Abstract
This study investigates the feasibility and the preliminary efficacy of a Cognitive Stimulating Play Intervention on cognitive functions. Thirty older people with early to moderate dementia were recruited from 2 day-care centers, which were randomized into intervention and control groups. The recruitment, attendance, completion rates, and the interview with staff showed that the intervention was feasible. Analysis of covariance results showed that there was a significant difference between groups on memory storage and retrieval functions. The mean memory storage and retrieval functions were 5.92 (95% confidence interval [CI]: 1.83-9.91; P = .006) and 4.12 (95% CI: 0.75-7.50; P = .018) points higher than that for the control group, respectively, which contributed moderate to large effects (partial η2 = 0.189-0.248). There was no significant difference between groups in global cognition measured using the Montreal Cognitive Assessment and verbal fluency. Practical issues that emerged during implementation were discussed.
Keywords: play, cognitive functions, memory, verbal fluency, dementia
Introduction
Dementia is a neurocognitive disease characterized by progressive and global deterioration in cognitive functions including memory, language, and other executive functions. Around 47 million people worldwide are affected by dementia, and the number is projected to triple in 2050. 1 Currently, there are no available treatments to reverse the pathological changes in the brain that are associated with degenerative dementia. It is therefore important to devise strategies to delay and/or halt the cognitive decline of People with Dementia (PWD). There are 3 main approaches to cognitive interventions aimed at improving the cognition of PWD, namely cognitive training, cognitive rehabilitation, and cognitive stimulations. 2 Cognitive stimulation is the only nonpharmacological approach that the UK’s National Institute for Health and Clinical Excellence has recommended for enhancing the cognitive functions of PWD. 3
Cognitive stimulation requires participants to engage in a range of activities and group discussions aimed at generally enhancing cognitive and social functioning. 4 These activities will activate the neurons and eventually lead to a general improvement in cognitive functions. 5 In addition, through engaging in pleasurable activities, excessive disability in cognitive functions can be minimized. 6 A Cochrane meta-analysis and several systematic reviews and/or meta-analyses have also confirmed the efficacy of cognitive stimulation in bringing about cognitive improvements. 7 –9 However, conventional cognitive stimulation programs place a great deal of emphasis on the domain of language and require participants to discuss and express their opinions verbally. 5 A recently developed conceptual framework advocates that nonpharmacological interventions for PWD should focus on the different mind–body functional domains in order to enhance or maintain general cognition and quality of life in PWD, namely, auditory music and rhythm, visuospatial and fine motor skills, language and verbal skills, executive functions, kinesthetic and gross motor skills, and social functioning. 10 Therefore, we are proposing an adapted intervention—the Cognitive Stimulating Play Intervention (CoS-Play)—that involves all of the abovementioned domains, to address the shortcoming of the heavy reliance on language of conventional cognitive stimulation programs.
Play is being advocated as essential in all stages of life, including for those with dementia. 11 There is some evidence demonstrated that playing games is beneficial to PWD. During the playing of games, an increase in self-confidence and social engagement with other participants has been observed in PWD. 12 A narrative review found that physical games and cognitive games (such as chess, jigsaw puzzles, and Bingo) may be useful in improving cognition and behavioral symptoms, yet the methodological quality of the studies that were included was generally inadequate 13 and not anchored in a conceptual framework. This study addresses these gaps in knowledge by exploring the feasibility of the CoS-Play as a means of cognitive stimulation for people with early to moderate dementia, and examining its preliminary effects on the cognitive functions.
Methods
This is a randomized controlled trial employing both quantitative measures and qualitative interviews with staff members of the 2 community day-care centers that were involved in the study, to evaluate the feasibility and preliminary efficacy of the intervention. This design allows us to reflect on the utility of the intervention in real practice, which is particularly important during the developmental stage of a complex intervention. 14 The project was carried out between August 2016 and April 2017 and was approved by the ethics committee of the corresponding university (HSEARS20160617002). The trial was registered with ClinicalTrial.gov under the identifier of NCT02846415.
Sample
Eligible participants were community dwelling adults aged 60 or above with a medically confirmed diagnosis of any type of dementia (such as Alzheimer disease, vascular dementia, etc). Those who were included as participants were people at the stage of early to moderate dementia (stages 4-6 according to the Global Deterioration Scale 15 ), able to sit independently, and physically stable. Those with acute physical or mental illnesses were excluded. Center staff who had assisted in the CoS-Play were invited to take part in interviews so that their opinions on the implementation of the program could be solicited.
Procedures
Two community day-care centers under the same operating organization were recruited through personal connections to take part in this study. These centers advertised the program and referred potential participants to the research team, after seeking initial consent from the proxies of the potential participants. The research team then verified the eligibility of the potential participants and collected informed written consent from their proxies after explaining the purpose of the program to both the participants and their proxies.
After collecting the baseline data, these 2 centers were randomized into either the treatment group or the social control group by an independent research assistant who had no knowledge of the 2 centers and was not involved in the collecting of data. Participants from the corresponding center fell under the group allocation of that center.
Intervention
The CoS-Play was derived from the Play Intervention for Dementia, which was developed in 2013 by a research team and senior service practitioners led by Prof Ka-tat Tsang of the University of Toronto, Canada. The original Play Intervention was designed based on the Strategies and Skills Learning and Development model and was aimed at enhancing the autonomy and quality of life of PWD through stimulation, activity, mental exercise, and interpersonal interaction. 16 The CoS-Play integrates elements of cognitive stimulation in the 6 mind–body functional domains mentioned above and follows the principles of cognitive stimulation. During the sessions, participants can exercise their creativity in a cheerful and respectful environment, without anyone judging their (dis-)ability or with any preset rules. Nobody will ask them such questions as “Do you remember today’s date?,” which may be extremely frustrating to PWD if they have forgotten. Therefore, the goal of the CoS-Play is to enhance the cognitive functions of the participants based on the principles of cognitive stimulation and on stimulating the 6 mind–body functional domains. Please see Table A1 for an example of a CoS-Play session.
Dosage of the intervention
Eight weekly group-based sessions of the CoS-Play, each 45 to 60 minutes in length.
Content of each session
Made up of activities comprising the 6 elements: visuospatial and fine motor activities (eg, making handicrafts), kinesthetic and gross motor activities (eg, batting a balloon), language and verbal activities (eg, telling stories), executive function activities (eg, card games), auditory music and rhythmic activities (eg, playing percussive musical instruments), and social interaction.
Materials
The toys used in the sessions were visually, auditorily, and tactilely stimulating. These activities have been shown to activate multiple neural networks, including the sensory, somatic, and cerebral networks, and to shape the functional capacity of the brain. 17
Tailoring
To tailor the activities to address an individual’s interests (which may affect their motivation) and strengths, the activities within the 6 domains can be different.
Group size
Ten to 16 participants, who were further divided into subgroups of around 4 to 6 participants and seated around an activity table.
Facilitators
One coordinator, 1 to 2 staff members of the center, and 2 to 3 trained assistants. The coordinator was responsible for overseeing the engagement of the participants and for providing training to the center’s staff. The center’s staff and assistants were responsible for setting up the activity room, responding positively to the needs of the participants, actively engaging them in the activities, transferring toys to them, and ensuring their safety.
Control Condition
Led by activity staff, the control group took part in social activities (reading newspapers, watching television) in a similar pattern as with the intervention group. To increase the likelihood of retention in this project, the participants in the control group received the same CoS-Play program after the last round of data collection.
Measures
The demographic data and clinical characteristics of the participants with dementia were collected at baseline before the randomization of the centers. To assess the feasibility of the study, we monitored the recruitment, attendance, and completion rates of the participants in the program; monitored adverse event that occurred; and interviewed the staff members who joined the program. Two staff members were interviewed individually which took place in the center they were working for. The staff were interviewed about their perceptions of: (a) the acceptability of the program, (b) the feasibility of integrating the program to the usual service operations of the center, (c) the practicality of the program, and (d) the effects of the program on participants. A trained research assistant who was blinded to the group allocation assessed the cognitive functions of the participants using the Montreal Cognitive Assessment (MoCA), 18 the Fuld Object Memory Evaluation (FOME), 19 and the Modified Verbal Fluency test (embedded in the FOME), 20 at baseline (T0), and immediately postintervention (T1).
Staff interview
Staff members were invited to participate in an in-depth interview to explore their perceptions about the feasibility of the CoS-Play. The questions that were asked were framed with reference to the guideline on feasibility studies for intervention trials. 14 The guiding questions were as follows: (a) Acceptability: What do you think about the acceptability or satisfaction of the intervention to people with moderate dementia? (b) Integration: What would you think if the intervention were to be integrated into the normal routine of your center? (c) Practicality: What are the practical concerns regarding the CoS-Play? (d) Efficacy: What changes did you observe in the participants after they had participated in the CoS-Play?
Montreal Cognitive Assessment
The global cognitive functions of the participants were measured using the Hong Kong version of the MoCA. 18 This instrument has high internal consistency (Cronbach α = .767), excellent inter-rater reliability (Intra-class Correlation Coefficient [ICC] = 0.987), and good construct validity as compared with the Mini Mental State Examination and Global Deterioration Scale. 18 It consists of 11 items, and lower total scores refer to lower levels of cognitive function.
Fuld Object Memory Evaluation
Memory was evaluated using the FOME. 21 The participants were asked to remember and recall 10 items across 5 recall trials and a delayed recall trial. The instrument has been validated in the Hong Kong Chinese population and found to have better construct validity than the Mini Mental State Examination (r = 0.69-0.74), and to have test–retest reliability (ICC = 0.91-0.96). 19 Three FOME scores, namely total storage (possible range of 0-50), total retrieval (possible range of 0-50), and delayed recall (0-10) were derived. Total storage represents the encoding function, while total retrieval and delayed recall refer to the retrieval function. Higher scores represent better memory.
Modified verbal fluency test
Verbal fluency was assessed using the Modified Fuld Verbal Fluency test, 20 which was modified from the original Fuld Verbal Fluency test embedded in the FOME as a distraction task. Participants were asked to name animals, fruits, and vegetables in 1 minute or 30 seconds. The construct validity was acceptable as compared with the Mini Mental State Examination (r = 0.76), and the test had good test–retest reliability (r = 0.74). 20 Total scores were the sum of the items being recalled, with higher total scores referring to better verbal fluency.
Analysis
SPSS Statistics 23 was used for all analyses. Data collection and entry were conducted by a research assistant who was blinded to the group allocations. The demographic data and the participants’ performance at baseline were compared with Fisher exact test for categorical data, and with the Mann-Whitney U test for continuous data to detect differences between intervention and control groups. Intention-to-treat methods were used for all analyses. Missing values were imputed with the last observation carried forward approach. Analysis of covariance (ANCOVA) was used to examine whether there were significant differences between groups on the outcome measures after 8 weeks of the intervention, using its baseline measures as a covariate. A 2-sided significance test (P < .05) was applied. The magnitude of the effects between the intervention and control groups was displayed as a partial η2 effect size. 22
A deductive content analysis approach was used to analyze the transcribed interview verbatim in relation to the feasibility of the intervention, which is considered suitable for a detailed analysis of the 4 indicators of the feasibility of the intervention—acceptability, integration, practicality, and effects. 23 The first author and a trained research assistant first immersed themselves in the data, decided on the analysis of manifest content together before coding the transcripts individually. After that, both of them discussed discrepancies in the coding and reached a consensus on the categories that were generated.
Results
Participant Characteristics
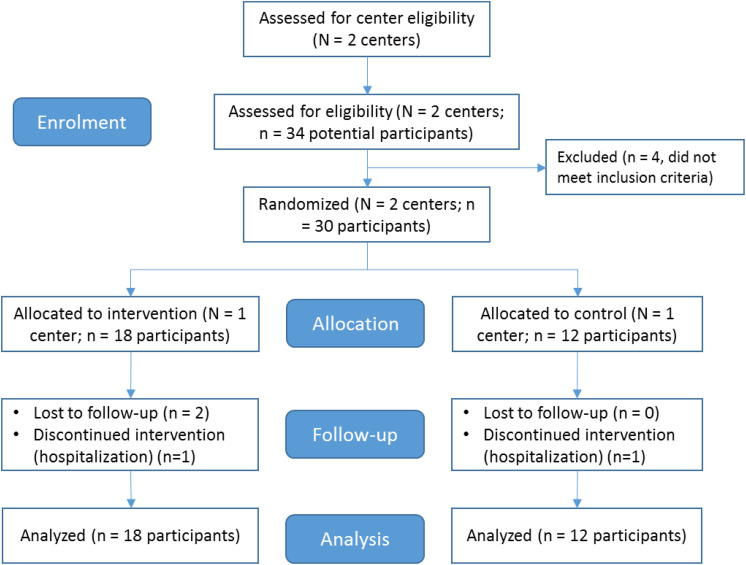
A total of 30 participants were recruited from 2 centers (CoS-Play group: n = 18; control group n = 12) (Please see Figure 1 for the COSORT flowchart), and 2 staff members working in the intervention site were recruited for interviews, who were the female frontline activity assistants worked in the same unit for 1 to 3 years. The mean age of the participants was 83.2 (standard deviation = 7.18), and the majority of them (73.3%) were female. Twelve (40.0%) were married, and most had received either a primary education or no education (73.3%). The participants’ characteristics are presented in Table 1. There were no statistical differences between the CoS-Play group and the control group in terms of demographic and clinical characteristics, except in their total MoCA score.
Figure 1.
Participant flow diagram.
Table 1.
Characteristics of the Participants at Baseline.
| Characteristics | Overall | CoS-Play | Control | P |
|---|---|---|---|---|
| N = 30 | n = 18 | n = 12 | ||
| n (%) | n (%) | n (%) | ||
| Age, mean (SD) | 83.2 (7.18) | 81.8 (7.41) | 85.3 (6.56) | .415a |
| Gender | ||||
| Male | 8 (26.7) | 5 (27.8) | 3 (25.0) | 1.000b |
| Female | 22 (73.3) | 13 (72.2) | 9 (75.0) | |
| Marital status | ||||
| Married | 12 (40.0) | 7 (38.9) | 5 (41.7) | 1.000b |
| Single/divorced/widowed | 18 (60.0) | 11 (61.1) | 7 (58.3) | |
| Education level | ||||
| No schooling/primary | 22 (73.3) | 12 (33.3) | 10 (83.3) | .419b |
| Secondary/Tertiary | 8 (26.7) | 6 (11.1) | 2 (10.7) | |
| Clinical characteristics | ||||
| Montreal Cognitive Assessment | 7.90 (4.4) | 9.2 (3.9) | 5.9 (4.5) | .028a,c |
| FOME—Total storage | 14.9 (11.7) | 13.3 (10.7) | 17.3 (13.3) | .369a |
| FOME—Total retrieval | 9.1 (8.1) | 7.5 (6.7) | 11.6 (1.6) | .182a |
| FOME—Delayed recall | 1.8 (1.7) | 1.6 (1.6) | 2.3 (1.7) | .270a |
| Modified Verbal Fluency Test | 11.8 (5.7) | 13.0 (4.9) | 9.9 (6.6) | .150a |
Abbreviations: CoS-Play, Cognitive Stimulating Play Intervention; FOME, Fuld Object Memory Evaluation; SD, standard deviation.
a Mann-Whitney U test.
b Fisher exact test.
c p < .005.
Recruitment, attendance, and completion rates
Thirty-four people were screened and 88.2% (n = 30) were found to be eligible. The average attendance rate of the CoS-Play group was 89.6% (ranging from 50% to 100%) and that of the control group was 75% (ranging from 25% to 100%). The χ2 test showed that the difference in attendance between 2 groups was insignificant (P = .238). Three participants dropped out from the CoS-Play group (16.7%) and 1 from the control group (8.3%), for an overall dropout rate of 13.3%. The reason for the dropping out of all 4 of these participants was sickness or hospitalization.
Adverse event
Although there was intensive manpower in delivering the intervention and to ensure the safety of the participants, a fall accident occurred during the fifth session, when a male participant stood up and played with a shuttlecock. The shuttlecock is a traditional Chinese toy that a person bats with different parts of the body. He ended up with a minor fracture in one of his wrists, but he resumed the remaining 2 sessions after treatment.
Staff Interview (Pseudonyms were used to protect the participants’ identities)
The interview lasted for 45 minutes to 1 hour, and the findings were as follow:
-
1. Acceptability:
The staff informed us that all of the participants appeared to accept the CoS-Play well.Some participants with wandering or agitated behaviors could participate in the whole 45-minute session without asking to leave. Terry and Iris used to ask to go to the washroom, walk away, or lose their temper when they participated in other activities.Iris even showed regret to staff that the program had come to an end.Some participants expressed thanks to the team for bringing them joy and happiness. -
2. Integration:
The staff said that the design of the program including the length of each session and the whole program, and the frequency and level of difficulty of the activities to participants with cognitive impairment, fitted in with their services, and commented that the CoS-Play could be integrated into their routine activities.
As the staff had come equipped with some toys prior to the CoS-Play program, they commented that they were willing to continue with the program. The other toys introduced by the project team were also easy to purchase.It is easy for us to continue the CoS-Play because its structure is similar to that of our existing programs.The toys being used [in the CoS-Play] are common and easy to buy. -
3. Practicality:
It was suggested that in the CoS-Play, 6 trained staff/intervention assistants be present for 18 participants (divided into 3 subgroups), in addition to an interventionist to oversee the implementation of the program. The staff commented that the implementation of the CoS-Play involved a considerable amount of manpower.
The staff reflected that they had other job commitments and were required to leave the participants during the sessions. In addition, throughout the program the trained assistants were required to work with different subgroups of older participants with cognitive impairment. They suggested that stable manpower be assigned so that the staff and assistants would gain better knowledge about the participants’ preferences in terms of activities and about their abilities, so as to be able to respond appropriately.We are delighted to see the positive changes in the participants after the CoS-Play; however, it requires much manpower.We came in and out the sessions sometimes and could not participate the whole session, which may have affected the effects. -
4. Effects on the participants
The staff reported their observations of the effects of the CoS-Play on the participants in 2 aspects: (a) experiences during the intervention, and (b) changes after the intervention.- Experiences during the intervention:
- Cheerful and happyDuring the intervention, Mary began to laugh more frequently and criticize others less.Most of the participants smiled or laughed while playing.Some participants expressed their thanks to the team for bringing them joy and happiness.John felt quite happy and proud when he led the whole group in singing his favorite song.
- EngagedSome participants were relatively passive at the beginning and required active encouragement. But after a few sessions, they joined in right after the start of the activities.Some participants could stay in the 45-minute activities without leaving the activity room, which was surprising.
- Complexity in responses“Tom drew a boat in a session. When we asked him to tell us why he had drawn a boat, he explained that his name carried the meaning of boat and he named the boat in his drawing “Tom’s boat.” We were astonished that he associated his drawing with his name and was able to explain this to us verbally.”
- Creativity“When they were asked to introduce their zodiacs, a participant used ancient Chinese idioms that included zodiacs to comment on others’ answers.”
- After the sessions
- More motivation and increased confidenceKaty told me that she felt much smarter after joining our [play] group.Although she couldn’t distinguish the cards, she was still willing to try.The participant was more willing to respond to questions instead of answering “I don’t know” right away.
- Increased complexity in vocabulary and semanticsAlex gradually began to express himself in full and longer sentences.Sam needs much less time to respond to the intervention assistants.
- Improved behavioral symptomsTerry has stopped harassing his teammates and has even befriended them.
Effects on cognitive functions
Group comparisons of outcome measures were conducted at baseline. The results showed a significant difference between groups on the MoCA score (CoS-Play = 9.2; control = 5.9; z = 2.19; P = .028). For the other outcome measures, including the 3 FOME scores (total storage, total retrieval, and delayed recall) and the Modified Verbal Fluency Test (MVFT) total score, there were no significant differences between groups at baseline as shown in Table 1. Table 2 summarized the ANCOVA results of the group comparison on the adjusted means of cognitive outcomes by controlling their baseline, after the 8-week intervention (ie, T1).
-
(1) Montreal Cognitive Assessment
There was no significant difference between groups for the adjusted MoCA scores at T1.
-
(2) Fuld Object Memory Evaluation
There was a significant difference between groups for the adjusted FOME-total storage and total retrieval scores, with the CoS-Play group having a mean score of 5.92 (95% confidence interval [CI]: 1.83-9.91; P = .006) and 4.12 (95% CI: 0.75-7.50; P = .018) points, respectively, higher than the control group at postintervention. The effect sizes for both the FOME-total storage and total retrieval scores were large (partial η2 = 0.248 and 0.189, respectively).
There was no significant difference between groups for the postintervention adjusted FOME-delay recall score.
(3) Modified Verbal Fluency Test
Table 2.
ANCOVA Results.
| Outcomes | Raw (Post-test) Mean | Adjusted (Post-test) Mean | Comparison Between Groups | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CoS-Play (n = 18) | Control (n = 12) | CoS-Play (n = 18) | Control (n = 12) | F | P | Partial η2 | |||
| Mean | 95% CI | Mean | 95% CI | ||||||
| MoCA | 10.06 | 5.6 | 8.84 | 7.51-10.17 | 7.40 | 5.75-9.06 | 1.801 | .191 | 0.063 |
| FOME-Total storagea | 17.50 | 15.2 | 18.92 | 16.38-21.45 | 13.00 | 9.93-16.16 | 8.885 | .006 | 0.248 |
| FOME-Total retrievalb | 11.06 | 10.5 | 12.48 | 10.39-14.58 | 8.36 | 5.78-10.94 | 6.285 | .018 | 0.189 |
| FOME-Delayed recall | 1.94 | 2.3 | 2.20 | 1.61-2.79 | 1.87 | 1.14-2.60 | 0.500 | .486 | 0.018 |
| Modified Verbal Fluency | 15.50 | 11.4 | 14.34 | 12.54-16.13 | 13.16 | 10.95-15.38 | 0.689 | .414 | 0.025 |
Abbreviations: ANCOVA, analysis of covariance; CI, confidence interval; CoS-Play, Cognitive Stimulating Play Intervention; FOME, Fuld’s Object Memory Evaluation; MoCA, Montreal Cognitive Assessment.
a P < .01.
b P < .05.
There was no significant difference between groups for the adjusted MVFT scores at T1.
Discussion
This is the first study aimed at determining the feasibility of using the CoS-Play as a medium of cognitive stimulation to promote the cognitive functions of people with moderate dementia. The findings from this study showed that although there were several practical issues that might affect its implementation, the CoS-Play can feasibly be implemented, and with positive effects on the participants.
Judging from the high attendance rate (90%) and low attrition rate (16.7%) of the CoS-Play, in addition to the positive feedback from the staff, the intervention was acceptable to both the PWD and the staff working in the community centers. The dropout rate of people with early to moderate dementia in cognitive interventions reported in previous studies ranged from 0% to 36.7%. 9 The attendance rate and attrition rate in this study were found similar to that of a local study using conventional cognitive stimulation therapy for early dementia, in which the attendance rate was 92% and the attrition rate was 13%. 24 In addition, the staff believed that the CoS-Play intervention could be incorporated into their routine. Taking into consideration, the attention span of older adults with moderate dementia, the length of each session of the CoS-Play was around 60 to 75 minutes, and most of the social activities delivered in the day-care service centers are of almost the same length. The cost of purchasing-related materials for this study was only around US$80 to US$100. The staff also mentioned that the center already had some of the recommended toys before taking part in the program, or that the toys were very easy to purchase.
We implemented the CoS-Play in an open area of a large center. The staff who participated in this intervention were required to sometimes walk away from the venue to assist with the operations of the center. Even if they were gone for only a short time, this might still have affected the implementation and distracted the participants. In addition, bystanders, who also had dementia, were attracted to the intervention when they saw the participants laugh or make noises when playing. Other staff members were required to lead these bystanders away, which definitely led to disappointment on the part of the bystanders. Therefore, it would be better to conduct the intervention in a closed, soundproof environment.
The staff commented that the implementation of the CoS-Play involved a considerable amount of manpower. However, conventional cognitive stimulation activities for a small group of 5 to 7 older adults with dementia usually require 2 staff members, 4,8 which is comparable to the manpower requirements of the CoS-Play. In the CoS-Play, it is suggested that 6 trained staff/intervention assistants be provided for 18 participants (divided into 3 subgroups), in addition to an interventionist, who would oversee the implementation of the program to ensure the safety of the participants and provide adequate attention to foster engagement. Although the staff to participant ratio of the CoS-Play is comparable to that of conventional cognitive interventions for people with dementia, we suggest reviewing it in later studies when the intervention is delivered to groups of participants who are less cognitively impaired or less physically frail, who might require less attention.
Although the trained staff and intervention assistants paid full attention to the participants, some physically healthy participants may want to engage in more vigorous movements, which may pose a risk of injury. We suggest that an attempt be made to achieve a balance between respecting the participants’ wish to determine their own abilities and protecting them from injury.
The CoS-Play adopted the principles of cognitive stimulation as well as the body-mind functional domains. The findings showed that the CoS-Play yielded moderate to large effects on memory. Although it is thought that conventional cognitive stimulation therapy can have general cognitive benefits for PWD, no significant changes in memory were identified. 25 In the CoS-Play, participants were encouraged to decide how to play with the toys and even lead the other group participants in playing if they were willing to. The staff members also noted the increased motivation and confidence of participants after the intervention sessions. Based on the Bandura’s Self-Efficacy Theory, people who had lower self-efficacy tend to had less interest in the assigned tasks and expend less effort and commitment that led to suboptimal performance. 26 A meta-analysis even showed that the self-efficacy was significantly related to episodic memory performance. 27 We suggested the features of CoS-Play that enhanced participants’ self-efficacy may lead to the improvement in episodic memory but yet to be confirmed with a larger scale study with the measurement of self-efficacy and motivation. The research assistant also reported that some of the participants were more willing to recall the objects during the FOME (ie, the test for measuring the episodic memory) instead of immediately claiming that they had forgotten. However, the research assistant was unable to identify whether these participants were in the intervention or control group as s/he was blinded to group allocation.
The positive experience of being in a group, as well as the effects, are similar to those of conventional cognitive stimulation therapy, such as becoming more positive, relaxed, confident, and experiencing improved verbal skills, 28 although the CoS-Play is relatively less reliant on verbal communication within the group. In contrast, there was no significant change in global cognition in this study. An explanation for this result is that the MoCA that was used in this study is less sensitive than the Mini Mental State Examination for this population. 29 Based on the interview, participants were described as having improved mood, motivation, and confidence through participation in the intervention. In previous studies, these factors have been shown to be associated with cognitive functions. 30,31 In future research on this CoS-Play intervention, we suggest adopting a validated tool such as the Nurse Observation Scale of Cognitive Assessment 32 to quantify the participants’ cognitive functions in daily activities, in order to measure the transferrable effects of the intervention. Other than cognitive functions, the staff reported that there were other positive changes in the participants, such as improvements in behavioral symptoms and mood. We suggest that the other possible effects be measured with validated instruments and that the effects be confirmed with a larger scale RCT.
This study is not without limitations. Although the findings are positive and certainly interesting, the effects of the intervention on cognitive functions are yet to be confirmed because of the small size of our sample as well as the absence of a follow-up study to evaluate the lasting effects. Conventional cognitive stimulation therapy usually consists of 14 sessions held twice weekly. 4 We do not yet know whether additional sessions or more frequently held sessions of the CoS-Play would lead to greater efficacy.
Conclusion
This is the first study to examine a cognitively stimulating intervention using play as a medium on people with dementia. We conclude that it is feasible to implement the CoS-Play, and the preliminary findings suggest that it has promising and positive effects on cognitive functions. The number of people who live with dementia is growing; therefore, effective interventions such as the CoS-Play, which can alleviate the negative impact of dementia on a person, are highly sought after. We suggest that a larger scale RCT be conducted to confirm the results.
Acknowledgments
The authors thank the organization and the people who participated in this study.
Appendix A
Table A1.
An Example of a CoS-Play Session.
| Game/Activity | Mind–Body Functional Domains | Duration (Minutes) |
|---|---|---|
| Opening ritual: singing and playing percussive instrument | Auditory music and rhythm Social functioning |
8 |
| Passing the rings | Kinesthetic and gross motor skills Social functioning |
8 |
| Passing big yoga ball | Kinesthetic and gross motor skills Social functioning |
8 |
| Moving back to sit around the table | 2 | |
| Tossing ball and naming fruits | Kinesthetic and gross motor skills Language and verbal skills Social functioning |
8 |
| Bean bags (pass, pick, and sort) | Visuospatial and fine motor skills Executive functioning |
9 |
| Bean bags (throw and target) | Visuospatial and fine motor skills Kinesthetic and gross motor skills |
8 |
| Matching card game | Executive functioning | 8 |
| Exit ritual: singing and playing percussive instrument |
Auditory music and rhythm Social functioning |
5 |
| Total: | 64 | |
Abbreviation: CoS-Play, Cognitive Stimulating Play.
Modified from: Tsang AKT. 16
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Internal research fund, School of Nursing, The Hong Kong Polytechnic University.
ORCID iD: Daphne Sze Ki Cheung  http://orcid.org/0000-0001-5651-9352
http://orcid.org/0000-0001-5651-9352
Angela Yee Man Leung  http://orcid.org/0000-0002-9836-1925
http://orcid.org/0000-0002-9836-1925
References
- 1. Prince M, Comas-Herrera A, Knapp M, Guerchet M, Karagiannidou M. World Alzheimer Report 2016: Improving Healthcare for People Living with Dementia: Coverage, Quality and Costs now and in the Future. London, England: Alzheimer Disease International; 2016. [Google Scholar]
- 2. Clare L, Woods RT. Cognitive training and cognitive rehabilitation for people with early-stage Alzheimers disease: a review. Neuropsychol Rehabil. 2004;14(4):385–401. doi:10.1080/09602010443000074. [Google Scholar]
- 3. National Institute for Health and Care Excellence. Dementia: Supporting People with Dementia and their Carers in Health and Social Care (CG42). United Kingdom: National Institute for Health and Care Excellence; 2006. Updated 2016. [Google Scholar]
- 4. Spector A, Thorgrimen L, Woods B, Orrell M. Making a Difference: an Evidence-Based Group Programme to Offer Cognitive Stimulation Therapy (CST) to People with Dementia. London, England: Hawker; 2006. [Google Scholar]
- 5. Hall L, Orrell M, Stott J, Spector A. Cognitive Stimulation Therapy (CST): neuropsychological mechanisms of change. Int Psychogeriatr. 2013;25(03):479–489. doi:10.1017/s1041610212001822. [DOI] [PubMed] [Google Scholar]
- 6. Cheung DSK, Chien WT, Lai CKY. Conceptual framework for cognitive function enhancement in people with dementia. J Clin Nurs. 2011;20(11-12):1533–1541. doi:10.1111/j.1365-2702.2010.03584.x. [DOI] [PubMed] [Google Scholar]
- 7. Huntley JD, Gould RL, Liu K, Smith M, Howard RJ. Do cognitive interventions improve general cognition in dementia? A meta-analysis and meta-regression. BMJ Open. 2015;5:e005247. doi:10.1136/bmjopen-2014-005247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Woods B, Spector AE, Prendergast L, Orrell M. Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database Syst Rev. 2012;(2):CD005562. doi:10.1002/14651858.cd005562. [DOI] [PubMed] [Google Scholar]
- 9. Aguirre E, Woods RT, Spector A, Orrell M. Cognitive stimulation for dementia: a systematic review of the evidence of effectiveness from randomised controlled trials. Ageing Res Rev. 2013;12(1):253–262. doi:10.1016/j.arr.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 10. Wong GHY, Ng CKM, Lai CKY, et al. Development of six arts, a culturally appropriate multimodal nonpharmacological intervention in Dementia. Gerontologist. 2014;55(5):865–874. doi:10.1093/geront/gnu102. [DOI] [PubMed] [Google Scholar]
- 11. Killick J. Playfulness and Dementia: A Practice Guide. London, England: Jessica Kingsley; 2013. [Google Scholar]
- 12. Miltiades HB, Thatcher WG. Social engagement during game play in persons with Alzheimer’s ‘innovative practice’. Dementia. 2017. doi:10.1177/1471301216687920. [DOI] [PubMed] [Google Scholar]
- 13. Zheng J, Chen X, Yu P. Game-based interventions and their impact on dementia: a narrative review. Australas Psychiatry. 2017;25(6):562–565. doi:10.1177/1039856217726686. [DOI] [PubMed] [Google Scholar]
- 14. O’Cathain A, Hoddinott P, Lewin S, et al. Maximising the impact of qualitative research in feasibility studies for randomised controlled trials: guidance for researchers. Pilot Feasibility Stud. 2015;1(32). doi:10.1186/s40814-015-0026-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reisberg B, Ferris SH, de Leon MJ, Crook T. The global deterioration scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136–1139. doi:10.1176/ajp.139.9.1136. [DOI] [PubMed] [Google Scholar]
- 16. Tsang AKT. Play intervention for Dementia. Toronto, Ontario, Canada: Centre for Learning and Change; 2017. [Google Scholar]
- 17. Perry B. The neuroarcheology of childhood maltreatment. In: Franey K, Feffner R, Falconer R, ed. The Cost of Child Maltreatment: Who Pays. San Diego, CA: Family Violence and Sexual Assault Institute; 2000:21–43. [Google Scholar]
- 18. Yeung PY, Wong LL, Chan CC, Leung JLM, Yung CY. A validation study of the Hong Kong version of Montreal Cognitive Assessment (HK-MoCA) in Chinese older adults in Hong Kong. Hong Kong Med J. 2014;20(6):504–510. doi:10.12809/hkmj144219. [DOI] [PubMed] [Google Scholar]
- 19. Chung JCC. Clinical validity of Fuld Object Memory Evaluation to screen for dementia in a Chinese society. Int J Geriatr Psychiatry. 2009;24(2):156–162. doi:10.1002/gps.2085. [DOI] [PubMed] [Google Scholar]
- 20. Chiu HFK, Chan CKY, Lam LCW, et al. The modified Fuld Verbal Fluency Test: a validation study in Hong Kong. J Gerontol B Psychol Sci Soc Sci. 1997;52B(5):P247–P250. doi:10.1093/geronb/52b.5.p247. [DOI] [PubMed] [Google Scholar]
- 21. Fuld PA. Fuld Object-Memory Evaluation: Instruction Manual. New York, NY: Stoelting; 1977. [Google Scholar]
- 22. Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof Psychol Res Pract. 2009;40(5):532–538. doi:10.1037/14805-020. [Google Scholar]
- 23. Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405. doi:10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- 24. Wong GHY, Yek OPL, Zhang AY, Lum TYS, Spector A. Cultural adaptation of cognitive stimulation therapy (CST) for Chinese people with dementia: multicentre pilot study. Int J Geriatr Psychiatry. 2017;33(6):841–848. doi:10.1002/gps.4663. [DOI] [PubMed] [Google Scholar]
- 25. Spector A, Orrell M, Woods B. Cognitive Stimulation Therapy (CST): effects on different areas of cognitive function for people with dementia. Int J Geriatr Psychiatry. 2010;25(12):1253–1258. doi:10.1002/gps.2464. [DOI] [PubMed] [Google Scholar]
- 26. Bandura A. Regulation of cognitive processes through perceived self-efficacy. Dev Psychol. 1989;25(5):729–735. [Google Scholar]
- 27. Beaudoin M, Desrichard O. Are memory self-efficacy and memory performance related? A meta-analysis. Psychol Bull. 2011;137(2):211–241. [DOI] [PubMed] [Google Scholar]
- 28. Toh HM, Ghazali SE, Subramaniam P. The acceptability and usefulness of cognitive stimulation therapy for older adults with Dementia: a narrative review. Int J Alzheimers Dis. 2016;2016:1–11. doi:10.1155/2016/5131570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Manning CA, Ducharme JK. Dementia syndromes in the older adult. In: Lichtenberg P, ed. Handbook of Assessment in Clinical Gerontology. New York, NY: Elsevier Academic Press; 2010:155–178. [Google Scholar]
- 30. Haslam C, Haslam SA, Knight C, Gleibs I, Ysseldyk R, Mccloskey LG. We can work it out: group decision-making builds social identity and enhances the cognitive performance of care residents. Br J Psychol. 2014;105(1):17–34. doi:10.1111/bjop.12012. [DOI] [PubMed] [Google Scholar]
- 31. Logan S, Medford E, Hughes N. The importance of intrinsic motivation for high and low ability readers reading comprehension performance. Learn Individ Differ. 2011;21(1):124–128. doi:10.1016/j.lindif.2010.09.011. [Google Scholar]
- 32. Persoon A, Schoonhoven L, Melis RJ, Achterberg TV, Kessels RP, Rikkert MGO. Validation of the NOSCA - nurses’ observation scale of cognitive abilities. J Clin Nurs. 2012;21(21-22):3025–3036. doi:10.1111/j.1365-2702.2012.04129.x. [DOI] [PubMed] [Google Scholar]