7 | The integration of simulation with manikin for the clinical skills teaching method helped me to link theory to practice | 0 | 0 | 2 | 18 | 21 |
A, agree; DA, disagree; N, neutral; SA, strongly agree; SDA, strongly disagree.
Assessing the confidence about simulation-based sessions (Table 2), 36 students with simulation along with conventional tutoring were confident in applying clinical skills learnt during simulation practical to real life clinical situations. Regarding mastering the content taught in simulation study, nine were neutral.
Table 2.
Confidence about simulation-based session (N=41)
| SN | Statement | SDA | DA | N | A | SA |
|---|---|---|---|---|---|---|
| 1 | I am confident that I am obtaining the required knowledge from integrated clinical skills sessions with simulation to perform necessary tasks in a clinical practice | 0 | 0 | 5 | 23 | 13 |
| 2 | I am confident that I am developing the required skills from integrated clinical skills sessions with simulation to perform necessary tasks in a clinical practice | 0 | 1 | 6 | 22 | 12 |
| 3 | I am certain that I can accomplish my intended learning objectives for these sessions | 0 | 1 | 4 | 28 | 8 |
| 4 | I am confident that I am mastering the content of the simulation activity that my facilitators presented to me | 0 | 1 | 15 | 20 | 5 |
| 5 | I am confident that the integrated clinical skills sessions with simulation covered all the necessary content mentioned in the curriculum | 0 | 0 | 8 | 18 | 15 |
A, agree; DA, disagree; N, neutral; SA, strongly agree; SDA, strongly disagree.
Discussion
Knowledge of clinical sciences and ability to identify it during clinical practice is the basis of clinical examination in medical practice. Our study shows that additional simulation on manikin helped students in identifying breath sounds more accurately than those with conventional tutoring only by more than four times in identifying vesicular, bronchial sounds, and stridor. There was not much difference in identifying fine and coarse crackles as those with simulation tutoring were confused in differentiating fine and coarse crackles suggesting that more focus should be given during tutoring in differentiating crackles. Majority of students with simulation based clinical examination of respiratory system were satisfied with simulation based practice and even were confident in identifying the pathological sounds as in concordance with the study by Mirza MB et al.11, although a single participant was not satisfied with simulation based practice in respect to simulation study conducted as students’ way of learning and very few participants were not confident in diagnosing pathology even after simulation based practice in context of developing required skills, accomplishing learning objectives, and mastering content of simulation study.
A similar simulation based study by Nassif J. et al.17 showed that hybrid simulation of clinical breast examination improved the sensitivity of pathological breast lesion identification, showing the advantage of simulation in clinical practice.
A quantitative meta-analysis by McGaghie et al.9 comparing the effectiveness of SBME with traditional clinical education methods showed the effect size of 0.71 (95% CI: 0.65–0.76; P<0.001) in achieving specific clinical skill, which showed that SBME is very effective in achieving clinical skills.
Another study on medical students by Nuzzo A et al.18 showed that students with clinical skills simulation based training scored higher than their counterparts even though exposure was 1 year before exam showing simulation training could be effective even in the long term. Similarly study by Arangalage D et al.19, a simulation based CVS examination showed increased appreciation and appreciation increased from first to second year showing the importance of repeated simulation programmes.
A study by Butter et al. and McKinney et al. showed that tutorial class along with simulation based auscultation training had improved accuracy and outcomes during examination of real patients signifying SBME as an effective educational strategy tool20,21.
A randomized controlled trial by Schroedl et al.22 showed that residents with SBME performed significantly better in assessing knowledge and skills in the medical intensive care unit (MICU) and SBME could be a valuable adjunct to the residents in addition to standard clinical training of MICU.
A review study by Akaike et al.23 showed that SBME was effective in integrating clinical and basic medicine, which is the main purpose of SBME and even use of technology in simulation training led to improvement in behaviors, skills, knowledge, and even patient related outcomes.
Contrary to our findings, one quasi-experimental pilot study conducted by Martins et al.24 comparing various domains for respiratory system clinical examination using high fidelity simulator mannequin reported no statistical difference in performance score of medical students with better results in human subjects. Martins et al.24 used standardized patients in their research whereas in our study the subjects were healthy peers of the same group of students, also the medical students in their research were in third year which in our study were second year students which could have resulted in this difference.
The group with simulation were asked to fill out questionnaire forms for assessing confidence level in identifying both normal and pathological breath sound, which was not done for the conventional teaching, which is a major limitation of our study as we did not assess confidence of the conventional group and compare it with the simulation group. The scoring of performance was based on a dichotomous scale so students could have a positive response bias that might have affected the result. The study was conducted for the respiratory system so it cannot be generalized to other system examinations (cardiovascular/neurosensory/gastrointestinal). The final score could be affected by recall bias while examining the respiratory system.
Conclusion
Students with additional simulation tutoring were able to identify all breath sounds more accurately as compared to those with conventional tutoring. Majorities of the students receiving simulation based clinical examination of respiratory system were satisfied with the simulation based practice and gained confidence on clinical examination. A practical curriculum can be planned in such a way that simulation sessions can be incorporated in the teaching learning method. Further study is required to find whether simulation study in manikin is as effective as study in real patients.
Ethical approval statement
The study was approved by the Institutional Review Committee (IRC) of the Nepalese Army Institute of Health Sciences (NAIHS) with reference number 705 in September, 2022.
Consent
All the participants were informed about the study and its objectives during the time of data collection. Written informed consent was obtained from the students for publication and any accompanying images. A copy of the written consent is available for review by Editor-in-Chief of this journal on request.
Sources of funding
None.
Author contribution
Y.S.R. and B.T.: literature review, conceptualization, methodology, data collection, formal analysis, writing – original draft, and review and edit; L.B.: literature review, methodology, data collection, writing – original draft, review and edit, and supervision; S.R.L.R.: literature review, conceptualization, methodology, data collection, writing – original draft, and review and edit; R.N.: literature review, methodology, formal analysis, writing – original draft, and review and edit; P.K.: literature review, methodology, writing – original draft, and review and edit. All the authors approved the final version of the manuscript.
Conflicts of interest disclosure
There are no conflicts of interest.
Research registration unique identifying number (UIN)
Name of registry: Research Registry.
Unique identifying number or registration: 9236.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-theregistry#home/registrationdetails/64a7951601f6990029e433ef/.
Guarantor
Yesha Shree Rajaure.
Provenance and peer review
Not commissioned, external peer review.
Data availability statement
Available upon reasonable request.
Acknowledgements
The authors are thankful to all the study participants (second year medical students) and the Principal.
The authors are thankful to all the second year medical students from Nepalese Army Institute of Health Sciences for their participation in this study.
Footnotes
Yesha Shree Rajaure and Bikalp Thapa equally contributing primary authors.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Yesha Shree Rajaure, Email: yeshashree.rajaure@naihs.edu.np.
Bikalp Thapa, Email: bikalp.thapa@naihs.edu.np.
Lee Budhathoki, Email: lee.budhathoki@naihs.edu.np.
Shavana R.L. Rana, Email: shavana.rana@naihs.edu.np.
Rajendra Neupane, Email: neupane.rajendra2016@gmail.com.
Parag Karki, Email: parag.karki@naihs.edu.np.
References
- 1.Michael J. Where’s the evidence that active learning works? Am J Physiol - Adv Physiol Educ 2006;30:19–67. [DOI] [PubMed] [Google Scholar]
- 2.Lam TP, Irwin M, Chow LW, et al. Early introduction of clinical skills teaching in a medical curriculum--factors affecting students’ learning. Med Educ 2002;36:233–240. [DOI] [PubMed] [Google Scholar]
- 3.Chen H, Kelly M, Hayes C, et al. The use of simulation as a novel experiential learning module in undergraduate science pathophysiology education. Adv Physiol Educ 2016;40:33–41. [DOI] [PubMed] [Google Scholar]
- 4.Bernardi S, Giudici F, Leone MF, et al. A prospective study on the efficacy of patient simulation in heart and lung auscultation. 2019;1–7. [DOI] [PMC free article] [PubMed]
- 5.Friederichs H, Weissenstein A, Ligges S, et al. Combining simulated patients and simulators: pilot study of hybrid simulation in teaching cardiac auscultation. Adv Physiol Educ 2014;38:343–347. [DOI] [PubMed] [Google Scholar]
- 6.Disler RT, Rochester SF, Kelly MA, et al. Delivering a large cohort simulation - beginning nursing students’ experience: a pre-post survey. J Nurs Educ Pract 2013;3:133–142. [Google Scholar]
- 7.Kelly MA, Hager P. Informal learning: relevance and application to health care simulation. Clin Simul Nurs 2015;11:376–382. [Google Scholar]
- 8.Rooney D, Hopwood N, Boud D, et al. The role of simulation in pedagogies of higher education for the health professions: through a practice-based lens. Vocat Learn 201;8:269–8. [Google Scholar]
- 9.McGaghie WC, Issenberg SB, Cohen ER, et al. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med J Assoc Am Med Coll 2011;86:706–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joseph N, Rai S, Jain A, et al. Perception towards problem based learning among medical students of a private medical college in South India. Br J Med Med Res 2015;9:1–10. [Google Scholar]
- 11.Mirza MB, Sulaiman A, Hashmi S, et al. Use of simulation based technology in pre-clinical years improves confidence and satisfaction among medical students. J Pak Med Assoc 2021;71:1296–1302. [DOI] [PubMed] [Google Scholar]
- 12.Kelly MA, Forbes JR, Carpenter C. Extending patient simulation: a novel prototype to produce tympanic thermal output. Simul Healthc 2012;7:192–195. [DOI] [PubMed] [Google Scholar]
- 13.Kaminsky J, Bianchi R, Eisner S, et al. Respiratory Auscultation Lab Using a Cardiopulmonary Auscultation Simulation Manikin. 2021;1–8. [DOI] [PMC free article] [PubMed]
- 14.Nepal Medical council . Accreditation standards for the MBBS (Bachelor of Medicine and Bachelor of Surgery). 2017;1–34. https://nmc.org.np/files/4/ACCREDITATIONSTANDARDSFORTHEMBBS.pdf
- 15.Medical Council of India . Competency based undergraduate curriculum for the Indian Medical Graduate volumes 1–3. [Internet]. https://www.nmc.org.in/information-desk/for-colleges/ug-curriculum
- 16.Mathew G, Agha R, for the STROCSS Group . STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg 2021;96:106165. [DOI] [PubMed] [Google Scholar]
- 17.Nassif J, Sleiman AK, Nassar AH, et al. Hybrid simulation in teaching clinical breast examination to medical students. J Cancer Educ 2019;34:194–200. [DOI] [PubMed] [Google Scholar]
- 18.Nuzzo A, Tran-Dinh A, Courbebaisse M, et al. University of Paris OSCE and SBT groups . Improved clinical communication OSCE scores after simulation-based training: Results of a comparative study. PLoS One 2020;1:e023842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arangalage D, Abtan J, Gaschignard J, et al. Implementation of a large-scale simulation-based cardiovascular clinical examination course for undergraduate medical students - a pilot study. BMC Med Educ 2019;19:361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Butter J, McGaghie WC, Cohen ER, et al. Simulation-based mastery learning improves cardiac auscultation skills in medical students. J Gen Intern Med 2010;25:780–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McKinney J, Cook DA, Wood D, et al. Simulation-based training for cardiac auscultation skills: systematic review and meta-analysis. J Gen Intern Med 2013;28:283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schroedl CJ, Corbridge TC, Cohen ER, et al. Use of simulation-based education to improve resident learning and patient care in the medical intensive care unit: a randomized trial. J Crit Care 2012;27:219.e7–219.e13. [DOI] [PubMed] [Google Scholar]
- 23.Akaike M, Fukutomi M, Nagamune M, et al. Simulation-based medical education in clinical skills laboratory. J Med Invest 2012;59:28–35. [DOI] [PubMed] [Google Scholar]
- 24.Martins RS, Sabzwari S, Iqbal M. Effectiveness of simulation-based clinical skills training for medical students in respiratory medicine: a pilot study. J Coll Physicians Surg Pak 2021;31:1468–1472. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available upon reasonable request.