Abstract
Coronavirus disease 2019 (COVID-19), a systemic illness caused by severe acute respiratory distress syndrome 2 (SARS-CoV-2), has triggered a worldwide pandemic with symptoms ranging from asymptomatic to chronic, affecting practically every organ. Melatonin, an ancient antioxidant found in all living organisms, has been suggested as a safe and effective therapeutic option for the treatment of SARS-CoV-2 infection due to its good safety characteristics and broad-spectrum antiviral medication properties. Melatonin is essential in various metabolic pathways and governs physiological processes, such as the sleep-wake cycle and circadian rhythms. It exhibits oncostatic, anti-inflammatory, antioxidant and anti-aging properties, exhibiting promise for use in the treatment of numerous disorders, including COVID-19. The preventive and therapeutic effects of melatonin have been widely explored in a number of conditions and have been well-established in experimental ischemia/reperfusion investigations, particularly in coronary heart disease and stroke. Clinical research evaluating the use of melatonin in COVID-19 has shown various improved outcomes, including reduced hospitalization durations; however, the trials are small. Melatonin can alleviate mitochondrial dysfunction in COVID-19, improve immune cell function and provide antioxidant properties. However, its therapeutic potential remains underexplored due to funding limitations and thus further investigations are required.
Keywords: melatonin, COVID-19, long COVID-19, mitochondrial dysfunction, antioxidant
1. Introduction
Severe acute respiratory coronavirus 2 (SARS-CoV-2) is the causative agent of the viral disease known as coronavirus disease 2019 (COVID-19). This illness was first identified in December 2019 in Wuhan, China, and has since spread throughout the globe, culminating in a pandemic (1-3). COVID-19 is a systemic disease that may present in a broad variety of clinical manifestations, ranging from patients who are asymptomatic to those who have significant respiratory symptoms and even conditions that are life-threatening (3-5). There are several underlying mechanisms and interactions with pre-existing conditions, such as obesity among others, that drive the pathogenesis of the disease, which includes the activation or dysregulation of localized (for example, vascular) and widespread inflammation, ultimately resulting in the failure of several organs and eventually, mortality (2,4,6-16).
With the pandemic now characterized passed the acute phase, attention is shifting to post-acute sequelae of COVID-19 (PASC), is often referred to as 'long COVID' and possible preventative and therapeutic approaches are warranted (17,18). PACS comprises from a variety of symptoms and clinical manifestations, which may include persistent tiredness, respiratory symptoms (including dyspnea, cough, chest tightness), joint rigidness, impaired smell and headache, whereas respiratory, cardiovascular, neurological, cognitive, psychiatric and gastrointestinal manifestations continue to be the most common and potentially gravest, presentations of PASC (17,19-21). Recent evidence suggests that a number of these manifestations may be linked to an unfavorable impact of the disease on the mitochondrial function of various tissues and organs (18,22).
Considering the numerous mechanisms and pathophysiological processes that spread from the deregulation of the immune system in acute COVID-19 and the potential mitochondrial basis of long COVID, an ideal and efficient therapeutic option could be a molecule which functionally behaves as a 'Swiss Army Knife', such as melatonin (23,24). Indeed, since the SARS-CoV-2 was classified as a pandemic, numerous studies have proposed that the use of melatonin should be investigated as a treatment option that is both safe and likely to be effective with regard to treating the infection (17,25-27). Its usage is justified not just by its superior safety profile, but also from its innumerable beneficial actions as already reviewed extensively elsewhere (27-30) and it has been demonstrated to even possess broad-spectrum antiviral drug characteristics (31,32). Moreover, various potentially harmful and costly repurposed medicines, such as colchicine, glucocorticoids, remdesivir and several others, have been advocated for or utilized as therapeutic options (25,27,33-37). Additionally, despite their importance, even the presently available vaccinations have major adverse effects on occasion (38,39). Furthermore, as the virus has evolved, the efficiency of the immunizations has reduced, several strains have already been found, and more are expected to emerge, reducing the efficacy of vaccinations even further (40). All these factors underlie the need for further therapeutic options despite the various preventive and already utilized medicinal options.
The present review provides a summary of the features of melatonin that provide support to its use in the treatment and/or prevention of SARS-CoV-2 infection and its complications. The present review initially presents several actions of melatonin in health and disease, followed by the key pathophysiological mechanisms of COVID-19 and the potential mechanisms through which melatonin would interact and mitigate them, with a focus on long COVID and the mitochondrial functions of melatonin.
Finally, the results of the available clinical trials examining the use of melatonin in individuals with COVID-19 are summarized, and future steps on further examining the use of melatonin are proposed.
2. Melatonin in health and disease
Melatonin is an ubiquitous molecule that can be found in all living organisms of the animal kingdom, with traces even found in higher plants, such as fruits, seeds and leaves. The term 'melatonin' originates from the Greek words 'melas', which means black or dark, and 'tonos', which means color or tune. Melatonin is ultimately used to describe the hormone that is responsible for darkness (41-44). It has been preserved over the course of evolution, perhaps for these and numerous other additional features, and it is regarded to be an evolutionarily old antioxidant, as it has the ability to scavenge free radicals and stimulate antioxidant enzymes (44-47). Melatonin is primarily synthesized and secreted (predominantly released at night) by the pineal gland via the process of hydroxylation of the essential amino acid tryptophan, whereas tryptophan hydroxylase is responsible for the formation of 5-hydroxytryptophan (42,43,45,47-49). Serotonin, also known as 5-hydroxytryptamine, is the neurotransmitter that is produced as a result of this process. Melatonin is the immediate precursor of serotonin (42,43,45,47,48). Other organs, including the retina, kidneys, gastrointestinal system, skin and lymphocytes, produce a modest amount of melatonin (42,43,45,47,48). The role of melatonin in various biosynthetic metabolic pathways is evident, with different species having distinct biosynthetic pathways and genes that encode the enzymes involved in the process of its biosynthesis (42,43,45,47,48). Hydoxyindole-O-methyltransferase, an enzyme that is indirectly controlled by the photo-neural system, is responsible for regulating the production of melatonin (42,43,45,47,48). Melatonin is primarily synthesized at night and is bound to albumin and orosomucoid glycoprotein and through the process of crossing the blood-brain barrier, it is able to go to all tissues in the body and regulate brain function (43,50,51). Melatonin production peaks at 3 months of age and decreases by 80% by the adult stage (43).
Melatonin is primarily considered to govern physiological processes, such as circadian rhythms in humans, the sleep-wake cycle, and it may be used as a natural sleep aid (43,45,52-54). It is a pleiotropic hormone that regulates several biological processes, including the release of other hormones, apoptosis and immunological responses (32,49,55,56). The effects of melatonin are mediated in various cells via either the melatonin receptors type 1 and type 2, G-protein coupled (membrane-independent pathway) or indirectly (membrane independent) with nuclear orphan receptors from either the RAR-related orphan receptor α/Z receptor family or through other pathways, as extensively reviewed elsewhere (57). The oncostatic, anti-inflammatory and antioxidant characteristics of melatonin indicate that it may have potential use in the treatment of a variety of disorders (32,43,58). Both the preventative and therapeutic benefits of melatonin have been the subject of substantial research in a variety of neurological conditions, including Alzheimer's disease, Parkinson's disease, Huntington's disease, amyotrophic lateral sclerosis, multiple sclerosis and epilepsy (47,59-62). In lipopolysaccharide-induced depression, melatonin has been shown to exert antidepressant effects, which are mediated via the regulation of autophagy (63). Additionally, it exhibits anti-aging properties and has the potential for use in the management and treatment of age-related disorders in human beings (55,64,65).
Melatonin has been widely investigated for its anti-proliferative and anti-apoptotic properties on cancer cells, revealing its oncostatic effects. Melatonin also reduces the loss of cells, which is a significant benefit (66,67). Melatonin, which has been found in both in vitro and in vivo studies, has been shown to inhibit the development of tumors through membrane-independent and membrane-dependent mechanisms. Melatonin has an effect on cancer during the initiation phase, such as through DNA repair, and in the development, progression and metastasis phases, of the tumorigenesis process (66-68). Melatonin has potent anti-angiogenic, anti-proliferative and ultimately anti-metastatic properties that may be used in the treatment of a wide range of malignancies, particularly those that have a high risk of cancer spreading to other parts of the body. Additionally, it exerts synergistic effects with conventional therapy, which increases the vulnerability of cancer cells to apoptosis (66-68). Melatonin significantly reduces the adverse effects of cardiotoxic drugs in patients with cancer and has been shown to have a beneficial effect on coagulopathy (49). Melatonin has been found to improve cardiac function and lower blood pressure in patients who have hypertension, according to clinical data from human studies and various lines of evidence from animal studies, which have been reviewed elsewhere (52,60,69-71). Melatonin, a substance that neutralizes free radicals, has been utilized to mitigate the harmful effects of certain chemical compounds, such as methamphetamine (42,50,60,72-74). The use of melatonin as a possible anti-viral drug for the treatment of viral illnesses, such as Ebola and COVID-19 has been suggested (27,31,75). As extensively reviewed elsewhere (31), melatonin exhibits a plethora of potential antiviral actions in various viral models (31,75), including the regulation of viral phase separation and epitranscriptomics in long COVID-19 (17).
Studies have indicated that the anti-inflammatory properties of melatonin involve suppressing interferon (IFN)-α, tumor necrosis factor α (TNF-α), interleukin (IL)-6 and IL-8, inhibiting Janus kinase (JNK) phosphorylation and monocyte chemoattractant protein-1, and promoting protein degradation for tight junction integrity, according to numerous studies (56,76-81). During the catastrophic hemorrhage that occurs during the late phase of Ebola virus infection, melatonin plays a crucial role in preserving the integrity of the blood vessels and shielding endothelial cells from damage (31,75,78,82,83). It also exhibits various biological activities, such as neuroprotective and immunomodulatory effects, regulatory effects on reproduction, tumor preventive effects, protective effects on gastrointestinal function and anti-aging effects (45,84).
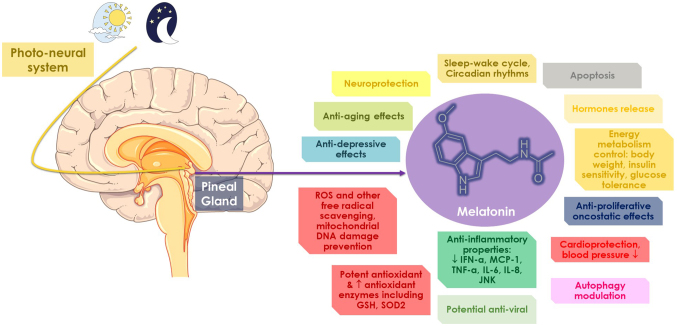
Melatonin is also a key factor in the regulation of energy homeostasis, which includes the regulation of body weight, insulin sensitivity and glucose tolerance of the body (45,85). It regulates energy metabolism, affecting intake, flow and expenditure in the energy balance, which in turn may be critical for preventing a variety of dysmetabolic conditions, particularly obesity, which in turn can affect the outcome of patients with COVID-19 (11,86-89). In addition to this, it synchronizes the needs for energy metabolism with the daily and yearly cyclical environmental photoperiod by means of its chronobiotic and seasonal effects (45,85). In experimental ischemia/reperfusion research, particularly in cases of myocardial infarction and stroke, melatonin has been shown to successfully prevent oxidative damage and the pathophysiological repercussions of such damage are essential (43,82,90,91). Of utmost importance is to further present the free radical scavenging properties of melatonin, as these protect against mitochondrial DNA damage induced by reactive oxygen species (ROS) displaying another of its significant effects on mitochondrial homeostasis (24,92,93). In preclinical studies, the administration of melatonin has been shown to increase the activity of several antioxidant markers/enzymes, including glutathione peroxidase and superoxide dismutase 2 (SOD2). The latter was achieved by promoting the function of sirtuin 3, that deacetylates SOD2, essentially facilitating its activation (24,92,94-97). Whether melatonin is present in the mitochondria has been debatable (24,92); however, experimental evidence demonstrates up to 100-fold higher levels of melatonin within the mitochondria post-administration on mitochondrial membranes (98). It appears that the highest concentration of melatonin occurs in the mitochondria, where the highest amount of ROS and oxidative stress occur (99). High amounts of melatonin in the mitochondria may be due to oligopeptide transporters 1/2 or mitochondria generating their own melatonin, with research indicating the existence of such enzymes in brain mitochondria (92,94,100-102). The effects of melatonin on mitochondria may be mediated via MT1/2 receptors, resulting in decreased ROS generation, higher antioxidant capabilities, and therefore, in less neural apoptosis, activating nuclear factor erythroid 2-related factor 2, as shown in preclinical models (24,92,103,104). Melatonin additionally prevents stress-induced cytochrome c release from mitochondrial outer membranes (100). Finally, melatonin appears to increase classes of oxidative phosphorylation (OXPHOS) proteins, thereby preventing damage (105). All these mitochondria-related features of melatonin are of key relevance, apart from the acute phase of COVID-19, which is strongly associated with oxidative stress, but also long COVID, which will be discussed in the following section. Based on novel data, melatonin is related to the mitochondrial dysfunction/downregulation of vital mitochondrial markers. The physiology of melatonin is summarized in the schematic diagram in Fig. 1.
Figure 1.
A summary of the physiological properties of melatonin. Please refer to main text for further details. ROS, reactive oxygen species; IFN, interferon; IL, interleukin; JNK, Janus kinase; MCP-1, monocyte chemoattractant protein-1; TNF, tumor necrosis factor; GSH, reduced glutathione; SOD2, superoxide dismutase 2. Parts of this image were derived from the free medical site http://smart.servier.com/ (accessed on September 15, 2023) by Servier, licensed under a Creative Commons Attribution 3.0 Unported Licence.
3. Pathophysiology and long-term repercussions of COVID-19
Although individuals with COVID-19 often have modest symptoms, 20% develop substantial to severe illness that requires hospitalization (106). The most common include respiratory system abnormalities; however, several other organs may also be affected (3,7,10-12,33,34). The features of the host, viral dynamics and immune response are associated with the severity of the disease and in general, severe COVID-19, as well as a higher mortality rate are linked to an older age, high body mass index, and comorbidities such as cardiovascular diseases, diabetes or cancer (3,8,10,11,87,107,108).
The pathophysiological symptoms of COVID-19 are partly mediated by the cell entrance of the virus, which is enhanced by the binding of the viral spike peptides to the angiotensin converting enzyme 2 (ACE2) receptors in diverse organs (2,7,8,109). In humans, ACE2 is expressed in numerous organ systems and tissues, including the lungs (e.g., the pneumocytes of alveolar sacs), hepatic, cardiac tissue, kidney, gastrointestinal endothelium, adipose tissue (AT) and vascular endothelium (3,49,110,111). This wide distribution likely explains the multisystem involvement of the infection, while also enhancing the magnitude of the illness in patients afflicted by SARS-CoV-2 (49). Interstitial pneumonia, the most prevalent lung involvement in patients with COVID-19, if left untreated, may lead to a hypoxic status, resulting in acute respiratory distress syndrome and/or systemic inflammatory response syndrome and fatal multiorgan failure (3,6,13,15,37, 108,112,113). These sepsis-related consequences occur from a pathophysiological perspective, have the same underlying backgrounds, ignited by the cytokine storm and hyperinflammatory statuses with significant oxidative damage caused by the reaction of the host to SARS-CoV-2 (49,114).
It is possible that the widespread extrapulmonary damage observed in patients with COVID-19 may be attributed to the presence of ACE2 receptors on cells other than those that lining the respiratory alveoli (113). Other organ involvement results in symptoms that are particular to the organ; for example, gastrointestinal involvement may cause symptoms such as nausea, vomiting, diarrhea and abdominal pain (113). Hepatic damage, as evidenced by increased levels of circulating liver enzymes, is also prevalent (3). There are several symptoms that may be associated with peripheral and central nervous system involvement, and these include headaches and dizziness, hyposmia or anosmia (indicative of encephalopathy), neuralgia and Guillain-Barré syndrome (115,116). Hospitalized patients are more likely to experience thromboembolic events, which have been established as an independent risk factor for a poor prognosis, and acute coronary modalities, cardiomyopathies, several types of arrhythmias, pericarditis and various thromboembolic events (49,117). Infections caused by SARS-CoV-2 may also result in coagulopathies, thrombocytopenia being the most prevalent, which play a crucial role in the development of extrapulmonary complications (8,49). In critically ill patients, deep venous thrombosis and/or pulmonary embolism are frequent, with pulmonary embolism being more prevalent in patients in intensive care units (49). Inflammation, immunological responses, coagulation cascades and the dysregulation of the renin-angiotensin system may cause acute kidney damage in 25% of hospitalized patients (8,49,118). Finally, AT from individuals with obesity is hypothesized to exhibit higher amounts of ACE2, perhaps serving as a SARS-CoV-2 repository with postponed viral shedding and may presumably contribute to long COVID (3).
Long COVID refers to patients who have experienced persistent impairments following infection with COVID-19, including various organs and tissues (18,119-122). A previous retrospective analysis of 193,113 participants found an elevated risk for respiratory impairment and pulmonary function impairment after 6 months in these patients (123). The most prevalent manifestation is impaired diffusion capacity for carbon monoxide (DLCO) (124). Survivors with a critical illness had a greater risk of DLCO impairment, lower residual volume and lower total lung capacity (124,125). Notably, the risk of developing long COVID appears to differ depending on the various strains. Studies have found a lower risk of complications, intensive care unit admission, ventilation requirement and mortality rate in omicron-infected individuals compared to those infected with other variants (126). Furthermore, as compared to the delta variant, the omicron variant has been shown to be associated with a lower likelihood of developing long COVID (127).
Mutations in antigenic sites are essential for antibody and immunological evasion, and chronic symptoms in patients with long COVID-19 may be partly due to a lessening of the antibody response to vaccination or to variant resistance (17,122,128,129). Of note, >100 persistent symptoms were recorded by participants at least 4 weeks after infection, according to a scoping analysis that included 50 trials (130). It is possible for the majority of 'long-haulers' to have a relapse as a result of either physical or mental stress, and cognitive impairment or memory issues are common regardless of age (18,131). The establishment of a viral reservoir in individuals with PASC may potentially be a possible explanation for the improvement in clinical symptoms that occurred following the administration of the SARS-CoV-2 immunization (132). Reservoirs of viruses are cells or anatomical locations where the virus may persist and accumulate with better kinetic stability than the primary pool of viruses that are actively reproducing (17,133,134). There is a increasing evidence of an association between the presence of viral RNA in probable SARS-CoV-2 reservoirs in extrapulmonary organs and tissues, and the continued manifestation of symptoms in PASC (17,18,133,134). Patients who have been diagnosed with COVID for a long period of time often have reactivated viruses, which may cause mitochondrial fragmentation and disrupt energy metabolism (18,135-137). In addition, there is evidence of oxidative stress, abnormal amounts of mitochondrial proteins and deficits in tetrahydrobiopterin (138,139).
In addition to the dysregulations of inflammatory responses, COVID-19 has been connected to mitochondrial function. Mitochondria play a critical role in the control of immune responses and cellular metabolism (22,140-143). The shape of the mitochondria is altered by infection, which results in a reduction in the number of OXPHOS proteins, a reduction in the number of mitochondrial inner membrane protein import systems, and an increase in the release of mitochondrial reactive oxygen species (144-146). The SARS-CoV-2 virus is capable of binding to a variety of host proteins, with mitochondrial proteins accounting for up to 16% of the total (22,147-149). Human cells and tissues that have been infected display a decrease in the amount of proteins and transcripts of OXPHOS genes, an increase in glycolysis, a suppression of OXPHOS, an increase in mitochondrial ROS production, inflammation factors, and an increase in hypoxia inducible factor-1α (HIF-1α) and its target genes (22,144,150-155). A disruption in the process of mitochondrial protein synthesis may lead to an imbalance in the proportion of mitochondrial proteins that are coded by nuclear DNA and mitochondrial DNA, which has the potential to activate the integrated stress response and have a number of unfavorable repercussions (22). Recently, Guarnieri et al (22) demonstrated that once the viral titter peaks, this causes a systemic reaction from the host, which includes the regulation of mitochondrial gene transcription and glycolysis, ultimately resulting in an antiviral immune defense mechanism. Nevertheless, despite the fact that lung clearance and lung mitochondrial function recovery were documented, mitochondrial function in the heart, kidney, liver and lymph nodes continues to be damaged, which may result in severe COVID-19 pathology (22).
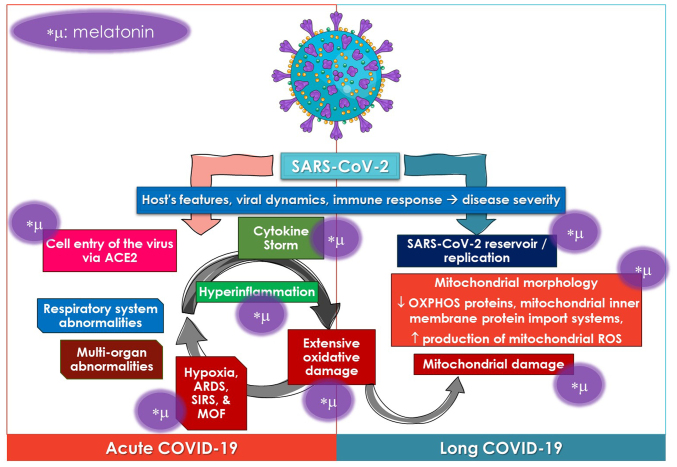
Melatonin, which is well-known for its antioxidant and anti-inflammatory qualities, has the potential to assist in overcoming the cytokine storm that is associated with virus-related infections, such as SARS-CoV-2, and may also be able to prevent mitochondrial-related chronic consequences of the disease. The anti-inflammatory and antioxidant properties of melatonin may potentially be beneficial for the treatment of possibly chronic inflammation in patients with long COVID-19. These views are discussed in the following section. The effects of melatonin on the pathophysiological mechanisms of COVID-19 are summarized in the schematic diagram in Fig. 2.
Figure 2.
Summary of the pathophysiological processes related to acute and long COVID-19 and sites of potential action of melatonin (symbolized with *μ) based on its physiopathological properties. Please refer to relevant parts of the text for further details. ACE2, angiotensin converting enzyme 2; ARDS, acute respiratory distress syndrome; MOF, multiorgan failure; OXPHOS, oxidative phosphorylation; ROS, reactive oxygen species; SIRS, systemic inflammatory response syndrome. Parts of this image were derived from the free medical site http://smart.servier.com/ (accessed on September 15, 2023) by Servier, licensed under a Creative Commons Attribution 3.0 Unported Licence.
4. Mechanisms through which melatonin can alleviate COVID-19
Melatonin supplementation has the potential to target and benefit the host by reducing the exaggeration of the innate immune system, which is essential for improving tolerance against the invasion of pathogens (156). There is a substantial association between the immunological response of the host, particularly the innate immune network, and the symptoms and the results of viral infections with the host (156,157). The overwhelming inflammatory response that is triggered by the cytokine storm is responsible for the majority of the detrimental effects caused by SARS-CoV-2 (36,114,156,157). Consequently, this excessive production of cytokines is harmful to organs and tissues, which ultimately results in oxidative damage to several organs (36,114,157,158). A considerable improvement in the outcomes of patients with SARS-CoV-2 infection may be achieved by downregulating the innate immune response and reducing the inflammatory reaction. This provides evidence for the use of this treatment method in the treatment of patients with severe COVID-19 (77,159).
Melatonin is a potent free radical scavenger and antioxidant that directly detoxifies a wide range of ROS and reactive nitrogen species (RNS). These ROS and RNS include hydroxyl radicals, peroxynitrite anion, hydrogen peroxide, superoxide anion radicals and hypoochlorous acid (25,27,50,93,160). Its electron-donating metabolites outperform traditional antioxidants, such as vitamins C and E, carotenoids, and NADH in reducing other oxidizing compounds (156,161). Additionally, melatonin has an advantageous cellular distribution due to its solubility in both water and lipids, and it may form hydrogen bonds with proteins and DNA to provide protection (60,161). Additionally, it upregulates the gene expression levels of several antioxidant enzymes, thus indirectly enhancing the cellular antioxidant capacity (161,162). By interacting on the mitochondrial metabolism, melatonin is also able to inhibit the production of ROS and RNS (60,156).
Melatonin is a potent anti-inflammatory chemical that functions by rescuing the peroxynitrite anion, which leads to the inhibition of inflammation that is not specific to any one substance, such as carrageenan or zymosan (79,163,164). Its anti-inflammatory mechanisms are diverse, including the suppression of the activity or downregulation of pro-inflammatory enzymes, such as cyclooxygenase-2, inducible nitric oxide synthase, eosinophilic peroxidase and matrix metalloproteinase 2 (MMP)2, which are responsible for the generation of inflammatory mediators (156,165-167). Furthermore, melatonin has the ability to inhibit the advancement of the NLR family pyrin domain containing 3 (NLRP3) inflammasome, which ultimately results in the activation of caspase-1 and the maturation of IL-1β and IL-18. This ultimately leads to pyroptosis, a damaging consequence of inflammation (168-170). Melatonin is able to effectively prevent the production of NLRP3 inflammasomes and reduce inflammation, both of which are connected to COVID-19. This affect is achieved by its interaction with signal transduction pathways (167-169). Melatonin has the ability to decrease the phosphorylation of IκBα, therefore reducing the translocation of NF-κB into the nucleus. This, in turn, helps to control the cytokine storm that occurs following infection with COVID-19 and may be associated with damaging inflammation (171-174). The downregulation of melatonin also stimulates autophagic capacity, which is often accompanied by a reduction in the creation of inflammasomes. This may speed up the process of tissue healing from inflammation (174,175).
Melatonin is a hormone that controls the immune system, reducing the excessive response of both the innate immune system and fostering the development of adaptive immunity (156,176). Some examples of pathogen associated molecular pattern receptors are Toll-like receptors (TLRs), Nod-like receptors (NLRs), AIM2-like receptors, GMP-AMP synthase (cGAS) and AIM2. These receptors are responsible for driving the innate immune system, which is the initial line of defense against the invasion of pathogens (156,177). Innate immune cells are able to eliminate infections with the assistance of these receptors, which are able to identify RNA, DNA, proteins and lipids that are associated with pathogens (156,177). However, their excessive responses often result in injury to the tissues. Melatonin is able to suppress the activation of TLR4, TLR9 and cGAS, which results in a reduction in the innate immune response and a reduction in the damage to tissue that is caused by infections, ischemia/reperfusion and other disturbances (156,178-180).
Innate immune cells are directly affected by melatonin, principally via the negative regulatory functions that it has (156,181). It does this by preventing ERK phosphorylation, which in turn prevents neutrophil migration and the tissue damage that is associated with it (182). The administration of melatonin lowers mast cell activation, TNF-α and IL-6 production, and IKK/NF-κB signal transduction in activated mast cells (155,182-185). Treatment with melatonin reverses the transformation from M2 anti-inflammatory macrophages to M1 pro-inflammatory subtypes, which assists in the elimination of SARS-CoV-2 and suppresses the dysfunctional hyper-inflammatory response that is mediated by M1 macrophages (156,186). Whens physiological circumstances are met, melatonin has the potential to boost innate immunity, thus maintaining its protective effects against the invasion of pathogens (31,187).
Melatonin may also have an effect on COVID-19 infection by preventing the virus from entering cells and replicating after first entry (17,25,156). There are three enzymes that are responsible for the entry of SARS-CoV-2 into cells: ACE2, transmembrane protease serine 2 and A disintegrin and metalloprotease 17 (188-190). It is possible that melatonin can target these molecules in order to delay the entry of the coronavirus into the cells (189). The progression of COVID-19 may be controlled by the circadian system, while the melatonin circadian rhythm may also be responsible for this regulation (155,188-190). It is also possible that melatonin may influence ACE2 activity in an indirect manner by binding to calmodulin or MMP9 (191). Recent research has indicated that melatonin has the potential for use as a therapeutic agent on ACE2. It has been found that transgenic mice exhibit greater vulnerability to SARS-CoV-2 infection, as well as delayed clinical signs and an enhanced survival (192,193). In addition, melatonin has the potential to decrease the activation of CD147 during a SARS-CoV-2 infection via inhibiting the production of HIF-1A (194). Research has demonstrated that melatonin may reduce the reproduction of some viruses, such as swine coronaviruses and Dengue virus, with the effectiveness of this effect being dose-dependent (195,196). Melatonin may suppress SARS-CoV-2 replication; however, to date, no animal research has shown this to be true (197). It is possible that melatonin inhibits viral replication by blocking growth factor signaling (27,198,199). Due to its uniqueness and lack of presence in host cells, the major protease (Mpro) of SARS-CoV-2 has emerged as a possible target for the development of replication inhibitors (156). According to the crystal structure of the SARS-CoV-2 Mpro and PF-07321332 complex, melatonin binds to the catalytic amino acid residues of C145 and H41 via pi-sulfur/conventional hydrogen bonds and carbon-hydrogen bonds. This suggests that melatonin works as an effective Mpro inhibitor (156,194,200,201). In the following section, the limited evidence of the beneficial effects of melatonin on patients with COVID-19 is discussed, building on these potential advantages derived from previous clinical or preclinical research.
5. Clinical evidence for COVID-19 and melatonin
Previous research on other viral diseases, together with the possible antiviral properties of melatonin, has led to its suggestion as a possible therapeutic agent for COVID-19 (17,49,202). Melatonin has been tested in clinical studies for the treatment of COVID-19. The results revealed that the drug improved sleep quality, reduced the duration of hospitalization and was useful as a preventative measure (155,180,202,203). However, the studies are restricted owing to inadequate financial assistance (melatonin is affordable and non-patentable) (156).
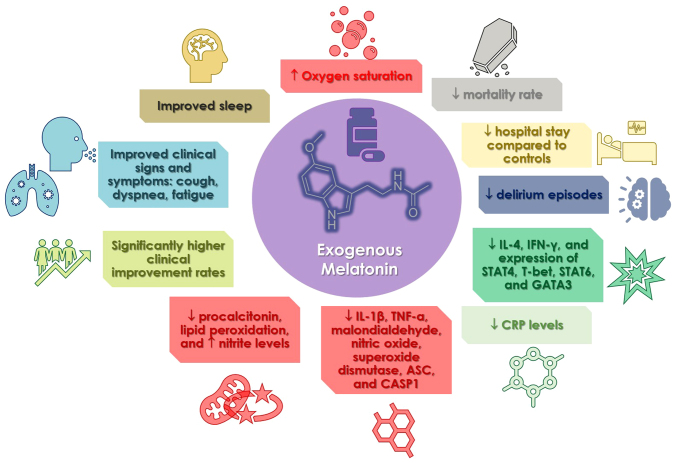
Only a small number of trials have studied the safety and effectiveness of melatonin and its therapeutic value in COVID-19, and they were only recently evaluated in a meta-analysis (202). The most notable findings were that patients using melatonin had a much higher clinical improvement rate than the control groups (202). Melatonin administration also resulted in a reduced death rate, reduced C-reactive protein (CRP) concentration, and length of hospital stay than the controls (202). The study concluded that melatonin had significant benefits on patients with COVID-19 when administered as adjuvant treatment, boosting clinical improvement and shortening recovery time owing to shorter hospital stays and mechanical ventilation durations (202). Other research included the following observations: The case group exhibited lower levels of IL-4 and IFN-γ in their plasma, as well as lower levels of signal transducer and activator of transcription (STAT)4, T-bet, STAT6 and GATA binding protein 3 expression in comparison to the control group (203). In their study, Alizadeh et al (204) discovered that the case group exhibited a reduction in CRP levels both before and after the ingestion of melatonin. On the other hand, the control group did not exhibit a significant reduction in CRP levels. A different case group exhibited an improvement in clinical signs and symptoms, such as cough, dyspnea and tiredness, while simultaneously exhibiting a decrease in CRP levels in comparison to the control group (205). When compared to the control group, the low dosage of melatonin resulted in a reduction in CRP levels, lung involvement, a shorter time to discharge from the hospital, and a shorter period after returning to baseline health (206). According to the findings of another study that examined the quality of sleep and other outcomes of patients with COVID-19, both oxygen saturation and sleep quality increased (207). Chavarría et al (208) demonstrated that melatonin supplementation in patients with moderate symptoms resulted in decreased levels of CRP, IL-6, procalcitonin and lipid peroxidation, and elevated nitrite levels. In addition, the levels of numerous pro-inflammatory indicators, such as IL-1β, TNF-α, malondialdehyde, nitric oxide, superoxide dismutase, ASC and CASP1, were found to be lower in persons who were administered melatonin in comparison to the group that served as the control (209). Finally, patients with COVID-19 and insomnia who received prolonged-release melatonin exhibited improvements in their sleep, a reduction in the number of episodes of delirium, a shorter length of hospitalization, a shorter stay in the sub-intensive care unit, and a shorter duration of therapy with non-invasive ventilation (210). The benefits associated with the use of melatonin in COVID-19 clinical studies are illustrated in Fig. 3.
Figure 3.
Schematic illustration summarizing the beneficial outcomes of melatonin supplementation from clinical studies in humans. ASC, apoptosis-associated speck-like protein containing a caspase recruitment domain; CASP1, caspase-1; CRP, C-reactive protein; GATA, GATA binding protein 3; IFN-γ, interferon γ; IL, interleukin; STAT, signal transducer and activator of transcription; T-bet, T-box expressed in T-cell; TNF, tumor necrosis factor. Parts of this image were derived from the free medical site http://smart.servier.com/ (accessed on September 15, 2023) by Servier, licensed under a Creative Commons Attribution 3.0 Unported Licence.
6. Conclusions and future perspectives
COVID-19 remains a critical global health concern. Acute COVID pathophysiology linked to the cytokine storm and oxidative stress, and long COVID research have yielded mitochondrial dysfunction among other mechanisms, all of which can be alleviated by providing melatonin (17). The treatment options that have been proposed include, in addition to enhancing the function of immune cells, the elimination of autoantibodies, immunosuppressants and antivirals, as well as agents that possess antioxidant properties, mitochondrial support and the generation of mitochondrial energy (18,159). A number of these could be achieved by including the use of melatonin as an adjuvant therapeutic option. However, despite promising and with positive outcomes based on a small number of clinical trials, its actions need to be investigated further, as an ample amount of the therapeutic potential of melatonin remains underexplored, also due to funding limitations (27,202). On the other hand, further clinical studies that are well-designed are warranted in order to validate these findings (202). Of utmost interest would be the design of trials with various time points primarily examining the acute phase anti-inflammatory properties and on a longer term, the preventive potential against mitochondrial damage and long COVID pathology (17). Finally, the factors influencing the effects of melatonin, including dosage also need to be thoroughly explored.
Acknowledgments
The title of the present review was inspired by William Shakespeare's theatrical masterpiece 'A Midsummer Night's Dream'.
Funding Statement
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
DAS and VEG conceptualized the study. IGL, VEG, RJR and DAS made a substantial contribution to the interpretation and analysis of data from the literature to be included in the review, and wrote and prepared the draft of the manuscript. DAS and RJR analyzed the data and provided critical revisions. All authors contributed to manuscript revision, and have read and approved the final version of the manuscript. Data authentication is not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had no personal involvement in the reviewing process, or any influence in terms of adjudicating on the final decision, for this article. The other authors declare that they have no competing interests.
References
- 1.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Georgakopoulou VE, Makrodimitri S, Triantafyllou M, Samara S, Voutsinas PM, Anastasopoulou A, Papageorgiou CV, Spandidos DA, Gkoufa A, Papalexis P, et al. Immature granulocytes: Innovative biomarker for SARS-CoV-2 infection. Mol Med Rep. 2022;26:217. doi: 10.3892/mmr.2022.12733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lempesis IG, Karlafti E, Papalexis P, Fotakopoulos G, Tarantinos K, Lekakis V, Papadakos SP, Cholongitas E, Georgakopoulou VE. COVID-19 and liver injury in individuals with obesity. World J Gastroenterol. 2023;29:908–916. doi: 10.3748/wjg.v29.i6.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gracia-Ramos AE, Jaquez-Quintana JO, Contreras-Omana R, Auron M. Liver dysfunction and SARS-CoV-2 infection. World J Gastroenterol. 2021;27:3951–3970. doi: 10.3748/wjg.v27.i26.3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gkoufa A, Maneta E, Ntoumas GN, Georgakopoulou VE, Mantelou A, Kokkoris S, Routsi C. Elderly adults with COVID-19 admitted to intensive care unit: A narrative review. World J Crit Care Med. 2021;10:278–289. doi: 10.5492/wjccm.v10.i5.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Georgakopoulou VE, Gkoufa A, Garmpis N, Makrodimitri S, Papageorgiou CV, Barlampa D, Garmpi A, Chiapoutakis S, Sklapani P, Trakas N, Damaskos C. COVID-19 and acute pancreatitis: A systematic review of case reports and case series. Ann Saudi Med. 2022;42:276–287. doi: 10.5144/0256-4947.2022.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Georgakopoulou VE, Lembessis P, Skarlis C, Gkoufa A, Sipsas NV, Mavragani CP. Hematological abnormalities in COVID-19 disease: Association with type I interferon pathway activation and disease outcomes. Front Med (Lausanne) 2022;9:850472. doi: 10.3389/fmed.2022.850472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: A review. JAMA Cardiol. 2020;5:831–840. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 10.Lempesis IG, Georgakopoulou VE. Implications of obesity and adiposopathy on respiratory infections; focus on emerging challenges. World J Clin Cases. 2023;11:2925–2933. doi: 10.12998/wjcc.v11.i13.2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lempesis IG, Georgakopoulou VE. Physiopathological mechanisms related to inflammation in obesity and type 2 diabetes mellitus. World J Exp Med. 2023;13:7–16. doi: 10.5493/wjem.v13.i3.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Georgakopoulou VE, Bali T, Adamantou M, Asimakopoulou S, Makrodimitri S, Samara S, Triantafyllou M, Voutsinas PM, Eliadi I, Karamanakos G, et al. Acute hepatitis and liver injury in hospitalized patients with COVID-19 infection. Exp Ther Med. 2022;24:691. doi: 10.3892/etm.2022.11627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mathioudakis N, Zachiotis M, Papadakos S, Triantafyllou M, Karapanou A, Samara S, Karamanakos G, Spandidos DA, Papalexis P, Damaskos C, et al. Onodera's prognostic nutritional index: Comparison of its role in the severity and outcomes of patients with COVID-19 during the periods of alpha, delta and omicron variant predominance. Exp Ther Med. 2022;24:675. doi: 10.3892/etm.2022.11611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cholongitas E, Bali T, Georgakopoulou VE, Kamiliou A, Vergos I, Makrodimitri S, Samara S, Triantafylou M, Basoulis D, Eliadi I, et al. Comparison of liver function test- and inflammation-based prognostic scores for coronavirus disease 2019: A single center study. Eur J Gastroenterol Hepatol. 2022;34:1165–1171. doi: 10.1097/MEG.0000000000002446. [DOI] [PubMed] [Google Scholar]
- 15.Georgakopoulou VE, Gkoufa A, Damaskos C, Papalexis P, Pierrakou A, Makrodimitri S, Sypsa G, Apostolou A, Asimakopoulou S, Chlapoutakis S, et al. COVID-19-associated acute appendicitis in adults. A report of five cases and a review of the literature. Exp Ther Med. 2022;24:482. doi: 10.3892/etm.2022.11409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cholongitas E, Bali T, Georgakopoulou VE, Giannakodimos A, Gyftopoulos A, Georgilaki V, Gerogiannis D, Basoulis D, Eliadi I, Karamanakos G, et al. Prevalence of abnormal liver biochemistry and its impact on COVID-19 patients' outcomes: A single-center Greek study. Ann Gastroenterol. 2022;35:290–296. doi: 10.20524/aog.2022.0709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loh D, Reiter RJ. Melatonin: Regulation of viral phase separation and epitranscriptomics in post-acute sequelae of COVID-19. Int J Mol Sci. 2022;23:8122. doi: 10.3390/ijms23158122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: Major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21:133–146. doi: 10.1038/s41579-022-00846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mehandru S, Merad M. Pathological sequelae of long-haul COVID. Nat Immunol. 2022;23:194–202. doi: 10.1038/s41590-021-01104-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vehar S, Boushra M, Ntiamoah P, Biehl M. Post-acute sequelae of SARS-CoV-2 infection: Caring for the 'long-haulers'. Cleve Clin J Med. 2021;88:267–272. doi: 10.3949/ccjm.88a.21010. [DOI] [PubMed] [Google Scholar]
- 21.Bali T, Georgakopoulou VE, Kamiliou A, Vergos I, Adamantou M, Vlachos S, Ermidis G, Sipsas NV, Samarkos M, Cholongitas E. Abnormal liver function tests and coronavirus disease 2019: A close relationship. J Viral Hepat. 2023;30:79–80. doi: 10.1111/jvh.13772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guarnieri JW, Dybas JM, Fazelinia H, Kim MS, Frere J, Zhang Y, Soto Albrecht Y, Murdock DG, Angelin A, Singh LN, et al. Core mitochondrial genes are down-regulated during SARS-CoV-2 infection of rodent and human hosts. Sci Transl Med. 2023;15:eabq1533. doi: 10.1126/scitranslmed.abq1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reiter RJ, Tan DX, Galano A. Melatonin: Exceeding expectations. Physiology (Bethesda) 2014;29:325–333. doi: 10.1152/physiol.00011.2014. [DOI] [PubMed] [Google Scholar]
- 24.Reiter RJ, Sharma R, Rosales-Corral S, de Campos Zuccari DAP, de Almeida Chuffa LG. Melatonin: A mitochondrial resident with a diverse skill set. Life Sci. 2022;301:120612. doi: 10.1016/j.lfs.2022.120612. [DOI] [PubMed] [Google Scholar]
- 25.Reiter RJ, Sharma R, Tan DX, Neel RL, Simko F, Manucha W, Rosales-Corral S, Cardinali DP. Melatonin use for SARS-CoV-2 infection: Time to diversify the treatment portfolio. J Med Virol. 2022;94:2928–2930. doi: 10.1002/jmv.27740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Romero A, Ramos E, López-Muñoz F, Gil-Martín E, Escames G, Reiter RJ. Coronavirus disease 2019 (COVID-19) and its neuroinvasive capacity: Is it time for melatonin? Cell Mol Neurobiol. 2022;42:489–500. doi: 10.1007/s10571-020-00938-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reiter RJ, Sharma R, Simko F, Dominguez-Rodriguez A, Tesarik J, Neel RL, Slominski AT, Kleszczynski K, Martin-Gimenez VM, Manucha W, Cardinali DP. Melatonin: Highlighting its use as a potential treatment for SARS-CoV-2 infection. Cell Mol Life Sci. 2022;79:143. doi: 10.1007/s00018-021-04102-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mouffak S, Shubbar Q, Saleh E, El-Awady R. Recent advances in management of COVID-19: A review. Biomed Pharmacother. 2021;143:112107. doi: 10.1016/j.biopha.2021.112107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wichniak A, Kania A, Siemiński M, Cubała WJ. Melatonin as a potential adjuvant treatment for COVID-19 beyond sleep disorders. Int J Mol Sci. 2021;22:8623. doi: 10.3390/ijms22168623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramos E, López-Muñoz F, Gil-Martín E, Egea J, Álvarez-Merz I, Painuli S, Semwal P, Martins N, Hernández-Guijo JM, Romero A. The coronavirus disease 2019 (COVID-19): key emphasis on melatonin safety and therapeutic efficacy. Antioxidants (Basel) 2021;10:1152. doi: 10.3390/antiox10071152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boga JA, Coto-Montes A, Rosales-Corral SA, Tan DX, Reiter RJ. Beneficial actions of melatonin in the management of viral infections: A new use for this 'molecular handyman'? Rev Med Virol. 2012;22:323–338. doi: 10.1002/rmv.1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Juybari KB, Pourhanifeh MH, Hosseinzadeh A, Hemati K, Mehrzadi S. Melatonin potentials against viral infections including COVID-19: Current evidence and new findings. Virus Res. 2020;287:198108. doi: 10.1016/j.virusres.2020.198108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Georgakopoulou VE, Gkoufa A, Makrodimitri S, Basoulis D, Tsakanikas A, Karamanakos G, Mastrogianni E, Voutsinas PM, Spandidos DA, Papageorgiou CV, et al. Early 3-day course of remdesivir for the prevention of the progression to severe COVID-19 in the elderly: A single-centre, real-life cohort study. Exp Ther Med. 2023;26:462. doi: 10.3892/etm.2023.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Basoulis D, Tsakanikas A, Gkoufa A, Bitsani A, Karamanakos G, Mastrogianni E, Georgakopoulou VE, Makrodimitri S, Voutsinas PM, Lamprou P, et al. Effectiveness of oral nirmatrelvir/ritonavir vs intravenous three-day remdesivir in preventing progression to severe COVID-19: A single-center, prospective, comparative, real-life study. Viruses. 2023;15:1515. doi: 10.3390/v15071515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Papadopoulou A, Karavalakis G, Papadopoulou E, Xochelli A, Bousiou Z, Vogiatzoglou A, Papayanni PG, Georgakopoulou A, Giannaki M, Stavridou F, et al. SARS-CoV-2-specific T cell therapy for severe COVID-19: a randomized phase 1/2 trial. Nat Med. 2023;29:2019–2029. doi: 10.1038/s41591-023-02480-8. [DOI] [PubMed] [Google Scholar]
- 36.Karlafti E, Paramythiotis D, Pantazi K, Georgakopoulou VE, Kaiafa G, Papalexis P, Protopapas AA, Ztriva E, Fyntanidou V, Savopoulos C. Drug-induced liver injury in hospitalized patients during SARS-CoV-2 infection. Medicina (Kaunas) 2022;58:1848. doi: 10.3390/medicina58121848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Georgakopoulou VE, Basoulis D, Voutsinas PM, Makrodimitri S, Samara S, Triantafyllou M, Eliadi I, Karamanakos G, Papageorgiou CV, Anastasopoulou A, et al. Factors predicting poor outcomes of patients treated with tocilizumab for COVID-19-associated pneumonia: A retrospective study. Exp Ther Med. 2022;24:724. doi: 10.3892/etm.2022.11660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gkoufa A, Saridaki M, Georgakopoulou VE, Spandidos DA, Cholongitas E. COVID-19 vaccination in liver transplant recipients (Review) Exp Ther Med. 2023;25:291. doi: 10.3892/etm.2023.11990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elrashdy F, Tambuwala MM, Hassan SS, Adadi P, Seyran M, Abd El-Aziz TM, Rezaei N, Lal A, Aljabali AAA, Kandimalla R, et al. Autoimmunity roots of the thrombotic events after COVID-19 vaccination. Autoimmun Rev. 2021;20:102941. doi: 10.1016/j.autrev.2021.102941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taskou C, Sarantaki A, Beloukas A, Georgakopoulou VE, Daskalakis G, Papalexis P, Lykeridou A. Knowledge and attitudes of healthcare professionals regarding perinatal influenza vaccination during the COVID-19 pandemic. Vaccines (Basel) 2023;11:168. doi: 10.3390/vaccines11010168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goeser S, Ruble J, Chandler L. Melatonin: Historical and clinical perspectives. J Pharmaceut Care Pain Symptom Contr. 1997;5:37–49. [Google Scholar]
- 42.Beyer CE, Steketee JD, Saphier D. Antioxidant properties of melatonin-an emerging mystery. Biochem Pharmacol. 1998;56:1265–1272. doi: 10.1016/s0006-2952(98)00180-4. [DOI] [PubMed] [Google Scholar]
- 43.Ahmad SB, Ali A, Bilal M, Rashid SM, Wani AB, Bhat RR, Rehman MU. Melatonin and health: Insights of melatonin action, biological functions, and associated disorders. Cell Mol Neurobiol. 2023;43:2437–2458. doi: 10.1007/s10571-023-01324-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hardeland R, Balzer I, Poeggeler B, Fuhrberg B, Uría H, Behrmann G, Wolf R, Meyer TJ, Reiter RJ. On the primary functions of melatonin in evolution: Mediation of photoperiodic signals in a unicell, photooxidation, and scavenging of free radicals. J Pineal Res. 1995;18:104–111. doi: 10.1111/j.1600-079x.1995.tb00147.x. [DOI] [PubMed] [Google Scholar]
- 45.Cipolla-Neto J, Amaral FGD. Melatonin as a hormone: New physiological and clinical insights. Endocr Rev. 2018;39:990–1028. doi: 10.1210/er.2018-00084. [DOI] [PubMed] [Google Scholar]
- 46.Manchester LC, Coto-Montes A, Boga JA, Andersen LP, Zhou Z, Galano A, Vriend J, Tan DX, Reiter RJ. Melatonin: An ancient molecule that makes oxygen metabolically tolerable. J Pineal Res. 2015;59:403–419. doi: 10.1111/jpi.12267. [DOI] [PubMed] [Google Scholar]
- 47.Hardeland R, Reiter R, Poeggeler B, Tan DX. The significance of the metabolism of the neurohormone melatonin: Antioxidative protection and formation of bioactive substances. Neurosci Biobehav Rev. 1993;17:347–357. doi: 10.1016/s0149-7634(05)80016-8. [DOI] [PubMed] [Google Scholar]
- 48.Reiter RJ. Pineal melatonin: Cell biology of its synthesis and of its physiological interactions. Endocr Rev. 1991;12:151–180. doi: 10.1210/edrv-12-2-151. [DOI] [PubMed] [Google Scholar]
- 49.Hosseinzadeh A, Bagherifard A, Koosha F, Amiri S, Karimi-Behnagh A, Reiter RJ, Mehrzadi S. Melatonin effect on platelets and coagulation: Implications for a prophylactic indication in COVID-19. Life Sci. 2022;307:120866. doi: 10.1016/j.lfs.2022.120866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tan DX, Hardeland R, Manchester LC, Paredes SD, Korkmaz A, Sainz RM, Mayo JC, Fuentes-Broto L, Reiter RJ. The changing biological roles of melatonin during evolution: From an antioxidant to signals of darkness, sexual selection and fitness. Biol Rev Camb Philos Soc. 2010;85:607–623. doi: 10.1111/j.1469-185X.2009.00118.x. [DOI] [PubMed] [Google Scholar]
- 51.Andersen LPH, Gögenur I, Rosenberg J, Reiter RJ. Pharmacokinetics of melatonin: The missing link in clinical efficacy? Clin Pharmacokinet. 2016;55:1027–1030. doi: 10.1007/s40262-016-0386-3. [DOI] [PubMed] [Google Scholar]
- 52.Reiter RJ, Tan DX, Korkmaz A. The circadian melatonin rhythm and its modulation: Possible impact on hypertension. J Hypertens Suppl. 2009;27:S17–S20. doi: 10.1097/01.hjh.0000358832.41181.bf. [DOI] [PubMed] [Google Scholar]
- 53.Vriend J, Reiter RJ. Melatonin feedback on clock genes: A theory involving the proteasome. J Pineal Res. 2015;58:1–11. doi: 10.1111/jpi.12189. [DOI] [PubMed] [Google Scholar]
- 54.Erren TC, Reiter RJ. Melatonin: A universal time messenger. Neuro Endocrinol Lett. 2015;36:187–192. [PubMed] [Google Scholar]
- 55.Mehrzadi S, Karimi MY, Fatemi A, Reiter RJ, Hosseinzadeh A. SARS-CoV-2 and other coronaviruses negatively influence mitochondrial quality control: Beneficial effects of melatonin. Pharmacol Ther. 2021;224:107825. doi: 10.1016/j.pharmthera.2021.107825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mauriz JL, Collado PS, Veneroso C, Reiter RJ, González-Gallego J. A review of the molecular aspects of melatonin's anti-inflammatory actions: Recent insights and new perspectives. J Pineal Res. 2013;54:1–14. doi: 10.1111/j.1600-079X.2012.01014.x. [DOI] [PubMed] [Google Scholar]
- 57.Slominski RM, Reiter RJ, Schlabritz-Loutsevitch N, Ostrom RS, Slominski AT. Melatonin membrane receptors in peripheral tissues: Distribution and functions. Mol Cell Endocrinol. 2012;351:152–166. doi: 10.1016/j.mce.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gurunathan S, Kang MH, Choi Y, Reiter RJ, Kim JH. Melatonin: A potential therapeutic agent against COVID-19. Melatonin Res. 2021;4:30–69. [Google Scholar]
- 59.Naskar A, Prabhakar V, Singh R, Dutta D, Mohanakumar KP. Melatonin enhances L-DOPA therapeutic effects, helps to reduce its dose, and protects dopaminergic neurons in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced Parkinsonism in mice. J Pineal Res. 2015;58:262–274. doi: 10.1111/jpi.12212. [DOI] [PubMed] [Google Scholar]
- 60.Reiter RJ, Mayo JC, Tan DX, Sainz RM, Alatorre-Jimenez M, Qin L. Melatonin as an antioxidant: Under promises but over delivers. J Pineal Res. 2016;61:253–278. doi: 10.1111/jpi.12360. [DOI] [PubMed] [Google Scholar]
- 61.Ramos E, Patiño P, Reiter RJ, Gil-Martín E, Marco-Contelles J, Parada E, de Los Rios C, Romero A, Egea J. Ischemic brain injury: New insights on the protective role of melatonin. Free Radic Biol Med. 2017;104:32–53. doi: 10.1016/j.freeradbiomed.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 62.Sanchez-Barcelo EJ, Rueda N, Mediavilla MD, Martinez-Cue C, Reiter RJ. Clinical uses of melatonin in neurological diseases and mental and behavioural disorders. Curr Med Chem. 2017;24:3851–3878. doi: 10.2174/0929867324666170718105557. [DOI] [PubMed] [Google Scholar]
- 63.Ali T, Rahman SU, Hao Q, Li W, Liu Z, Ali Shah F, Murtaza I, Zhang Z, Yang X, Liu G, Li S. Melatonin prevents neuroinflammation and relieves depression by attenuating autophagy impairment through FOXO3a regulation. J Pineal Res. 2020;69:e12667. doi: 10.1111/jpi.12667. [DOI] [PubMed] [Google Scholar]
- 64.Vriend J, Reiter RJ. Melatonin as a proteasome inhibitor. Is there any clinical evidence? Life Sci. 2014;115:8–14. doi: 10.1016/j.lfs.2014.08.024. [DOI] [PubMed] [Google Scholar]
- 65.Mayo JC, Sainz RM, González Menéndez P, Cepas V, Tan DX, Reiter RJ. Melatonin and sirtuins: A 'not-so unexpected' relationship. J Pineal Res. 2017;62:e12391. doi: 10.1111/jpi.12391. [DOI] [PubMed] [Google Scholar]
- 66.Gurunathan S, Qasim M, Kang MH, Kim JH. Role and therapeutic potential of melatonin in various type of cancers. Onco Targets Ther. 2021;14:2019–2052. doi: 10.2147/OTT.S298512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pourhanifeh MH, Mehrzadi S, Kamali M, Hosseinzadeh A. Melatonin and gastrointestinal cancers: Current evidence based on underlying signaling pathways. Eur J Pharmacol. 2020;886:173471. doi: 10.1016/j.ejphar.2020.173471. [DOI] [PubMed] [Google Scholar]
- 68.Reiter RJ, Rosales-Corral SA, Tan DX, Acuna-Castroviejo D, Qin L, Yang SF, Xu K. Melatonin, a full service anti-cancer agent: inhibition of initiation, progression and metastasis. Int J Mol Sci. 2017;18:843. doi: 10.3390/ijms18040843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Reiter RJ, Tan DX, Paredes SD, Fuentes-Broto L. Beneficial effects of melatonin in cardiovascular disease. Ann Med. 2010;42:276–285. doi: 10.3109/07853890903485748. [DOI] [PubMed] [Google Scholar]
- 70.Galano A, Tan DX, Reiter RJ. Melatonin: A versatile protector against oxidative DNA damage. Molecules. 2018;23:530. doi: 10.3390/molecules23030530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Simko F, Baka T, Paulis L, Reiter RJ. Elevated heart rate and nondipping heart rate as potential targets for melatonin: A review. J Pineal Res. 2016;61:127–137. doi: 10.1111/jpi.12348. [DOI] [PubMed] [Google Scholar]
- 72.Reiter RJ, Tan DX, Kim SJ, Qi W. Melatonin as a pharmacological agent against oxidative damage to lipids and DNA. Proc West Pharmacol Soc. 1998;41:229–236. [PubMed] [Google Scholar]
- 73.Reiter RJ, Tan DX, Rosales-Corral S, Manchester LC. The universal nature, unequal distribution and antioxidant functions of melatonin and its derivatives. Mini Rev Med Chem. 2013;13:373–384. doi: 10.2174/1389557511313030006. [DOI] [PubMed] [Google Scholar]
- 74.García JJ, López-Pingarrón L, Almeida-Souza P, Tres A, Escudero P, García-Gil FA, Tan DX, Reiter RJ, Ramírez JM, Bernal-Pérez M. Protective effects of melatonin in reducing oxidative stress and in preserving the fluidity of biological membranes: A review. J Pineal Res. 2014;56:225–237. doi: 10.1111/jpi.12128. [DOI] [PubMed] [Google Scholar]
- 75.Tan DX, Korkmaz A, Reiter RJ, Manchester LC. Ebola virus disease: Potential use of melatonin as a treatment. J Pineal Res. 2014;57:381–384. doi: 10.1111/jpi.12186. [DOI] [PubMed] [Google Scholar]
- 76.Reiter RJ, Ma Q, Sharma R. Treatment of Ebola and other infectious diseases: Melatonin 'goes viral'. Melatonin Res. 2020;3:43–57. [Google Scholar]
- 77.Reiter RJ, Sharma R, Ma Q, Liu C, Manucha W, González P, Dominguez-Rodriguez A. Metabolic plasticity of activated immune cells: Advantages for suppression of COVID-19 disease by melatonin. Melatonin Res. 2020;3:362–379. [Google Scholar]
- 78.Reiter RJ, Sharma R, Ma Q, Dominquez-Rodriguez A, Marik PE, Abreu-Gonzalez P. Melatonin inhibits COVID-19-induced cytokine storm by reversing aerobic glycolysis in immune cells: A mechanistic analysis. Med Drug Discov. 2020;6:100044. doi: 10.1016/j.medidd.2020.100044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sarkar S, Chattopadhyay A, Bandyopadhyay D. Multiple strategies of melatonin protecting against cardiovascular injury related to inflammation: A comprehensive overview. Melatonin Res. 2021;4:1–29. [Google Scholar]
- 80.Esposito E, Cuzzocrea S. Antiinflammatory activity of melatonin in central nervous system. Curr Neuropharmacol. 2010;8:228–242. doi: 10.2174/157015910792246155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hardeland R, Cardinali DP, Brown GM, Pandi-Perumal SR. Melatonin and brain inflammaging. Prog Neurobiol. 2015;127-128:46–63. doi: 10.1016/j.pneurobio.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 82.Farez MF, Mascanfroni ID, Méndez-Huergo SP, Yeste A, Murugaiyan G, Garo LP, Balbuena Aguirre ME, Patel B, Ysrraelit MC, Zhu C, et al. Melatonin contributes to the seasonality of multiple sclerosis relapses. Cell. 2015;162:1338–1352. doi: 10.1016/j.cell.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dominguez-Rodriguez A, Abreu-Gonzalez P, Marik PE, Reiter RJ. Melatonin, cardiovascular disease and COVID-19: A potential therapeutic strategy? Melatonin Res. 2020;3:318–321. [Google Scholar]
- 84.Ozdemir G, Ergün Y, Bakariş S, Kılınç M, Durdu H, Ganiyusufoğlu E. Melatonin prevents retinal oxidative stress and vascular changes in diabetic rats. Eye (Lond) 2014;28:1020–1027. doi: 10.1038/eye.2014.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gheban BA, Rosca IA, Crisan M. The morphological and functional characteristics of the pineal gland. Med Pharm Rep. 2019;92:226–234. doi: 10.15386/mpr-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cipolla-Neto J, Amaral F, Afeche SC, Tan DX, Reiter RJ. Melatonin, energy metabolism, and obesity: A review. J Pineal Res. 2014;56:371–381. doi: 10.1111/jpi.12137. [DOI] [PubMed] [Google Scholar]
- 87.Lempesis IG, Hoebers N, Essers Y, Jocken JWE, Dineen R, Blaak EE, Manolopoulos KN, Goossens GH. Distinct inflammatory signatures of upper and lower body adipose tissue and adipocytes in women with normal weight or obesity. Front Endocrinol (Lausanne) 2023;14:1205799. doi: 10.3389/fendo.2023.1205799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lempesis IG, Varrias D, Sagris M, Attaran RR, Altin ES, Bakoyiannis C, Palaiodimos L, Dalamaga M, Kokkinidis DG. Obesity and peripheral artery disease: Current evidence and controversies. Curr Obes Rep. 2023;12:264–279. doi: 10.1007/s13679-023-00510-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lempesis IG, Apple SJ, Duarte G, Palaiodimos L, Kalaitzopoulos DR, Dalamaga M, Kokkinidis DG. Cardiometabolic effects of SGLT2 inhibitors on polycystic ovary syndrome. Diabetes Metab Res Rev. 2023;39:e3682. doi: 10.1002/dmrr.3682. [DOI] [PubMed] [Google Scholar]
- 90.Lempesis IG, Tsilingiris D, Liu J, Dalamaga M. Of mice and men: Considerations on adipose tissue physiology in animal models of obesity and human studies. Metabol Open. 2022;15:100208. doi: 10.1016/j.metop.2022.100208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Simko F, Hrenak J, Dominguez-Rodriguez A, Reiter RJ. Melatonin as a putative protection against myocardial injury in COVID-19 infection. Expert Rev Clin Pharmacol. 2020;13:921–924. doi: 10.1080/17512433.2020.1814141. [DOI] [PubMed] [Google Scholar]
- 92.Mirza-Aghazadeh-Attari M, Reiter RJ, Rikhtegar R, Jalili J, Hajalioghli P, Mihanfar A, Majidinia M, Yousefi B. Melatonin: An atypical hormone with major functions in the regulation of angiogenesis. IUBMB Life. 2020;72:1560–1584. doi: 10.1002/iub.2287. [DOI] [PubMed] [Google Scholar]
- 93.Melhuish Beaupre LM, Brown GM, Gonçalves VF, Kennedy JL. Melatonin's neuroprotective role in mitochondria and its potential as a biomarker in aging, cognition and psychiatric disorders. Transl Psychiatry. 2021;11:339. doi: 10.1038/s41398-021-01464-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Reiter RJ, Rosales-Corral S, Tan DX, Jou MJ, Galano A, Xu B. Melatonin as a mitochondria-targeted antioxidant: One of evolution's best ideas. Cell Mol Life Sci. 2017;74:3863–3881. doi: 10.1007/s00018-017-2609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Reiter RJ, Ma Q, Sharma R. Melatonin in mitochondria: Mitigating clear and present dangers. Physiology (Bethesda) 2020;35:86–95. doi: 10.1152/physiol.00034.2019. [DOI] [PubMed] [Google Scholar]
- 96.Wakatsuki A, Okatani Y, Shinohara K, Ikenoue N, Kaneda C, Fukaya T. Melatonin protects fetal rat brain against oxidative mitochondrial damage. J Pineal Res. 2001;30:22–28. doi: 10.1034/j.1600-079x.2001.300103.x. [DOI] [PubMed] [Google Scholar]
- 97.Reiter RJ, Tan DX, Rosales-Corral S, Galano A, Jou MJ, Acuna-Castroviejo D. Melatonin mitigates mitochondrial meltdown: Interactions with SIRT3. Int J Mol Sci. 2018;19:2439. doi: 10.3390/ijms19082439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Han L, Wang H, Li L, Li X, Ge J, Reiter RJ, Wang Q. Melatonin protects against maternal obesity-associated oxidative stress and meiotic defects in oocytes via the SIRT3-SOD2-dependent pathway. J Pineal Res. 2017;63:e12431. doi: 10.1111/jpi.12431. [DOI] [PubMed] [Google Scholar]
- 99.Mar tín M, Macías M, Escames G, León J, Acuña-Castroviejo D. Melatonin but not vitamins C and E maintains glutathione homeostasis in t-butyl hydroperoxide-induced mitochondrial oxidative stress. FASEB J. 2000;14:1677–1679. doi: 10.1096/fj.99-0865fje. [DOI] [PubMed] [Google Scholar]
- 100.Venegas C, García JA, Escames G, Ortiz F, López A, Doerrier C, García-Corzo L, López LC, Reiter RJ, Acuña-Castroviejo D. Extrapineal melatonin: Analysis of its subcellular distribution and daily fluctuations. J Pineal Res. 2012;52:217–227. doi: 10.1111/j.1600-079X.2011.00931.x. [DOI] [PubMed] [Google Scholar]
- 101.Suofu Y, Li W, Jean-Alphonse FG, Jia J, Khattar NK, Li J, Baranov SV, Leronni D, Mihalik AC, He Y, et al. Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release. Proc Natl Acad Sci USA. 2017;114:E7997–E8006. doi: 10.1073/pnas.1705768114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.He C, Wang J, Zhang Z, Yang M, Li Y, Tian X, Ma T, Tao J, Zhu K, Song Y, et al. Mitochondria synthesize melatonin to ameliorate its function and improve mice oocyte's quality under in vitro conditions. Int J Mol Sci. 2016;17:939. doi: 10.3390/ijms17060939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tan DX, Reiter RJ. Mitochondria: The birth place, battle ground and the site of melatonin metabolism in cells. Melatonin Res. 2019;2:44–66. [Google Scholar]
- 104.Chumboatong W, Thummayot S, Govitrapong P, Tocharus C, Jittiwat J, Tocharus J. Neuroprotection of agomelatine against cerebral ischemia/reperfusion injury through an antiapoptotic pathway in rat. Neurochem Int. 2017;102:114–122. doi: 10.1016/j.neuint.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 105.de Vries HE, Witte M, Hondius D, Rozemuller AJ, Drukarch B, Hoozemans J, van Horssen J. Nrf2-induced antioxidant protection: A promising target to counteract ROS-mediated damage in neurodegenerative disease? Free Radic Biol Med. 2008;45:1375–1383. doi: 10.1016/j.freeradbiomed.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 106.Martin M, Macias M, Escames G, Reiter RJ, Agapito MT, Ortiz GG, Acuña-Castroviejo D. Melatonin-induced increased activity of the respiratory chain complexes I and IV can prevent mitochondrial damage induced by ruthenium red in vivo. J Pineal Res. 2000;28:242–248. doi: 10.1034/j.1600-079x.2000.280407.x. [DOI] [PubMed] [Google Scholar]
- 107.Sheleme T, Bekele F, Ayela T. Clinical presentation of patients infected with coronavirus disease 19: A systematic review. Infect Dis (Auckl) 2020;13:1178633720952076. doi: 10.1177/1178633720952076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lempesis IG, Georgakopoulou VE, Papalexis P, Chrousos GP, Spandidos DA. Role of stress in the pathogenesis of cancer (Review) Int J Oncol. 2023;63:124. doi: 10.3892/ijo.2023.5572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Georgakopoulou VE, Gkoufa A, Bougea A, Basoulis D, Tsakanikas A, Makrodimitri S, Karamanakos G, Spandidos DA, Angelopoulou E, Sipsas NV. Characteristics and outcomes of elderly patients with Parkinson's disease hospitalized due to COVID-19-associated pneumonia. Med Int (Lond) 2023;3:34. doi: 10.3892/mi.2023.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, Bolling MC, Dijkstra G, Voors AA, Osterhaus AD, et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19) J Pathol. 2020;251:228–248. doi: 10.1002/path.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ozkurt Z, Çınar Tanrıverdi E. COVID-19: Gastrointestinal manifestations, liver injury and recommendations. World J Clin Cases. 2022;10:1140–1163. doi: 10.12998/wjcc.v10.i4.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhang Q, Xiang R, Huo S, Zhou Y, Jiang S, Wang Q, Yu F. Molecular mechanism of interaction between SARS-CoV-2 and host cells and interventional therapy. Signal Transduct Target Ther. 2021;6:233. doi: 10.1038/s41392-021-00653-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Georgakopoulou VE, Gkoufa A, Tsakanikas A, Makrodimitri S, Karamanakos G, Basoulis D, Voutsinas PM, Eliadi I, Bougea A, Spandidos DA, et al. Predictors of COVID-19-associated mortality among hospitalized elderly patients with dementia. Exp Ther Med. 2023;26:395. doi: 10.3892/etm.2023.12094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Thakur V, Ratho RK, Kumar P, Bhatia SK, Bora I, Mohi GK, Saxena SK, Devi M, Yadav D, Mehariya S. Multi-organ involvement in COVID-19: Beyond pulmonary manifestations. J Clin Med. 2021;10:446. doi: 10.3390/jcm10030446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Martín Giménez VM, de las Heras N, Ferder L, Lahera V, Reiter RJ, Manucha W. Potential Effects of melatonin and micronutrients on mitochondrial dysfunction during a cytokine storm typical of oxidative/inflammatory diseases. Diseases. 2021;9:30. doi: 10.3390/diseases9020030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bougea A, Georgakopoulou VE, Palkopoulou M, Efthymiopoulou E, Angelopoulou E, Spandidos DA, Zikos P. New-onset non-motor symptoms in patients with Parkinson's disease and post-COVID-19 syndrome: A prospective cross-sectional study. Med Int (Lond) 2023;3:23. doi: 10.3892/mi.2023.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ahmad I, Rathore FA. Neurological manifestations and complications of COVID-19: A literature review. J Clin Neurosci. 2020;77:8–12. doi: 10.1016/j.jocn.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020;38:1504–1507. doi: 10.1016/j.ajem.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Legrand M, Bell S, Forni L, Joannidis M, Koyner JL, Liu K, Cantaluppi V. Pathophysiology of COVID-19-associated acute kidney injury. Nat Rev Nephrol. 2021;17:751–764. doi: 10.1038/s41581-021-00452-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Thaweethai T, Jolley SE, Karlson EW, Levitan EB, Levy B, McComsey GA, McCorkell L, Nadkarni GN, Parthasarathy S, Singh U, et al. Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA. 2023;329:1934–1946. doi: 10.1001/jama.2023.8823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Efstathiou V, Stefanou MI, Demetriou M, Siafakas N, Makris M, Tsivgoulis G, Zoumpourlis V, Kympouropoulos SP, Tsoporis JN, Spandidos DA, et al. Long COVID and neuropsychiatric manifestations (Review) Exp Ther Med. 2022;23:363. doi: 10.3892/etm.2022.11290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Efstathiou V, Stefanou MI, Demetriou M, Siafakas N, Katsantoni E, Makris M, Tsivgoulis G, Zoumpourlis V, Kympouropoulos SP, Tsoporis JN, et al. New-onset neuropsychiatric sequelae and 'long-COVID'syndrome (Review) Exp Ther Med. 2022;24:705. doi: 10.3892/etm.2022.11641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Daugherty SE, Guo Y, Heath K, Dasmariñas MC, Jubilo KG, Samranvedhya J, Lipsitch M, Cohen K. Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: Retrospective cohort study. BMJ. 2021;373:n1098. doi: 10.1136/bmj.n1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Huang L, Li X, Gu X, Zhang H, Ren L, Guo L, Liu M, Wang Y, Cui D, Wang Y, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: A longitudinal cohort study. Lancet Respir Med. 2022;10:863–876. doi: 10.1016/S2213-2600(22)00126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, et al. 6-Month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.E E, R F, Öi E, Im L, M L, S R, E W, C J, M H, A M. Impaired diffusing capacity for carbon monoxide is common in critically ill Covid-19 patients at four months post-discharge. Respir Med. 2021;182:106394. doi: 10.1016/j.rmed.2021.106394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Antonelli M, Pujol JC, Spector TD, Ourselin S, Steves CJ. Risk of long COVID associated with delta versus omicron variants of SARS-CoV-2. Lancet. 2022;399:2263–2264. doi: 10.1016/S0140-6736(22)00941-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Quaglia F, Salladini E, Carraro M, Minervini G, Tosatto SCE, Le Mercier P. SARS-CoV-2 variants preferentially emerge at intrinsically disordered protein sites helping immune evasion. FEBS J. 2022;289:4240–4250. doi: 10.1111/febs.16379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lipsitch M, Krammer F, Regev-Yochay G, Lustig Y, Balicer RD. SARS-CoV-2 breakthrough infections in vaccinated individuals: Measurement, causes and impact. Nat Rev Immunol. 2022;22:57–65. doi: 10.1038/s41577-021-00662-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hayes LD, Ingram J, Sculthorpe NF. More than 100 persistent symptoms of SARS-CoV-2 (long COVID): A scoping review. Front Med (Lausanne) 2021;8:750378. doi: 10.3389/fmed.2021.750378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re'em Y, Redfield S, Austin JP, Akrami A. Characterizing long COVID in an international cohort: 7 Months of symptoms and their impact. EClinicalMedicine. 2021;38:101019. doi: 10.1016/j.eclinm.2021.101019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gaebler C, Wang Z, Lorenzi JCC, Muecksch F, Finkin S, Tokuyama M, Cho A, Jankovic M, Schaefer-Babajew D, Oliveira TY, et al. Evolution of antibody immunity to SARS-CoV-2. Nature. 2021;591:639–644. doi: 10.1038/s41586-021-03207-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Proal AD, VanElzakker MB. Long COVID or post-acute sequelae of COVID-19 (PASC): An overview of biological factors that may contribute to persistent symptoms. Front Microbiol. 2021;12:698169. doi: 10.3389/fmicb.2021.698169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kalkeri R, Goebel S, Sharma GD. SARS-CoV-2 shedding from asymptomatic patients: Contribution of potential extrapulmonary tissue reservoirs. Am J Trop Med Hyg. 2020;103:18–21. doi: 10.4269/ajtmh.20-0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zubchenko S, Kril I, Nadizhko O, Matsyura O, Chopyak V. Herpesvirus infections and post-COVID-19 manifestations: A pilot observational study. Rheumatol Int. 2022;42:1523–1530. doi: 10.1007/s00296-022-05146-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Su Y, Yuan D, Chen DG, Ng RH, Wang K, Choi J, Li S, Hong S, Zhang R, Xie J, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022;185:881–895.e20. doi: 10.1016/j.cell.2022.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Schreiner P, Harrer T, Scheibenbogen C, Lamer S, Schlosser A, Naviaux RK, Prusty BK. Human herpesvirus-6 reactivation, mitochondrial fragmentation, and the coordination of antiviral and metabolic phenotypes in myalgic encephalomyelitis/chronic fatigue syndrome. Immunohorizons. 2020;4:201–215. doi: 10.4049/immunohorizons.2000006. [DOI] [PubMed] [Google Scholar]
- 138.Peluso MJ, Deeks SG, Mustapic M, Kapogiannis D, Henrich TJ, Lu S, Goldberg SA, Hoh R, Chen JY, Martinez EO, et al. SARS-CoV-2 and mitochondrial proteins in neural-derived exosomes of COVID-19. Ann Neurol. 2022;91:772–781. doi: 10.1002/ana.26350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Villaume WA. Marginal BH4 deficiencies, iNOS, and self-perpetuating oxidative stress in post-acute sequelae of Covid-19. Med Hypotheses. 2022;163:110842. doi: 10.1016/j.mehy.2022.110842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Saleh J, Peyssonnaux C, Singh KK, Edeas M. Mitochondria and microbiota dysfunction in COVID-19 pathogenesis. Mitochondrion. 2020;54:1–7. doi: 10.1016/j.mito.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Singh KK, Chaubey G, Chen JY, Suravajhala P. Decoding SARS-CoV-2 hijacking of host mitochondria in COVID-19 pathogenesis. Am J Physiol Cell Physiol. 2020;319:C258–C267. doi: 10.1152/ajpcell.00224.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Marchi S, Guilbaud E, Tait SWG, Yamazaki T, Galluzzi L. Mitochondrial control of inflammation. Nat Rev Immunol. 2023;23:159–173. doi: 10.1038/s41577-022-00760-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.West AP, Shadel GS. Mitochondrial DNA in innate immune responses and inflammatory pathology. Nat Rev Immunol. 2017;17:363–375. doi: 10.1038/nri.2017.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Wang P, Luo R, Zhang M, Wang Y, Song T, Tao T, Li Z, Jin L, Zheng H, Chen W, et al. A cross-talk between epithelium and endothelium mediates human alveolar-capillary injury during SARS-CoV-2 infection. Cell Death Dis. 2020;11:1042. doi: 10.1038/s41419-020-03252-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Cortese M, Lee JY, Cerikan B, Neufeldt CJ, Oorschot VMJ, Köhrer S, Hennies J, Schieber NL, Ronchi P, Mizzon G, et al. Integrative imaging reveals SARS-CoV-2-induced reshaping of subcellular morphologies. Cell Host Microbe. 2020;28:853–866.e5. doi: 10.1016/j.chom.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Hui DS, I Azhar E, Madani TA, Ntoumi F, Kock R, Dar O, Ippolito G, Mchugh TD, Memish ZA, Drosten C, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health-the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Gordon DE, Hiatt J, Bouhaddou M, Rezelj VV, Ulferts S, Braberg H, Jureka AS, Obernier K, Guo JZ, Batra J, et al. Comparative host-coronavirus protein interaction networks reveal pan-viral disease mechanisms. Science. 2020;370:eabe9403. doi: 10.1126/science.abe9403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Gordon DE, Jang GM, Bouhaddou M, Xu J, Obernier K, White KM, O'Meara MJ, Rezelj VV, Guo JZ, Swaney DL, et al. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature. 2020;583:459–468. doi: 10.1038/s41586-020-2286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Stukalov A, Girault V, Grass V, Karayel O, Bergant V, Urban C, Haas DA, Huang Y, Oubraham L, Wang A, et al. Multilevel proteomics reveals host perturbations by SARS-CoV-2 and SARS-CoV. Nature. 2021;594:246–252. doi: 10.1038/s41586-021-03493-4. [DOI] [PubMed] [Google Scholar]
- 150.Li S, Ma F, Yokota T, Garcia G, Jr, Palermo A, Wang Y, Farrell C, Wang YC, Wu R, Zhou Z, et al. Metabolic reprogramming and epigenetic changes of vital organs in SARS-CoV-2-induced systemic toxicity. JCI insight. 2021;6:e145027. doi: 10.1172/jci.insight.145027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Bojkova D, Klann K, Koch B, Widera M, Krause D, Ciesek S, Cinatl J, Münch C. Proteomics of SARS-CoV-2-infected host cells reveals therapy targets. Nature. 2020;583:469–472. doi: 10.1038/s41586-020-2332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Miller B, Silverstein A, Flores M, Cao K, Kumagai H, Mehta HH, Yen K, Kim SJ, Cohen P. Host mitochondrial transcriptome response to SARS-CoV-2 in multiple cell models and clinical samples. Sci Rep. 2021;11:3. doi: 10.1038/s41598-020-79552-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Medini H, Zirman A, Mishmar D. Immune system cells from COVID-19 patients display compromised mitochondrial-nuclear expression co-regulation and rewiring toward glycolysis. iScience. 2021;24:103471. doi: 10.1016/j.isci.2021.103471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Codo AC, Davanzo GG, Monteiro LB, de Souza GF, Muraro SP, Virgilio-da-Silva JV, Prodonoff JS, Carregari VC, de Biagi Junior CAO, Crunfli F, et al. Elevated glucose levels favor SARS-CoV-2 infection and monocyte response through a HIF-1α/glycolysis-dependent axis. Cell Metab. 2020;32:437–446.e5. doi: 10.1016/j.cmet.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Tian M, Liu W, Li X, Zhao P, Shereen MA, Zhu C, Huang S, Liu S, Yu X, Yue M, et al. HIF-1α promotes SARS-CoV-2 infection and aggravates inflammatory responses to COVID-19. Signal Transduct Target Ther. 2021;6:308. doi: 10.1038/s41392-021-00726-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Tan DX, Reiter RJ. Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality. Life Sci. 2022;294:120368. doi: 10.1016/j.lfs.2022.120368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Huang PY, Wu JY, Liu TH, Tsai YW, Chen PT, Liao CT, Toh HS. The clinical efficacy of melatonin in the treatment of patients with COVID-19: A systematic review and meta-analysis of randomized controlled trials. Front Med (Lausanne) 2023;10:1171294. doi: 10.3389/fmed.2023.1171294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Fara A, Mitrev Z, Rosalia RA, Assas BM. Cytokine storm and COVID-19: A chronicle of pro-inflammatory cytokines. Open Biol. 2020;10:200160. doi: 10.1098/rsob.200160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Reiter RJ, Abreu-Gonzalez P, Marik PE, Dominguez-Rodriguez A. Therapeutic algorithm for use of melatonin in patients with COVID-19. Front Med (Lausanne) 2020;7:226. doi: 10.3389/fmed.2020.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Tan DX, Manchester LC, Terron MP, Flores LJ, Reiter RJ. One molecule, many derivatives: A never-ending interaction of melatonin with reactive oxygen and nitrogen species? J Pineal Res. 2007;42:28–42. doi: 10.1111/j.1600-079X.2006.00407.x. [DOI] [PubMed] [Google Scholar]
- 161.Tan DX, Hardeland R, Manchester LC, Poeggeler B, Lopez-Burillo S, Mayo JC, Sainz RM, Reiter RJ. Mechanistic and comparative studies of melatonin and classic antioxidants in terms of their interactions with the ABTS cation radical. J Pineal Res. 2003;34:249–259. doi: 10.1034/j.1600-079x.2003.00037.x. [DOI] [PubMed] [Google Scholar]
- 162.Rodriguez C, Mayo JC, Sainz RM, Antolín I, Herrera F, Martín V, Reiter RJ. Regulation of antioxidant enzymes: A significant role for melatonin. J Pineal Res. 2004;36:1–9. doi: 10.1046/j.1600-079x.2003.00092.x. [DOI] [PubMed] [Google Scholar]
- 163.Cuzzocrea S, Zingarelli B, Costantino G, Caputi AR. Protective effect of melatonin in a non-septic shock model induced by zymosan in the rat. J Pineal Res. 1998;25:24–33. doi: 10.1111/j.1600-079x.1998.tb00382.x. [DOI] [PubMed] [Google Scholar]
- 164.Cuzzocrea S, Zingarelli B, Gilad E, Hake P, Salzman AL, Szabó C. Protective effect of melatonin in carrageenan-induced models of local inflammation: Relationship to its inhibitory effect on nitric oxide production and its peroxynitrite scavenging activity. J Pineal Res. 1997;23:106–116. doi: 10.1111/j.1600-079x.1997.tb00342.x. [DOI] [PubMed] [Google Scholar]
- 165.El-Sokkary GH, Omar HM, Hassanein AFMM, Cuzzocrea S, Reiter RJ. Melatonin reduces oxidative damage and increases survival of mice infected with Schistosoma mansoni. Free Radic Biol Med. 2002;32:319–332. doi: 10.1016/s0891-5849(01)00753-5. [DOI] [PubMed] [Google Scholar]
- 166.Costantino G, Cuzzocrea S, Mazzon E, Caputi AP. Protective effects of melatonin in zymosan-activated plasma-induced paw inflammation. Eur J Pharmacol. 1998;363:57–63. doi: 10.1016/s0014-2999(98)00673-6. [DOI] [PubMed] [Google Scholar]
- 167.Kong J, Zhang Y, Liu S, Li H, Liu S, Wang J, Qin X, Jiang X, Yang J, Zhang C, Zhang W. Melatonin attenuates angiotensin II-induced abdominal aortic aneurysm through the down-regulation of matrix metalloproteinases. Oncotarget. 2017;8:14283–14293. doi: 10.18632/oncotarget.15093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Zhang Y, Li X, Grailer JJ, Wang N, Wang M, Yao J, Zhong R, Gao GF, Ward PA, Tan DX, Li X. Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome. J Pineal Res. 2016;60:405–414. doi: 10.1111/jpi.12322. [DOI] [PubMed] [Google Scholar]
- 169.Kaivola J, Nyman TA, Matikainen S. Inflammasomes and SARS-CoV-2 infection. Viruses. 2021;13:2513. doi: 10.3390/v13122513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Kucia M, Ratajczak J, Bujko K, Adamiak M, Ciechanowicz A, Chumak V, Brzezniakiewicz-Janus K, Ratajczak MZ. An evidence that SARS-Cov-2/COVID-19 spike protein (SP) damages hematopoietic stem/progenitor cells in the mechanism of pyroptosis in Nlrp3 inflammasome-dependent manner. Leukemia. 2021;35:3026–3029. doi: 10.1038/s41375-021-01332-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Davies DA, Adlimoghaddam A, Albensi BC. The effect of COVID-19 on NF-κB and neurological manifestations of disease. Mol Neurobiol. 2021;58:4178–4187. doi: 10.1007/s12035-021-02438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Manik M, Singh RK. Role of toll-like receptors in modulation of cytokine storm signaling in SARS-CoV-2-induced COVID-19. J Med Virol. 2022;94:869–877. doi: 10.1002/jmv.27405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Li HW, Ying P, Cai QQ, Yang ZH, Wu XL. Exogenous melatonin alleviates hemorrhagic shock-induced hepatic ischemic injury in rats by inhibiting the NF-κB/IκBα signaling pathway. Mol Med Rep. 2021;23:341. doi: 10.3892/mmr.2021.11980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Qin M, Liu Y, Sun M, Li X, Xu J, Zhang L, Jiang H. Protective effects of melatonin on the white matter damage of neonatal rats by regulating NLRP3 inflammasome activity. Neuroreport. 2021;32:739–747. doi: 10.1097/WNR.0000000000001642. [DOI] [PubMed] [Google Scholar]
- 175.Cao S, Shrestha S, Li J, Yu X, Chen J, Yan F, Ying G, Gu C, Wang L, Chen G. Melatonin-mediated mitophagy protects against early brain injury after subarachnoid hemorrhage through inhibition of NLRP3 inflammasome activation. Sci Rep. 2017;7:2417. doi: 10.1038/s41598-017-02679-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Tan DX, Hardeland R. Targeting host defense system and rescuing compromised mitochondria to increase tolerance against pathogens by melatonin may impact outcome of deadly virus infection pertinent to COVID-19. Molecules. 2020;25:4410. doi: 10.3390/molecules25194410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Sygitowicz G, Sitkiewicz D. Molecular mechanisms of organ damage in sepsis: An overview. Braz J Infect Dis. 2020;24:552–560. doi: 10.1016/j.bjid.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Luo J, Song J, Zhang H, Zhang F, Liu H, Li L, Zhang Z, Chen L, Zhang M, Lin D, et al. Melatonin mediated Foxp3-downregulation decreases cytokines production via the TLR2 and TLR4 pathways in H. pylori infected mice. Int Immunopharmacol. 2018;64:116–122. doi: 10.1016/j.intimp.2018.08.034. [DOI] [PubMed] [Google Scholar]
- 179.Xu X, Wang G, Ai L, Shi J, Zhang J, Chen YX. Melatonin suppresses TLR9-triggered proinflammatory cytokine production in macrophages by inhibiting ERK1/2 and AKT activation. Sci Rep. 2018;8:15579. doi: 10.1038/s41598-018-34011-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Feng R, Adeniran SO, Huang F, Li Y, Ma M, Zheng P, Zhang G. The ameliorative effect of melatonin on LPS-induced Sertoli cells inflammatory and tight junctions damage via suppression of the TLR4/MyD88/NF-κB signaling pathway in newborn calf. Theriogenology. 2022;179:103–116. doi: 10.1016/j.theriogenology.2021.11.020. [DOI] [PubMed] [Google Scholar]
- 181.Tan DX, Reiter RJ. Melatonin reduces the mortality of severely-infected COVID-19 patients. Melatonin Res. 2021;4:613–616. [Google Scholar]
- 182.Ren DL, Sun AA, Li YJ, Chen M, Ge SC, Hu B. Exogenous melatonin inhibits neutrophil migration through suppression of ERK activation. J Endocrinol. 2015;227:49–60. doi: 10.1530/JOE-15-0329. [DOI] [PubMed] [Google Scholar]
- 183.Maldonado MD, Mora-Santos M, Naji L, Carrascosa-Salmoral MP, Naranjo MC, Calvo JR. Evidence of melatonin synthesis and release by mast cells. Possible modulatory role on inflammation. Pharmacol Res. 2010;62:282–287. doi: 10.1016/j.phrs.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 184.Muxel SM, Pires-Lapa MA, Monteiro AWA, Cecon E, Tamura EK, Floeter-Winter LM, Markus RP. NF-κB drives the synthesis of melatonin in RAW 264.7 macrophages by inducing the transcription of the arylalkylamine-N-acetyltransferase (AA-NAT) gene. PLoS One. 2012;7:e52010. doi: 10.1371/journal.pone.0052010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Maldonado MD, García-Moreno H, González-Yanes C, Calvo JR. Possible involvement of the inhibition of NF-κB factor in anti-inflammatory actions that melatonin exerts on mast cells. J Cell Biochem. 2016;117:1926–1933. doi: 10.1002/jcb.25491. [DOI] [PubMed] [Google Scholar]
- 186.Hasan MZ, Islam S, Matsumoto K, Kawai T. Meta-analysis of single-cell RNA-seq data reveals phenotypic switching of immune cells in severe COVID-19 patients. Comput Biol Med. 2021;137:104792. doi: 10.1016/j.compbiomed.2021.104792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Cardinali DP, Brown GM, Pandi-Perumal SR. An urgent proposal for the immediate use of melatonin as an adjuvant to anti-SARS-CoV-2 vaccination. Melatonin Res. 2021;4:206–212. [Google Scholar]
- 188.Zipeto D, Palmeira JDF, Argañaraz GA, Argañaraz ER. ACE2/ADAM17/TMPRSS2 interplay may be the main risk factor for COVID-19. Front Immunol. 2020;11:576745. doi: 10.3389/fimmu.2020.576745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Shukla M, Htoo HH, Wintachai P, Hernandez JF, Dubois C, Postina R, Xu H, Checler F, Smith DR, Govitrapong P, Vincent B. Melatonin stimulates the nonamyloidogenic processing of βAPP through the positive transcriptional regulation of ADAM10 and ADAM17. J Pineal Res. 2015;58:151–165. doi: 10.1111/jpi.12200. [DOI] [PubMed] [Google Scholar]
- 190.Zlacká J, Stebelová K, Zeman M, Herichová I. Interactions of renin-angiotensin system and COVID-19: The importance of daily rhythms in ACE2, ADAM17 and TMPRSS2 expression. Physiol Res. 2021;70(S2):S177–S194. doi: 10.33549/physiolres.934754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Hazra S, Chaudhuri AG, Tiwary BK, Chakrabarti N. Matrix metallopeptidase 9 as a host protein target of chloroquine and melatonin for immunoregulation in COVID-19: A network-based meta-analysis. Life Sci. 2020;257:118096. doi: 10.1016/j.lfs.2020.118096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Cecon E, Izabelle C, Poder SL, Real F, Zhu A, Tu L, Ghigna MR, Klonjkowski B, Bomsel M, Jockers R, Dam J. Therapeutic potential of melatonin and melatonergic drugs on K18-hACE2 mice infected with SARS-CoV-2. J Pineal Res. 2022;72:e12772. doi: 10.1111/jpi.12772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Cecon E, Fernandois D, Renault N, Coelho CFF, Wenzel J, Bedart C, Izabelle C, Gallet S, Le Poder S, Klonjkowski B, et al. Melatonin drugs inhibit SARS-CoV-2 entry into the brain and virus-induced damage of cerebral small vessels. Cell Mol Life Sci. 2022;79:361. doi: 10.1007/s00018-022-04390-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Loh D. The potential of melatonin in the prevention and attenuation of oxidative hemolysis and myocardial injury from cd147 SARS-CoV-2 spike protein receptor binding. Melatonin Res. 2020;3:380–416. [Google Scholar]
- 195.Morchang A, Malakar S, Poonudom K, Noisakran S, Yenchitsomanus PT, Limjindaporn T. Melatonin inhibits dengue virus infection via the sirtuin 1-mediated interferon pathway. Viruses. 2021;13:659. doi: 10.3390/v13040659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Zhai X, Wang N, Jiao H, Zhang J, Li C, Ren W, Reiter RJ, Su S. Melatonin and other indoles show antiviral activities against swine coronaviruses in vitro at pharmacological concentrations. J Pineal Res. 2021;71:e12754. doi: 10.1111/jpi.12754. [DOI] [PubMed] [Google Scholar]
- 197.Tesarik J. Melatonin attenuates growth factor receptor signaling required for SARS-CoV-2 replication. Melatonin Res. 2020;3:534–537. [Google Scholar]
- 198.Reiter RJ, Cardinali DP, Neel RL, Rodriguez AD, Brown GM, Tesarik J. Rationale for the continued use of melatonin to combat the delta variant of SARS-CoV-2. Melatonin Res. 2021;4:495–500. [Google Scholar]
- 199.Klann K, Bojkova D, Tascher G, Ciesek S, Münch C, Cinatl J. Growth factor receptor signaling inhibition prevents SARS-CoV-2 replication. Mol Cell. 2020;80:164–174 e4. doi: 10.1016/j.molcel.2020.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Behl T, Kaur I, Aleya L, Sehgal A, Singh S, Sharma N, Bhatia S, Al-Harrasi A, Bungau S. CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target. Sci Total Environ. 2022;808:152072. doi: 10.1016/j.scitotenv.2021.152072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Wang K, Chen W, Zhang Z, Deng Y, Lian JQ, Du P, Wei D, Zhang Y, Sun XX, Gong L, et al. CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells. Signal Transduct Target Ther. 2020;5:283. doi: 10.1038/s41392-020-00426-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Mohamed Taha A, Adel Abdelkader Saed S, Hossam-Eldin Moawad M, Abd El-Tawab Moawad W, Al-Hejazi T, Mousa Y, Sharma R, Reiter RJ. Safety and efficacy of melatonin as an adjuvant therapy in COVID-19 patients: Systematic review and meta-analysis. Adv Med Sci. 2023;68:341–352. doi: 10.1016/j.advms.2023.09.007. [DOI] [PubMed] [Google Scholar]
- 203.Hosseini A, Esmaeili Gouvarchin Ghaleh H, Aghamollaei H, Fasihi Ramandi M, Alishiri G, Shahriary A, Hassanpour K, Tat M, Farnoosh G. Evaluation of Th1 and Th2 mediated cellular and humoral immunity in patients with COVID-19 following the use of melatonin as an adjunctive treatment. Eur J Pharmacol. 2021;904:174193. doi: 10.1016/j.ejphar.2021.174193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Alizadeh Z, Keyhanian N, Ghaderkhani S, Dashti-Khavidaki S, Shokouhi Shoormasti R, Pourpak Z. A Pilot study on controlling coronavirus disease 2019 (COVID-19) inflammation using melatonin supplement. Iran J Allergy Asthma Immunol. 2021;20:494–499. [PubMed] [Google Scholar]
- 205.Darban M, Malek F, Memarian M, Gohari A, Kiani A, Emadi A, Lavvaf S, Bagheri B. Efficacy of high dose vitamin C, melatonin and zinc in iranian patients with acute respiratory syndrome due to coronavirus infection: A pilot randomized trial. J Cell Mol Anesth. 2021;6:164–167. [Google Scholar]
- 206.Farnoosh G, Akbariqomi M, Badri T, Bagheri M, Izadi M, Saeedi-Boroujeni A, Rezaie E, Ghaleh HEG, Aghamollaei H, Fasihi-Ramandi M, et al. Efficacy of a low dose of melatonin as an adjunctive therapy in hospitalized patients with COVID-19: A randomized, double-blind clinical trial. Arch Med Res. 2022;53:79–85. doi: 10.1016/j.arcmed.2021.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Mousavi SA, Heydari K, Mehravaran H, Saeedi M, Alizadeh-Navaei R, Hedayatizadeh-Omran A, Shamshirian A. Melatonin effects on sleep quality and outcomes of COVID-19 patients: An open-label, randomized, controlled trial. J Med Virol. 2022;94:263–271. doi: 10.1002/jmv.27312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Chavarría AP, Vázquez RRV, Cherit JGD, Bello HH, Suastegui HC, Moreno-Castañeda L, Alanís Estrada G, Hernández F, González-Marcos O, Saucedo-Orozco H, et al. Antioxidants and pentoxifylline as coadjuvant measures to standard therapy to improve prognosis of patients with pneumonia by COVID-19. Comput Struct Biotechnol J. 2021;19:1379–1390. doi: 10.1016/j.csbj.2021.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Esmaeili Gouvarchin Ghaleh H, Hosseini A, Aghamollaei H, Fasihi-Ramandi M, Alishiri G, Saeedi-Boroujeni A, Hassanpour K, Mahmoudian-Sani MR, Farnoosh G. NLRP3 inflammasome activation and oxidative stress status in the mild and moderate SARS-CoV-2 infected patients: Impact of melatonin as a medicinal supplement. Z Naturforsch C J Biosci. 2021;77:37–42. doi: 10.1515/znc-2021-0101. [DOI] [PubMed] [Google Scholar]
- 210.Bologna C, Madonna P, Pone E. Efficacy of prolonged-release melatonin 2 mg (PRM 2 mg) prescribed for insomnia in hospitalized patients for COVID-19: A retrospective observational study. J Clin Med. 2021;10:5857. doi: 10.3390/jcm10245857. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.