Abstract
The purpose of the project, Centers for Medicare & Medicaid Services (CMS) Innovation study, was to evaluate the impact on 12 quality measures including 10 Minimum Data Set (MDS) publicly reported measures and 2 nursing home process measures using habilitation therapy techniques and a behavior team to manage dementia-related behaviors. A prospective design was used to assess the changes in the measures. A total of 30 Massachusetts nursing homes participated in the project over a 12-month period. Project participation required the creation of an interdisciplinary behavior team, habilitation therapy training, facility visit by the program coordinator, attendance at bimonthly support and sharing calls, and monthly collection of process measure data. Participating facilities showed improvement in 9 of the 12 reported measures. Findings indicate potential quality improvement in having nursing homes learn habilitation therapy techniques and know how to use the interdisciplinary team to manage problem behaviors.
Keywords: habilitation therapy, interdisciplinary behavior team, nursing home, quality measures
Introduction
In August 2013, the Centers for Medicare & Medicaid Services (CMS) awarded the Quality Improvement Organization (QIO) for the state of Massachusetts a 1-year innovation special project to study the use of habilitation therapy in skilled nursing facilities (SNFs). The CMS innovation projects are designed to focus on health-care quality issues by ensuring that Medicare beneficiaries receive better care. The purpose of the awarded projects is to identify the gaps in quality improvement and test promising evidence-based practices that have not made it into mainstream use. The special innovation project aligns with the quality improvement work of the 10th Scope of Work supporting the CMS 3 broad aims:
better health care for individuals,
better health for people and communities, and
affordable care through lowering cost by improvement.
Habilitation therapy, developed by Paul Raia, PhD, from the Alzheimer’s Association of Massachusetts and New Hampshire, is a milieu therapy designed to bring about positive emotions in people with dementia and to maintain those emotions over the course of the day. The amygdala portion of the brain (the emotion center) is the last area to be affected by Alzheimer’s disease (AD) and provides a window of opportunity to communicate with the individual until the later stages of disease. 1 By recognizing the underlying meaning of an individual’s emotions and knowing how to use that knowledge to care for and communicate with the person with dementia, caregivers can effectively manage most problematic behaviors.
The need for specialized knowledge in caring for people with dementia has become evident. According to the 2015 Alzheimer’s Association Facts and Figures, 2 as the American population ages, the rate of people with dementia will escalate. Currently:
5.3 million Americans have AD, of which an estimated 5.1 million people are aged 65 years and older.
Only 45% of people with the disease have been told they have AD.
Two-thirds of Americans with AD are women.
One in 3 seniors who dies have AD or another dementia.
Alzheimer’s disease is the sixth leading cause of death for Americans and is the only disease among the top 10 diseases that cannot be prevented, cured, or even slowed.
According to the Alzheimer’s 2015 Facts and Figures report, it is estimated that by 2025, the number of Americans with dementia will reach 7.1 million. Many of these afflicted individuals will be cared for in nursing homes. Also, it is estimated that by 2015, the costs associated with Alzheimer’s could rise as high as US$1.1 trillion.
The care of individuals with dementia is complicated. The majority of these individuals have concurrent chronic health conditions, and many with AD lose ability to perform activities of daily living and to effectively communicate their needs. According to a 2000 article by Zeisel and Raia: Non-pharmacological treatment for Alzheimer’s Disease: a mind brain approach, published in the American Journal of Alzheimer’s Disease, habilitation therapy is a non-pharmacologic approach to managing difficult behaviors. 6 By learning why and how to maintain positive emotions throughout the day, caregivers are better prepared to manage difficult behaviors and retain the individual’s personal abilities for as long as possible.
Habilitation Therapy
Habilitation therapy is an approach to dementia care that focuses on connecting emotionally with the person who has dementia. In most forms of dementia, the person’s ability to feel, respond, and perceive emotion in others remains relatively intact until the later stages of the disease. 5
Habilitation therapy, a new starscape by Raia, is an approach defined by 6 domains that contribute to the emotional status of the individual. The domains include:
Physical—Reducing the potential for fear and disorientation by directing cognition without the person’s awareness. Everyday activities, like getting dressed, can cause anxiety and confusion. Rather than asking the individual to select an outfit in the closet, the caregiver preselects 2 outfits, provides a comment on why they were selected, and then asks the individual which one he or she would like.
Social—Developing and providing a failure-free and meaningful activity plan keeping in mind the intention of the activity is not on the retention of information, but rather, on the joy of being with peers.
Communication—Including the increase use of body language, gestures, demonstrations, signs, and pictures. Also, never using the word “no” but refocusing and redirecting to help distract the individual from behaviors or requests deemed inappropriate.
Functional—Using body language that matches the caregiver’s message. For example, always using short, simple sentences that breakdown a task into basic steps of little pieces of information and imparted one at a time.
Behavioral—Accepting that the caregiver cannot change the person’s behavior directly but only indirectly by changing either the caregiver’s approach technique or the person’s physical environment.
Perceptual—Involves heightening the person’s sensory experience using hand gestures indicating an action or applying gently pressure, like behind the knees to initiate sitting action, since sensory messages to the brain are not fully captured or no longer recognizable.
Habilitation therapy differs from “rehabilitation” since it does not strive to restore what is lost but focuses on the person’s remaining capabilities and potential over the course of the disease.
Population
The project participants consisted of 30 SNFs in Massachusetts—in urban, suburban, and rural locations. Twenty-three of the facilities were for-profit and 7 were not-for-profit centers. The bed size per participating SNF averaged 130 certified beds; 5 of the SNFs had fewer than 100 beds and 1 SNF had more than 200 beds. During the study period, occupancy rates averaged 92%. Most of the participating homes had dedicated dementia units. However, the existence of a dedicated unit was not a requirement since individuals with dementia are common to all SNF eldercare units.
All individuals involved in the project had a dementia diagnosis. The SNF behavior teams were asked to identify a few residents with the most concerning behaviors as those where habilitation therapy techniques would be used and monitored for effectiveness.
Recruitment
The July 2013 CMS Star report 3 was used to identify possible project participants. The SNFs having an overall 1- or 2-star rating were targeted first.
The Star report is a national quality rating system for each SNF. The rating system features 1 to 5 stars based on SNF performance noted in the State Health Inspections Survey outcomes, staffing levels, and the Minimum Data Set (MDS) Quality Measures (QMs). From the 3 focus areas of the report, 1 overall star rating is determined.
The numbers of SNFs by the overall star rating included in this study were 9 with 5 stars, 8 with 4 stars, 5 with 3 stars, 6 with 2 stars, and 2 with 1 star. The SNFs participating in other QIO-led quality improvement activities were determined not eligible for the project. Since recruitment for the other QIO-led quality improvement activities focused on lower performing SNFs, more of the higher performing SNFs were available to participate in the habilitation therapy program.
Interventions
The technical approach focused on the use of a facility-based behavior team to lead efforts related to problem behaviors. Each SNF agreed to establish an interdisciplinary behavior team that would meet once per week. Team members were asked to commit to a 10-hour habilitation therapy training offered over 2 days. Habilitation therapy training addressed the types of dementia, strategy and technique information for each habilitation therapy domain, function of the interdisciplinary behavior team, behavior care plan development, and the importance of developing a resident-centered activity program. The focus of training was on the individual’s remaining capabilities—not striving to restore what is lost but giving the person a sense of purpose and meaning.
All participants received several tools and resources to assist with care for individuals with dementia and development of behaviorally focused care plans. The tools and resources included training slides, case studies, steps in writing a behavioral plan, information on classifying behaviors, behavior and data collection logs, and a sample framework to memorialize performance improvement efforts related to habilitation therapy. The participants were expected to train other staff, over all shifts, using the tools and resources to implement the interventions in their homes.
The interdisciplinary behavior teams included the administrator and/or director of nursing services, unit nurse(s), activities director, social worker, certified nursing assistant(s), therapist(s), and others as determined by the team and based on patient need. Regular behavior team participation by physicians and/or physician extenders (nurse practitioners or physician assistants) was discouraged to allow teams to focus attention on root causes of behavioral problems with behavior care plans using nonpharmacological approaches. Paul Raia, PhD, was concerned that with physician-led teams, care staff would be reluctant to bring forth tried behavior management strategies and offer possible solutions. As an alternative, SNFs were asked to have physician and physician extenders invited to facility behavior meetings on an as-needed basis. A sample nursing center memo to physicians and physician extenders was offered to SNFs to use in gaining physician support for the project and for managing difficult behaviors by first using a nonpharmacological approach.
The facility-based behavior team was developed as a means of identifying triggers involved in troublesome behaviors and then controlling them. The team was taught how to develop a behavior care plan—a statement of the problem that contains the goal of care, a description of the behavioral problem, and states a working hypothesis as to the cause/triggers of the behavior. The plan also identifies who will be responsible for plan application and oversight and who will implement the intervention on each shift. The team also decides on the duration of the intervention and how often the team needs to meet to evaluate the effectiveness of the care plan interventions and/or consider the relevance of other behavior triggers.
To gather information needed to formulate the care plan, the behavior team developed behavior investigation logs on 1 to 2 individuals with the most problematic behaviors. The log identifies the behavior, like yelling or repeated verbalizations, identifies when the behavior occurred, possible triggers, any care and approach changes made, and outcomes. The behavior team uses the investigation log to reaffirm care plan strategies or to identify needed care plan changes expected as the disease progresses and cognition and abilities decline.
Behavior teams were asked to attend bimonthly phone calls hosted by Paul Raia, PhD, and the QIO. Calls were designed to allow project participants to consult with the expert in solving problem behaviors and learn from each other in ways to implement care processes and approaches.
The QIO staff visited each SNF to assess the behavior team function and design, its ability to apply learned techniques in identifying behaviors and approaches, and development of behavior care plans. A sample performance improvement framework was shared with participants to help them articulate and formally note the workings of the behavior team.
Results
Data used to calculate quality improvement include data on 10 publicly reported QMs from the MDS for all 30 SNFs and self-reported data on 2 process measures from 28 SNFs. Data from 2 SNFs were excluded due to a delay in project start that resulted in incomplete data submitted for evaluation.
For the 10 public reported QMs, data for quarter 2 of 2013 are used as baseline data with data for quarter 2 of 2014 as remeasurement data after the implementation of habilitation therapy techniques.
Table 1 shows performance improvement from baseline to remeasurement for each of the 12 QMs. Participating SNFs improved on 9 of 12 QMs from baseline to remeasurement. The greatest improvements were found in self-reported resident-on-staff physical altercations and the MDS-based QM for urinary tract infection, with improvements of 42.03% and 11.73%, respectively. There is no change for the QM of depression symptoms. Two QMs, physical restraints and resident-on-resident altercations, showed worse outcomes. The physical restraint measure indicates the percentage of long-stay SNF residents who are physically restrained on any day or days during the measurement period. By definition, restraint includes any of the following: trunk restraint used in bed or chair or out of bed, limb restraint used in bed or chair or out of bed, or a chair that prevents rising.
Table 1.
Minimum Data Set Quality Measure and Self-Reported Measures.
| Quarter 2 of 2013 | Quarter 2 of 2014 | Percent Decrease | |
|---|---|---|---|
| Antianxiety–hypnotic (L) | 7.85% | 7.50% | 4.46% |
| Antipsychotic med (L) | 20.82% | 19.04% | 8.55% |
| Antipsychotic med (S) | 2.53% | 2.36% | 6.65% |
| Behavior symptoms affect others (L) | 30.73% | 28.57% | 7.03% |
| Depression symptoms (L) | 3.52% | 3.51% | 0.28% |
| Falls (L) | 39.87% | 39.26% | 1.53% |
| Falls with major injury (L) | 2.95% | 2.75% | 6.78% |
| Increase in ADLs help (L) | 14.67% | 14.48% | 1.30% |
| Physical restraints | 0.90% | 1.09% | −11.00% |
| UTI (L) | 7.93% | 7.00% | 11.73% |
| Self-reported resident-on-resident altercations | 1.21% | 1.23% | −2.03% |
| Self-reported resident-on-staff altercations | 18.63% | 10.80% | 42.03% |
Abbreviations: ADLs, activities of daily living; med, medication; UTI, urinary tract infection; S, short-stay residents; L, long-stay residents.
The increase in restraint use from quarter 2 of 2013 (0.90% of residents) to quarter 2 of 2014 (1.09% of residents) can be associated with resident need for more help. In addition, the definitions of restraints were clarified during training, and staff attention to reporting may have become more focused. However, the finding of an 11.00% increase in restraint use, while suggesting a negative trend, remains below the state QM average of 1.5% resident restraint use and national QM average of 1.2%. 4
For the 2 self-reported QMs, data were collected from each participating SNF monthly. Results were reported as incidents of resident population of the home. Quarterly results were then averaged for all participating SNFs.
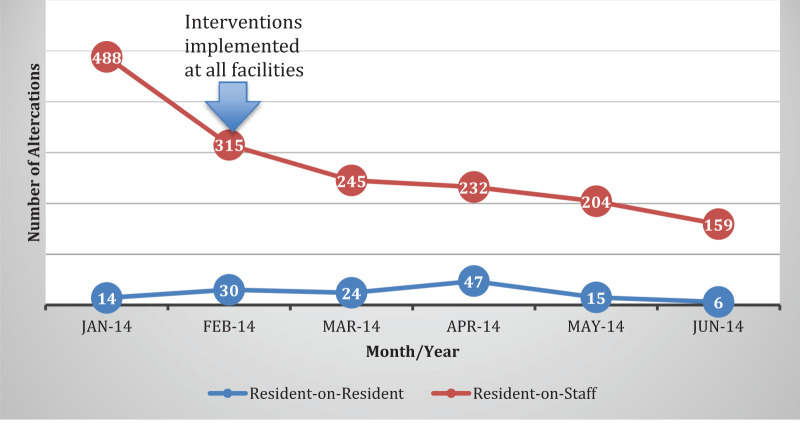
Figure 1 shows the decreasing number of resident-on-staff physical altercation and resident-on-resident physical altercations reported by participating SNFs over the 6-month period following habilitation therapy staff training and process implementation. All SNF training were completed by January 2014. Following training, SNFs were instructed to apply learned techniques. The significant decrease, starting in February 2014 and at least 1 month following training, in the number of resident-on-staff physical altercation is attributed to improved care approaches and behavior management techniques. For example, care staff reported using the technique “spend 5 minutes to save 20 minutes” as an effective approach in establishing a positive relationship with the resident before initiating daily care. “Spend 5 minutes to save 20 minutes” is a technique where the caregiver establishes a positive connection with the resident, perhaps by talking about the individual’s hobby or a cherished personal item, before directing and asking the resident to perform activities like morning care. The approach reduces fear and anxiety associated with not remembering daily routine and caregivers.
Figure 1.
Physical altercations by month.
The number of resident-on-resident physical altercations did not show a significant outcome over the 6-month reporting period. Resident-on-resident physical altercations are not as common as resident-on-staff incidents and were reported as being related to a particular resident, usually a male not liking another male resident. When these incidents occurred, caregivers were instructed to modify the care environment by ensuring that the 2 residents were kept apart and engaged in meaningful activities.
Discussion
This is the first time data were collected systematically from 30 SNFs to assess and evaluate implementation of habilitation therapy under the direction of an interdisciplinary behavior team. With only 6 months of project results, data showed benefits of using a habilitation therapy approach in SNFs. Habilitation therapy provides the rationale behind person-centered dementia care approaches, as well as offering a process for developing an interdisciplinary behavior team, using behavior logs to note and test strategies, and adding and communicating successful strategies to the behavior care plan.
The 30 participating SNFs demonstrated a commitment to improved dementia care. The health-care teams were excited to learn about habilitation therapy and to share how they could improve care and communicate with individuals having dementia. The SNF leaders paid staff to attend the 2 days of training while paying for covering staff at their facilities. Study engagement led to behavior teams being successfully formed, use of behavioral analysis techniques, and development of effective behavior plans. The SNF teams reported meeting regularly to review behaviors and ongoing care plans.
The value of the habilitation therapy model as a heuristic theoretical framework for behavior management is that it is a “hands-on” approach that enables SNF staff to discover and learn independently and in a group. The model offers an approach to address problems using the behavioral team in which decision-making and accountabilities are shared and based on the team’s collective direction.
The main barriers to SNF recruitment and engagement include conflicts with engagement in other quality improvement programs, issues with staff turnover, and changes in facility ownership. Data related to staff turnover and changes in SNF ownership were not captured. Knowing that staffing could not be controlled, staffing ratios within and between SNFs were left random so as to not influence the outcomes. For the participating SNFs, care staff turnover, including the project leader (Director and Assistant Director of Nursing Services or Unit Managers), impacted behavior team leadership and participation. However, the behavior team included 6 to 8 staff members (most of who were involved in the project training), and the interdisciplinary behavior teams affected by leadership turnover were able to continue project participation. Program sustainment during key staff turnover was related to having the program accountability lie with the behavior team, not 1 person.
Considering potential impact from staff turnover and to help refresh learning and to aid in continued habilitation therapy education for existing and new staff, a toolkit was developed and disseminated to the participating SNFs at the conclusion of the project. The toolkit used a competency-based education and training framework to allow staff to focus on 1 or more domains and/or competencies at a time to support self-paced learning. However, the project time line did not allow evaluation of the usefulness and effectiveness of the competency-based education tool.
Having the QIO work with SNF staff in developing a performance improvement plan for habilitation therapy (a component of Quality Assurance and Performance Improvement) to frame the function of the behavior team helped to note team function and accountability.
Implications for Further Research
Project results showed a successful working partnership among the Alzheimer’s Association, CMS, and a QIO contractor. The CMS special innovation project focused on identifying strengths and weaknesses in areas of quality care and interventions that have the potential to improve outcomes. Considering the innovation focus, the project showed promising results.
However, the project was conducted over a short-time span for interventions and monitored with limited data collection. More time is needed to monitor key outcomes, over at least 4 quarters to determine the actual impact without influence of seasonal variations on some QMs. Also, the impact on outcomes and behavior team function from staff turnover and change in SNF ownership needs to be included for monitoring.
Studies related to physician and family education on behavioral management are needed. Physicians need to support the behavioral approach to dementia care by asking SNF staff if they have identified the triggers to a particular behavior before prescribing an antipsychotic drug. Family members can also support the behavioral management approach by learning about the risks associated with antipsychotic drug use and how to visit with their family member with dementia to ensure that positive resident emotions are supported and maintained throughout the course of the day. We recommend that future interventions include physicians and family members on the behavior teams.
Research is needed on the relationship among the use of behavioral approaches for dementia care, falls, use of restraints, hospitalizations, and antipsychotic drug use. A cost feasibility study should also be considered to determine whether cost would be a deterrent or an incentive to the development of a national model.
Conclusion
Habilitation therapy is a promising approach to improving dementia care in SNFs. Individuals with dementia need to be engaged on an emotional level and have positive emotions maintained throughout the course of the day. A facility-based, interdisciplinary behavior team can successfully lead efforts related to problem behavior identification and management and strategy development. Staff, residents, and families as well as physicians will benefit from applied habilitation therapy approaches and techniques and the efforts and direction of the interdisciplinary behavior team.
Footnotes
Authors’ Note: The content of this publication does not necessarily reflect the views or policies of CMS or DHHS.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Centers for Medicare & Medicaid Services (CMS), an agency of the US Department of Health and Human Services (DHHS), under Contract Number HHSM-500-2011-MA, titled “Improving Dementia Care in Skilled Nursing Facilities” in the state of Massachusetts.
References
- 1. Jellinger KA. Neuropathology of Alzheimer’s disease and clinical relevance. In: Alzheimer’s Disease and Related Disorders: Research Advances. Iqbal K, Winblad B, eds. Bucharest: Ana AsIan International Academy on Aging; 2003:153–169. [Google Scholar]
- 2. Alzheimer’s Association, 2015 Alzheimer’s Disease Facts and Figures. Includes a Special Report on Disclosing a Diagnosis of Alzheimer’s Disease. 2015;11(3)322. [Google Scholar]
- 3. Nursing Home Compare Quality Measurement Report; The Official U.S. Government Site for Medicare. Web site. http://www.medicare.gov/nursinghomecompare/profile.html.
- 4. American Health Care Association, Nursing Home Compare Quality Measurement Report October 2014 - Nursing Home Compare Quality Measures by State for Quarter 3 Average October 2013-June 2014 data. Web site. www.ahcancal.org/research_data/quality/Documents.
- 5. Raia P. Habilitation therapy: a new starscape. In: Enhancing the Quality of Life in Advanced Dementia. Volicer L, Bloom-Charette L, eds. Brunner/Mazel Publishing Co; 1999:21–37. [Google Scholar]
- 6. Zeisel J, Raia P. Non-pharmacological treatment for Alzheimer’s disease: a mind brain approach. Am J Alzheimer’s Disease. 2000;15(6):331–340 [Google Scholar]