Abstract
Background
The purpose of this meta-analysis was to provide a pooled prevalence estimate of self-reported disordered eating (SRDE) in athletes based on the available literature, and to identify risk factors for their occurrence.
Methods
Across ten academic databases, an electronic search was conducted from inception to 7th January 2024. The proportion of athletes scoring at or above predetermined cutoffs on validated self-reporting screening measures was used to identify disordered eating (DE). Subgroup analysis per country, per culture, and per research measure were also conducted. Age, body mass index (BMI), and sex were considered as associated/correlated factors.
Results
The mean prevalence of SRDE among 70,957 athletes in 177 studies (132 publications) was 19.23% (17.04%; 21.62%), I2 = 97.4%, τ2 = 0.8990, Cochran's Q p value = 0. Australia had the highest percentage of SRDE athletes with a mean of 57.1% (36.0%-75.8%), while Iceland had the lowest, with a mean of 4.9% (1.2%-17.7%). The SRDE prevalence in Eastern countries was higher than in Western countries with 29.1% versus 18.5%. Anaerobic sports had almost double the prevalence of SRDE 37.9% (27.0%-50.2%) compared to aerobic sports 19.6% (15.2%-25%). Gymnastics sports had the highest SRDE prevalence rate, with 41.5% (30.4%-53.6%) while outdoor sports showed the lowest at 15.4% (11.6%-20.2%). Among various tools used to assess SRDE, the three-factor eating questionnaire yielded the highest SRDE rate 73.0% (60.1%-82.8%). Meta-regression analyses showed that female sex, older age, and higher BMI (all p < 0.01) are associated with higher prevalence rates of SRDE.
Conclusion
The outcome of this review suggests that factors specific to the sport affect eating behaviors throughout an athlete's life. As a result, one in five athletes run the risk of developing an eating disorder. Culture-specific and sport-specific diagnostic tools need to be developed and increased attention paid to nutritional deficiencies in athletes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40337-024-00982-5.
Keywords: Anorexia, Aerobic energy, Athletes, Eating disorders, Sport type, World region
Plain language summary
Disordered eating (DE) refers to eating behaviors that limit food choices, reduce or exaggerate food intake, cause physical discomfort, create a sense of loss of control, or lead to negative emotions like shame or guilt. The DE label does not signify the presence of a diagnosed mental health disorder, but, rather, describes self-reported, regular eating patterns that psychiatrists consider to fall into the at-risk category for an eating disorder. In this review, we performed a search of academic databases to find all relevant studies that measured the frequency of self-reported DE in athletes. We analyzed 177 studies involving over 70,000 athletes in total. In this study, DE was defined as a score above cut-off on validated screening tests for problematic eating behaviors. Our goal was to estimate the prevalence of DE in athletes globally and to determine the factors that increase risk. We found that approximately 1 in 5 athletes (19%) endorsed DE behaviors such as, among others, restrictive dieting, bingeing, and purging. These behaviors were seen most commonly in indoor sports like gymnastics and less commonly in the context of outdoor sports. Rates were highest in female athletes, older athletes, athletes with high body mass index (BMI) scores, and those from Eastern countries and cultures. Australia had the highest rates (over 50%), while rates were lowest in Iceland. We suggest the development of screening tests specifically tailored and applicable to athletes. In addition, we recommend raising public awareness of the health effects of nutrition in sports.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40337-024-00982-5.
Introduction
Eating disorders (EDs) are serious, all too often chronic, mental illnesses that usually begin in adolescence or young adulthood [1, 2]. Approximately thirty million people globally suffer from EDs, disorders that are frequently misdiagnosed and under (ineffectively) treated [3]. There is general agreement that a variable and complicated combination of biological, psychological, social, and cultural factors cumulatively increases the risk of ED [4].
In the general adult population, anorexia nervosa (AN) and bulimia nervosa (BN) are clinically recognized EDs that, at least in part, reflect the extremes of a continuum of traits that include negative body image, food restraint, and preoccupation with weight and musculature in the formation of self-identity [5, 6]. According to longitudinal risk factor studies [5, 6], negative body image and "disordered eating" (DE), and "screening for at-risk" individuals is where this continuity assumption is most visibly present [7, 8]. Continuity assumption in this context refers to the assumption that DE lies on a continuum from normal eating to clinical disorders [9].
Negative body image and DE are the strongest predictors of the development of full-blown EDs [10]. Together, they constitute an "at risk" state [11]. While usually associated with women, and attributed to occupations such as modeling or ballet where weight must be restricted, EDs are also prevalent in males, and especially in both male and female sports [12, 13]. They are most likely to develop in athletes who compete in sports that a) promote leanness as a way to improve performance, b) divide team eligibility according to weight, or c) receive points based on appearance [14]. Athletes' risk of acquiring EDs varies according to their gender, sport, and also level of competition [15]. Self-reported measures for DE are useful as screening tools because they are inexpensive, and easy to apply [8, 16]. They help identify preclinical "at risk" DE behavior [8, 16].
In a recent published meta-analysis [5] of SRDE in university students, our research team applied the Levine and Smolak definition of DE [17, 18]. This definition consists of: a) unhealthy, maladaptive, and stress-inducing levels of negative body image, weight and shape concerns, dietary restrictions and/or binge eating [2, 17]; b) at least two of the following: individual ED symptoms such as self-induced vomiting after eating, abuse of laxatives, diuretics, diet pills, and exercise, unrealistic beauty standards, including an idealization of thinness, irrational and maladaptive beliefs about body fat and fat people, often coupled with a strong drive for thinness, relatively high levels of negative affect that is difficult to endure and manage, and harsh self-surveillance and self-criticism, often accompanied by low and unstable self-esteem [5]. Noting the lack of a previously agreed-upon definition of DE and thus the lack of research data about its point prevalence, Levine and Smolak [2]estimated their definition of DE to be present in 15–20% of the general population. They noted, however, that available studies used different definitions and different cut-off points for DE on questionnaires such as the Eating Attitudes Test (EAT-26) [2].
The connection between DE and sports, has been gaining attention over the last two decades[8]. Up to 5% of people in the community have ED, and, athletes report higher frequencies of EDs than non-athletes. In one study, when compared to non-athletes, female athletes showed a 45% higher prevalence of DE practices (i.e., under the threshold for a diagnosis of full-blown ED). In male athletes, the rate was 19% higher than for non-athletes [19]. A recent article from Jordan by Ghazzawi et al., (2022) indicated that overall, 35% (1%-62%) of Jordanian athletes were at substantial risk for ED [20]. As mentioned earlier, several factors explain discrepancies among reports and account for the broad prevalence range cited by Ghazzawi et al. [20–23].
Recent studies point to the promotion of a healthy body image as a helpful foundation for addressing athletes' DE [24, 25]. Athletes may be susceptible to EDs because the prevalent idealized body image in sports emphasizes leanness or low body weight, particularly so in endurance, aesthetic, and weight class competitions [15, 24, 26]. Other contributing factors are: early sport-specific training, participation in weight-class sports, the engrained habit of frequent dieting and subsequent weight fluctuation[27], the wearing of skimpy sportswear, coaching pressure, and involvement in elite-level competition [20, 26, 28]. Female athletes are considered more vulnerable than males to concerns regarding body mass and shape; they may, therefore, use more extreme weight-control techniques than men [29].[29]Athletes who base their identity and, hence, their self-esteem, on their love of the game they play have less trouble with SRDE than those whose identity is based on their personal game skills and successes (which fluctuate). Low self-esteem is a significant risk factor leading to body image problems and subsequent ED [15].
Athletes may not, however, be more at risk for ED than the general population. Some meta-analyses [21] have shown a higher frequency of risky eating behaviors in non-athletes. Either way, the evidence for an elevated risk of EDs among athletes is not conclusive [22, 30, 31] In an attempt to help resolve the debate and to extend our previous meta-analytic reviews of SRDE in athletes [5, 6, 32], we conducted a meta-analysis of its global prevalence. To the best of our knowledge, based on searches of the literature and various registration platforms, this is the first such meta-analysis of DE and potential moderators in this population. In this meta-analysis, we aimed to synthesize the available literature to provide a pooled estimate of the prevalence of SRDE in athletes.
Materials and Methods
The study's methodology was submitted to Open Science Framework (OSF; 10.17605/OSF.IO/EJ2QN) in September 2022. OSF is a freely available platform that enables researchers to share their research ideas with peers and to receive assistance over the duration of a study.
The review follows the guidelines for reporting, as recommended by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA2020) [33]. The Meta-analysis of Observational Studies in Epidemiology (MOOSE) [34] procedure was followed in relation to the statistical analyses and to the reporting of results.
Search strategy
In September 2022, two authors (HJ and HG) conducted an online literature review using ten databases. 1) PubMed/MEDLINE, 2) American Psychological Association PsycINFO, 3) ScienceDirect, 4) Springer, 5) EBSCOhost, 6) Embase, 7) Cumulative Index to Nursing and Allied Health Literature (CINAHL), 8) Scopus, 9) Web of Science, and 10) SportDiscus. The following keywords and lists were used in the full-text search: Athletes, gymnasts, or elite, are on List A. On List B are eating disorders, eating habits, feeding disorders, eating symptoms, eating attitudes, or eating issues. The punctuation marks (*) ensure that the phrase's reverse word order is considered in the search method. For instance, "disordered eating" and "eating disorders" are included when searching for "eating disord*."
The authors also manually searched the citation lists of included articles. The manual reference list checking helps safeguard against missing relevant literature, but incorporating as wide a range of terms as possible directly into the database searches aids the process. Meta-analyses that exclude grey literature have a higher propensity to overstate effect sizes and thus produce less accurate effect size estimations. As a result, we deliberately sought out organizational reports, unreleased studies, and research in lesser-known journals.
Three members of the team (LN, AH, and HT) independently evaluated the initial article selection. After screening titles, abstracts, and complete texts and eliminating duplicate studies, initial data were extracted, and their quality was assessed independently by two team members (LN and AH). Discussion among all team members was able to resolve any differences regarding a study's eligibility.
Criteria for exclusion, inclusion, and eligibility (selection process)
The complete text of English-language papers on SRDE among athletes of all sports types and all ages around the globe was obtained for meta-analysis.
Inclusion criteria: 1) English language 2) original research 3) all types of sports, all ages, anywhere in the world 4) the prevalence of DE needed to be included 5) evaluation was performed by a screening tool with well-defined cut-offs for clinical diagnosis of eating disorders.
Exclusion criteria: 1) studies of current or former players who did not meet athlete criteria at the time of the study 2) mental health studies in athletes unrelated to DE 3) data unavailable even after attempt to contact authors directly 4) book chapters and review articles (systematic and meta-analysis) 5) studies in which prevalence rates were reported but only in the form of group means.
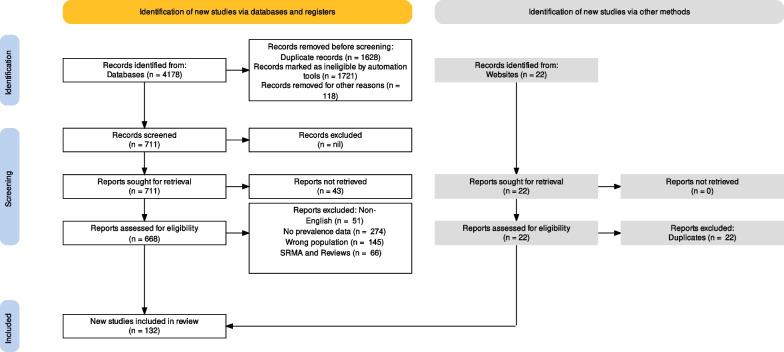
The PRISMA2020 process flow for research selection is shown in Fig. 1.
Fig. 1.
PRISMA2020 flow diagram for study selection
Procedure (data collection process)
The 648 included papers were scanned and categorized using ASReview, an online free service that integrates digital tools (such as natural-language processing) with machine learning tools. By using a free, open-source, web-based program WebPlotDigitizer v4.5, data could be taken from plot images.
To ensure uniform data description, authors LN, AH, HT, and HG individually collected the following eight factors: author names, year of publication, country of data collection, representativeness of the sample, average BMI (kg/m2), gender (% of female participants), and average age (in years), and method utilized to identify SRDE presence or absence. Using the regional categories of member states created by the United Nations, this meta-analysis study included data from forty countries, which were then categorized as Eastern or Western. Eastern countries were those with emerging markets or economies in development. Western countries are defined as advanced economies with high GDP per capita, such as those in Western Europe, the U.S., Australia [35].
Evaluation of study quality and bias risk (risk of bias assessment)
Participant selection (sample), comparability, and statistical analysis/results make up the first three items on the Newcastle–Ottawa Scale (NOS) checklist [36]. Each item in the NOS is rated on a scale of one to three (or four) stars. The highest possible rating for each study, therefore, would either be nine (for cohort studies and cross-sectional studies) or ten stars (case–control studies). Studies that score an eight are still judged to be of good quality with little chance of bias. A 5–7 score is judged to be of moderate quality with some chance of bias, and a 0–4 score is low quality with a significant chance of bias.
As noted earlier, the prevalence estimate for each study was based on a pre-defined cut-off score of a validated screening tool, that is, a continuous measure of DE risk such as the EAT-26 and Sick, Control, One stone, Fat, Food test (SCOFF) (Table 1).
Table 1.
Characteristics of the studies involved in the systematic review and meta-analysis about the prevalence of disordered eating in Athletes
| SN | REF | Study | Country | Sample Characteristics | Design | Measure |
|---|---|---|---|---|---|---|
| 1 | [59] | Abbott et al., 2021 | Multiple | Female sex = 30.8%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 2 | [46] | Akesdotter et al., 2022 | Sweden | Female sex = 68%; mean age 23.5 years; mean BMI NR Kg/m2 | Cohort study | RD |
| 3 | [48] | Al-Jumayan et al., 2021 | Saudi Arabia | Female sex = 48.9%; mean age 31 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 4 | [60] | Alwan et al., 2022 | UK | Female sex = 100%; mean age 29 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 5 | [61] | Anderson and Petrie 2012 | USA | Female sex = 100%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | QEDD |
| 6 | [62] | Armento et al., 2023 | Colorado | Female sex = 70%; mean age 40.9 years; mean BMI 22.8 kg/m2 | Cross-sectional study | EDEQ |
| 7 | [63] | Barrack et al., 2008 | USA | Female sex = 100%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EDEQ |
| 8 | [64] | Barrack et al., b 2023 | USA | Female sex = 100%; mean age 15.7 years; mean BMI 22.0 kg/m2 | Cross-sectional study | EDEQ |
| 9 | [65] | Beals and Hill, 2006 | USA | Female sex = 100%; mean age 19.5 years; mean BMI 22.9 kg/m2 | Cross-sectional study | EDEQ |
| 10 | [66] | Beals and Manore 2002 | USA | Female sex = 100%; mean age 19 years; mean BMI 22.5 kg/m2 | Cross-sectional study |
M1 = EAT-26 M2 = EDI-3 |
| 11 | [67] | Beals, 2002 | USA | Female sex = 100%; mean age 15.8 years; mean BMI 22.2 kg/m2 | Cross-sectional study | EDI |
| 12 | [68] | Beekley et al., 2009 | USA | Female sex = 14%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 13 | [69] | Borgelt and Burmeister 2022 | USA | Female sex = 100%; mean age 22 years; mean BMI 23.26 kg/m2 | Cross-sectional study | EAT-26 |
| 14 | [70] | Borowiec et al., b 2023 | Poland |
Female sex = NR%; mean age 23.2 years; mean BMI NR Kg/m2 |
Cross-sectional study | EAT-26 |
| 15 | [71] | Brook et al., a 2019 | Multiple | Female sex = 42.3%; mean age 31.7 years; mean BMI NR Kg/m2 | Cohort study T1 & T2 | EDEQ |
| 16 | [47] | Brown et al., 2014 | USA | Female sex = 100%; mean age 22 years; mean BMI 20.88 kg/m2 | Cross-sectional study | RD |
| 17 | [72] | Brown et al., 2020 | USA | Female sex = 100%; mean age 20.15 years; mean BMI 23.29 kg/m2 | Cohort study | EAT-26 |
| 18 | [73] | Burrows et al., 2007 | Canada | Female sex = 100%; mean age 31.1 years; mean BMI NR Kg/m2 | Cross-sectional study | SIAB-S |
| 19 | [74] | Byrne and McLean 2002 | Australia | Female sex = 59%; mean age 19.55 years; mean BMI 21.25 kg/m2 | Cross-sectional study | EDI-2 |
| 20 | [75] | Carvalhais et al., 2019 | Portugal | Female sex = 100%; mean age 20.8 years; mean BMI NR Kg/m2 | Cross-sectional study | EDEQ |
| 21 | [76] | Chatterton and Petrie 2013 | USA | Female sex = 0%; mean age 19.9 years; mean BMI 24.3 kg/m2 | Cross-sectional study | QEDD |
| 22 | [77] | Checa Olmos et al., b 2023 | Spain | Female sex = 35.9%; mean age 14.1 years; mean BMI NR Kg/m2 | SCOFF | |
| 23 | [78] | Cobb et al., 2003 | USA | Female sex = 100%; mean age 21.75 years; mean BMI 21.35 kg/m2 | Cross-sectional study | EDI |
| 24 | [79] | Coelho et al., a 2013 | Brazil | Female sex = 100%; mean age 14.77 years; mean BMI NR Kg/m2 | Cross-sectional study |
M1 = EAT-26 M2 = BITE M3 = BSQ |
| 25 | [80] | Cox et al., 1997 | USA | Female sex = 92%; mean age 19.3 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 26 | [81] | De Borja et al., a 2021 | USA | Female sex = 100%; mean age 19.8 years; mean BMI 22.86 kg/m2 | Cross-sectional study |
M1 = BEDA-Q M2 = RD M3 = ESP |
| 27 | [82] | Dervish et al., b 2023 | USA | Female sex = 100%; mean age NR years; mean BMI NR Kg/m2 | Cross-sectional study | FAST |
| 28 | [83] | Devrim et al., 2018 | Turkey | Female sex = 0%; mean age 28.25 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-40 |
| 29 | [84] | Doyle-Lucas et al., 2010 | USA | Female sex = 100%; mean age 24.3 years; mean BMI 18.9 kg/m2 | Cross-sectional study | EAT-26 |
| 30 | [85] | Escobar-Molina et al., 2015 | Spain | Female sex = 46%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-40 |
| 31 | [86] | Ferrand and Brunet 2004 | France | Female sex = 0%; mean age 21.8 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 32 | [87] | Filaire et al., 2011 | France | Female sex = 50%; mean age 19.5 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 33 | [88] | Flatt et al., 2021 | Multiple | Female sex = 92%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | RD |
| 34 | [22] | Fortes et al., 2014 | Brazil | Female sex = 20%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 35 | [20] | Ghazzawi et al., 2022 | Jordan | Female sex = 41%; mean age 31 years; mean BMI 25 kg/m2 | Cross-sectional study | EAT-26 |
| 36 | [89] | Gibson et al., 2019 | New Zealand | Female sex = 0%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EDI-3 |
| 37 | [1] | Giel et al., 2016 | German | Female sex = 44%; mean age 16.3 years; mean BMI NR Kg/m2 | Cross-sectional study | SCOFF |
| 38 | [90] | Glotz et al., a 2013 | Brazil | Female sex = 0%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study |
M1 = EAT-26 M2 = BITE |
| 39 | [91] | Godoy-Izquierdo and Díaz 2021 | Spain | Female sex = 100%; mean age 20.9 years; mean BMI 23.1 kg/m2 | Cross-sectional study | EAT-26 |
| 40 | [92] | Gouttebarge and Kerkhoffs, a 2017 | Multiple | Female sex = 0%; mean age 22 years; mean BMI NR Kg/m2 | Cohort study | RD |
| 41 | [93] | Gouttebarge et al., 2017 | Multiple | Female sex = 64%; mean age 27.3 years; mean BMI NR Kg/m2 | Cross-sectional study | RD |
| 42 | [94] | Gouttebarge et al., 2017 | Multiple | Female sex = 50%; mean age 33 years; mean BMI NR Kg/m2 | Cohort study | RD |
| 43 | [95] | Greenleaf et al., 2009 | USA | Female sex = 100%; mean age 20 years; mean BMI 23 kg/m2 | Cross-sectional study | QEDD |
| 44 | [53] | Gullivera et al., 2015 | Australia | Female sex = 53%; mean age 24.9 years; mean BMI NR Kg/m2 | Cross-sectional study | SCOFF |
| 45 | [96] | Hauck et al., 2020 | German | Female sex = 56.4%; mean age 36.44 years; mean BMI 22.83 kg/m2 | Cross-sectional study | EDDS |
| 46 | [97] | Hoch et al., 2011 | USA | Female sex = 100%; mean age 23.2 years; mean BMI 19 kg/m2 | Cohort study | EDEQ |
| 47 | [98] | Hoch et al., 2009 | USA | Female sex = 100%; mean age 16.5 years; mean BMI 21.6 kg/m2 | Cross-sectional study | EAT-26 |
| 48 | [99] | Hopkinson and Lock, a 2004 | USA | Female sex = 48%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study |
M1 = EAT-26 M2 = EDEQ |
| 49 | [100] | Hulley and Hill 2001 | UK | Female sex = 100%; mean age 28.5 years; mean BMI 21.05 kg/m2 | Cross-sectional study | EDEQ |
| 50 | [101] | Janout and Janoutová c 2004 | Czech Republic | Female sex = 100%; mean age 22 years; mean BMI 18 kg/m2 | Cross-sectional study | EAT-26 |
| 51 | [102] | Joubert et al., 2022 | USA | Female sex = 100%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | RD |
| 52 | [103] | Joubert et al., 2020 | Multiple | Female sex = 23.1%; mean age 32.5 years; mean BMI 22.4 kg/m2 | Cross-sectional study | EAT-26 |
| 53 | [104] | Junge and Hauschild 2023 | German | Female sex = 55.8%; mean age NR years; mean BMI NR Kg/m2 | Cross-sectional study | EDE-QS |
| 54 | [105] | Kampouri et al., 2019 | Greece | Female sex = 100%; mean age 23.66 years; mean BMI 22.07 kg/m2 | Cross-sectional study | EDEQ |
| 55 | [106] | Karlson et al., 2001 | USA | Female sex = 100%; mean age 19.89 years; mean BMI 20.21 kg/m2 | Cross-sectional study | EDEQ |
| 56 | [107] | Karlsson et al., 2023 | Sweden | Female sex = 100%; mean age 32.4 years; mean BMI NR Kg/m2 | Cross-sectional study | EDEQ |
| 57 | [108] | Kennedy et al., 2017 | USA | Female sex = 52.11%; mean age 40.3 years; mean BMI 23.7 kg/m2 | Cross-sectional study | EAT-26 |
| 58 | [109] | Kristjánsdóttir et al., a 2019 | Iceland | Female sex = 68.9%; mean age 24.8 years; mean BMI NR Kg/m2 | Cross-sectional study |
M1 = EDEQ M2 = BULIT-R |
| 59 | [110] | Lauder et al., 1999 | USA | Female sex = 100%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EDI |
| 60 | [111] | Lauder et al., 1999 | USA | Female sex = 100%; mean age 27.5 years; mean BMI 23.5 kg/m2 | Cross-sectional study | EDI |
| 61 | [56] | Lichtenstein et al., 2021 | Denmark | Female sex = 51%; mean age 19.3 years; mean BMI 21.55 kg/m2 | Cross-sectional study | SCOFF |
| 62 | [112] | Marshall and Harber 1996 | Canada | Female sex = 100%; mean age 20.8 years; mean BMI 23.5 kg/m2 | Cross-sectional study | EDI |
| 63 | [113] | Martínez Rodríguez et al., 2015 | Spain | Female sex = 35%; mean age 20.9 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 64 | [114] | Martinovic et al., 2022 | China | Female sex = 45%; mean age 24.2 years; mean BMI 24.2 kg/m2 | Cross-sectional study | ORTO-15 |
| 65 | [115] | McLester et al., 2014 | Multiple | Female sex = 100%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EDI-2 |
| 66 | [116] | Meng et al., b 2020 | China | Female sex = 100%; mean age 20 years; mean BMI 18.6 kg/m2 | Cross-sectional study | EDI-3 |
| 67 | [117] | Michaels et al., 2023 | USA | Female sex = 92.9%; mean age NR years; mean BMI NR Kg/m2 | Cross-sectional study | RD |
| 68 | [118] | Monthuy-Blanc et al., a 2010 | France | Female sex = 100%; mean age 14.1 years; mean BMI 19.3 kg/m2 | Cross-sectional study | EDI-3 |
| 69 | [54] | Muros et al., b 2020 | Spain | Female sex = 15.5%; mean age 34.54 years; mean BMI 22.85 kg/m2 | Cross-sectional study | SCOFF |
| 70 | [43] | Neves et al., a 2017 | Brazil | Female sex = 100%; mean age 13.1 years; mean BMI NR Kg/m2 | Cohort study T1& T2 & T3 | EAT-26 |
| 71 | [119] | Nichols et al., 2006 | Multiple | Female sex = 100%; mean age 15.7 years; mean BMI 21.8 kg/m2 | Cross-sectional study | EDEQ |
| 72 | [120] | Nieves et al., 2016 | USA | Female sex = 100%; mean age 18.4 years; mean BMI 22.8 kg/m2 | Cohort study | EDI |
| 73 | [121] | O'Connell et al., 2024 | Canada | Female sex = 66.1%; mean age 20.1 years; mean BMI NR Kg/m2 | Cross-sectional study | DESA-6 |
| 74 | [122] | O'Connor et al., 1995 | Georgia | Female sex = 100%; mean age 19.8 years; mean BMI NR Kg/m2 | Cross-sectional study | EDI-2 |
| 75 | [42] | Okano et al., c 2004 | Multiple | Female sex = 100%; mean age 22 years; mean BMI 20.8 kg/m2 | Cross-sectional study | EAT-26 |
| 76 | [123] | O'Leary et al., b 2023 | UK | Female sex = 100%; mean age NR years; mean BMI NR Kg/m2 | Cross-sectional study |
M1 = BEDA-Q M2 = FAST |
| 77 | [124] | Pallotto et al., 2022 | USA | Female sex = 100%; mean age 19.9 years; mean BMI 22.4 kg/m2 | Cross-sectional study | EAT-26 |
| 78 | [125] | Peklaj et al., 2022 | Slovenia | Female sex = 51%; mean age 22 years; mean BMI 21.6 kg/m2 | Cross-sectional study | RD |
| 79 | [126] | Pensgaard et al., 2021 | Norway | Female sex = 40%; mean age 26.86 years; mean BMI NR Kg/m2 | Cross-sectional study | EDEQ |
| 80 | [127] | Pernick et al., 2006 | USA | Female sex = 100%; mean age 15.7 years; mean BMI NR Kg/m2 | Cross-sectional study | EDEQ |
| 81 | [15] | Petisco-Rodríguez et al., a 2020 | Spain | Female sex = 100%; mean age 17.29 years; mean BMI 20.59 kg/m2 | Cross-sectional study |
M1 = EAT-40 M2 = SCOFF |
| 82 | [128] | Petrie et al., 2009 | USA | Female sex = 100%; mean age 19.7 years; mean BMI 22.6 kg/m2 | Cross-sectional study | QEDD |
| 83 | [129] | Pettersen et al., c 2016 | Norway | Female sex = 100%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EDI-2 |
| 84 | [130] | Poucher et al., d 2022 | Canada | Female sex = 50%; mean age 22 years; mean BMI NR Kg/m2 | Cohort study | EAT-26 |
| 85 | [131] | Prather et al., 2016 | USA | Female sex = 100%; mean age 16.4 years; mean BMI 20.8 kg/m2 | Cross-sectional study | EAT-26 |
| 86 | [132] | Pritchett et al., 2021 | Multiple | Female sex = 50%; mean age 27 years; mean BMI NR Kg/m2 | Cross-sectional study | EDEQ |
| 87 | [133] | Rauh et al., 2010 | USA | Female sex = 100%; mean age 15.7 years; mean BMI 21.7 kg/m2 | Cohort study | EDEQ |
| 88 | [134] | Ravaldi et al., b 2003 | Italy | Female sex = 0%; mean age 19.6 years; mean BMI 22.1 kg/m2 | Cross-sectional study | EDE-12 |
| 89 | [135] | Ravi et al., 2021 | Finland | Female sex = 100%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | RD |
| 90 | [136] | Reinking and Alexander, b 2005 | USA | Female sex = 100%; mean age 19.8 years; mean BMI NR Kg/m2 | Cross-sectional study | EDI-2 |
| 91 | [137] | Reinking, 2006 | USA | Female sex = 100%; mean age 19.3 years; mean BMI 22.9 kg/m2 | Cohort study | FAST |
| 92 | [138] | Riebl et al., 2007 | USA | Female sex = 0%; mean age 31.6 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 93 | [52] | Robbeson et al., b 2015 | USA | Female sex = 100%; mean age 19 years; mean BMI 21.2 kg/m2 | Cross-sectional study | TFEQ |
| 94 | [139] | Roberts and Kreipe 2003 | USA | Female sex = 100%; mean age 14.9 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 95 | [55] | Rogers et al., 2021 | Australia | Female sex = 100%; mean age 19 years; mean BMI NR Kg/m2 | Cross-sectional study | SCOFF |
| 96 | [31] | Rosendahl et al., 2009 | German | Female sex = 36.5%; mean age 15.7 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 97 | [140] | Rousselet et al., 2017 | France | Female sex = 37.3%; mean age 16.8 years; mean BMI NR Kg/m2 | Cross-sectional study | EDI |
| 98 | [141] | Rouveix et al., 2007 | France | Female sex = 50%; mean age 22 years; mean BMI 21 kg/m2 | Cross-sectional study | EAT-26 |
| 99 | [142] | Schtscherbyna et al., a 2009 | Brazil | Female sex = 100%; mean age 14.6 years; mean BMI NR Kg/m2 | Cross-sectional study |
M1 = EAT-26 M2 = BITE M3 = BSQ |
| 100 | [143] | Sharps et al., a 2022 | UK | Female sex = 100%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | M1 = FAST |
| 101 | [144] | Smith et al., 2020 | Multiple | Female sex = 26.5%; mean age 20 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 102 | [145] | Sophia et al., 2022 | USA | Female sex = 100%; mean age 30.8 years; mean BMI 19.41 kg/m2 | Cross-sectional study | LEAF-Q |
| 103 | [146] | Staal et al., 2018 | Denmark | Female sex = 50%; mean age 24.8 years; mean BMI 20.2 kg/m2 | Cross-sectional study | EDI-3 |
| 104 | [147] | Stackeov et al., 2023 | Prague, Czechia | Female sex = 79%; mean age NR years; mean BMI NR Kg/m2 | Pilot study | EAT-26 |
| 105 | [148] | Sundgot-Borgen 1993 | Norway | Female sex = 100%; mean age 20.3 years; mean BMI 21.9 kg/m2 | Cross-sectional study | EDI |
| 106 | [149] | Sundgot-Borgen 1994 | Norway | Female sex = 100%; mean age 20 years; mean BMI 21 kg/m2 | Cross-sectional study | EDI |
| 107 | [150] | Sundgot-Borgen and Torstveit 2004 | Norway | Female sex = 93%; mean age 22.3 years; mean BMI 22.6 kg/m2 | Cross-sectional study | EDI |
| 108 | [151] | Sundgot‐Borgen et al., 2003 | Norway | Female sex = 100%; mean age 21.4 years; mean BMI NR Kg/m2 | Cross-sectional study | EDI |
| 109 | [152] | Syed et al., 2022 | Pakistan | Female sex = 100%; mean age 23.57 years; mean BMI 21.97 kg/m2 | Cross-sectional study | EAT-26 |
| 110 | [153] | Teixidor-Batlle et al., 2021 | Spain | Female sex = 51.08%; mean age 16.7 years; mean BMI 21.25 kg/m2 | Cross-sectional study | EAT-26 |
| 111 | [154] | Tenforde et al., 2022 | Multiple | Female sex = 40.7%; mean age 13.2 years; mean BMI 19.2 kg/m2 | Cross-sectional study | EDEQ |
| 112 | [155] | Terry et al., 1999 | UK | Female sex = 43%; mean age 23.9 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 113 | [156] | Thein-Nissenbaum et al., 2011 | USA | Female sex = 100%; mean age 15.4 years; mean BMI 21.1 kg/m2 | Cohort study | EDEQ |
| 114 | [157] | Thein-Nissenbaum et al., 2014 | USA | Female sex = 100%; mean age 15.3 years; mean BMI 21.1 kg/m2 | Cohort study | EDEQ |
| 115 | [158] | Thiel et al., 1993 | German | Female sex = 0%; mean age 21.1 years; mean BMI 21.05 kg/m2 | Cross-sectional study | EDI |
| 116 | [159] | Thompson 2007 | USA | Female sex = 19.6%; mean age 20.5 years; mean BMI NR Kg/m2 | Cross-sectional study | RD |
| 117 | [160] | Thompsonnet al., a 2017 | USA | Female sex = 100%; mean age 19.24 years; mean BMI 22.55 kg/m2 | Cohort study | QEDD |
| 118 | [161] | Torres-McGehee et al., 2009 | USA | Female sex = 100%; mean age 19.2 years; mean BMI 22.5 kg/m2 | Cross-sectional study | EAT-26 |
| 119 | [162] | Torres-McGehee et al., 2011 | USA | Female sex = 100%; mean age 19.88 years; mean BMI 22.6 kg/m2 | Cross-sectional study | EAT-26 |
| 120 | [163] | Torres-McGehee et al., 2023 | Columbia | Female sex = 69.3%; mean age 19.8 years; mean BMI 22.6 kg/m2 | Cross-sectional study | EAT-26 |
| 121 | [164] | Torstveit and Sundgot-Borgen 2005 | Norway | Female sex = 100%; mean age 21.3 years; mean BMI 21.6 kg/m2 | Cross-sectional study | EDI |
| 122 | [165] | Torstveit et al., 2008 | Norway | Female sex = 100%; mean age 22.2 years; mean BMI 21.7 kg/m2 | Cross-sectional study | EDI |
| 123 | [166] | Uriegas et al., a 2021 | USA | Female sex = 69%; mean age 19.6 years; mean BMI 23.6 kg/m2 | Cross-sectional study |
M1 = EAT-26 M2 = ORTO-15 |
| 124 | [167] | Uriegas et al., 2023 | Columbia | Female sex = 69.6%; mean age 19.8 years; mean BMI 22.5 kg/m2 | Cross-sectional study | EAT-26 |
| 125 | [168] | Vardar et al., 2005 | Turkey | Female sex = 100%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-40 |
| 126 | [169] | Vardar et al., 2007 | Turkey | Female sex = 100%; mean age 19 years; mean BMI 20 kg/m2 | Cross-sectional study | EAT-40 |
| 127 | [170] | Walberg and Johnston 1991 | USA | Female sex = 100%; mean age 22 years; mean BMI NR Kg/m2 | Cross-sectional study | EDI |
| 128 | [171] | Waryasz et al., 2020 | USA | Female sex = 100%; mean age 26.9 years; mean BMI NR Kg/m2 | Cross-sectional study | RD |
| 129 | [172] | Wheeler et al., 1986 | Canada | Female sex = 50%; mean age 33.6 years; mean BMI NR Kg/m2 | Cross-sectional study | EAT-26 |
| 130 | [29] | Whitehead et al., d 2020 | Australia | Female sex = 100%; mean age 32.9 years; mean BMI 22.9 kg/m2 | Cross-sectional study |
M1 = TFEQ M2 = EDI |
| 131 | [173] | Wollenberg et al., 2015 | USA | Female sex = 100%; mean age 19.5 years; mean BMI 22.1 kg/m2 | Cross-sectional study | EAT-26 |
| 132 | [174] | Wu et al., 2022 | Multiple | Female sex = 40.6%; mean age 13.2 years; mean BMI 19.1 kg/m2 | Cross-sectional study | EDEQ |
ANIS Anorexia Nervosa Inventory for Self-Rating, BEDS-7 Binge Eating Disorder Screener-7, DEBQ Dutch Eating Behavior Questionnaire, EAT-26 Eating Attitudes Test-26, EAT-40 Eating Attitudes Test-40, EDDS The Eating Disorder Diagnostic Scale, EDE-Q Eating Disorder Examination- Questionnaire, EDI Eating Disorder Inventory-I/II, FEDS feeding and eating disorders, ORTO-11 ORTO-11, ORTO-15 ORTO-15, QEDD Questionnaire for Eating Disorder Diagnoses, SCOFF Sick, Control, One Stone, Fat, Food, SD Self-developed, TFEQ The Three-Factor Eating Questionnaire, WCS The Weight Concern Scale
Data visualization and analysis (synthesis method)
With the understanding that the real effects will change over time, a traditional meta-analysis utilizing the random-effects approach was applied. We estimated and corrected for the between-study variation in effects using the DerSimonian-Laird technique and the generic inverse contrast technique with logit transformed (PLO) ratios. The random effect model was adopted (e.g., EAT and SCOFF; Table 1) since various study sets assess distinct, conceptually connected consequences using various metrics. Ninety-five percent confidence intervals, and pooled prevalence are presented for each study.
A forest plot was used to present the data. Forest plots have the limitation of only offering confidence intervals at significant levels, i.e., p < 0.05. Drapery plots and p-curve analysis were also used since confidence intervals are needed to ascertain whether results are significant and replicable. The p-value function is represented in the drapery plot by curves which stand for the forecast value from one study to the next, as well as for the combined meta-analytic values.
We employed the I2 statistic to estimate between-study variability; a result between 75 and 100% indicates a greater standard of heterogeneity. Additionally, we assessed heterogeneity using tau2 (τ2), tau (τ), as well as Cochran's Q statistics. The square root for the following is the H statistic: Cochran's χ2 heterogeneity statistic divided by the level of freedom. We utilized a standard Galbraith radial plot to illustrate heterogeneity, where the opposite of standard errors (horizontal axis) is shown in relation to the actual effect magnitude or results normalized with their corresponding standard errors (vertical axis). An arc displays matching effect sizes or outcomes just on the right side of an entire Galbraith plot.
Outlier inclusion could reduce the reliability and validity of meta-analysis. Studies are characterized as outliers whenever their confidence intervals do not match those of the pooled effects and sensitivity analysis can be used to address these studies. To avoid having an excessive amount of influence from any given study, we used a Jackknife sensitivity analysis to exclude studies one at a time. In this analysis, the primary meta-analysis is repeated one additional time for every study analyzed, with a different study being discarded every time.
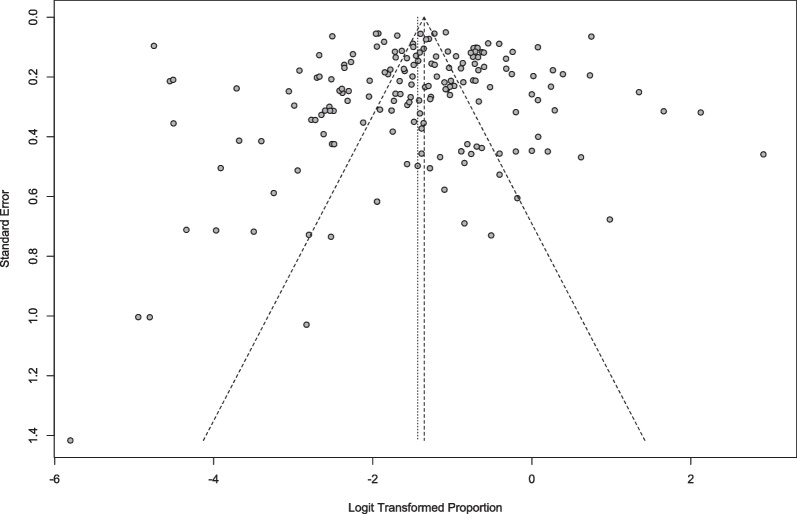
Publication bias can occur if, for instance, studies with positive results are published more often than studies with negative results. As a first visual, funnel plots were used to examine publication bias. The Doi plot replaces the traditional scatter plot (funnel plot) of the ratio of accuracy to efficiency with a plot of the ratio of the normal quantile (z-score) to efficiency [37]. If there is asymmetry, either the two ends of the graph are unequally offset from the midpoint, or one end has more trials than the other. If there is no asymmetry, a line drawn perpendicular to the x-axis from the top of the Doi graph is expected to divide the graph into two areas of equal area; the LFK index quantifies the difference between the two areas as the difference between their respective areas under the graph and the number of studies included at each edge; an LFK index closer to 0, the more symmetrical the Doi graph; LFK index values outside the range between -1 and + 1 are considered consistent with asymmetry (i.e., publication bias) [38]. The trim and fill method was applied (if needed) to develop modified point estimates. Peters' correlations and Egger’s regression also were employed as additional benchmarks for a more thorough analysis of publication bias.
Subgroup meta-analyses were utilized to look into varied results and respond to particular questions about various study characteristics or populations. Subgroup analyses were performed on categorical variables including participants’ nationality, culture (Western versus Eastern), and frequently included clinical characteristics. Sports energy system and sports category subgroup meta-analysis was performed to examine differences between aerobic, anaerobic, and mixed sports. Aerobic sports are defined as sports that require prolonged aerobic metabolism. This includes long-distance running, cycling, swimming, rowing, and cross-country skiing [39]. Anaerobic sports are defined as sports relying on anaerobic metabolism and involving short bursts of high-intensity activity such as sprinting, weightlifting, and gymnastics [39]. Mixed sports are defined as sports that involve both anaerobic and aerobic energy systems, e.g., soccer, basketball, tennis, volleyball, lacrosse, and hockey [39].
Any subgroup of four papers or more was addressed by the subgroup meta-analyses, and all findings were represented by graphical representation utilizing forest plots.
In essence, meta-regressions are essentially regression models where the outcomes of one or more explanatory factors have been used to forecast the amount of variance. Meta-regressions were conducted to examine associations between sample characteristics and SRDE prevalence estimates [40]. When an explanatory variable is raised by one unit in a meta-regression study, the regression coefficient shows how the output variable changes [40]. R2 was used to calculate the effect size in statistically significant meta-regression models, where 1–8%, 9–24%, and ≥ 25% of the variance corresponded to small, medium, and major effect size [40].
All data were analyzed using statistical computer software termed R. All classic meta-analyses were carried out using the packages "meta" and "metafor”. Risk-of-bias plotlines were produced for use in evaluating quality, using the package "robvis". An overview plot (weighted) was developed for all studies to indicate the amount of data contained within every judgment for each topic. A traffic light plot shows the total risk as well as the bias risk for each domain.
Results
Descriptive results
The literature search, ending 7th January 2024, yielded 4178 relevant studies. One hundred and thirty-two unique studies involving one hundred and seventy-seven studies (due to multiple screening tools or multiple data collection times) with a total sample size of 70,950 participants (K = 177 data points; N of participants = 70,950) met our inclusion and exclusion criteria. The details of those studies are shown in Table 1. The PRISMA2020 process flow for research selection is shown in Fig. 1.
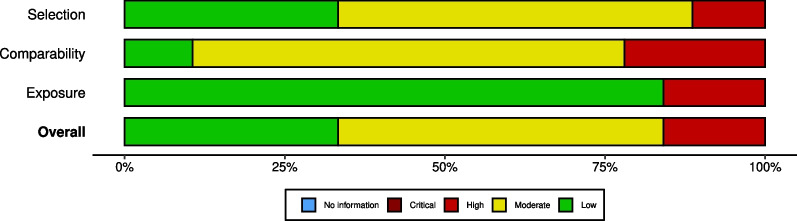
Twenty-seven countries were represented in our sample (Table 1), of which 92.1% were categorized as Western culture (33.3% were from the USA). Thirty percent of the studies addressed aerobic sports systems although most studies (59.9%) reported on sports that were mixed between aerobic and anaerobic exercise energy systems. Only 10.7% were purely anaerobic. Moreover, while 54.2% of the studies were of mixed indoor/outdoor sports, 26.5% were of purely outdoor sports. The EAT-26 was used in 31.1% of the studies (Table 2). A clear majority 88.1% of the studies were cross-sectional, while, in 11.9%, the design was longitudinal. None of the studies meeting the inclusion and exclusion criteria were conducted during the lockdown period of the COVID-19 pandemic. Figure 2 shows that approximately 80% of the studies were at low or moderate risk of bias. A detailed assessment of the risk of bias of each study is presented in Additional file 1.
Table 2.
Random and common effects meta-analysis models of the prevalence of disordered eating in Athletes
| Analysis | Descriptive | Random-effects meta-analysis | Common-effects meta-analysis | Visual Results | Heterogeneity | Moderators | Publication bias | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| K | N | Pooled results (95%CI) |
Pooled results (95%CI) |
Forest Plot | H | I2 | τ2 | τ | Q | p | Age | Sex | Egger's test | Rank test | |
| All Data | 177 | 70,957 | 19.23% [17.04; 21.62] | 20.52% [20.15; 20.89] | Figure 3 | 6.17 | 97.4% | 0.9 | 0.9 | 6699.62 | 0 | NS | NS | NS | NS |
|
By Country Turkey China Czech Republic German France UK Canada Spain Norway Australia Brazil Multi USA |
3 3 4 5 7 7 8 10 10 11 12 17 59 |
580 466 172 2879 711 6558 857 6066 3506 1005 1258 10,888 27,017 |
30.4% [9.1; 65.6] 51.4% [40.7; 61.9] 28.3% [20.3; 37.9] 13.9% [8.3; 22.4] 29.0% [21.5; 37.9] 18.7% [12.3; 28.0] 7.7% [3.5; 16.4] 12.8% [8.01; 19.7] 22.6% [15.2; 32.3] 57.1% [36.0; 75.8] 20.8% [13.7; 30.4] 10.9% [7.0; 16.6] 17.0% [12.9; 22.0] |
28.4% [24.4; 32.8] 48.7% [44.1; 53.2] 29.1% [22.7; 36.5] 16.3% [14.9; 17.8] 30.6% [27.2; 34.1] 14.0% [13.2; 14.9] 15.7%[12.6; 19.3] 20.0% [19.0; 21.1] 18.4% [17.1; 20.0] 39.1% [35.4; 42.9] 19.0% [16.7; 21.6] 11.2% [10.5; 12.0] 24.0% [23.2; 24.8] |
Additional file 9 | – |
98.0% 75.7% 22.2% 95.6% 76.0% 95.6% 89.0% 97.6% 95.8% 96.2% 86.6% 97.2% 98.2% |
1.7 0.1 0.05 0.4 0.2 0.3 1.2 0.6 0.6 2.0 0.6 1.0 1.5 |
1.3 0.3 0.2 0.6 0.4 0.5 1.1 0.8 0.8 1.4 0.8 1.0 1.2 |
101.8 8.2 3.9 91.0 25.0 137 63.7 377.1 215.9 265.0 82.3 577.8 3207.6 |
< 0.0001 | – | – | – | – |
|
By Culture Eastern Western |
14 163 |
1980 68,977 |
29.1% [20.1; 40.2] 18.5% [16.3; 20.9] |
33.6% [31.3; 35.9] 19.96% [19.95; 20.34] |
Additional file 10 | – |
97.4% 94.5% |
0. 9 0.8 |
0.9 0.9 |
6291.2 237.6 |
– | – | – | – | – |
|
By sports energy system Anaerobic Aerobic Both |
19 52 106 |
1828 16,287 52,842 |
37.9% [27.0; 50.2] 19.6% [15.2; 25.0] 17% [14.6; 19.4] |
38.3% [35.8; 40.9] 25.5% [24.7; 26.4 18.1% [17.7; 18.5] |
Additional file 11 | – |
93.9% 97.7% 97.2% |
1.1 1.2 0.7 |
1.0 1.1 0.8 |
297.3 2187.52 3684.5 |
– | – | – | – | – |
|
By sport category Swimming Martial arts Gymnastics Outdoor Mixed |
3 11 20 47 96 |
234 507 1680 29,195 39,341 |
20.2% [8.6; 40.6] 26.3% [18.1; 36.4] 41.5% [30.4; 53.6] 15.4% [11.6; 20.2] 17.6% [15.2; 20.4] |
25.2% [19.6; 31.7] 25.8% [21.8; 30.2] 40.9% [38.2; 43.6] 15.8% [16.2; 17.4] 21.3% [20.9; 21.8] |
Additional file 12 | – |
88.3% 76.6% 92.9% 98.0% 97.4% |
0.7 0.5 1.0 1.2 0.7 |
0.8 0.7 1.0 1.1 0.9 |
17.1 42.7 267.5 2154.3 3714.3 |
< 0.0001 | – | – | – | – |
|
By Measurement tool BITE TFEQ EAT–40 QEDD FAST EDI–2 EDI–3 SCOFF RD EDI EDEQ EAT–26 |
3 5 5 6 6 8 9 9 13 19 25 55 |
258 228 804 2336 4371 1034 968 6775 6398 4513 9145 27,055 |
12.2% [2.8; 40.3] 73.0% [60.1; 82.8] 18.6% [6.7; 42.1] 7.3% [2.9; 17.1] 22.0% [11.6; 37.7] 15.0% [10.5; 20.9] 34.0% [25.4; 43.9] 19.4% [13.9; 26.6] 14.8% [10.6; 20.2] 35.1% [27.2; 44.0] 15.1% [10.4; 21.3] 15.9% [12.4; 20.1] |
19.5% [13.6; 27.1] 75.4% [69.1; 80.7] 23.9% [20.6; 27.5] 16.9% [15.0; 19.0] 18.0% [16.8; 19.3] 13.5% [11.5; 15.9] 34.9% [31.9; 38.1] 21.1% [20.1; 22.2] 13.6% [12.8; 14.6] 25.1% [23.7; 26.5] 19.1% [18.0; 20.2] 19.0% [18.4; 19.7] |
Additional file 13 | – |
90.0% 65.7% 97.0% 97.4% 98.3% 71.5% 86.0% 97.3% 94.9% 95.6% 96.9% 97.4% |
1.7 0.3 1.7 1.4 0.9 0.2 0.3 0.3 0.4 0.6 1.1 1.0 |
1.3 0.5 1.3 1.2 0.9 0.5 0.6 0.6 0.6 0.8 1.0 1.0 |
20.0 11.7 135.0 194.8 292.5 24.5 57.0 292.5 233.8 408.3 778.7 2095.6 |
– | – | – | – | – |
|
By Design Cohort study Cross–sectional |
21 156 |
3419 67,538 |
22.2% [18.1; 27.0] 19.1% [16.8; 21.7] |
25.7% [24.1; 27.3] 20.1% [19.8; 20.7] |
Additional file 14 | – |
86.2% 97.6% |
0.3 0.9 |
0.5 1.0 |
145.2 6504 |
– | – | – | – | – |
K included studies numbers,
N included samples numbers
I2 Statistic refereed to the percentage of variation across samples due to heterogeneity rather than chance
τ2 Describe the extent of variation among the effects observed in different samples (between-sample variance)
H Describe confidence intervals of heterogeneity
dSignificant differences between samples in meta-analysis
eDetects publication bias in meta-analysis
fRepresent the correlation between effect sizes and sample variation
Fig. 2.
Summary risk of bias of the included studies
Meta-analysis of the prevalence of SRDE
Meta-analysis results and the raw prevalence data of each study are presented in Fig. 3. According to the random-effects meta-analysis, the SRDE prevalence among athletes (K = 177, N = 70,957) was (95% CI) = 19.23% (17.04%; 21.62%), I2 = (95% CI) = 97.4% (97.2%-97.6%),τ (95% CI) = 0.9481 (0.9374; 1.2182), τ2 = 0.8990 (0.8787–1.4840), H (95% CI) = 6.17 (5.95%-6.40%), p-value Cochran's Q = 0.00. Visual inspection of the funnel plot (Fig. 4), radial plot (Additional file 2), DOI plot (Additional file 3) as well as non-significant (at 0.05) Egger's regression and Peter's tests, indicated that the likelihood of publication bias was low. Additional file 4 represents the Drapery plot of DE in athletes; the drapery plot displays all primary study P-value functions in one graph, along with a P-value curve for each pooled estimate and a shaded prediction region. In contrast to the forest plot, the drapery plot displays results for any possible confidence level, not just one arbitrary confidence level. The results from our Drapery plot confirm that the results of the original/primary studies included are replicable. Additional file 5 presents possible outliers. The effect of outliers was minimal and required no accommodation.
Fig. 3.
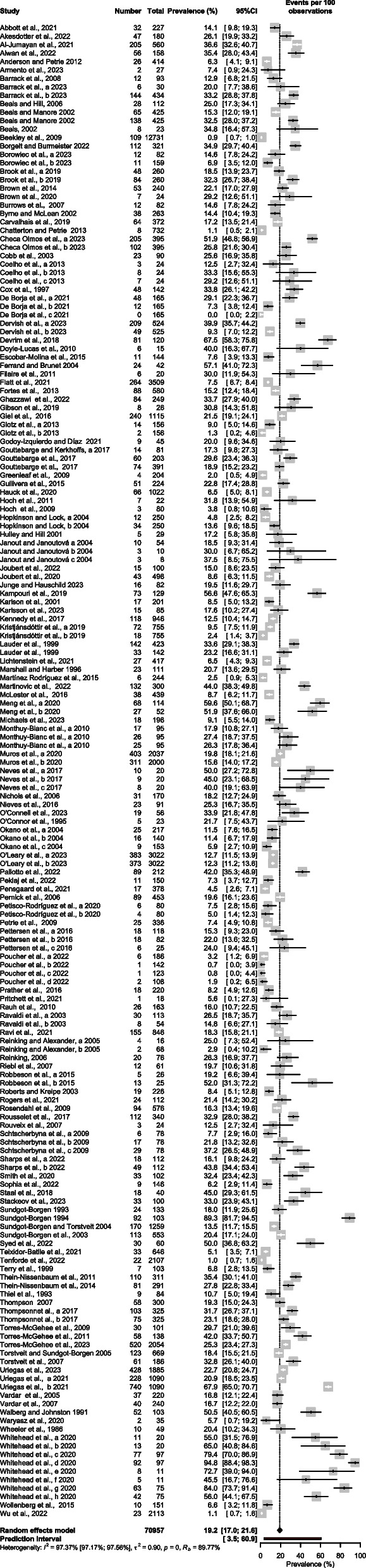
Meta-analysis of disordered eating in athletes
Fig. 4.
Funnel plot of disordered eating in athletes
Meta-regression and subgroup meta-analyses
Table 2 presents the analyses of subgroups, with the stipulation that there are at least three studies in a subgroup.
Age, BMI, and sex
Meta-regression analyses (Additional file 6, Additional file 7, and Additional file 8, respectively) demonstrate that age, BMI, and sex were statistically significant predictors/correlates, all p < 0.01. The effect sizes were very small: age R2 = ~ 0.00%; BMI R2 = ~ 4.5%; and sex R2 = 0.00%.
Country and culture
Additional file 9 and Additional file 10 show the weighted prevalence levels of SRDE as a function of the country and culture in which the data were collected. These varied substantially, and, as noted above, for many countries the number of studies meeting the inclusion and exclusion criteria was low. Australia (K = 11, N = 1,005) at 57.1% (36.0%- 75.8%) had the greatest prevalence of SRDE among athletes, followed by Greece (k = 1, N = 129) at 56.6% (47.9%-64.9%), followed by China (k = 3, N = 466) at 51.38% (40.7%-61.9%), then Pakistan (k = 1, N = 60) at 50% (37.6%-62.4%). The United States had the highest number of included studies (k = 59, N = 27,017). Nine countries had only one study and the results were distinctly divergent; Sweden reported SRDE of ~ 22.5%, Jordan 33.7%, Saudi Arabia 36.6%, New Zealand 30.8%, Portugal 17.2%, and Slovenia 7.3%.
As a group, Western countries (k = 163, N = 68,977) had a slightly lower prevalence of SRDE among athletes at 18.5% (16.3%-20.9%) than Eastern countries (k = 14, N = 1,980) at 29.1% (20.1%-40.2%), with statistically significant differences between East and West (p = 0.02).
Sports energy system and sports category
Additional file 11 shows the weighted prevalence levels of SRDE according to the energy system (aerobic vs anaerobic) of the sport. There were large variations. Most studies reported a mix of energy systems (k = 106, N = 52,842) with 17% (14.6%-19.4%). However, aerobic energy system sports were nearly three times more often reported on as anaerobic ones, (k = 52, N = 16,287) versus (k = 19, N = 1,828) respectively. Anaerobic sports had the highest prevalence rate of SRDE at 37.9% (27%-50.2%). Aerobic sports came next at 19.6% (15.2%-25%), while mixed sports showed the lowest prevalence rate of SRDE at 17% (14.6%-19.4%).
Results according to the sport were very similar, as shown in Additional file 12, which illustrates the fact that mixed sports were most commonly studied and swimming was the sport least studied, (k = 96, N = 39,341) versus (k = 3, N = 234). The martial arts (k = 11, N = 507) versus (k = 47, N = 29,195) for outdoor sports. Gymnastics had the highest prevalence rate of SRDE at 41.5% (30.4%-53.6%). Martial arts had the next highest prevalence rate of SRDE at 26.3% (18.1%-36.4%), while outdoor sports had the lowest prevalence rate of SRDE at 15.6% (11.6%-20.2%).
Measures of SRDE
Meta-analysis showed significant heterogeneity amongst the measurement tools used in the studies (Table 2, Additional file 13) I2 = 97.4%, τ2 = 0.8990, p = 0.00. Of all 22 measures, the TFEQ = Three-Factor Eating Questionnaire (k = 5, N = 228) produced the highest prevalence at 73% (60.1; 82.8%), while the QEDD or Questionnaire for Eating Disorder Diagnoses (k = 6, N = 2,336) yielded the lowest prevalence at 7.3% (2.9%-17.1%). The main measure used, the EAT-26, yielded a prevalence of 15.9% (12.4%; 20.1%), (k = 55, N = 27,055).
Seven tools were used only once (k = 1); the Leisuretime Exercise and Anorexia Nervosa Questionnaire (LEAF-Q) (N = 146), the Bulimia Test Revised (BULIT-R) (N = 755), the Eating Disorder Diagnostic Scale (EDDS) (N = 1022), the Eating Disorder Screen for Primary Care (ESP) (N = 165), the Disordered Eating Screen for Athletes (DESA-6) (N = 56), the Structured Inventory for Anorexic, the Bulimic Syndromes (SIAB-S) (N = 82) and Female Athlete Screening Tool (N = 4371).
Study design
Almost one-fifth of studies (k = 156) were cross-sectional involving (N = 67,538) participants. Only 21 studies were cohort studies, with 3,419 participants. The prevalence of SRDE in cohort studies was 22.2% (18.1%-27%), as shown in Additional file 14.
Discussion
The purpose of this meta-analysis was to estimate the prevalence of DE in athletes, based on published studies that used validated screening measures. The search and selection process resulted in 177 studies, conducted in 27 countries (total N of participants = 70,957). This meta-analysis indicates an estimate of CI 95% = 19.23% (17.0%-21.6%) as the global prevalence of SRDE in athletes. This is higher than in the general population [20]. Given the physical and mental health consequences of DE and considering its status as a risk factor for clinically significant EDs, the prevalence rates are considered high [20].
The most frequently associated with SRDE was competing in gymnastics and sports divided along weight lines [20, 41–43]. With advance knowledge of risk, health care professionals are better equipped to provide early treatment when required [17, 44]. In general practice, this knowledge paired with an ongoing patient-provider trusting relationship, puts the physician in a unique position to diagnose and treat SRDE, thus preventing progression to an ED [23]. Knowledge about risk factors is also important for health promotion and targeted preventive measures. Results of this research are recommended reading for athletes as well as trainers, coaches, physicians, Olympic committees and administrators of athletic organizations [28, 45–47].
The prevalence estimate of 19% was, significantly associates with age, the proportion of females in the sample, and sample's mean BMI level. The prevalence of SRDE was higher in Eastern countries. Of interest to Arab countries, the prevalence of SRDE in athletes was only available in two Arabic countries: 36.6% among Saudi athletes [48] and, in Jordan 33.7% [20].
Since self-screening leads to early risk identification and effective prevention, it will be important to survey self-identified DE and examine its history and symptom patterns in more detail [49]. In a recent study of 249 Jordanian athletes aged over 18 years, Ghazzawi et al. [20] found an overall prevalence of SRDE of 33.7%, which is far higher than the mean estimate of 19.23% in our meta-analysis. In the Ghazzawi et al., 2022 study, outdoor sports (running, cycling, and walking), relevant to 8% of the participants, showed the lowest percentage of DE (3% of the 34%); the highest percentage (10% out of the 34%) was among gymnasts who accounted for 30% of all participants[20].
More studies, using established epidemiological methods (e.g., representative sampling), are needed to clarify the prevalence and correlates of SRDE in athletes. In this regard, the published research to date has been limited to samples from only 27 countries, that is about 10% of the world's approximately 250 independent territorial entities. Notably absent in the literature that met our criteria are studies from Latin American countries (other than one from Brazil), and there is either zero or one sole study from several countries that have contributed to the general literature on DE, such as Sweden, New Zealand, Portugal, Slovenia and the Middle East countries (other than Saudi Arabia and Jordan).
Researchers seeking to understand the prevalence of DE as a multifaceted construct have many screening tools from which to choose (Table 1). Based on the substantial variability (heterogeneity) of the prevalence estimates in our meta-analysis, and in order to facilitate comparisons across studies from different countries while avoiding estimates that are almost certainly far too high or too low, we recommend the standardized use of the EAT-26 [50] plus the TFEQ [51].
The EAT-26 has been extensively validated across ages, sex groups, and cultural contexts as a screening tool with strong psychometric properties for identifying DE attitudes and behaviors [50]. The TFEQ thoroughly assesses different problematic eating patterns such as restrained-, and emotional- eating that may represent risk factors for the development of EDs [29, 52]. Together, these two instruments capture a comprehensive range of symptoms and eating behavior anomalies indicative of risk. The self-report format makes them possible to use for large population screenings where clinician interviews are impractical. Furthermore, both questionnaires have been translated and validated in various languages, enabling consistent implementation globally [29, 52]. Standardizing to widely-used instruments like the EAT-26 and TFEQ with robust psychometric properties that comprehensively assesses DE will help generate prevalence estimates across studies that are more homogeneous, allowing for meaningful cross-national comparisons and meta-analytic examination [29, 52].
The TFEQ, which was used in five data points [29, 52] included in this meta-analysis, is a valid and widely used measure of ED behaviors, and, therefore, it can add behavioral information to the screening items included in the EAT-26. If the EAT-26 is impractical due to its length, then we recommend substituting the 5-item SCOFF, which, according to Table 1, has thus far been used in only seven studies of SRDE in athletes [15, 53–56].
TFEQ has been previously used in studies samples that included athletes, its psychometric properties and validity have not yet been investigated specifically in athletic populations, representing an important direction for further research [51].
Furthermore, the hormonal and metabolic dysregulation of DE can negatively impact athletic performance in various ways. Decreased estrogen and testosterone levels hinder the building and maintenance of muscle mass [11, 57]. Reduced IGF-1 and growth hormone lead to impaired bone development, and increased fracture risk [11, 57, 58]. Electrolyte abnormalities from purging behaviors can disrupt cardiac function [57, 58]. Low energy availability alters substrate metabolism, making it difficult to meet energy demands during training and competition [11, 57]. Extreme weight loss and nutritional deficiencies can also impede recovery after exercise [11, 57, 58].
Study strengths and limitations
To the best of our knowledge, this is the first meta-analysis of the prevalence of SRDE among athletes. The substantial number of studies and participants included adds strength to this review. Limitations include the reliance of many studies on convenience samples rather than representative samples and our inability to review articles published in languages other than English. The limited nature of the information about participants also ruled out statistical examination of potentially important moderating variables such as ethnicity, immigration status, sexual orientation, and family history.
An additional limitation of our analysis stems from the small number of studies conducted in Eastern countries, as well as our ability to examine differences among countries solely along the Western vs. Eastern dichotomy. The small sample of studies from Eastern nations limits conclusions about the seemingly high prevalence rates found in these settings. Furthermore, grouping diverse countries into binary Western and Eastern categories obscures important heterogeneity within regions in terms of specific sociocultural factors influencing DE. Future research should include more studies across a wider range of Eastern countries and examine country-level differences using more nuanced categorization systems. Relatedly, our study was limited by its focus on the gender binary, when DE prevalence among transgender and nonbinary populations warrants dedicated investigation.
To maximize the breadth of the literature captured, we did manually search the reference lists of included studies to help identify any relevant articles that our search may have missed. However, we acknowledge that it is possible we may have inadvertently excluded some studies by not including a wider range of activity-specific terms in the database searches. For future updates to this meta-analysis, we will consider broadening the search to include additional keywords related to different sports, as well as other physical activities such as dance, mountain climbing, boating, and others.
Conclusion
The prevalence of SRDE in a meta-analysis of a very large sample of athletes from 27 countries was shown to be 19.23%, or one in every five athletes. DE is a health problem in itself, but it is also a strong risk factor for EDs. Our meta-analysis strongly suggests that, in the sports world, it affects females and males to an equal degree. While concentrating on sports injuries, public health has neglected the nutritional needs of athletes and the health consequences of dietary deficiencies in persons with high energy expenditure.
Supplementary Information
Additional file 1 Traffic light of the included studies.
Additional file 2 Radial plot of disordered eating in athletes.
Additional file 3 DOI plot of disordered eating in athletes.
Additional file 4 Drapery plot of disordered eating in athletes.
Additional file 6 Meta-regression of disordered eating in athletes by Age.
Additional file 7 Meta-regression of disordered eating in athletes by BMI.
Additional file 8 Meta-regression of disordered eating in athletes by Sex (%Female Sex).
Additional file 9 Subgroup meta-analysis by country.
Additional file 10 Subgroup meta-analysis by culture.
Additional file 11 Subgroup meta-analysis by the sports energy system .
Additional file 12 Subgroup meta-analysis by sports category.
Additional file 13 Subgroup meta-analysis by disordered eating measurement tool.
Additional file 14 Subgroup meta-analysis by study design.
Author contributions
Conceptualization, HJ, and HG; Methodology, HJ; Software, HJ; Formal Analysis, HJ; Writing – Original Draft Preparation, HG, AH, HT and LN; Writing – Review & Editing, HG, LN, AA, OA, SRP, KT, MVS, and HJ; Funding Acquisition, not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
Data is available in Table 1.
Declarations
Ethics approval and consent to participate
Not applicable. This is a systematic review and meta-analysis of published studies that are indexed in the public domain. This is a systematic review and meta-analysis of published studies that are indexed in the public domain. All authors have seen and approved the manuscript.
Consent for publication
Not applicable. This is a systematic review and meta-analysis of published studies that are indexed in the public domain.
Competing interests
All authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Giel KE, Hermann-Werner A, Mayer J, Diehl K, Schneider S, Thiel A, et al. Eating disorder pathology in elite adolescent athletes. Int J Eat Disord. 2016;49:553–562. doi: 10.1002/eat.22511. [DOI] [PubMed] [Google Scholar]
- 2.Levine MP, Smolak L. The prevention of eating problems and eating disorders: theories, research, and applications. Routledge; 2020.
- 3.Kutz AM, Marsh AG, Gunderson CG, Maguen S, Masheb RM. Eating disorder screening: a systematic review and meta-analysis of diagnostic test characteristics of the SCOFF. J Gen Intern Med. 2020;35:885–893. doi: 10.1007/s11606-019-05478-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Culbert KM, Racine SE, Klump KL. Research Review: What we have learned about the causes of eating disorders: a synthesis of sociocultural, psychological, and biological research. J Child Psychol Psychiatry. 2015;56:1141–1164. doi: 10.1111/jcpp.12441. [DOI] [PubMed] [Google Scholar]
- 5.Alhaj OA, Fekih-Romdhane F, Sweidan DH, Saif Z, Khudhair MF, Ghazzawi H, et al. The prevalence and risk factors of screen-based disordered eating among university students: a global systematic review, meta-analysis, and meta-regression. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity. 2022. 10.1007/s40519-022-01452-0. [DOI] [PMC free article] [PubMed]
- 6.Fekih-Romdhane F, Daher-Nashif S, Amthal ·, Alhuwailah H, Haifa ·, Saleh M, et al. The prevalence of feeding and eating disorders symptomology in medical students: an updated systematic review, meta-analysis, and meta-regression. 2022;27:1991–2010 [DOI] [PMC free article] [PubMed]
- 7.Esmaeil Mousavi Asl, Behzad Mahaki, Yousef Asmari Bardezard, Youkhabeh Mohammadian. Eating Disorders Screening Tools: The Psychometric Properties of the Persian version of Eating Attitude Test. 2020. 10.4103/ijpvm.IJPVM_355_19. [DOI] [PMC free article] [PubMed]
- 8.Azhar Shah S, Safian N. Eating disorder screening tools for athletes: A systematic review of literature focusing on scales developed in the last 10 years (2011–2021). 2022. 10.1080/19357397.2022.2095179.
- 9.Sander W. Measures of Information. Handbook of Measure Theory. 2002;:1523–65.
- 10.Mathisen TF, Hay P, Bratland-Sanda S. How to address physical activity and exercise during treatment from eating disorders: a scoping review. Curr Opin Psychiatry. 2023;36:427–437. doi: 10.1097/YCO.0000000000000892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quesnel D, Disorders MC-… E, 2023 undefined. Medical and physiological complications of exercise for individuals with an eating disorder: A narrative review. jeatdisord.biomedcentral.com. [DOI] [PMC free article] [PubMed]
- 12.Cisneros A, Quesnel DA, Robert-McComb JJ. A modern understanding of the models of energy deficits in athletes. In: The Active Female: Health Issues throughout the Lifespan. 2023.
- 13.Foster L, Lundh LG, Daukantaité D. Disordered eating in a 10-year perspective from adolescence to young adulthood: Stability, change, and body dissatisfaction as a predictor. Scand J Psychol. 2023 doi: 10.1111/sjop.12950. [DOI] [PubMed] [Google Scholar]
- 14.Gusfa OMS-IV D, Mancine OMS-IV R, Kennedy S do, Bashir DA, Saffarian M do. The relationship between disordered eating behaviors and injury rates in adolescent athletes. 2021. 10.1002/eat.23642. [DOI] [PubMed]
- 15.Petisco-Rodríguez C, Sánchez-Sánchez LC, Fernández-García R, Sánchez-Sánchez J, García-Montes JM. Disordered eating attitudes, anxiety, self-esteem and perfectionism in young athletes and non-athletes. Int J Environ Res Public Health. 2020;17:1–18. doi: 10.3390/ijerph17186754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berger U, Wick K, Hölling H, Schlack R, Bormann B, Brix C, et al. Screening of disordered eating in 12 year old girls and boys: Psychometric analysis of the German versions of SCOFF and EAT-26. European Psychiatry. 2011;26. [DOI] [PubMed]
- 17.Neumark-Sztainer D, Levine M, Paxton S, Smolak L, Piran N, Wertheim E. Prevention of body dissatisfaction and disordered eating: What next? Eat Disord. 2006;14:265–285. doi: 10.1080/10640260600796184. [DOI] [PubMed] [Google Scholar]
- 18.Smolak L, Levine MP. The Wiley handbook of eating disorders. John Wiley & Sons; 2015.
- 19.Eichstadt M, Luzier J, Cho D, Weisenmuller C. Eating Disorders in Male Athletes. 2020 doi: 10.1177/1941738120928991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghazzawi HA, Alhaj OA, Nemer LS, Amawi AT, Trabelsi K, Jahrami HA. The Prevalence of “at Risk” Eating Disorders among Athletes in Jordan. Sports. 2022;10:182. doi: 10.3390/sports10110182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smolak L, Murnen SK, Ruble AE. Female athletes and eating problems: a meta-analysis. Int J Eat Disord. 2000;27:371–380. doi: 10.1002/(SICI)1098-108X(200005)27:4<371::AID-EAT1>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 22.Fortes L de SDS, Kakeshita IS, Almeida SS, Gomes AR, Ferreira MECC. Eating behaviours in youths: A comparison between female and male athletes and non-athletes. 2014;24:e62–8. [DOI] [PubMed]
- 23.Mancine RP, Gusfa DW, Moshrefi A, Kennedy SF. Prevalence of disordered eating in athletes categorized by emphasis on leanness and activity type - A systematic review. Journal of Eating Disorders. 2020;8. [DOI] [PMC free article] [PubMed]
- 24.de Bruin APK, Oudejans RRD. Athletes’ body talk: The role of contextual body image in eating disorders as seen through the eyes of elite women athletes. J Clin Sport Psychol. 2018;12:675–698. doi: 10.1123/jcsp.2018-0047. [DOI] [Google Scholar]
- 25.van de Schoot R, de Bruin J, Schram R, Zahedi P, de Boer J, Weijdema F, et al. An open source machine learning framework for efficient and transparent systematic reviews. Nat Mach Intell. 10.1038/s42256-020-00287-7.
- 26.Byrne S, Mclean N. Eating disorders in athletes: a review of the literature. [DOI] [PubMed]
- 27.Ghazzawi HA, Hussain MA, Raziq KM, Alsendi KK, Alaamer RO, Jaradat M, et al. Exploring the Relationship between Micronutrients and Athletic Performance: A Comprehensive Scientific Systematic Review of the Literature in Sports Medicine. Sports. 2023;11. [DOI] [PMC free article] [PubMed]
- 28.Bergeron MF, Mountjoy M, Armstrong N, Chia M, Côté J, Emery CA, et al. International Olympic Committee consensus statement on youth athletic development. Br J Sports Med. 2015;49:843–851. doi: 10.1136/bjsports-2015-094962. [DOI] [PubMed] [Google Scholar]
- 29.Whitehead J, Slater G, Wright H, Martin L, O’Connor H, Mitchell L. Disordered eating behaviours in female physique athletes. Eur J Sport Sci. 2020;20:1206–1214. doi: 10.1080/17461391.2019.1698659. [DOI] [PubMed] [Google Scholar]
- 30.Michou M, Costarelli V. Perceived stress in relation to socioeconomic and lifestyle characteristics in Greece: a cross-sectional study. Int J Home Econ. 2021;14:108–115. [Google Scholar]
- 31.Rosendahl J, Bormann B, Aschenbrenner K, Aschenbrenner F, Strauss B. Dieting and disordered eating in German high school athletes and non-athletes. Scand J Med Sci Sports. 2009;19:731–739. doi: 10.1111/j.1600-0838.2008.00821.x. [DOI] [PubMed] [Google Scholar]
- 32.Chapa DAN, Johnson SN, Richson BN, Bjorlie K, Won YQ, Nelson S V., et al. Eating-disorder psychopathology in female athletes and non-athletes: a meta-analysis. International Journal of Eating Disorders. 2022;55. [DOI] [PMC free article] [PubMed]
- 33.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. Syst Rev. 2020;2021:10. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Consensus Statement International Olympic Committee Consensus Statement Methods for Recording and Reporting of Epidemiological Data on Injury and Illness in Sports 2020 (Including the STROBE Extension for Sports Injury and Illness Surveillance (STROBE-SIIS)) International Olympic Committee Injury and Illness Epidemiology Consensus Group* †. 10.1177/2325967120902908. [DOI] [PMC free article] [PubMed]
- 35.Regional groups of Member States | Department for General Assembly and Conference Management. https://www.un.org/dgacm/en/content/regional-groups. Accessed 3 Jan 2024.
- 36.Wells G, Shea B, O’Connell D, Peterson J. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, ON: Ottawa Hospital Research Institute. 2000.
- 37.Doi SA. Rendering the Doi plot properly in meta-analysis. Int J Evid Based Healthc. 2018;16:242–243. doi: 10.1097/XEB.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 38.Furuya-Kanamori L, Barendregt JJ, Doi SAR. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int J Evid Based Healthc. 2018;16:195–203. doi: 10.1097/XEB.0000000000000141. [DOI] [PubMed] [Google Scholar]
- 39.Chamari K, Padulo J. ‘Aerobic’ and ‘Anaerobic’ terms used in exercise physiology: a critical terminology reflection. Sports Med Open. 2015;1. [DOI] [PMC free article] [PubMed]
- 40.Thompson SG, Higgins JPT. How should meta-regression analyses be undertaken and interpreted? Stat Med. 2002;21. [DOI] [PubMed]
- 41.Karrer Y, Halioua R, Mötteli S, Iff S, Seifritz E, Jäger M, et al. Disordered eating and eating disorders in male elite athletes: A scoping review. BMJ Open Sport and Exercise Medicine. 2020;6. [DOI] [PMC free article] [PubMed]
- 42.Okano G, Holmes RA, Mu Z, Yang P, Lin Z, Nakai Y. Disordered eating in Japanese and Chinese female runners, rhythmic gymnasts and gymnasts. Int J Sports Med. 2005;26:486–491. doi: 10.1055/s-2004-821058. [DOI] [PubMed] [Google Scholar]
- 43.Neves CM, Filgueiras Meireles JF, Berbert de Carvalho PH, Schubring A, Barker-Ruchti N, Caputo Ferreira ME. Body dissatisfaction in women’s artistic gymnastics: a longitudinal study of psychosocial indicators. J Sports Sci. 2017;35:1745–51. [DOI] [PubMed]
- 44.Köse G, Tayfur M, Karayigit R. BMI, Physical activity, sleep quality, eating attitudes, emotions: which one is affected by mindful eating? Progress in Nutrition. 2021;23.
- 45.Mountjoy M, Sundgot-Borgen J, Burke L, Ackerman KE, Blauwet C, Constantini N, et al. International Olympic Committee (IOC) Consensus statement on relative energy deficiency in sport (red-s): 2018 update. Int J Sport Nutr Exerc Metab. 2018;28:316–331. doi: 10.1123/ijsnem.2018-0136. [DOI] [PubMed] [Google Scholar]
- 46.Åkesdotter C, Kenttä G, Eloranta S, Håkansson A, Franck J. Prevalence and comorbidity of psychiatric disorders among treatment-seeking elite athletes and high-performance coaches. BMJ Open Sport Exerc Med. 2022;8:e001264. doi: 10.1136/bmjsem-2021-001264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brown KN, Wengreen HJ, Beals KA. Knowledge of the female athlete triad, and prevalence of triad risk factors among female high school athletes and their coaches. J Pediatr Adolesc Gynecol. 2014;27:278–282. doi: 10.1016/j.jpag.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 48.Al-Jumayan AA, Al-Eid NA, AlShamlan NA, AlOmar RS. Prevalence and associated factors of eating disorders in patrons of sport centers in Saudi Arabia. J Family Community Med. 2021;28:94–102. doi: 10.4103/jfcm.jfcm_113_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Breton É, Dufour R, Côté SM, Dubois L, Vitaro F, Boivin M, et al. Developmental trajectories of eating disorder symptoms: A longitudinal study from early adolescence to young adulthood. J Eat Disord. 2022;10. [DOI] [PMC free article] [PubMed]
- 50.Peláez-Fernández MA, Ruiz-Lázaro PM, Labrador FJ, Raich RM. Validación del Eating Attitudes Test como instrumento de cribado de trastornos de la conducta alimentaria en población general. Med Clin (Barc) 2014;142:153–155. doi: 10.1016/j.medcli.2013.03.018. [DOI] [PubMed] [Google Scholar]
- 51.Stice E, Telch CF, Rizvi SL. Erratum: Development and validation of the eating disorder diagnostic scale. A brief self-report measure of anorexia, bulimia, and binge-eating disorder (Psychological Assessment (2000) 12:2 (123-131)). Psychological Assessment. 2000;12. [DOI] [PubMed]
- 52.Robbeson JG, Kruger HS, Wright HH. Disordered eating behavior, body image, and energy status of female student dancers. Int J Sport Nutr Exerc Metab. 2015;25:344–352. doi: 10.1123/ijsnem.2013-0161. [DOI] [PubMed] [Google Scholar]
- 53.Gulliver A, Griffiths KM, Mackinnon A, Batterham PJ, Stanimirovic R. The mental health of Australian elite athletes. J Sci Med Sport. 2015;18:255–261. doi: 10.1016/j.jsams.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 54.Muros JJ, Ávila-Alche Á, Knox E, Zabala M. Likelihood of suffering from an eating disorder in a sample of Spanish cyclists and triathletes. J Eat Disord. 2020;8. [DOI] [PMC free article] [PubMed]
- 55.Rogers MA, Appaneal RN, Hughes D, Vlahovich N, Waddington G, Burke LM, et al. Prevalence of impaired physiological function consistent with relative energy deficiency in Sport (RED-S): an Australian elite and pre-elite cohort. Br J Sports Med. 2021;55:38–45. doi: 10.1136/bjsports-2019-101517. [DOI] [PubMed] [Google Scholar]
- 56.Lichtenstein MB, Melin AK, Szabo A, Holm L. The Prevalence of exercise addiction symptoms in a sample of national level elite athletes. Front Sports Act Living. 2021;3. [DOI] [PMC free article] [PubMed]
- 57.Kontele I, Children TV-, 2021 undefined. Nutritional risks among adolescent athletes with disordered eating. mdpi.com. 2010. 10.3390/children8080715. [DOI] [PMC free article] [PubMed]
- 58.Dipla K, Kraemer RR, Constantini NW, Hackney AC. Relative energy deficiency in sports (RED-S): elucidation of endocrine changes affecting the health of males and females. Hormones. 2021;20:35–47. doi: 10.1007/s42000-020-00214-w. [DOI] [PubMed] [Google Scholar]
- 59.Abbott W, Brett A, Brownlee TE, Hammond KM, Harper LD, Naughton RJ, et al. The prevalence of disordered eating in elite male and female soccer players. Eat Weight Disord. 2021;26:491–498. doi: 10.1007/s40519-020-00872-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Alwan N, Moss SL, Davies IG, Elliott-Sale KJ, Enright K. Weight loss practices and eating behaviours among female physique athletes: Acquiring the optimal body composition for competition. PLoS ONE. 2022;17:1. doi: 10.1371/journal.pone.0262514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anderson C, Petrie TA. Prevalence of disordered eating and pathogenic weight control behaviors among NCAA division I female collegiate gymnasts and swimmers. Res Q Exerc Sport. 2012;83:120–124. doi: 10.1080/02701367.2012.10599833. [DOI] [PubMed] [Google Scholar]
- 62.Armento AM, VanBaak KD, Seehusen CN, Howell DR. Differences in Training and Health Characteristics Between Trail Ultrarunners and Shorter Distance Runners. Wilderness Environ Med. 2023;34:182–186. doi: 10.1016/j.wem.2022.12.002. [DOI] [PubMed] [Google Scholar]
- 63.Barrack MT, Rauh MJ, Barkai H-S, Nichols JF. Dietary restraint and low bone mass in female adolescent endurance runners 1–3. 2008. [DOI] [PubMed]
- 64.Barrack MT, Domino S, Gray VB, Cotter JA, Rauh MJ, Nichols JF. Support for inadvertent undereating in female adolescent athletes with clinical indicators of low energy availability. J Sci Med Sport. 2023;26:285–290. doi: 10.1016/j.jsams.2023.04.003. [DOI] [PubMed] [Google Scholar]
- 65.Beals KA, Hill AK. The prevalence of disordered eating, menstrual dysfunction, and low bone mineral density among US Collegiate Athletes. 2006. [DOI] [PubMed]
- 66.Beals KA, Beals KA, Manore MM. Disorders of the Female Athlete Triad / 281 Disorders of the Female Athlete Triad Among Collegiate Athletes. 2002. [DOI] [PubMed]
- 67.Katherin A. Beals. Eating Behaviors, nutritional status, and menstrual function in elite female adolescent volleyball players. [DOI] [PubMed]
- 68.Matthew D. Beekley, Robert Byrne, Trudy Yavorek, Kelli Kidd, Janet Wolff, Michael Johnson. Incidence, prevalence, and risk of eating disorder behaviors in military academy cadets. [DOI] [PubMed]
- 69.Borgelt S, Burmeister JM. Disordered eating in collegiate English equestrian athletes in aesthetic and nonaesthetic disciplines. Eat Behav. 2022;46. [DOI] [PubMed]
- 70.Borowiec J, Banio-Krajnik A, Malchrowicz-Mośko E, Kantanista A. Eating disorder risk in adolescent and adult female athletes: the role of body satisfaction, sport type, BMI, level of competition, and training background. BMC Sports Sci Med Rehabil. 2023;15. [DOI] [PMC free article] [PubMed]
- 71.Brook EM, Tenforde AS, Broad EM, Matzkin EG, Yang HY, Collins JE, et al. Low energy availability, menstrual dysfunction, and impaired bone health: A survey of elite para athletes. Scand J Med Sci Sports. 2019;29:678–685. doi: 10.1111/sms.13385. [DOI] [PubMed] [Google Scholar]
- 72.Brown K, Yates M, Meenan M, Brown AF. Increased female athlete triad knowledge among collegiate dancers following a brief educational video intervention. J Dance Med Sci. 2020;24:161–167. doi: 10.12678/1089-313X.24.4.161. [DOI] [PubMed] [Google Scholar]
- 73.Burrows M, Shepherd H, Bird S, Macleod K, Ward B. The components of the female athlete triad do not identify all physically active females at risk. J Sports Sci. 2007;25:1289–1297. doi: 10.1080/02640410601129714. [DOI] [PubMed] [Google Scholar]
- 74.Byrne S, Mclean N. Elite Athletes: Effects of the pressure to be thin. [DOI] [PubMed]
- 75.Carvalhais A, Araújo J, Natal Jorge R, Bø K. Urinary incontinence and disordered eating in female elite athletes. J Sci Med Sport. 2019;22:140–144. doi: 10.1016/j.jsams.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 76.Chatterton JM, Petrie TA. Prevalence of disordered eating and pathogenic weight control behaviors among male collegiate athletes. Eat Disord. 2013;21:328–341. doi: 10.1080/10640266.2013.797822. [DOI] [PubMed] [Google Scholar]
- 77.Checa Olmos JC, Monserrat Hernández M, Belmonte García T, Jiménez Rodríguez D, Rodríguez Martínez A, Berenguel Martínez P, et al. Social and individual factors associated with eating disorders in young athletes: effects on concentration and fatigue. Sports. 2023;11. [DOI] [PMC free article] [PubMed]
- 78.Cobb KL, Bachrach LK, Greendale G, Marcus R, Neer RM, Nieves J, et al. Disordered eating, menstrual irregularity, and bone mineral density in female runners. Med Sci Sports Exerc. 2003;35:711–719. doi: 10.1249/01.MSS.0000064935.68277.E7. [DOI] [PubMed] [Google Scholar]
- 79.Coelho GM de O, Farias MLF de, Mendonça LMC de, Mello DB de, Lanzillotti HS, Ribeiro BG, et al. The prevalence of disordered eating and possible health consequences in adolescent female tennis players from Rio de Janeiro, Brazil. Appetite. 2013;64:39–47. [DOI] [PubMed]
- 80.Lori Cox, Chrisopher Lantz, Jerry Mayhew. The role of social physique anxiety and other variables in predicting eating behaviors in college students. [DOI] [PubMed]
- 81.de Borja C, Holtzman B, McCall LM, Carson TL, Moretti LJ, Farnsworth N, et al. Specific dietary practices in female athletes and their association with positive screening for disordered eating. J Eat Disord. 2021;9:1. doi: 10.1186/s40337-021-00407-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dervish RA, Wilson LJ, Curtis C. Investigating the prevalence of low energy availability, disordered eating and eating disorders in competitive and recreational female endurance run. Eur J Sport Sci. 2023;23:869–876. doi: 10.1080/17461391.2022.2079423. [DOI] [PubMed] [Google Scholar]
- 83.Devrim A, Bilgic P, Hongu N. Is there any relationship between body image perception, eating disorders, and muscle dysmorphic disorders in male bodybuilders? Am J Mens Health. 2018;12:1746–1758. doi: 10.1177/1557988318786868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Doyle-Lucas AF, Akers JD, Davy BM. Energetic efficiency, menstrual irregularity, and bone mineral density in elite professional female ballet dancers. [PubMed]
- 85.Escobar-Molina R, Rodríguez-Ruiz S, Gutiérrez-García C, Franchini E. Weight loss and psychological-related states in high-level judo athletes. Int J Sport Nutr Exerc Metab. 2015;25:110–118. doi: 10.1123/ijsnem.2013-0163. [DOI] [PubMed] [Google Scholar]
- 86.Ferrand C, Brunet E. Perfectionism and risk for disordered eating among young french male cyclists o f high performance1. Owens & Haase; 2004. [DOI] [PubMed]
- 87.Filaire E, Larue J, Rouveix M. Eating behaviours in relation to emotional intelligence. Int J Sports Med. 2011;32:309–315. doi: 10.1055/s-0030-1269913. [DOI] [PubMed] [Google Scholar]
- 88.Flatt RE, Thornton LM, Fitzsimmons-Craft EE, Balantekin KN, Smolar L, Mysko C, et al. Comparing eating disorder characteristics and treatment in self-identified competitive athletes and non-athletes from the National Eating Disorders Association online screening tool. Int J Eat Disord. 2021;54:365–375. doi: 10.1002/eat.23415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gibson C, Hindle C, McLay-Cooke R, Slater J, Brown R, Smith B, et al. Body image among elite rugby union players. J Strength Cond Res. 2019;33:2217–2222. doi: 10.1519/JSC.0000000000002312. [DOI] [PubMed] [Google Scholar]
- 90.Goltz FR, Stenzel LM, Schneider CD. Disordered eating behaviors and body image in male athletes. Rev Bras Psiquiatr. 2013;35:237–242. doi: 10.1590/1516-4446-2012-0840. [DOI] [PubMed] [Google Scholar]
- 91.Godoy-Izquierdo D, Díaz I. Inhabiting the Body(ies) in female soccer players: the protective role of positive body image. Front Psychol. 2021;12:718836. doi: 10.3389/fpsyg.2021.718836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gouttebarge V, Kerkhoffs GMMJ. A prospective cohort study on symptoms of common mental disorders among current and retired professional ice hockey players. Phys Sportsmed. 2017;45:252–258. doi: 10.1080/00913847.2017.1338497. [DOI] [PubMed] [Google Scholar]
- 93.Gouttebarge V, Johnson U, Rochcongar P, Rosier P, Kerkhoffs G. Symptoms of common mental disorders among professional football referees: a one-season prospective study across Europe. Phys Sportsmed. 2017;45:11–16. doi: 10.1080/00913847.2017.1248796. [DOI] [PubMed] [Google Scholar]
- 94.Gouttebarge V, Jonkers R, Moen M, Verhagen E, Wylleman P, Kerkhoffs G. The prevalence and risk indicators of symptoms of common mental disorders among current and former Dutch elite athletes. J Sports Sci. 2017;35:2148–2156. doi: 10.1080/02640414.2016.1258485. [DOI] [PubMed] [Google Scholar]
- 95.Greenleaf C, Petrie T, Carter J, Reel J. Female collegiate athletes: prevalence of eating disorders and disordered eating behaviors. J Am Coll Health. 2009;57:489–496. doi: 10.3200/JACH.57.5.489-496. [DOI] [PubMed] [Google Scholar]
- 96.Hauck C, Schipfer M, Ellrott T, Cook B. The relationship between food addiction and patterns of disordered eating with exercise dependence: in amateur endurance athletes. Eat Weight Disord. 2020;25:1573–1582. doi: 10.1007/s40519-019-00794-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hoch AZ, Papanek P, Szabo A, Widlansky ME, Schimke JE, Gutterman DD. Association between the female athlete triad and endothelial dysfunction in dancers. 2011. [DOI] [PMC free article] [PubMed]
- 98.Hoch AZ, Pajewski NM, Moraski L, Carrera GF, Wilson CR, Hoffmann RG, et al. Prevalence of the female athlete Triad in high school athletes and sedentary students. Clin J Sport Med. 2009;19:421–428. doi: 10.1097/JSM.0b013e3181b8c136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lock J, Hopkinson RA, Lock J. Athletics, perfectionism, and disordered eating. 2004. [DOI] [PubMed]
- 100.Hulley AJ, Hill AJ. Eating disorders and health in elite women distance runners. 2001. [DOI] [PubMed]
- 101.Janout V, Janoutová G. Eating disorders risk groups in the czech republic-cross-sectional epidemiologic pilot study. [PubMed]
- 102.Balas J, Augste C, Bratland-Sanda S, Joubert L. Prevalence of amenorrhea in elite female competitive climbers. [DOI] [PMC free article] [PubMed]
- 103.Joubert LM, Gonzalez GB, Larson AJ. Prevalence of disordered eating among international sport lead rock climbers. Front Sports Act Living. 2020;2:86. doi: 10.3389/fspor.2020.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Junge A, Hauschild A. Behind the curtain: prevalence of symptoms of depression, generalised anxiety and eating disorders in 147 professional dancers from six opera houses or state theatres. Sports Med Open. 2023 doi: 10.1186/s40798-023-00638-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kampouri D, Kotopoulea-Nikolaidi M, Daskou S, Giannopoulou I. Prevalence of disordered eating in elite female athletes in team sports in Greece. Eur J Sport Sci. 2019;19:1267–1275. doi: 10.1080/17461391.2019.1587520. [DOI] [PubMed] [Google Scholar]
- 106.Karlson KA, Becker B, Merkur ‡amanda. Prevalence of eating disordered behavior in collegiate lightweight women rowers and distance runners. 2001. [DOI] [PubMed]
- 107.Karlsson E, Alricsson M, Melin A. Symptoms of eating disorders and low energy availability in recreational active female runners. BMJ Open Sport Exerc Med. 2023;9:e001623. doi: 10.1136/bmjsem-2023-001623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kennedy SF, Ley AF, Fugate BN, Hayek A. Factors associated with disordered eating behaviors among triathletes. Spartan Med Res J. 2017;2:5958. doi: 10.51894/001c.5958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kristjánsdóttir H, Sigurðardóttir P, Jónsdóttir S, Þorsteinsdóttir G, Saavedra J. Body image concern and eating disorder symptoms among elite icelandic athletes. Int J Environ Res Public Health. 2019;16:2728. doi: 10.3390/ijerph16152728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lauder TD. The female athlete triad: prevalence in military women. 1999. [PubMed]
- 111.Lauder TD;, Williams MV;, Campbell CS;, Davis GD;, Sherman RA. Abnormal eating behaviors in military women. [DOI] [PubMed]
- 112.Marshall D, Harber VJ, Marshall JD, Harber V. Body dissatisfaction and drive for thinness in high performance field hockey athletes. 1996. [DOI] [PubMed]
- 113.Rodríguez AM, Salar NV, Carretero CM, Gimeno EC, Collado ER. Eating disorders and diet management in contact sports; EAT-26 questionnaire does not seem appropriate to evaluate eating disorders in sports. Nutr Hosp. 2015;32:1708–1714. doi: 10.3305/nh.2015.32.4.9214. [DOI] [PubMed] [Google Scholar]
- 114.Martinovic D, Tokic D, Martinovic L, Vilovic M, Vrdoljak J, Kumric M, et al. Adherence to mediterranean diet and tendency to orthorexia nervosa in professional athletes. Nutrients. 2022;14:237. doi: 10.3390/nu14020237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.McLester CN, Hardin R, Hoppe S. Susceptibility to eating disorders among collegiate female student-athletes. J Athl Train. 2014;49:406–410. doi: 10.4085/1062-6050-49.2.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Meng K, Qiu J, Benardot D, Carr A, Yi L, Wang J, et al. The risk of low energy availability in Chinese elite and recreational female aesthetic sports athletes. J Int Soc Sports Nutr. 2020;17:1. doi: 10.1186/s12970-020-00344-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Michaels C, Holman A, Teramoto M, Bellendir T, Krautgasser-Tolman S, Willick SE. Descriptive analysis of mental and physical wellness in collegiate dancers. J Dance Med Sci. 2023;27:173–179. doi: 10.1177/1089313X231178091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Monthuy-Blanc J, Maïano C, Therme P. Prévalence des symptômes de troubles du comportement alimentaire chez des danseuses classiques et des joueuses de basket-ball ne pratiquant pas à un haut niveau: une étude exploratoire et contrôlée auprès d’adolescentes fran. Rev Epidemiol Sante Publique. 2010;58:415–424. doi: 10.1016/j.respe.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 119.Nichols JF, Rauh MJ, Lawson MJ, Ji M, Barkai H-S. Prevalence of the female athlete triad syndrome among high school athletes. 2006. [DOI] [PubMed]
- 120.Nieves JW, Ruffing JA, Zion M, Tendy S, Yavorek T, Lindsay R, et al. Eating disorders, menstrual dysfunction, weight change and DMPA use predict bone density change in college-aged women. Bone. 2016;84:113–119. doi: 10.1016/j.bone.2015.12.054. [DOI] [PubMed] [Google Scholar]
- 121.O’Connell S. Disordered eating is not associated with musculoskeletal injury in university athletes. Appl Physiol Nutr Metab. 2024;49:87–92. doi: 10.1139/apnm-2023-0244. [DOI] [PubMed] [Google Scholar]
- 122.Patrick O’Connor, Richard Lewis, Elsiabeth Kirchner. Eating disorder symptoms in female college gymnasts. [PubMed]
- 123.O’Leary TJ, Coombs CV, Perrett C, Double RL, Keay N, Wardle SL, et al. Menstrual function, eating disorders, low energy availability, and musculoskeletal injuries in British servicewomen. Med Sci Sports Exerc. 2023;55:1307–1316. doi: 10.1249/MSS.0000000000003154. [DOI] [PubMed] [Google Scholar]
- 124.Pallotto IK, Sockol LE, Stutts LA. General and sport-specific weight pressures as risk factors for body dissatisfaction and disordered eating among female collegiate athletes. Body Image. 2022;40:340–350. doi: 10.1016/j.bodyim.2022.01.014. [DOI] [PubMed] [Google Scholar]
- 125.Peklaj E, Reščič N, Koroušic´ Seljak B, Rotovnik Kozjek N. Is RED-S in athletes just another face of malnutrition? Clin Nutr ESPEN. 2022;48:298–307. [DOI] [PubMed]
- 126.Pensgaard AM, Oevreboe TH, Ivarsson A. Mental health among elite athletes in Norway during a selected period of the COVID-19 pandemic. BMJ Open Sport Exerc Med. 2021;7. [DOI] [PMC free article] [PubMed]
- 127.Pernick Y, Nichols JF, Rauh MJ, Kern M, Ji M, Lawson MJ, et al. Disordered eating among a multi-racial/ethnic sample of female high-school athletes. J Adolesc Health. 2006;38:689–695. doi: 10.1016/j.jadohealth.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 128.Petrie TA, Greenleaf C, Reel JJ, Carter JE. An examination of psychosocial correlates of eating disorders among female collegiate athletes. Res Q Exerc Sport. 2009;80:621–632. doi: 10.1080/02701367.2009.10599601. [DOI] [PubMed] [Google Scholar]
- 129.Pettersen I, Hernaes E, Skårderud F. Pursuit of performance excellence: a population study of Norwegian adolescent female cross-country skiers and biathletes with disordered eating. 10.1136/bmjsem-2016. [DOI] [PMC free article] [PubMed]
- 130.Poucher ZA, Tamminen KA, Sabiston CM, Cairney J. A longitudinal examination of changes in mental health among elite Canadian athletes. J Sports Sci. 2022;40:733–741. doi: 10.1080/02640414.2021.2015908. [DOI] [PubMed] [Google Scholar]
- 131.Prather H, Hunt D, McKeon K, Simpson S, Meyer EB, Yemm T, et al. Are elite female soccer athletes at risk for disordered eating attitudes, menstrual dysfunction, and stress fractures? PM and R. 2016;8:208–213. doi: 10.1016/j.pmrj.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Pritchett K, Difolco A, Glasgow S, Pritchett R, Williams K, Stellingwerff T, et al. Risk of low energy availability in national and international level paralympic athletes: an exploratory investigation. Nutrients. 2021;13:1–12. doi: 10.3390/nu13030979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Rauh MJ, Nichols JF, Barrack MT. Relationships among injury and disordered eating, menstrual dysfunction, and low bone mineral density in high school athletes: a prospective study. [DOI] [PMC free article] [PubMed]
- 134.Ravaldi C, Vannacci A, Zucchi T, Mannucci E, Cabras PL, Boldrini M, et al. Eating disorders and body image disturbances among ballet dancers, gymnasium users and body builders. Psychopathology. 2003;36:247–254. doi: 10.1159/000073450. [DOI] [PubMed] [Google Scholar]
- 135.Ravi S, Ihalainen JK, Taipale-Mikkonen RS, Kujala UM, Waller B, Mierlahti L, et al. Self-reported restrictive eating, eating disorders, menstrual dysfunction, and injuries in athletes competing at different levels and sports. Nutrients. 2021;13. [DOI] [PMC free article] [PubMed]
- 136.Reinking MF, Alexander LE. by the national athletic trainers. Association, Inc; 2005.
- 137.Reinking MF. Exercise-related leg pain in female collegiate athletes: the influence of intrinsic and extrinsic factors. Am J Sports Med. 2006;34:1500–1507. doi: 10.1177/0363546506287298. [DOI] [PubMed] [Google Scholar]
- 138.Riebl SK, Subudhi AW, Broker JP, Schenck K, Berning JR. The prevalence of subclinical eating disorders among male cyclists. J Am Diet Assoc. 2007;107:1214–1217. doi: 10.1016/j.jada.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 139.Roberts TA, Glen J, Kreipe RE. Disordered eating and menstrual dysfunction in adolescent female athletes participating in school-sponsored sports. [DOI] [PubMed]
- 140.Rousselet M, Guérineau B, Paruit MC, Guinot M, Lise S, Destrube B, et al. Disordered eating in French high-level athletes: association with type of sport, doping behavior, and psychological features. Eat Weight Disord. 2017;22:61–68. doi: 10.1007/s40519-016-0342-0. [DOI] [PubMed] [Google Scholar]
- 141.Rouveix M, Bouget M, Pannafieux C, Champely S, Filaire E. Eating attitudes, body esteem, perfectionism and anxiety of judo athletes and nonathletes. Int J Sports Med. 2007;28:340–345. doi: 10.1055/s-2006-924334. [DOI] [PubMed] [Google Scholar]
- 142.Schtscherbyna A, Soares EA, de Oliveira FP, Ribeiro BG. Female athlete triad in elite swimmers of the city of Rio de Janeiro. Brazil Nutrition. 2009;25:634–639. doi: 10.1016/j.nut.2008.11.029. [DOI] [PubMed] [Google Scholar]
- 143.Sharps FRJ, Wilson LJ, Graham CAM, Curtis C. Prevalence of disordered eating, eating disorders and risk of low energy availability in professional, competitive and recreational female athletes based in the United Kingdom. Eur J Sport Sci. 2022;22:1445–1451. doi: 10.1080/17461391.2021.1943712. [DOI] [PubMed] [Google Scholar]
- 144.Smith A, Emerson D, Winkelmann Z, Potter D, Torres-Mcgehee T. Prevalence of eating disorder risk and body image dissatisfaction among ROTC cadets. Int J Environ Res Public Health. 2020;17:1–13. doi: 10.3390/ijerph17218137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sophia B, Kelly P, Ogan D, Larson A. Olympic marathon trials. [DOI] [PMC free article] [PubMed]
- 146.Staal S, Sjödin A, Fahrenholtz I, Bonnesen K, Melin AK. Low RMRratio as a surrogate marker for energy deficiency, the choice of predictive equation vital for correctly identifying male and female ballet dancers at risk. Int J Sport Nutr Exerc Metab. 2018;28:412–418. doi: 10.1123/ijsnem.2017-0327. [DOI] [PubMed] [Google Scholar]
- 147.Stackeová D, Barešová T, Přibylová B. A pilot study of a modification EAT-26 questionnaire for screening pathological eating behavior in competitive athletes. Front Psychol. 2023;14(1):166129. doi: 10.3389/fpsyg.2023.1166129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Jorunn Sundgot-Borgen. Prevalence of eating disorders in elite female athletes jorunn sundgot-borgen. 1993. [DOI] [PubMed]
- 149.Jorunn Sundgot-Borgen. Risk and trigger factors for the development of eating disorders in female elite athletes. 1993. [PubMed]
- 150.Sundgot-Borgen J, Torstveit MK. Prevalence of eating disorders in elite athletes is higher than in the general population. 2004. [DOI] [PubMed]
- 151.Sundgot-Borgen J, Fasting K, Brackenridge C, Torstveit MK, Berglund B. Sexual harassment and eating disorders in female elite athletes ± a controlled study. [DOI] [PubMed]
- 152.Syed J, Jamil A, Namroz N, Shakeel M, Malik A, Kanwal S, et al. Prevalence of risk factors of the female athlete triad among young elite athletes of Pakistan. Int J Sports Phys Ther. 2022;17:210–217. doi: 10.26603/001c.31641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Teixidor-Batlle C, Ventura C, Andrés A. Eating disorder symptoms in elite Spanish athletes: prevalence and sport-specific weight pressures. Front Psychol. 2021;11:3612. doi: 10.3389/fpsyg.2020.559832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Tenforde AS, DeLuca S, Wu AC, Ackerman KE, Lewis M, Rauh MJ, et al. Prevalence and factors associated with bone stress injury in middle school runners. PM and R. 2022;14:1056–1067. doi: 10.1002/pmrj.12673. [DOI] [PubMed] [Google Scholar]
- 155.Terry PC, Lane AM, Warren L. Eating attitudes, body shape perceptions and mood of elite rowers. [DOI] [PubMed]
- 156.Thein-Nissenbaum JM, Rauh MJ, Carr KE, Loud KJ, Mcguine TA. Associations between disordered eating, menstrual dysfunction, and musculoskeletal injury among high school athletes. J Orthop Sports Phys Ther. 2011;41:60–69. doi: 10.2519/jospt.2011.3312. [DOI] [PubMed] [Google Scholar]
- 157.Thein-Nissenbaum JM, Carr KE, Hetzel S, Dennison E. Disordered eating, menstrual irregularity, and musculoskeletal injury in high school athletes: a comparison of oral contraceptive pill users and nonusers. Sports Health. 2014;6:313–320. doi: 10.1177/1941738113498852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.A. THiel, h. Gottfriend, F.W. Hesse. Subclinical eating disorders in male athletes. [DOI] [PubMed]
- 159.Thompson SH. Characteristics of the female athlete triad in collegiate cross-country runners. J Am Coll Health. 2007;56:129–136. doi: 10.3200/JACH.56.2.129-136. [DOI] [PubMed] [Google Scholar]
- 160.Thompson A, Petrie T, Anderson C. Eating disorders and weight control behaviors change over a collegiate sport season. J Sci Med Sport. 2017;20:808–813. doi: 10.1016/j.jsams.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 161.Torres-McGehee TM, Green JM, Leeper JD, Leaver-Dunn D, Richardson M, Bishop PA. Body image, anthropometric measures, and eating-disorder prevalence in auxiliary unit members. 2009. [DOI] [PMC free article] [PubMed]
- 162.Torres-McGehee TM, Monsma E v, Gay JL, Minton DM, Mady-Foster AN. Prevalence of eating disorder risk and body image distortion among national collegiate athletic association division I varsity equestrian athletes. 2011. [DOI] [PMC free article] [PubMed]
- 163.Torres-McGehee TM, Uriegas NA, Hauge M, Monsma EV, Emerson DM, Smith AB. Eating disorder risk and pathogenic behaviors among collegiate student-athletes. J Athl Train. 2023;58:803–812. doi: 10.4085/1062-6050-0539.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Torstveit MK, Sundgot-Borgen J. The female athlete triad: are elite athletes at increased risk? Med Sci Sports Exerc. 2005;37:184–193. doi: 10.1249/01.MSS.0000152677.60545.3A. [DOI] [PubMed] [Google Scholar]
- 165.Torstveit MK, Rosenvinge JH, Sundgot-Borgen J. Prevalence of eating disorders and the predictive power of risk models in female elite athletes: a controlled study. Scand J Med Sci Sports. 2008;18:108–118. doi: 10.1111/j.1600-0838.2007.00657.x. [DOI] [PubMed] [Google Scholar]
- 166.Uriegas NA, Winkelmann ZK, Pritchett K, Torres-McGehee TM. Examining eating attitudes and behaviors in collegiate athletes, the association between orthorexia nervosa and eating disorders. Front Nutr. 2021;8:763838. doi: 10.3389/fnut.2021.763838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Uriegas NA, Moore K, Torres-McGehee TM. Prevalence and association of exercise dependence and eating disorder risk in collegiate student-athletes. J Athl Train. 2023;58:813–820. doi: 10.4085/1062-6050-0553.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Arzu Vardar S, Vardar E, Durmus Altun G, Kurt C, Öztürk L. Prevalence of the female athlete triad in edirne, TURKEY. 2005. [PMC free article] [PubMed]
- 169.Vardar E, Vardar SA, Kurt C. Anxiety of young female athletes with disordered eating behaviors. Eat Behav. 2007;8:143–147. doi: 10.1016/j.eatbeh.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 170.Janet Walberg, Cutting Johnston. Menstrual function and eating behavior in female recreational weight lifters and competitive body builders. [PubMed]
- 171.Waryasz G, Gil JA, Chiou D, Eberson C, Waryasz GR, Ferreira B; K, et al. Investigation of the injury rate of female fitness competitors. [PubMed]
- 172.Wheeler GD, Wall SR, Belcastro AN, Conger P, Cumming DC. Are anorexic tendencies prevalent in the habitual runner? 1986. [DOI] [PMC free article] [PubMed]
- 173.Wollenberg G, Shriver LH, Gates GE. Comparison of disordered eating symptoms and emotion regulation difficulties between female college athletes and non-athletes. Eat Behav. 2015;18:1–6. doi: 10.1016/j.eatbeh.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 174.Wu AC, Rauh MJ, DeLuca S, Lewis M, Ackerman KE, Barrack MT, et al. Running-related injuries in middle school cross-country runners: prevalence and characteristics of common injuries. PM R. 2022;14:793–801. doi: 10.1002/pmrj.12649. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1 Traffic light of the included studies.
Additional file 2 Radial plot of disordered eating in athletes.
Additional file 3 DOI plot of disordered eating in athletes.
Additional file 4 Drapery plot of disordered eating in athletes.
Additional file 6 Meta-regression of disordered eating in athletes by Age.
Additional file 7 Meta-regression of disordered eating in athletes by BMI.
Additional file 8 Meta-regression of disordered eating in athletes by Sex (%Female Sex).
Additional file 9 Subgroup meta-analysis by country.
Additional file 10 Subgroup meta-analysis by culture.
Additional file 11 Subgroup meta-analysis by the sports energy system .
Additional file 12 Subgroup meta-analysis by sports category.
Additional file 13 Subgroup meta-analysis by disordered eating measurement tool.
Additional file 14 Subgroup meta-analysis by study design.
Data Availability Statement
Data is available in Table 1.