Abstract
Purpose
To investigate a novel marker to diagnose posterior staphylomas by measuring the radius of the steepest curvature on the retinal pigment epithelium (RPE) segmentation line using optical coherence tomography (OCT).
Study Design
Retrospective Cross-sectional Study.
Methods
The authors developed a prototype software to measure the radius of curvature on the RPE segmentation line of OCT. Twelve images of 9-mm radial OCT scans were used. The radius of curvature was measured at the steepest area of the RPE segmentation line, and the macular curvature (MC) index was calculated based on its reciprocal. Based on the wide-field fundus findings, the study sample was divided into three groups: definite posterior staphyloma, no posterior staphyloma, and undetermined. The differences of MC index among the groups and the correlation between the MC index, age, and axial length were analyzed.
Results
The present study analyzed 268 eyes, with 54 (20.1%) with definite posterior staphyloma, 202 (75.4%) with no posterior staphyloma, and 12 (4.5%) with undetermined disease status. A maximum MC index of 37.5 was observed in the group with no posterior staphyloma, which was less than the minimum MC index of 42.7 observed in the group with definite posterior staphyloma. The MC index had strong correlations with the axial length and age in eyes with high myopia.
Conclusions
Eyes with posterior staphyloma have a steeper curvature than those with radius 8.44 mm, while eyes without posterior staphyloma do not. MC index 40 (radius 8.44 mm) might act as a reference to distinguish between those with and those without posterior staphyloma.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12886-024-03321-z.
Keywords: Diagnosis, Curvature, OCT, Posterior staphyloma, Pathologic myopia, Radius, Retinal pigment, Epithelium
Introduction
The prevalence of myopia is rapidly increasing worldwide [1, 2]. Myopic eyes with very long axial lengths or a high degree of myopic refractive error, like 26 mm or longer or -6 diopter or less are classified as eyes with high myopia [3–6]. Pathologic myopia is defined as myopia having pathologic changes related to myopia, and posterior staphyloma is a key component of these pathologic changes [7–9]. However, no consensus has yet been established regarding the diagnosis of posterior staphyloma.
Posterior staphyloma is a structural deformity of the eyeball defined as “an outpouching of the posterior wall of the eye” [10]. Fundus photography [4, 11–14], ultrasonography [3, 15], three-dimensional magnetic resonance imaging (3D MRI) [14], and ultra-widefield optical coherent tomography (OCT) [3, 16–18] have been used to detect posterior staphyloma through the identification of inflection points.
However, posterior staphyloma is typically a progressive condition [3, 16, 19]. As inflection lines are difficult to detect during the early stages of development, their utility in the early diagnosis of posterior staphyloma remains limited [16]. Additionally, the method of identifying inflection is not suitable for monitoring the progression or change in posterior staphyloma.
Posterior staphyloma, a deformity of the posterior eyeball, has a steep curvature of the retinal pigment epithelium (RPE) segmentation line in OCT. We hypothesized that the radius of curvature might be a marker that reflects the severity of posterior staphyloma. We measured the radius of the steepest curvature on the RPE segmentation line and attempted to utilize the radius to detect posterior staphyloma and to follow up its progression.
Methods
The Institutional Review Board of Pusan National University Hospital approved the study protocol (1901-011-075), which complied with the tenets of the Declaration of Helsinki. The current retrospective study included 268 patients who underwent swept-source OCT (Atlantis or Triton, Topcon, Japan) imaging with 12 9-mm radial scans and IOL master (Carl Zeiss Meditec, Dublin, CA) to measure axial length between January 2015 and December 2018. Twelve 9 mm-radial OCT scan of patients whose eyes had information of axial lengths measured by IOL master were reviewed. Eyes with macular edema or a history of vitreoretinal surgery were excluded from the study. Epiretinal membrane that seems stable was not excluded. Among patients with two eligible eyes for inclusion, the eye with the longer axial length was included.
We developed a prototype software to measure the radius of curvature on the RPE segmentation line in OCT images. Our software was developed for Windows using Microsoft Visual Studio 2015, C# language with a dot net library, and Telerik library for advanced user interface (supplementary Fig. 1). The measurements were performed on 12 9-mm radial scans. The segmentation errors were manually corrected. The software automatically detected the RPE segmentation line (Fig. 1A). As the presenting image was elongated to twice the size in the vertical dimension in the machine software, the horizontal-to-vertical pixel ratio was corrected to 1:1 (Fig. 1B). The region of interest was defined by excluding 100 pixels in the horizontal dimension on both sides of the image.
Fig. 1.
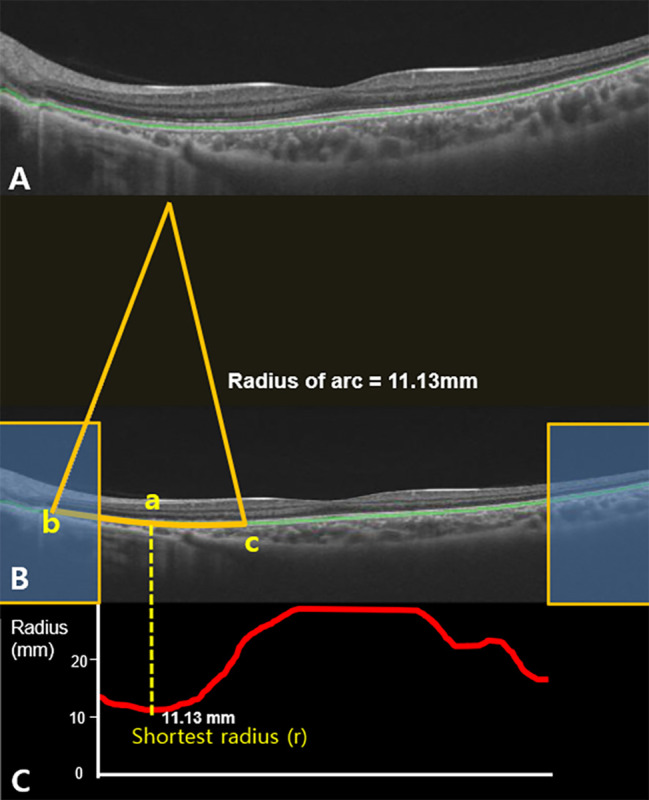
The prototype software to automatically measure radii of arcs on retinal pigment epithelium (RPE) segmentation line on OCT images. (A) The machine software automatically detects the RPE segmentation line (green line). (B) Given that the raw OCT images were elongated to twice the size in the vertical dimension in the machine software, the horizontal to vertical pixel ratio was corrected to 1:1. The region of interest was defined by excluding 100 pixels in the horizontal dimension on both sides of the image (Yellow box). The arc at the pixel (a) was made by connecting two pixels (b and c) apart by 1.4 mm [100 pixels apart from the pixel (a)] on RPE segmentation line. (C) The radius of arc was calculated at every pixel on the RPE segmentation line in the region of interest and they were presented as the graph (red line). Among graphs of the radii of arc (red line), the shortest radius was named ‘r’ (mm) (Fig. 1C). The average ‘r’ of the 12 radial OCT scans was designated as ‘R’ (mm)
The radius of the arc was calculated at every pixel on the RPE segmentation line in the region of interest; an arc on each pixel was made by connecting two pixels that were 1.4 mm apart (100 pixels apart from the pixel) on the RPE segmentation line, and its radius was calculated by the software (Fig. 1B). Among the measured radii, the shortest radius in a single radial OCT scan image was considered as ‘r’ (mm) (Fig. 1C). The average ‘r’ of the 12 radial scans was designated as ‘R’ (mm). The reciprocal of R was multiplied by a constant (337.5). The calculated parameter was defined as the macular curvature index (MC index = 337.5/R).
The presence of posterior staphyloma was assessed by a single expert (SWP) using ultra-wide fundus photography (Optos PLC; Dunfermline, Scotland, UK). Eyes with a distinct inflection line of the surrounding macula were classified in the “definite posterior staphyloma” group. Eyes with no inflection line were included in the “no posterior staphyloma” group. If it was difficult to decide the presence of posterior staphyloma based on the ultra-wide fundus photo alone or if the presence of nasal, inferior, or peripapillary staphyloma was suspected, they were included in the “undetermined” group.
Statistical analysis
The calculated values are presented as mean ± standard deviation. Fisher’s exact test and Mann–Whitney U test were used to compare categorical and continuous variables, respectively. The Pearson correlation coefficient test was used to determine the significance of the associations between the MC index, age, and axial length. All statistical analyses were performed using the Statistical Package for the Social Sciences for Windows 22.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was defined as P values < 0.05.
Results
This study involved 268 subjects. The characteristics of the study subject are listed in Table 1. The mean age of the study subjects was 60.5 ± 15.8 years, and the mean axial length was 25.416 ± 2.935 mm. The mean MC index was 33.02 ± 22.62. We were able to determine whether the presence of posterior staphyloma or not in 256 eyes (95.5%) using ultra-wide fundus photography. Among them, 54 eyes (20.1%) were included in the definite staphyloma group, and 202 eyes (75.4%) were included in the no posterior staphyloma group. In the undetermined group (n = 12), half of the participants were < 45 years of age. One eye was diagnosed with retinitis pigmentosa, and three eyes were suspected to have a staphyloma other than posterior staphyloma (Table 2).
Table 1.
Summary of the age, axial length and macular curvature (MC) index in the three groups
| Number of eyes | Age | Axial length(mm) | MC index | Maximum MC index | Minimum MC index | |
|---|---|---|---|---|---|---|
| No posterior staphyloma | 202 | 60.9 ± 16.2 | 24.069 ± 1.587 | 20.62 ± 6.04 | 37.5 | 11.4 |
| Definite posterior Staphyloma | 54 | 62.2 ± 11.9 | 29.911 ± 2.044 | 71.9 ± 16.78 | 109.6 | 42.7 |
| Undetermined | 12 | 46.3 ± 18.2 | 27.863 ± 1.979 | 40.79 ± 9.57 | 55.5 | 21.3 |
| Total | 268 | 60.5 ± 15.8 | 25.416 ± 2.935 | 32.02 ± 22.62 | 109.6 | 11.4 |
| P value | < 0.001 | < 0.001 | < 0.001 |
Table 2.
Demographic characteristics of the study subjects in the group undetermined
| Age | Axial length(mm) | MC index | Specific notification | |
|---|---|---|---|---|
| 1 | 8th decade | 26.22 | 51.6 | Inferior staphyloma suspected |
| 2 | 4th decade | 27.11 | 39 | Young age |
| 3 | 5th decade | 27.22 | 39.6 |
Young Peripapillary staphyloma suspected |
| 4 | 6th decade | 27.29 | 34.5 | None |
| 5 | 7th decade | 28.01 | 40.1 | None |
| 6 | 6th decade | 28.05 | 21.3 | None |
| 7 | 5th decade | 28.71 | 30.6 | Young age |
| 8 | 3rd decade | 29.17 | 39.2 | Young age |
| 9 | 4th decade | 30.97 | 49.8 | Young age |
| 10 | 2nd decade | 31.24 | 55.5 | Young age |
| 11 | 6th decade | 24.43 | 48.6 | Retinitis pigmentosa |
| 12 | 6th decade | 25.93 | 39.7 |
Peripapillary staphyloma suspected |
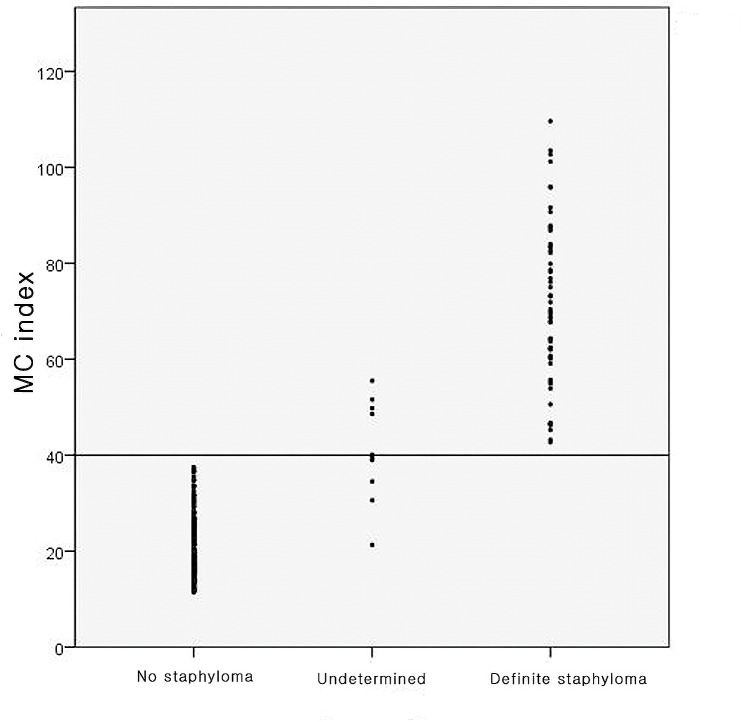
In the no posterior staphyloma group, the average MC index was 20.62 ± 6.04, the minimum MC index was 11.4, and the maximum MC index was 37.5. In the definite posterior staphyloma group, the average MC index was 71.90 ± 16.78 and ranged from 42.7 to 109.6. In the undetermined group, the average MC index was 40.79 ± 9.57, the maximum MC index was 55.5, and the minimum was 21.3 (Table 1). These results suggest that an MC index value of 40 is suggestive of posterior staphyloma (Fig. 2).
Fig. 2.
Q1The distribution of macular curvature (MC) index among the three groups. Among the 202 eyes in the no staphyloma group, the maximum MC index was 37.5. Among the 54 eyes in the definite staphyloma group, the minimum MC index was 42.7
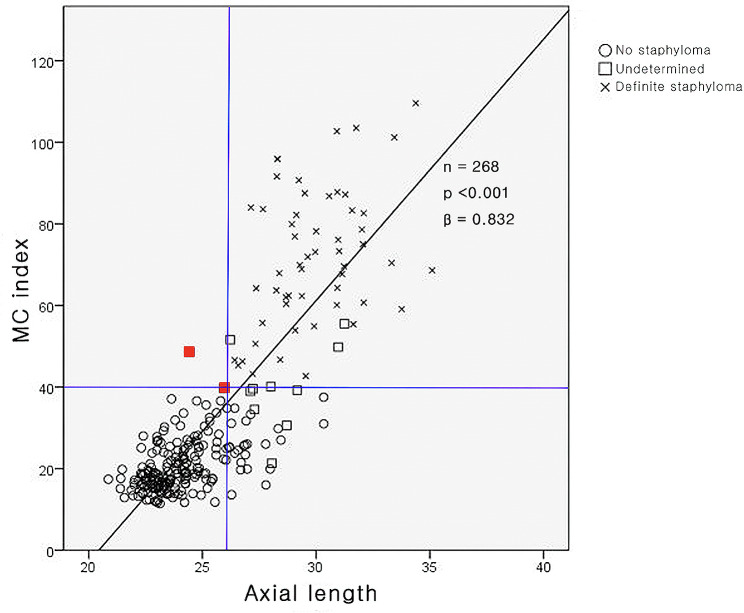
The association between the MC index and axial length is shown in Fig. 3. The MC index had a strong positive correlation with axial length (P < 0.001, r = 0.848). All eyes (n = 178) with axial length < 26 mm were classified into the no posterior staphyloma group, except for two eyes in the undetermined group (one eye with retinitis pigmentosa with an axial length of 24.43 mm and the other with an axial length of approximately 26 mm [25.93 mm]). Eyes (n = 90) with an axial length > 26 mm were classified into the no posterior staphyloma (26 eyes, 28.9%), undetermined (10 eyes, 11.1%), and definite posterior staphyloma (54 eyes, 60.0%) groups.
Fig. 3.
Correlation of the macular curvature (MC) index with the axial length. The MC index was observed to have a strong positive correlation with the axial length (P < 0.001, r = 0.848). All eyes (178 eyes) with axial length < 26 mm were classified in the no staphyloma group, except two eyes (red dots) in the undetermined group
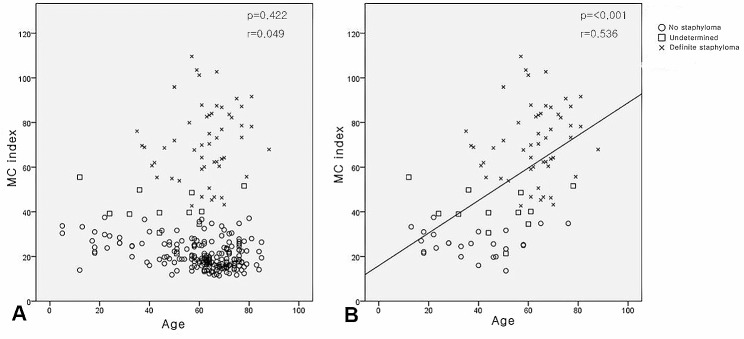
No statistically significant correlation was observed between the MC index and age (Fig. 4A, P = 0.422, r = 0.049). However, a significant correlation between the MC index and age was observed in patients with high myopia (n = 90; Fig. 4B, P < 0.001, r = 0.536).
Fig. 4.
Correlation of the macular curvature (MC) index with age. (A) Correlation of the MC index with age of patients (P = 0.422, r = 0.049), and it was not significant. (B) Correlation of the MC index with age in high myopic eyes (axial length longer than 26 mm, n = 90). A strong positive correlation was observed between the MC index and age in high myopic eyes (P < 0.001, r = 0.536)
Discussion
Spaide [10] defined posterior staphyloma as, “an outpouching of the wall of the eye that has a radius of curvature that is less than the surrounding curvature of the wall of the eye”. Two main methods have been reported for diagnosing posterior staphylomas.
The first method is to identify an inflection line, which is the boundary line between the posterior staphyloma and its surrounding posterior wall. The inflection line of the posterior staphyloma can be determined using fundus photography [4, 11–14], ultrasonography [3, 15], 3D MRI [14], and ultra-widefield OCT [16–18]. Among these, ultra-widefield OCT is widely recognized as the superior method because of its ease of use and high resolution, with inflection lines displayed as outward protrusions of the sclera along with a thin choroid [16–18]. However, there are two limitations to this. First, ultra-widefield OCT is not widely available, and conventional OCT systems lack the scan length to adequately diagnose posterior staphyloma using this method. Second, as posterior staphyloma usually progresses [3], inflection lines in its early stage may not show a definite outward protrusion of the sclera or a thin choroid. Hence, ultra-widefield OCT may lack sensitivity to detect posterior staphyloma in its early stages [16]. Therefore, the lack of inflection lines on ultra-widefield OCT may not rule out the presence of posterior staphyloma.
The second method involves measuring the curvature of the posterior ocular wall. Several studies by a research group from Kyoto University [20–23] have investigated the detection of posterior staphyloma using OCT. Given the irregular curvature of the posterior wall in eyes with staphyloma, two values have been suggested to characterize the curvature of the posterior wall: the average of its total radius and the mean deviation of the posterior wall. However, this study did not report a definite reference value for the diagnosis of posterior staphyloma.
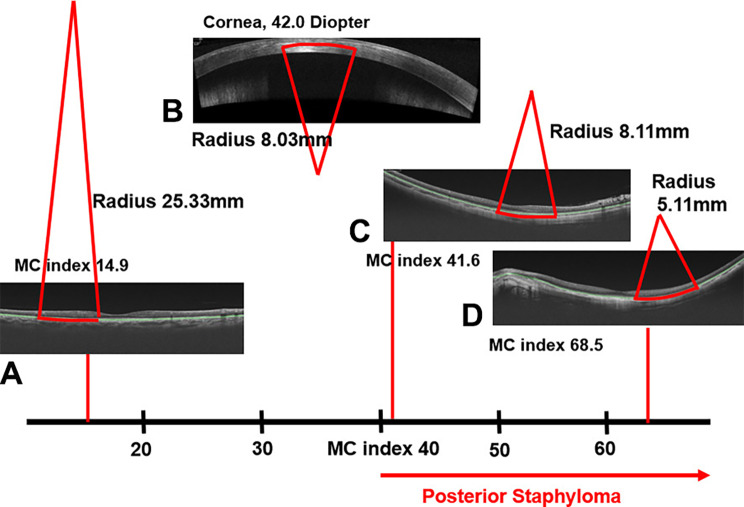
Given that structural deformity related to posterior staphyloma should present as a steep curvature of the RPE segmentation line, the current study suggests a new marker for posterior staphyloma. It detects the steepest curvature on the RPE segmentation line and measures the radius of curvature. Focal deformities on the RPE segmentation line were neglected by the software, and the average radius (R) was obtained by averaging twelve radii from 12 9 mm-radial OCT images of each eye. The MC index was calculated by taking the reciprocal of R and multiplying by the constant of 337.5. This is similar to a formula to convert the corneal radius into corneal diopters. As the principles of the two formulas are same, it is possible to indirectly compare the curvature of the RPE segmentation line to the curvature of the central cornea by using the MC index and keratometry value (radius or diopters). For example, the steepest curvature on the RPE segmentation line with an MC index of 40 (radius, 8.44 mm) corresponds to the curvature of the central cornea with 40 diopters (radius, 8.44 mm) (Fig. 5).
Fig. 5.
MC index: meaning and application in clinical practice. The MC index is the reciprocal of the radius of curvature at the steepest RPE segmentation line. (MC index = 337.5/R). This is similar to a formula to convert the corneal radius into corneal diopters. In the current cohort, the MC index was > 40 in all eyes with posterior staphyloma (C, D). This seems to be an exclusive feature compared with eyes without posterior staphyloma (A). A steeper retinal pigment epithelium (RPE) segmentation line indicated a higher MC index. As the principles of the two formulas are the same, it is possible to indirectly compare the curvature of the RPE segmentation line to that of the cornea measured through keratometry. The curvature of the RPE with an MC index of 41.6 (B) is similar to the curvature of the central cornea with 42.0 diopter (B and C)
The MC index was greater than 40 (radius shorter than 8.44 mm) in all eyes with definite posterior staphyloma. In contrast, eyes with no posterior staphyloma had an MC index of less than 40, suggesting that the MC index of 40 (radius, 8.44 mm) could be a potential biomarker for the diagnosis of posterior staphyloma. The MC index also has a significant correlation with axial length and age. Given the previously reported notion that the severity of posterior staphyloma is associated with age and axial length [20], the authors propose that the MC index may be utilized to monitor the severity of posterior staphyloma, although further studies are needed for confirmation.
Limitations
This study had some limitations. To assess the suitability and efficacy of a new diagnostic tool, it must be verified using existing methods. However, data regarding ultra-wide OCTs were not available for comparison. Hence, in the present study, the MC index was verified against the findings of the ultra-wide fundus photography. The current study included a relatively small number of eyes, so not enough eyes with atypical features may have been included. In addition, it was difficult to determine the presence of posterior staphyloma in eyes with suspected peripapillary, nasal, or inferior staphylomas, or early features of posterior staphyloma. These eyes were assigned to an undetermined group and excluded from validation of the new diagnostic value. Future studies are required to elucidate the application of our method to various types of eyes, including various subtypes of staphylomas. This retrospective study was based on cross-sectional data obtained from a single referral hospital. Considering posterior staphyloma would change by aging, the findings of the current study need to be validated in future longitudinal studies.
In addition, the current cohort did not represent the characteristics of the general population, as only eyes with a documented axial length were included in the study.
Conclusions
Eyes with posterior staphyloma have a steeper curvature than those with a radius of 8.44 mm, while eyes without posterior staphyloma do not. An MC index of 40 (radius, 8.44 mm) might act as a reference to distinguish between patients with or without posterior staphyloma. The MC index reflects the severity of posterior staphyloma; hence, it can be used as a diagnostic criterion for posterior staphyloma as well as a value to monitor its severity.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Author contributions
Sungwho Park, Sun Ho Park wrote the main manuscript text. Keun Heung Park made a software analyzing radius of posterior staphyloma. Sang Choel dealt with patients’ data Ik Soo Byon and Ji Eun Lee advised and revised the whole manuscript and figures. All authors read and approved the final manuscript.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT)(IRIS 2018047398)
Data availability
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
This study received approval of the institutional review board of Pusan national university Hospital (1901-011-075), in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was obtained from all subjects and/or their legal guardian.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Morgan IG, Ohno-Matsui K, Saw SM, Myopia The Lancet. 2012;379(9827):1739–48. doi: 10.1016/S0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- 2.Ohno-Matsui K, Akiba M, Modegi T, Tomita M, Ishibashi T, Tokoro T, et al. Association between Shape of Sclera and Myopic Retinochoroidal Lesions in patients with pathologic myopia. Invest Opthalmology Visual Sci. 2012;53(10):6046. doi: 10.1167/iovs.12-10161. [DOI] [PubMed] [Google Scholar]
- 3.Hsiang HW, Ohno-Matsui K, Shimada N, Hayashi K, Moriyama M, Yoshida T, et al. Clinical characteristics of posterior staphyloma in eyes with pathologic myopia. Am J Ophthalmol. 2008;146(1):102–110e2. doi: 10.1016/j.ajo.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 4.Chang L, Pan CW, Ohno-Matsui K, Lin X, Cheung GCM, Gazzard G, et al. Myopia-related Fundus changes in Singapore adults with high myopia. Am J Ophthalmol. 2013;155(6):991–999e1. doi: 10.1016/j.ajo.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 5.Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology. 2002;109(4):704–11. doi: 10.1016/S0161-6420(01)01024-7. [DOI] [PubMed] [Google Scholar]
- 6.Liu HH, Xu L, Wang YX, Wang S, You QS, Jonas JB. Prevalence and progression of myopic retinopathy in Chinese adults: the Beijing Eye Study. Ophthalmology. 2010;117(9):1763–8. doi: 10.1016/j.ophtha.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 7.Freund KB. Peripapillary detachment in pathologic myopia. Arch Ophthalmol. 2003;121(2):197. doi: 10.1001/archopht.121.2.197. [DOI] [PubMed] [Google Scholar]
- 8.Chen L. Rhegmatogenous Retinal Detachment due to Paravascular Linear Retinal breaks over patchy Chorioretinal Atrophy in Pathologic Myopia. Arch Ophthalmol. 2010;128(12):1551. doi: 10.1001/archophthalmol.2010.284. [DOI] [PubMed] [Google Scholar]
- 9.Ohno-Matsui K, Jonas JB. Understanding Pathologic Myopia. In: Ang M, Wong TY, editors. Updates on Myopia: A Clinical Perspective [Internet]. Singapore: Springer Singapore; 2020. pp. 201–18. 10.1007/978-981-13-8491-2_9.
- 10.Spaide RF, Staphyloma . Pathologic myopia. New York, NY: Springer New York; 2014. Part 1; pp. 167–76. [Google Scholar]
- 11.Chen SJ, Cheng CY, Li AF, Peng KL, Chou P, Chiou SH, et al. Prevalence and Associated Risk factors of myopic Maculopathy in Elderly Chinese: the Shihpai Eye Study. Invest Opthalmology Visual Sci. 2012;53(8):4868. doi: 10.1167/iovs.12-9919. [DOI] [PubMed] [Google Scholar]
- 12.Gao LQ. Prevalence and characteristics of myopic retinopathy in a Rural Chinese Adult Population. Arch Ophthalmol. 2011;129(9):1199. doi: 10.1001/archophthalmol.2011.230. [DOI] [PubMed] [Google Scholar]
- 13.Samarawickrama C, Mitchell P, Tong L, Gazzard G, Lim L, Wong TY, et al. Myopia-related Optic Disc and retinal changes in adolescent children from Singapore. Ophthalmology. 2011;118(10):2050–7. doi: 10.1016/j.ophtha.2011.02.040. [DOI] [PubMed] [Google Scholar]
- 14.Ohno-Matsui K. Proposed classification of posterior Staphylomas based on analyses of Eye shape by three-Dimensional magnetic resonance imaging and wide-field Fundus Imaging. Ophthalmology. 2014;121(9):1798–809. doi: 10.1016/j.ophtha.2014.03.035. [DOI] [PubMed] [Google Scholar]
- 15.STEIDL SM. Macular complications Associated with posterior staphyloma. Am J Ophthalmol. 1997;123(2):181–7. doi: 10.1016/S0002-9394(14)71034-7. [DOI] [PubMed] [Google Scholar]
- 16.Tanaka N, Shinohara K, Yokoi T, Uramoto K, Takahashi H, Onishi Y, et al. Posterior staphylomas and scleral curvature in highly myopic children and adolescents investigated by ultra-widefield optical coherence tomography. PLoS ONE. 2019;14(6):e0218107. doi: 10.1371/journal.pone.0218107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shinohara K, Tanaka N, Jonas JB, Shimada N, Moriyama M, Yoshida T, et al. Ultrawide-Field OCT to Investigate relationships between myopic macular retinoschisis and Posterior Staphyloma. Ophthalmology. 2018;125(10):1575–86. doi: 10.1016/j.ophtha.2018.03.053. [DOI] [PubMed] [Google Scholar]
- 18.Shinohara K, Shimada N, Moriyama M, Yoshida T, Jonas JB, Yoshimura N, et al. Posterior staphylomas in pathologic myopia imaged by Widefield Optical Coherence Tomography. Invest Opthalmology Visual Sci. 2017;58(9):3750. doi: 10.1167/iovs.17-22319. [DOI] [PubMed] [Google Scholar]
- 19.Ohno-Matsui K, Wu PC, Yamashiro K, Vutipongsatorn K, Fang Y, Cheung CMG, et al. IMI Pathologic Myopia Investigative Opthalmology & Visual Science. 2021;62(5):5. doi: 10.1167/iovs.62.5.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wakazono T, Yamashiro K, Miyake M, Hata M, Miyata M, Uji A, et al. Time-Course Change in Eye shape and development of Staphyloma in highly myopic eyes. Invest Opthalmology Visual Sci. 2018;59(13):5455. doi: 10.1167/iovs.18-24754. [DOI] [PubMed] [Google Scholar]
- 21.Wakazono T, Yamashiro K, Miyake M, Nakanishi H, Oishi A, Ooto S, et al. Association between Eye shape and myopic traction Maculopathy in High Myopia. Ophthalmology. 2016;123(4):919–21. doi: 10.1016/j.ophtha.2015.10.031. [DOI] [PubMed] [Google Scholar]
- 22.Miyake M, Yamashiro K, Akagi-Kurashige Y, Oishi A, Tsujikawa A, Hangai M, et al. Analysis of Fundus shape in highly myopic eyes by using curvature maps constructed from Optical Coherence Tomography. PLoS ONE. 2014;9(9):e107923. doi: 10.1371/journal.pone.0107923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Numa S, Yamashiro K, Wakazono T, Yoshikawa M, Miyake M, Nakanishi H, et al. Prevalence of posterior staphyloma and factors associated with its shape in the Japanese population. Sci Rep. 2018;8(1):4594. doi: 10.1038/s41598-018-22759-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article.