Abstract
This systematic review aimed to evaluate the effect of telerehabilitation on improving physical activity, physical function, and quality of life in patients with osteoarthritis (OA). A systematic review of randomized controlled trial studies was conducted without a time limit by searching for keywords in the title, abstract, and study keywords in the scientific databases Embase, Web of Science, Scopus, and PubMed on October 20, 2021. This study was conducted according to Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. Titles and abstracts were retrieved based on the inclusion, exclusion, and quality assessment criteria. Then, full texts were retrieved and reviewed independently by two separate authors based on the eligibility criteria. Disputes were resolved through discussion. A form with the same predefined elements was used to extract data. Totally, eight eligible articles were found through this review. The studies on telerehabilitation approaches were categorized into three categories, which are: home-based exercise programs by online mobile applications, sports counseling and physiotherapist support via telephone calls, and Internet-based exercise training (IBET). In four studies (57%), telerehabilitation was effective in the short term for some months and improved the performance, self-efficacy, and quality of life of participants. On the other hand, in the long-term effects, there was no difference in participants' improvement (43%). In long-term follow-up, there was no difference between the efficiency of traditional rehabilitation and telerehabilitation in improving the physical performance and quality of life. However, telerehabilitation can be a viable alternative to traditional physiotherapy in patients with OA.
Keywords: Exercise, osteoarthritis, telemedicine, telerehabilitation
Introduction
Osteoarthritis (OA) is the most prevalent chronic condition of the knees. The worldwide prevalence estimates for OA are about 13% in women and 10% in men aged 60 years and older.[1,2] Thus, the demand for health services increases. Over time, knee OA causes pain, inactivity, and thereby negatively affects the quality of life of patients.[3] Often, immobility caused by knee OA causes obesity, which increases the problems and complications caused by OA because obesity increases the load on the knee joint due to the heavy weight that the knee bears.[4]
Physical therapist intervention consisting of muscle strengthening exercises and patient education has shown to be effective in reducing the levels of pain and improving physical functioning.[5] These therapeutic strategies may also have beneficial effects on a person's mental and behavioral health.[6] In this regard, the American College of Sports Medicine states that “exercise is medicine.” It continues that exercise, which includes both aerobic and resistance exercises, is an effective interventional recommendation for the treatment of knee OA.[5]
Traditional (face-to-face) physical therapy sessions are costly for many people and their access is restricted by geography.[7] Telerehabilitation is a promising strategy, particularly for the early stage of a remote therapeutic exercise program.[8] Telerehabilitation provides rehabilitation services using various technologies, including virtual reality, mobile phone applications, artificial intelligence, iPad, mobile games, online video conferencing, and others.[9,10,11,12,13,14] Previous studies have shown that telerehabilitation is effective, safe, and feasible in patients with chronic obstructive pulmonary disease,[15] patients with coronavirus disease 2019 (COVID-19),[16] and patients undergoing chemotherapy.[17] Also, Baigi et al.[18] reported that telerehabilitation services are more cost-effective and, at the same time, have the same treatment results compared to traditional (face-to-face) rehabilitation. On the other hand, Jiang et al.[19] reported in their systematic review and meta-analysis that telerehabilitation for patients after knee arthroplasty, in contrast to traditional rehabilitation, had a better effect on functional improvement and subsequently the quality of life of patients. Due to the moment-to-moment access to treatment, telerehabilitation improves treatment compliance, reduces trips to the doctor's office, and ultimately improves patient satisfaction.[20] A recent systematic review found that telerehabilitation improved treatment adherence and may offer promising results.[21]
To date, many studies have investigated the effect of telerehabilitation in patients with OA. However, randomized controlled trials (RCTs) provide the strongest evidence in any field. Therefore, this systematic review of RCT studies was conducted with the aim of evaluating the effect of telerehabilitation on improving physical activity, physical function, and quality of life in patients with OA. In other words, we are looking to investigate the effect of telerehabilitation compared to traditional (face-to-face) rehabilitation in patients with OA. To address the objective, the Population, Intervention, Comparison and Outcomes PICOS criteria were set, as outlined in Appendix 1.
Materials and Methods
Study design
This study was conducted according to Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines to report on evidence from the studies that were included in this systematic review.[22,23] This study was approved by the ethical committee of Mashhad University of Medical Sciences (approval number IR.MUMS.REC.1400.296). We conducted a literature search without a time limit on the PubMed, Embase, Scopus, and Web of Science databases on October 20, 2021. The following keywords and MeSH terms were used to conduct the databases search: (“physical therapy modalities,” “exercise therapy,” “ physical therapy,” “physiotherapy,” “exercise”) AND (“telemedicine,” “telerehabilitation,” “telehealth,” “mobile health,” “eHealth,” “mHealth”). The “randomized control trial” filter was applied to the search strategy. All articles from the systematic search were collected, and duplicate articles were excluded from this study. Titles and abstracts were retrieved based on the inclusion, exclusion, and quality assessment criteria. Then, full texts were retrieved and reviewed independently by two separate authors based on the eligibility criteria. Disputes were resolved through discussion.
Eligibility criteria
Studies were included if they met the following inclusion criteria: original RCTs that used telerehabilitation or tele physiotherapy modalities to improve the physical function and physical activity in patients with OA. On the other hand, the exclusion criteria were 1) type of publication other than journal articles (e.g., books, review papers, and letters); 2) lack of availability of the full text in the English language; and 3) lack of relation of the title, abstract, or full text of the papers to the aim of the study.
Data extraction and synthesis
A form with the same predefined elements was used to extract data. The data items in this form included the following: publication title, first author's name, publication year, participants' characteristics, study design, the telerehabilitation approach that was used, intervention characteristics, study goals, and main study findings.
Quality assessment
The evaluation of the quality of the included studies in this review was done using the evaluation checklist of the Joanna Briggs Institute (JBI) for RCTs.[24] This checklist contains 13 questions for evaluating RCT studies, for example, questions such as blinding of the researcher, participants, analyst, how to randomize, data analysis, and so on. If the answer to a question was “yes,” it was scored “1,” and otherwise, it was scored “0.” As a result, the maximum quality score of the included studies was 13, and studies with an evaluation score of less than 7 were excluded from this systematic review.
Results
Study selection
As shown in Figure 1, in total, 2142 documents were initially retrieved through scientific database searching and three documents from gray literature searching, 683 of which were duplicates. Among the retrieved articles, 83 documents were excluded after the title and abstract screening. Finally, eight eligible articles were found through this review.
Figure 1.
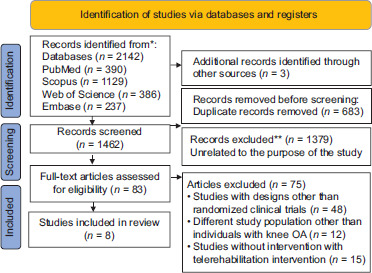
Flow diagram of the literature search and study selection
Quality assessment
Table 1 shows the result of the quality assessment of the included studies. There was no significant bias in the studies, and most of the included studies were of moderate to high quality. Therefore, all RCT studies were included in this systematic review.
Table 1.
Results of quality assessment of the included studies based on the JBI checklist for RCTs
| Reference | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | Quality assessment score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [25](2020, Saudi Arabia) | Ya | Y | Y | Nb | N | N | Y | Y | Y | Y | Y | Y | Y | 10 |
| [26](2020, Australia) | Y | Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | 10 |
| [27](2021, Taiwan) | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | 11 |
| [28](2018, The Netherlands) | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | Y | Y | 10 |
| [29](2018, Australia) | Y | Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | 10 |
| [30](2017, Australia) | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | Y | Y | 10 |
| [31](2017, Iran) | Y | N | Y | N | N | N | Y | Y | N | Y | Y | Y | Y | 8 |
| [32](2018, USA) | Y | N | Y | Y | N | N | Y | Y | N | Y | Y | Y | Y | 9 |
JBI=Joanna Briggs Institute, RCT=randomized controlled trial. aY=Yes. bN=No
Study characteristics
This review included 8 eligible studies.[25,26,27,28,29,30,31,32] The characteristics of all included studies are reported in Table 2. Of the eight included studies, three (30%) studies were conducted in Australia[26,29,30] and other studies in Taiwan,[27] the Netherlands,[28] Saudi Arabia,[25] Iran,[31] and the USA.[32] Studies' sample sizes ranged from 40[25] to 350 participants.[32] The average or median age of participants ranged from 54.4[25] to 65.3 years.[32] Study designs were classified into two categories: RCTs (7/8, 87.5%)[25,26,27,29,30,31,32] and cluster RCT (1/8, 12.5(.[28] Follow-up periods ranged from 6 weeks[31] to 12 months.[26,28,32]
Table 2.
Summary of study characteristics of participants from all included studies
| Reference | Participants' characteristics |
Duration of interventions | |
|---|---|---|---|
| Number of participants | Mean age of participants | ||
| [25](2020, Saudi Arabia) | 40 | 54.4 | 14 weeks |
| [26](2020, Australia) | 175 | 62.45 | 12 months |
| [27](2021, Taiwan) | 66 | 65.26 | 12 weeks |
| [28](2018, The Netherlands) | 208 | 62.9 | 12 months |
| [29](2018, Australia) | 148 | 60.8 | 9 months |
| [30](2017, Australia) | 168 | 62.25 | 6 months |
| [31](2017, Iran) | 54 | 55.5 | 6 weeks |
| [32](2018, the USA) | 350 | 65.3 | 12 months |
Telerehabilitation approaches
As shown in Table 3, telerehabilitation approaches included studies that were categorized into three groups: of the eight studies, two (25%) used home-based exercise programs by online mobile applications,[25,28] four (50%) used sports counseling and physiotherapist support via telephone calls,[26,27,30,31] and two (25%) used Internet-based exercise training (IBET).[29,32] These programs provide guidance on exercise performance and exercise movements. For example, isometric quadriceps contractions, isotonic quadriceps contractions, isotonic hamstring contractions, resistance band isotonic quadriceps contractions, straight leg raises, lateral hip abductions, partial squats, dynamic stepping exercises, side steps with resistance around the thigh or ankle, etc., These programs support features such as alerts and a monitoring system controlled by the physiotherapist. It also offers automatic recording of exercise adherence, including time and sessions completed. Hence, it enables the physiotherapist to monitor the participant's adherence to the prescribed exercises.
Table 3.
Summary of characteristics of all included studies
| Reference | Study goals | Telerehabilitation approach | Study results | Study conclusions |
|---|---|---|---|---|
| [25](2020, Saudi Arabia) | The effects of an Arabic smartphone application on adherence to home exercise programs and the effectiveness of these programs on pain, physical function, and muscle strength of the lower extremities in elderly women with osteoarthritis of the knee | Smartphone application | The intervention group was more committed to home exercise programs (P=002) and reported a significant reduction in pain (P=015) | A mobile phone-based app with motivational and engaging features can increase adherence to HEPs in patients with knee OA. Mobile phone-based applications supported by attractive and motivational features can be an effective strategy to increase HEP adherence among elderly with knee OA |
| [26](2020, Australia) | Evaluation of telephone exercise recommendations and physiotherapist supportive intervention for people with knee OA | Telephone consultation with physiotherapist consultation to receive a personal plan | At 6 months, exercise counseling and support improved performance (mean difference 4.7), but overall pain did not improve (0.7). At 12 months, most results were similar between groups | Exercise advice and physical therapist support over the phone improved the physical performance of patients with knee OA, but the joint outcome of knee pain at 6 months was not sufficient. Functional benefits were not maintained at 12 months. The clinical significance of this effect is unclear |
| [27](2021, Taiwan) | Evaluation of the effects of nutrition-based resistance interventions and telemedicine at home on improving body composition, blood biochemistry, and functional activity of the lower extremities | Diet control plus elastic band exercise group (D+E) via telephone calls or a communication application | After 12 weeks of intervention, the control group (P<0.001) and the intervention group (P<0.001) achieved significant weight loss | A personalized diet control intervention combined with a telemedicine-based resistance training intervention effectively improved body composition, blood biochemistry, and functional activity of the lower limbs in patients with knee OA |
| [28](2018, the Netherlands) | Evaluation of short-term and long-term efficacy of e-exercise in comparison to conventional physiotherapy in people with hip/knee OA | Online mobile application | No significant difference in initial outcomes was found between the e-exercise group and the conventional physiotherapy group | The combined intervention, e-exercise, was no more effective than conventional physical therapy in subjects with hip/knee OA. However, within-group differences showed that both interventions were significantly effective with regard to physical function and most secondary outcomes immediately after treatment and after 12 months. Reducing face-to-face meetings may lead to lower health-care costs |
| [29](2018, Australia) | Evaluation of the effect of an Internet-based intervention on changes in pain and physical function in people with OA of the knee | Internet training + online interactive automated pain-coping skills training program | The intervention group had significantly more pain reduction at 3 months than the control group (P=0.02) | Patients who were employed and had higher self-efficacy at baseline were more likely to experience greater improvement in pain at 3 months after an Internet-based exercise, education, and pain-coping skills program. The results support the effectiveness of Internet-based care for a wide range of people with knee OA, but future confirmatory research is needed |
| [30](2017, Australia) | Investigate whether simultaneous telephone coaching improves the clinical effectiveness of a physiotherapist-prescribed home-based physical activity program for knee OA | Five 30-min consultations with a physiotherapist + telephone coaching sessions | Change in pain and physical function at 6 months did not differ between groups. However, both groups showed clinically relevant improvements. Some secondary outcomes related to physical activity and exercise behavior favored coaching at 6 months, but not overall at 12 or 18 months. There were no between-group differences in most other outcomes | Adding concurrent telephone coaching did not increase the pain and performance benefits of a physical therapist-administered home-based physical activity program. However, a mobile phone program improved patient adherence |
| [31](2017, Iran) | Comparison of the efficacy of telerehabilitation to OBPT in patients with knee OA | Telerehabilitation (pamphlet containing descriptions and pictures detailing and phone call) | There was no significant difference between telerehab and OBPT groups in any of the studied scales | Telerehabilitation program is as effective as OBPT in improving the function of patients with knee OA. Due to the much lower time and cost involved in telerehabilitation, this program is recommended for the older population living in remote locations |
| [32](2018, the USA) | Comparison of the effectiveness of physical therapy (evidence-based approach) and IBET, each vs a WL control, among individuals with knee OA | IBET | Similarly, at 12 months, the mean differences compared to WL were not statistically significant for either group. IBET was noninferior to physical therapy at both time points | There was no significant difference between the investigated outcomes in the two groups. Further studies are needed to investigate strategies to maximize the benefits of exercise-based interventions for patients with knee OA |
IBET=Internet-based exercise training, OA=osteoarthritis, OBPT=office-based physical therapy, WL=waitlist, HEPs=Home-based exercise programs
Effects of telerehabilitation on patients with OA
In three studies, no significant differences were reported between traditional (face-to-face) physiotherapy and telerehabilitation approaches in improving participants' performance.[28,31,32] In addition, in one study, the effect of telerehabilitation as an adjunct intervention along with face-to-face physiotherapy counseling was measured, but there was no significant difference in improving the physical function in participants between the control and intervention groups.[30] However, in three of the studies, the results showed better improvement in performance and reduction of pain in the telerehabilitation approach.[25,27,29] Also, one study supported the short-term effects of an exercise program with a telerehabilitation approach.[26]
Discussion
Principal findings
This systematic review aimed to evaluate the effect of telerehabilitation on improving physical activity, physical function, and quality of life in patients with OA. The results of the systematic review showed that telerehabilitation was effective in the short term (3–4 months) and improved the performance, self-efficacy, and quality of life of participants.[25,26,27,29] Alasfour et al.[25] conducted a study with the aim of investigating the effects of an Arabic smartphone application on adherence to home exercise programs and its effectiveness on improving pain, physical function, and muscle strength of the lower limbs in older women with knee OA. They concluded that at the end of the sixth week, the intervention group was more adherent to the treatment. They also stated that the adherence rate in the intervention group was better due to the features of the remote rehabilitation program, the patient's adherence to exercise at home requires behavioral changes, and the features of the program can have the potential to change the patient's behavior. These features include automatic reminders to follow the program, a physical therapist monitoring system that promotes better adherence to treatment.[25] Also, Hinman et al.[26] reported that physical therapist-led exercise advice and support over the phone moderately improved patients' physical activity, but this improvement was not maintained at 12 months.
This may be justified in this way. Just as the body gets used to a drug after a while and no longer responds to it, a monotonous telerehabilitation intervention loses its appeal to its users after a short period of time. Therefore, as Mousavi et al.[15,16] stated in their recent study, the use of multiple technologies in combination may have a better effect than a program based on one technology.
Pérez-Manchَn et al.[33] stated that asynchronous telemedicine can be an efficient way to provide remote health-care services. However, this method still requires the active participation of therapists to review the videotaped session. Sensor-based telerehabilitation programs are more independent services than video communication, as they use one or more sensors to record the patient's physical activity and collect motion data using software that runs on a computer device (computer, smartphone, tablet). Ayoade and Baillie[34] demonstrated that a sensor-based telerehabilitation program can increase flexibility and time independence for patients using semi-supervised training sessions.
On the other hand, interactive telerehabilitation can provide real-time graphical feedback of the patient's performance using software, enabling users to review their performance over time.
Recent studies have shown that the expert system can partially or completely interact with the patient and assume the responsibilities of the therapist.[35,36]
Russell[37] also identified telerehabilitation programs based on virtual reality as a mode of telerehabilitation. On the other hand, colleagues found that video-based remote rehabilitation programs can be considered the best alternative solution to conventional treatment. Allegue et al.[38] also stated that a combined approach of telerehabilitation may have a better effect than single interventions.
On the other hand, in the long-term effects (9–12 months), there was no difference in participants' improvement.[28,30,32] Kloek et al.[28] reported that no significant difference was observed in the functional status of patients in both groups (in-person physical therapy vs. in-person physical therapy plus online exercise program), However, the participants in the physical therapy group attended 12 sessions and the participants in the intervention attended only five sessions. This reduction in face-to-face visit sessions may lead to a reduction in patient rehabilitation costs.
On the other hand, telerehabilitation is a cost-effective, safe, efficient, and feasible approach.[25,26,27,28,29,30,32,39,40,41,42,43,44,45,46,47,48,49] The type of telerehabilitation approach was simultaneous in all interventions and did not show a difference in performance or physical improvement.
In line with the results of this study, Latif-Zade et al.[50] conducted a systematic review to evaluate the effectiveness of telerehabilitation in reducing pain in patients with OA of the knee. The results of three RCT studies obtained by them showed that telerehabilitation has a similar efficiency in reducing pain in people with OA. In addition, Jansson et al.,[51] in their systematic review, concluded that patients who completed telerehabilitation showed an improvement in physical function, which was similar to that of patients who underwent routine outpatient physiotherapy, without increased side effects or resource use. However, the effect of telerehabilitation on physical performance was assessed as a heterogeneous evidence of moderate to low quality.
Strengths and limitations
This study was the first systematic review of RCT studies to investigate the effect of telerehabilitation on improving physical activity, physical function, and quality of life in patients with OA. One of the limitations of this systematic review was the small number of included studies, which makes definitive conclusions impossible. Also, the included studies used different methods to measure telerehabilitation outcomes. Therefore, it was not possible to conduct a meta-analysis and examine the effect of these studies as a group.
Conclusion
This review shows that in recent years, technology-based solutions have also become more popular due to rapid advances and improved patient adherence to treatment. Especially for improving the physical activity and subsequently the quality of life of patients with knee OA, one of the most important requirements that helps in their recovery is long-term adherence to the treatment process. Although in the short term, the follow-up of patients with knee OA in the remote rehabilitation group showed a better improvement in the physical activity compared to traditional rehabilitation, these results were not maintained in the long term. The use of combined technology approaches may improve these outcomes by increasing attractiveness and encouraging patients to adhere to treatment. However, future studies are needed to confirm this.
Author's contributions
Conceptualization and Design: SFMB, MS. Literature search: SFMB, KK. Data acquisition: KGH, MRM, ASM. Screening and analysis: KK, ASM. Manuscript preparation: SFMB, KGH. Manuscript editing: KK, MS. All authors read and approved the final version of the manuscript.
Compliance with ethical guidelines
This study was approved by the ethical committee of Mashhad University of Medical Sciences (approval number IR.MUMS.REC.1400.296).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We hereby thank and appreciate all the researchers around the world who have done research in the field of telerehabilitation in improving the physical activity of patients with osteoarthritis. In addition, we are also grateful to the members of the Student Research Committee of Mashhad University of Medical Sciences who helped us in conducting this research.
Appendix 1: PICOS Criteria
| Criteria | PICOS question |
|---|---|
| Population | Patients with OA |
| Intervention | Telerehabilitation interventions |
| Comparison | Standard (face - to – face) care procedures. |
| Outcomes | The outcome of physical activity, physical function and quality of life related to the use of telerehabilitation interventions |
| Study | Randomized controlled trials |
References
- 1.Dekker J.Exercise and Physical Functioning in Osteoarthritis: Medical, Neuromuscular and Behavioral Perspectives. Springer Science & Business Media; 2013 [Google Scholar]
- 2.Zhang Y, Jordan JM.Epidemiology of osteoarthritis Clin Geriatr Med 201026355–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anwer S, Alghadir A, Brismée J-M.Effect of home exercise program in patients with knee osteoarthritis: A systematic review and meta-analysis J Geriatr Phys Ther 20163938–48 [DOI] [PubMed] [Google Scholar]
- 4.Blagojevic M, Jinks C, Jeffery A, Jordan K.Risk factors for onset of osteoarthritis of the knee in older adults: A systematic review and meta-analysis Osteoarthritis Cartilage 20101824–33 [DOI] [PubMed] [Google Scholar]
- 5.Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;1:CD004376. doi: 10.1002/14651858.CD004376.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moreira-Neto A, Martins B, Miliatto A, Nucci MP, Silva-Batista C. Can remotely supervised exercise positively affect self-reported depressive symptoms and physical activity levels during social distancing? Psychiatr Res. 2021;301:113969. doi: 10.1016/j.psychres.2021.113969. [DOI] [PubMed] [Google Scholar]
- 7.Bates S, Smedley C, Wong M, Kayess R, Fisher K.Arthritis and Disability. Social Policy Research Centre; 2014 [Google Scholar]
- 8.Kolasinski SL Neogi T Hochberg MC Oatis C Guyatt G Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee Arthritis Rheumatol 202072220–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghaddaripouri K, Baigi SFM, Noori N, Habibi MRM. Investigating the effect of virtual reality on reducing the anxiety in children: A systematic review. Front Health Inform. 2022;11:114. [Google Scholar]
- 10.Mousavi Baigi SF, Moradi F, Vasseifard F, Mohammad Abadi F, Mazaheri Habibi MR.The effect of nutrition training on knowledge of students at university of medical sciences Top Clin Nutr 202237236–41 [Google Scholar]
- 11.Mousavi Baigi SF, Sarbaz M, Marouzi P, Kimiafar K.Evaluating the Impact of Digital Game on Learning Medical Terminology of Paramedical Students: Protocol for a Randomized Controlled Trial Advances in Informatics, Management and Technology in Healthcare: IOS Press; 2022. p. 51–4 [DOI] [PubMed] [Google Scholar]
- 12.Mousavi Baigi SF, Aval RN, Sarbaz M, Kimiafar K.Evaluation tools for digital educational games: A systematic review Acta Med Iran 2022;60. doi: 10.18502/acta.v60i8.10835 [Google Scholar]
- 13.Baigi SFM, Baigi SMM, Habibi MRM. Challenges and opportunities of using telemedicine during Covid-19 epidemic: A systematic review. Front Health Inform. 2022;11:109. [Google Scholar]
- 14.Ku BPS, Tse AWS, Pang BCH, Cheung NT, Pang JYW, Chan JKY, et al. Tele-rehabilitation to combat rehabilitation service disruption during COVID-19 in Hong Kong: Observational study. JMIR Rehabil Assist Technol. 2021;8:e19946. doi: 10.2196/19946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baigi SFM, Sarbaz M, Ghaddaripouri K, Noori N, Kimiafar K. The effect of tele-rehabilitation on improving physical activity in patients with chronic obstructive pulmonary disease: A systematic review of randomized controlled clinical trials. Front Health Inform. 2022;11:113. [Google Scholar]
- 16.Mousavi Baigi SF, Raei Mehneh M, Sarbaz M, Norouzi Aval R, Kimiafar K.Telerehabilitation in response to critical coronavirus: A systematic review based on current evidence J Isfahan Med Sch 202240498–508 [Google Scholar]
- 17.Sarbaz M, Monazah FM, Eslami S, Kimiafar K, Baigi SF. Effect of mobile health interventions for side effects management in patients undergoing chemotherapy: A systematic review. Health Policy Technol. 2022;11:100680. [Google Scholar]
- 18.Baigi SFM, Mousavi AS, Kimiafar K, Sarbaz M. Evaluating the cost effectiveness of tele-rehabilitation: A systematic review of randomized clinical trials. Front Health Inform. 2022;11:118. [Google Scholar]
- 19.Jiang S, Xiang J, Gao X, Guo K, Liu B.The comparison of telerehabilitation and face-to-face rehabilitation after total knee arthroplasty: A systematic review and meta-analysis J Telemed Telecare 201824257–62 [DOI] [PubMed] [Google Scholar]
- 20.Peretti A, Amenta F, Tayebati SK, Nittari G, Mahdi SS. Telerehabilitation: Review of the state-of-the-art and areas of application. JMIR Rehabil Assist Technol. 2017;4:e7511. doi: 10.2196/rehab.7511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Valenzuela T, Okubo Y, Woodbury A, Lord SR, Delbaere K.Adherence to technology-based exercise programs in older adults: A systematic review J Geriatr Phys Ther 20184149–61 [DOI] [PubMed] [Google Scholar]
- 22.Liberati A Altman DG Tetzlaff J Mulrow C Gøtzsche PC Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration J Clin epidemiol 200962e1–e34 [DOI] [PubMed] [Google Scholar]
- 23.Moher D Liberati A Tetzlaff J Altman DG Altman D Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement (Chinese edition) J Chin Integr Med 20097889–96 [Google Scholar]
- 24.Joanna Briggs Institute Critical Appraisal Checklist for Randomized Controlled Trials. 2017. Avaliable from [https://jbi.global/sites/default/files/2019-05/JBI_RCTs_Appraisal_tool2017_0.pdf] [Google Scholar]
- 25.Alasfour M, Almarwani M.The effect of innovative smartphone application on adherence to a home-based exercise programs for female older adults with knee osteoarthritis in Saudi Arabia: A randomized controlled trial Disabil rehabil 2022442420–7 [DOI] [PubMed] [Google Scholar]
- 26.Hinman RS Campbell PK Lawford BJ Briggs AM Gale J Bills C, et al. Does telephone-delivered exercise advice and support by physiotherapists improve pain and/or function in people with knee osteoarthritis? Telecare randomised controlled trial Br J Sports Med 202054790–7 [DOI] [PubMed] [Google Scholar]
- 27.Hsu Y-I, Chen Y-C, Lee C-L, Chang N-J. Effects of diet control and telemedicine-based resistance exercise intervention on patients with obesity and knee osteoarthritis: A randomized control trial. Int J Environ Res Public Health. 2021;18:7744. doi: 10.3390/ijerph18157744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kloek CJ, Bossen D, Spreeuwenberg PM, Dekker J, de Bakker DH, Veenhof C.Effectiveness of a blended physical therapist intervention in people with hip osteoarthritis, knee osteoarthritis, or both: A cluster-randomized controlled trial Phys Ther 201898560–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lawford BJ, Hinman RS, Kasza J, Nelligan R, Keefe F, Rini C, et al. Moderators of effects of internet-delivered exercise and pain coping skills training for people with knee osteoarthritis: Exploratory analysis of the IMPACT randomized controlled trial. J Med Intern Res. 2018;20:e10021. doi: 10.2196/10021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bennell KL Campbell PK Egerton T Metcalf B Kasza J Forbes A, et al. Telephone coaching to enhance a home-based physical activity program for knee osteoarthritis: A randomized clinical trial Arthritis Care Res 20176984–94 [DOI] [PubMed] [Google Scholar]
- 31.Azma K, RezaSoltani Z, Rezaeimoghaddam F, Dadarkhah A, Mohsenolhosseini S.Efficacy of tele-rehabilitation compared with office-based physical therapy in patients with knee osteoarthritis: A randomized clinical trial J Telemed Telecare 201824560–5 [DOI] [PubMed] [Google Scholar]
- 32.Allen K Arbeeva L Callahan LF Golightly YM Goode AP Heiderscheit B, et al. Physical therapy vs internet-based exercise training for patients with knee osteoarthritis: Results of a randomized controlled trial Osteoarthritis Cartilage 201826383–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pérez-Manchَn D, Caramés-Sلnchez C, Pfang B.An asynchronous telemedicine program: Three years' experience with African patients treated in Spain J Telemed Telecare 201623558–60 [DOI] [PubMed] [Google Scholar]
- 34.Ayoade M, Baillie L.A novel knee rehabilitation system for the home New York NY United States: Association for Computing Machinery; 2014. Presented at: Proceedings of the 32nd annual ACM conference on Human factors in computing systems-CHI '14; 26 Apr-1 May; Toronto Ontario Canada. p. 2521–30 [Google Scholar]
- 35.Bossen D, Veenhof C, Van Beek KE, Spreeuwenberg PM, Dekker J, De Bakker DH. Effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis: Randomized controlled trial. J Med Intern Res. 2013;15:e257. doi: 10.2196/jmir.2662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rini C Porter LS Somers TJ McKee DC DeVellis RF Smith M, et al. Automated Internet-based pain coping skills training to manage osteoarthritis pain: A randomized controlled trial Pain 2015156837–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Russell TG.Physical rehabilitation using telemedicine J Telemed Telecare 200713217–20 [DOI] [PubMed] [Google Scholar]
- 38.Allegue D, Kairy D, Higgins J, Archambault P, Michaud F, Miller W, et al. Optimization of upper extremity rehabilitation by combining telerehabilitation with an exergame in people with chronic stroke: Protocol for a mixed methods study. JMIR Res Protoc. 2020;9:e14629. doi: 10.2196/14629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mousavi Baigi SF, Sarbaz M, Ghaddaripouri K, Ghaddaripouri M, Mousavi AS, Kimiafar K. Attitudes, knowledge, and skills towards artificial intelligence among healthcare students: A systematic review. Health Sci Rep. 2023;6:e1138. doi: 10.1002/hsr2.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mousavi Baigi SF, Sarbaz M, Sobhani-Rad D, Kimiafar K.A comparative study of rehabilitation information systems in 8 countries: a literature review Iran Rehabil J 2023211–6 [Google Scholar]
- 41.Ghaddaripouri K, Mousavi Baigi SF, Abbaszadeh A, Mazaheri Habibi MR. Attitude, awareness, and knowledge of telemedicine among medical students: A systematic review of cross-sectional studies. Health Sci Rep. 2023;6:e1156. doi: 10.1002/hsr2.1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baigi SF, Sarbaz M, Sobhani-Rad D, Mousavi AS, Kimiafar K. Rehabilitation registration systems: Current recommendations and challenges. Frontiers in Health Informatics. 2022;11:124. [Google Scholar]
- 43.Baigi SF Sarbaz M Sobhani-Rad D Dahmardeh F Mehneh MR Mousavi AS, et al. Rehabilitation information systems: What we know and what we want Int J Health Sci 2022648241–55 [Google Scholar]
- 44.Mousavi Biagi SF, Mousavi AS, Kimiafar K, Sarbaz M.The effect of telerehabilitation on people with sensory disabilities: A systematic review Health Management & Information Science (JHMI) 20229119–28 [Google Scholar]
- 45.Mousavi AS, Baigi SF, Dahmardeh F, Mehneh MR, Darrudi R. Teleophthalmology: A Systematic Review of Randomized Controlled Trials. Frontiers in Health Informatics. 2023;12:141. [Google Scholar]
- 46.Sarbaz M, Yazdipour AB, Fatemeh S.Use of Digital Games for Educational Purposes Among Medical and Paramedical Sciences Students, Mashhad, Iran Stud Health Technol Inform 2023302443–7 [DOI] [PubMed] [Google Scholar]
- 47.Mousavi AS, Darroudi R, Abbaszadeh A, Dahmardeh F, Fatemeh S, Baigi M.The Effect of Telemedicine on the Recovery of Patients with Chronic Gastrointestinal Disease: A Systematic Review of Randomized Controlled Trials Paramedical Sciences and Military Health 20231761–71 [Google Scholar]
- 48.Kimiafar K Mousavi AS Baigi SF Dahmardeh F Layen GS Monazah FM, et al. Effect of Mobile Health Interventions for Side Effects Management in Patients Undergoing Radiotherapy: A Systematic Review Clin Cancer Investig J 202211;1S; CCLS220384 [Google Scholar]
- 49.Mousavi Baigi SF, Kimiafar K, Sarbaz M, Abbaszadeh A, Mousavi AS.Effect of Telemedicine in Military Medicine: A Literature Review Paramedical Sciences and Military Health 20231777–89 [Google Scholar]
- 50.Latif-Zade T, Tucci B, Verbovetskaya D, Bialkin E, Ng B, Heddon S, et al. Systematic review shows tele-rehabilitation might achieve comparable results to office-based rehabilitation for decreasing pain in patients with knee osteoarthritis. Medicina. 2021;57:764. doi: 10.3390/medicina57080764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jansson MM, Rantala A, Miettunen J, Puhto A-P, Pikkarainen M.The effects and safety of telerehabilitation in patients with lower-limb joint replacement: A systematic review and narrative synthesis J Telemed Telecare 20222896–114 [DOI] [PubMed] [Google Scholar]


