Abstract
Purpose
We examine referral sources and clinical characteristics for youth presenting to an outpatient interdisciplinary pediatric chronic pain program.
Patients and Methods
Referral data were extracted from the electronic health record. PROMIS Pediatric Anxiety and Pain Interference Scales were administered at an initial evaluation visit.
Results
The program received 1488 referrals between 2016 and 2019, representing 1338 patients, with increasing volume of referrals over time. Referrals were primarily from orthopedics (19.6%), physical medicine and rehabilitation (18.8%), neurology (14.4%), and rheumatology (12.6%). Patients referred were primarily female (75.4%), White (80.1%), English-speaking (98.4%) adolescents (median=15.0 years). Of those referred, 732 (54.7%) attended an interdisciplinary evaluation (ie, with ≥2 disciplines). Adolescent anxiety was within the expected range by self-report (N=327, MT-score=55.67) and parent proxy-report (N=354, MT-score=57.70). Pain interference was moderately elevated by self-report (N=323, MT-score=61.52) and parent proxy-report (N=356, MT-score=64.02). There were no differences between patients referred who attended versus did not attend an interdisciplinary evaluation based on age, sex, ethnicity, or language. A smaller than expected proportion of referred Black patients (44%, P=0.02) and patients referred from orthopedics (40%) or pulmonology (11%) attended an evaluation, whereas a larger than expected proportion of those referred from physical medicine and rehabilitation (78%) were evaluated (P<0.001).
Conclusion
Results highlight the demand for outpatient interdisciplinary pediatric chronic pain treatment. Findings can inform decisions related to staffing and service design for pediatric hospitals that aim to establish or grow outpatient pediatric chronic pain programs.
Keywords: chronic pain, interdisciplinary, pediatric, referral, treatment
Introduction
Pediatric chronic pain is associated with increased risk for a wide range of functional impairments, including social difficulties,1 sleep problems,2 frequent school absences and decreased academic performance,3–5 elevated anxiety and depressive symptoms,6,7 and reduced quality of life.8 Families of youth with chronic pain also experience negative effects including missed days of work and lost employment,9 caregiving stress,10 and impaired family functioning.11 The financial burden of pediatric chronic pain on health-care systems is enormous, costing $19.5 billion dollars annually within the United States alone.9 Youth with untreated or poorly managed chronic pain are likely to continue to experience chronic pain and related disability into adulthood.6,12–17 In turn, chronic pain in adults results in an estimated economic burden of more than $600 billion each year because of health-care costs, lost work productivity, and disability programs.18
Comprehensive treatment for pediatric chronic pain involves interdisciplinary teams of health-care providers from various specialties, including but not limited to medicine, psychology, physical therapy, occupational therapy, psychiatry, nutrition, social work, and alternative or integrative medicine (eg, acupuncture, massage, and yoga).19 These providers work collaboratively with the patient and family to develop a treatment plan, often consisting of a combination of these services, with the ultimate goal of improving the youth’s functioning. Research demonstrates the effectiveness of interdisciplinary chronic pain treatment approaches, including improvements in functioning and reductions in distress.20–22 Interdisciplinary outpatient clinics are also a cost-effective approach for treating pediatric chronic pain.23
Unfortunately, interdisciplinary pediatric chronic pain treatment programs are limited in number, and emerging research suggests inequities in access to these services. According to childpain.org, there are only 90 interdisciplinary pediatric chronic pain treatment programs available worldwide. Across several studies, females were more likely than their male counterparts to be referred to chronic pain treatment programs.20,24,25 Additional predictors of referrals to pediatric chronic pain clinics include presence of generalized chronic pain, regional pain syndromes, mental health or musculoskeletal comorbidities, and recent hospitalization or surgery.25 Lower income and socioeconomic status are associated with increased risk of chronic pain,26 yet reduced access to and use of interdisciplinary chronic pain management services.27–29 Considering the high prevalence and substantial effects of pediatric chronic pain, additional interdisciplinary pediatric chronic pain treatment programs are urgently needed.30
To guide program development in ways that optimize efficient and equitable access to care for the diverse population of youth who experience chronic pain, understanding the characteristics of youth currently served in this setting is essential. This study sought to build on the existing literature by examining referral sources as well as sociodemographic and clinical characteristics of youth referred to an outpatient interdisciplinary pediatric chronic pain treatment program over a 4-year period. To identify potential disparities in access to these services, we also compared patients who attended versus did not attend an interdisciplinary evaluation within the program based on referral sources and sociodemographic characteristics.
Materials and Methods
Procedures
The Nemours Children’s Health Institutional Review Board reviewed this quality improvement study and determined that it did not require IRB oversight. Informed consent was not obtained, as the IRB concluded that this was not human subjects research. Referral orders placed for an interdisciplinary outpatient pediatric chronic pain treatment program within a mid-size children’s hospital (195 inpatient beds) located in the Mid-Atlantic region of the United States between January 1, 2016, and December 31, 2019, and associated patient demographic data were extracted directly from the electronic health record (EHR). The hospital is located within a tri-state area (PA, NJ, DE), which serves families from rural, suburban, and urban communities. There are 27 locations associated with the hospital system, including those that offer primary care, specialty care, and emergency services. The health system accepts both private and public insurance, including Medicaid, and serves a diverse patient population (eg, approximately 53% White, 24% Black, 12% Hispanic, 2% multiracial; 48% female; see Phan et al31 for more information on sociodemographic characteristics of patients served by this health system). For each referral order placed during this period, manual review of the EHR was conducted to ensure data quality (eg, removing duplicate or cancelled referral orders) and record information on patient attendance at subsequent evaluation visits with medical, psychological, occupational therapy, and/or physical therapy providers within the interdisciplinary chronic pain program. Questionnaires assessing pain interference and anxiety were mailed to families or provided during the check-in process at the initial program evaluation visit. There were no exclusion or inclusion criteria; all youth presenting to the clinic and their caregivers were invited to complete questionnaires.
This interdisciplinary outpatient chronic pain treatment program offers individualized treatment plans including weekly cognitive-behavioral therapy sessions with a licensed pediatric pain psychologist or a pediatric psychology trainee supervised by the licensed psychologist, weekly or twice weekly physical and/or occupational therapy, medication management by a physician or advanced practice nurse, and/or integrative therapies (ie, healing touch, yoga, and massage). Typical waitlist time for this treatment program is 4–6 weeks. Patient-reported data presented in this manuscript were collected prior to participation in the treatment program.
Measures
Demographics
Demographic characteristics for patients referred to the program, including age, sex, ethnicity, and race, were extracted directly from the EHR. Our hospital’s EHR uses sex, ethnicity, and race categories conforming to the US Department of Health & Human Services and the Office of Management and Budget data collection standards. These include the following categories: sex (Male, Female), ethnicity (Hispanic or Latino, Not Hispanic or Latino, Information Not Available, Refused), and race (American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, White, Some Other Race, Information Not Available, Refused). Patients or their parent/legal guardian can select one or more categories to describe their race; those who identified as more than one race were coded as “Multi-racial”.
PROMIS Pediatric Pain Interference Scale (v2.0, Short Form 8a)
This eight-item questionnaire assesses the extent to which pain interferes with functioning (eg, emotional, academic, and physical) over the past 7 days by self-report and parent proxy-report.32 Items are rated from 1 (never) to 5 (almost always). Normative data are available, and raw scores are transformed into T-scores. Higher scores indicate greater pain interference. This instrument has demonstrated strong psychometric properties.32 Internal reliability was good in the current sample for both the adolescent self-report (α=0.85) and parent proxy-report versions (α=0.86).
PROMIS Pediatric Anxiety Scale (v2.0, Short Form 8a)
This eight-item survey assesses symptoms of anxiety experienced by adolescents during the past 7 days by self-report and parent proxy-report. Items are rated on a 5-point Likert scale from 1 (never) to 5 (almost always).33 Raw scores are transformed into T-scores using normative data. Higher scores indicate greater anxiety. This questionnaire has demonstrated good psychometric properties,34 including among youth with chronic pain.35 Internal consistency was excellent in the current sample for both the adolescent self-report (α=0.94) and parent proxy-report versions (α=0.93).
Data Analysis
All analyses were conducted in SPSS, version 27. PROMIS measures were scored using the HealthMeasures Scoring Service (www.assessmentcenter.net/ac_scoringservice), which utilizes response pattern scoring to handle missing item-level data; among the subset who completed PROMIS measures, 0.66% (self-report) and 1.58% (parent-report) of all Pain Interference and 0.42% (self-report) and 1.24% (parent-report) of all Anxiety item responses were missing. Descriptive statistics were used to summarize referral sources and demographic and clinical characteristics of the sample. An independent samples t-test was used to compare age for patients referred who attended versus did not attend an interdisciplinary evaluation (ie, visits with chronic pain program providers from two or more disciplines). Chi-square tests were utilized to examine differences between patients referred who attended versus did not attend an interdisciplinary evaluation based on sex, race, ethnicity, language, and referral source. Alpha was set to 0.05 for all analyses.
Results
Patients Referred to the Program
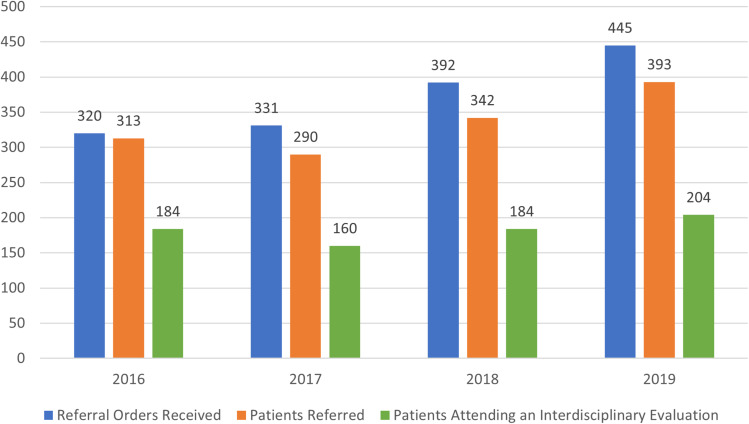
The program received 1488 referrals between January 2016 and December 2019 (M=372 referrals per calendar year; see Figure 1), representing 1338 unique patients. Referrals increased steadily over the study period, from 320 referrals in 2016 to 445 referrals in 2019. Referrals were primarily from orthopedics (19.6%), physical medicine and rehabilitation (18.8%), neurology (14.4%), rheumatology (12.6%), diagnostic medicine/consultative pediatrics (8.9%), psychology (7.5%), and gastroenterology (6.5%). Patients referred to the program were primarily female (75.4%), White (80.1%), non-Hispanic (92.7%), English-speaking (98.4%) adolescents (median age=15.0 years; see Table 1 for complete demographic characteristics).
Figure 1.
Referrals placed and patients evaluated within an interdisciplinary pediatric chronic pain treatment program between 2016 and 2019.
Notes: Some patients were referred to the program more than once within a given year. “Referral Orders Received” represents all referrals placed to the program, whereas “Patients Referred” represents unique patients referred to the program.
Table 1.
Demographic Characteristics of Patients Referred to an Interdisciplinary Pediatric Chronic Pain Program Between 2016 and 2019 (N=1338) and Those Who Attended an Evaluation (N=732)
| Characteristic | Patients Referred to Program (N=1338) | Patients Attending an Evaluation (N=732) |
|---|---|---|
| N (%) | N (%) | |
| Sex | ||
| Female | 1009 (75.4%) | 560 (76.5%) |
| Male | 329 (24.6%) | 172 (23.5%) |
| Race | ||
| White | 1071 (80.1%) | 596 (81.4%) |
| Black or African American | 123 (9.2%) | 54 (7.4%) |
| Some Other Race | 76 (5.7%) | 46 (6.3%) |
| Multiracial | 38 (2.8%) | 25 (3.4%) |
| Asian | 17 (1.1%) | 7 (0.9%) |
| Declined to Report | 9 (0.7%) | 2 (0.3%) |
| American Indian or Alaska Native | 2 (0.1%) | 2 (0.3%) |
| Hawaiian Native or Other Pacific Islander | 1 (0.1%) | – |
| Ethnicity | ||
| Not Hispanic or Latino | 1240 (92.7%) | 678 (92.6%) |
| Hispanic or Latino | 84 (6.3%) | 46 (6.3%) |
| Declined to Report | 14 (1.0%) | 8 (1.1%) |
| Preferred Language | ||
| English | 1317 (98.4%) | 723 (98.8%) |
| Spanish | 16 (1.2%) | 7 (1.0%) |
| Other or Unknown | 4 (0.3%) | 2 (0.2%) |
| American Sign | 1 (0.1%) | – |
| Referring Department | ||
| Orthopedics | 273 (20.4%) | 109 (14.9%) |
| Physical Medicine and Rehabilitation | 263 (19.7%) | 206 (28.1%) |
| Neurology | 180 (13.5%) | 98 (13.4%) |
| Rheumatology | 174 (13.0%) | 100 (13.7%) |
| Diagnostic Referral | 116 (8.7%) | 58 (7.9%) |
| Psychology | 100 (7.5%) | 55 (7.5%) |
| Gastroenterology | 86 (6.4%) | 41 (5.6%) |
| Inpatient Pediatrics | 40 (3.0%) | 21 (2.9%) |
| Urology | 23 (1.7%) | 9 (1.2%) |
| Hematology/Oncology | 13 (1.0%) | 5 (0.7%) |
| Neuropsychology | 10 (0.7%) | 4 (0.5%) |
| Pulmonology | 9 (0.7%) | 1 (0.1%) |
| Adolescent Medicine | 8 (0.6%) | 5 (0.7%) |
| Emergency Medicine | 7 (0.5%) | 3 (0.4%) |
| Primary Care | 6 (0.4%) | 4 (0.5%) |
| Infectious Disease | 5 (0.4%) | 2 (0.3%) |
| Otolaryngology | 5 (0.4%) | 3 (0.4%) |
| Genetics | 4 (0.3%) | 2 (0.3%) |
| Neurosurgery | 3 (0.2%) | – |
| Palliative Care | 3 (0.2%) | – |
| Nephrology | 2 (0.1%) | – |
| Physical Therapy | 2 (0.1%) | 1 (0.1%) |
| Weight Management | 2 (0.1%) | 2 (0.3%) |
| Cardiology | 1 (0.1%) | 1 (0.1%) |
| Integrative Medicine | 1 (0.1%) | – |
| Psychiatry | 1 (0.1%) | 1 (0.1%) |
| Surgery | 1 (0.1%) | 1 (0.1%) |
| Range (M, SD) | Range (M, SD) | |
| Age (years) | 2–21 (13.92, 2.80) | 4–21 (13.90, 2.78) |
Notes: Demographic data were extracted from the electronic health record. For patients who were referred more than once to the program, demographic data at the time of their initial referral are included here.
Patients Attending an Initial Evaluation Visit
Of the patients referred to the pediatric chronic pain treatment program (N=1338), 934 (69.8%) were evaluated by at least one provider within the program (ie, medical, psychology, physical therapy, and/or occupational therapy). Of these, 732 patients (78.4%) attended an interdisciplinary evaluation visit (ie, evaluated by two or more disciplines) within the pediatric chronic pain treatment program. Patients who attended an interdisciplinary evaluation visit (N=732) were predominantly female (76.5%), White (81.4%), non-Hispanic (92.6%), English-speaking (98.8%) adolescents (median age=14.0 years; see Table 1). These patients were primarily referred from physical medicine and rehabilitation (28.1%), orthopedics (14.9%), rheumatology (13.7%), neurology (13.4%), diagnostic medicine/consultative pediatrics (7.9%), psychology (7.5%), and gastroenterology (5.6%; see Table 1 for complete list of referring departments). The proportion of patients referred to the program who attended an interdisciplinary evaluation declined slightly across the study period, from 58.8% in 2016 to 51.9% in 2019 (see Figure 1).
The subset of patients who attended an initial interdisciplinary evaluation visit within the program and completed PROMIS measures demonstrated anxiety within the expected range for the general population by both self-report (N=327, MT-score=55.67, SD=13.01) and parent proxy-report (N=354, MT-score=57.70, SD=11.95) and moderately elevated pain interference by self-report (N=323, MT-score=61.52, SD=8.44) and parent proxy-report (N=356, MT-score=64.02, 6.83).
There were no differences between patients referred who attended (N=732) versus did not attend an interdisciplinary evaluation (N=606) based on age (t(1336)=.36, P=0.72), sex (X2(1)=1.04, p=0.31), ethnicity (X2(1)<.001, P=0.99), or language (X2(4)=3.38, P=0.50). There were significant differences based on race, with a smaller proportion of referred Black or African American patients attending an evaluation visit (44%) than expected (X2(4)=12.27, P=0.02, Cramer’s V=0.096). There were also differences based on referring departments, with a smaller than expected proportion of patients referred from orthopedics (n=109, 40%) and from pulmonology (n=1, 11%) and a greater than expected proportion of patients referred from physical medicine and rehabilitation (n=206, 78%) attending an initial evaluation visit (X2(26)=114.57, P<0.001, Cramer’s V=0.29).
Discussion
This study examined referral sources, demographic information, and clinical characteristics of youth referred and presenting to an outpatient interdisciplinary pediatric chronic pain program. Results highlight the high demand for outpatient interdisciplinary pediatric chronic pain treatment, with steadily increasing referrals placed over the 4-year period from a wide variety of specialists within the hospital system. This study can serve as a model for examining potential disparities in referral and access to pediatric chronic pain programs in other clinical settings through use of data that are readily available in most EHRs. Findings can inform decisions related to staffing and service design for other pediatric hospitals that aim to establish or grow outpatient pediatric chronic pain programs, with an emphasis on health equity.
On average, our interdisciplinary outpatient pediatric chronic pain program received 372 referrals per year, with a trend of increasing volume of referrals over time. There is a paucity of published data on the number of referrals placed and patients served by outpatient interdisciplinary pain programs within the United States. In one study examining outpatient chronic pain clinic referrals at a large Midwestern children’s hospital over a 5-year period, 778 adolescents were identified as potentially eligible for a referral because of a chronic pain diagnosis, yet only 96 (12%) were subsequently referred to the clinic.25 An outpatient interdisciplinary pain clinic within a large West Coast children’s hospital reported serving approximately 350 patients annually.23 Given that this study was conducted in a comparatively smaller children’s hospital, our high referral volume is notable. Additional research is needed to examine referral patterns for interdisciplinary pain programs, including the potential influence of contextual factors such as hospital size and catchment area, pain management approaches provided through other services, and variation between individual providers.
Interestingly, we found several differences in attendance at the initial interdisciplinary pain program evaluation by referral source. Specifically, a lower than expected proportion of patients referred by pulmonology and orthopedics underwent an interdisciplinary program evaluation. Conversely, a greater than expected proportion of patients referred by physical medicine and rehabilitation (PMR) completed an interdisciplinary evaluation visit. Given that very few patients were referred by pulmonology during the study period, this finding may represent statistical error. On the other hand, orthopedics and PMR were two of the largest referral sources to the program within our hospital. Despite referring a similar number of patients (orthopedics: n=273, PMR: n=263), only 40% of those referred from orthopedics participated in an interdisciplinary evaluation versus 78% of those referred from PMR. At our hospital, one physician within PMR also provides services through the interdisciplinary pain program and is active in educating PMR colleagues and trainees on chronic pain. As such, it may be that enhanced education around chronic pain for both PMR health-care providers and youth and families seen by this service facilitates more appropriate referrals to the program and/or allows for greater follow-through with attending an interdisciplinary program evaluation. In addition, youth referred by orthopedics may be more likely to have experienced an injury resulting in acute rather than persistent pain. Additional research is needed to examine how pain education and management approaches within medical subspecialties may influence the referral process to pediatric chronic pain programs.
Patients referred to this outpatient chronic pain program were largely White, non-Hispanic, English-speaking, adolescent females. It is also notable that a smaller than expected proportion of Black or African American patients who were referred to the program attended an interdisciplinary evaluation. These findings are consistent with prior research, which suggests that patients who are referred and served by interdisciplinary pediatric chronic pain clinics are primarily White, female adolescents.22,25,36 A robust body of work highlights the role of implicit bias, prejudice, and systemic racism in perpetuating disparities in pain management.37–39 For example, pediatricians with high implicit pro-White bias are less likely to recommend opioids for Black children.40 In addition, a significant subset of medical trainees endorses implicit attitudes that Black people feel less pain38 or are more pain-tolerant than White people.41 In instances of high clinical or diagnostic uncertainty (eg, chronic pain), these biases may be especially likely to be activated40 and influence treatment recommendations, including referral to specialized pain care services, and the ways in which these recommendations are communicated to patients and families. In addition, barriers to accessing healthcare (eg, inadequate insurance coverage, limited transportation, inflexible employment, and inadequate language translation services) that disproportionally impact marginalized communities may result in disparities in receiving interdisciplinary pain care even when referrals are made.27–29
Several potential clinical implications can be drawn from these findings. Inadequate pain education for health-care providers has been widely recognized as a leading contributor to poorly managed pain,18 with 96% of medical schools in the United States and United Kingdom lacking compulsory pain medicine courses.42 Similar deficiencies in pain education have also been identified across other health sciences programs.43,44 When pain is incorporated into curricula for health-care providers, physiological systems and pharmacological treatments are prioritized,42 despite decades of evidence supporting the biopsychosocial model and interdisciplinary approaches to pain management.45 Improving pain education for health-care providers (eg, mandatory curricula and interprofessional education opportunities) may enhance referrals to interdisciplinary chronic pain treatment programs by both ensuring that the patients who would most benefit from these programs are identified and that accurate information is provided to families receiving these referrals. However, these changes must go beyond addressing inadequate or outdated knowledge and include strategies for health-care providers to identify and actively dismantle their own biases to prevent harm to oppressed and historically marginalized groups experiencing pain. Moreover, changes at the health-care systems level are necessary, such as implementing standardized chronic pain prognostic screening tools to help guide referral decisions, EHR workflows that automate referrals based on pre-specified criteria, and incorporating social determinants of health data that are increasingly available in the EHR into the scheduling process for chronic pain clinics (eg, offering social work supports in instances where insurance or transportation challenges have been identified) and may help to ensure more efficient and equitable access to interdisciplinary pain care services.
Limitations of this work should be considered when interpreting our findings. First, sociodemographic characteristics were extracted from the EHR and may not always accurately reflect how youth identify their gender, racial, or ethnic background. We also were not able to collect or analyze detailed information regarding patients’ medical histories, chronic pain diagnoses, or health insurance coverage. Future research should explore associations between these variables and interdisciplinary chronic pain program referrals and service utilization. We were also unable to calculate average time from referral to initial evaluation in this sample, as date of evaluation was not extracted during our manual review of EHRs. This is a high priority area for further investigation, as lengthy waitlists may have negative impacts on quality of life for adults with chronic pain,46 and wait times appear highly variable for pediatric chronic pain treatment programs.47,48 This study was conducted within one Mid-Atlantic pediatric hospital in the United States; multisite collaborative research is needed to examine referrals and access to interdisciplinary treatment programs at broader regional, national, or international levels, which may highlight contextual factors driving potential disparities in referral and access to care for youth with chronic pain. Additional research is also needed to more closely examine how patients, families, and clinicians make decisions regarding referral to specialized chronic pain programs and specific barriers to participating in interdisciplinary pain care services.
Conclusion
This study documented referral sources, demographic information, and clinical characteristics of youth referred to and evaluated by an outpatient interdisciplinary pediatric chronic pain program. Findings underline the demand for outpatient interdisciplinary pain clinics and may help guide program design and development in other pediatric health-care settings that aim to expand their capacity to effectively serve youth experiencing chronic pain. In addition, this study highlights how standardized tracking of referrals and service uptake can inform targeted strategies to ensure equity in access to and utilization of interdisciplinary pain care services.
Acknowledgement
Publication made possible in part by support from the Nemours Grants for Open Access from Library Services.
Disclosure
The authors report no conflicts of interest or financial support for this work.
References
- 1.Forgeron PA, King S, Stinson JN, McGrath PJ, MacDonald AJ, Chambers CT. Social functioning and peer relationships in children and adolescents with chronic pain: a systematic review. Pain Res Manag. 2010;15(1):27–41. doi: 10.1155/2010/820407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pavlova M, Ference J, Hancock M, Noel M. Disentangling the sleep-pain relationship in pediatric chronic pain: the mediating role of internalizing mental health symptoms. Pain Res Manag. 2017;2017:1586921. doi: 10.1155/2017/1586921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Groenewald CB, Giles M, Palermo TM. School absence associated with childhood pain in the United States. Clin J Pain. 2019;35(6):525–531. doi: 10.1097/AJP.0000000000000701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Groenewald CB, Tham SW, Palermo TM. Impaired school functioning in children with chronic pain: a national perspective. Clin J Pain. 2020;36(9):693–699. doi: 10.1097/AJP.0000000000000850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Logan DE, Simons LE, Stein MJ, Chastain L. School impairment in adolescents with chronic pain. J Pain. 2008;9(5):407–416. doi: 10.1016/j.jpain.2007.12.003 [DOI] [PubMed] [Google Scholar]
- 6.Noel M, Groenewald CB, Beals-Erickson SE, Gebert JT, Palermo TM. Chronic pain in adolescence and internalizing mental health disorders: a nationally representative study. Pain. 2016;157(6):1333–1338. doi: 10.1097/j.pain.0000000000000522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simons LE, Sieberg CB, Claar RL. Anxiety and impairment in a large sample of children and adolescents with chronic pain. Pain Res Manag. 2012;17(2):93–97. doi: 10.1155/2012/420676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kashikar-Zuck S, Zafar M, Barnett K, et al. Quality of life and emotional functioning in youth with chronic migraine and juvenile fibromyalgia. Clin J Pain. 2013;29(12):1066–1072. doi: 10.1097/AJP.0b013e3182850544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Groenewald CB, Essner BS, Wright D, Fesinmeyer MD, Palermo TM. The economic costs of chronic pain among a cohort of treatment-seeking adolescents in the United States. J Pain. 2014;15(9):925–933. doi: 10.1016/j.jpain.2014.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eccleston C, Crombez G, Scotford A, Clinch J, Connell H. Adolescent chronic pain: patterns and predictors of emotional distress in adolescents with chronic pain and their parents. Pain. 2004;108(3):221–229. doi: 10.1016/j.pain.2003.11.008 [DOI] [PubMed] [Google Scholar]
- 11.Lewandowski AS, Palermo TM, Stinson J, Handley S, Chambers CT. Systematic review of family functioning in families of children and adolescents with chronic pain. J Pain. 2010;11(11):1027–1038. doi: 10.1016/j.jpain.2010.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brna P, Dooley J, Gordon K, Dewan T. The prognosis of childhood headache: a 20-year follow-up. Arch Pediatr Adolesc Med. 2005;159(12):1157–1160. doi: 10.1001/archpedi.159.12.1157 [DOI] [PubMed] [Google Scholar]
- 13.Hassett AL, Hilliard PE, Goesling J, Clauw DJ, Harte SE, Brummett CM. Reports of chronic pain in childhood and adolescence among patients at a tertiary care pain clinic. J Pain. 2013;14(11):1390–1397. doi: 10.1016/j.jpain.2013.06.010 [DOI] [PubMed] [Google Scholar]
- 14.Horst S, Shelby G, Anderson J, et al. Predicting persistence of functional abdominal pain from childhood into young adulthood. Clin Gastroenterol Hepatol. 2014;12(12):2026–2032. doi: 10.1016/j.cgh.2014.03.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Larsson B, Sigurdson JF, Sund AM. Long-term follow-up of a community sample of adolescents with frequent headaches. J Headache Pain. 2018;19(1):79. doi: 10.1186/s10194-018-0908-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murray CB, Groenewald CB, de la Vega R, Palermo TM. Long-term impact of adolescent chronic pain on young adult educational, vocational, and social outcomes. Pain. 2020;161(2):439–445. doi: 10.1097/j.pain.0000000000001732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walker LS, Dengler-Crish CM, Rippel S, Bruehl S. Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. Pain. 2010;150(3):568–572. doi: 10.1016/j.pain.2010.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. The National Academies Collection: reports funded by National Institutes of Health. In: Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US); 2011. [PubMed] [Google Scholar]
- 19.Odell S, Logan DE. Pediatric pain management: the multidisciplinary approach. J Pain Res. 2013;6:785–7890. doi: 10.2147/JPR.S37434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bruce BK, Ale CM, Harrison TE, et al. Getting back to living: further evidence for the efficacy of an interdisciplinary pediatric pain treatment program. Clin J Pain. 2017;33(6):535–542. doi: 10.1097/AJP.0000000000000433 [DOI] [PubMed] [Google Scholar]
- 21.Coakley R, Wihak T. Evidence-based psychological interventions for the management of pediatric chronic pain: new directions in research and clinical practice. Children (Basel). 2017;4(2):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simons LE, Logan DE, Chastain L, Cerullo M. Engagement in multidisciplinary interventions for pediatric chronic pain: parental expectations, barriers, and child outcomes. Clin J Pain. 2010;26(4):291–299. doi: 10.1097/AJP.0b013e3181cf59fb [DOI] [PubMed] [Google Scholar]
- 23.Mahrer NE, Gold JI, Luu M, Herman PM. A cost-analysis of an interdisciplinary pediatric chronic pain clinic. J Pain. 2018;19(2):158–165. doi: 10.1016/j.jpain.2017.09.008 [DOI] [PubMed] [Google Scholar]
- 24.Cucchiaro G, Schwartz J, Hutchason A, Ornelas B. Chronic pain in children: a look at the referral process to a pediatric pain clinic. Int J Pediatr. 2017;2017:8769402. doi: 10.1155/2017/8769402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tumin D, Miller R, Hakim M, et al. Predictors of referral to a pediatric outpatient chronic pain clinic. Clin J Pain. 2019;35(3):205–211. doi: 10.1097/AJP.0000000000000664 [DOI] [PubMed] [Google Scholar]
- 26.Tran ST, Koven ML, Castro AS, Goya Arce AB, Carter JS. Sociodemographic and environmental factors are associated with adolescents’ pain and longitudinal health outcomes. J Pain. 2020;21(1–2):170–181. doi: 10.1016/j.jpain.2019.06.007 [DOI] [PubMed] [Google Scholar]
- 27.Jay MA, Howard RF. Inequalities in access to a tertiary children’s chronic pain service: a cross-sectional study. Arch Dis Child. 2016;101(7):657–661. doi: 10.1136/archdischild-2015-310280 [DOI] [PubMed] [Google Scholar]
- 28.Ruhe AK, Wager J, Hirschfeld G, Zernikow B. Household income determines access to specialized pediatric chronic pain treatment in Germany. BMC Health Serv Res. 2016;16:140. doi: 10.1186/s12913-016-1403-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Toliver-Sokol M, Murray CB, Wilson AC, Lewandowski A, Palermo TM. Patterns and predictors of health service utilization in adolescents with pain: comparison between a community and a clinical pain sample. J Pain. 2011;12(7):747–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hechler T, Dobe M, Zernikow B. Commentary: a worldwide call for multimodal inpatient treatment for children and adolescents suffering from chronic pain and pain-related disability. J Pediatr Psychol. 2010;35(2):138–140. doi: 10.1093/jpepsy/jsp066 [DOI] [PubMed] [Google Scholar]
- 31.Phan T-LT, Enlow PT, Lewis AM, et al. Persistent disparities in pediatric health care engagement during the COVID-19 Pandemic. Public Health Rep. 2023;138(4):633–644. doi: 10.1177/00333549231163527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varni JW, Stucky BD, Thissen D, et al. PROMIS pediatric pain interference scale: an item response theory analysis of the pediatric pain item bank. J Pain. 2010;11(11):1109–1119. doi: 10.1016/j.jpain.2010.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Irwin DE, Stucky B, Langer MM, et al. An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Qual Life Res. 2010;19(4):595–607. doi: 10.1007/s11136-010-9619-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Varni JW, Magnus B, Stucky BD, et al. Psychometric properties of the PROMIS® pediatric scales: precision, stability, and comparison of different scoring and administration options. Qual Life Res. 2014;23(4):1233–1243. doi: 10.1007/s11136-013-0544-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kashikar-Zuck S, Carle A, Barnett K, et al. Longitudinal evaluation of patient-reported outcomes measurement information systems measures in pediatric chronic pain. Pain. 2016;157(2):339–347. doi: 10.1097/j.pain.0000000000000378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zernikow B, Wager J, Hechler T, et al. Characteristics of highly impaired children with severe chronic pain: a 5-year retrospective study on 2249 pediatric pain patients. BMC Pediatr. 2012;12:54. doi: 10.1186/1471-2431-12-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain. 2009;10(12):1187–1204. doi: 10.1016/j.jpain.2009.10.002 [DOI] [PubMed] [Google Scholar]
- 38.Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A. 2016;113(16):4296–4301. doi: 10.1073/pnas.1516047113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mossey JM. Defining racial and ethnic disparities in pain management. Clin Orthop Relat Res. 2011;469(7):1859–1870. doi: 10.1007/s11999-011-1770-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health. 2012;102(5):988–995. doi: 10.2105/AJPH.2011.300621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miller MM, Williams AE, Zapolski TCB, Rand KL, Hirsh AT. Assessment and treatment recommendations for pediatric pain: the influence of patient race, patient gender, and provider pain-related attitudes. J Pain. 2020;21(1–2):225–237. doi: 10.1016/j.jpain.2019.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shipton EE, Bate F, Garrick R, Steketee C, Shipton EA, Visser EJ. Systematic review of pain medicine content, teaching, and assessment in medical school curricula internationally. Pain Ther. 2018;7(2):139–161. doi: 10.1007/s40122-018-0103-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Darnall BD, Scheman J, Davin S, et al. Pain psychology: a global needs assessment and national call to action. Pain Med. 2016;17(2):250–263. doi: 10.1093/pm/pnv095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Doorenbos AZ, Gordon DB, Tauben D, et al. A blueprint of pain curriculum across prelicensure health sciences programs: one NIH pain consortium center of excellence in pain education (CoEPE) experience. J Pain. 2013;14(12):1533–1538. doi: 10.1016/j.jpain.2013.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gatchel RJ, Kishino ND, Watts L, Bevers K. The biopsychosocial model of the assessment, prevention, and treatment of chronic pain. US Neurol. 2016;12(2):98–104. [Google Scholar]
- 46.Lynch ME, Campbell F, Clark AJ, et al. A systematic review of the effect of waiting for treatment for chronic pain. Pain. 2008;136(1–2):97–116. doi: 10.1016/j.pain.2007.06.018 [DOI] [PubMed] [Google Scholar]
- 47.Peng P, Stinson JN, Choiniere M, et al. Dedicated multidisciplinary pain management centres for children in Canada: the current status. Can J Anaesth. 2007;54(12):985–991. doi: 10.1007/BF03016632 [DOI] [PubMed] [Google Scholar]
- 48.Palermo TM, Slack M, Zhou C, Aaron R, Fisher E, Rodriguez S. Waiting for a pediatric chronic pain clinic evaluation: a prospective study characterizing waiting times and symptom trajectories. J Pain. 2019;20(3):339–347. doi: 10.1016/j.jpain.2018.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]