Abstract
Introduction
Medication adherence is important for optimal management of chronic conditions, including hypertension and hypercholesterolemia. This study describes adherence to antihypertensive and statin medications, individually and collectively, and examines variation in adherence by demographic and geographic characteristics.
Methods
2017 prescription drug event data for beneficiaries with Medicare Part D coverage were assessed. Beneficiaries with a proportion of days covered ≥80% were considered adherent. Adjusted prevalence ratios were estimated to quantify associations between demographic and geographic characteristics and adherence. Adherence estimates were mapped by county of residence using a spatial empirical Bayesian smoothing technique to enhance stability. Analyses were conducted 2019–2021.
Results
Among the 22.5 million beneficiaries prescribed antihypertensive medications, 77.1% were adherent; among the 16.1 million prescribed statin medications, 81.9% were adherent; and, among the 13.5 million prescribed antihypertensive and statin medications, 70.3% were adherent to both. Adherence varied by race/ethnicity: American Indian/Alaska Native (adjusted prevalence ratio 0.83, 95% confidence limit 0.82–0.842, Hispanic (0.90, 0.90–0.91) and non-Hispanic Black beneficiaries (0.87, 0.86–0.87) were less likely to be adherent compared to non-Hispanic White beneficiaries. County-level adherence ranged across the United States from 25.7% to 88.5% for antihypertensive medications, 36.0% to 93.8% for statin medications, and 20.8% to 92.9% for both medications combined, and tended to be the lowest in the southern United States.
Conclusions
This study highlights opportunities for efforts to remove barriers and support medication adherence, especially among racial/ethnic minority groups and within the regions at greatest risk for adverse cardiovascular outcomes.
Keywords: medication adherence, hypertension, hypercholesterolemia, antihypertensive
Introduction
Hypertension and hypercholesterolemia are leading chronic disease risk factors that contribute substantially to excess morbidity, mortality, and health care spending in the United States.1–3 Poor management of these highly prevalent conditions is associated with increased risk for multiple negative health outcomes—most notably for cardiovascular disease.2, 4–6 Improving blood pressure control and reducing blood low-density lipoprotein (LDL) cholesterol levels have been identified as two of the most important efforts to decrease the burden of death from heart disease and stroke, the 1st and 5th leading causes of death in the United States.7–9
While hypertension and hypercholesterolemia can be improved through modifications in diet and physical activity, pharmacologic therapy is often required to achieve optimal management.4, 5, 10 To reduce cardiovascular disease risk, effective management typically involves ongoing tailoring of medications and clinical interactions to support patients in remaining adherent.11 Many patients have concurrent hypertension and hyperlipidemia,12 and medication nonadherence is an important factor limiting optimal management.13–16 Having both hypertension and hyperlipidemia confers greater cardiovascular risk than having either condition alone,17 and it is important to understand medication adherence for both conditions, individually and collectively.12, 18 Few published studies have assessed adherence levels to both antihypertensive and statin medications when taken concurrently across a large segment of the population, including populations at high risk for cardiovascular events like Medicare beneficiaries.19
The purpose of this paper is to describe levels of adherence to antihypertensive and statin medication, individually and collectively, among Medicare Part D beneficiaries and assess how these levels of adherence vary by demographic and geographic characteristics. Examining factors related to adherence may help identify populations in greater need of services supporting adherence.20–22 We describe adherence to antihypertensive and statin medications, individually and collectively, at the state and county levels and observing the variation in adherence by race-ethnicity and by county of residence urbanicity (metropolitan, micropolitan, or rural). These findings can inform public health, clinical, and health system efforts to improve adherence among those groups with lowest adherence.
Methods
Administrative and prescription medication data for all beneficiaries with Medicare Part D coverage in 2017 were accessed using the Centers for Medicare & Medicaid (CMS) Chronic Conditions Data Warehouse via the CMS Virtual Research Data Center (https://www.ccwdata.org/web/guest/homeexternal icon). There were 33.1 million beneficiaries aged ≥65 years as of January 1, 2017 who were in continuous enrollment in full fee-for-service (FFS) Medicare (i.e., Part A and Part B coverage within Original Medicare) with additional prescription medication plan (PDP) coverage or in a Medicare Advantage prescription medication (MA-PD) plan during January 1–December 31, 2017 and were not receiving care in long-term care facilities.23, 24 Of these, 25.1 million had at least one antihypertensive or statin prescription filled in 2017, leaving them eligible for analysis (see Supplemental Figure 1).
Analyses were limited to beneficiaries with two or more antihypertensive prescriptions filled within the same pharmacologic therapeutic class or two or more statin prescriptions filled with different service dates during a measurement period of >90 days (N = 25.1 million); the >90-day measurement period helps ensure an adequate amount of time is available to assess adherence. The Uniform System of Classification25 pharmaceutical product classification schema was used to identify the following antihypertensive therapeutic classes: angiotensin converting enzyme inhibitors and angiotensin II receptor blockers, beta blockers, calcium channel blockers, diuretics, and other antihypertensive medications, which included selective aldosterone receptor inhibitors, peripheral vasodilators, alpha blockers, and centrally acting agents; as well as to identify statin medications. Control of hypertension often requires the use of more than one antihypertensive medication class.4 Current guidance recommends HMG-CoA reductase inhibitors (statin medications) as the first line therapy for hypercholesterolemia,5,26 and these were used as a proxy for cholesterol-lowering therapy in this study.
Nonadherence was measured using the proportion of days covered (PDC) metric which represents the percentage of days a beneficiary had access to the prescribed medication from the date of the first fill through the end of 2017 or the beneficiary’s death in 2017.21, 27 A PDC was calculated for each class for which a beneficiary met the inclusion criteria. If multiple prescriptions for the same target medication (i.e., same generic ingredient) were dispensed on different days such that the prescriptions overlapped, the start date for the new prescription accounted for the remaining medication from the previous fill. Days’ supply that extended beyond the end of the measurement period was not included in the PDC calculation. Beneficiaries with a PDC ≥80% were considered adherent; a standard threshold that has been shown to be associated with improved health outcomes.28, 29 Among beneficiaries taking multiple antihypertensive medications from different classes, an overall PDC was calculated as an average of the PDCs calculated for each therapeutic class.
Adherence among beneficiaries taking both antihypertensive and statin medications was further summarized by describing the percentage with a PDC ≥80% for both medication types. Factors assessed for relationship with adherence were age; sex; race/ethnicity (non-Hispanic White, non-Hispanic Black, Asian/Pacific Islander, American Indian/Alaska Native, Hispanic, Other and Unknown); income status (Standard or Low Income Subsidy status (LIS), which includes persons eligible for both Medicare and Medicaid)30; prescription medication plan (PDP) type (Fee for Service (FFS-PDP) or Medicare Advantage (MA-PD)); and beneficiaries’ county of residence urbanicity (metropolitan core-based statistical area [CBSA], micropolitan CBSA, or rural [i.e., non-CBSA]). Additional factors assessed included if the beneficiary had any fills for fixed-dose combinations, which are medications that contain multiple active ingredients in one pill (No; Yes, which includes the following: 1) a single pill containing ≥2 antihypertensive drugs; 2) a single pill containing ≥1 antihypertensive drugs and a statin); if ≥1 fills were obtained via mail order pharmacies; the number of prescribers for each medication type, as a proxy for continuity of care for hypertension and hypercholesteremia management with the number of unique prescribers in 2017 grouped into three categories (one, two, and three or more prescribers; the larger the number of unique prescribers may indicate less continuity of care); and out of pocket costs for medications (calculated as the mean out of pocket cost per 30-day supply (cost per therapy day * 30) of either an antihypertensive medication, a statin medication, or both, and categorized as quartiles).
Adherence was stratified by beneficiaries’ state or territory of residence and mapped by county of residence using a spatial empirical Bayesian smoothing technique to enhance estimate stability.31 The minimum and maximum adherence county-level values were calculated for each state, as well as the percentage of counties that met the ≥80% adherence threshold. Crude prevalence estimates were calculated for each factor assessed, as well as prevalence ratios based on average marginal predictions32, 33 that adjusted for, where appropriate, age, sex, race/ethnicity, income status, prescription medication plan type (PDP), county urbanicity, any fixed-dose combination use, any mail order use, and continuity of care level. Analyses used SAS Version 9.4 (SAS Institute Inc, Cary, North Carolina). This study was considered exempt from Institutional Review Board review under federal regulations covering Department of Health and Human Services projects designed to study, evaluate, or examine public benefit or service programs.
Results
In 2017, 25.1 million Medicare Part D beneficiaries were taking antihypertensive and/or statin medications. Among the 22.5 million who were taking antihypertensive medications, 77.1% were adherent; among the 16.1 million taking statin medications, 81.9% were adherent; and, among the 13.5 million taking antihypertensive and statin medications,70.3% were adherent to both (Table 1). Non-Hispanic White beneficiaries were the racial/ethnic group with the greatest adherence (72.4%) to both medication types (Table 1).
Table 1.
Adherencea to antihypertensive and statin medications by beneficiary characteristics, Medicare Part D, 2017
| Participant Characteristics | Antihypertensive medication adherence | Statin medication adherence | Antihypertensive and Statin medication adherence (to both) | |
|---|---|---|---|---|
| Total beneficiaries N | Total beneficiaries with PDC N (% adherent) | Total beneficiaries with PDC N (% adherent) | Total beneficiaries with PDC N (% adherent) | |
| Total | 25,062,387 | 22,518,824 | 16,089,559 | 13,545,996 |
| N adherent (% adherent) | 17,371,021 (77.1) | 13,183,785 (81.9) | 9,516,062 (70.3) | |
| Sex, by age (years) | ||||
| Female | ||||
| 65–74 | 7,004,430 | 77.1 | 80.2 | 69.1 |
| 75–84 | 5,127,363 | 76.9 | 81.2 | 69.2 |
| ≥85 | 2,433,298 | 75.4 | 81.4 | 68.3 |
| Male | ||||
| 65–74 | 5,524,450 | 78.5 | 83.1 | 72.5 |
| 75–84 | 3,779,908 | 77.7 | 83.9 | 71.5 |
| ≥85 | 1,192,938 | 74.5 | 83.1 | 68.7 |
| Race/Ethnicity | ||||
| White, non-Hispanic | 19,060,049 | 78.9 | 83.9 | 72.4 |
| Black | 2,259,943 | 69.0 | 73.4 | 61.0 |
| Asian/Pacific Islander | 864,884 | 77.6 | 81.6 | 71.1 |
| American Indian/Alaska Native | 64,440 | 63.5 | 71.2 | 56.9 |
| Hispanic | 2,295,176 | 71.4 | 73.8 | 62.0 |
| Other | 204,509 | 77.2 | 81.4 | 70.3 |
| Unknown | 313,386 | 81.3 | 84.7 | 75.1 |
| Income status | ||||
| Standard | 20,451,812 | 78.4 | 82.7 | 71.5 |
| LIS or Medicaid dual eligible | 4,610,575 | 72.0 | 78.4 | 65.4 |
| Prescription medication plan type | ||||
| FFS-PDP | 13,183,329 | 77.0 | 82.0 | 70.1 |
| MA-PD | 11,879,058 | 77.3 | 81.9 | 70.5 |
| Urban/Rural Classification | ||||
| Metro | 20,787,808 | 77.1 | 81.8 | 70.2 |
| Micro | 2,468,380 | 77.4 | 82.7 | 70.8 |
| Rural | 1,806,199 | 76.8 | 82.3 | 70.2 |
| Any fixed-dose combination use | ||||
| No | 958,782 | 77.9 | 77.6 | 71.5 |
| Yes | 24,103,605 | 77.1b | 82.8c | 70.2d |
| Any mail order use | ||||
| No | 19,933,072 | 75.6 | 80.6 | 68.6 |
| Yes | 51,293,315 | 83.2 | 87.0 | 75.9 |
| Continuity of care for medication management proxy | ||||
| 1 prescriber | 14,044,693 | 80.5 | 82.2 | 74.8 |
| 2 prescribers | 6,957,169 | 74.6 | 80.7 | 68.7 |
| ≥3 prescribers | 4,060,525 | 68.3 | 82.1 | 61.9 |
| Out of pocket cost (mean cost per 30-day supply) |
||||
| Quartile 1 (Lowest) | 5,630,027 | 78.9 | 83.5 | 72.0 |
| Quartile 2 | 6,086,063 | 76.8 | 82.1 | 70.5 |
| Quartile 3 | 5,171,727 | 77.1 | 83.3 | 71.2 |
| Quartile 4 (Highest) | 5,631,007 | 75.7 | 78.9 | 67.2 |
Abbreviations: PDC = Proportion of days covered; FFS-PDP = Medicare fee-for-service prescription medication plan; MA-PD = Medicare Advantage prescription medication plan; LIS = Low-Income Subsidy
Measured as PDC ≥ 0.8
= Percent adherent to antihypertensive medication among users taking a fixed-dose combination (i.e., a single pill containing ≥2 antihypertensive drugs with or without a statin).
= Percent adherent to statin medication among users taking a fixed-dose combination (i.e., a single pill containing ≥1 antihypertensive drugs and a statin).
= Percent adherent to both antihypertensive and statin medications among users taking a fixed-dose combination (i.e., a single pill containing either ≥2 antihypertensive drugs with or without a statin OR a single pill containing ≥1 antihypertensive drugs and a statin).
Among beneficiaries taking both an antihypertensive and a statin, American Indian/Alaska Native (adjusted prevalence ratio 0.83, 95% confidence limit 0.82–0.84), Hispanic (0.90, 0.90–0.91) and non-Hispanic Black beneficiaries (0.87, 0.86–0.87) were less likely to be adherent compared to non-Hispanic White beneficiaries (Table 2). These disparities persisted when stratified by county urbanicity (Figure 1). For example, in rural counties, adherence to antihypertensive and statin medications combined was lower among American Indian/Alaska Native (0.77, 0.74–0. 79) and non-Hispanic Black beneficiaries (0.84, 0.83–0.85) when compared to non-Hispanic White beneficiaries. Similarly, in micropolitan counties, adherence to antihypertensive and statin medications combined was lower among American Indian/Alaska Native (0.81, 0.78–0.83) and non-Hispanic Black beneficiaries (0.84,0.83–0.85) when compared to non-Hispanic White beneficiaries. These racial/ethnic disparities persisted even after controlling for U.S. Region/territory (not shown).
Table 2.
Adjusteda prevalence ratio for adherence to antihypertensive and statin medications, by beneficiary characteristics, Medicare Part D, 2017
| Category | Antihypertensive medication adherence aPRb (95% CL) |
Statin medication adherence aPRb (95% CL) |
Antihypertensive and statin medication adherence (to both) aPRb (95% CL) |
|
|---|---|---|---|---|
| Sex, by age (years) | ||||
| Female | ||||
| 65–74 | referent | referent | referent | |
| 75–84 | 0.9997(0.9983, 1.001) | 1.0052(1.0036, 1.0068) | 1.001(0.9991, 1.0029) | |
| ≥85 | 0.9836(0.9818, 0.9853) | 1.0037(1.0015, 1.006) | 0.9903(0.9877, 0.9928) | |
| Male | ||||
| 65–74 | referent | referent | referent | |
| 75–84 | 0.9912(0.9896, 0.9928) | 1.0046(1.0029, 1.0063) | 0.9888(0.9868, 0.9908) | |
| ≥85 | 0.9537(0.9514, 0.9559) | 0.9931(0.9904, 0.9958) | 0.9529(0.9499, 0.956) | |
| Race/Ethnicity | ||||
| White, non-Hispanic | referent | referent | referent | |
| Black | 0.8974(0.8958, 0.8989) | 0.8854(0.8834, 0.8873) | 0.8659(0.8638, 0.868) | |
| Asian/Pacific Islander | 1.0002(0.9975, 1.0029) | 0.985(0.9818, 0.9882) | 0.9856(0.9821, 0.989) | |
| American Indian/Alaska Native | 0.8491(0.8406, 0.8577) | 0.8724(0.8616, 0.8832) | 0.8296(0.8181, 0.8412) | |
| Hispanic | 0.9488(0.947, 0.9506) | 0.9235(0.9213, 0.9257) | 0.9048(0.9025, 0.9071) | |
| Other | 0.9818(0.9766, 0.9869) | 0.9714(0.9653, 0.9776) | 0.9678(0.9612, 0.9744) | |
| Unknown | 1.0129(1.0086, 1.0173) | 1.0058(1.0004, 1.0111) | 1.0129(1.0071, 1.0187) | |
| Income status | ||||
| Standard | referent | referent | referent | |
| LIS or Medicaid dual eligible | 0.9656(0.9643, 0.9669) | 0.9867(0.9851, 0.9882) | 0.9781(0.9763, 0.9799) | |
| Prescription medication plan type | ||||
| FFS-PDP | referent | referent | referent | |
| MA-PD | 1.0156(1.0146, 1.0166) | 1.0178(1.0167, 1.019) | 1.0265(1.0252, 1.0278) | |
| Urban/Rural Classification | ||||
| Large central metro | referent | referent | referent | |
| Micropolitan | 0.9942(0.9926, 0.9958) | 0.9985(0.9966, 1.0004) | 0.9951(0.9929, 0.9972) | |
| Rural | 0.9930(0.9912, 0.9948) | 0.9965(0.9943, 0.9987) | 0.9947(0.9921, 0.9972) | |
| Region | ||||
| Northeast | referent | referent | referent | |
| Midwest | 0.9941(0.9926, 0.9955) | 1.0063(1.0046, 1.0080) | 0.9964(0.9945, 0.9984) | |
| South | 0.9535(0.9523, 0.9548) | 0.9818(0.9803, 0.9833) | 0.9450(0.9433, 0.9467) | |
| West | 0.9652(0.9637, 0.9667) | 1.0021(1.0004, 1.0039) | 0.9738(0.9718, 0.9758) | |
| Territories | 0.8566(0.8526, 0.8606) | 0.7990(0.7945, 0.8035) | 0.7744(0.7694, 0.7795) | |
| Any fixed-dose combination use | ||||
| No | referent | referent | referent | |
| Yes | 1.0070(1.0052, 1.0088) | 1.0769(1.0752, 1.0785) | 1.0005(0.9977, 1.0033) | |
| Any mail order use | ||||
| No | referent | referent | referent | |
| Yes | 1.0756(1.0743, 1.0769) | 1.0611(1.0597, 1.0625) | 1.0711(1.0695, 1.0727) | |
| Continuity of care for medication management proxyc | ||||
| 1 prescriber | referent | referent | referent | |
| 2 prescribers | 0.9325(0.9315, 0.9335) | 0.9875(0.9861, 0.9889) | 0.9236(0.9222, 0.9249) | |
| ≥3 prescribers | 0.8600(0.8587, 0.8612) | 1.0150(1.0117, 1.0183) | 0.8372(0.8357, 0.8386) | |
| Out of pocket cost (mean cost per 30-day supply) |
||||
| Quartile 1 (Lowest) | referent | referent | referent | |
| Quartile 2 | 0.9642(0.9630, 0.9655) | 0.9905(0.9890, 0.9920) | 0.9564(0.9546, 0.9581) | |
| Quartile 3 | 0.9544(0.9530, 0.9558) | 0.9779(0.9763, 0.9795) | 0.9436(0.9418, 0.9455) | |
| Quartile 4 (Highest) | 0.9359(0.9345, 0.9373) | 0.9267(0.9252, 0.9282) | 0.8898(0.8880, 0.8916) |
Fully adjusted, where appropriate, by age, sex, race/ethnicity, income status, medication plan type, urban/rural classification, fixed-dose use (any), mail order user (any), and continuity of care,
aPR-Adjusted prevalence ratio,
Number of unique antihypertensive and/or statin medications prescribers in 2017 as a proxy for continuity of care for medication management.
Abbreviations: FFS-PDP = Medicare fee-for-service prescription medication plan; MA-PD = Medicare Advantage prescription medication plan; LIS = Low-income subsidy
FIGURE 1.
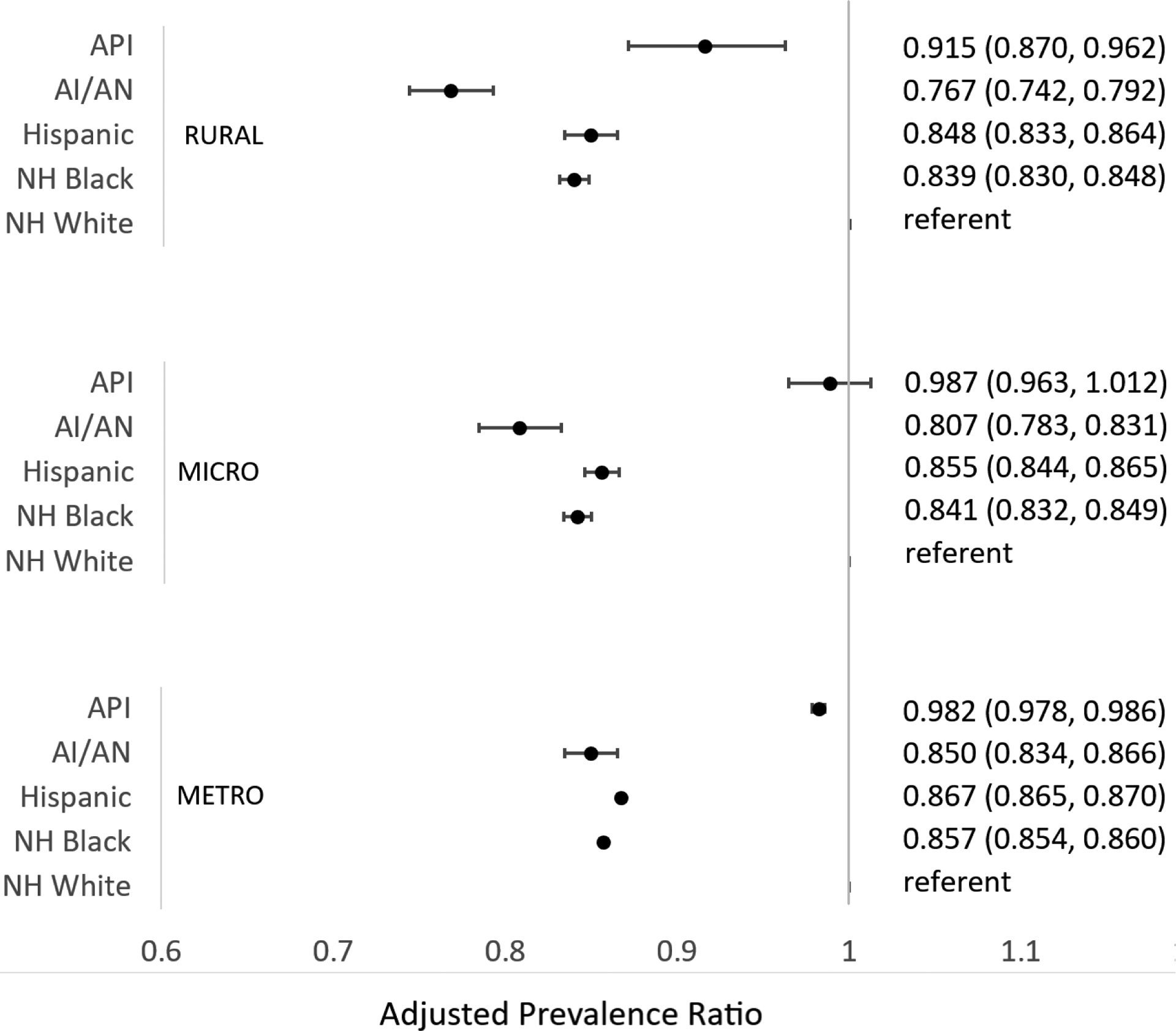
Adjusted a prevalence ratio for adherence to antihypertensive and statin medications, by county urbanicity and race/ethnicity, Medicare Part D, 2017
Abbreviations: API= Asian/Pacific Islander; AI/AN= American Indian/Alaska Native; NH = Non-Hispanic
a Fully adjusted, where appropriate, by age, sex, income status, medication plan type, urban/rural classification, fixed-dose use (any), mail order user (any), and continuity of care. The referent group is non-Hispanic White beneficiaries.
Overall, county urbanicity had minimal association with adherence to both antihypertensive and statin medications (Table 2). Adherence to both antihypertensive and statin medications was higher among beneficiaries with Standard income status (71.5%) than Low Income Subsidy status (LIS) (65.4%) (Table 1). However, in adjusted models, adherence was nearly equivalent among those with LIS compared to Standard income status (0.98,0.98–0.98) (Table 2). Adherence to both antihypertensive and statin medications was higher among mail order pharmacy users (1.07, 1.07–1.07). Beneficiaries who may have lacked continuity of care (i.e., with ≥ 3 prescribers) were less likely to be adherent to both antihypertensive and statin medications (0.84, 0.84–0.84) compared to beneficiaries with only 1 prescriber. Beneficiaries with the highest out of pocket costs for antihypertensive and statin medications were less likely to be adherent to both (0.89, 0.89–0.89) when compared to beneficiaries with the lowest out of pocket costs.
By state/territory, adherence to antihypertensive medications ranged from 52.0% (U.S. Virgin Islands) to 83.8% (North Dakota), adherence to statin medications ranged from 48.5% (U.S. Virgin Islands) to 88.2% (Vermont), and adherence to both medication types ranged from 39.3% (U.S. Virgin Islands) to 78.5% (Vermont) (Supplemental Table 1). County-level adherence ranged across the United States from 25.7% (Alaska) to 88.5% (North Dakota) for antihypertensives, 36.0%% (Alaska) to 93.8% (Montana) for statin medications, and 20.8% (Alaska) to 92.9% (Colorado) for both medications combined and tended to be the lowest in the southeastern United States (Figure 2). Four states had 100% of counties with antihypertensive adherence ≥80% (Minnesota, New Hampshire, Rhode Island, and Vermont); 11 had 100% of counties with statin medication adherence ≥80%; none had 100% of counties with adherence ≥80% to both medication types. Fifteen states/territories had 0% of counties with antihypertensive medication adherence ≥80%; 5 had 0% of counties with statin medication adherence ≥80%; and most (N=43) had 0% of counties with adherence ≥80% to both medication types (Supplemental Table 2).
FIGURE 2:

Prevalence of antihypertensive and statin medication adherence among Medicare Part D beneficiaries aged ≥65 years, by county — United States, Puerto Rico, and U.S. Virgin Islands, 2017
Discussion
In 2017, 25.1 million Medicare Part D beneficiaries were taking one or more antihypertensive medications and/or a statin medication. Among those, 5.1 million beneficiaries were considered nonadherent to their antihypertensive medication therapy, 2.9 million to their statin medication therapy, and 4.0 million to the combination of antihypertensive and statin medication therapy. This places millions of older U.S. adults at potentially elevated risk for having uncontrolled hypertension and unmanaged hypercholesterolemia and, as a result, at elevated risk for having a cardiovascular event.28, 29 Blood pressure control rates have decreased recently in the United States, including among older adults,34 and, despite cholesterol levels improving over the past decade with dietary changes and increased use of lipid-lowering medications, high cholesterol continues to contribute significantly to cardiovascular disease-related mortality.35, 36 Therefore, actions to support improved adherence to the medications used to treat these conditions may be necessary, as adherence is a crucial component of the overall strategy needed to improve management of these conditions.
In this study, adherence to statin medications was slightly higher (~82%) among beneficiaries compared to adherence to antihypertensive medications (~77%). This may be partly because of patient-related factors, such as personal perceptions about the effectiveness of statin medication therapy,37 self-reported experiences with clinicians,38 or attitudes and beliefs about taking medications.39 Physician-related factors, such as disparities in treatment intensification or the role of specialty care, may also influence adherence (e.g., in one study, patients under a cardiologist’s care were more likely to be adherent to statin medications).22, 40 In addition, medication-related factors, such as the complexity of antihypertensive regimens and the need to take more than once-daily medications,41–45 and use of home remedies,46 may influence adherence.
As evidenced in other studies,20–22, 47 continued demographic disparities and geographic variation in adherence were observed for use of both medication types. These findings likely contribute, in part, to specific groups (e.g., non-Hispanic Black) and regions (e.g., Southeastern United States) having poorer hypertension and cholesterol management and elevated risk for cardiovascular events.2, 48
Previous research has identified multiple barriers that affect adherence.49 Medication-related barriers include the complexity of the medication regimen as well as side effects.49 Patient-related factors can include the presence of comorbidities or chronic conditions, perceptions, and medication-taking behaviors.37, 50 Socioeconomic factors include health literacy, as well as medication costs and copayments.49 Healthcare system barriers can include lack of continuity of care, poor access to healthcare or poor quality of the patient-physician relationship,51 or bureaucratic processes associated with insurance claims.14
In this study, low levels of adherence were consistently identified among beneficiaries living in U.S. territories, which aligns with other evidence of gaps in key hospital performance measures and poorer outcomes for Medicare beneficiaries in the territories.52 Furthermore, within most states, even many that have relatively high rates of adherence, considerable variation was observed at the county level. For example, the median difference between the counties with the lowest and highest adherence to both antihypertensive and statin medications within each state was around 15 percentage points. This level of county variation has also been found for heart disease mortality.53 Therefore, it is important to note that county-level variation in adherence to antihypertensive and statin medication can be masked when adherence is only assessed at the state level.
There is evidence in the literature about differences in the prevalence of hypertension and in the prevalence of antihypertensive medication use across counties by urbanicity.54 However, in this study, adherence levels did not vary by county urbanicity among all beneficiaries combined. Racial/ethnic disparities in adherence were observed across all county urbanicity types, with the most pronounced disparities among American Indian/Alaska Native beneficiaries in rural counties. Poor health care experiences and difficulties in getting needed care in rural counties have been reported by American Indian/Alaska Native beneficiaries.55 Additionally, most (92%) rural counties with American Indian/Alaska Native populations have been identified as health professional shortage areas, compared with 65% of all rural counties nationally.56 Trends previously observed in rural communities that may possibly undermine medication adherence include decreased access to care,57, 58 not having a primary care provider,58 and having difficulty in getting to the clinic to get medications.59 Other factors, such as perceived social standing in the community, specifically among African Americans,60 and language concordance, particularly among Hispanics,61 may play a role in medication adherence, as well as other health disparities and health inequities.62
A metanalysis of medication adherence interventions among adults with hypertension found treatment subjects taking, on average, only 4% more of their prescribed daily doses than control subjects.63 However, among treatment subjects, the intervention effect was sufficient to show a difference that may lead to meaningful clinical improvement, as reductions of as small as 3 mmHg in systolic blood pressure have been found to be associated with 8% reductions in stroke mortality and 5% reductions in mortality from coronary heart disease.64 One strategy that has been shown to improve adherence is to simplify the treatment regimen, such as limiting pill burden by using fixed-dose combinations.65–67 Other strategies focus on enhancing continuity of care and team-based care,68 including management of hypertension and cholesterol by pharmacists using a team-care approach as described in the Million Hearts Hypertension Control Change package.69–71 For healthcare providers, training resources are available on how to discuss medication adherence with patients and how to incorporate such discussions in routine visits.72 Additional patient-focused strategies can include using education materials in different languages and formats, and supporting patient use of self-measured blood pressure monitoring.73
This study has limitations. First, PDC calculations assess the availability of medication and not the actual compliance with medication, which may lead to the overestimation of adherence especially among mail order recipients who can receive automatic refills. Although use of administrative data to assess nonadherence has previously correlated well with other methods of adherence assessment, including among older adults,14, 74 increasing use of PDC as a performance measure and expansion of programs that incentivize pharmacies to utilize automated refill programs may have led to overestimation of adherence by PDC.75, 76 Second, because we excluded members with only one antihypertensive or statin fill and were unable to include those who were prescribed medication but never initiated treatment, adherence was likely overestimated. About 762,785 beneficiaries in this study had only one filled prescription within an antihypertensive class and 1.24 million beneficiaries had just one fill for a statin medication and, therefore, did not have a PDC calculated. Other studies have found that up to one fourth of prescriptions for newly prescribed antihypertensive are never filled.77 Third, adherence might be underestimated among beneficiaries who discontinued a medication, switched antihypertensive classes based on their clinician’s recommendation, or sometimes directly purchased low-priced generic medications without involvement of their prescription medication plan but were considered nonadherent. Fourth, the continuity of care proxy measure might not accurately reflect its intended purpose, as a higher number of prescribers per patient might indicate better team-based care rather than fractured care. Fifth, diagnostic codes for hypertension or hyperlipidemia were unavailable for Medicare Advantage prescription drug plans. Some patients may have been taking these medications for other conditions; however, among Medicare Fee for Service beneficiaries in our analyses, the percentage taking antihypertensive medications without a diagnosis for hypertension was low (3%) and the percentage taking statin medications without a diagnosis of hyperlipidemia was 4%.
In conclusion, adherence to antihypertensive and statin medications remain suboptimal among Medicare Part D beneficiaries. Collectively, adherence to concurrent use of both medications is even lower, which is concerning given that millions of beneficiaries are at increased risk for potentially having a life-altering and costly cardiovascular event. Additional public health and clinical efforts can be implemented to address social determinants of health, remove structural barriers to healthcare, improve access to medications, and address adherence, especially among minority groups and within the regions at greatest risk for adverse cardiovascular outcomes.
Supplementary Material
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflicts of Interest: The authors have no conflicts of interest to disclose.
References
- 1.Ritchey MD, Wall HK, George MG, Wright JS. US trends in premature heart disease mortality over the past 50 years: Where do we go from here? Trends Cardiovasc Med 2020;30(6):364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation 2021;143(8):e254–e743. [DOI] [PubMed] [Google Scholar]
- 3.Zhang D, Wang G, Zhang P, Fang J, Ayala C. Medical Expenditures Associated With Hypertension in the U.S., 2000–2013. Am J Prev Med 2017;53(6S2):S164–S171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71(6):1269–1324. [DOI] [PubMed] [Google Scholar]
- 5.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;139(25):e1082–e1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Control Hypertension. . In: Services USDoHaH, editor. Washington, DC; 2020. [Google Scholar]
- 7.Wright JS, Wall HK, Ritchey MD. Million Hearts 2022: Small Steps Are Needed for Cardiovascular Disease Prevention. JAMA 2018;320(18):1857–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ford ES, Capewell S. Proportion of the decline in cardiovascular mortality disease due to prevention versus treatment: public health versus clinical care. Annu Rev Public Health 2011;32:5–22. [DOI] [PubMed] [Google Scholar]
- 9.Ahmad FB, Anderson RN. The Leading Causes of Death in the US for 2020. JAMA 2021;325(18):1829–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Micha R, Peñalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association Between Dietary Factors and Mortality From Heart Disease, Stroke, and Type 2 Diabetes in the United States. JAMA 2017;317(9):912–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allen JD, Curtiss FR, Fairman KA. Nonadherence, clinical inertia, or therapeutic inertia? J Manag Care Pharm 2009;15(8):690–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmieder RE, Ruilope LM. Blood Pressure Control in Patients With Comorbidities. The Journal of Clinical Hypertension 2008;10(8):624–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bosworth HB, Granger BB, Mendys P, Brindis R, Burkholder R, Czajkowski SM, et al. Medication adherence: a call for action. Am Heart J 2011;162(3):412–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation 2009;119(23):3028–35. [DOI] [PubMed] [Google Scholar]
- 15.Chapman RH, Benner JS, Petrilla AA, Tierce JC, Collins SR, Battleman DS, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med 2005;165(10):1147–52. [DOI] [PubMed] [Google Scholar]
- 16.Yusuf S, Lonn E, Pais P, Bosch J, López-Jaramillo P, Zhu J, et al. Blood-Pressure and Cholesterol Lowering in Persons without Cardiovascular Disease. N Engl J Med 2016;374(21):2032–43. [DOI] [PubMed] [Google Scholar]
- 17.Neaton JD, Wentworth D. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316,099 white men. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med 1992;152(1):56–64. [PubMed] [Google Scholar]
- 18.Egan BM, Li J, Qanungo S, Wolfman TE. Blood pressure and cholesterol control in hypertensive hypercholesterolemic patients: national health and nutrition examination surveys 1988–2010. Circulation 2013;128(1):29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krumholz HM, Nuti SV, Downing NS, Normand SL, Wang Y. Mortality, Hospitalizations, and Expenditures for the Medicare Population Aged 65 Years or Older, 1999–2013. JAMA 2015;314(4):355–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ritchey M, Chang A, Powers C, Loustalot F, Schieb L, Ketcham M, et al. Vital Signs: Disparities in Antihypertensive Medication Nonadherence Among Medicare Part D Beneficiaries - United States, 2014. MMWR Morb Mortal Wkly Rep 2016;65(36):967–76. [DOI] [PubMed] [Google Scholar]
- 21.Chang TE, Ritchey MD, Park S, Chang A, Odom EC, Durthaler J, et al. National Rates of Nonadherence to Antihypertensive Medications Among Insured Adults With Hypertension, 2015. Hypertension 2019;74(6):1324–1332. [DOI] [PubMed] [Google Scholar]
- 22.Colantonio LD, Rosenson RS, Deng L, Monda KL, Dai Y, Farkouh ME, et al. Adherence to Statin Therapy Among US Adults Between 2007 and 2014. J Am Heart Assoc 2019;8(1):e010376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Medicare.gov. Your Medicare Coverage Choices. [cited 2022 Jan 6]; Available from: https://www.medicare.gov/what-medicare-covers/your-medicare-coverage-choices
- 24.Medicare.gov. How do Medicare Advantage Plans work?. [cited 2022 Jan 6]; Available from: https://www.medicare.gov/sign-up-change-plans/types-of-medicare-health-plans/medicare-advantage-plans
- 25.IQVIA. The Uniform System of Classification. . 2020 October 17 [cited 2022 Jan 6]; Available from: https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/the-uniform-system-of-classification.pdf;
- 26.Mercado C, DeSimone AK, Odom E, Gillespie C, Ayala C, Loustalot F. Prevalence of Cholesterol Treatment Eligibility and Medication Use Among Adults--United States, 2005–2012. MMWR Morb Mortal Wkly Rep 2015;64(47):1305–11. [DOI] [PubMed] [Google Scholar]
- 27.Raebel MA, Schmittdiel J, Karter AJ, Konieczny JL, Steiner JF. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med Care 2013;51(8 Suppl 3):S11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Will JC, Zhang Z, Ritchey MD, Loustalot F. Medication Adherence and Incident Preventable Hospitalizations for Hypertension. Am J Prev Med 2016;50(4):489–499. [DOI] [PubMed] [Google Scholar]
- 29.Yang Q, Chang A, Ritchey MD, Loustalot F. Antihypertensive Medication Adherence and Risk of Cardiovascular Disease Among Older Adults: A Population-Based Cohort Study. J Am Heart Assoc 2017;6(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.CMS.gov. Medicare-Medicaid General Information: Medicare-Medicaid Enrollee Categories. [cited 2022 Jan 6]; Available from: https://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/MedicareMedicaidGeneralInformation
- 31.Marshall RJ. Mapping disease and mortality rates using empirical Bayes estimators. J R Stat Soc Ser C Appl Stat 1991;40(2):283–94. [PubMed] [Google Scholar]
- 32.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol 2010;171(5):618–23. [DOI] [PubMed] [Google Scholar]
- 33.Tamhane AR, Westfall AO, Burkholder GA, Cutter GR. Prevalence odds ratio versus prevalence ratio: choice comes with consequences. Stat Med 2016;35(30):5730–5735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, et al. Trends in Blood Pressure Control Among US Adults With Hypertension, 1999–2000 to 2017–2018. JAMA 2020;324(12):1190–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patel N, Bhargava A, Kalra R, Parcha V, Arora G, Muntner P, et al. Trends in Lipid, Lipoproteins, and Statin Use Among U.S. Adults: Impact of 2013 Cholesterol Guidelines. J Am Coll Cardiol 2019;74(20):2525–2528. [DOI] [PubMed] [Google Scholar]
- 36.Repositioning of the global epicentre of non-optimal cholesterol. Nature 2020;582(7810):73–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nanna MG, Navar AM, Zakroysky P, Xiang Q, Goldberg AC, Robinson J, et al. Association of Patient Perceptions of Cardiovascular Risk and Beliefs on Statin Drugs With Racial Differences in Statin Use: Insights From the Patient and Provider Assessment of Lipid Management Registry. JAMA Cardiol 2018;3(8):739–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ogedegbe G, Harrison M, Robbins L, Mancuso C, Allegrante J. Barriers and facilitators of medication adherence in hypertensive African Americans: a qualitative study. Ethn Dis 2004;14(1):3–12. [PubMed] [Google Scholar]
- 39.Kressin NR, Wang F, Long J, Bokhour BG, Orner MB, Rothendler J, et al. Hypertensive patients’ race, health beliefs, process of care, and medication adherence. J Gen Intern Med 2007;22(6):768–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Manze M, Rose AJ, Orner MB, Berlowitz DR, Kressin NR. Understanding racial disparities in treatment intensification for hypertension management. J Gen Intern Med 2010;25(8):819–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dunbar-Jacob J, Bohachick P, Mortimer MK, Sereika SM, Foley SM. Medication adherence in persons with cardiovascular disease. J Cardiovasc Nurs 2003;18(3):209–18. [DOI] [PubMed] [Google Scholar]
- 42.Syed ST, Sharp LK, Kim Y, Jentleson A, Lora CM, Touchette DR, et al. Relationship Between Medication Adherence and Distance to Dispensing Pharmacies and Prescribers Among an Urban Medicaid Population with Diabetes Mellitus. Pharmacotherapy 2016;36(6):590–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ingersoll KS, Cohen J. The impact of medication regimen factors on adherence to chronic treatment: a review of literature. J Behav Med 2008;31(3):213–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Eisen SA, Miller DK, Woodward RS, Spitznagel E, Przybeck TR. The effect of prescribed daily dose frequency on patient medication compliance. Arch Intern Med 1990;150(9):1881–4. [PubMed] [Google Scholar]
- 45.Turner BJ, Hollenbeak C, Weiner MG, Ten Have T, Roberts C. Barriers to adherence and hypertension control in a racially diverse representative sample of elderly primary care patients. Pharmacoepidemiol Drug Saf 2009;18(8):672–81. [DOI] [PubMed] [Google Scholar]
- 46.Cuffee YL, Rosal M, Hargraves JL, Briesacher BA, Akuley S, Altwatban N, et al. Does Home Remedy Use Contribute to Medication Nonadherence Among Blacks with Hypertension? Ethn Dis 2020;30(3):451–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Couto JE, Panchal JM, Lal LS, Bunz TJ, Maesner JE, O’Brien T, et al. Geographic variation in medication adherence in commercial and Medicare part D populations. J Manag Care Spec Pharm 2014;20(8):834–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ferdinand KC, Yadav K, Nasser SA, Clayton-Jeter HD, Lewin J, Cryer DR, et al. Disparities in hypertension and cardiovascular disease in blacks: The critical role of medication adherence. J Clin Hypertens (Greenwich) 2017;19(10):1015–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Burnier M, Egan BM. Adherence in Hypertension. Circ Res 2019;124(7):1124–1140. [DOI] [PubMed] [Google Scholar]
- 50.Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. 2008;336(7653):1114–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bokhour BG, Berlowitz DR, Long JA, Kressin NR. How do providers assess antihypertensive medication adherence in medical encounters? J Gen Intern Med 2006;21(6):577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rodriguez-Vila O, Nuti SV, Krumholz HM. Healthcare Disparities Affecting Americans in the US Territories: A Century-Old Dilemma. Am J Med 2017;130(2):e39–e42. [DOI] [PubMed] [Google Scholar]
- 53.Vaughan AS, Ritchey MD, Hannan J, Kramer MR, Casper M. Widespread recent increases in county-level heart disease mortality across age groups. Ann Epidemiol 2017;27(12):796–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Samanic CM, Barbour KE, Liu Y, Wang Y, Fang J, Lu H, et al. Prevalence of Self-Reported Hypertension and Antihypertensive Medication Use by County and Rural-Urban Classification - United States, 2017. MMWR Morb Mortal Wkly Rep 2020;69(18):533–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Martino SC, Mathews M, Agniel D, Orr N, Wilson-Frederick S, Ng JH, et al. National racial/ethnic and geographic disparities in experiences with health care among adult Medicaid beneficiaries. Health Serv Res 2019;54 Suppl 1(Suppl 1):287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Probst JC, Moore CG, Glover SH, Samuels ME. Person and place: the compounding effects of race/ethnicity and rurality on health. Am J Public Health 2004;94(10):1695–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mainous AG 3rd, King DE, Garr DR, Pearson WS. Race, rural residence, and control of diabetes and hypertension. Ann Fam Med 2004;2(6):563–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.James CV, Moonesinghe R, Wilson-Frederick SM, Hall JE, Penman-Aguilar A, Bouye K. Racial/Ethnic Health Disparities Among Rural Adults - United States, 2012–2015. MMWR Surveill Summ 2017;66(23):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Martin MY, Kim YI, Kratt P, Litaker MS, Kohler CL, Schoenberger YM, et al. Medication adherence among rural, low-income hypertensive adults: a randomized trial of a multimedia community-based intervention. Am J Health Promot 2011;25(6):372–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cummings DM, Wu J-R, Cene C, Halladay J, Donahue KE, Hinderliter A, et al. Perceived Social Standing, Medication Nonadherence, and Systolic Blood Pressure in the Rural South. J Rural Health 2016;32(2):156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to Cardiovascular Disease Medications: Does Patient-Provider Race/Ethnicity and Language Concordance Matter? J Gen Intern Med 2010;25(11):1172–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liao Y, Bang D, Cosgrove S, Dulin R, Harris Z, Taylor A, et al. Surveillance of health status in minority communities - Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. MMWR Surveill Summ 2011;60(6):1–44. [PubMed] [Google Scholar]
- 63.Conn VS, Ruppar TM, Chase JA, Enriquez M, Cooper PS. Interventions to Improve Medication Adherence in Hypertensive Patients: Systematic Review and Meta-analysis. Curr Hypertens Rep 2015;17(12):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Collins R, Peto R, Godwin J, MacMahon S. Blood pressure and coronary heart disease. Lancet 1990;336(8711):370–1. [DOI] [PubMed] [Google Scholar]
- 65.Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med 2004;164(7):722–32. [DOI] [PubMed] [Google Scholar]
- 66.Baird MG, Bentley-Taylor MM, Carruthers SG, Dawson KG, Laplante LE, Larochelle P, et al. A study of efficacy, tolerance and compliance of once-daily versus twice-daily metoprolol (Betaloc) in hypertension. Betaloc Compliance Canadian Cooperative Study Group. Clin Invest Med 1984;7(2):95–102. [PubMed] [Google Scholar]
- 67.Girvin B, McDermott BJ, Johnston GD. A comparison of enalapril 20 mg once daily versus 10 mg twice daily in terms of blood pressure lowering and patient compliance. J Hypertens 1999;17(11):1627–31. [DOI] [PubMed] [Google Scholar]
- 68.Warren JR, Falster MO, Tran B, Jorm L. Association of continuity of primary care and statin adherence. PLoS One 2015;10(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hypertension Control Change Package In: Services USDoHaH, editor. 2nd ed. Atlanta, GA: Centers for Disease Control and Prevention; 2020. [Google Scholar]
- 70.Overwyk KJ, Dehmer SP, Roy K, Maciosek MV, Hong Y, Baker-Goering MM, et al. Modeling the Health and Budgetary Impacts of a Team-based Hypertension Care Intervention That Includes Pharmacists. Med Care 2019;57(11):882–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Community Preventive Services Task F. Team-based care to improve blood pressure control: recommendation of the Community Preventive Services Task Force. Am J Prev Med 2014;47(1):100–2. [DOI] [PubMed] [Google Scholar]
- 72.HHS.gov. Million Hearts: Medication Adherence. [cited 2022 Jan 7]; Available from: https://millionhearts.hhs.gov/tools-protocols/medication-adherence.html
- 73.Fletcher BR, Hartmann-Boyce J, Hinton L, McManus RJ. The Effect of Self-Monitoring of Blood Pressure on Medication Adherence and Lifestyle Factors: A Systematic Review and Meta-Analysis. Am J Hypertens 2015;28(10):1209–21. [DOI] [PubMed] [Google Scholar]
- 74.Sattler EL, Lee JS, Perri M 3rd. Medication (re)fill adherence measures derived from pharmacy claims data in older Americans: a review of the literature. Drugs Aging 2013;30(6):383–99. [DOI] [PubMed] [Google Scholar]
- 75.Lester CA, Mott DA, Chui MA. The Influence of a Community Pharmacy Automatic Prescription Refill Program on Medicare Part D Adherence Metrics. Journal of managed care & specialty pharmacy 2016;22(7):801–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Leslie RS, Tirado B, Patel BV, Rein PJ. Evaluation of an integrated adherence program aimed to increase Medicare Part D star rating measures. J Manag Care Spec Pharm 2014;20(12):1193–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fischer MA, Choudhry NK, Brill G, Avorn J, Schneeweiss S, Hutchins D, et al. Trouble getting started: predictors of primary medication nonadherence. Am J Med 2011;124(11):1081 e9–22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


