Abstract
Introduction:
Caregiver intervention studies typically assess whether participants attain general goals (eg, improved mental/physical health) but not their own individual goals. We used goal attainment scaling to evaluate whether participants of a telephone intervention based on cognitive behavioral therapy (CBT) attained their personal goals. We also evaluated treatment compliance and implementation.
Methods:
A sample of 139 family caregivers of people with dementia received 12 telephone sessions over 6 months. Participants personal goals were specified during the first and second sessions. Participants and therapists assessed goal attainment at the end of the intervention.
Results:
Nearly all participants reported meaningful improvements with regard to their personal goals. Specifically, 20.9% exceeded, 56.4% completely attained, and 21.8% partially attained at least one of their personal goals. There was high agreement between self- and therapist ratings. Treatment compliance and implementation were highly satisfactory.
Conclusions:
The CBT telephone intervention successfully helped participants attain their personal goals.
Keywords: goal attainment scaling, treatment compliance, psychotherapy, dementia, family caregivers, evaluation, telephone, cognitive behavioral therapy
Introduction
Interventions based on various strategies (eg, problem solving, cognitive restructuring, family-based interventions, role play, psycho-education) can improve caregivers’ mental and physical health. 1 –8 Using data from a random controlled trial, we recently demonstrated that the Tele.TAnDem intervention based on 12 telephone sessions of cognitive behavioral therapy (CBT) similarly improved participants mental and physical health, as well as their coping abilities. 9,10 While previous evaluations have demonstrated that interventions can effectively help caregivers achieve general goals like improved mental and/or physical health, to date little is known about how effectively interventions can also help caregivers to achieve their own, individual goals. Therefore, we assess the extent to which the Tele.TAnDem intervention helped participants attain their personal goals. As a secondary aim, we also evaluate treatment implementation and compliance.
In psychotherapy research and practice, considering the patient’s ideas about what they want to achieve in therapy is considered essential for planning and evaluation. 11 To date, however, caregiver intervention studies have typically focused on how the intervention affected participants’ mental and physical health according to psychometric scale scores. In fact, with just 1 exception from our group, 12 no other caregiver intervention study has used an individualized, intervention-specific outcome measure specifically tailored to the different challenges caregivers encounter in their daily lives. 5,13 While psychometric scale scores for general quality of life, depressive symptoms, or somatic complaints are certainly relevant outcome measures, they are unlikely to capture participants’ progress on what they themselves see as their most pressing problems. Furthermore, widely used clinical screening instruments may not be sensitive enough to measure small changes in nonclinical samples. 14,15 Thus, comprehensively evaluating an intervention necessitates the use of other, more individualized measures that are also appropriate for nonclinical samples.
To improve on previous caregiver interventions, the Tele.TAnDem intervention used the goal attainment scaling (GAS) method to assess participants’ progress on their own, most personally relevant problems. 16 With GAS, therapists and caregivers work together to specify caregivers’ own personal goals at the beginning of the intervention. Progress on each of these self-defined goals is then assessed at the end of the intervention. One advantage of GAS is that it involves family caregivers in the goal-setting process, which means that the success of an intervention can be evaluated with regard to the caregivers’ own goals. 17 In the words of Bouwens et al, 18 the involvement of the clients in GAS can be seen as a “safeguard for the clinical relevance of this outcome measure.”
Furthermore, because it is more flexible than standardized measures and can track progress across multiple goals, GAS is appropriate for evaluating interventions for family caregivers who face multiple and diverse problems. Indeed, family caregivers of people with dementia encounter many different challenges and burdensome situations, and they are responsible for assisting care recipients with a wide range of daily activities. 15 Thus, caregivers are likely to have a variety of goals such as better managing the care recipient’s challenging behavior and personality changes, dealing with loss, taking more time for other activities (eg, leisure, paid work, children), and constructively dealing with negative emotions like anger, grief, or guilt. Moreover, caregivers are likely to find some goals more important than others. For instance, younger caregivers may face the challenge of coordinating their caregiving duties with their occupation and other family responsibilities, while retired caregivers caring for a spouse having dementia confront problems such as loss of marital life, role change, social isolation, and physical impairments. 19 With GAS, caregivers can specify multiple goals and can select whichever goals are most important for their own unique situation. In the current study, we used GAS to evaluate the extent to which the Tele.TAnDem intervention helped participants attain their personal goals. In our previous trial of a similar but shorter intervention which included just 7 sessions of CBT, 72.3% of caregivers reported improvements concerning at least one of their most personally relevant problems. 12 We expected that the longer Tele.TAnDem intervention with 12 sessions of CBT would successfully help the majority of participants attain their personal goals. Because involving clients in therapeutic decisions and goal setting improves treatment satisfaction, completion rates, clinical outcomes, and compliance, 20,21 we expected that treatment compliance would be high. Based on our previous intervention trial, 8,12 we similarly expected that implementation would be highly feasible.
Methods
Participants and Study Design
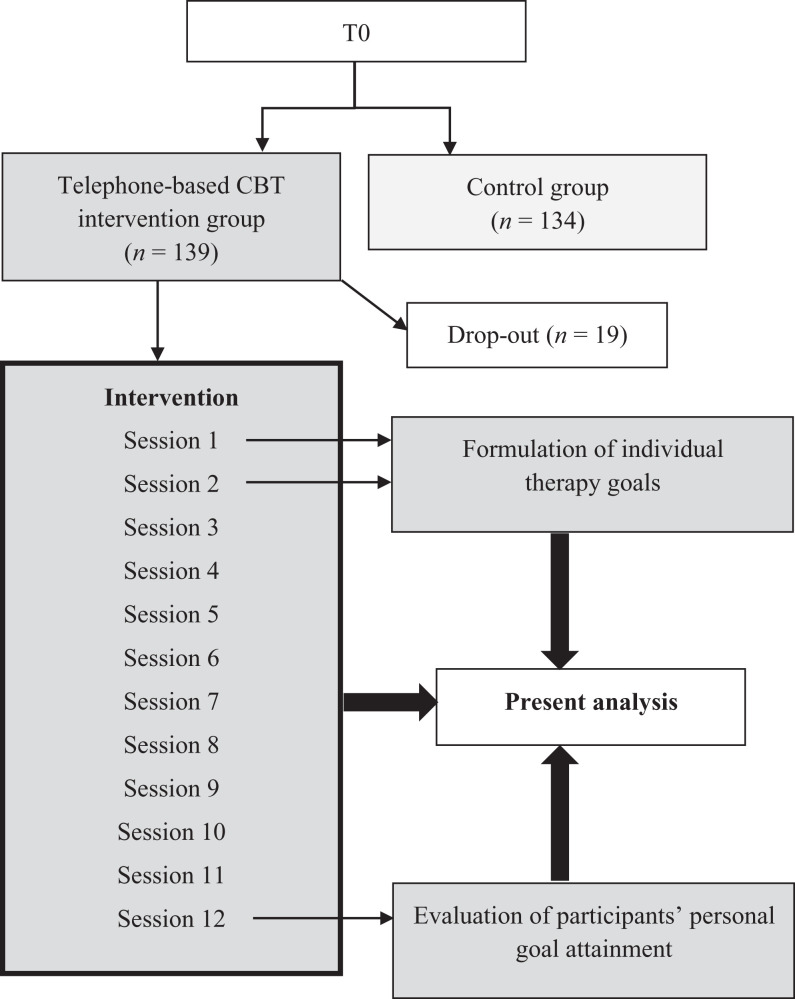
The Tele.TAnDem study was approved by the ethics commission of the Friedrich Schiller University Jena, Germany, and it is registered in the German Clinical Trials Register (DRKS00006355). Participants were recruited mostly via newspapers and magazines from June 2012 to November 2013 (for details, see Wilz et al). 9,10 Only full-time, in-home caregivers of a person diagnosed with dementia could participate. Participants in psychotherapeutic treatment or who had an acute and severe physical illness, cognitive impairment, and/or psychiatric disorder were excluded. Additionally, participants were excluded if the care recipient was institutionalized or if institutionalization was planned within the next 6 months. Of the 273 randomized participants, 139 were allocated to the telephone-based CBT intervention group and 134 to the control group. Only the control group received a compensation for participation of 40 EUR (for details, see the study protocol). 10 The current analyses were conducted within the Tele.TAnDem study as secondary data analyses. The present study focuses exclusively on the intervention group (N = 139), since personal goal attainment, treatment implementation, and treatment compliance could only be assessed for these participants. Figure 1 illustrates the flow model of the study and present analysis.
Figure 1.
Flow model of the study and present analysis.
Intervention
Intervention participants received 12 fifty-minute telephone sessions of CBT over a 6-month period. The intervention concept was based on principles and methods of classical CBT and the third wave of CBT (ie, acceptance and emotion regulation strategies). Details are available in the study protocol, 10 the intervention manual, 22 and in a previously published evaluation. 9 To ensure that the intervention was properly and uniformly delivered, sessions were administered exclusively by experienced CBT therapists who had additionally completed an 8-hour preintervention training. Furthermore, therapists had regular supervision and completed structured documentation sheets for each participant and session. 10 Four independent raters evaluated a random sample of each therapist’s audiotaped sessions (6.0% of all sessions, n = 93) and confirmed the intervention’s therapeutic integrity. 9
Measures
Personal goal attainment
We used GAS 16 to evaluate participants’ personal goal attainment. The steps of GAS are formulating goals, describing goals in observable terms, establishing a hierarchy of goals, and defining potential outcomes. During the first and/or second telephone sessions, the therapist and the caregiver worked together to specify the caregiver’s personal goals for the intervention (see module 2 of the study protocol). 10 As they formulated their goals, participants were encouraged to think of constructive ways that they could ameliorate their particular problems in the medium and long term. Therapists helped participants to specify goals that could realistically be achieved and also evaluated whether proposed goals were appropriate or whether they were too unspecific or unproductive (cf. Berking et al.). 11 Caregivers could define up to 4 personal goals and indicated the personal relevance of each goal. Together, the therapist and the caregiver established criteria for different levels of goal attainment. Finally, the therapist and the caregiver created a written list of the caregiver’s personal goals for the intervention, ranked in order of importance (eg, the first goal was the most important goal of caregiver) along with suggestions of how each goal could be achieved. In the last telephone session, the therapist reviewed the specified personal goals with the caregiver and explained the 5-point scale for goal attainment (described below). To provide an external rating of goal attainment, therapists used the same scale to similarly rate the participant’s progress on each personal goal.
Figure 2 illustrates the scale used to assess personal goal attainment. The scale structure was similar to that of Rockwood et al 23 with the baseline level set to zero, which in our opinion fits best to the caregiving situation and to psychotherapeutic treatment.
Figure 2.
Scale construction: goal attainment scale (GAS).
Treatment compliance and implementation
Therapists used standardized documentation sheets to record session date, session duration, session content, if and why an appointment was changed, if and why a session was interrupted, and intervention and/or study dropout. We used the proportion of participants who completed all 12 sessions and the level of dropout as measures of treatment compliance. We used intervention duration, session duration, the proportion of changed appointments, the proportion of interrupted sessions, and documentation of problems encountered during the GAS process as measures of treatment implementation. We examined whether goal setting was indeed conducted during the first and second sessions to check how well GAS could be implemented in the telephone setting.
Data Analysis
Data were analyzed with SPSS version 21.0 (IBM Corp, Armonk, New York). We examined the descriptive statistics of the compliance and implementation measures. We examined the number of personal goals defined overall and the proportion of participants with 1, 2, 3, and 4 personal goals. We then categorized each goal according to how it was related to the targets of CBT (related to problem-solving, dysfunctional cognitions, emotion regulation, or other themes).
Next, we used Pearson correlation to assess the congruency between caregivers’ and therapists’ ratings. We calculated average personal goal attainment according to the self- and therapist ratings by first calculating the average personal goal attainment for each participant across all of his/her specified goals and then calculating the average goal attainment across all participants. As a global measure of personal goal attainment, we examined each participant’s highest level of personal goal attainment to calculate the proportion of participants who exceeded at least one of their goals, completely attained at least one of their goals, partially attained at least one of their goals, experienced at best no change with regard to their personal goals, and the proportion who reported deterioration on all goals. Finally, we separately examined the frequencies of each level of goal attainment with respect to the caregivers’ most important personal goal, second, third, and fourth most important personal goal.
Results
Sample Description
At baseline, the 139 caregivers in the intervention group had a mean age of 63.91 years (standard deviation [SD] = 11.47, range: 23-85) and were predominantly female (n = 112, 80.6%). Most caregivers were taking care of a spouse (n = 83, 59.7%) or parent with dementia (n = 54, 38.9%). Caregivers had been fulfilling caregiving duties for an average of 4.02 (SD = 3.34, range: 2 months to 19 years) years, and the majority (n = 111, 81.6%) was living with the care recipient. Care recipients had a mean age of 78.55 years (SD = 9.31) and 51.8% (n = 72) were female. The half of the care recipients had been diagnosed with Alzheimer’s disease (n = 67, 48.6%), and the majority was in the moderate (n = 53, 38.4%) or severe (n = 47, 34.1%) stages of dementia (see Wilz et al for all sociodemographic details). 9
Table 1 displays the average physical and mental health of the sample. In comparison to general community samples, the participants reported more burden, more physical complaints, and more symptoms of depression. 9
Table 1.
Baseline Physical and Mental Health of Caregivers Randomized to the Intervention Group (N = 139).
| Characteristics at baseline | M (SD) |
|---|---|
| Age (in years) | 63.91 (11.47) |
| Depressiona | 21.73 (9.66) |
| Quality of lifeb | 50.18 (18.00) |
| Physical symptomsc | 25.73 (14.30) |
| Caregiving burden | 72.70 (19.98) |
| Well-being | 48.88 (23.93) |
| Duration of caregiving (in months) | 48.28 (40.05) |
Treatment Compliance
Most participants (n = 120, 86.3%) completed all 12 CBT sessions (for the flow chart of the whole trial, see Wilz et al). 9 Four (2.9%) caregivers dropped out of the intervention prematurely but continued to participate in the study and delivered data at the second assessment. Another 15 (10.8%) caregivers dropped out of the study altogether.
Treatment Implementation
The intervention lasted on average 5.93 (SD = 0.54, range: 5-8) months. Appointments were rarely rescheduled/postponed, with an average of 2 appointment changes per participant. Reasons for postponements included caregiver and/or therapist illness or another urgent appointment (eg, doctor appointment, family occasion). Almost all (92.9%) of the sessions could be conducted without interruption. Interruptions were associated with demands of the care recipient, other telephone calls, or visits. Sessions lasted for an average of 50.84 (SD = 4.67, range: 20-79) minutes. A small minority of sessions lasted longer than 60 (8.1%) minutes or were shorter than 45 (7.1%) minutes. Reasons for shorter sessions were caregiver illness, other urgent appointments, and needing to care for the care recipient.
Implementation of GAS
Overall, therapists reported few difficulties with the personal goal setting process. For most participants, personal goals could be established during the first or second session (78.7%, 17.6% first session, 61.1% second session); in some cases, personal goals were established during the third session (16.6%) and in few cases in session 4 (4.7%) to 6. A minority of caregivers (n = 12, 8.6%) found it difficult to formulate goals with appropriate attainment scaling. In 6 of these 12 cases, caregivers were unable to specify any concrete goals for therapy and the therapist decided not to perform GAS. In the other 6 cases, the therapist defined 1 or more personal goals for the caregiver (eg, increasing acceptance of role change or emotion regulation). In sum, self-ratings were available for 110 participants and therapist ratings were available for 116 participants.
Caregivers’ Personal Goals
In sum, a total of 253 personal goals were defined. Most participants defined multiple goals (or had multiple goals defined for them). Specifically, 23.6% (n = 26) had 1 goal, 47.3% (n = 52) had 2 goals, 26.4% (n = 29) had 3 goals, and 8.2% (n = 9) had 4 goals. As displayed in Table 2, the most frequently mentioned problems were the care recipient’s challenging behavior and personality changes, social isolation, lack of support, high level of burden/emotional load, as well as neglect of one’s own needs. Most of the problems were related to problem-solving (n = 109, 43.1%), emotion regulation (n = 96, 37.9%), or dysfunctional cognitions (n = 26, 10.3%), with a few related to other themes (n = 22, 8.7%).
Table 2.
Examples of Individual Goals Organized by Theme.
| Goal theme | Example Individual Goals |
|---|---|
| Problem-solving | – Better manage care recipient’s behavioral symptoms (eg, aggressive behavior) – Increase time for own needs and activities – Get more support with caregiving – Learn how to better handle problems in daily life (eg, when the family member with dementia is agitated and shouting) – Learn how to deal with recurring questions from the person with dementia |
| Dysfunctional cognitions | – Reduce the permanent worries that something could happen to my family member with dementia when I am not around – Learn to deal with feelings of guilt when doing pleasant things without my family member with dementia – Enjoy life more and see things in a more positive way – Better manage my guilty conscience when delegating caregiving tasksReduce my own perfectionistic standard of caregiving |
| Emotion regulation | – Better cope with all the changes in my life and increase my acceptance of the disease – Feel calmer when dealing with the care recipient’s behavioral symptoms (eg, distrust or aggression) – Learn how to handle and accept feelings of loss and grief – Talk to someone for emotional relief – Deal with fear about the future and death of my family member with dementia |
Personal Goal Attainment
Self-ratings correlated highly with therapists’ ratings (r = .73, P < .001). On average and across all specified goals, caregivers rated their own personal goal attainment as 1.69 (SD = 0.67) on the 5-point scale (−1 to 3). Similarly, therapists rated caregivers’ personal goal attainment as 1.56 (SD = 0.60).
Nearly all (99.1%) of the caregivers reported improvements with regard to at least one of their most personally relevant problems. More specifically, 20.9% (n = 23) indicated that they exceeded at least one of their goals, 56.4% (n = 62) indicated completely attaining at least one of their goals, and 21.8% (n = 24) indicated partially attaining at least one of their goals, and 0.9% (n = 1) declared that, at best, they experienced no change with respect to their personal goals. No participant indicated deterioration across all goals. Similarly, therapists reported positive changes for all participants, with 14.7% (n = 17) exceeding at least one goal, 55.2% (n = 64) completely attaining at least 1 goal, and 30.1% (n = 35) partially attaining at least 1 goal.
With respect to caregivers’ first, most important goal (n = 109 participant ratings, n =116 therapist ratings), 14.7% (n = 16) of the caregivers indicated exceeding their goal, 49.6% (n = 54) indicated complete goal attainment, 33.9% (n = 37) partial attainment, and 1.8% (n = 2) declared no change. Similarly, according to the therapists, 10.3% (n = 12) of the participants exceeded their most important goal, 44.0% (n = 51) completely attained their goal, 43.1% (n = 50) partially attained their goal, and 2.6% (n = 3) experienced no change.
The results for second to fourth most important goals are summarized in Table 3. With respect to the second most important goal (n = 80 participant ratings, n = 90 therapist ratings), 13.8% (n = 11) of the participants indicated that they exceeded their goal, 43.8% (n = 35) indicated complete goal attainment, and 37.5% (n = 30) indicated partial goal attainment. Three (3.8%) participants indicated no change, and 1 (1.3%) participant indicated deterioration. According to the therapists, 8.9% (n = 8) of the participants exceeded their goal, 43.3% (n = 39) completely attained their goal, and 42.2% (n = 38) partially attained their goal. Therapists indicated that 4.4% (n = 4) experienced no change and that 1 (1.1%) participant experienced deterioration.
Table 3.
Caregivers’ Personal Goal Attainment According to Self- and Therapist Ratings.
| Caregiver Ratings | Therapist Ratings | |
|---|---|---|
| N (%) | N (%) | |
| Second goala | ||
| Exceeding (+3) | 11 (13.8) | 8 (8.9) |
| Completely attained (+2) | 35 (43.8) | 39 (43.3) |
| Partially attained (+1) | 30 (37.5) | 38 (42.2) |
| No change (0) | 3 (3.7) | 4 (4.5) |
| Deterioration (−1) | 1 (1.2) | 1 (1.1) |
| Third goalb | ||
| Exceeding (+3) | 2 (6.1) | 1 (2.6) |
| Completely attained (+2) | 10 (30.3) | 11 (29.0) |
| Partially attained (+1) | 15 (45.4) | 23 (60.5) |
| No change (0) | 6 (18.2) | 3 (7.9) |
| Deterioration (−1) | 0 (0) | 0 (0) |
| Fourth goalc | ||
| Exceeding (+3) | 1 (14.3) | 0 (0) |
| Completely attained (+2) | 1 (14.3) | 1 (11.1) |
| Partially attained (+1) | 4 (57.1) | 7 (77.8) |
| No change (0) | 1 (14.3) | 1 (11.1) |
| Deterioration (−1) | 0 (0) | 0 (0) |
an = 80 participant ratings.
bn = 90 therapist ratings; n = 33 participant ratings; n = 38 therapist ratings.
cn = 7 participant ratings; n = 9 therapist ratings.
With respect to the third most important goal (n = 33 participant ratings, n = 38 therapist ratings), 6.1% (n = 2) of the participants indicated that they exceeded their goal, 30.3% (n = 10) indicated complete goal attainment, and 45.5% (n = 15) indicated partial goal attainment. The remaining 6 (18.2%) participants reported no change. According to therapists, 2.6% (n = 1) exceeded their goal, 28.9% (n = 11) completely attained their goal, 60.5% (n = 23) partially attained their goal, and 7.9% (n = 3) experienced no change.
Finally, with respect to the fourth most important goal (n = 7 participant ratings, n = 9 therapist ratings), 1 participant indicated that he/she exceeded their goal, 1 indicated that he/she completely attained their goal, 4 indicated that they partially attained their goal, and 1 participant indicated no change. According to the therapists, 1 participant completely attained their goal, 7 participants partially attained their goal, and 1 participant experienced no change.
Discussion
An innovation of the current study is that we evaluated how effectively the Tele.TAnDem intervention helped participants attain their own, individual goals. The results confirm that the CBT-based telephone intervention not only led to improvements in participants’ mental and physical health and coping abilities 9 but was also highly successful with regard to helping caregivers achieve their personal goals. Nearly all of the participating caregivers (99.1%) reported meaningful improvements with regard to at least one of their most personally relevant problems. Over half of the caregivers were able to completely attain at least one of their most personally relevant goals, and another one fourth even exceeded at least one of their personal goals. Not a single caregiver indicated overall deterioration, and just 1 participant indicated experiencing at best no change with regard to his/her personal goals. The high agreement between caregivers and therapists is an indication of the reliability of the goal attainment ratings.
As in our previous trial, implementation of the intervention was highly successful. 8,12 The results also indicate that implementing GAS was highly feasible in the telephone setting. In most cases, participants’ individual goals could be specified during the first or second session and, in a few cases, during the following sessions. Therapists had to identify individualized goals for just a small minority of the caregivers. Some of these caregivers were overloaded by stress and were at first unable to conceive of anything that could improve their situation. Other caregivers were solely focused on the care recipient at the beginning of the intervention, and therapists had to first work on helping them to shift their focus toward self-care before setting personal goals became either possible or appropriate.
In addition, treatment compliance was very high as indicated by the low dropout rate and few postponed or disrupted sessions. The high compliance might be due to active telephone calls from the therapists and caregivers’ satisfaction with the intervention. The current results confirm that actively involving the caregiver in intervention decision-making (eg, considering their individual needs) is associated with higher treatment success and compliance. 20,21
Participants tended to define multiple goals which differed greatly from person to person, demonstrating that caregivers face a diversity of problems that also depend on their own individual situation. Almost all of the goals were related to problem-solving, emotion-regulation strategies, or cognitive restructuring, 3 of the main targets of CBT. Thus, CBT represents an appropriate therapeutic approach for working with family caregivers of people with dementia. In a previous trial of a similar but shorter intervention including 7 sessions of CBT, just 72.3% of caregivers reported improvements on at least one of their most personally relevant problems. 12 Comparing the results of the shorter intervention and the Tele.TAnDem intervention with 12 CBT sessions indicates that a sufficient number of sessions and adequate time are needed for the therapeutic process to be most successful. 6,9,27
Given that the majority of caregivers in both the 7- and 12-session telephone-based CBT interventions reported progress with regard to their personal goals, personal goal attainment appears to be an important and highly relevant outcome also for other intervention concepts.
Future research could address some of the limitations of the current study. Because therapists collected the data on participants’ personal goal attainment, participants may have been inclined to evaluate their goal attainment particularly positively. Future follow-up studies which assess participants’ long-term personal goal attainment independently from their therapists would therefore be helpful to corroborate the current findings. Therefore, future trials should also have an independent, blinded interviewer who assess participants’ personal goal attainment.
Another limitation is that we lacked a control group. As personal goal setting necessitates time (in the majority of cases more than 1 session) and therapeutic support, it would be difficult to similarly assess personal goal attainment in a control group of caregivers who do not receive any therapeutic intervention. An untrained interviewer would not, for instance, be able to assess caregivers’ personal goal attainment in a comparable way. Further research is needed to establish other means of measuring personal goal attainment and/or appropriate control conditions.
Furthermore, according to our experience, GAS is inappropriate for assessing progress on certain types of problems. For instance, it may be impossible or even inappropriate to formulate specific goals with regard to acceptance or coping with loss and grief within the first therapy sessions. Future studies could have independent raters analyze the content of the audiotaped sessions or use specific measures (eg, caregiver grief questionnaire) 28 to assess how well the intervention helps participants make progress on problems that are difficult to formulate within the GAS framework. Future studies could also investigate the extent to which participant characteristics (eg, age, relationship with the care recipient, dementia severity) are associated with particular personal goals.
In all, the results suggest that the Tele.TAnDem CBT-based telephone intervention can help family caregivers of people with dementia to achieve important general goals such as improved mental and physical health 9 as well as make progress on their own unique, diverse, and most personally relevant problems. The success of the intervention confirms that the modular intervention concept is a useful tool for addressing caregivers’ diverse and individual needs. Apparently, therapists were able to use the manual to select appropriate therapeutic strategies to address each specific problem. Furthermore, as other recent clinical trials have demonstrated, 8,29,30 telephone interventions fit the special circumstances of family caregivers and support in underserved and rural regions. Thus, telephone-based CBT intervention programs represent an effective and low-threshold alternative to face-to-face interventions for caregivers.
Acknowledgments
The authors acknowledge the support provided by the following individuals: The authors thank Dr. Catherine Bowen for skillfully editing and proofreading the manuscript. Sabine Jansen at the German Alzheimer’s Association and Bianca Broda at the Munich chapter of the German Alzheimer’s Association for their contribution to the study organization and participant recruitment. Kathi Albrecht, Graduate Psychologist, Anna Machmer, MSc, Christina Reiter, MSc, and Tanja Kalytta, Graduate Psychologist, Nils Töpfer, MSc, for their contribution to study organization and data collection. Denise Schinköthe, MSc, and Lisette Weise, MSc, to the study organization and analysis of treatment implementation. Beate Czerwon, Graduate Psychologist, Lydia Franke, Graduate Psychologist, Katharina Grams, Graduate Psychologist, Ruth Haferkamp, Graduate Psychologist, Friederike Huget, Graduate Psychologist, Marie Jüngst, Graduate Psychologist, Franka Möllmann-Hofman, Graduate Psychologist, Silvana Polotzek, Graduate Psychologist, Tamara Thurn, Graduate Psychologist, Michael Wenz, Graduate Psychologist, Katharina Wurm, Graduate Psychologist, Johanna Zimmer, Graduate Psychologist for delivering the intervention. Finally, we wish to thank all family caregivers who participated in the study.
Authors’ Note: German Clinical Trials Register DRKS00006355, URL: http://www.drks.de/DRKS00006355. The funder had no role in in study design and in the collection, analysis, and interpretation of data.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the German Federal Ministry of Health [IIA5-2512FSB555].
References
- 1. Belle SH, Burgio L, Burns R, et al. ; Resources for Enhancing Alzheimer’s Caregiver Health (REACH) II Investigators. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups – a randomized, controlled trial. Ann Intern Med. 2006;145(10):727–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychol Aging. 2007;22(1):37–51. doi:10.1037/0882-7974.22.1.37. [DOI] [PubMed] [Google Scholar]
- 3. Losada A, Márquez-González M, Romero-Moreno R, et al. Cognitive-behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for dementia family caregivers with significant depressive symptoms: results of a randomized clinical trial. J Consult Clin Psychol. 2015;83(4):760–772. doi:10.1037/ccp0000028. [DOI] [PubMed] [Google Scholar]
- 4. Mittelman MS, Haley WE, Clay OJ, Roth DL. Improving caregiver well-being delays nursing home placement of patients with Alzheimer disease. Neurology. 2006;67(9):1592–1599. doi:10.1212/01.wnl.0000242727.81172.91. [DOI] [PubMed] [Google Scholar]
- 5. Schulz R, Martire LM, Klinger JN. Evidence-based caregiver interventions in geriatric psychiatry. Psychiatr Clin North Am. 2005;28(4):1007–1038. doi:10.1016/j.psc.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 6. Selwood A, Johnston K, Katona C, Lyketsos C, Livingston G. Systematic review of the effect of psychological interventions on family caregivers of people with dementia. J Affect Disord. 2007;101(1-3):75–89. doi:10.1016/j.jad.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 7. Wilz G, Meichsner F, Soellner R. Are psychotherapeutic effects on family caregivers of people with dementia sustainable? Two-year long-term effects of a telephone-based cognitive behavioral intervention. Aging Ment Health. 2017;21(7):774–781. doi:10.1080/13607863.2016.1156646. [DOI] [PubMed] [Google Scholar]
- 8. Wilz G, Soellner R. Evaluation of a short-term telephone-based cognitive behavioral intervention for dementia family caregivers. Clin Gerontologist. 2016;39(1):25–47. doi:10.1080/07317115.2015.1101631. [Google Scholar]
- 9. Wilz G, Reder M, Meichsner F, Soellner R. The Tele.TAnDem intervention: telephone CBT for family carers of people with dementia. Gerontologist. 2018;58(2):e118–e129. [DOI] [PubMed] [Google Scholar]
- 10. Soellner R, Reder M, Machmer A, Holle R, Wilz G. The Tele.TAnDem intervention: Study protocol for a psychotherapeutic intervention for family caregivers of people with dementia. BMC Nurs. 2015;14(11):1–6. doi:10.1186/s12912-015-0059-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Berking M, Holtforth MG, Jacobi C, Kröner-Herwig B. Empirically based guidelines for goal-finding procedures in psychotherapy: are some goals easier to attain than others? Psychother Res. 2005;15(3):316–324. doi:10.1080/10503300500091801. [DOI] [PubMed] [Google Scholar]
- 12. Wilz G, Schinköthe D, Soellner R. Goal attainment and treatment compliance in a cognitive-behavioral telephone intervention for family caregivers of persons with dementia. GeroPsych. 2011;24(3):115–125. doi:10.1024/1662-9647/a000043. [Google Scholar]
- 13. Acton GJ, Winter MA. Interventions for family members caring for an elder with dementia. Annu Rev Nurs Res. 2002;20:149–179. [PubMed] [Google Scholar]
- 14. Cooke DD, McNally L, Mulligan KT, Harrison MJG, Newman SP. Psychosocial interventions for caregivers of people with dementia: a systematic review. Aging Ment Health. 2001;5(2):120–135. doi:10.1080/713650019. [DOI] [PubMed] [Google Scholar]
- 15. Schoenmakers B, Buntinx F, DeLepeleire J. Supporting the dementia family caregiver: the effect of home care intervention on general well-being. Aging Ment Health. 2010;14(1):44–56. doi:10.1080/13607860902845533. [DOI] [PubMed] [Google Scholar]
- 16. Kiresuk TJ, Sherman RE. Goal attainment scaling – general method for evaluating comprehensive community mental health programms. Community Ment Health J. 1968;4(6):443–453. doi:10.1007/BF01530764. [DOI] [PubMed] [Google Scholar]
- 17. Stolee P, Awad M, Byrne K, DeForge R, Clements S, Glenny C; Day Hospital Goal Attainment Scaling Interest Group of the Regional Geriatric Programs of Ontario. A multi-site study of the feasibility and clinical utility of Goal Attainment Scaling in geriatric day hospitals. Disabil Rehabil. 2012;34(20):1716–1726. doi:10.3109/09638288.2012.660600. [DOI] [PubMed] [Google Scholar]
- 18. Bouwens SFM, van Heugten CM, Verhey FRJ. Review of goal attainment scaling as a useful outcome measure in psychogeriatric patients with cognitive disorders. Dement Geriatr Cogn Disord. 2008;26(6):528–540. doi:10.1159/000178757. [DOI] [PubMed] [Google Scholar]
- 19. Kurz A, Wilz G. Die Belastung pflegender Angehöriger bei Demenz: Entstehungsbedingungen und Interventionsmöglichkeiten [Dementia caregiver burden: origins and intervention]. Nervenarzt. 2011;82(3):336–342. doi:10.1007/s00115-010-3108-3. [DOI] [PubMed] [Google Scholar]
- 20. Swift JK, Callahan JL. The impact of client treatment preferences on outcome: a meta-analysis. J Clin Psychol. 2009;65(4):368–381. doi:10.1002/jclp.20553. [DOI] [PubMed] [Google Scholar]
- 21. Chee YK, Gitlin LN, Dennis MP, Hauck WW. Predictors of adherence to a skill-building intervention in dementia caregivers. J Gerontol A Biol Sci Med Sci. 2007;62A(6):673–678. doi:10.1093/gerona/62.6.673. [DOI] [PubMed] [Google Scholar]
- 22. Wilz G, Schinköthe D, Kalytta T. Therapeutische Unterstützung für pflegende Angehörige für Menschen mit Demenz. Das Tele.TAnDem Behandlungskonzept [Therapist support for dementia caregivers: The Tele.TAnDem Intervention Program]. Göttingen, Germany: Hogrefe; 2015. [Google Scholar]
- 23. Rockwood K, Graham JE, Fay S. Goal setting and attainment in Alzheimer’s disease patients treated with donepezil. J Neurol Neurosurg Psychiatry. 2002;73(5):500–507. doi:10.1136/jnnp.73.5.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hautzinger M, Bailer M, Hofmeister D, Keller F. Allgemeine Depressions Skala. Manual [German Version of the Center for Epidemiologic Studies Depression Scale. Manual]. Göttingen, Germany: Hogrefe; 2012. [Google Scholar]
- 25. Angermeyer MC, Kilian R, Matschinger H. WHOQOL-100 und WHOQOL- BREF. Handbuch für die deutschsprachigen Versionen der WHO-Instrumente zur internationalen Erfassung von Lebensqualität [WHOQOL-100 and WHOQOL-BREF. Handbook for the German Version of the WHO Instruments for the International Assessment of Quality of Life]. Göttingen, Germany: Hogrefe; 2000. [Google Scholar]
- 26. Brähler E, Hinz E, Scheer JW. GBB-24. Der Gießener Beschwerdebogen. Manual [GBB-The Gießen Body Complaint List. Manual]. Berlin, Germany: Hans Huber; 2008. [Google Scholar]
- 27. Pinquart M, Sörensen S. Helping caregivers of persons with dementia: which interventions work and how large are their effects? Int Psychogeriatr. 2006;18(4):577–595. doi:10.1017/S1041610206003462. [DOI] [PubMed] [Google Scholar]
- 28. Meichsner F, Schinköthe D, Wilz G. The caregiver grief scale: development, exploratory and confirmatory factor analysis, and validation. Clin Gerontologist. 2015;39(4):342–361. doi:10.1080/07317115.2015.1121947. [Google Scholar]
- 29. Tremont G, Davis JD, Papandonatos GD, et al. Psychosocial telephone intervention for dementia caregivers: a randomized, controlled trial. Alzheimers Dement. 2015;11(5):541–548. doi:10.1016/j.jalz.2014.05.1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Steffen AM, Gant JR. A telehealth behavioral coaching intervention for neurocognitive disorder family carers. Int J Geriatr Psychiatry. 2016;31(2):195–203. doi:10.1002/gps.4312. [DOI] [PMC free article] [PubMed] [Google Scholar]