Abstract
This study examined the determinants of physical activity (PA) for older adults with Alzheimer’s disease (AD) to learn more about how to promote PA in this population. Caregivers of older adults with AD (N = 99) provided information related to care recipient’s PA, as well as addressed sociodemographics and perceptions about their care recipient’s PA. Gender of care recipient was a significant predictor of PA (β = .80, P < .05); men with AD participated in more PA than women with AD. Also, caregiver's outcome expectation for care recipient's PA also predicted more PA (β = .82, P < .05). Caregiver’s perceived benefits of PA (outcome expectation) for their care recipient partially mediated the relationship between self-efficacy for care recipient’s PA and the reported levels of PA for the care recipient. This study demonstrated the importance of caregiver perceptions about care recipient’s PA.
Keywords: Alzheimer’s disease, caregivers, physical activity, outcome expectation, self-efficacy, well-being, intervention
Introduction
Alzheimer’s disease (AD) is a major public health concern. Approximately 5.2 million adults aged 65 and older are diagnosed with AD in the United States alone, and this number is expected to continue to rise. 1 Unfortunately, there is no cure for AD, and currently available medications, including cholinesterase inhibitors and memantine, temporarily delay or slow deterioration in cognitive symptoms of AD. 1 These medications also have nonnegligible side effects, and the effectiveness of the medications varies by individuals and AD stages. 1 Accordingly, given no current cure for dementia, more studies on nonpharmacological interventions like physical activity are needed to promote well-being and meet the needs of those with AD. Also, individuals with AD require high levels of assistance, making it a difficult disease for family caregivers to manage. Furthermore, managing AD is financially burdensome as well as physically and emotionally demanding. 1 –3 Therefore, attention to beneficial and cost-effective programs that promote well-being of those with AD and reduce stress on caregivers is much needed.
Researchers have demonstrated the feasibility and effectiveness of physical activity for older adults with AD and other dementias. 4 –13 According to Perez and Carral, 6 physical exercise plays a positive role in the health of older adults with AD. For example, there are metabolic and neuropathological effects of physical activity in those with AD 6,12 that positively affect cerebral structure and function. 12 In addition, physical activity increases physical fitness such as muscle strength and promotes better physical functioning abilities and mobility such as walking speed, stride length, and double-limb support. 7,9,13,14 Moreover, some intervention studies demonstrated cognitive improvement from physical activity. 5,7,15 Improved global cognition, test of attentional matrix, verbal span test, and supraverbal span test among participants demonstrated positive impacts of exercise on cognitive function. 5,7,15 With regard to effects on independence, physical activity helps individuals with AD to maintain levels of basic activities of daily living 7 and reduces days of restricted activities. 9 Furthermore, physical activity contributes to improvement in psychological and behavioral symptoms, for example, better mood, positive affect, fewer depressive symptoms, and reduction in unwanted behaviors such as wandering and aggressive behaviors. 7,9,16 Finally, physical activity contributes to improvements in communication and social participation for older adults with AD. 6
It is apparent that physical activity interventions for those with AD and other dementias have supported positive impacts on their physical, cognitive, and emotional conditions. In spite of the advantages of physical activity for those with AD, the majority of older adults with AD and other dementias live a sedentary lifestyle and few are engaged in regular physical activity due to physical fragility, cognitive vulnerability, and lack of information and programs available. 17 Therefore, to promote physical activity participation and develop physical activity programs and interventions for those with AD, it is important to identify factors that determine participation in physical activity for older adults with AD and other dementias.
There is limited information about determinants of physical activity specifically for older adults with AD. Studies on determinants of physical activity among a general population of older adults aged 65 and older found that major predictors of increased physical activity were sociodemographic factors such as being younger, male, white, married, and higher socioeconomic status (SES). 18 –21 Additionally, physical and mental health status, past experience with physical activity, and positive feelings and thoughts about physical activity, such as strong self-efficacy and outcome expectation for physical activity, predicted levels of physical activity for older adults. 19 –21 Finally, perceived social influence factors such as advice from health professionals have also influenced physical activity participation among older adults. 19 –21
Undoubtedly, caregivers play a critical role in the life of older adults with AD. Generally, caregivers undertake direct care provision, emotional support, care coordination, financial management, and decision-making. 2,3 Therefore, caregivers are an integral component in their care recipients’ physical activity participation because they may make decisions about program participation, transportation, treatment, and interventions; provide task assistance; or encourage engagement. However, little is known about caregiver attitudes and beliefs about physical activity for their care recipients with AD, which likely impacts initiation and maintenance of physical activity for their care recipients.
Bandura’s social cognitive theory 22 is a useful framework to better understand physical activity behavior. Self-efficacy and outcome expectations have a significant impact on “behavior, motivational level, thought patterns, and emotional reactions in response to any situation.” 23 Perceived self-efficacy, or people’s beliefs about their ability to control behaviors to complete tasks, is a relevant construct in which to examine physical activity for older adults. Researchers have found that the more confident that older adults feel doing physical activity, the more they initiate and maintain physical activity. 21,23 –25 Outcome expectation, defined as the perceived benefits of participating in physical activity, also has an important influence on older adults’ physical activity behaviors. 23,26,27 Individuals with a high level of outcome expectation may be more motivated to pursue and maintain physical activity.
In addition, caregiver's self-efficacy for managing dementia has been suggested as an important contributor to the well-being of care recipients with AD. 28 –30 A caregiver with strong self-efficacy for managing dementia is associated with positive feelings about caregiving, reduction in depressive symptoms and burnout, effective coping strategies, provision of high-quality care, and the use of innovative care strategies, all of which can contribute to well-being of those with AD. 28 –30 Correspondingly, caregiver's self-efficacy and outcome expectations for care recipient's physical activity as well as caregiver's self-efficacy for managing dementia should be examined in the context of physical activity among individuals with AD.
Research Questions
To date, it is unclear which factors contribute to physical activity participation among older adults with AD. Therefore, we explored both caregiver and care recipient factors theorized to be associated with physical activity among individuals with AD and addressed 4 hypotheses. First, we hypothesized that older adults with AD would have similar individual-level determinants of physical activity as community-dwelling older adults (eg, age, gender, education level, health condition, prior exercise experience, and advice from a health professional). Second, because caregivers are critical to the well-being and activities of their care recipients with AD, we also examined the role of caregivers in determining the physical activity level of their care recipients. More specifically, we expected that caregiver attitudinal and psychosocial variables regarding physical activity and well-being of care recipients would also be linked to care recipient's physical activity. Third, we also hypothesized that caregiver sociodemographic factors (ie, age, gender, race, education attainment, marital status), health condition, level of physical activity, prior physical activity experiences, mood, and aging perceptions were related to care recipient's physical activity participation. Finally, we expected that caregiver psychological factors (eg, willingness to introduce innovative interventions, attitudes concerning physical activity, caregiver's outcome expectation, and self-efficacy) would also be associated with care recipient's physical activity participation. In line with this and social cognitive theory, we also explored how caregiver's outcome expectation potentially mediated the relationship between caregiver's self-efficacy for providing physical activity and reported levels of physical activity among care recipients.
Method
Design and Sample
The eligibility for inclusion in this study was broad and included any persons currently caring for or with experience in caring for an older adult with AD or other dementias. The recruitment process of this study consisted of 2 parts: online and in person. First, participants were recruited from both online dementia caregiver support websites and social network services (Facebook and Google+). We recruited participants from the most frequently mentioned helpful websites for dementia caregiving as recommended by experts in the field (eg, dementia caregiver bloggers, staff from the State Department of Social and Health Services, county community service administrators). Second, in-person recruitment occurred in various family caregiver support programs facilitated by state and community aging service agencies in Washington State. Eligible participants were asked to complete an online or paper survey that consisted of 117 questions. Most participants completed online surveys, but 2 participants completed paper-based surveys. Participants were recruited from late May to late June in 2014, and the total number of participants was 127. We deleted 28 cases who responded to only the first few questions but did not answer most of the survey questions. This resulted in 99 cases utilized in the data analysis (N = 99: women = 80, men = 6). See Table 1 for a list of participant characteristics. The institutional review board ofWashington State University reviewed the study procedures and assigned this study to “exempt” status.
Table 1.
Characteristics of Caregivers and Their Care Recipients.a
| Category | n (%) | |
|---|---|---|
| Caregivers | ||
| Gender | Men | 6 (7) |
| Women | 80 (93) | |
| Race | White | 83 (97.6) |
| Asian | 2 (2.4) | |
| Education | Grade school | 1 (1.1) |
| High school | 16 (18.4) | |
| 2-year college | 31 (35.6) | |
| 4-year college | 20 (23) | |
| Postgraduate | 19 (21.8) | |
| Marital status | Married | 68 (78.2) |
| Single | 8 (9.2) | |
| Separated/divorced | 9 (10.3) | |
| Widowed | 2 (2.3) | |
| Health | Very good | 25 (30.1) |
| Good | 40 (48.2) | |
| Poor | 5 (6) | |
| Relation to CR | Spouse | 22 (25.6) |
| Adult child | 50 (58.1) | |
| Spouse of adult child | 3 (3.5) | |
| Sibling | 3 (3.5) | |
| Other relatives | 2 (2.3) | |
| Employee | 2 (2.3) | |
| Types of caregivers | Primary | 59 (67.8) |
| Secondary | 4 (4.6) | |
| Working | 10 (11.5) | |
| Long distance | 11 (12.6) | |
| Occasional | 3 (3.4) | |
| Care recipients | ||
| Gender | Men | 41 (41.8) |
| Women | 57 (58.2) | |
| Race | White | 96 (97) |
| Asian | 3 (3) | |
| Education | Grade school | 11 (11.5) |
| High school | 57 (59.4) | |
| 2-year college | 8 (8.3) | |
| 4-year College | 11 (11.5) | |
| Postgraduate | 9 (9.4) | |
| Marital status | Married | 43 (43.4) |
| Single | 1 (1) | |
| Separated/divorced | 12 (12.1) | |
| Widowed | 43 (43.4) | |
| Health | Very good | 16 (16.7) |
| Good | 37 (38.5) | |
| Fair | 22 (22.9) | |
| Poor | 21 (21.9) | |
| AD severity | Mild decline | 9 (9.8) |
| Moderate decline | 38 (41.3) | |
| Severe decline | 45 (48.9) | |
Abbreviations: AD, Alzheimer’s disease; CR, care recipient; PA, physical activity.
aN = 99.
Measures
Demographics of caregiver and care recipient
Participants were asked to report their sociodemographic information including age, gender, race/ethnicity, education attainment, and marital status. They were also asked to provide similar sociodemographic information on the person for whom they provided care. For assessing health status, participants were asked to rate their health compared with that of their peers and rate their care recipient’s health compared with that of care recipient’s peers on a 5-point Likert-type scale. In addition, participants were asked to provide their care recipient’s progress of AD (ie, mild, moderate, and severe).
Physical activity of caregiver and care recipient
Care recipient's level of physical activity was measured by the Rapid Assessment of Physical Activity (RAPA). 31 The RAPA has 9 items assessing level and intensity of physical activity, with a specific focus on strength and flexibility. Good reliability and validity have been reported for RAPA. 32 In addition to care recipient's level of physical activity, caregiver level of physical activity was also measured by asking how many days participants engaged in physical activity per week. Additionally, participants were asked about care recipients’ prior experiences with physical activity (ie, type of activity, length of activity) as well as their own prior physical activity experience (ie, type of activity, length of activity). Finally, participants were asked 2 dichotomous (yes/no) questions about whether their health-care providers had discussed the benefits of physical activity or recommended that their care recipient receive more physical activity.
Caregiver variables
A number of attitudinal, psychosocial, and psychological measures were used to measure caregiver influence on level of care recipient's physical activity.
Willingness
Caregiver willingness and openness to introduce their care recipient to innovative interventions (ie, physical activity) was measured with items developed for this study. Three items asked how much they were willing to help their care recipient do physical activity as well as how open they were to innovative interventions for people with AD. A 5-point Likert-type scale ranging from “not at all” (1) to “extremely” (5) was utilized. Internal consistency reliability was acceptable (Cronbach α = .86).
Well-being
Caregiver well-being was measured with Watson, Clark, and Tellegen’s Positive Affect and Negative Affect Scale (PANAS). 33 This scale consisted of 20 words that describe different feelings and emotions. Participants rated if they experienced these feelings on a 5-point Likert-type scale. There is evidence supporting the reliability and validity of the PANAS. 33 Internal consistency reliability was acceptable (Cronbach α = .92).
Perceptions about aging and physical activity
We included a measure regarding perceptions of aging in case negative age stereotypes potentially influence caregiver perceptions regarding physical activity in later life. The Brief Aging Perceptions Questionnaire (B-APQ) measured caregiver views and experiences of getting older to assess caregiver attitudes and feelings about aging. 34 The B-APQ includes 17 items associated with physical, social, and psychological aspects of aging measured on a 5-point Likert-type scale. There is supporting evidence for the reliability and validity of the B-APQ. 34 Internal consistency reliability was acceptable (Cronbach α = .84).
Attitudes about physical activity
Caregiver's attitude about physical activity was assessed with the physical activity attitude items for community-dwelling older adults developed by Benjamin and colleagues. 35 These 13 items measured both direct and indirect caregiver's attitudes on a 5-point Likert-type scale. Higher scores indicate more positive attitudes toward physical activity. Initial evidence of reliability and validity has been documented. 35 Internal consistency reliability was acceptable (Cronbach α = .89).
Outcome expectation and self-efficacy
Caregiver outcome expectation was measured by the Outcome Expectation for Exercise (OEE) scale designed by Resnick and colleagues. 26 The relationship between perceived benefits of exercise and exercise behaviors (especially for older adults) was assessed. Nine items were adapted to reflect the caregiver context. These items were scored on a 5-point Likert-type scale. Resnick and colleagues 26 found support for the internal consistency and validity of the OEE. Internal consistency reliability was acceptable (Cronbach α = .94).
The self-efficacy for physical activity scale 36 was used to assess caregiver confidence regarding care recipient's participation in physical activity. The scale has 9 items measuring caregiver's self-efficacy related to the ability to continue to exercise in the face of perceived barriers. Items were adapted to reflect the caregiver context. A confidence rating was determined on a scale from 0 to 10. There is supporting evidence of construct validity and internal consistency for this scale. 36 The internal consistency reliability of 9 items was acceptable (Cronbach α = .96).
Caregiver's self-efficacy for managing dementia was measured by questions developed by Fortinsky and colleagues. 28 Ten items assessed how certain caregivers could manage dementia symptoms and cope with challenging situations, as well as their ability to find and arrange support services in the community to supplement their own care. Participants were asked to rate themselves on a 10-point scale. Reliability and validity were documented by Fortinsky and colleagues. 28 The internal consistency reliability was acceptable (Cronbach α = .90).
Analytic Strategy
Hierarchical multiple regression (HMR) was used to test study hypotheses. Care recipient demographic variables including age, gender, education attainment, health condition, stage of dementia, past experiences with exercise, and health-care provider’s advice were entered into the first block of HMR as covariates. Next, caregiver demographic characteristics, health status, and prior physical activity experiences were entered into the second block as covariates. Finally, caregiver psychosocial factors (eg, attitudes, perceptions, outcome expectation) theorized to be associated with care recipient's physical activity were entered into the third block to test the main hypothesis of the study. Finally, a parsimonious model was tested that only included significant and marginally significant predictors from the hierarchical regression model in order to increase power and test the strength of those predictors. To analyze the hypothesized mediating relationships, the Baron and Kenny mediation regression analysis approach 37 was used. We used SPSS 22 to analyze the data.
Results
Descriptive Statistics
The data screening process included missing value analysis (Little’s Missing Completely at Random test) and the examination of outliers and normality. The assumptions of normality, linearity, homoscedasticity, multicollinearity, independence of errors, and lack of autocorrelation were all met. The age of care recipients ranged from 50 to 98 years, with the mean age of 77.52 years (standard deviation [SD] = 10.76). The average level of care recipient's physical activity (mean [M] = 3.30, SD = 2.24) was considered underactive/regular–light activities. 31 Approximately 34% of care recipients (n = 30) did not participate in any physical activity at all, while 66% (n = 59) participated in some type of physical activity. The majority (63%) of caregivers responded that a health-care provider told them about the benefits of physical activity for their care recipients, and 54% (n = 47) reported that a health-care provider recommended their care recipients do physical activity. The age of caregivers ranged from 33 to 73 years (M = 55 years, SD = 8.36). The majority were women (93%, n = 80) and white (97.6%, n = 83). See Table 1 for more descriptive information about caregivers and care recipients.
Bivariate Correlations Between Caregiver and Care Recipient Variables
Care recipient's physical activity was negatively correlated with health condition (r = −.25, P < .05) and severity of AD (r = −.38, P < .05). Caregiver's physical activity was positively related to care recipient's level of physical activity (r = .25, P < .05). With the exception of caregiver's attitudes toward physical activity, all caregiver psychosocial factors were correlated with care recipient's level of physical activity. See Table 2 for bivariate correlations among variables.
Table 2.
Bivariate Correlations Among Caregiver and Care Recipient Variables Associated With Care Recipient's Physical Activity.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. CR PA | – | |||||||||||||
| 2. CR age | −.01 | – | ||||||||||||
| 3. CR health | −.25a | −.15 | – | |||||||||||
| 4. CR AD severity | −.38a | .27a | .12 | – | ||||||||||
| 5. CG age | .07 | .03 | −.21 | .05 | – | |||||||||
| 6. Length of caregiving | −.03 | .01 | .14 | .26a | .22a | – | ||||||||
| 7. CG health | −.07 | −.08 | .20 | .01 | −.19 | .11 | – | |||||||
| 8. CG affect | −.01 | .02 | −.14 | −.13 | .24 | .03 | .23a | – | ||||||
| 9. CG aging perception | −.06 | .12 | -.07 | .09 | .32a | .09 | .30a | .54a | – | |||||
| 10. CG PA | .25a | −.01 | −.23a | −.10 | .14 | .02 | .23a | .22a | .19 | – | ||||
| 11. CG willingness | .35a | −.10 | −.11 | −.27a | −.04 | −.05 | .25 | .10 | −.22 | .21 | – | |||
| 12. CG PA attitude | .09 | −.05 | -.05 | .04 | .14 | .10 | .36a | .10 | .29a | .28a | .29a | – | ||
| 13. CG outcome expectation | .52a | −.07 | −.28a | −.41a | −.19 | −.18 | .25a | .10 | .09 | .28a | .48a | .28a | – | |
| 14. CG self-efficacy | .51a | −.03 | −.27a | −.33a | −.03 | .06 | .14 | .15 | .06 | .17 | .42a | .10 | .52a | – |
| 15. CG dementia self-efficacy | .26a | −.01 | −.06 | −.09 | .26 | .12 | .17 | .42a | .29a | .07 | .22a | .01 | .11 | .36a |
Abbreviations: AD, Alzheimer’s disease; CG, caregiver; CR, care recipient; PA, physical activity.
a P < .05.
Hierarchical Regression Modeling of Physical Activity
In the initial 3-stage hierarchical regression model, the majority of care recipient factors and caregiver sociodemographic factors were not statistically significant (P > .05). A parsimonious model was needed to capture greater variance with fewer variables. To derive the most parsimonious model, only variables associated with care recipient's physical activity at a conservatively significant level (P < .10) were retained in the simplified model. This included care recipient gender, the clinical stage of AD, caregiver perceptions toward aging, and caregiver psychosocial factors.
In the first step, care recipient gender and the severity of AD were entered. The model was significant (F 2, 63 = 7.49, P < .01) with 19.2% of variance in levels of care recipient's physical activity explained by these 2 factors. The severity of AD was a significant negative predictor (β = −1.36, P < .05), but gender was not associated with level of care recipient's physical activity (β = .64, P > .05).
When caregiver perceptions toward aging was added to the second step, the model remained significant (F 3, 62 = 4.91, P < .05), but the addition of caregiver perception toward aging did not contribute to additional explained variance. The severity of AD remained a significant predictor (β = −1.35, P < .05).
The third step included care recipient gender, AD severity, caregiver perceptions toward aging, and caregiver psychosocial factors. It was also significant (F 8, 57 = 6.20, P < .05) and explained 46.5% of variance in care recipient's physical activity. Caregiver psychosocial factors explained an additional 27% of variance in care recipient's physical activity over and above the 19.2% of variance accounted for by just the care recipient variables. Gender was a significant predictor with men participating in more physical activity (β = .80, P < .05). Caregiver's outcome expectancy for their care recipient's physical activity was also a significant and positive predictor (β = .82, P <.05). Furthermore, caregiver's self-efficacy for care recipient's physical activity had a marginally significant positive association with physical activity (β = .23, P = .07). For the summary of simplified regression analyses, see Table 3.
Table 3.
Summary of Hierarchical Regression Analysis for Variables Predicting Care Recipient PA.
| Variables | B | SE | t | R | R2 | ΔR2 |
|---|---|---|---|---|---|---|
| Step 1 | .44 | .19a | .19a | |||
| CR gender | .64 | .43 | −1.50 | |||
| AD progress | -1.36 | .32 | −4.29a | |||
| Step 2 | .48 | .19a | .00 | |||
| CR gender | .65 | .43 | −1.50 | |||
| AD progress | -1.35 | .32 | −4.23a | |||
| Caregiver aging perception | -.093 | .45 | −.21 | |||
| Step 3 | .68 | .46a | .27a | |||
| CR gender | .80 | .38 | −2.09a | |||
| AD progress | -.43 | .32 | −1.35 | |||
| Caregiver aging perception | -.66 | .39 | −1.69 | |||
| Caregiver willingness | .14 | .19 | .70 | |||
| Caregiver PA attitude | -.04 | .39 | −.11 | |||
| Caregiver PA Outcome expectation | .82 | .25 | 3.27a | |||
| Caregiver PA self-efficacy | .23 | .13 | 1.83b | |||
| Caregiver managing dementia self-efficacy | .14 | .11 | 1.27 |
Abbreviations: CR, care recipient; AD, Alzheimer’s disease; PA, physical activity.
a P < .05.
b P < .10.
Mediation Analysis
It was hypothesized that caregiver's self-efficacy for care recipient's physical activity would indirectly predict levels of physical activity by way of the caregiver's outcome expectation for care recipient's physical activity (see Figure 1). To test this hypothesis, a formal mediation test was used. 38 Since all preceding models (model 1, 2, 3) were significant (see Table 4), model 4 tested the relationship between 2 predictors (i.e., caregiver's self-efficacy and outcome expectations for care recipient's physical activity) and 1 outcome (i.e., level of care recipient's physical activity). Two predictors were significantly associated with care recipient's physical activity (see Table 4). Specifically, caregiver's self-efficacy for care recipient's physical activity was a significant variable in both model 1 and model 4, but the β for caregiver's self-efficacy in model 1 (β = .52) was greater than the β for caregiver's self-efficacy in model 4 (β =.34). Therefore, caregiver's outcome expectation for care recipient's physical activity partially mediated the relationship between caregiver's self-efficacy and care recipient's physical activity (see Figure 1). See Table 4 for the summary of mediation analysis.
Figure 1.
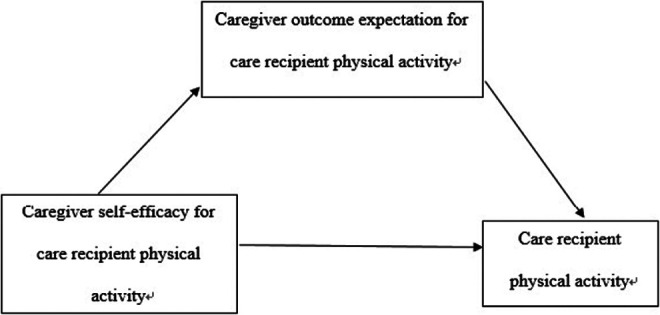
Relationships among caregiver's self-efficacy for care recipient's physical activity, caregiver's outcome expectations for care recipient's physical activity, and care recipient's physical activity.
Table 4.
Caregivers’ Self-Efficacy, Outcome Expectations, and Levels of Care Recipient's PA.
| R | R2 | F (df) | β | ||
|---|---|---|---|---|---|
| CG self-efficacy | |||||
| Model 1 | |||||
| ΔLevels of AD PA | .56 | .31 | 33.03 (1, 72) | .52a | |
| Model 2 | |||||
| Δ CG outcome expectations | .58 | .34 | 36.28 (1, 72) | .22a | |
| CG outcome expectations | |||||
| Model 3 | |||||
| ΔLevels of AD PA | .56 | .31 | 34.48 (1, 76) | 1.24a | |
| CG self-efficacy | CG outcome expectations | ||||
| Model 4 | |||||
| ΔLevels of AD PA | .63 | .40 | 23.36 (2, 70) | .34a | .85a |
Abbreviations: CG, caregiver; AD, Alzheimer’s disease; PA, physical activity.
a P < .05.
Discussion
This study was among the first to examine caregiver and care recipient factors associated with physical activity participation among older adults with AD. Our findings demonstrated the unique importance of caregivers, especially caregiver psychosocial factors (eg, attitudes, feelings, perceptions), in relation to care recipient's physical activity.
Gender and severity of AD were the only care recipient characteristics associated with physical activity. Consistent with past studies on factors related to physical activity among older adults, 18 –21 men with AD were also more likely to engage in physical activity than women with AD. Also, there was a significant negative correlation between severity of AD and care recipient's physical activity. That is, as health declines, those with AD were less physically active.
Caregiver Factors
None of the caregiver sociodemographic factors or physical or emotional health conditions were associated with care recipient's level of physical activity. There was a significant correlation between level of caregiver's physical activity and level of care recipient's physical activity, suggesting that care recipients with physically active caregivers are more likely to participate in physical activity. Thus, promoting caregiver's physical activity might be another mechanism for increasing care recipient's physical activity. Physical activity programs aimed at care recipient–caregiver dyads may be a beneficial intervention. In addition to positive health impacts of physical activity on both caregivers and care recipients, the care recipient–caregiver dyad physical activity interventions might show additional advantageous impacts such as reduced caregiver distress and improved relationships between caregiver and care recipient, which might not be captured with regular physical activity interventions for AD. Also, care recipient–caregiver dyad interventions might help to improve effects of existing physical activity interventions for people with AD. For example, weak effects and mixed outcomes of physical activity interventions for AD are critical limitations of physical activity interventions for AD which might be improved by the inclusion of caregivers in the interventions.
A substantial amount of care recipient's physical activity, however, can be attributed to caregiver psychosocial factors (27% of variance). Caregiver's self-efficacy for managing dementia, willingness to encourage care recipient's physical activity and introduce innovative interventions to improve care recipient's quality of life, and outcome expectation and self-efficacy for care recipient's physical activity were all significantly associated with level of care recipient's physical activity. In particular, caregiver's outcome expectation for care recipient's physical activity was significantly linked to level of physical activity, and caregiver's self-efficacy for care recipient's physical activity was marginally significant. This is consistent with previous research which demonstrated that outcome expectations are better predictors for older adults’ physical activity behaviors than self-efficacy for physical activity. 23,27,39 The results also supported the hypothesis that caregiver's self-efficacy constructs are an important influence on care recipient's physical activity: Caregiver beliefs in their capability to have care recipients participate in physical activity and beliefs that physical activity produces benefits for care recipients led to increased physical activity participation. Consequently, caregiver's feelings and thoughts about care recipient's physical activity appear to be the most influential factors in level of care recipient's physical activity.
Most notable, caregiver's outcome expectation for care recipient's physical activity showed strong association with levels of care recipient's physical activity. This finding was consistent with past studies on the impact of self-efficacy and outcome expectations on physical activity in older adults. 23,26,27,39 –44 For older adults, the benefits of physical activity (eg, fall prevention, stronger bones, and muscles) are a more significant motivator for doing physical activity than whether they believe they are capable of performing physical activity. 23,26,27,39 –44 Therefore, caregiver's outcome expectation for care recipient's physical activity was a better predictor of care recipient's physical activity levels than caregiver's self-efficacy for physical activity.
Mediation of Caregiver Outcome Expectations
Caregiver's outcome expectation for care recipient's physical activity partially mediated the relationship between caregiver's self-efficacy for care recipient's physical activity and reported care recipient's physical activity. This finding means that caregiver's self-efficacy for care recipient's physical activity directly predicts the care recipient's physical activity level as well as indirectly predicts care recipient's physical activity through caregiver's outcome expectation for care recipient's physical activity. The result is consistent with previous studies on outcome expectancy for physical activity among older adults. 27 Moreover, this result aligns with social cognitive theory 22 : Self-efficacy influences human behaviors through outcome expectation of the behavior. While several studies have emphasized the role of outcome expectations in physical activity participation for older adults, 23,26,27,39 –44 no study has demonstrated the impact of caregiver's outcome expectation for care recipient's physical activity on reported levels of care recipient's physical activity. This study found that caregivers’ perceived benefits of their care recipients’ physical activity on health was linked to increased physical activity in care recipients.
Practical Implications
Identifying physical activity determinants for this population can help promote physical activity interventions for those with AD in institutional or community settings. This is a crucial need, especially for women with AD. The information could further be used to develop and introduce physical activity programs/nonpharmacological interventions targeting older adults with AD and other dementias. In addition, our results suggest that caregivers are an integral key in promoting physical activity participation for older adults with AD. Therefore, interventions that teach caregivers the benefits of physical activity participation for care recipients and increase caregiver's confidence to support care recipient's participation in physical activity could help older adults with AD increase levels of physical activity. Additionally, support from aging, social, and health services providers may be especially crucial to interventions for strengthening caregiver's self-efficacy and ultimately increasing physical activity.
Limitations
There were several limitations associated with this study. First, the sample size was small relative to the number of independent variables, which might introduce bias. Another aspect of selection bias was the sample included predominantly white women. Therefore, a diverse representation of caregivers was not reflected in this study. Another limitation is that this study fully depended on caregiver self-report to get information on care recipient characteristics and level of care recipient's physical activity. Direct measurements using accelerometers would generate more reliable measures of care recipient's physical activity. Finally, this study used a cross-sectional correlational survey, which does not permit inferences about causal relationships. Generally, since mediation includes causal processes which unfold over time, longitudinal study designs are needed to fully test mediation. Despite these limitations, this study has strengths. It was the first study to examine a breadth of determinants of physical activity for older adults with AD and other dementias. Also, this study focused on the role of caregivers to which less attention has been paid in physical activity of older adults with AD. These findings contribute to the development of not only physical activity interventions but also other programs for enhancing well-being of those with AD.
Future Research
Future studies on physical activity interventions for individuals with AD should focus on appropriate levels of physical activity and safety guidelines about physical activity for older adults with AD. Additionally, possible risks of physical activity participation for individuals with AD and additional burdens or stresses of caregivers derived from care recipient's physical activity participation should be studied. Additionally, a larger, representative sample with diverse age ranges, ethnicity, and SES is crucial. In particular, ethnicity of caregiver might have a significant impact on care recipient physical activity because different ethnic groups could have different perspectives of aging and dementia care and a different perspective on well-being of individuals with AD. Finally, to fully understand the pathways of caregiver's self-efficacy on care recipient's physical activity, more study on the physical activity self-efficacy construct is needed.
In conclusion, this study identified correlates of physical activity for older adults with AD. In particular, this study highlighted the important role of caregivers in their care recipients’ physical activity. Educating caregivers about the importance of physical activity for their care recipients with AD and encouraging caregivers to help provide opportunities for their care recipients to be physically active could be beneficial for optimal mental and physical health.
Footnotes
Authors’ Note: We warrant that this study is the authors’ original work. This work has not been submitted for publication and is not under consideration for publication elsewhere. This study was a master’s thesis of the first author.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Alzheimer’s Association. Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):208–245. doi:10.1016/j.jalz.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 2. Gibson MJ, Kelly KA, Kaplan AK. Family caregiving and transitional care: a critical review. https://www.caregiver.org/sites/caregiver.org/files/pdfs/FamCGing_TransCare_CritRvw_FINAL10.31.2012.pdf. Updated October 31, 2012. Accessed July 20, 2013.
- 3. Schulz R, Martire LM. Family caregiving of persons with dementia. Am J Geriatr Psychiatry. 2004;12(3):240–249. doi:10.1097/00019442-200405000-00002. [PubMed] [Google Scholar]
- 4. Heyn P, Abreu CB, Ottenbacher JK. The effects of exercise training on elderly persons with cognitive impairment and dementia: a meta-analysis. Arch Phys Med Rehabil. 2004;85(10):1694–1704. doi:10.1016/j.apmr.1004.03.019. [DOI] [PubMed] [Google Scholar]
- 5. Kemoun G, Thibaud M, Roumagne N, et al. Effect of a physical training programme on cognitive function and walking efficiency in elderly persons with Alzheimer’s disease. Dement Geriatr Cogn Disord. 2010;29(2):505–512. doi:10.1159/000272435. [DOI] [PubMed] [Google Scholar]
- 6. Perez CA, Carral JMC. Benefits of physical exercise for older adults with Alzheimer’s disease. Geriatr Nurs. 2008;29(6):384–391. doi:10.1016/j.gerinurse.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 7. Rolland Y, Rival L, Pillard F. Feasibility of regular physical exercise for patients with moderate to severe Alzheimer’s disease. J Nutr Health Aging. 2000;4(2):109–113. [PubMed] [Google Scholar]
- 8. Suttanon P, Hill DK, Said MC, Byrne NK, Dodd JK. Factors influencing commencement and adherence to a home-based balance exercise program for reducing risk of falls: perceptions of people with Alzheimer’s disease and their caregivers. Int J Geriatr Psychiatry. 2012;24(7):1172–1182. doi:10.1017/S1041610211002729. [DOI] [PubMed] [Google Scholar]
- 9. Teri L, Gibbons EL, McCurry MS, et al. Exercise plus behavioral management in patient with Alzheimer disease: a randomized controlled trial. JAMA. 2003;290(15):2015–2022. [DOI] [PubMed] [Google Scholar]
- 10. Yu F, Kolanowski A. Facilitating aerobic exercise training in older adults with Alzheimer’s disease. Geriatr Nurs. 2009;30(4):250–259. doi:10.1016/j.jerinurse.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 11. Yu F, Swartwood MR. Feasibility and perception of the impact from aerobic exercise in older adults with Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2012;27(6):397–405. doi:10.1177/1533317512453492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yu F. Guiding research and practices a conceptual model for aerobic exercise training in Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2011;26(3):184–194. doi:10.1177/1533317511402317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Forbes D, Forbes S, Morgan DG, Markle-Reid M, Wood J, Culum I. Physical activity programs for persons with dementia. Cochrane Database System Rev. 2008:CD006489. [DOI] [PubMed] [Google Scholar]
- 14. Akin MS. Elder rehab: a student-supervised exercise program for Alzheimer’s patients. Gerontologist. 1999;39(6):729–735. [DOI] [PubMed] [Google Scholar]
- 15. Stevens J, Killeen M. A randomized controlled trial testing the impact of exercise on cognitive symptoms and disability of residents with dementia. Contemp Nurse. 2006;21(1):35–40. doi:10.5172/conu.2006.21.1.32. [DOI] [PubMed] [Google Scholar]
- 16. Williams LC, Tappen MR. Effect of exercise on mood in nursing home residents with Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2007;22(5):389–397. doi:10.1177/1533317507305588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van Alphen H, Volkers MK, Blankevoort CG, Scherder EJA, Hortobágyi T, van Heuvelen MJG. Older adults with dementia are sedentary for most of the day. PLoS One. 2016;11(3):e0152457. doi:10.1371/journal.pone.0152457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Burton CL, Shapiro S, German SP. Determinants of physical activity initiation and maintenance among community-dwelling older persons. Prev Med. 1999;29(5):422–430. doi:10.1006/pmed.1999.0561. [DOI] [PubMed] [Google Scholar]
- 19. King CA. Intervention to promote physical activity by older adults. J Gerontol A Biol Sci Med Sci. 2001;56(Spec no 2):36–46. doi:10.1093/gerona/56.suppl_2.36. [DOI] [PubMed] [Google Scholar]
- 20. Koeneman AM, Verheijden WM, Chinapaw JMM, Hopman-Rock M. Determinants of physical activity and exercise in healthy older adult: a systematic review. Int J Behav Nutr Phys Act. 2011;8(142):1–15. doi:10.1186/1479-5868-8-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rhodes RE, Martin AD, Taunton JE, Rhodes EC, Donnelly M, Elliot J. Factors associated with exercise adherence among older adults. Sports Med. 1999;28(26):397–411. doi:10.2165/00007256-199928060-00003. [DOI] [PubMed] [Google Scholar]
- 22. Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: W. H. Freeman and Company; 1997. [Google Scholar]
- 23. Resnick B. The impact of self-efficacy and outcome expectations on functional status in older adults. Top Geriatr Rehabil. 2002;17(4):1–10. [Google Scholar]
- 24. McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exerc Sport Sci Rev. 2000;28(2):85–88. [PubMed] [Google Scholar]
- 25. McAuley E, Courneya KS, Rudolph DL, Lox CL. Enhancing exercise adherence in middle aged males and females. Prev Med. 1994;23(4):498–506. doi:10.1006/pmed.1994.1068. [DOI] [PubMed] [Google Scholar]
- 26. Resnick B, Zimmerman IS, Orwig D, Furstenberg AL, Magaziner J. Outcome expectations for exercise scale: utility and psychometrics. J Gerontol B Psychol Sci Soc Sci. 2000;55(6):S352–SS356. doi:10.1093/geronb/55.6.S352. [DOI] [PubMed] [Google Scholar]
- 27. Resnick B, Palmer MH, Jenkins LS, Spellbring AM. Path analysis of efficacy expectations and exercise behaviour in older adults. J Adv Nurs. 2000;31(6):1309–1315. doi:10.1046/j.1365-2648.2000.01463.x. [DOI] [PubMed] [Google Scholar]
- 28. Fortinsky RH, Kercher K, Burant CJ. Measurement and correlates of family caregiver self-efficacy for managing dementia. Aging Ment Health. 2002;6(2):153–160. doi:10.1080/13607860220126763. [DOI] [PubMed] [Google Scholar]
- 29. Steffen AM, McKibbin C, Zeiss AM, Gallagher-Thompson D, Bandura A. The revised scale for caregiving self-efficacy: reliability and validity studies. J Gerontol B Psychol Sci Soc Sci. 2002;57(1):74–86. doi:10.1093/geronb/57.1.P7429. [DOI] [PubMed] [Google Scholar]
- 30. Semiatin AM, O’Connor MK. The relationship between self-efficacy and positive aspects of caregiving in Alzheimer’s disease caregivers. Aging Ment Health. 2012;16(6):683–688. doi:10.1080/13607863.2011.651437. [DOI] [PubMed] [Google Scholar]
- 31. University of Washington, Health Promotion Research Center. Physical activity assessments tools. http://depts.washington.edu/hprc/rapa. Published 2006. Accessed April 8, 2014.
- 32. Topolski TD, LoGerfo J, Patrick DL, Williams B, Walwick J, Patrick MB. The Rapid Assessment of Physical Activity (RAPA) among older adults. Prev Chronic Dis. 2006;2(4):1–8. [PMC free article] [PubMed] [Google Scholar]
- 33. Watson D, Clark AL, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. doi:10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 34. Sexton E, King-Kallimanis LB, Morgan K, McGee H. Development of the Brief Ageing Perceptions Questionnaire (B-APQ): a confirmatory factor analysis approach to item reduction. BMC Geriatr. 2014;14(44):1–11. doi:10.1186/1471-2318-14-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Benjamin K, Edward NC, Bharti VK. Attitudinal, perceptual, and normative beliefs influencing the exercise decisions of community-dwelling physically frail seniors. J Aging Phys Act. 2005;13(3):276–293. [DOI] [PubMed] [Google Scholar]
- 36. Resnick B, Jenkins SL. Reliability and validity of the self-efficacy for exercise and outcome expectations for exercise scales with minority older adults. J Nurs Meas. 2004;12(3):235–247. doi:10.1891/jnum.12.3.235. [DOI] [PubMed] [Google Scholar]
- 37. Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi:10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 38. Kenny DA. Baron-Kenny mediation. http://davidakenny.net/cm/mediate.htm. Updated September 28, 2016. Accessed November 2, 2014.
- 39. Resnick B. Functional performance of older adults in long term care setting. Clin Nurs Res. 1998;7(3):230–246. [DOI] [PubMed] [Google Scholar]
- 40. Resnick B. A prediction model of aerobic exercise in older adults living in a continuing-care retirement community. J Aging Health. 2001;13(2):287–310. doi:10.1177/089826430101300207. [DOI] [PubMed] [Google Scholar]
- 41. Resnick B. Testing a model of exercise behavior in older adults. Res Nurs Health. 2001;24:83–92. doi:10.1002/nur.1011. [DOI] [PubMed] [Google Scholar]
- 42. Resnick B. Testing a model of overall activity in older adults. J Aging Phys Act. 2001;9:142–160. [Google Scholar]
- 43. Resnick B, Orwig D, Magaziner J, Wynne C. The effect of social support on exercise behavior in older adults. Clin Nurs Res. 2002;11(1):52–70. doi:10.1177/105477380201100105. [DOI] [PubMed] [Google Scholar]
- 44. Williams DM, Anderson ES, Winett RA. A review of the outcome expectancy construct in physical activity research. Ann Behav Med. 2005;29(1):70–79. doi:10.1207/s15324796abm2901_10. [DOI] [PubMed] [Google Scholar]


