Abstract
Background:
Paratonia is a major underlying motor problem impeding functionality and locomotion in dementia. Despite its undeniable impact on patient’s quality of life and daily care, there is a lack of evidence-based therapy on patients with this condition.
Methods:
We surveyed physiotherapists working in nursing homes in Flanders (Belgium) concerning the use and perceived effect of therapeutic strategies and positioning methods/aids.
Results:
Positioning and soft passive mobilization were the most applied and positively appraised therapeutic interventions. Highest ratings for positioning were found for C-shaped positioning cushions and multi-position wheelchair. According to the respondents, key points for paratonia approach were relaxation, positioning, active movement stimulation, and—to some extent—passive mobilization. Indispensable for any success however is multidisciplinary cooperation.
Conclusion:
These findings might provide an inspirational path for research to verify possible (evidence based) beneficial treatments that could be applied to improve current and future treatment of patients with paratonia.
Keywords: dementia, paratonia, therapeutic strategy, positioning, survey
Introduction
Although cognitive deterioration is the most predominant impairment in dementia, motor problems are also commonly observed during the course of the disease and may even in some forms precede the cognitive deficits. 1 –6 In vascular dementia and Lewy body dementia, motor problems are already prominent in the early stages, whereas in Alzheimer’s dementia, these may be initially very subtle (eg, clumsiness) and thereby often only noticed by close relatives. 7 As dementia progresses, motor disturbances become more prominent and disabling in all types, until the ability of locomotion is lost and patients become bedridden. 7,8
One of the major underlying motor problems impeding functionality and locomotion in dementia is paratonia (Figure 1). 8,9 This is a form of hypertonia, with an involuntary, variable resistance against passive movement, in which the degree of resistance depends on the speed of movement and the applied force. 10 Paratonia increases with progression of dementia. Prevalence estimates vary according to the stage of dementia, ranging from 10% in the early stages to 90% to 100% in end-stage dementia. 8,11 –14
Figure 1.

Patient with severe paratonia.
The presence of paratonia has an undeniable impact on the quality of life (QoL) of people with this condition. 8 For instance, persons with paratonia are likely to experience difficulties in adjusting their own movements/postures to those of other persons. As a result, cooperative mobility actions in daily care procedures, such as washing, dressing, positioning, and so on, become hampered and annoying for patients and their caregivers. 8 Frequently, uninformed caregivers will estimate the offered resistance against imposed movements as being intentional and therefore judge the patient as “difficult”, resulting in a strenuous and painful struggle during daily care procedures. As a consequence, patients as well as caregivers are confronted with a challenging discomfort in receiving or giving care, especially in severe stages of paratonia. 8,9,11 Furthermore, paratonia is often related to a further decline in functional mobility, 9,13 which commonly leads to the development of contractures and pressure ulcers. 11,15 The pain caused by the contractures and pressure ulcers can in turn raise the muscle tone incrementally, creating a self-maintaining decline process.
Despite the high prevalence of dementia with accompanying paratonia and the obvious impact of this form of hypertonia on patients’ QoL and caregivers’ burden, the body of knowledge concerning this phenomenon and its pathogenesis is scarce and most often hypothetical. 12 –14,16 –19 This jeopardizes any attempt to correctly make informed decisions about the care of patients with paratonia. Based on this restricted knowledge, the lack of any evidence-based therapy or even any attempt for that matter is evident. More specifically, in residential care or in nursing homes, the lack of any (evidence based) advice or guideline can be professionally embarrassing and clinically challenging for health-care workers since the high number of patients confronts them on daily basis with this gap in knowledge and abilities. As a reaction, many attempts are made by physiotherapists and other caregivers to empirically explore strategies to deal with the consequences of paratonia, or—if possible—to postpone or slow down the process of paratonia. However, results of these individual empirical attempts are most frequently unknown by other caregivers or researchers while they could have inspiring potential.
This manuscript reports the results of a survey among physiotherapists, a group of primary caregivers often consulted for matters of muscle tone and (restricted) mobility. In absence of any evidence, this group of health-care workers seemed to be an appropriate source of information regarding this topic. The aim of this survey was as follows: (1) to distinguish the most currently therapeutic strategies and positioning methods/aids used in Flanders, with their corresponding perceived effect on paratonia and (2) to reveal the key points of the clinical approach to manage paratonia, as experienced by certified physiotherapists in the region of Flanders.
Methods
Study Design
This study is a quantitative descriptive design using a self-report survey questionnaire.
Procedure
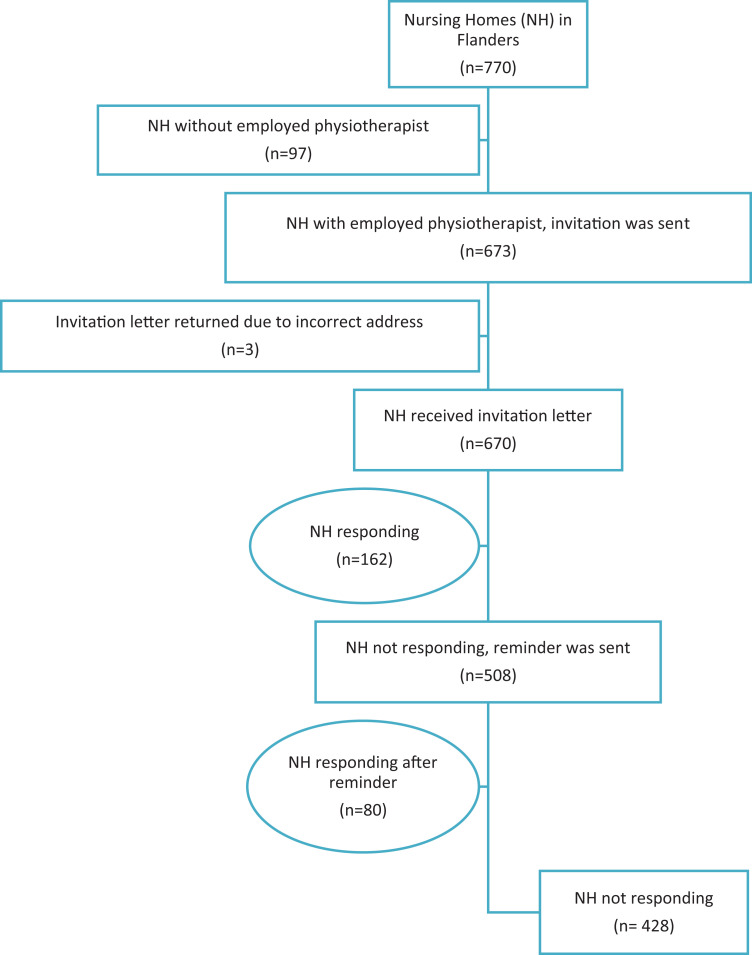
A list of all nursing homes in Flanders, the northern part of Belgium, was extracted from the website of the Belgian National Institute for Health and Disability Insurance. From this list (n = 770), the nursing homes labeled with one or more employed physiotherapist(s) were selected (n = 673). An invitation letter for participation was sent out to these nursing homes addressed to the physiotherapists, with a unique entry code and a web-address to access an online survey. After 1 month, a reminder was sent to nonresponding physiotherapists (Figure 2).
Figure 2.
Flow-chart of responses.
Survey
The online survey consisted of 68 questions distributed over 5 main sections: (1) estimated prevalence of paratonia and eventual existence of a paratonia policy, (2) perceived effect of currently used therapeutic strategies, (3) perceived effect of currently used positioning methods/aids, (4) “passivities” of daily living (a 24-hour concept of comfort care for passive patients), and (5) general information on the nursing home and the responding physiotherapist.
Most questions were obligatory and presented in a multiple-choice format with a single-answer option, though the option “other” could also be selected in some of the questions. Besides several open-response questions were added to render respondents the opportunity to clarify and refine the given closed answers and to give additional remarks and suggestions if desired.
The topics included in this survey were chosen after thorough discussion by the researchers. A list of possible therapeutic interventions as well as positioning methods/aids was composed based on the researcher’s own experiences, in consultation with experts from the work field (incompleteness was counterbalanced by adding the option “other”). These interventions and methods are listed and briefly explained in the explanatory boxes 1 to 3. Before final dissemination, 6 volunteers (all familiar with the topic, some with an academic background, others working in nursing homes) were asked to criticize a pilot version, with special attention for both clarity in description as relevance/completeness and flaws in content. Based on the feedback we collected from this first pilot, appropriate modifications and improvements were made.
Explanatory Box 1.
Brief explanation of the proposed therapeutic strategies.
Stretching: Manually applied stretch in order to increase tissue extensibility.
Soft passive mobilization: Soft (gentle) passive movement of the limbs in order to increase range of motion (ROM).
Motomed: Device for (activo-)passive motor-supported cycling.
Active mobilization: Active exercise therapy, most often with the intention of maintaining/increasing ROM. This can also include gait or standing exercises, power training.
Gait training: Walking with/without assistance of physiotherapist(s)/walking aids.
Pulsations/rocking: Passive movements with a rhythmic, pulsing, or rocking character, can be applied to different parts of the body. The character of these movements is rather relaxing than mobilizing.
Snoezelen: This is a form of multisensory stimulation, most often in a separate room with pleasant lights, music, aroma therapy, soft comfortable furnishings, and so on.
Relaxation bath: Bathing with the intention to relax (gentle movements, pleasant atmosphere, often combined with multisensory stimulation eg, music, aromatherapy).
Massage: The use of any massage technique to any part of the body (eg, hand, back, legs, etc).
Positioning: Putting the resident in a comfortable, well-supported (seated/lying) position, according to individual needs. Diverse materials/devices can be used to obtain this position.
Soft bracing: The use of correcting/supporting orthoses with soft outer materials, with the intention of preventing (further) formation of contractures.
Heat application: Any kind of application of warmth/heat, for example, heat packages.
No physiotherapy: no therapeutic strategies applied.
Explanatory Box 2.
Brief explanation of the proposed positioning methods/aids in bed.
GSP: “Gravitational stretch position”, that is, a position in which a limb that has a contracture is not fully supported, in order to achieve a kind of stretch exerted by the gravity of the limb.
Normal cushions LL or UL: Any available cushion (pillow, decorative cushions, etc) that can be used to support the lower limbs (LLs) or upper limbs (ULs).
Positioning cushion LL or UL (Figure 3): Long, C-shaped comfort cushion used to support the LL or UL. According to the chosen application, support of the head and/or stabilization of the trunk can be simultaneously obtained. Usually, when applied to the UL, the tail ends support the UL while the middle part supports the head and shoulders. When applied to the LL, most often the middle part is under the knees and the tail ends stabilize the pelvis and trunk on both sides.
Custom-made cushion LL or UL: Custom-made supporting cushion orthoses for LL or UL, according to individual needs and supporting eventual contractures.
MSP: “Modular system of positioning cushions and supports”, that is, a system for individualized positioning, consisting of separate cushions of diverse formats, that can be fixated by movable supports (usually secured by Velcro to the mattress). This system is adaptable to different lying positions and changing needs of the patient.
Therapeutic blanket: A weighted blanket (filled with plastic balls or polystyrene grains) to provide extra tactile input to the body and stimulation of the sensory system when patients are lying in their bed.
Swaddling: Wrapping the resident’s body tightly in a sheet, in order to provide tactile information and stimulate body awareness. It is comparable to swaddling infants in order to help them fall asleep.
Explanatory Box 3.
Brief explanation of the proposed positioning methods/aids for sitting.
Inclinable armchair: Standard armchair in nursing homes, with possibility to recline position.
S/M wheelchair: Standard/modular lightweight wheelchair. A standard wheelchair has a straight back and seating and cannot be inclined, whereas a modular wheelchair can have a preformed seating/back (lateral support) and leg supports and is inclinable.
MPW: “Multi-position wheelchair”, that is, a wheelchair with preformed seating, back and head rest and adjustable leg supports, that provides good lateral support in variable positions (allows inclination to semi-lying position).
Wheelchair with SO: Wheelchair with a custom-made sitting orthosis for individualized positioning. Adjustable in diverse positions.
CMS: Comfort modular seating system (eg, Kelvin wheelchair): wheelchair with several adjustment options (eg, degree of support and filling of seating/back), in order to provide a maximum top-to-toe support. A soft, flexible, “embracing” arm support can be provided to give a sense of security.
Statistical Analysis
Data were imported and analyzed using the Statistical Package for the Social Sciences version 22 (SPSS 22), by means of descriptive statistics. For the calculation of appraisal of therapeutic interventions and positioning methods/aids, data from respondents answering “not used” were excluded.
Qualitative Data
Despite the quantitative descriptive design of the study, open-answer questions provided qualitative data. These data were used for additional remarks and interpretation of quantitative results.
Results
Respondents
Six hundred seventy physiotherapist received an invitation letter (3 letters returned due to incorrect address). Two hundred forty-two of these potential respondents completed the online survey (162 after the first invitation, 80 after a reminder), with an attained response rate of 36% (Figure 2). In all, 70.5% of the responders were female, with a mean age of 42 (±9.1) years. The average experience in working with persons with dementia was 13.7 (±8.5) years.
Prevalence of Paratonia and Presence of Paratonia Policy
Ninety-six percent of the respondents indicated that, at the moment of the survey, at least 1 resident in their nursing home had difficulties in daily care and/or comfortable positioning due to paratonia. The mean capacity of the nursing homes was 110 (±52) residents. The respondents estimated that out of the total population of their nursing home, on average, 42% (±17%) had dementia, out of which an estimated 41% (±22%) had paratonia. In this paratonia subsample, 63% (±29%) had difficulties in daily care and/or comfortable positioning and 42% (±25%) had contractures. In 76% of the nursing homes, there was a trained “reference person for dementia” (a professional specifically trained and engaged to improve the quality of care for persons with dementia); this was mostly a nurse (41%) or an occupational therapist (39%).
In 17% of the nursing homes, a standardized paratonia policy or guideline was available. If present, this protocol was mostly based on multidisciplinary deliberation, in which mainly physiotherapists, nurses, and occupational therapists were involved. Whenever difficulties in daily care or positioning were experienced, 54% of the respondents reported that any approach was discussed during multidisciplinary meetings, 31% indicated that nurses and nursing auxiliaries deliberated among themselves in view of any approach without consulting with other disciplines, and 14% of the respondents stated that every caregiver acted according to his or her own preferences, without any kind of intra- or interdisciplinary deliberation.
Therapeutic Strategies
Thirteen therapeutic strategy choices in addition to the choice of “other” were offered in this survey (explanatory box 1). Respondents were asked to estimate and individually grade each of the therapeutic strategies. For each strategy, participants were asked to give their personal estimation/appreciation and experience concerning the effect on muscle tone and range of motion (ROM) in persons having severe paratonia. Notably, it was possible to indicate whether a particular strategy was not used in this population.
Table 1 provides an overview of the responses for therapeutic strategies. Positioning (97.9%) and soft passive mobilizations (95.4%) were found to be the most commonly applied therapeutic strategies. The highest positive appraisals concerning the subjective effect on muscle tone and ROM were retrieved for positioning (94.4%), relaxation baths (94.2%), and pulsations/rocking (92.1%). According to the respondents, none of the therapeutic strategies had a beneficial effect on muscle tone and ROM that lasted longer than 2 hours, except for positioning and soft bracing.
Table 1.
Use and Subjective Estimation of Influence on Muscle Tone and ROM of Different Therapeutic Strategies for Persons Having Severe Paratonia.
| Application | Appraisal | |||
|---|---|---|---|---|
| Percentage Used | Negative | Neutral | Positive | |
| Stretching | 75.3% | 9.8% | 26.4% | 63.8% |
| Soft passive mobilization | 95.4% | 2.6% | 9.6% | 87.8% |
| Motomed | 60.7% | 5.8% | 11.5% | 82.7% |
| Active mobilization | 67.9% | 10.6% | 24.8% | 64.6% |
| Gait training | 73.5% | 6.3% | 18.3% | 75.4% |
| Pulsations/rocking | 65.8% | 2.0% | 5.9% | 92.1% |
| Snoezelen | 54.8% | 1.7% | 9.2% | 89.1% |
| Relaxation bath | 77.2% | 0.0% | 5.8% | 94.2% |
| Massage | 73.7% | 2.9% | 23.6% | 73.6% |
| Positioning | 97.9% | 0.4% | 5.2% | 94.4% |
| Soft bracing | 33.6% | 9.6% | 20.5% | 69.9% |
| Heat application | 46.5% | 4.7% | 20.8% | 74.5% |
| No physiotherapy | 43.0% | 62.2% | 33.7% | 4.1% |
Abbreviation: ROM, range of motion.
The respondents were asked to rate the effect of the used therapeutic strategies on alleviation of caregiver burden during daily care for paratonia patients. Regardless of the therapeutic strategy applied, 20% of the respondents reported an evident positive effect, 68% a rather positive effect, only 6% reported no effect, and 6% answered they didn’t know. In 61% of the cases, respondents stated that their answer on this question was based on appreciation that was communicated to them by the nursing staff, 39% reported their own estimation.
Also, the effect of the used therapeutic strategies on (estimations of) alleviation of pain experienced by the resident during daily care was inquired. Regardless of the therapeutic strategy applied, 77% estimated the effect to be evident (15%) to rather positive (62%), in 10% no effect was observed, and 13% did not know. For this question, 44% of the responding physiotherapists based their answer on feedback from their nursing staff.
Positioning Methods
A selection of 7 possible bed positioning methods/aids, plus the choice of “other”, was presented (explanatory box 2). The rating procedure was the same as for therapeutic strategies, that is, each positioning method/aid was rated individually.
Table 2 provides an overview of the responses for positioning in bed. “Positioning” cushions (Figure 3) and “normal” cushions, both for upper limbs (ULs) and lower limbs (LLs), were the most commonly used, whereas positioning cushions (UL: 91.5%, LL: 91.1%), custom-made cushions (UL: 88.4%, LL: 87.2%), and a modular system of positioning cushions and supports (81.2%) were the methods/aids with the highest positive ratings concerning subjective effect on muscle tone and ROM in this population.
Table 2.
Subjective Estimation of Influence on Muscle Tone and ROM of Different Positioning Methods/Aids in Bed for Persons Having Severe Paratonia.
| Application | Appraisal | |||
|---|---|---|---|---|
| Percentage Used | Negative | Neutral | Positive | |
| GSP | 41.6% | 26.6% | 20.2% | 53.2% |
| Normal cushions LL | 87.6% | 4.4% | 19.1% | 76.5% |
| Normal cushions UL | 84.8% | 4.1% | 18.9% | 77.0% |
| Positioning cushion LL | 96.1% | 0.9% | 8.0% | 91.1% |
| Positioning cushion UL | 95.7% | 1.3% | 7.2% | 91.5% |
| Custom-made cushion LL | 33.9% | 2.6% | 10.3% | 87.2% |
| Custom-made cushion UL | 30.0% | 1.4% | 10.1% | 88.4% |
| MSP | 31.4% | 2.9% | 15.9% | 81.2% |
| Therapeutic blanket | 17.1% | 7.9% | 18.4% | 73.7% |
| Swaddling | 13.6% | 6.9% | 17.2% | 75.9% |
Abbreviations: GSP, gravitational stretch position; LL, lower limb; MSP, modular system of positioning cushions and supports; ROM, range of motion; UL, upper limb.
Figure 3.

Positioning cushion.
In general, installation and removal of positioning materials was reported to cause (nearly) no extra work load for the nursing staff. In 45% of the cases, respondents reported that their answer was based on appreciation that was explicitly communicated to them by the nursing staff, and 55% made their own estimation for this matter.
Similarly, a selection of 5 possible positioning methods/aids for sitting, plus the choice of “other”, was presented. An overview and brief explanation of the proposed positioning methods/aids can be found in the explanatory box 3. Again, every positioning aid/method was rated individually.
Table 3 provides an overview of the responses for positioning methods/aids for sitting. The multi-position wheelchair (MPW) was obviously the most frequently used positioning aid (95%), whereas the highest subjective positive effect on muscle tone and ROM was reported for the wheelchair with sitting orthosis (92.5%), MPW (87.7%), and the comfort modular seating system (CMS; 81.3%).
Table 3.
Subjective Estimation of Influence on Muscle Tone and ROM of Different Sitting Positioning Methods/Aids for Persons Having Severe Paratonia.
| Application | Appraisal | |||
|---|---|---|---|---|
| Percentage Used | Negative | Neutral | Positive | |
| Inclinable armchair | 74.9% | 17.6% | 27.8% | 54.5% |
| S/M wheelchair | 71.3% | 36.1% | 31.4% | 32.5% |
| MPW | 95.0% | 2.6% | 9.6% | 87.7% |
| Wheelchair with SO | 78.2% | 2.2% | 5.4% | 92.5% |
| CMS | 14.7% | 0.0% | 18.8% | 81.3% |
Abbreviations: CMS, comfort modular seating system; MPW, multi-position wheelchair; S/M wheelchair, standard/modular lightweight wheelchair; SO, sitting orthosis.
Additionally, the respondents were asked to what extent any agreement concerning positioning of a patient was respected by all staff members: 8% of the respondents answered “seldom”, 31% “sometimes”, 54% “mostly”, 3% “always”, and 2% did not know. Here, only 2% of the respondents stated that agreements concerning positioning were never made.
“Passivities” of Daily Living
“Passivities of daily living” (PDL) is the description used in Flanders and the Netherlands for a global, 24-hour concept of comfort care for patients who are no longer able to perform the “activities of daily living” (ADL). A prerequisite for PDL is that the caregiver accepts the situation of passivity of the resident. The main goal is to maximize quality of care and the well-being of both the resident and the caregiver. 20,21 The PDL concept has been elaborated in the Netherlands, but it is widespread in Flanders as well. In residents with paratonia, for example, changes in the order of routine washing and clothing actions can be implemented, with the intention of restricting pushing, pulling, and turning maneuvers during daily activities and avoid subsequent increase of muscle tone. Also, adapted clothing can be helpful to limit uncomfortable actions (eg, creating an opening on the back of a dress can avoid the need of high raising of the arms).
Seventy-nine percent of the respondents reported that PDL is used in their nursing homes. Thirty-six percent of the responding physiotherapist received a training in it; in 62%, another staff member (mostly occupational therapists) followed a PDL training.
However, the use of adapted clothing is not well established yet. In 24% of the respondents, none of the residents with difficulties in daily care due to severe paratonia wore adapted clothing. Of the 76% who did use adapted clothing, the majority (60%) only used it in ≤25% of the residents with such difficulties.
The most important reasons for not using adaptive clothing were too expensive (31%), the team was not familiar with it (19%), or the close relatives refused because of esthetical reasons (8%). Respondents remarked that adapting the residents’ own clothes is helpful to reduce the price, and it is more likely to be accepted by the close relatives since the resident can continue wearing his/her own familiar outfit.
Discussion
In all, 242 physiotherapists completed the full survey. The interest of more than one-third of these residency physiotherapists in responding to a long survey expresses the relevance of paratonia in dementia for daily practice. Several respondents explicitly mentioned and asked in open remark sections the need for a coherent set of advices and a generic guideline. Also, respondents frequently reported the lack of attention given to this topic in regular education in all care disciplines and consistently stressed the need for additional posteducational courses for this matter.
The present study revealed that most nursing homes (83%) do not have any kind of standardized paratonia policy. Furthermore, only in half of the residential care settings (54%), consultation at a multidisciplinary level takes place when difficulties in daily care or positioning are experienced due to paratonia. Respondents stated, however, that a multidisciplinary concerted 24-hour approach seems imperative for the management of paratonia-related challenges. Since none of the present therapeutic interventions, or attempts for that matter, was rated as being potentially successful unless an appropriate interdisciplinary communication and a well-organized cooperation within the whole team was ensured. This is in agreement with Arnts et al, who underlined the importance of a good collaboration between physiotherapists, nurses, and physicians in case of paratonia. 22
According to the results of our survey, the therapeutic strategy most commonly applied (97.9%) is positioning. This strategy implies in general the use of a lot of cushions to support all parts of the body, to provide stability and comfort (and thereby relaxation) and to create a sense of security for the patient. It is suggested that the surrounding with cushions also increases the amount of tactile information. 23 This kind of somatosensory information can be considered as a necessity to enforce the cortical representation of the body parts. 24 Interestingly, this representation could be hampered by the natural neurodegenerative process itself as well as by a reduction of proprioceptive input caused by inactivity. 25 –27 In addition, position sense can be affected by age, particularly in absence of weight bearing. 28,29 It is hypothesized that to compensate for the supposed loss of body perception, patients search for additional information concerning their own body by means of tactile stimuli, for instance by pressing knees or feet together. 30 Hence, it can be assumed that offering tactile stimuli, for example, by means of supporting cushions, can have a positive effect on paratonia for that matter. However, literature concerning this topic is scarce and mainly based on case-wise experiences. Empirical findings from this type of studies have shown an apparent decline in muscle tone after supporting the LLs with a triangular cushion and also a decrease in contracture formation. 22,30 In a pilot study by Hobbelen et al, supporting cushions have shown a beneficial effect on the severity of paratonia in the ULs of 5 participants; however, the beneficial effects of good supporting cushions could not be generalized to all limbs and movement directions. 31 This emphasizes the need for further research in a larger group of patients to confirm the positive effect of this commonly used intervention on paratonia.
Positive experiences concerning positioning were also frequently mentioned in open-answer questions, additional remarks, and suggestions. Respondents often stated that this positioning should not be conducted in view of gaining ROM but in attempt of maintaining it after any achieved improvement, for example, after relaxation intervention. Another frequently mentioned comment was that discomfort arises rapidly when a certain position is maintained for a long period, especially while seated. This is regarded as a consequence of the fact that many patients are not able to change their position independently. Therefore, regular variation in positioning should be pursued not only between lying and sitting positions but also between different types of sitting/lying (eg, other device, changing degree of inclination, etc). In this respect, an attentive attitude (for a quick and adequate response to any alteration in the resident’s condition and needs) and engagement of all staff members within a 24-hour positioning program is mentioned by several respondents as being of utmost importance to maintain any long-term positive effect on muscle tone, ROM, comfort/pain, and so on. However, respondents reported a rather low compliance to agreements on positioning (8% reported agreements were rarely met by all staff members). This ascertainment justifies again the essential need for good interdisciplinary communication and additional education. If consistently implemented, the 24-hour continuity of positioning programs is probably a motivated explanation for the fact that—in contrast to other therapeutic strategies—the effect of positioning and soft bracing lasts for more than 2 hours. It seems likely that the long-lasting effect is mainly due to a longer duration of application. Another fundamental remark concerning positioning was that—to date—seemingly valuable aids such as a CMS or a therapeutic blanket are not reimbursed by the Belgian medical insurance system. It can be assumed that reimbursement of these (rather expensive) aids would encourage their use, since at this moment, there is an apparent discrepancy between the high positive appraisal and the low use rates of these devices. This emphasizes even more the need for further research in a larger group of patients to investigate the effect of these positioning aids on paratonia.
An additional commonly applied, and from a physiotherapeutic point of view, essential therapeutic strategy is soft passive mobilization therapy (PMT). A pilot study from Hobbelen et al has suggested a beneficial short-term effect (average effect of single treatment, immediately after session) of PMT on paratonia, whereas long-term effects (after 3 weeks of treatment) were uncertain. 31 A subsequent multicenter randomized controlled trial found no positive long-term effect (after 4 weeks of treatment) of PMT, neither on paratonia nor on comfort for the caregiver or the patient. 32 On the contrary, the trend of effect of PMT was negative increasing the muscle tone, even though PMT was applied with a slow conduct and under the pain threshold according to the empirical advices given by Arnts et al. 22,32 Also, though frequently applied for that purpose, the effect of PMT for the treatment or prevention of contractures also remains unclear. 33 Regular stretching techniques turned out to be not effective for contracture management; a long-lasting stretch (eg, repeated or sustained over days/weeks/months as in splinting) would be needed since most stretch techniques induce only a transient increase in tissue extensibility due to viscous deformation, which disappears quickly after removal of the stretch. 34 Besides, an animal study indicated that, when stretch is applied to activated muscle fibers, susceptibility to injury on sarcomere level was higher in older than in younger rats. 35 Since paratonia patients are frequently actively resisting the imposed movements during PMT, it could be speculated that small microtraumata might arise in the frail muscle tissue, causing pain and consequently raising muscle tone. 32 In the present study, respondents disagreed on the effect of PMT. Some respondents reported a definitely positive effect of PMT and started this therapy as soon as possible, others stated to use PMT only when active movement therapy became impossible, and others reported no added value of PMT at all. Also, several respondents reported the use of pulsating mobilization and harmonic techniques as an alternative for PMT. Pulsating/oscillating movements used in harmonic techniques are believed to influence muscle tone, provide proprioceptive stimuli, reduce pain perception, and evoke a relaxation response. 36 The mentioned experience in relation to the proposed effects of this techniques motivates and further warrants the investigation of the effect of these techniques on paratonia.
In this survey, the positive appraisals on active mobilization are fairly moderate. Importantly, however, the questions were asked for the effect of the given therapeutic strategies in patients with severe paratonia. In these patients, the feasibility of performing active exercises is often low. On the other hand, open-answer questions revealed that in the first stages an active or activating approach might be a valuable strategy to slow down or prevent further development of paratonia. Apart from the beneficial effects on cardiorespiratory fitness and behavior, physical, and cognitive function, 37 –42 physical activity and weight-bearing exercises can also stimulate proprioception and improve the reconstruction of the cortical representation of the body parts. 29,43 Functional training (eg, sit-to-stand) can improve ADL function 44 and thereby decrease the amount of care the patient needs. Furthermore, active movement and maintaining ambulation is helpful in prevention of contractures. 45 –47 Most respondents reported the importance of encouraging the residents as long as possible to perform active movements. In an early stage, this could be achieved through supervised exercise therapy or organized group gymnastics or dance activities. Later on, the focus should be placed mainly on functional training (ie, gait, sit-to-stand, etc) and assisted activation (ie, mechanotherapy, pulleys, Motomed). At final stages, when gait is completely lost, standing should still be encouraged.
The respondents also mentioned the use of several relaxation techniques, such as rocking movements, application of heat, massage, hydrotherapy, snoezelen, aromatherapy, and so on. The choice for a certain technique should be subject to the preferences of both therapists and residents. In paratonia patients, relaxation will often result in a short-term gain of ROM. To the best of our knowledge, there are no studies investigating the effect of relaxation techniques on paratonia. Reviews considering the effect of sensory stimulation, such as “snoezelen,” massage, and aromatherapy in persons with dementia could not demonstrate a clear long-term beneficial effect on behavior or QoL. 23,48 –52 However, lack of quality and excess in diversity is mentioned, and a wide variety between studies in treatment approaches made it difficult to draw general conclusions. 23,48 –52
Also, several respondents highlighted the importance of a relaxed tranquil approach of persons with paratonia. Since paratonia is highly influenced by external stimuli (such as a sudden loud noise, an abrupt touch, a light being turned on, a hurried or angry voice, etc), 8,23,31 it is essential that all caregivers are aware of this and try to avoid such external provocations. Nevertheless, this calm unclenched approach is often challenged by stress, due to a lack of staff and shortage of time, which unfortunately seem to be omnipresent in residential care settings. Notably, a relaxed tranquil approach, in spite of the probable haste, might save a lot of time in the end.
Furthermore, respondents mentioned that special attention should be paid to prevention of decubitus. Although alternating pressure mattresses are frequently used, their inherent instability might increase muscle tone in patients with paratonia. 30 A case study of Van de Rakt described a patient with severe paratonia and contractures and at high risk of decubitus who did not develop pressure ulcers after changing an alternating pressure mattress into a firm, solid mattress and triangular cushion supporting the legs. 30 Besides the improved sense of stability, the use of supporting cushions to fill up the gap under the contractured limbs can increase the contact area and enhance the spread of pressure. Nevertheless, careful follow-up of the high-risk zones remains vital.
Also, in patients with paratonia, one should be attentive to possible underlying pain, which might have an influence on muscle tone. Actually, the use of analgesics is lower in patients with dementia than in elderly patients without dementia, though both patient groups experience pain. This could indicate an “undertreatment” of pain in patients with dementia. 42 Pain might remain unnoticed by the caregivers due to communication problems, especially in patients with severe dementia. For pain assessment in noncommunicative patients, observation scales, such as Pain Assessment IN Advanced Dementia (PAINAD), Pain Assessment Checklist for Seniors with Limited Ability to Communicate (PACSLAC), Discomfort Scale - Dementia of Alzheimer Type (DS-DAT), are frequently used. 42,53,54 Yet, the detection of pain partially depends on the attentiveness and perceptivity of the caregiver for pain signals. Also, observation scales mostly rely on facial expression of pain, which might be blurred in specific subtypes of dementia (eg, extrapyramidal symptoms in Lewy body dementia). 42
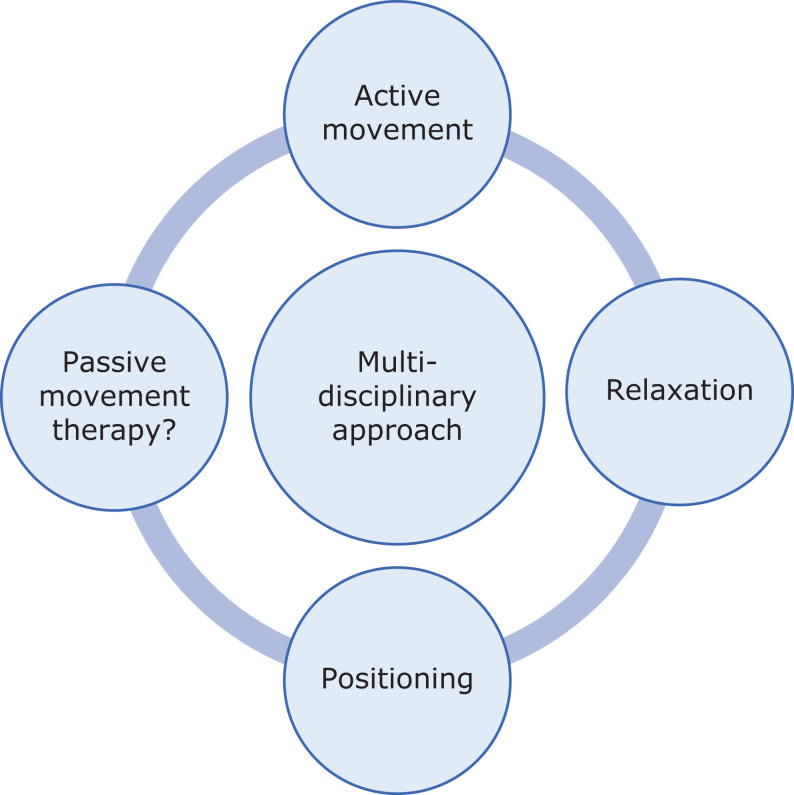
Figure 4 provides the key points of the most effective paratonia approach according to the respondents of our survey. To summarize, all respondents agreed on the importance of active movement, relaxation, and positioning, while opinions on (modalities of) passive movement were nonunanimous. Finally, we would like to highlight that nearly all respondents advocated that the key factor to success is a multidisciplinary approach.
Figure 4.
Key points of paratonia approach.
Study Limitations
This study had some limitations. First of all, no differentiation was made between dementia subtypes or dementia stage. As a consequence, it is not possible to differentiate in effectiveness of interventions according to stage or subtype. Although we specifically addressed residents with “severe paratonia” in a number of questions. In the survey, the definition of Hobbelen et al 10 was provided to make sure that all respondents used the same criteria; however, it was not explicitly asked how paratonia was diagnosed. Additionally, we purposefully included the eventual presence of other comorbidities. Secondly, predefined answer possibilities were offered. For instance, all different types of therapeutic interventions were explicitly given (eg, positioning methods, etc). This was done purposefully to facilitate the analysis of the gathered data and to enhance the time efficiency in completing the survey. However, this could have restricted the answer options, which is a direct disadvantage of any closed-ended questions. Importantly, however, the option “other” was most of the time provided to offer the possibility of additional answer options. Furthermore, as in any survey study, it is inherently difficult to ensure that every respondent interprets each question and answer possibility in the exactly same way. To address this last issue, a pilot version was first tested to improve the clarity and interpretation of each question. Additionally, space for remarks were offered, to give respondents the opportunity to clarify or refine each answer. Even when taking all these aspects into consideration, differences in the respondent’s interpretation cannot be fully excluded.
Conclusions
Though paratonia was estimated to be present in 41% of the nursing home residents having dementia, only a minority (17%) of nursing homes has stipulated a (standard) paratonia policy. The present study shows that the most applied and subjectively positive appraised therapeutic interventions were positioning and soft passive mobilization. According to the majority of the respondents, active movement should be encouraged as long as possible, and also several relaxation techniques can be used. Remarkably, a tranquil approach by all caregivers is needed, and one should be attentive for possible underlying pain. Indispensable for the success of any therapeutic intervention for paratonia is a multidisciplinary involvement and good communication and cooperation between all staff members. These findings might provide inspiration for mandatory further research to verify subjective findings evolving into possible evidence-based beneficial treatment of patients with paratonia.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Shin HY, Kim SW, Kim JM, Shin IS, Yoon JS. Association of grip strength with dementia in a Korean older population. Int J Geriatr Psychiatry. 2012;27(5):500–505. [DOI] [PubMed] [Google Scholar]
- 2. Yan JH, Rountree S, Massman P, Doody RS, Li H. Alzheimer’s disease and mild cognitive impairment deteriorate fine movement control. J Psychiatr Res. 2008;42(14):1203–1212. [DOI] [PubMed] [Google Scholar]
- 3. Franssen EH, Souren LE, Torossian CL, Reisberg B. Equilibrium and limb coordination in mild cognitive impairment and mild Alzheimer’s disease. J Am Geriatr Soc. 1999;47(4):463–469. [DOI] [PubMed] [Google Scholar]
- 4. Beauchet O, Annweiler C, Callisaya ML, et al. Poor gait performance and prediction of dementia: results from a meta-analysis. J Am Med Dir Assoc. 2016;17(6):482–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kluger A, Gianutsos JG, Golomb J, et al. Patterns of motor impairment in normal aging, mild cognitive decline, and early Alzheimer’s disease. J Gerontol B Psychol Sci Soc Sci. 1997;52B(1):P28–P39. [DOI] [PubMed] [Google Scholar]
- 6. Kueper JK, Speechley M, Lingum NR, Montero-Odasso M. Motor function and incident dementia: a systematic review and meta-analysis. Age Ageing. 2017:46(5):729–738. [DOI] [PubMed] [Google Scholar]
- 7. Alzheimer’s Association. 2016. Alzheimer’s disease facts and figures. Alzheimers Dement. 2016;12(4):459–509. [DOI] [PubMed] [Google Scholar]
- 8. Souren LE, Franssen EH, Reisberg B. Neuromotor changes in Alzheimer’s disease: implications for patient care. J Geriatr Psychiatry Neurol. 1997;10(3):93–98. [DOI] [PubMed] [Google Scholar]
- 9. Middelveld-Jacobs I, Van den Boogerd M. Paratonia, a form of hypertonia in a nursing home population. Nederlands tijdschrift voor Fysiotherapie. 1986;96:85–87. [Google Scholar]
- 10. Hobbelen JS, Koopmans RT, Verhey FR, Van Peppen RP, de Bie RA. Paratonia: a Delphi procedure for consensus definition. J Geriatr Phys Ther. 2006;29(2):50–56. [PubMed] [Google Scholar]
- 11. Franssen EH, Kluger A, Torossian CL, Reisberg B. The neurologic syndrome of severe Alzheimer’s disease. Relationship to functional decline. Arch Neurol. 1993;50(10):1029–1039. [DOI] [PubMed] [Google Scholar]
- 12. Risse SC, Lampe TH, Bird TD, et al. Myoclonus, seizures, and paratonia in Alzheimer disease. Alzheimer Dis Assoc Disord. 1990;4(4):217–225. [DOI] [PubMed] [Google Scholar]
- 13. Hobbelen JS, Tan FE, Verhey FR, Koopmans RT, de Bie RA. Prevalence, incidence and risk factors of paratonia in patients with dementia: a one-year follow-up study. Int Psychogeriatr. 2011;23(7):1051–1060. [DOI] [PubMed] [Google Scholar]
- 14. Vahia I, Cohen CI, Prehogan A, Memon Z. Prevalence and impact of paratonia in Alzheimer disease in a multiracial sample. Am J Geriatr Psychiatry. 2007;15(4):351–353. [DOI] [PubMed] [Google Scholar]
- 15. Souren LE, Franssen EH, Reisberg B. Contractures and loss of function in patients with Alzheimer’s disease. J Am Geriatr Soc. 1995;43(6):650–655. [DOI] [PubMed] [Google Scholar]
- 16. Beversdorf DQ, Heilman KM. Facilitory paratonia and frontal lobe functioning. Neurology. 1998;51(4):968–971. [DOI] [PubMed] [Google Scholar]
- 17. Chatterjee A. Feeling frontal dysfunction: facilitory paratonia and the regulation of motor behavior. Neurology. 1998;51(4):937–939. [DOI] [PubMed] [Google Scholar]
- 18. Gladstone DJ, Black SE. The neurological examination in aging, dementia and cerebrovascular disease. Part 2: motor examination. Geriatr Ageing. 2002;5(8):44–49. [Google Scholar]
- 19. Branten J. The relationship between resistance to passive movement and muscle tone. Fysiotherapie en Ouderenzorg. 2000;2:9–14. [Google Scholar]
- 20. van Eijle J. Guidebook PDL. Middelharnis: Mobicare; 2008. [Google Scholar]
- 21. Van Dijk GC. Passivities of Daily Living (PDL); Quality of Life Is More than Numbers. Middelharnis: Mobicare; 2008. [Google Scholar]
- 22. Arnts W, Van Oostwaard P, Rooyakkers A. Physiotherapy treatment for paratonia. Nederlands tijdschrift voor Fysiotherapie. 1989;99:216–220. [Google Scholar]
- 23. Fung JK, Tsang HW, Chung RC. A systematic review of the use of aromatherapy in treatment of behavioral problems in dementia. Geriatr Gerontol Int. 2012;12(3):372–382. [DOI] [PubMed] [Google Scholar]
- 24. Merzenich MM, Jenkins WM. Reorganization of cortical representations of the hand following alterations of skin inputs induced by nerve injury, skin island transfers, and experience. J Hand Ther. 1993;6(2):89–104. [DOI] [PubMed] [Google Scholar]
- 25. Lindberg PG, Schmitz C, Engardt M, Forssberg H, Borg J. Use-dependent up- and down-regulation of sensorimotor brain circuits in stroke patients. Neurorehabil Neural Repair. 2007;21(4):315–326. [DOI] [PubMed] [Google Scholar]
- 26. Lissek S, Wilimzig C, Stude P, et al. Immobilization impairs tactile perception and shrinks somatosensory cortical maps. Curr Biol. 2009;19(10):837–842. [DOI] [PubMed] [Google Scholar]
- 27. Gil R, Arroyo-Anllo EM, Ingrand P, et al. Self-consciousness and Alzheimer’s disease. Acta Neurol Scand. 2001;104(5):296–300. [DOI] [PubMed] [Google Scholar]
- 28. Marks R, Quinney HA, Wessel J. Proprioceptive sensibility in women with normal and osteoarthritic knee joints. Clin Rheumatol. 1993;12(2):170–175. [DOI] [PubMed] [Google Scholar]
- 29. Bullock-Saxton JE, Wong WJ, Hogan N. The influence of age on weight-bearing joint reposition sense of the knee. Exp Brain Res. 2001;136(3):400–406. [DOI] [PubMed] [Google Scholar]
- 30. Van de Rakt J. The development of a fetal position in psychogeriatric patients; a hypothesis. Fysiotherapie en ouderenzorg. 1997;juni:2–6. [Google Scholar]
- 31. Hobbelen J, de Bie R, van Rossum E. The effect of passive movement on severity of paratonia: a partially blinded, randomized clinical trial. Nederlands tijdschrift voor Fysiotherapie. 2003;113:132–137. [Google Scholar]
- 32. Hobbelen JH, Tan FE, Verhey FR, Koopmans RT, de Bie RA. Passive movement therapy in severe paratonia: a multicenter randomized clinical trial. Int Psychogeriatr. 2012;24(5):834–844. [DOI] [PubMed] [Google Scholar]
- 33. Prabhu RK, Swaminathan N, Harvey LA. Passive movements for the treatment and prevention of contractures. Cochrane Database Syst Rev. 2013(12):CD009331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Katalinic OM, Harvey LA, Herbert RD. Effectiveness of stretch for the treatment and prevention of contractures in people with neurological conditions: a systematic review. Phys Ther. 2011;91(1):11–24. [DOI] [PubMed] [Google Scholar]
- 35. Brooks SV, Faulkner JA. The magnitude of the initial injury induced by stretches of maximally activated muscle fibres of mice and rats increases in old age. J Physiol. 1996;497(Pt 2):573–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lederman E. Harmonic Technique. London, UK: Harcourt Publishers Limited; 2000. [Google Scholar]
- 37. Heyn P, Abreu BC, Ottenbacher KJ. The effects of exercise training on elderly persons with cognitive impairment and dementia: a meta-analysis. Arch Phys Med Rehabil. 2004;85(10):1694–1704. [DOI] [PubMed] [Google Scholar]
- 38. Venturelli M, Scarsini R, Schena F. Six-month walking program changes cognitive and ADL performance in patients with Alzheimer. Am J Alzheimers Dis Other Demen. 2011;26(5):381–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kemoun G, Thibaud M, Roumagne N, et al. Effects of a physical training programme on cognitive function and walking efficiency in elderly persons with dementia. Dement Geriatr Cogn Disord. 2010;29(2):109–114. [DOI] [PubMed] [Google Scholar]
- 40. Edwards N, Gardiner M, Ritchie DM, Baldwin K, Sands L. Effect of exercise on negative affect in residents in special care units with moderate to severe dementia. Alzheimer Dis Assoc Disord. 2008;22(4):362–368. [DOI] [PubMed] [Google Scholar]
- 41. Blankevoort CG, van Heuvelen MJ, Boersma F, Luning H, de Jong J, Scherder EJ. Review of effects of physical activity on strength, balance, mobility and ADL performance in elderly subjects with dementia. Dement Geriatr Cogn Disord. 2010;30(5):392–402. [DOI] [PubMed] [Google Scholar]
- 42. Scherder EJA. Aging and Dementia. Neuropsychology, Motor Skills, and Pain. Amsterdam: VU University Press; 2011. [Google Scholar]
- 43. Oouchida Y, Sudo T, Inamura T, Tanaka N, Ohki Y, Izumi S. Maladaptive change of body representation in the brain after damage to central or peripheral nervous system. Neurosci Res. 2016;104:38–43. [DOI] [PubMed] [Google Scholar]
- 44. Kristinsdottir EK, Baldursdottir B. Effect of multi-sensory balance training for unsteady elderly people: pilot study of the “Reykjavik model”. Disabil Rehabil. 2014;36(14):1211–1218. [DOI] [PubMed] [Google Scholar]
- 45. Spier BE, Meis M. Maintenance ambulation: its significance and the role of nursing. A walking program not only can benefit frail elders, it also can raise the level of a nurse’s awareness about the ability of a resident to ambulate. Geriatr Nurs. 1994;15(5):277–281. [DOI] [PubMed] [Google Scholar]
- 46. Resnick B. Functional performance and exercise of older adults in long-term care settings. J Gerontol Nurs. 2000;26(3):7–16. [DOI] [PubMed] [Google Scholar]
- 47. Wagner LM, Clevenger C. Contractures in nursing home residents. J Am Med Dir Assoc. 2010;11(2):94–99. [DOI] [PubMed] [Google Scholar]
- 48. Lancioni GE, Cuvo AJ, O’Reilly MF. Snoezelen: an overview of research with people with developmental disabilities and dementia. Disabil Rehabil. 2002;24(4):175–184. [DOI] [PubMed] [Google Scholar]
- 49. Moyle W, Murfield JE, O’Dwyer S, Van Wyk S. The effect of massage on agitated behaviours in older people with dementia: a literature review. J Clin Nurs. 2013;22(5-6):601–610. [DOI] [PubMed] [Google Scholar]
- 50. Viggo Hansen N, Jorgensen T, Ortenblad L. Massage and touch for dementia. Cochrane Database Syst Rev. 2006;(4):CD004989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Nguyen QA, Paton C. The use of aromatherapy to treat behavioural problems in dementia. Int J Geriatr Psychiatry. 2008;23(4):337–346. [DOI] [PubMed] [Google Scholar]
- 52. Strom BS, Ytrehus S, Grov EK. Sensory stimulation for persons with dementia: a review of the literature. J Clin Nurs. 2016;25(13-14):1805–1834. [DOI] [PubMed] [Google Scholar]
- 53. Malara A, De Biase GA, Bettarini F, et al. Pain assessment in elderly with behavioral and psychological symptoms of dementia. J Alzheimers Dis. 2016;50(4):1217–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. van der Steen JT, Sampson EL, Van den Block L, et al. Tools to assess pain or lack of comfort in dementia: a content analysis. J Pain Symptom Manage. 2015;50(5):659–675 e653. [DOI] [PubMed] [Google Scholar]