Abstract
Background
The COVID-19 epidemic generated different forms of stress. From this period, there has been a remarkable increase in the quantity of studies on stress conducted by scholars. However, few used bibliometric analyses to focus on overall trends in the field.
Purpose
This study sought to understand the current status and trends in stress development during COVID-19, as well as the main research drives and themes in this field.
Methods
2719 publications from the Web of Science(WOS) core repository on stress during COVID-19 were analyzed by utilizing Co-Occurrence (COOC), VOS viewer, and Cite Space bibliometric software. The overall features of research on stress during COVID-19 were concluded by analyzing the quantity of publications, keywords, countries, and institutions.
Results
The results indicated that the United States had the largest number of publications and collaborated closely with other countries with each other. University of Toronto was the most prolific institution worldwide. Visualization and analysis demonstrated that the influence of stress during COVID-19 on the work, life, mental and spiritual dimensions is a hot research topic. Among other things, the frequency of each keyword in research on stress during COVID-19 increased from 2021 to 2022, and the researchers expanded their scope and study population; the range of subjects included children, nurses, and college students, as well as studies focusing on different types of stress, and emphasizing the handling of stress.
Conclusion
Our findings reveal that the heat of stress research during COVID-19 has declined, and the main research forces come from the United States and China. Additionally, subsequent research should concern more on coping methods with stress, while using more quantitative and qualitative studies in the future.
Keywords: COOC analysis, VOS viewer, Cite Space, stress during COVID-19, bibliometric analysis
1. Introduction
Since December 2019, the COVID-19 pandemic, generated by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), has impacted people and systems around the globe. Due to the high transmission and mortality rates of the disease, as well as the continuous media coverage, it has attracted a significant attention, thereby elevating stress levels and anxiety, and causing social panic (1–4). When people are in a state of extreme stress, they tend to experience a series of psychological problems such as anxiety and depression (5–9). Moreover, the forceful variation in daily lifestyle due to the pandemic enhances the development of poor mental health conditions and behaviors, such as alcohol abuse, lack of exercise, and insomnia (10–13). Therefore, research related to stress during the COVID-19 period plays an essential role for keeping individuals in good mental health.
Current research on stress during COVID-19 has focused on four primary areas: causes of stress, influential elements, impacts on individuals, and relief measures. First, on the formation causes of stress during COVID-19, the COVID-19 lockdown enhanced changes in human lifestyles, thereby increasing the incidence of anxieties, stresses and depressions and creating a wide range of stresses (14–17). For instance, for remote workers, the COVID-19 lockdown rendered work technologically more stressful (18–21). Second, scholars investigated the influence of stress during COVID-19 on individual, institutional, and societal levels (22–25). Sagherian et al. demonstrated that optimizing nursing schedules and practices reduced stress among nursing staff (26). Third, regarding the human impact of stress during COVID-19, stress during COVID-19 affects the daily life of different population groups (college students, pregnant women, and healthcare workers, among others), and enhances mental health problems (27–31). For example, the study found that the COVID-19 epidemic negatively impacted the psychological well-being of undergraduate medical students, with increased incidence as well as levels of anxiety and stress (32–35). Fourth, in terms of methods of stress relief during COVID-19, scholars have explored ways to relieve stress, such as improving lifestyle and adopting positive health behaviors (36–40). Mattioli et al. demonstrated that isolation is associated with stress and depression, and that global action must be engendered to support healthy diet and physical activity, thereby promoting good lifestyles (41). In addition, utilizing external group music therapy with group speech therapy during COVID-19 lead to better stress management (42).
Despite many studies on stress during COVID-19, most have specific inclinations, and lack a holistic perspective and a systematic analysis of the literature in this field using bibliometric methods. For example, Khanal et al. focused on factors related to anxiety, depression, and insomnia within the healthcare workforce during the pandemic (43), whereas Tabur et al. focused on job stress, social support, and turnover intention among the same group (44). Even the review literature mostly focused on specific aspects of different population groups (older adults, adolescents, pregnant women, college students, and healthcare workers), and research methods used are mostly meta-analyses that waives the application of bibliometric methods for systematically analyzing the literature (45–47). Safi-keykaleh et al. utilized meta-analysis to assess the incidence of postpartum depression during COVID-19 (48). In addition, Chutiyami et al. utilized meta-analysis to synthesize the overall psychological well-being of healthcare professionals during COVID-19 (49). Therefore, it is important to perform a systematic analysis of stress research during COVID-19 using bibliometrics to evaluate the present state of application and developmental trends in the field.
Moreover, bibliometric analysis is a valuable tool for quantitative assessment of various parameters associated with scientific publications in a given area, revealing insights into prevalent research topics, developmental trends, critical researchers, and scientific organizations (50). However, articles in this area of stress during COVID-19 waived the method of bibliometric to analyze literature. Therefore, we employed an innovated method of literature review by a systematic review using COOC, VOS viewer and Cite space software as research tools. Besides, the use of COOC and VOS viewer allows visual analysis and mapping of scientific knowledge to demonstrate the structure, evolution, cooperation and other relationships in the field (51). Moreover, Cite Space software presents the structure of knowledge in a specific research area and summarizes trends in the development and evolution of that domain (52). A systematic literature review is a way of locating, evaluating and synthesizing evidence, as well as an orderly way of reviewing and summarizing research findings (53). This makes it significant during COVID-19. For instance, the analyze of the literature can characterize the overall magnitude of stress and depressive symptoms caused by the COVID-19 outbreak, which will lead policymakers to more judiciously measure the burden caused by similar public health events (54, 55). Thus, it is vital to conduct systematic reviews of previous relevant publications on stress during COVID-19 in order to realize the current state of application and trends of stress during large-scale public health events. Specifically, the six following research questions were proposed:
RQ 1: What are the dynamics of literature issuance in the field of stress during COVID-19 epidemic according to volume and frequency of citations?
RQ 2: Which countries, institutions and authors are more prolific based on the volume of publications?
RQ 3: What is the collaboration between countries, institutions and authors?
RQ 4: Based on citation frequency, which articles are important in the area of stress during COVID-19?
RQ 5: What are the research topics of interest in the field of stress during COVID-19?
RQ 6: What is the trend of research evolution in the field of stress during COVID-19?
2. Methodology
2.1. Data collection and pre-processing
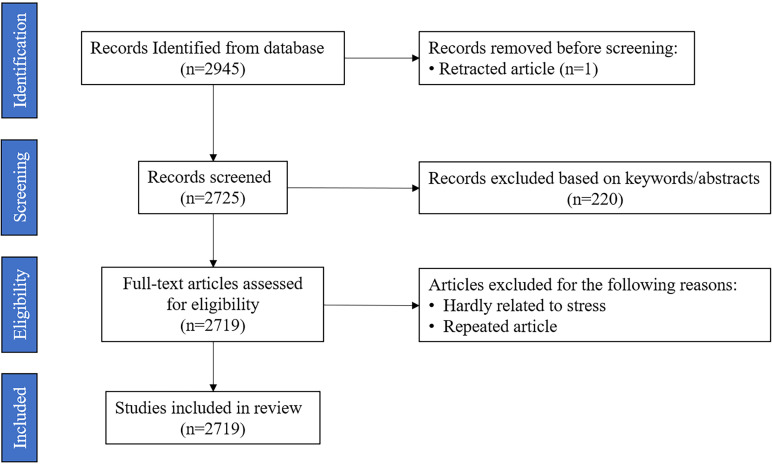
This study was implemented on June 15, 2023, where data was collected from relevant literature in Web of Science (WOS)—a comprehensive, multidisciplinary, core journal citation indexing database—which is a common tool for bibliometrics. The data utilized in this study are derived from the WOS Core Collection, with a search date of June 15, 2023. To ensure the accuracy of the search, this study followed the PRISMA guidelines for literature collection, and constructed the search formula TS = “Stress” AND “During COVID-19”, the language was “English”, the literature types were “Dissertation”, “Online publication”, “Review paper”, and the time was not limited; this study obtained 2,946 papers (see Figure 1 ). After manual screening, 2,719 valid papers were retained.
Figure 1.
Flowchart of the data collection.
Data preprocessing was the first part of data analysis. The following data preprocessing steps were implemented in this study. First, the researcher exported the full records of retrieved articles and cited references in plain text format. Second, key elements of all articles (year, citation frequency, title, author keywords, additional keywords, journal, author, institution, and country) were extracted into.elsx files. Third, duplicate articles were removed. Fourth, missing elements were added in the articles. Fifth, irrelevant terms were screened and excluded, and synonyms were merged. Sixth, the format of the elements was standardized by removing extra spaces and punctuation.
2.2. Research tools and data processing methods
Visualization helps to analyze, and explore large-scale and complex data. In this study, COOC, VOS viewer and Cite Space software were used as research analysis tools. First, COOC software was used to count the valid literature. Second, VOS viewer and Cite Space software were used to analyze the partnerships, and key themes of the research topic of stress during COVID-19.
Part I: COOC Analysis Procedure
In the WOS database, 2,946 articles were retrieved from 2020 to 2023 using a search formula, and 2,719 articles meeting the inclusion criteria were screened after data preprocessing using COOC software. Afterwards, the COOC software was used to analyze the valid literature, and the chronological volume and evolutionary trend maps were generated.
Part II: VOS viewer and Cite Space analysis program
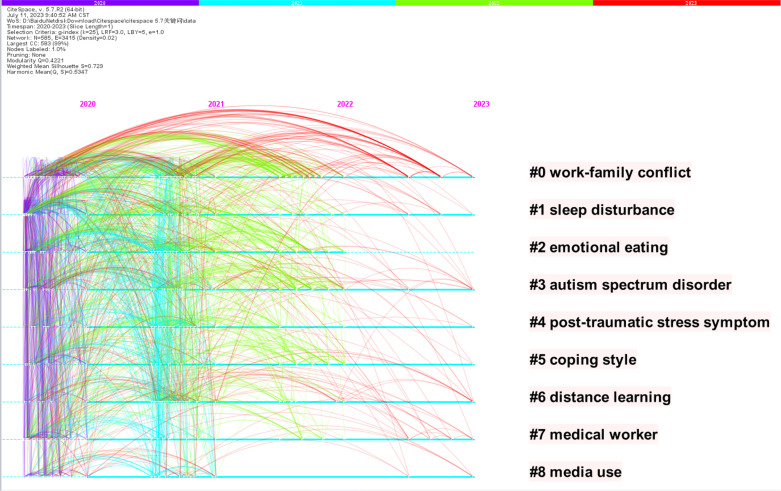
For analyzing collaborative relationships and critical topics, this study relied on the data processed by the COOC software and used the VOS viewer to map the collaborative networks of nations, institutions, and authors, as well as keyword clustering maps. This study equally analyzed the literature descriptively by counting the quantity of publications, authors, nations, institutions, cited literature, as well as authors’ keywords. In particular, the data restriction for the mapping was countries with more than 5 publications, institutions with more than 15 publications, authors with more than 5 publications, and author keywords with more than 10 occurrences. Furthermore, the pre-processed WOS data was imported into Cite Space and analyzed in order to report clustering labels. In Figure 2 , 9 clustering labels were generated using Cite Space, with the largest cluster being work-family conflict (#0), active from 2020 to 2023. The second largest cluster was sleep disorders (#1), active from 2020 to 2023. The third to tenth largest clusters were emotional eating (#2), autism spectrum disorder (#3), post-traumatic stress disorder (#4), coping styles (#5), distance learning (#6), healthcare workers (#7), and media use (#8).
Figure 2.
Cluster labels and terms produced between 2020 and 2023.
3. Results
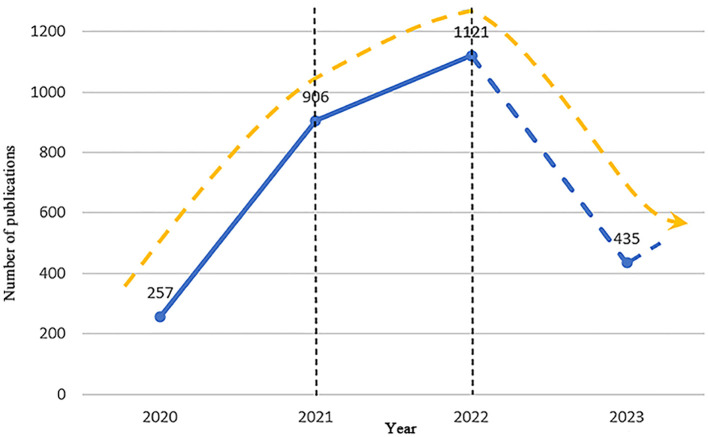
3.1. Documentation developments
The valid sample selected for this study consisted of 2,719 articles with 13,502 authors affiliated with 4,028 institutions in 115 countries, citing 92,558 references 5,256 author keywords. From Figure 3 , the growth in the quantity of papers related to stress during the COVID-19 period can be divided into three phases: the phase of rapid growth, the phase of stable growth, and the phase of quality enhancement. A phase of rapid growth occurred between 2020 and 2021, with a significant increase in the quantity of articles published, by a rate of 649 articles in one year. The stable growth phase occurred from 2021 to 2022, with slower growth within the year compared with the previous phase, with an increase rate of 215 articles in one year. The quality improvement phase occurred from 2022 to 2023, with a substantial decrease in the number of articles published in this phase compared to the previous phase, and as of June 15, 2023, 435 articles have been published in this phase.
Figure 3.
Number of publications.
3.2. Analysis of countries, institutions, authors and journals
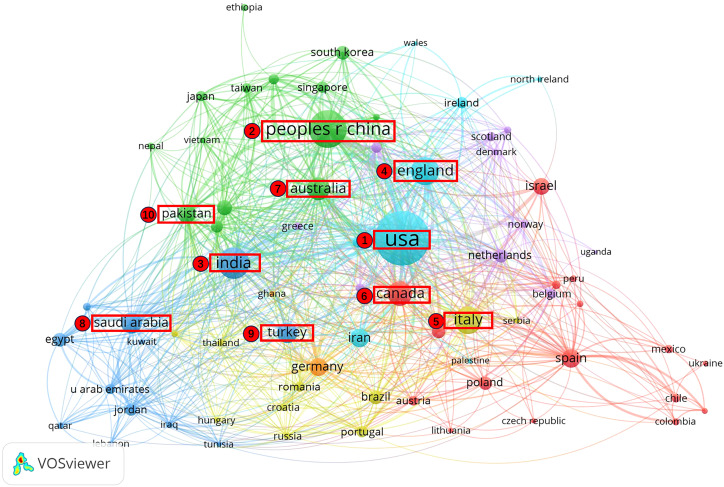
1. Highly productive countries and partnerships
The study compiled the top ten nations that published the greatest quantity of articles ( Table 1 ). Among 115 countries and regions, the USA is the country with the largest number of articles, and it has far more articles than other countries and regions, surpassing China by 374 articles. This indicates that the USA leads in the area of stress during COVID-19. Among the ten high-producing countries and regions, two are located in North America, two in Europe, five in Asia, one in Oceania, with South America and Africa missing on the list. This reveals the low research power in South America and Africa. To further understand the collaborative relationships between countries, this study mapped collaborative relationships (Publication ≥ 5) for 73 countries, as illustrated in Figure 4 . In the figure, the size of the nodes signifies the quantity of publications, the thickness of the lines signifies the closeness of the cooperation, and different colors signify different sub-network collaboration. Countries in Asia, North America and Europe collaborate closely, while those in South America and Africa do not collaborate closely.
Table 1.
Most prolific countries/regions ranked by number of publications.
| Rank | Country | Publication | Citation | Average Citation/Publication |
|---|---|---|---|---|
| 1 | USA | 711 | 9783 | 13.76 |
| 2 | Peoples R China | 337 | 4708 | 13.97 |
| 3 | India | 230 | 4245 | 18.46 |
| 4 | England | 190 | 2954 | 15.55 |
| 5 | Italy | 179 | 4047 | 22.61 |
| 6 | Canada | 148 | 3787 | 25.59 |
| 7 | Australia | 127 | 2511 | 19.77 |
| 8 | Saudi Arabia | 107 | 1263 | 11.8 |
| 9 | Turkey | 98 | 1961 | 20.01 |
| 10 | Pakistan | 85 | 648 | 7.62 |
Figure 4.
Map of co-countries network.
2. Highly productive institutions and collaborative relationships
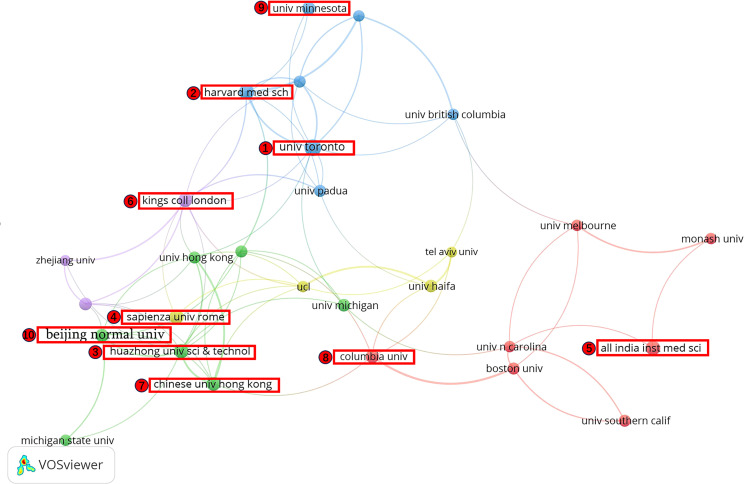
In order to analyze the collaborative relationships between institutions in the area of stress during COVID-19, this study mapped institutional collaborations (Publication ≥ 15) and compiled the top ten institutions in terms of publications, as shown in Table 2 and Figure 5 . The institutions with publications were the University of Toronto (30 articles) in Canada and Harvard Medical School (25 articles) in the United States. Among them, University of Toronto has shown the highest average citation rate (68.8), which reflects the high quality of its research. Based on the ranking table and the corresponding cooperation chart of institutions, it is obvious that universities were the mainstay of studies on stress during COVID-19. Among which, most are from USA and China. Universities in these countries are more energetic in this field of research, and at the same time there are stronger links between universities in different countries.
Table 2.
Most prolific institutions ranked by number of publications.
| Rank | Institution | Publication | Citation | Average Citation/Publication |
|---|---|---|---|---|
| 1 | University of Toronto, Canada | 30 | 2064 | 68.8 |
| 2 | Harvard Medical School, USA | 25 | 512 | 20.48 |
| 3 | Huazhong University Science & Technology, Peoples R China | 23 | 485 | 21.09 |
| 4 | Sapienza University of Rome, Italy | 23 | 155 | 6.74 |
| 5 | All India Institute of Medical Sciences, India | 23 | 428 | 18.61 |
| 6 | Kings College London, England | 22 | 574 | 26.09 |
| 7 | Chinese University Hong Kong, Peoples R China | 22 | 195 | 8.86 |
| 8 | Columbia University, USA | 20 | 174 | 8.7 |
| 9 | University of Minnesota, USA | 20 | 190 | 9.5 |
| 10 | Beijing Normal University, Peoples R China | 20 | 118 | 5.9 |
Figure 5.
Map of co-institutions network.
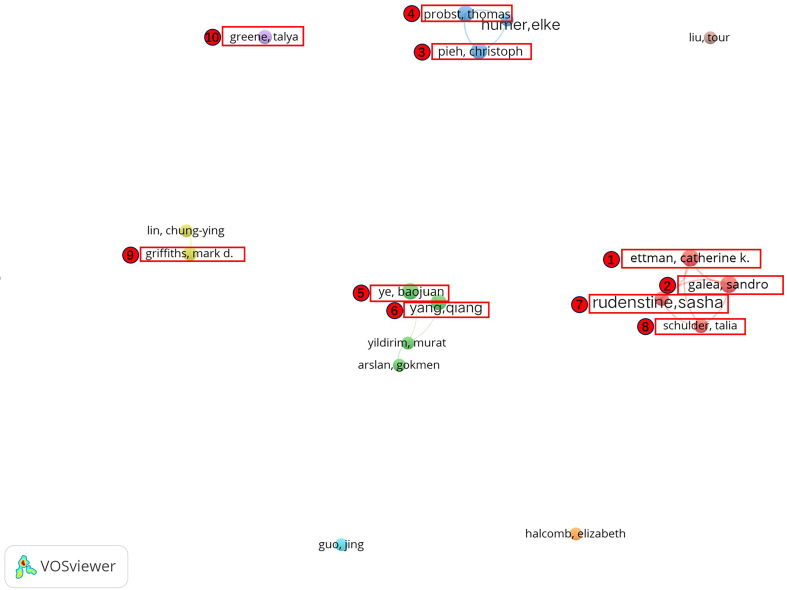
3. Highly productive authors and collaborations
This study compiled the number of articles, citation frequency, as well as corresponding mean of citations of the top ten high-producing authors in research related to stress during COVID-19 ( Table 3 ). Among these, Ettman, Catherine K. and Galea, Sandro published most, both with nine articles. In addition, although Greene, Talya published less, his average citation percentage is higher than that of the other authors, suggesting that his studies are at a high level. Among the top ten highly productive authors, Ettman, Catherine K., Galea, Sandro, Schulder, Talia, and Rudenstine, Sasha collaborated closely and formed a collaborative subnetwork. Moreover, there was a close collaboration between Ye, BaoJuan, and Yang, Qiang; Probst, Thomas, Pieh, Christoph and some other authors formed a collaborative subnetwork. Griffiths, Mark D. and some other authors formed a collaborative subnetwork, while Greene, Talya is relatively independent ( Figure 6 ).
Table 3.
Most prolific authors ranked by number of publications.
| Rank | Author | Country | Publication | Citation | Average Citation/Publication |
|---|---|---|---|---|---|
| 1 | Ettman, Catherine K. | USA | 9 | 191 | 21.22 |
| 2 | Galea, Sandro | USA | 9 | 191 | 21.22 |
| 3 | Pieh, Christoph | Austria | 8 | 216 | 27 |
| 4 | Probst, Thomas | Germany | 8 | 216 | 27 |
| 5 | Ye, BaoJuan | Peoples R China | 8 | 53 | 6.63 |
| 6 | Yang, Qiang | Peoples R China | 7 | 42 | 6 |
| 7 | Rudenstine, Sasha | USA | 6 | 32 | 5.33 |
| 8 | Schulder, Talia | USA | 6 | 32 | 5.33 |
| 9 | Griffiths, Mark D. | UK | 6 | 83 | 13.83 |
| 10 | Greene,Talya | Israel | 6 | 193 | 32.17 |
Figure 6.
Map of co-authors network.
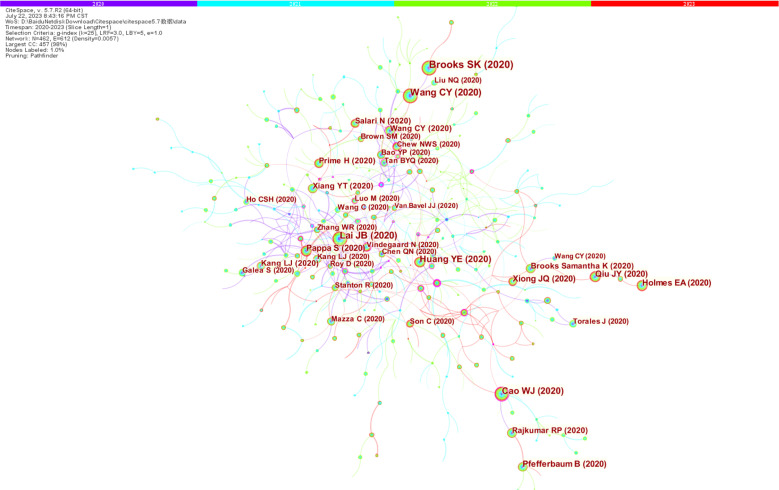
4. Analysis of influential journals and cited literature
This study obtained the co-occurrence map of cited literature using Cite Space software ( Figure 7 ) and all the records screened were analyzed using VOS viewer software. Four journals are listed in the top ten for both publications and citations, including International Journal of Environmental Research and Public Health, Frontiers in psychology, Frontiers in psychiatry and Journal of affective disorders. It indicates that these journals paid more attention to studies in the area of stress, and they represent the spotlights of research in the field of study ( Table 4 ).
Figure 7.
Map of co-cited references.
Table 4.
Top 10 influential journals ranked by number of publications.
| Rank | Journal | Publication | Citation | Average citation/publication |
|---|---|---|---|---|
| 1 | International Journal of Environmental Research and Public Health | 165 | 2895 | 17.55 |
| 2 | Frontiers in Psychology | 111 | 1760 | 15.86 |
| 3 | Frontiers in Psychiatry | 87 | 959 | 11.02 |
| 4 | Frontiers in Public Health | 63 | 353 | 5.6 |
| 5 | Healthcare | 35 | 157 | 4.49 |
| 6 | Journal of Affective Disorders | 32 | 1447 | 45.22 |
| 7 | Current Psychology | 30 | 252 | 8.4 |
| 8 | Sustainability | 25 | 404 | 16.16 |
| 9 | BMJ Open | 23 | 416 | 18.09 |
| 10 | Journal of American College Health | 17 | 159 | 9.35 |
From Table 5 , Wang, cy, Cohen, s, Brooks, sk, Kroenke, k, Lai, jb, Spitzer, rl, and Cao, wj were the most highly cited scholars in the field of stress during the COVID-19 period, and their results were among the top ten most cited literature (Wang cy, 2020; Cohen s, 1983; Brooks sk, 2020; Kroenke k, 2001; Lai jb, 2020; Spitzer rl, 2006; Cao wj, 2020). This reveals that they made a significant contribution to research on stress during COVID-19.
Table 5.
Top 10 most cited authors and references in “Stress during COVID-19”.
| Rank | Cited author | Citation | Rank | Cited reference | Citation |
|---|---|---|---|---|---|
| 1 | World Health, Organization | 498 | 1 | Brooks sk (2020) | 306 |
| 2 | Wang, cy | 470 | 2 | Lai jb (2020) | 252 |
| 3 | Cohen, s | 414 | 3 | Cohen s (1983) | 223 |
| 4 | Brooks, sk | 350 | 4 | Wang cy (2020) | 217 |
| 5 | Who | 292 | 5 | Spitzer rl (2006) | 184 |
| 6 | Kroenke, k | 264 | 6 | Cao wj (2020) | 177 |
| 7 | Lai, jb | 252 | 7 | Huang ye (2020) | 147 |
| 8 | Lazarus, rs | 228 | 8 | Kroenke k (2001) | 134 |
| 9 | Spitzer, rl | 209 | 9 | Qiu jy (2020) | 125 |
| 10 | Cao, wj | 177 | 10 | Xiong jq (2020) | 125 |
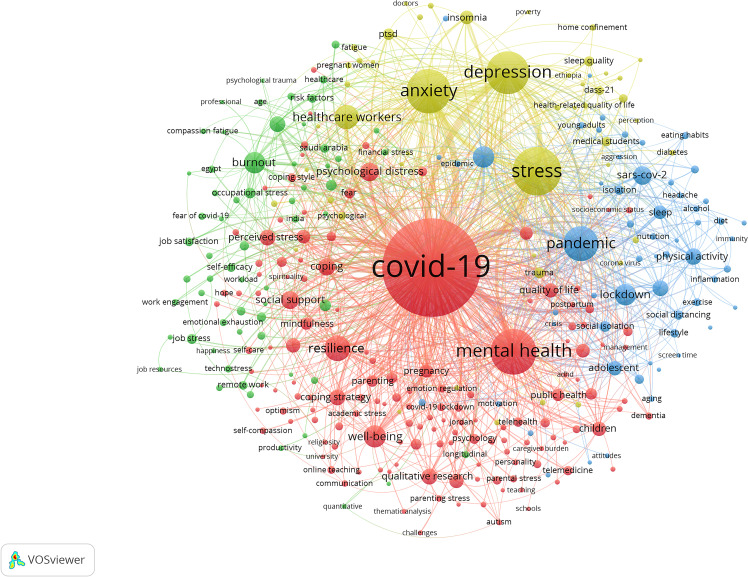
3.3. Thematic analysis
This study used the COOC software to analyze the keywords in the area of stress during COVID-19, and finally gained the top twenty high-frequency author keywords, as listed in Table 6 . These include COVID-19 (2089 times), stress (509 times), mental health (451 times), anxiety (428 times), depression (397 times), pandemic (264 times), resilience (142 times), healthcare workers (136 times), well-being (106 times), lockdown (99 times), burnout (99 times), and coronavirus (98 times) are more popular in the stress studies during COVID-19. In addition, psychological distress (76 times), social support (71 times), coping (64 times), physical activity (58 times), nurses (57 times), coping strategy (56 times), qualitative research (55 times), and quarantine (54 times) have also gained significant attention.
Table 6.
High-frequency keywords.
| Rank | Keyword | Frequency | Rank | Keyword | Frequency |
|---|---|---|---|---|---|
| 1 | COVID-19 | 2089 | 11 | BURNOUT | 99 |
| 2 | STRESS | 509 | 12 | CORONAVIRUS | 98 |
| 3 | MENTAL HEALTH | 451 | 13 | PSYCHOLOGICAL DISTRESS | 76 |
| 4 | ANXIETY | 428 | 14 | SOCIAL SUPPORT | 71 |
| 5 | DEPRESSION | 397 | 15 | COPING | 64 |
| 6 | PANDEMIC | 264 | 16 | PHYSICAL ACTIVITY | 58 |
| 7 | RESILIENCE | 142 | 17 | NURSES | 57 |
| 8 | HEALTHCARE WORKERS | 136 | 18 | COPING STRATEGY | 56 |
| 9 | WELL-BEING | 106 | 19 | QUALITATIVE RESEARCH | 55 |
| 10 | LOCKDOWN | 99 | 20 | QUARANTINE | 54 |
In addition, in order to explore the research theme, this study obtained the keywords using the VOS viewer after constructing the keyword co-occurrence matrix using the COOC software and excluding some meaningless keywords, as shown in Figure 8 . The graph contained 128 items (Frequencies ≥ 10), 1903 links and 4 categories; the degree of the nodes, the strength of the connecting lines, and the number of citations influenced the size of the elements; the colors represented the clusters to which they belong. The topics of greatest interest in the research field were divided into 4 clusters: the influence of stress on the psychological level during COVID-19, the influence of stress on the life level during COVID-19, the influence of stress in the work level during COVID-19, and the influence of stress on the spiritual status during COVID-19.
Figure 8.
Map of keywords clustering.
1. Impact of stress on psychological dimensions during COVID-19 (red)
The major keywords included: COVID-19 (2089 times), mental health (451 times), well-being (106 times), coping strategy (56 times), perceived stress (53 times), children (46 times), students (40 times), loneliness(36 times), psychological stress (26 times), fear (24 times), depressive symptoms (20 times), psychological resilience (15 times), emotional regulation (15 times), emotional distress (12 times), parenting stress (10 times) and so on. This cluster focused on the psychological responses of different population groups, concerned strategies for countering stress during COVID-19, and had an emphasis on people’s mental health.
2. Impact of stress on life dimensions during COVID-19 (green)
The major keywords included: lockdown (99 times), physical activity (58 times), quarantine (54 times), sleep (43 times), social distancing (19 times), lifestyle (18 times), eating habits (11 times), diet (11 times), domestic violence (11 times), and epidemics (10 times). This cluster focuses on the influence of stress generated during COVID-19 on the lifestyle of individuals, as well as the changes during COVID-19 in people’s lifestyles, social interactions and so on.
3. Impact of stress on job level during COVID-19 (blue)
The main keywords included: burnout (99 times), occupational stress (25 times), job stress (23 times), job satisfaction (18 times), self-efficacy (18 times), emotional exhaustion (12 times), turnover intention (11 times), etc. This cluster focuses on the effects of stress during COVID-19 on the working level, and explored ways to alleviate this stress among staff.
4. Impact of stress on mental dimensions during COVID-19 (yellow)
The main keywords included: stress (509 times), anxiety (428 times), depression (397 times), insomnia (41 times), ptsd (31 times), mental well-being (21 times), psychological impact (17 times), post-traumatic stress disorder (14 times). Most words in this cluster are related to the spiritual status of individuals, focusing on the effect of stress during COVID-19, such as anxiety and depression, and exploring measures to mitigate the effects.
3.4. Evolutionary trends
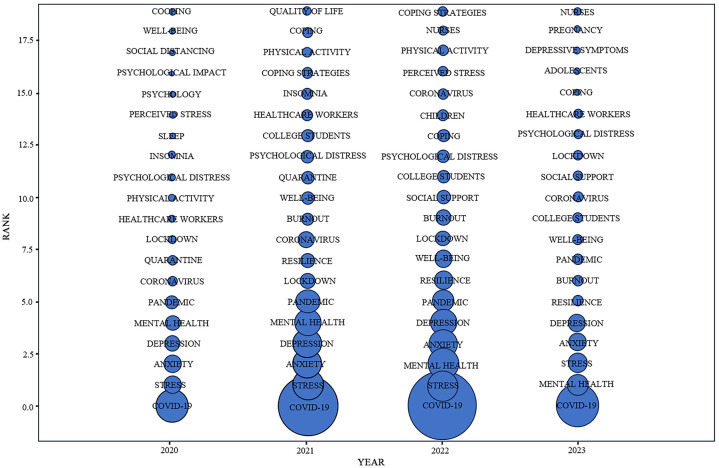
In this study, a time zone map of the authors’ keywords was plotted using COOC software ( Figure 9 ) to explore the trend of stress studies over time during COVID-19. Figure 9 illustrates the top 20 author keywords with the highest frequency of occurrence in stress studies during the COVID-19 period, with the circle size representing the frequency of occurrence of the keyword in the corresponding year. The results showed that the evolutionary trend of stress studies during COVID-19 can be categorized into three phases: developmental, exploratory, and evolutionary.
Figure 9.
Time zone view of keywords.
In 2020, studies of stress during COVID-19 concentrated on the types of stress (“Anxiety” 2020; “Depression” 2020 and “Perceived stress” 2020), psychological impact (“Psychological impact” 2020; “Psychological distress”2020 and “Mental health” 2020), and reactions to stress (“Sleep” 2020; “Insomnia” 2020 and “Physical activity” 2020).
From 2021 to 2022, the frequency of each keyword in studies on stress during COVID-19 increased, and the researchers expanded the population and scope. The range of subjects included children, nurses, and college students (“College students” 2021,2022; “Nurses” 2022; “Children” 2022), as well as studies focusing on different types of stress (“Stress” 2021,2022; “Anxiety” 2021,2022; “Mental health” 2021,2022; “Depression” 2021,2022; “Perceived stress” 2022), and emphasizing the handling of stress (“Coping” 2021,2022; “Coping strategies” 2022; “Resilience” 2021,2022).
In 2023, COVID-19, Mental health, and Stress were the top keywords on the list used, suggesting a steady trend of studies on stress during COVID-19. However, since COVID-19 is essentially over after 2022, studies in this phase are no longer limited to discovering the types of stresses during COVID-19, but focus more on the treatment of stresses after COVID-19 (“Coping” 2023; “Resilience “ 2023; and “Social support” 2023).
In summary, studies on stress during COVID-19 continue to evolve and focus more on dealing with stress during COVID-19.
4. Discussion
4.1. Discussion of results
This paper presents a comprehensive review of stress research during COVID-19 using visualization and scientometric methods. After analyzing 2719 articles on WOS by using COOC, VOS viewer and Cite Space, we ascertained (1): trends in publications (2); high-producing countries, institutions, and authors, as well as collaborations between institutions and authors (3); important journals and cited literature (4); topics of greatest interest; and (5) trends in research area. All discoveries in this study were rooted in the analysis results described above.
First, the year 2022 can be considered as a turning point in the published literature in the area of stress during COVID-19, as measured by the publication volume. Before 2022, the number of publications in this research area grew rapidly. After 2022, the growth in the published literature slows down. This could be due to the fact that the COVID-19 period rendered people susceptible to stress in the face of a pandemic, thereby justifying the increase in the number of studies on stress during this period (56–58). However, the COVID-19 pandemic essentially ended after 2022, and the number of studies on stress during COVID-19 have declined. Despite this decline, research findings in this area will serve as a reference for countries and regions facing similar major public health events.
Second, by counting the most prolific countries, institutions and authors, and analyzing collaborative relationships, the study discovered that the U.S. is the major research power in the field of stress during COVID-19. First, regarding the most fruitful countries, the U.S. contributes the most to research in this area, with 26% of the all publications, exceeding China’s 12%, and has close collaborations with the next nine countries in the list in a decreasing order. Second, regarding the most prolific institutions, 3 of the top 10 organizations belong to the U.S., but they are not the most productive institutions. In contrast, University of Toronto is the most prolific institution, though Canada ranks sixth in the top ten most prolific countries in terms of publishing volumes. This suggests that the U.S. has many organizations involved in research related to this field, whereas Canada’s research efforts are more concentrated in a single institution. In addition, all ten institutions have close collaborative relationships. Finally, regarding the most prolific authors, there are four of the top ten most productive authors from the United States. Ettman, Catherine K. and Galea, Sandro are those with the most publications. In addition, all ten prolific authors have formed their own stable research teams and research directions. It is possible that authors communicated less with other author groups outside of their own collaborative subnetwork due to outbreak closure and geographic location constraints during COVID-19.
Third, this study identified important journals and cited literature in this research area by counting highly productive journals, highly cited authors and literature. First, in terms of high-yield journals, International Journal of Environmental Research and Public Health, Frontiers in Psychology, Frontiers in Psychiatry and Journal of affective disorders—four journals listed in the top ten in terms of publications and citations—are the leading journals in this area of stress during COVID-19. Second, for highly cited authors and cited literature, Wang, cy, Cohen, s, Brooks, sk, Kroenke, k, Lai, jb, Spitzer, rl, and Cao, wj were among the top ten in the number of citations and outcomes cited. Among the top ten cited frequency literature, two were studies on stress, including psychological stress and perceived stress (cao wj, 2020, cohen s, 1983); two were studies on psychological effects and psychological distress during COVID-19 (brooks sk, 2020, qiu jy, 2020); four were studies on psychological health and mental resilience during COVID-19 (huang ye, 2020, lai jb, 2020, wang cy, 2020, xiong jq, 2020); two were studies on psychiatric disorders, including anxiety disorders, depression (kroenke k, 2001, spitzer rl, 2006).
Fourth, COVID-19, Stress, Mental health, Anxiety, and Depression featured most as keywords. This indicates that studies on stress during COVID-19 focused more on stress and related conditions, such as anxiety, and depression, while emphasizing on optimizing mental health (9, 59–61). Through cluster analysis, this study summarized four themes of focus for studies on stress during COVID-19. First, the influence of stress on the psychological dimension during COVID-19. Here, the pandemic forced changes in daily life and shrunk social space leading to different forms of stress (psychological, perceived and parenting stresses). This gives the possibility for interventions to alleviate stress, thereby optimizing mental health for different population groups (healthcare workers, manufacturing workers and pregnant women) during the pandemic (62–67). Second, the influence of stress on the life dimension during COVID-19. COVID-19 quarantine imposed restrictions on activities, created a social distance, and incited stress affecting daily habits and lifestyles (68, 69). In addition, these lifestyle changes differed with genders (70–72) and affected the treatment of other diseases (41, 73–76). Third, the influence of stress on the work dimension during COVID-19. The COVID-19 outbreak changed work patterns of all working groups (teachers, healthcare workers and hotel staff) to varying degrees (77, 78), forcing people to shift their workplaces to their homes. This affected job satisfaction negatively and added work stress (79–81). This could be mitigated by improving the working environment and engaging in fitness exercise (82–85). Moreover, COVID-19 impacted the work of healthcare workers, leading to increased work pressure, and burnout. This could be mitigated by developing stress resilience to ensure optimal physical and mental health (25, 86–88). Fourth, the influence of stress on the spiritual dimension during COVID-19. In the face of stress since from the COVID-19 outbreak, people were highly susceptible to anxiety and frustration (89–92). In addition, the higher the perceived threat from stress or from news in the number of people around them infected with COVID-19, the higher the chance of becoming anxious and depressed, with healthcare workers being the most affected (93–96).
Fifth, the evolution of the area of stress research during COVID-19 can be divided into three phases: developmental, exploratory, and evolving. At the developmental stage, scholars focus on the study and concentrate more on the types of stress and responses from those stressed. This is because of the forced change in daily life (97–99). The exploratory phase involves increasing the quantity of published studies and broadening the scope and target audience while focusing on the types of stress in the pandemic (100). Finally, in the evolving phase, there is a decreasing trend in the growth of the volume of publications, an increase in quality, a greater focus on the management of stress and the maintenance of optimal mental health. This might be due to the fact that the COVID-19 epidemic is essentially over after 2022, and more attention is given to methods of stress relief and mental health maintenance.
4.2. Implications
The importance of this research is expressed in three areas. First, in this study, scientific bibliometric tools (COOC, VOS viewer and Cite Space) were utilized to reveal the research structure, hot spots and evolving trends in the research area of stress during COVID-19, in order to deliver accurate and comprehensive information about this field. Second, by analyzing journals, countries, institutions, and authors, this study revealed the current status of research in this field of stress during COVID-19, which can help scholars to rapidly understand the basics of this field and locate target journals or publications. Third, using bibliometric methods, clustering and predicting stress during COVID-19 helps researchers accurately capture the research hot spots in the field and offers ideas for future research.
4.3. Limitations and directions for future research
This study deduced a comprehensive framework of studies on stress during the pandemic, despite some limitations we encountered in the process. First, the study sample was drawn from the WOS core collection, which is highly representative, but it does not cover all papers in this research field of stress during the COVID-19 period. We recommend that future endeavors should track literature in 2023 and broaden data sources, such as EBSCO and PubMed. In addition, while bibliometric analyses using specialized software are objective, interpretation of results are subjective. However, we overcame this through several conversations among multiple authors. We will continue to track, create and adopt more interpretive and stipulative models in the future.
5. Conclusion
First, this research found that the heat of stress research during COVID-19 has declined, and the main research forces come from the United States and China. In addition, Countries in Asia, North America and Europe collaborate closely. Institutions have close cooperation with each other and authors have formed their own collaborative networks. Second, in terms of research hot spots, the research area of stress during the COVID-19 period has paid particular attention to the influence of stress on the psychological, spiritual, job and life levels, and gradually focuses on stress management strategies. In total, this study of stress during COVID-19 informs future exploration of stress in the setting of similar public health events and provides insight into the direction of subsequent research.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
LL: Conceptualization, Validation, Visualization, Writing – original draft. GL: Conceptualization, Validation, Visualization, Writing – original draft. YX: Methodology, Writing – original draft, Writing – review & editing. JJ: Formal Analysis, Visualization, Writing – original draft. ZW: Formal Analysis, Visualization, Writing – original draft.
Acknowledgments
We are grateful to the language editors who assisted us in proofreading and editing this paper.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Science and Technology of the Department of Education of Jiangxi Province Fund “A study on the horizontal differentiation of residents’ pro-environmental behaviors based on spatio-temporal trajectory data mining” [Grant numbers GJJ220034].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Majeed M, Irshad M, Fatima T, Khan J, Hassan MM. Relationship between problematic social media usage and employee depression: A moderated mediation model of mindfulness and fear of COVID-19. Front Psychol (2020) 11:557987. doi: 10.3389/fpsyg.2020.557987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Khoury JMB, Watt MC, MacLean K. Anxiety sensitivity mediates relations between mental distress symptoms and medical care utilization during COVID-19 pandemic. Int J Cognit Ther (2021) 14:515–36. doi: 10.1007/s41811-021-00113-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nicomedes CJC, Avila RMA. An analysis on the panic during COVID-19 pandemic through an online form. J Affect Disord (2020) 276:14–22. doi: 10.1016/j.jad.2020.06.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Phalswal U, Pujari V, Sethi R, Verma R. Impact of social media on mental health of the general population during Covid-19 pandemic: A systematic review. J Educ Health Promot (2023) 12:23. doi: 10.4103/jehp.jehp_460_22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bigalke JA, Greenlund IM, Carter JR. Sex differences in self-report anxiety and sleep quality during COVID-19 stay-at-home orders. Biol Sex Differ (2020) 11:56. doi: 10.1186/s13293-020-00333-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hawes MT, Szenczy AK, Klein DN, Hajcak G, Nelson BD. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med (2022) 52:3222–30. doi: 10.1017/S0033291720005358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rehman U, Yildirim M, Shahnawaz MG. A longitudinal study of depression, anxiety, and stress among Indians during COVID-19 pandemic. Psychol Health Med (2023) 28:60–8. doi: 10.1080/13548506.2021.2023751 [DOI] [PubMed] [Google Scholar]
- 8. Kim SY, Yoo DM, Kwon M-J, Kim J-H, Kim J-H, Bang W-J, et al. Changes in the Mean of and Variance in Psychological Disease Incidences before and during the COVID-19 Pandemic in the Korean Adult Population. J Pers Med (2022) 12:576. doi: 10.3390/jpm12040576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lakhan R, Agrawal A, Sharma M. Prevalence of depression, anxiety, and stress during COVID-19 pandemic. JNRP (2020) 11:519–25. doi: 10.1055/s-0040-1716442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sidor A, Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients (2020) 12:1657. doi: 10.3390/nu12061657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang Y, Lu H, Hu M, Wu S, Chen J, Wang L, et al. Alcohol consumption in China before and during COVID-19: preliminary results from an online retrospective survey. Front Psychiatry (2020) 11:597826. doi: 10.3389/fpsyt.2020.597826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wardell JD, Kempe T, Rapinda KK, Single A, Bilevicius E, Frohlich JR, et al. Drinking to cope during COVID-19 pandemic: the role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcohol Clin Exp Res (2020) 44:2073–83. doi: 10.1111/acer.14425 [DOI] [PubMed] [Google Scholar]
- 13. Ingram J, Maciejewski G, Hand CJ. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front Psychol (2020) 11:588604. doi: 10.3389/fpsyg.2020.588604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Isha ASN, Naji GMA, Saleem MS, Brough P, Alazzani A, Ghaleb EAA, et al. Validation of “Depression, Anxiety, and Stress Scales” and “Changes in Psychological Distress during COVID-19” among University Students in Malaysia. Sustainability (2023) 15:4492. doi: 10.3390/su15054492 [DOI] [Google Scholar]
- 15. Zhang Y, Tao S, Qu Y, Mou X, Gan H, Zhou P, et al. The correlation between lifestyle health behaviors, coping style, and mental health during the COVID-19 pandemic among college students: Two rounds of a web-based study. Front Public Health (2023) 10:1031560. doi: 10.3389/fpubh.2022.1031560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nishida Y, Hosomi S, Fujimoto K, Nakata R, Itani S, Ohminami M, et al. Effect of the coronavirus disease 2019 lockdown on lifestyle factors in Japanese patients with inflammatory bowel disease. Intern Med (2022) 61:1329–36. doi: 10.2169/internalmedicine.8825-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hu Y, Ye B, Luo X-B, Ma T, Feng Z, Yang Q. The Effect of Stress of COVID-19 on Chinese Adults’ Work-Family Conflict: Testing a Moderated Mediation Model. PRBM (2023) 16:373–382. doi: 10.2147/PRBM.S381056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Andrulli R, Gerards R. How new ways of working during COVID-19 affect employee well-being via technostress, need for recovery, and work engagement. Comput Hum Behav (2023) 139:107560. doi: 10.1016/j.chb.2022.107560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Molino M, Ingusci E, Signore F, Manuti A, Giancaspro ML, Russo V, et al. Wellbeing costs of technology use during covid-19 remote working: an investigation using the italian translation of the technostress creators scale. Sustainability (2020) 12:5911. doi: 10.3390/su12155911 [DOI] [Google Scholar]
- 20. Siddiqui S, Arif I, Hinduja P. Technostress: A catalyst to leave the teaching profession-A survey designed to measure technostress among teachers in Pakistan during COVID-19 pandemic. E-Learn Digit Media (2023) 20:53–79. doi: 10.1177/20427530221107506 [DOI] [Google Scholar]
- 21. Bahamondes-Rosado ME, Cerda-Suarez LM, de Zevallos GFDO, Espinosa-Cristia JF. Technostress at work during the COVID-19 lockdown phase (2020-2021): a systematic review of the literature. Front Psychol (2023) 14:1173425. doi: 10.3389/fpsyg.2023.1173425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Said RM, El-Shafei DA. Occupational stress, job satisfaction, and intent to leave: nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt. Environ Sci Pollut Res (2021) 28:8791–8801. doi: 10.1007/s11356-020-11235-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Elbay RY, Kurtulmus A, Arpacioglu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res (2020) 290:113130. doi: 10.1016/j.psychres.2020.113130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hokett E, Arunmozhi A, Campbell J, Duarte A. Factors that protect against poor sleep quality in an adult lifespan sample of non-Hispanic Black and non-Hispanic White adults during COVID-19: A cross-sectional study. Front Psychol (2022) 13:949364. doi: 10.3389/fpsyg.2022.949364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Buchbinder M, Browne A, Jenkins T, Berlinger N, Buchbinder L. Hospital physicians’ Perspectives on occupational stress during COVID-19: a qualitative analysis from two US cities. J Gen Intern Med (2023) 38:176–84. doi: 10.1007/s11606-022-07848-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sagherian K, Steege LM, Cobb SJ, Cho H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: A cross-sectional survey of hospital nursing staff in the United States. J Clin Nurs (2023) 32:5382–95. doi: 10.1111/jocn.15566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Khatri S, Murthy AK, Hashim U, Kuruthukulangara S, Kumari A, Lele PR. Psychological status of pregnant women during COVID-19 pandemic: A cross-sectional study from Mumbai. J Mar Med Soc (2020) 22:113–7. doi: 10.4103/jmms.jmms_120_20 [DOI] [Google Scholar]
- 28. Hajduk M, Dancik D, Januska J, Strakova A, Turcek M, Heretik A, et al. Depression and anxiety among College Students in Slovakia - Comparison of the Year 2018 and during COVID-19 pandemic. Bratisl Med J (2022) 123:44–9. doi: 10.4149/BLL_2022_007 [DOI] [PubMed] [Google Scholar]
- 29. Cameron EE, Joyce KM, Delaquis CP, Reynolds K, Protudjer JLP, Roos LE. Maternal psychological distress & mental health service use during the COVID-19 pandemic. J Affect Disord (2020) 276:765–74. doi: 10.1016/j.jad.2020.07.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mallhi TH, Ahmad N, Salman M, Tanveer N, Shah S, Butt MH, et al. Estimation of Psychological Impairment and Coping Strategies during COVID-19 Pandemic among University Students in Saudi Arabia: A Large Regional Analysis. Int J Environ Res Public Health (2022) 19:14282. doi: 10.3390/ijerph192114282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Perveen A, Hamzah HB, Othamn A, Ramlee F. Prevalence of Anxiety, Stress, Depression among Malaysian Adults during COVID-19 Pandemic Movement Control Order. Indian J Community Health (2020) 32:579–85. doi: 10.47203/IJCH.2020.v32i03.020 [DOI] [Google Scholar]
- 32. Peng P, Hao Y, Liu Y, Chen S, Wang Y, Yang Q, et al. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord (2023) 321:167–81. doi: 10.1016/j.jad.2022.10.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yuan L, Lu L, Wang X, Qu M, Gao Y, Pan B. Comorbid anxiety and depressive symptoms and the related factors among international medical students in China during COVID-19 pandemic: a cross-sectional study. BMC Psychiatry (2023) 23:165. doi: 10.1186/s12888-023-04638-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mishra J, Panigrahi A, Samanta P, Dash K, Mahapatra P, Behera MR. Sleep quality and associated factors among undergraduate medical students during Covid-19 confinement. Clin Epidemiol Glob Health (2022) 15:101004. doi: 10.1016/j.cegh.2022.101004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Saraswathi I, Saikarthik J, Kumar KS, Srinivasan KM, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ (2020) 8:e10164. doi: 10.7717/peerj.10164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Yang H, Zhao Q, Zhang Z, Jia W. Associations between lifestyle changes, risk perception and anxiety during COVID-19 lockdowns: A case study in xi’an. Int J Environ Res Public Health (2022) 19:13379. doi: 10.3390/ijerph192013379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Vilovic T, Bozic J, Zuzic Furlan S, Vilovic M, Kumric M, Martinovic D, et al. Mental Health Well-Being and Attitudes on Mental Health Disorders among Family Physicians during COVID-19 Pandemic: A Connection with Resilience and Healthy Lifestyle. J Clin Med (2022) 11:438. doi: 10.3390/jcm11020438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Huang C, Feng Q, Zhang B, Ren H, Liu Z, Kang Y, et al. Income and social support related with mental health during COVID-19 outbreak in China. Med (Baltimore) (2022) 101:e29022. doi: 10.1097/MD.0000000000029022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Aslan GK, Kilinc E, Kartal A. The effect of COVID-19 pandemic on lifestyle-related behaviours in Turkey: A web-based cross-sectional study. Int J Nurs Pract (2022) 28:e13053. doi: 10.1111/ijn.13053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Knell G, Robertson MC, Dooley EE, Burford K, Mendez KS. Health behavior changes during COVID-19 pandemic and subsequent “Stay-at-home” Orders. Int J Environ Res Public Health (2020) 17:6268. doi: 10.3390/ijerph17176268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mattioli AV, Sciomer S, Cocchi C, Maffei S, Gallina S. Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutrition Metab Cardiovasc Dis (2020) 30:1409–17. doi: 10.1016/j.numecd.2020.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Finnerty R, McWeeny S, Trainor L. Online group music therapy: proactive management of undergraduate students’ stress and anxiety. Front Psychiatry (2023) 14:1183311. doi: 10.3389/fpsyt.2023.1183311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Global Health (2020) 16:89. doi: 10.1186/s12992-020-00621-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Tabur A, Choudhury A, Emhan A, Mengenci C, Asan O. Clinicians’ Social support, job stress, and intent to leave healthcare during COVID-19. Healthcare (2022) 10:229. doi: 10.3390/healthcare10020229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ghahramani S, Lankarani KB, Yousefi M, Heydari K, Shahabi S, Azmand S. A systematic review and meta-analysis of burnout among healthcare workers during COVID-19. Front Psychiatry (2021) 12:758849. doi: 10.3389/fpsyt.2021.758849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Gao S, Su S, Zhang E, Liu R, Zhang Y, Wang C, et al. Psychological health status in postpartum women during COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord (2022) 319:99–111. doi: 10.1016/j.jad.2022.08.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Yunitri N, Chu H, Kang XL, Jen H-J, Pien L-C, Tsai H-T, et al. Global prevalence and associated risk factors of posttraumatic stress disorder during COVID-19 pandemic: A meta-analysis. Int J Nurs Stud (2022) 126:104136. doi: 10.1016/j.ijnurstu.2021.104136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Safi-Keykaleh M, Aliakbari F, Safarpour H, Safari M, Tahernejad A, Sheikhbardsiri H, et al. Prevalence of postpartum depression in women amid the COVID-19 pandemic: A systematic review and meta-analysis. Int J Gynecol Obstet (2022) 157:240–7. doi: 10.1002/ijgo.14129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chutiyami M, Cheong AMY, Salihu D, Bello UM, Ndwiga D, Maharaj R, et al. COVID-19 pandemic and overall mental health of healthcare professionals globally: A meta-review of systematic reviews. Front Psychiatry (2022) 12:804525. doi: 10.3389/fpsyt.2021.804525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Donthu N, Kumar S, Mukherjee D, Pandey N, Lim WM. How to conduct a bibliometric analysis: An overview and guidelines. J Bus Res (2021) 133:285–96. doi: 10.1016/j.jbusres.2021.04.070 [DOI] [Google Scholar]
- 51. van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics (2010) 84:523–38. doi: 10.1007/s11192-009-0146-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Chen Y, Chen C-m, Liu Z-y, Hu Z-g, Wang X-w. The methodology function of Cite Space mapping knowledge domains. Stud Sci Sci (2015) 33:242–53. doi: 10.16192/j.cnki.1003-2053.2015.02.009 [DOI] [Google Scholar]
- 53. Petticrew M. Systematic reviews from astronomy to zoology: myths and misconceptions. BMJ (2001) 322:98–101. doi: 10.1136/bmj.322.7278.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lee K, Jeong G-C, Yim J. Consideration of the psychological and mental health of the elderly during COVID-19: A theoretical review. Int J Environ Res Public Health (2020) 17:8098. doi: 10.3390/ijerph17218098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sharma SK, Joseph J, Varkey BP, Dhandapani M, Varghese A, Sharma S, et al. Prevalence of anxiety and depressive symptoms during COVID-19 pandemic among the general population in India: A systematic review and meta-analysis. J Neurosci Rural Pract (2022) 13:608–17. doi: 10.25259/JNRP-2022-1-21-R3-(2324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Alkhamees AA, Aljohani MS, Alghesen MA, Alhabib AT. Psychological distress in quarantine designated facility during COVID-19 pandemic in Saudi Arabia. Risk Manag Healthc Policy (2020) 13:3103–20. doi: 10.2147/RMHP.S284102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Thakur B, Pathak M. Burden of predominant psychological reactions among the healthcare workers and general population during COVID-19 pandemic phase: A systematic review and meta-analysis. Indian J Commun Med (2021) 46:600–5. doi: 10.4103/ijcm.IJCM_1007_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Verma S, Mishra A. Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19. Int J Soc Psychiatr (2020) 66:756–62. doi: 10.1177/0020764020934508 [DOI] [PubMed] [Google Scholar]
- 59. Fernandez RS, Crivelli L, Guimet NM, Allegri RF, Pedreira ME. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. J Affect Disord (2020) 277:75–84. doi: 10.1016/j.jad.2020.07.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bower M, Smout S, Donohoe-Bales A, O’Dean S, Teesson L, Boyle J, et al. A hidden pandemic? An umbrella review of global evidence on mental health in the time of COVID-19. Front Psychiatry (2023) 14:1107560. doi: 10.3389/fpsyt.2023.1107560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Pieh C, Budimir S, Delgadillo J, Barkham M, Fontaine JRJ, Probst T. Mental health during COVID-19 lockdown in the United Kingdom. Psychosom Med (2021) 83:328–37. doi: 10.1097/PSY.0000000000000871 [DOI] [PubMed] [Google Scholar]
- 62. Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Srivastava M, Ghosh A. Online gratitude interventions during COVID- 19 pandemic on youth: randomized trial. J Evidence-Based Soc Work (2023) 20:272–98. doi: 10.1080/26408066.2022.2157691 [DOI] [Google Scholar]
- 64. Vajpeyee M, Tiwari S, Jain K, Modi P, Bhandari P, Monga G, et al. Yoga and music intervention to reduce depression, anxiety, and stress during COVID-19 outbreak on healthcare workers. Int J Soc Psychiatry (2022) 68:798–807. doi: 10.1177/00207640211006742 [DOI] [PubMed] [Google Scholar]
- 65. Hassanie S, Olugbade OA, Karadas G, Altun Ö. The impact of workload on workers’ Traumatic stress and mental health mediated by career adaptability during COVID-19. Sustainability (2022) 14:12010. doi: 10.3390/su141912010 [DOI] [Google Scholar]
- 66. Khan R, Roy MK, Chowdhury SH. The impact of work-family balance on manufacturing employees? mental health during pandemic br. Organ Psikol (2022) 12:29–40. doi: 10.17323/2312-5942-2022-12-4-29-40 [DOI] [Google Scholar]
- 67. Mikolajkow A, Małyszczak K. Stress level and general mental state in Polish pregnant women during COVID-19 pandemic. J Reprod Infant Psychol (2023) 41:165–82. doi: 10.1080/02646838.2021.1976402 [DOI] [PubMed] [Google Scholar]
- 68. Charkazi A, Salmani F, Moodi M, Norozi E, Zarei F, Lotfizadeh M, et al. Effects of the COVID-19 pandemic on lifestyle among Iranian population: A multicenter cross-sectional study. J Res Med Sci (2022) 27:22. doi: 10.4103/jrms.jrms_506_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. ALkharashi NA. Comparison of general dietary and lifestyle habits before and during COVID-19 among the saudi adult population in riyadh. Curr Nutr Food Sci (2022) 18:419–26. doi: 10.2174/1573401318666211224123653 [DOI] [Google Scholar]
- 70. Wang C, Havewala M, Fan Q, Wang Q, Bali D. The relations between COVID-19 stress, social connectedness, and mental health: a longitudinal investigation comparing Chinese and American college students. Curr Psychol (2023) 25:1–14. doi: 10.1007/s12144-023-04290-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bonfrate L, Di Ciaula A, Khalil M, Farella I, Chirico R, Vilahur G, et al. Gender-dependent impact of COVID-19 lockdown on metabolic and psychological aspects. Intern Emerg Med (2023) 18:385–395. doi: 10.1007/s11739-022-03173-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Shikuma J, Nagai Y, Sakurai M, Udagawa K, Ito R, Miwa T, et al. Impact of gender differences on lifestyle and glycemic control in Japanese patients with diabetes during COVID-19 lockdowns. Primary Care Diabetes (2022) 16:350–4. doi: 10.1016/j.pcd.2022.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun (2020) 87:100–6. doi: 10.1016/j.bbi.2020.04.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Rocha T de O, de Oliveira W, de Paula AR, Oliveira DL, Rode S de M. Psychological factors in temporomandibular disorders patients during COVID-19 pandemic: A cross-sectional study. Pesqui Bras Odontopediatria Clin Integr (2022) 22:e200246. doi: 10.1590/pboci.2022.020 [DOI] [Google Scholar]
- 75. Tashakori-Miyanroudi M, Souresrafil A, Hashemi P, Ehsanzadeh SJ, Farrahizadeh M, Behroozi Z. Prevalence of depression, anxiety, and psychological distress in patients with epilepsy during COVID-19: A systematic review. Epilepsy Behav (2021) 125:108410. doi: 10.1016/j.yebeh.2021.108410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Ghosh A, Arora B, Gupta R, Anoop S, Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab Syndr-Clin Res Rev (2020) 14:917–20. doi: 10.1016/j.dsx.2020.05.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lipert A, Musiał K, Rasmus P. Working mode and physical activity as factors determining stress and sleep quality during COVID-19 pandemic lockdown in Poland. Life (2021) 12:28. doi: 10.3390/life12010028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Abdou AH, Khalil AAF, Mahmoud HME, Elsaied MA, Elsaed AA. The impact of hospitality work environment on employees’ Turnover intentions during COVID-19 pandemic: the mediating role of work-family conflict. Front Psychol (2022) 13:890418. doi: 10.3389/fpsyg.2022.890418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kasemy ZA, Sharif AF, Barakat AM, Abdelmohsen SR, Hassan NH, Hegazy NN, et al. Technostress creators and outcomes among Egyptian medical staff and students: A multicenter cross-sectional study of remote working environment during COVID-19 pandemic. Front Public Health (2022) 10:796321. doi: 10.3389/fpubh.2022.796321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Kapoor V, Yadav J, Bajpai L, Srivastava S. Perceived stress and psychological well-being of working mothers during COVID-19: a mediated moderated roles of teleworking and resilience. Empl Relat (2021) 43:1290–309. doi: 10.1108/ER-05-2020-0244 [DOI] [Google Scholar]
- 81. Serrao C, Rodrigues AR, Teixeira A, Castro L, Duarte I. The impact of teleworking in psychologists during COVID-19: Burnout, depression, anxiety, and stress. Front Public Health (2022) 10:984691. doi: 10.3389/fpubh.2022.984691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Tao B, Lu T, Chen H, Yan J. The relationship between psychological stress and emotional state in chinese university students during COVID-19: the moderating role of physical exercise. Healthcare (2023) 11:695. doi: 10.3390/healthcare11050695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Jung G, Oh J. Factors Affecting Health-Related Quality of Life among Healthcare Workers during COVID-19: A Cross-Sectional Study. Med Lith (2023) 59:38. doi: 10.3390/medicina59010038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Wadhen V, Cartwright T. Feasibility and outcome of an online streamed yoga intervention on stress and wellbeing of people working from home during COVID-19. WOR (2021) 69:331–49. doi: 10.3233/WOR-205325 [DOI] [PubMed] [Google Scholar]
- 85. Tleuken A, Turkyilmaz A, Sovetbek M, Durdyev S, Guney M, Tokazhanov G, et al. Effects of the residential built environment on remote work productivity and satisfaction during COVID-19 lockdowns: An analysis of workers’ perceptions. Building Environ (2022) 219:109234. doi: 10.1016/j.buildenv.2022.109234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Calegari JG, Russo S, Luciani M, Strepparava MG, Di Mauro S, Ausili D. Association between coping strategies and professional quality of life in nurses and physicians during COVID-19: A cross-sectional study. J Nurs Manag (2022) 30:4054–63. doi: 10.1111/jonm.13845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Pountney J, Butcher I, Donnelly P, Morrison R, Shaw RL. How the COVID-19 crisis affected the well-being of nurses working in paediatric critical care: A qualitative study. Br J Health Psychol (2023) 28:914–929. doi: 10.1111/bjhp.12661 [DOI] [PubMed] [Google Scholar]
- 88. Dabou EAR, Ilesanmi RE, Mathias CA, Hanson VF. Work-related stress management behaviors of nurses during COVID-19 pandemic in the United Arab Emirates. SAGE Open Nurs (2022) 8:237796082210849. doi: 10.1177/23779608221084972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Al-Qahtani AM, Elgzar WT, Ibrahim HA-F. Covid-19 pandemic: psycho-social consequences during the social distancing period among najran city population. Psychiatr Danub (2020) 32:280–6. doi: 10.24869/psyd.2020.280 [DOI] [PubMed] [Google Scholar]
- 90. Oliveira ACDS, Gallego MG, Martinez CG, Martinez EC, Molina JM, Morante JJH, et al. Psychosocial changes during COVID-19 lockdown on nursing home residents, their relatives and clinical staff: a prospective observational study. BMC Geriatr (2023) 23:71. doi: 10.1186/s12877-023-03764-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Khademian F, Delavari S, Koohjani Z, Khademian Z. An investigation of depression, anxiety, and stress and its relating factors during COVID-19 pandemic in Iran. BMC Public Health (2021) 21:275. doi: 10.1186/s12889-021-10329-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Kishimoto T, Kinoshita S, Bun S, Sato Y, Kitazawa M, Kikuchi T, et al. Japanese Project for Telepsychiatry Evaluation during COVID-19: Treatment Comparison Trial (J-PROTECT): Rationale, design, and methodology. Contemp Clin Trials (2021) 111:106596. doi: 10.1016/j.cct.2021.106596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Lee BEC, Ling M, Boyd L, Olsson C, Sheen J. The prevalence of probable mental health disorders among hospital healthcare workers during COVID-19: A systematic review and meta-analysis. J Affect Disord (2023) 330:329–45. doi: 10.1016/j.jad.2023.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Joseph R, Lucca JM, Alshayban D, Alshehry YA. The immediate psychological response of the general population in Saudi Arabia during COVID-19 pandemic: A cross-sectional study. J Infection Public Health (2021) 14:276–83. doi: 10.1016/j.jiph.2020.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Ali EA, Sehlo MG, Hussein RA, Ali ET, Abdalla AM. Prevalence and correlates of depressive symptoms among nurses during COVID-19 pandemic. Egypt J Neurol Psychiatr Neurosurg (2023) 59:15. doi: 10.1186/s41983-023-00616-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Chura S, Saintila J, Mamani R, Mamani PGR, Morales-Garcia WC. Predictors of depression in nurses during COVID-19 health emergency; the mediating role of resilience: A cross-sectional study. J Prim Care Community Health (2022) 13:1–8. doi: 10.1177/21501319221097075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog Neuro-Psychopharmacol Biol Psychiatry (2021) 109:110236. doi: 10.1016/j.pnpbp.2020.110236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Daniali H, Martinussen M, Flaten MA. A global meta-analysis of depression, anxiety, and stress before and during COVID-19. Health Psychol (2023) 42:124–38. doi: 10.1037/hea0001259 [DOI] [PubMed] [Google Scholar]
- 99. Rogowska AM, Kusnierz C, Bokszczanin A. Examining anxiety, life satisfaction, general health, stress and coping styles during COVID-19 pandemic in polish sample of university students. Psychol Res Behav Manag (2020) 13:797–811. doi: 10.2147/PRBM.S266511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Wang D, Zhao J, Zhai S, Ye H, Bu L, Fan F. Does sleep disturbance predicts posttraumatic stress disorder and depression among college students during COVID-19 lockdown? A longitudinal survey. Front Public Health (2022) 10:986934. doi: 10.3389/fpubh.2022.986934 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.