Abstract
Alzheimer’s disease (AD) and dementia with Lewy bodies (DLB) are the 2 most common neurodegenerative dementias. Identification of patients with DLB is necessary to guide appropriate clinical management and medication trials. Patients with DLB are reported to perform poorly on tasks of visuospatial and executive function, compared to patients with AD who perform poorly on memory tasks. Using the Montreal Cognitive Assessment, we found that patients with DLB (n = 73) had statistically significant lower performance in clock drawing (visuospatial and executive function) and higher performance in delayed recall (memory) subscores compared to patients with AD (n = 57). This score pattern should raise suspicion for a DLB diagnosis at initial evaluation of patients with dementia.
Keywords: dementia with Lewy bodies, cognitive assessment, Alzheimer’s dementia, clock drawing
Introduction
Alzheimer’s disease (AD) and dementia with Lewy bodies (DLB) are the 2 most common neurodegenerative dementias. Many studies have demonstrated difficulty in early differentiation of patients with AD from patients with DLB by clinical criteria. 1 -3 Identification of DLB is critical because the treatment approaches for DLB and AD differ. Many patients with DLB have adverse reactions to antipsychotic agents and may not respond favorably to anticholinergic agents. 2
Over the last several decades, clinical diagnostic criteria for DLB have been refined, thus allowing for greater specificity in diagnosis. 2 Clinical criteria for a DLB diagnosis include “core” features of fluctuating cognition, visual hallucinations which are often incredibly detailed, and motor features of parkinsonism. Also associated with DLB are “suggestive” features which include rapid eye movement sleep behavior disorder, neuroleptic sensitivity, and decreased signal on neuroimaging of dopamine transporter uptake. Using these core and suggestive features, patients can be classified into probable DLB with at least 1 core feature and at least 1 suggestive feature or possible DLB with at least 1 suggestive feature in the setting of dementia without any of the core features. 4 A new diagnostic criteria for DLB has been recently developed after completion of this study.
Despite these improvements, distinguishing patients with AD and DLB remains challenging. A large study utilizing the National Alzheimer’s Coordinating Center Registry found the sensitivity of DLB clinical diagnosis to be 32.1%, though specificity was greater than 95%. 3 This study included patients who were diagnosed both before and after DLB Consortium recommendations. 4
While not a component of the clinical criteria for DLB, numerous studies support distinct cognitive profiles for AD and DLB. Patients with AD are reported to have poor performance on memory tasks, whereas patients with DLB perform poorly on tasks of visuospatial and executive function. 5 Visuospatial or constructional impairment has been noted in 74% of patients with early stage, pathologically confirmed DLB as compared to 45% of patients with AD. 2 These studies were initially based on the use of cognitive domain-specific neuropsychological tests such as the Selective Reminding Test, Rosen Drawing Test, or Digit Span evaluations. These batteries are time-consuming additions to an initial evaluation. Thus, we sought to determine whether the Montreal Cognitive Assessment (MoCA), a commonly administered test during initial evaluation and subsequent monitoring of cognitive impairment, could be used to differentiate AD and DLB on initial assessment.
Methods
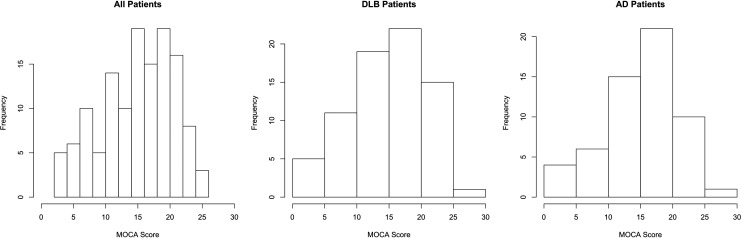
This study was in compliance with the institutional review board of Cleveland Clinic. All patients with an eighth-grade education or above who presented for an initial evaluation at our memory clinic were assessed using the MoCA by a trained nurse. Patients who presented to our clinic from 2012 to 2015 and were diagnosed as probable DLB were included in this study. The AD sample consisted of patients with AD of our clinic, whose information had been entered into a separate database (biorepository) by the start of this study. Patients who were subsequently diagnosed as probable DLB (n = 73) and probable AD (n = 57) were included in the study. The diagnoses of probable DLB and AD were made according to the clinical criteria of the consortium on DLB 4 and the National Institute on Aging–Alzheimer’s Association workgroups on diagnostic guidelines for AD. 6 Demographic information was recorded from the electronic medical records, and disease duration was determined by patient and caregiver report of symptom onset. The MoCA was administered and scored in the original format. Comparisons between disease groups were made using the independent t test. Normal distribution was assumed by the normal distribution of MoCA scores (Figure 1) and sample size of 130. Bonferroni corrections were applied for multiple comparisons, and effect size was also reported.
Figure 1.
Distribution of MoCA scores for all patients, patients with DLB, and patients with AD. AD indicates Alzheimer’s disease; DLB, dementia with Lewy bodies; MoCA, Montreal Cognitive Assessment.
Results
Patients with AD and DLB did not differ in age (71.8 [10] vs 73.3 [7.3] years, respectively) or disease duration (3.1 [1.7] vs 3.6 [2.4] years, respectively) at initial evaluation (Table 1). The majority of patients in both groups were Caucasian (AD 89%, DLB 92%) and not Hispanic (AD 100%, DLB 95%).
Table 1.
Patient Demographics.
| Patient Characteristic | AD (n = 57) | DLB (n = 73) | P Value | ||
|---|---|---|---|---|---|
| Mean or % | SD | Mean or % | SD | ||
| Age at visit, years | 71.8 | 10.0 | 73.3 | 7.3 | .325 |
| Disease duration, years | 3.1 | 1.7 | 3.6 | 2.4 | .185 |
| Female gender | 54 | – | 45 | – | .821 |
| Race | |||||
| Caucasian | 89 | – | 92 | – | .561 |
| African American | 7 | – | 7 | – | 1.000 |
| Asian | 4 | – | 0 | – | .086 |
| Unknown/declined | 0 | – | 1 | – | .451 |
| Ethnicity | |||||
| Not Hispanic | 100 | – | 95 | – | .088 |
| Hispanic | 0 | – | 1 | – | .451 |
| Unknown/declined | 0 | – | 4 | – | .128 |
Abbreviations: AD, Alzheimer’s disease; DLB, dementia with Lewy bodies; SD, standard deviation.
Performance scores on the MoCA and its component parts for both AD and DLB groups are shown in Table 2. The mean total MoCA score showed no difference between AD and DLB (Table 2). In addition, the distributions of total MoCA scores for both groups were similar (Figure 1). The MoCA subscores between the groups were significantly different for the clock drawing test and delayed recall (Figure 1). Patients with DLB scored lower than patients with AD on clock contour (0.84 vs 0.95, P = .037), number placement (0.40 vs 0.68, P < .001), and the overall clock drawing score (1.40 vs 1.91, P < .001). Patients with DLB also scored lower in the hand placement category, but this did not reach significance. In contrast, delayed recall was significantly lower for AD compared to patients with DLB (0.26 vs 1.01, P < .001). All other subscores of the MoCA showed no difference (Table 2).
Table 2.
MoCA Performance.
| Assessment component | AD (n = 57) | DLB (n = 73) | Independent t Test | Post Hoc | |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | P Value | Effect Size | ||
| MoCA total score | 15.56 (5.47) | 15.26 (5.85) | .763 | 0.020 | – |
| Trail | 0.26 (0.44) | 0.16 (0.37) | .181 | 0.129 | – |
| Cube | 0.18 (0.38) | 0.18 (0.39) | .969 | 0.129 | – |
| Clock | 1.91 (0.81) | 1.40 (0.88) | <.001a | 0.580 | AD > DLB |
| Contour | 0.95 (0.23) | 0.84 (0.37) | .037 | 0.330 | AD > DLB |
| Numbers | 0.68 (0.68) | 0.40 (0.49) | <.001a | 0.570 | AD > DLB |
| Hands | 0.28 (0.45) | 0.16 (0.37) | .120 | 0.271 | – |
| Animal naming | 4.70 (0.86) | 2.47 (0.71) | .660 | 0.270 | – |
| Attention | 3.81 (1.92) | 3.59 (1.76) | .507 | 0.094 | – |
| Language | 1.37 (1.14) | 1.42 (0.93) | .763 | 0.052 | – |
| Abstraction | 1.19 (0.83) | 0.95 (0.91) | .109 | 0.252 | – |
| Delayed recall | 0.26 (0.79) | 1.01 (1.27) | <.001a | 0.609 | DLB > AD |
| Orientation | 4.10 (1.80) | 4.11 (1.91) | .864 | 0.030 | – |
Abbreviations: AD, Alzheimer’s disease; DLB, dementia with Lewy bodies; MoCA, Montreal Cognitive Assessment; SD, standard deviation.
aSignificant comparisons (P < .00385) following Bonferroni correction for 13 comparisons.
Comparisons were made between patients with AD and DLB for 13 scored categories, which increases the likelihood of finding significant differences in one of these comparisons by sampling error. A Bonferroni correction was applied, resulting in more stringent criteria (P < .00385) to achieve significance. This did not impact the significance of our results.
Discussion
Despite being the second most common neurodegenerative dementia, DLB achieves relatively little awareness in the medical community. In the past few decades, revisions to the clinical criteria for DLB diagnosis have facilitated recognition. An easy and efficient method of recognizing patients who would benefit from further DLB investigations would facilitate dementia diagnosis and management.
This is, to our knowledge, the first time that an MoCA score pattern has been shown to favor a DLB rather than AD diagnosis at initial evaluation. There was no significant difference in disease duration between groups, suggesting that both were assessed early and at comparable times in the disease course. Our data support that a pattern of low MoCA subscores in the clock drawing test and higher scores in delayed recall are associated with DLB as compared to AD. The clock drawing test and delayed recall assess executive and visuospatial function and memory, respectively. The more pronounced memory deficit seen in the AD group is clinically relevant as short-term memory deficits occur early in AD. In contrast, the DLB cognitive profile has been associated with deficits in executive and visuospatial function, measured on the MoCA by the Trail Making Test, Cube Copy, or clock drawing. 7 Interestingly, clock drawing deficits were greater than other MoCA measures of executive or visuospatial function in patients with DLB.
The clock drawing test was originally used to assess visuospatial function, but it is also a good measure of executive cognitive dysfunction. In 1 study, the clock drawing test alone was shown to differentiate AD from other forms of dementia; however, 3 other studies reported no difference between dementia groups. 8 Variability in these results may in part be due to inconsistent scoring systems and differences in clinical diagnostic accuracy, as only one of these studies utilized autopsy-confirmed diagnoses. 8
The MoCA and Mini-Mental State Examination (MMSE) are commonly used assessment tools, and the MMSE has also been evaluated as a tool to differentiate AD and DLB. 9 Similar to our findings, total MMSE score was not shown to be a valid tool for differentiating these patient groups. 9,10,11 There is no executive function test in the MMSE comparable to clock drawing in the MoCA. However, the pentagon copy test was found to be impaired in DLB. Specifically, the number of pentagon angles, but not the total pentagon copy test score, was significantly different between AD and DLB groups. An erroneous number of angles on this test demonstrated a sensitivity of 41.4% and a specificity of 91% for prodromal DLB. Interestingly, these same patients with DLB showed a significantly lower score than patients with AD on the clock drawing test. 9
Recently, another study compared the cognitive function of patients with DLB and AD. Scharre et al reported greater impairment in executive function in patients with DLB via the Self-administered Gerocognitive Examination and greater impairment in orientation in patients with AD by MMSE. 11 In addition, they reported lower scores in delayed recall by patients with AD via the Consortium to Establish a Registry for Alzheimer’s Disease , though differences in recall as measured by the MMSE were not significant after post hoc analysis. 11 Patients in that study were matched by MMSE score, which strengthens the comparisons made between groups. Using different testing modalities, their results also support the cognitive pattern highlighted in this study.
Studies have also evaluated the predictive value of visual hallucinations, extrapyramidal symptoms, and visuospatial impairment, reporting visual hallucinations and visuospatial impairment to be the best positive and negative predictors of DLB, respectively. 12 Imaging techniques can support a diagnosis of AD or DLB. There is a range of imaging modalities available including magnetic resonance imaging (MRI), functional MRI, positron emission tomography, single-photon emission computed tomography, and dopamine transporter (DAT) imaging. 13 The loss of DATs reliably differentiates DLB from other dementias and is considered a “gold standard” for diagnostic imaging. 13 Although these neuroimaging characteristics are beneficial in aiding antemortem diagnosis, these studies are costly.
This study is limited by its retrospective design. The manner in which data were collected for patients with DLB and AD donors in the biorepository limits the data available to comment on basic patient information including years of education and reduces the generalizability of our findings. Although we included each probable patient with DLB who met the listed criteria, there may be sampling bias in the AD group which was derived from an existing biorepository. The underlying circumstances for the participation of patient with AD in the biorepository are not known. Disease duration was determined by patient and caregiver report, which provides a rough estimate of duration, is a subjective report, and is influenced by recall bias. Differences in disease duration would certainly have an impact on cognitive abilities of both groups and likely be reflected in the MoCA score.
We did not match patients with AD and DLB based on age, gender, disease duration, or educational background. We utilized the information that existed in the database to demonstrate that age and disease duration did not significantly differ between DLB and AD groups. This study uses the MoCA with its original scoring system for all domains.
Diagnoses of probable AD and DLB are based on their respective criteria. Definitive autopsy-proven diagnoses were not obtained, thus we are unable to perform true sensitivity and specificity analyses. Doing so would have allowed us to determine how well this MoCA scoring pattern is able to identify patients with DLB and AD.
Our findings support previous cognitive patterns in DLB and suggest added utility in using the MoCA for initial assessment of cognitive impairment. Clock drawing deficits in the MoCA were greater than other MoCA measures of executive or visuospatial function deficits in patients with DLB. The MoCA score pattern of poor clock drawing and relatively preserved delayed recall as noted in our study recapitulate a DLB cognitive profile. Thus, using the MoCA promotes efficiency during an initial evaluation by drawing attention to patients who may benefit from further neuroimaging studies. This score pattern should raise clinical suspicion for a DLB diagnosis and prompt the assessor for further DLB-specific questioning and evaluation.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was partially funded by the Harold C. Schott Foundation.
References
- 1. McKeith I, Mintzer J, Aarsland D, et al. Dementia with Lewy bodies. Lancet Neurol. 2004;3(1):19–28. [DOI] [PubMed] [Google Scholar]
- 2. Walker Z, Possin KL, Boeve BF, Aarsland D. Lewy body dementias. Lancet. 2015;386(10004):1683–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nelson PT, Jicha GA, Kryscio RJ, et al. Low sensitivity in clinical diagnoses of dementia with Lewy bodies. J Neurol. 2010;257(3):359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McKeith IG, Dickson DW, Lowe J, et al. Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology. 2005;65(12):1863–1872. [DOI] [PubMed] [Google Scholar]
- 5. Yoshizawa H, Vonsattel JPG, Honig LS. Early neuropsychological discriminants for Lewy body disease: an autopsy series. J Neurol Neurosurg Psychiatry. 2013;84(12):1326–1330. [DOI] [PubMed] [Google Scholar]
- 6. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National institute on Aging-Alzheimer’s association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kipps CM, Hodges JR. Cognitive assessment for clinicians. J Neurol Neursurg Psychiatry. 2005;76(supp I):i22–i30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tan LPL, Herrmann N, Mainland BJ, Shulman K. Can clock drawing differentiate Alzheimer’s disease from other dementias?. Int Psychogeriatrics. 2015;27(10):1649–1660. [DOI] [PubMed] [Google Scholar]
- 9. Cagnin A, Bussè C, Jelcic N, Gnoato F, Mitolo M, Caffarra P. High specificity of MMSE pentagon scoring for diagnosis of prodromal dementia with Lewy bodies. Parkinsonism Relat Disord. 2015;21(3):303–305. [DOI] [PubMed] [Google Scholar]
- 10. Mitolo M, Salmon DP, Gardini S, Galasko D, Grossi E, Caffarra P. The new Qualitative Scoring MMSE Pentagon Test (QSPT) as a valid screening tool between autopsy-confirmed dementia with Lewy bodies and Alzheimer’s disease. J Alzheimers Dis. 2014;39(4):823–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Scharre DW, Chang SI, Nagaraja HN, et al. Paired studies comparing clinical profiles of Lewy body dementia with Alzheimer’s and Parkinson’s diseases. J Alzheimers Dis. 2016;54(3):995–1004. [DOI] [PubMed] [Google Scholar]
- 12. Tiraboschi P, Salmon DP, Hansen LA, et al. What best differentiates Lewy body from Alzheimer’s disease in early-stage dementia?. Brain. 2006;129(3):729–735. [DOI] [PubMed] [Google Scholar]
- 13. Mak E, Su L, Williams GB, O’Brien JT. Neuroimaging characteristics of dementia with Lewy bodies. Alzheimers Res Ther. 2014;6(2):18. [DOI] [PMC free article] [PubMed] [Google Scholar]