Abstract
Objective
The aim of this study was to identify clinical phenotypes using sensor-based measures of posture and movement, pain behavior, and psychological factors in Hispanic/Latino people with chronic low back pain (CLBP).
Methods
Baseline measures from an ongoing clinical trial were analyzed for 81 Hispanic/Latino people with CLBP. Low back posture and movement were measured using commercial sensors during in-person testing and 8 hours of ecological monitoring. Magnitude, frequency, and duration of lumbar movements, sitting and standing postures were measured. Movement-evoked pain was assessed during in-person movement testing. Psychological measures included the Pain Catastrophizing Scale and the Fear Avoidance Beliefs Questionnaire. Random forest analysis was conducted to generate 2 groups and identify important variables that distinguish groups. Group differences in demographics, pain, psychological, and posture and movement variables were examined using t-tests and chi-square analyses.
Results
Two subgroups of Hispanic/Latino people with CLBP were identified with minimal error (7.4% misclassification [“out-of-bag” error]). Ecological posture and movement measures best distinguished groups, although most movement-evoked pain and psychological measures did not. Group 1 had greater height and weight, lower movement frequency, more time in sitting, and less time in standing. Group 2 had a greater proportion of women than men, longer low back pain duration, higher movement frequency, more time in standing, and less time in sitting.
Conclusion
Two distinct clinical phenotypes of Hispanic/Latino people with CLBP were identified. One group was distinguished by greater height and weight and more sedentary posture and movement behavior; the second group had more women, longer duration of low back pain, higher lumbar spine movement frequency, and longer duration of standing postures.
Impact
Ecological measures of posture and movement are important for identifying 2 clinical phenotypes in Hispanic/Latino people with CLBP and may provide a basis for a more personalized plan of care.
Lay Summary
Wearable sensors were used to measure low back posture and movement in Hispanic/Latino people with chronic low back pain. These posture and movement measures helped to identify 2 different clinical subgroups that will give physical therapists more information to better personalize treatment for chronic low back pain in Hispanic/Latino patients.
Keywords: Chronic Pain, Low Back Pain, Movement, Posture
Introduction
Nearly 80% of the population has reported having low back pain (LBP) at some point during their lifetime.1 An average of 62% of people report developing chronic LBP after a first episode,2 and in many cases pain and disability can persist after a year.3 LBP can have a profound impact on the individual and society. In a global burden of disease study, LBP ranked highest among the most disabling diseases globally.4 As one of the leading causes of health care visits, patients with LBP spend nearly $4,000 (in 2005 dollars) for 1 episode of LBP,5 and the estimated annual cost of LBP to society is $100 billion, including decreased productivity and lost wages.6
Epidemiologic studies have begun to explore racial and ethnic disparities in rates of LBP. Although some investigators have reported lower prevalence rates7 and odds8 of chronic LBP in Hispanic/Latino people9 than in non-Hispanic White people, this could be explained by younger age8 and is based on a low overall percentage of Hispanic/Latino participants in study samples (4%–14.5%).7,8 Other investigators have reported a high prevalence of LBP in specific samples of Hispanic/Latino participants. In 1 study, 66% of Latino farmworkers reported LBP, and those who worked longer (>5 years) were more likely to have LBP.10 In another study of older adults, 55% of people who were Latino reported having chronic LBP.11 Furthermore, in a recent secondary analysis of a cohort study, Hispanic participants demonstrated higher self-reported disability and were at higher risk of persistent disability due to chronic LBP than non-Hispanic White people.12 These data underscore the need for more research on diverse samples including Hispanic/Latino people with LBP.
Physical therapist management of LBP often includes assessment and intervention addressing posture and movement dysfunction.13 Current evidence suggests that differences in movement exist between people with and without LBP. In a systematic review with meta-analysis, Laird et al reported that across studies, people with LBP displayed reduced range of motion during flexion, extension, lateral bending, and rotation compared to people without LBP.14 However, another systematic review noted that prior studies on movement in people with LBP failed to consider multidirectional movements of the spine that occur throughout the day; of the studies evaluated, only 17% measured movement in multiple planes in the same sample.15 Furthermore, there are conflicting findings in terms of the relative importance of change in pain during movement (movement-evoked pain) and the extent to which pain is associated with movement.15,16 An understanding of movement-evoked pain may be important for informing physical therapist recommendations for modifying movements that evoke pain during a clinical examination.16 Despite these limitations, evidence from a number of different investigative groups supports the existence of movement-based subgroups and use of these subgroups to guide treatment for people with chronic low back pain (CLBP).17–25
Although there have been extensive studies characterizing posture and movement in people with LBP, most studies have either not reported racial and ethnic characteristics of the sample or have not included a diverse sample. Only a limited number of studies have used laboratory measures to examine differences in low back posture and movement between racial and ethnic groups. Investigators of 2 studies reported greater lordosis and more extension movement in Black women compared to White women.26,27 In another study, significant differences in spine movement parameters were identified among Black, White, and Asian participants.28 These data underscore the importance of considering race and ethnicity when examining low back posture and movement. In addition to limited diversity of samples, most studies on posture and movement have utilized clinical and laboratory measures. Only a limited number of studies have reported ecological measures of posture and movement in people with LBP to reflect actual behavior during everyday life and in a person’s natural environment, and none have included diverse samples.17,29 With the emergence of new sensor technologies that are smaller, lighter weight, lower cost, more accurate, and with a longer battery life, it is now more feasible to derive these ecological measures of lumbar spine posture and movement for a variety of clinical populations.30 Although data on provider and patient acceptability of using spine sensors in clinical practice are limited, a recent study on the clinical use of sensors reported high patient acceptability (92%–98%) and provider agreement (100%) that information derived from sensors was informative for their clinical impression.31
In addition to posture and movement, a number of different psychological factors have been associated with CLBP32–34; subgroups of people with CLBP based on psychological factors have been identified.35 Psychological factors such as fear of movement and pain catastrophizing have been proposed to be associated with both posture and movement behavior as well as clinical outcomes in people with LBP.36,37 However, the extent to which psychological factors influence daily movement behavior and their association with identified LBP subgroups is unclear.38 Therefore, it may be important to consider these psychological factors, in addition to posture and movement factors, when identifying clinical phenotypes to help direct physical therapist intervention. Psychological factors may be of particular importance for Hispanic/Latino people with CLBP because people who are Latino have reported higher levels of pain-related anxiety, pain severity, and pain catastrophizing than non-Latino people with chronic pain.39
Understanding the combined influence of posture and movement, movement-evoked pain, and psychological factors may be helpful for identifying clinical phenotypes with the goal of developing more targeted physical therapist interventions for Hispanic/Latino people with CLBP. Therefore, the purpose of this study was to identify clinical phenotypes based on the intersection of factors including sensor-based measures of posture and movement during an in-person assessment and ecological monitoring, movement-evoked pain, and psychological factors in Hispanic/Latino people with CLBP.
Methods
This study is a cross-sectional, observational secondary analysis of baseline data from an ongoing randomized clinical trial (protocol ID: 228489; registration number: NCT05005416).
Participants
Participants were recruited via consecutive sampling of a referral database for patients who self-reported Hispanic ethnicity, were 18 to 66 years old, and were referred to physical therapy for chronic spine pain at a federally qualified health center with integrated physical therapist services in San Diego, California. Patients were contacted via telephone for eligibility screening based on the following inclusion criteria: self-identify as Hispanic or Latino; chronic spine pain for  3 months and on at least half of the days in the past 6 months; Brief Pain Inventory pain severity subscale score of
3 months and on at least half of the days in the past 6 months; Brief Pain Inventory pain severity subscale score of  4/1040–42; and STarT Back screening tool score of
4/1040–42; and STarT Back screening tool score of  4/9.43 Exclusion criteria included severe cognitive impairment (<8/15 on the Brief Interview for Mental Status)44; self-reported history of tumor, infection, or other systemic medical problems affecting the spine; health problems that severely affect the ability to move; external incentives for nonrecovery (litigation, worker’s compensation); pregnant or lactating women; plans to start any new behavioral health or psychological treatment for pain; diagnosis of a major psychological condition other than depression or anxiety; unable to provide a stable address with access to a telephone; or residing in the same household as another study participant. Only participants with CLBP were included in the current analysis. The study was approved by the Institutional Review Board of San Diego State University, and all participants provided written informed consent prior to data collection.
4/9.43 Exclusion criteria included severe cognitive impairment (<8/15 on the Brief Interview for Mental Status)44; self-reported history of tumor, infection, or other systemic medical problems affecting the spine; health problems that severely affect the ability to move; external incentives for nonrecovery (litigation, worker’s compensation); pregnant or lactating women; plans to start any new behavioral health or psychological treatment for pain; diagnosis of a major psychological condition other than depression or anxiety; unable to provide a stable address with access to a telephone; or residing in the same household as another study participant. Only participants with CLBP were included in the current analysis. The study was approved by the Institutional Review Board of San Diego State University, and all participants provided written informed consent prior to data collection.
Demographics and Patient-Reported Outcomes
Instructions and questionnaires were provided in the participant’s preferred language, either English or Spanish. Participant characteristics were collected and included sex at birth, age, employment status, and duration of LBP. Participant height and weight were measured, and body mass index was calculated.
Participants completed the following questionnaires to assess LBP characteristics and psychological factors proposed to be associated with movement: Brief Pain Inventory, modified Oswestry Disability Index, Pain Catastrophizing Scale, and Fear Avoidance Beliefs Questionnaire (FABQ).
The Brief Pain Inventory is a self-report measure used to assess chronic pain conditions and includes a pain diagram and questions to assess pain; specifically, pain severity and interference subscales are derived with scores ranging from 0 to 10 (higher scores indicate more pain severity and interference).40,45 The Brief Pain Inventory has demonstrated acceptable validity for people with LBP.41,42
The modified Oswestry Disability Index is one of the most commonly used disease-specific, patient-reported outcome measures for functional disability related to LBP.46,47 Scores on the modified Oswestry Disability Index range from 0% to 100% (higher scores are associated with greater disability), and the measure has demonstrated acceptable validity and reliability.48,49
The Pain Catastrophizing Scale is a self-report measure that characterizes different aspects of catastrophic cognition related to pain including pain rumination, magnification, and helplessness.50 Total scores on the Pain Catastrophizing Scale range from 0 to 52 (higher scores are associated with more pain catastrophizing), and the measure has been found to have good internal consistency, validity, and reliability.51,52
The FABQ is another self-report measure that quantifies fear and avoidance beliefs, focusing specifically on patients’ beliefs about how movement affects their LBP.53 The FABQ has demonstrated acceptable validity and reliability for assessing fear avoidance beliefs in people with LBP.54 The FABQ-PA subscore (0–24) reflects a patient’s fear avoidance beliefs related to physical activity, and the FABQ-W subscore (0–42) reflects fear avoidance beliefs related to work. Higher scores on the FABQ indicate greater fear avoidance beliefs for both scales.
Sensor Measurements
Low back posture and movement were measured using dorsaVi portable motion-tracking sensors (Fig. 1) (dorsaVi, Inc, Melbourne, Victoria, Australia). dorsaVi sensors have demonstrated acceptable reliability (ICCs = 0.86–0.95).55 The sensors have demonstrated concurrent validity with optical motion capture systems for measuring lumbar posture and movement under the following conditions: incremental ranges in sagittal (root-mean-square error [RMSE] = 1.9–2.1 degrees), frontal (RMSE = 2.1–2.4 degrees), and axial (RMSE=4.1–5.2 degrees) planes during 1-, 2-, and 3-dimensional movements (53 total movements) in individuals with healthy backs56; during end-range flexion, extension, and lateral flexion movements in people with and without LBP (RMSE = 0.7–1.8 degrees)57; and with flexion movements throughout ranges of symmetrical (RMSE = 1.3 [standard deviation (SD) = 1.3] degrees) and asymmetrical (RMSE= 1.7 [SD = 1.5] degrees) lifting tasks in individuals with and without LBP.58
Figure 1.
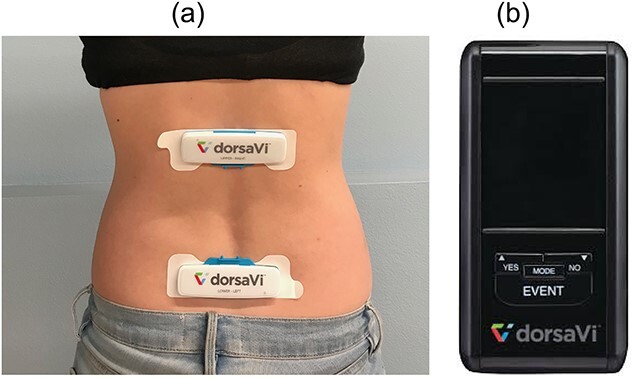
(a) dorsaVi sensor placement and (b) data collection device.
An in-person movement assessment was scheduled in the morning to allow for an 8-hour ecological monitoring session immediately following the in-person session. At the in-person movement assessment, the lower dorsaVi sensor was placed in alignment with the posterior superior iliac spines. Standardized dorsaVi templates (sizes ranging from small to extra-large) were selected based on each participant’s height and were used to place the upper sensor on the lumbar spine. Sensors were then secured with Tegaderm (3M, Minneapolis, MN) in preparation for ecological monitoring. Adhesives and Tegaderm were secured, while the participant’s spine was in a flexed position to allow for stretch during movements throughout the day. Position and movement of the upper sensor relative to the lower sensor were used to characterize lumbar spine alignment and movement. Lumbar spine alignment was measured in self-selected standing and sitting postures and instructed upright and slumped sitting postures during the in-person assessment. The start position for movement tests for each participant was their self-selected posture in either sitting or standing. The participant was then instructed to perform the following trunk movements to end range in standing: flexion, extension, lateral flexion, and pelvic tilt. End-range trunk rotation and pelvic tilt also were assessed in sitting. Each movement was performed 3 times. Movement tests were performed in a prescribed order; start side (left, right) was randomized for lateral flexion and rotation movements. To characterize movement-evoked pain, subjective reports of change in pain (increase, decrease, no change) were assessed when the participant performed each test movement during the in-person assessment. Maximum range of motion, relative to standing or sitting alignment, was calculated for each movement and an average of the 3 trials was calculated. Posture and movement tests during the in-person assessment were used as a basis for categorizing postures and movements during ecological monitoring based on established algorithms in the dorsaVi software program.
Ecological Monitoring
Following the in-person assessment, participants were instructed to wear the dorsaVi sensors for 8 consecutive hours of ecological monitoring. Ecological monitoring sessions were conducted during a workday or nonworkday at the participants’ convenience, and this information was documented. Participants carried a wireless device in a lanyard around their neck. The device recorded data from the sensors throughout the duration of the ecological monitoring session (Fig. 1). Throughout the day, the sensors monitored and recorded the magnitude, frequency, and duration of lumbar movements. Specific posture and movement measures derived from the 8-hour monitoring session were evaluated using dorsaVi software and included maximum range of motion into flexion, extension, and left/right lateral flexion; frequency of movement events into lumbar flexion, extension, and left/right lateral flexion; duration of the longest period of uninterrupted standing and sitting postures; number of uninterrupted posture periods in standing, sitting, and sitting slouched; and percentage of total sitting time spent in usual, slumped, and upright postures (Suppl. Material 1). All postures and movements during ecological monitoring were identified on the basis of individualized posture and movement during the in-person assessment and using default thresholds in the dorsaVi software based on ranges of movement and temporal parameters (Tab. 1). The frequency of movement events into flexion, extension, and right/left lateral flexion was subcategorized into short-term events and long-term events using temporal parameters; the frequency of movement events was also subcategorized on the basis of different phases of movement, including early range, midrange, and end-range. Table 1 includes each parameter used for subcategorizing movement events during ecological monitoring for each direction of movement.
Table 1.
Parameters for Movement Variables During Ecological Monitoring in dorsaVi Software Program
| Parameter | Description | Flexion | Extension | Lateral Flexion |
|---|---|---|---|---|
| Threshold for movement detection, ° | Threshold required to detect movement in each direction during ecological monitoring |
 20
20 |
 10
10 |
 10
10 |
| Short-term events, s | Duration of movement in each direction used to identify short-duration movement | 1.5–30 | 1.5–15 | 1.5–15 |
| Long-term events, s | Duration of movement in each direction used to identify longer duration movement |
 30
30 |
 15
15 |
 15
15 |
| Early range movement, ° | Degree of movement in each direction used to identify early range movement | 20–40 | 10–15 | 10–15 |
| Midrange movement, ° | Degree of movement in each direction used to identify midrange movement | 40–60 | 15–20 | 15–20 |
| End-range movement, ° | Degree of movement in each direction used to identify end-range movement |
 60
60 |
 20
20 |
 20
20 |
Statistical Analysis
Random forest analyses were used to identify clinical phenotypes for Hispanic/Latino people with CLBP using sensor-based measures of posture and movement, movement-evoked pain during in-person movement testing, and psychological factors. In a random forest analysis, a collection of “classification trees” in which each tree is “grown” with a different bootstrap sample of the original data is developed.59 Using data for each participant, each tree “votes” for a classification or subgroup, and the majority rule is used for the final prediction of subgroup membership. Because each tree is grown with a bootstrap sample of the data, out-of-sample data are available to calculate misclassification (“out-of-bag” error). The out-of-sample data also can be used to determine variable importance for each variable. This is done by randomly permuting each variable one at a time to represent the exclusion of each variable in the out-of-sample data for each tree and recording the prediction. The magnitude of the decrease in accuracy when a variable is excluded from the prediction indicates the importance of that variable. For classification and clustering, random forest analysis can be used for both identifying new subgroups (unsupervised) and determining variables that are most important for differentiating existing groups (supervised). Random forest analysis has been used previously to identify clinical phenotypes60 and is preferred to other analytic approaches with this type of data because it is less affected by intercorrelated variables included in the analysis.59
A 3-step approach was used and included the following: step 1 was an unsupervised random forest analysis to identify subgroups of Hispanic/Latino people with CLBP on the basis of all variables (2 subgroups); step 2 was a supervised random forest analysis to determine which variables were statistically important (P < .10) for identifying subgroups; and step 3 was a final supervised random forest analysis including only important variables identified in step 2 for identifying subgroups. The number of subgroups (2) was determined by examining the average silhouette plot over a range of subgroup numbers. The silhouette is a measure of how close each point in 1 subgroup is to the points in the neighboring subgroup and can be averaged over all points in the dataset. The largest average silhouette value was obtained for 2 subgroups.61 A conservative threshold of P < .10 in step 2 was used for dimension reduction purposes to determine variable inclusion in the final supervised analysis.
For step 1, the unsupervised random forest, a proximity matrix was generated using 12 posture and movement variables and 8 measures of movement-evoked pain from the in-person assessment, 63 posture and movement measures from ecological monitoring, and 3 psychological measures (Pain Catastrophizing Scale, FABQ-PA, and FABQ-W) for all participants. A list of all variables included in the unsupervised random forest analysis is included in Supplementary Material 1. The initial 2 subgroups were generated through clustering using this proximity matrix and the partitioning around medoids algorithm. The partitioning around medoids algorithm is more robust to noise and outliers than the more common k-means algorithm. For step 2, a supervised random forest analysis of the subgroups identified in step 1 was used to evaluate variable importance by providing a ranking of the variables on the basis of their importance for discriminating between subgroups. The mean decrease in accuracy was chosen as the measure of variable importance, which reflects the extent to which model accuracy for identifying subgroups would decrease if the variables were removed from the analysis. Thus, higher variable importance metrics are seen for variables that are more important for distinguishing subgroups. For step 3, a final supervised random forest analysis of the subgroups was conducted and included only important variables (P < .10) from the first supervised random forest analysis to reduce error from extraneous variables in the final prediction model. P values were determined by a permutation test. Error for identifying each subgroup individually and overall out-of-bag error were calculated for distinguishing subgroups with the model. Out-of-bag error reflects the error associated with classifying participants in the out-of-sample data for each tree who were not used to derive the original model. Random forest analyses were performed in R.62
Differences in demographics, pain characteristics, psychological factors, and all posture and movement variables identified as important in the final supervised random forest analysis were compared between subgroups using independent sample t-tests for ratio scale measures and chi-square analyses for nominal and ordinal scale measures. These differences were used to characterize clinical phenotypes of Hispanic/Latino people with CLBP. These comparative analyses were performed in SPSS version 28.0 (IBM SPSS, Chicago, IL).
Results
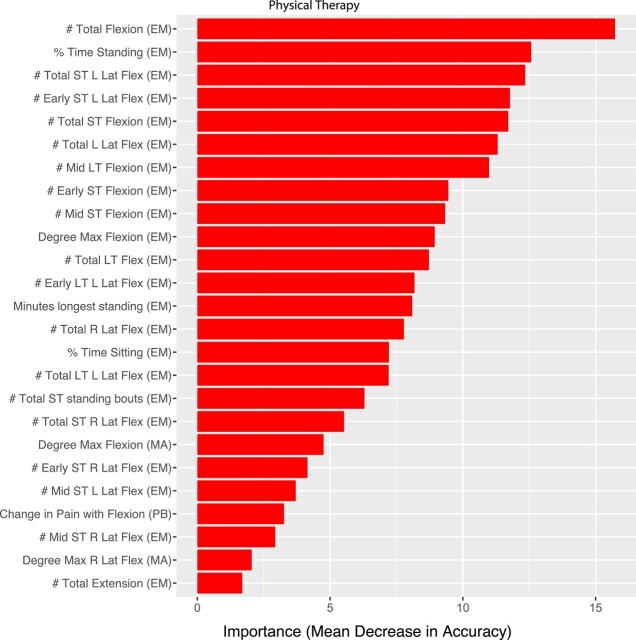
Eighty-one Hispanic/Latino people with CLBP (53 women and 28 men; 47.7 [SD = 12.5] years old) were eligible and participated in baseline testing at the time of this secondary analysis. The unsupervised random forest analysis identified 2 subgroups of Hispanic/Latino people with CLBP, representing 2 distinct clinical phenotypes. Group differences in demographic and LBP characteristics are presented in Table 2. The grouping can be visualized in 2 dimensions using a multidimensional scaling plot (Fig. 2). The multidimensional scaling plot is a way of displaying a closeness or proximity between data points on multiple dimensions, similar to a principal components plot. The dimensions reflect different nonlinear combinations of the variables included in the analysis. Error for identifying participants in group 1 was 4.0%, and error for identifying participants in group 2 was 12.9%, resulting in an overall out-of-bag error of 7.4% for identifying both subgroups. Variables that best distinguished subgroups in the final supervised random forest analyses, based on a mean decrease in accuracy (P values of <.10), were predominantly measures of ecological posture and movement from sensors. Most end-range measures of posture and movement from in-person movement testing with sensors, movement-evoked pain during the in-person assessment, and psychological measures did not significantly distinguish groups (P values of >.10). The magnitude of importance based on the mean decrease in accuracy for each variable that distinguished groups is displayed in Figure 3, and P values for variable importance are provided in Table 3.
Table 2.
Group Differences in Demographic and Clinical Characteristics
| Measure | Group 1 (n = 50) a | Group 2 (n = 31) a | Group Difference (P) |
|---|---|---|---|
| Demographics | |||
| Age, yb | 48.7 (13.5) | 46.0 (10.8) | .361 |
| Sex assigned at birth | .006c | ||
| Female | 54.0 | 83.9 | |
| Male | 46.0 | 16.1 | |
| Height, cmb | 165.4 (8.9) | 160.4 (7.2) | .011c |
| Weight, kgb | 85.6 (19.6) | 77.3 (13.8) | .043c |
| Body mass index, kg/m2b | 31.2 (6.4) | 30.1 (5.3) | .413 |
| Employment status | .007c | ||
| Full time | 40.0 | 16.1 | |
| Part time | 12.0 | 48.4 | |
| Homemaker | 14.0 | 19.4 | |
| Unemployed | 10.0 | 3.2 | |
| Disabled | 16.0 | 9.7 | |
| Retired | 4.0 | 0.0 | |
| Student | 0.0 | 3.2 | |
| Not reported | 4.0 | 0.0 | |
| Type of day on which ecological monitoring data were collectedd | .190 | ||
| Workday | 44.4 | 64.7 | |
| Non-workday | 55.6 | 35.3 | |
| Low back pain characteristics | |||
| Brief Pain Inventory pain severity subscaleb | 5.5 (1.5) | 5.7 (1.8) | .602 |
| Brief Pain Inventory pain interference subscaleb | 6.0 (1.9) | 5.2 (2.2) | .110 |
| Modified Oswestry Disability Indexb | 39.6 (15.0) | 35.0 (14.6) | .173 |
| Duration of low back pain | .008c | ||
| 3–6 mo | 8.0 | 3.2 | |
| >6–12 mo | 6.0 | 9.7 | |
| >1–5 y | 50.0 | 16.1 | |
| >5 y | 36.0 | 71.0 |
Data are reported as percentages unless otherwise indicated.
Data are reported as mean (SD).
Statistically significant at P < .05.
Data were collected on self-reported workday vs nonworkday for a subgroup of participants (n = 44).
Figure 2.
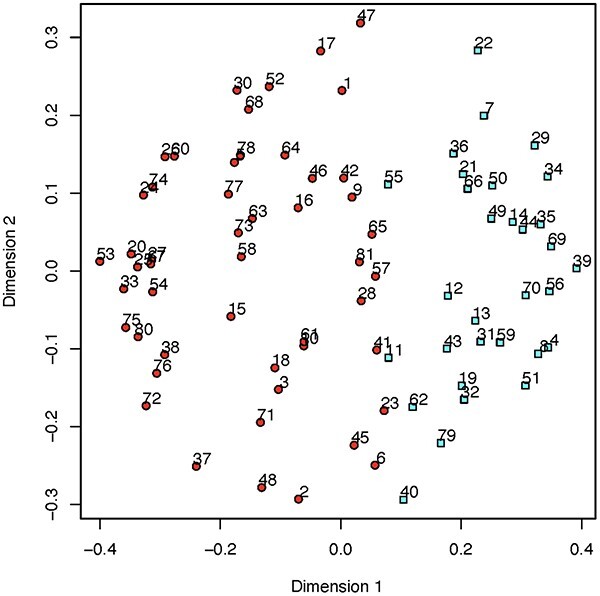
Multidimensional scaling plot showing a 2-dimensional projection of distances between the 2 groups distinguishing individual participants from group 1 (circles) and group 2 (squares) on dimension 1 (x-axis) and dimension 2 (y-axis) from the unsupervised random forest analysis. Multidimensional scaling (MDS) is a dimension-reduction technique to project high dimensional data down to 2 dimensions while preserving the proximity or distance between observations as closely as possible. It is used to visualize proximities. The dimensions (dimension 1 and dimension 2) represent a nonlinear transformation of proximities which are calculated using the tree-based measure of closeness.
Figure 3.
Importance based on mean decrease in accuracy for variables that best distinguished subgroups of people who are Latino with chronic low back pain. Early = early range movements; EM = ecological monitoring variables; Flex = flexion; L = left; Lat Flex = lateral flexion; LT = long term; MA = in-person movement assessment variables; Max = maximum; Mid = midrange movements; PB = movement-evoked pain variables; R = right; ST = short term.
Table 3.
Group Differences in Sensor-Based Measures and Pain Behavior Variables Most Important for Distinguishing Clinical Phenotypes
| Measure | Group 1 (n = 50) a | Group 2 (n = 31) a | Variable Importance (P) | Group Difference (P) |
|---|---|---|---|---|
| Sensor measures of lumbar spine posture and movement during in-person assessment, ° | ||||
| Self-selected standing alignment | 46.3 (13.0) | 56.9 (11.9) | .040 | <.001b |
| Flexion | 19.2 (4.8) | 22.1 (5.1) | .099 | .011c |
| Right lateral flexion | 46.3 (13.0) | 56.9 (11.9) | .040 | <.001b |
| Movement-evoked pain during in-person movement assessment | ||||
| Standing (% of participants) | .069 | .026c | ||
| Increase with flexion | 60 | 35.5 | ||
| Decrease with flexion | 0 | 9.7 | ||
| No change with flexion | 40 | 51.6 | ||
| No pain with flexion | 0 | 3.2 | ||
| Sensor measures of lumbar spine posture and movement during ecological monitoring | ||||
| Positions (% time) | ||||
| Standing | 20.0 (10.2) | 39.4 (10.9) | .010 | <.001b |
| Sitting | 55.5 (16.0) | 37.4 (12.5) | .010 | <.001b |
| Uninterrupted posture periods | ||||
| No. of periods of short-term (10-30 min.) standing | 1.9 (1.7) | 4.8 (2.5) | .020 | <.001b |
| Longest period of standing, min | 23.5 (16.1) | 58.0 (35.9) | .040 | <.001b |
| Maximum movement, ° | ||||
| Flexion | 40.3 (9.5) | 52.6 (8.6) | .010 | <.001b |
| Frequency of flexion | ||||
| Total | 15.0 (10.0) | 60.5 (40.6) | .010 | <.001b |
| Total short term | 10.0 (7.6) | 45.3 (40.8) | .010 | <.001b |
| Total long term | 5.0 (5.0) | 15.3 (7.9) | .010 | <.001b |
| Early range short term | 8.7 (6.6) | 33.1 (26.7) | .010 | <.001b |
| Midrange short term | 1.3 (3.0) | 11.7 (23.0) | .020 | <.001b |
| Midrange long term | 1.0 (1.9) | 5.5 (3.7) | .010 | <.001b |
| Frequency of extension | ||||
| Total | 1.3 (2.9) | 4.4 (11.1) | .080 | .061 |
| Frequency of left lateral flexion | ||||
| Total | 9.6 (11.6) | 54.1 (49.6) | .010 | <.001b |
| Total short term | 8.8 (11.3) | 48.2 (42.0) | .010 | <.001b |
| Total long term | 0.8 (1.1) | 5.9 (8.8) | .010 | <.001b |
| range short term | 7.8 (10.5) | 42.2 (34.1) | .010 | <.001b |
| Early range long term | 0.6 (0.9) | 4.4 (5. 6) | .010 | <.001b |
| Midrange short term | 0.9 (1.5) | 5.8 (8.6) | .040 | <.001b |
| Frequency of right lateral flexion | ||||
| Total | 7.8 (10.5) | 31.2 (31.8) | .020 | .016c |
| Total short term | 11.76 (22.573) | 28.68 (29.353) | .020 | .005b |
| Early range short term | 10.10 (18.039) | 24.84 (24.481) | .030 | .003b |
| Midrange short term | 1.48 (4.215) | 3.74 (5.440) | .050 | .039c |
Data are reported as mean (SD) unless otherwise indicated.
Statistically significant at P < .01
Statistically significant at P < .05.
Ecological posture and movement measures that were most important for distinguishing groups included frequency of flexion and lateral flexion movements and percentages of standing and sitting periods throughout the day (Tab. 3). Differences between groups revealed that participants in group 1 were significantly taller (P = .01) and heavier (P = .043) and that more were employed full time (40%) than part time (12%) (P = .007). A greater percentage of participants in group 1 reported increased pain with end-range lumbar flexion during the in-person assessment (P = .026). With sensor-based ecological monitoring, participants in group 1 moved less frequently into lumbar flexion and lateral bending and spent less time in standing and more time in sitting (P values of <.001). More participants in group 2 were women (84%) (P = .006), more were employed part time (48%) than full time (16%) (P = .007), and more had CLBP lasting 5 years or more (71%) (P = .008). Participants in group 2 moved more frequently into lumbar flexion and lateral bending and spent more time standing and less time sitting (P values of <.001), as determined with sensor-based ecological monitoring. There were no significant group differences in Brief Pain Inventory pain intensity (P = .602) or interference (P = .110) or in LBP-related disability on the modified Oswestry Disability Index (P = .173).
Role of the Funding Source
The funders played no role in the design, conduct, or reporting of this study.
Discussion
This study aimed to examine the interplay of in-person and ecological measures of posture and movement using mobile sensors, movement-evoked pain, and psychological factors to identify 2 distinct clinical phenotypes among Hispanic/Latino people with CLBP. Sensor measures of ecological posture and movement were most important for classifying participants, including frequency of lumbar flexion and lateral flexion movements, and prolonged standing and sitting throughout the day. Of the 25 variables that best distinguished groups (Fig. 3), 76% were lumbar spine movements during ecological monitoring, whereas only 16% were related to generalized postures during ecological monitoring (time sitting and standing) and 8% were related to spine movements and movement-evoked pain during the in-person assessment. One group was distinguished by significantly greater height and weight and displayed more sedentary posture and movement during daily activities despite being more often employed full time (group 1). More participants in this group reported an increase in pain with end-range trunk flexion movements and displayed less frequent lumbar flexion movement during ecological monitoring. Collectively, these data suggest that movement-evoked pain may have influenced daily movement in group 1. The second group was composed of more women than men, reported a longer duration of LBP, and displayed a higher frequency of lumbar movements and a longer duration of standing postures during ecological monitoring despite being more often employed part time (group 2). The 2 identified groups had similar levels of pain-related disability and interference, but perhaps with different underlying mechanisms, suggesting that sensors may provide important information above and beyond patient-reported clinical outcomes.
Identification of these clinical phenotypes, distinguished based on ecological monitoring of posture and movement, highlights the importance of gathering ecological data on posture and movement to provide a basis for developing a more personalized plan of care. For group 1, interventions may include recommendations for increased movement while managing the associated pain, whereas for group 2, addressing higher frequency of movement and prolonged standing postures with adequate rest periods to reduce cumulative loads on the spine may be appropriate. In general, studies of interventions that include active components and exercise63 or that include aerobic exercise64 are more effective than passive interventions or no intervention for people with CLBP, but effect sizes are small. Our findings may suggest that general recommendations for increased movement may not be indicated for all patients, but rather more specific attention to modification of frequency and duration of specific postures and movements across the day may be an important focus of physical therapist intervention. Future research is needed to examine whether these sensor-based measures and clinical phenotypes can be used clinically to direct care, and to what extent individualized interventions for these different clinical phenotypes are effective. In a pilot clinical trial, investigators reported that individualized interventions based on feedback on posture and movement using mobile sensors were more effective than guidelines-based care.65
The use of sensors for ecological measures of lumbar spine posture and movement throughout the day in Hispanic/Latino people with CLBP is novel. Most prior studies have been limited to assessment of posture and movement in a laboratory or clinical setting, under the supervision of a trained clinician or investigator, which may not allow for a person to move as they naturally would during functional activities throughout a typical day. Furthermore, many prior studies examined participants with CLBP in only 1 or 2 planes of motion and for a preselected movement or sequence of movements.15 However, these conditions may not accurately reflect the conditions and physical demands of a person’s real-life environment. Additionally, because of the heterogeneity of posture and movement factors that may contribute to a person’s experience of CLBP, prior studies may have missed identifying the particular posture and movement behavior that is related to the LBP problem for an individual participant. Our study’s use of ecological monitoring with sensor-based technology aimed to better characterize movement behavior and identify the postures and movements that are relevant to individual participants in their natural environment.
Relative to ecological measures, few in-person measures of posture and movement, movement-evoked pain, or psychological factors were important for distinguishing subgroups. Although pain catastrophizing and fear of movement have been identified as factors associated with posture and movement in people with CLBP, these psychological measures did not distinguish clinical phenotypes in Hispanic/Latino people with CLBP. These data are consistent with a prior study in which the prevalence of high scores on psychological measures was distributed equally among subgroups using 3 different clinical classification systems.38 Fear of movement is commonly addressed in the examination and treatment of CLBP, and there is evidence to support a positive relationship between fear of movement and pain-related disability in individuals with CLBP.32,66 However, emerging evidence contradicts the link between fear of movement and activity behaviors. Specifically with respect to ecological measures, Carvahlo et al reported that physical activity levels measured objectively with an accelerometer were not associated with fear of movement among 119 participants with nonspecific CLBP.67 Demoulin et al also reported no correlation between pain-related fear and physical capacity with 3 specific spine tests assessing trunk extensor flexibility, strength, and endurance.68 Collectively, these data may suggest that psychological factors may need to be considered for individual patients independent of their relationship to posture and movement when developing the plan of care.
There are several limitations of the current study. First, because this was a cross-sectional study, our analysis is based on a single time point and does not account for potential changes in posture and movement or pain over time. However, changes in posture and movement and pain will be evaluated as secondary outcomes in our ongoing clinical trial of the same cohort. Second, although sensors have established validity for measuring lumbar spine movement in all planes and during functional tasks, sensor measures of lumbar spine movement cannot be validated outside of the laboratory because no gold standard measure exists for measuring lumbar spine movement in an ecological setting. Thus, the results of this study related to these ecological measures of generalized postures should be interpreted with caution. Future studies could examine the validity of generalized ecological measures (ie, time sitting, standing, frequency of movement) that are possible outside of the laboratory. A third limitation is that because all participants were Hispanic/Latino, this affects the generalizability of our results to other racial and ethnic groups and did not allow us to examine differences between racial and ethnic groups. However, to our knowledge, this is the first study to characterize posture and movement in Hispanic/Latino people with CLBP. Also, because all participants had CLBP, we were unable to identify differences between Hispanic/Latino people with and without LBP. However, we did identify clinical phenotypes in Hispanic/Latino people with CLBP that could help direct treatment. Although ecological monitoring is a novel aspect of this study, we did not record environmental factors that could have influenced movement, such as activities performed during the workday or during nonworkdays, which might influence day-to-day variability of movement. However, based on available data, ecological measures taken during workdays versus non-workdays did not differ between subgroups. Furthermore, more participants in group 1 who displayed less and less frequent lumbar movement were working full time, and more participants in group 2 who displayed more and more frequent lumbar movements were working part time. Future studies could further evaluate the influence of workday and nonworkday activities throughout the day on lumbar spine posture and movement, or conduct multiple days of ecological monitoring including both workdays and nonworkdays. Last, a random forest analysis was utilized to cluster and classify participants using the important variables and not by examining associations among variables. A limitation of the random forest is that it cannot be used to describe relationships within data that are possible with correlational analyses.
Conclusion
This study identified 2 distinct clinical phenotypes of Hispanic/Latino people with CLBP using sensor-based in-person and ecological measures of posture and movement, movement-evoked pain, and psychological factors. These findings support a multidimensional and individualized approach to the assessment of factors associated with CLBP in Hispanic/Latino people that can be addressed during intervention. The goal is to optimize management of CLBP by guiding clinicians toward more personalized intervention strategies based on clinical phenotypes.
Supplementary Material
Contributor Information
Sara P Gombatto, Doctor of Physical Therapy Program, Department of Exercise and Nutritional Sciences, San Diego State University, San Diego, California, USA; SDSU HealthLINK Center for Transdisciplinary Health Disparities Research, San Diego, California, USA.
Barbara Bailey, Department of Mathematics and Statistics, San Diego State University, San Diego, California, USA.
Monica Bari, Doctor of Physical Therapy Program, Department of Exercise and Nutritional Sciences, San Diego State University, San Diego, California, USA.
Juna Bouchekara, Doctor of Physical Therapy Program, Department of Exercise and Nutritional Sciences, San Diego State University, San Diego, California, USA.
Alyssa Holmes, Doctor of Physical Therapy Program, Department of Exercise and Nutritional Sciences, San Diego State University, San Diego, California, USA.
Stephanie Lenz, Doctor of Physical Therapy Program, Department of Exercise and Nutritional Sciences, San Diego State University, San Diego, California, USA.
Kerry Simmonds, Doctor of Physical Therapy Program, Department of Exercise and Nutritional Sciences, San Diego State University, San Diego, California, USA.
Alexandra Vonarb, Doctor of Physical Therapy Program, Department of Exercise and Nutritional Sciences, San Diego State University, San Diego, California, USA.
Kim Whelehon, Doctor of Physical Therapy Program, Department of Exercise and Nutritional Sciences, San Diego State University, San Diego, California, USA.
Cristina Rangel Batalla, SDSU HealthLINK Center for Transdisciplinary Health Disparities Research, San Diego, California, USA.
Katrina S Monroe, Doctor of Physical Therapy Program, Department of Exercise and Nutritional Sciences, San Diego State University, San Diego, California, USA; SDSU HealthLINK Center for Transdisciplinary Health Disparities Research, San Diego, California, USA.
Author Contributions
S.P. Gombatto and K.S. Monroe were involved in the conceptualization, funding acquisition, investigation, methodology, project administration, data curation and formal analysis, and writing of the original draft, review and editing.
B. Bailey was involved with data curation and formal analysis, visualization, and writing of the original draft, review, and editing.
C. Rangel Batalla was involved with data curation, and writing of the original draft, review, and editing.
M. Bari, J. Bouchekara, A. Holmes, S. Lenz, K. Simmonds, Al. Vonarb, K. Whelehon were involved with conceptualization, data curation and formal analysis, and writing of the original draft, review, and editing.
All authors read and approved the final manuscript prior to submission.
Ethics Approval
This study was approved and is being monitored by the San Diego State University Institutional Review Board (HS-2021-0121).
Funding
Research reported in this manuscript was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number U54MD012397. REDCap Cloud services at SDSU are supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Numbers S21MD010690 (SDSU HealthLINK Endowment) and U54MD012397 (SDSU HealthLINK Center).
Clinical Trial Registration
This study is a cross-sectional, observational secondary analysis of baseline data from an ongoing randomized clinical trial (Protocol ID: 228489; NCT05005416).
Disclosure and Presentations
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The abstract for this study was presented at the APTA Combined Sections Meeting; February 22–25, 2023; San Diego, CA; and published online at JOSPT (https://www.jospt.org/doi/10.2519/jospt.2023.53.2.CSM55).
References
- 1. Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354:581–585. 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 2. Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J. 2003;12:149–165. 10.1007/s00586-002-0508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. D, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LO. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ. 2012;184:E613–E624. 10.1503/cmaj.111271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hoy D, Roth A, Viney K, Souares Y, Lopez AD. Findings and implications of the Global Burden of Disease 2010 Study for the Pacific Islands. Prev Chronic Dis. 2014;11:E75. 10.5888/pcd11.130344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ritzwoller DP, Crounse L, Shetterly S, Rublee D. The association of comorbidities, utilization and costs for patients identified with low back pain. BMC Musculoskelet Disord. 2006;7:72. 10.1186/1471-2474-7-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88:21–24. 10.2106/JBJS.E.01273. [DOI] [PubMed] [Google Scholar]
- 7. Shmagel A, Foley R, Ibrahim H. Epidemiology of chronic low back pain in US adults: data from the 2009-2010 National Health and Nutrition Examination Survey. Arthritis Care Res. 2016;68:1688–1694. 10.1002/acr.22890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Carey TS, Freburger JK, Holmes GM et al. Race, care seeking, and utilization for chronic back and neck pain: population perspectives. J Pain. 2010;11:343–350. 10.1016/j.jpain.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hispanic Community Health Study / Study of Latinos. Accessed August 21, 2023. https://sites.cscc.unc.edu/hchs/StudyOverview.
- 10. Kearney GD, Allen DL, Balanay JA, Barry P. A descriptive study of body pain and work-related musculoskeletal disorders among Latino farmworkers working on sweet potato farms in eastern North Carolina. J Agromedicine. 2016;21:234–243. 10.1080/1059924X.2016.1178613. [DOI] [PubMed] [Google Scholar]
- 11. Bazargan M, Loeza M, Ekwegh T et al. Multi-dimensional impact of chronic low back pain among underserved African American and Latino older adults. Int J Environ Res Public Health. 2021;18:7246. 10.3390/ijerph18147246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Roseen EJ, Smith CN, Essien UR et al. Racial and ethnic disparities in the incidence of high-impact chronic pain among primary care patients with acute low back pain: a cohort study. Pain Med. 2023;24:633–643. 10.1093/pm/pnac193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. George SZ, Fritz JM, Silfies SP et al. Interventions for the management of acute and chronic low back pain: revision 2021. J Orthop Sports Phys Ther. 2021;51:CPG1–CPG60. 10.2519/jospt.2021.0304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Laird RA, Gilbert J, Kent P, Keating JL. Comparing lumbo-pelvic kinematics in people with and without back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2014;15:229. 10.1186/1471-2474-15-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wernli K, Tan JS, O'Sullivan P, Smith A, Campbell A, Kent P. Does movement change when low back pain changes? A systematic review. J Orthop Sports Phys Ther. 2020;50:664–670. 10.2519/jospt.2020.9635. [DOI] [PubMed] [Google Scholar]
- 16. Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom N. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. Arch Phys Med Rehabil. 2003;84:313–322. 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- 17. Laird RA, Keating JL, Kent P. Subgroups of lumbo-pelvic flexion kinematics are present in people with and without persistent low back pain. BMC Musculoskelet Disord. 2018;19:309. 10.1186/s12891-018-2233-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Karayannis NV, Jull GA, Hodges PW. Movement-based subgrouping in low back pain: synergy and divergence in approaches. Physiotherapy. 2016;102:159–169. 10.1016/j.physio.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 19. Werneke MW, Hart D, Oliver D et al. Prevalence of classification methods for patients with lumbar impairments using the McKenzie syndromes, pain pattern, manipulation, and stabilization clinical prediction rules. J Man Manip Ther. 2010;18:197–204. 10.1179/106698110X12804993426965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom NJ. Movement system impairment-based categories for low back pain: stage 1 validation. J Orthop Sports Phys Ther. 2003;33:126–142. 10.2519/jospt.2003.33.3.126. [DOI] [PubMed] [Google Scholar]
- 21. Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine (Phila Pa 1976). 2003;28:1363–1371. 10.1097/01.BRS.0000067115.61673. [DOI] [PubMed] [Google Scholar]
- 22. Dankaerts W, O'Sullivan PB, Burnett AF, Straker LM. The use of a mechanism-based classification system to evaluate and direct management of a patient with non-specific chronic low back pain and motor control impairment—a case report. Man Ther. 2007;12:181–191. 10.1016/j.math.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 23. Gombatto SP, D'Arpa N, Landerholm S et al. Differences in kinematics of the lumbar spine and lower extremities between people with and without low back pain during the down phase of a pick up task, an observational study. Musculoskelet Sci Pract. 2017;28:25–31. 10.1016/j.msksp.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 24. Hernandez A, Gross K, Gombatto S. Differences in lumbar spine and lower extremity kinematics during a step down functional task in people with and people without low back pain. Clin Biomech. 2017;47:46–52. 10.1016/j.clinbiomech.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 25. Mitchell K, Porter M, Anderson L et al. Differences in lumbar spine and lower extremity kinematics in people with and without low back pain during a step-up task: a cross-sectional study. BMC Musculoskelet Disord. 2017;18:369. 10.1186/s12891-017-1721-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Trudelle-Jackson E, Fleisher LA, Borman N, MorrowJR Jr, Frierson GM. Lumbar spine flexion and extension extremes of motion in women of different age and racial groups: the WIN study. Spine (Phila Pa 1976). 2010;35:1539–1544. 10.1097/BRS.0b013e3181b0c3d1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Been E, Kalichman L. Lumbar lordosis. Spine J. 2014;14:87–97. 10.1016/j.spinee.2013.07.464. [DOI] [PubMed] [Google Scholar]
- 28. Arima H, DimarJR 2nd, Glassman SD et al. Differences in lumbar and pelvic parameters among African American, Caucasian and Asian populations. Eur Spine J. 2018;27:2990–2998. 10.1007/s00586-018-5743-5. [DOI] [PubMed] [Google Scholar]
- 29. Laird RA, Keating JL, Ussing K, Li P, Kent P. Does movement matter in people with back pain? Investigating 'atypical' lumbo-pelvic kinematics in people with and without back pain using wireless movement sensors. BMC Musculoskelet Disord. 2019;20:28. 10.1186/s12891-018-2387-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hodges PW, van den HoornW. A vision for the future of wearable sensors in spine care and its challenges: narrative review. J Spine Surg. 2022;8:103–116. 10.21037/jss-21-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ferguson SAB, Berner RS, Bridger MA et al. Patient and practitioner experience with clinical lumbar motion monitor wearable technology. Heal Technol. 2019;9:289–295. 10.1007/s12553-019-00330-7. [DOI] [Google Scholar]
- 32. Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80:329–339. 10.1016/s0304-3959(98)00229-2. [DOI] [PubMed] [Google Scholar]
- 33. Linton SJ. Do psychological factors increase the risk for back pain in the general population in both a cross-sectional and prospective analysis? Eur J Pain. 2005;9:355–361. 10.1016/j.ejpain.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 34. Marshall PWM, Schabrun S, Knox MF. Physical activity and the mediating effect of fear, depression, anxiety, and catastrophizing on pain related disability in people with chronic low back pain. PLoS One. 2017;12:e0180788. 10.1371/journal.pone.0180788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rabey M, Smith A, Beales D, Slater H, O'Sullivan P. Differing psychologically derived clusters in people with chronic low back pain are associated with different multidimensional profiles. Clin J Pain. 2016;32:1015–1027. 10.1097/AJP.0000000000000363. [DOI] [PubMed] [Google Scholar]
- 36. Beneciuk JM, Robinson ME, George SZ. Low back pain subgroups using fear-avoidance model measures: results of a cluster analysis. Clin J Pain. 2012;28:658–666. 10.1097/AJP.0b013e31824306ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Al-Obaidi SM, Al-Zoabi B, Al-Shuwaie N, Al-Zaabie N, Nelson RM. The influence of pain and pain-related fear and disability beliefs on walking velocity in chronic low back pain. Int J Rehabil Res. 2003;26:101–108. 10.1097/00004356-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 38. Karayannis NV, Jull GA, Nicholas MK, Hodges PW. Psychological features and their relationship to movement-based subgroups in people living with low back pain. Arch Phys Med Rehabil. 2018;99:121–128. 10.1016/j.apmr.2017.08.493. [DOI] [PubMed] [Google Scholar]
- 39. Gagnon CM, Matsuura JT, Smith CC, Stanos SP. Ethnicity and interdisciplinary pain treatment. Pain Pract. 2014;14:532–540. 10.1111/papr.12102. [DOI] [PubMed] [Google Scholar]
- 40. Cleeland CS, Ryan KM. Pain assessment: global use of the brief pain inventory. Ann Acad Med Singap. 1994;23:129–138. [PubMed] [Google Scholar]
- 41. Song C, Lin S, Huang C, Wu HC, Chen CH, Hsieh CL. Validation of the brief pain inventory in patients with low back pain. Spine (Phila Pa 1976). 2016;41:E937–E942. 10.1097/BRS.0000000000001478. [DOI] [PubMed] [Google Scholar]
- 42. Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain. 2004;20:309–318. 10.1097/00002508-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 43. Butera KA, Lentz TA, Beneciuk JM, George SZ. Preliminary evaluation of a modified STarT back screening tool across different musculoskeletal pain conditions. Phys Ther. 2016;96:1251–1261. 10.2522/ptj.20150377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mansbach WE, Mace RA, Clark KM. Differentiating levels of cognitive functioning: a comparison of the Brief Interview for Mental Status (BIMS) and the Brief Cognitive Assessment Tool (BCAT) in a nursing home sample. Aging Ment Health. 2014;18:921–928. 10.1080/13607863.2014.899971. [DOI] [PubMed] [Google Scholar]
- 45. Poquet N, Lin C. The brief pain inventory (BPI). J Physiother. 2016;62:52. 10.1016/j.jphys.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 46. Fairbank JC, Pynsent PB. The Oswestry disability index. Spine (Phila Pa 1976). 2000;25:2940–2952discussion 2952. 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 47. Fritz JM, Irrgang JJ. A comparison of a modified Oswestry low back pain disability questionnaire and the Quebec back pain disability scale. Phys Ther. 2001;81:776–788. 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 48. Brodke DS, Goz V, Lawrence BD, Spiker WR, Neese A, Hung M. Oswestry disability index: a psychometric analysis with 1,610 patients. Spine J. 2017;17:321–327. 10.1016/j.spinee.2016.09.020. [DOI] [PubMed] [Google Scholar]
- 49. Lee CP, Fu TS, Liu CY, Hung CI. Psychometric evaluation of the Oswestry disability index in patients with chronic low back pain: factor and Mokken analyses. Health Qual Life Outcomes. 2017;15:192. 10.1186/s12955-017-0768-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sullivan MJL, Bishop SR, Pivik, J. The Pain Catastrophizing Scale: Development and validation. Psych Assess. 1995; 7:524–532. 10.1037/1040-3590.7.4.524. [DOI]
- 51. Wheeler CHB, Williams ACC, Morley SJ. Meta-analysis of the psychometric properties of the pain catastrophizing scale and associations with participant characteristics. Pain. 2019;160:1946–1953. 10.1097/j.pain.0000000000001494. [DOI] [PubMed] [Google Scholar]
- 52. Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O'Neill E. Factor structure, reliability, and validity of the Pain Catastrophizing Scale. J Behav Med. 1997;20:589–605. 10.1023/A:1025570508954. [DOI] [PubMed] [Google Scholar]
- 53. Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 54. Swinkels-Meewisse EJ, Swinkels RA, Verbeek AL, Vlaeyen JW, Oostendorp RA. Psychometric properties of the Tampa Scale for kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Man Ther. 2003;8:29–36. 10.1054/math.2002.0484. [DOI] [PubMed] [Google Scholar]
- 55. Ronchi AJ, Lech M, Taylor NF, Cosic I. A reliability study of the new back strain monitor based on clinical trials. Annu Int Conf IEEE Eng Med Biol Soc. 2008;2008:693–696. 10.1109/IEMBS.2008.4649247. [DOI] [PubMed] [Google Scholar]
- 56.Charry E, Umer M, and Taylor S. Design and validation of an ambulatory inertial system for 3-D measurements of low back movements, presented at: 2011 Seventh International Conference on Intelligent Sensors, Sensor Networks and Information Processing; (2011). Adelaide, SA, Australia.
- 57. Mjosund HL, Boyle E, Kjaer P, Mieritz RM, Skallgard T, Kent P. Clinically acceptable agreement between the ViMove wireless motion sensor system and the Vicon motion capture system when measuring lumbar region inclination motion in the sagittal and coronal planes. BMC Musculoskelet Disord. 2017;18:124. 10.1186/s12891-017-1489-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chang RP, Smith A, Kent P et al. Concurrent validity of DorsaVi wireless motion sensor system version 6 and the Vicon motion analysis system during lifting. BMC Musculoskelet Disord. 2022;23:909. 10.1186/s12891-022-05866-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Breiman L. Random forests. Mach Learn. 2001;45:5–32. 10.1023/A:1010933404324. [DOI] [Google Scholar]
- 60. Conrad DJ, Bailey BA. Multidimensional clinical phenotyping of an adult cystic fibrosis patient population. PLoS One. 2015;10:e0122705. 10.1371/journal.pone.0122705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Rousseeuw PJ. Silhouettes: a graphical aid to the interpretation and validation of cluster analysis. J Comput Appl Math. 1987;20:53–65. 10.1016/0377-0427(87)90125-7. [DOI] [Google Scholar]
- 62. Team RC. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2021. https://www.R-project.org/.
- 63. Hayden JA, Ellis J, Ogilvie R, Malmivaara A, van TulderMW. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev. 2021;2021:CD009790. 10.1002/14651858.CD009790.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Meng XG, Yue SW. Efficacy of aerobic exercise for treatment of chronic low back pain: a meta-analysis. Am J Phys Med Rehabil. 2015;94:358–365. 10.1097/PHM.0000000000000188. [DOI] [PubMed] [Google Scholar]
- 65. Kent P, Laird R, Haines T. The effect of changing movement and posture using motion-sensor biofeedback, versus guidelines-based care, on the clinical outcomes of people with sub-acute or chronic low back pain-a multicentre, cluster-randomised, placebo-controlled, pilot trial. BMC Musculoskelet Disord. 2015;16:131. 10.1186/s12891-015-0591-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. George SZ, Calley D, Valencia C, Beneciuk JM. Clinical investigation of pain-related fear and pain catastrophizing for patients with low back pain. Clin J Pain. 2011;27:108–115. 10.1097/AJP.0b013e3181f21414. [DOI] [PubMed] [Google Scholar]
- 67. Carvalho FA, Maher CG, Franco MR et al. Fear of movement is not associated with objective and subjective physical activity levels in chronic nonspecific low back pain. Arch Phys Med Rehabil. 2017;98:96–104. 10.1016/j.apmr.2016.09.115. [DOI] [PubMed] [Google Scholar]
- 68. Demoulin C, Huijnen IP, Somville PR et al. Relationship between different measures of pain-related fear and physical capacity of the spine in patients with chronic low back pain. Spine J. 2013;13:1039–1047. 10.1016/j.spinee.2013.02.037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.