Abstract
The prevalence of Alzheimer’s disease (AD) is projected to grow dramatically, but efforts to treat its progression have been unsuccessful. Fear of AD among older persons is greater than fear of cancer, and lingering worries about developing AD can be detrimental to well-being. Yet, much remains to be known about such worries and their precursors. This study, based on data from the Health and Retirement Survey, examines correlates of worry. Results of multivariate analyses show the following to be independent and significant correlates: present memory ratings, perceived changes in memory, personal familiarity with AD, belief that being a first-degree relative of someone with AD heightens the chance of developing AD, and age. Interaction analyses show that memory ratings and perceived changes in memory functioning are associated with worry regardless of personal familiarity. These findings will enable practitioners to identify patients and clients at risk of being worried about getting AD.
Keywords: Alzheimer’s disease, memory, fears, concerns, worries
Introduction
Virtually all projections point to a dramatically increasing incidence of cases of Alzheimer’s disease (AD) in the coming decades. More accurate premortem diagnosis will be 1 factor contributing to the growth in numbers. But of equal if not greater consequence in the upward trajectory of AD prevalence is population aging. 1 Age is universally agreed to be the best predictor of someone being diagnosed with AD, so gains in life expectancy occurring throughout the world will inevitably lead to major increases in the incidence and prevalence of AD. In the United States, and in the absence of effective prevention measures, 1 study 2 suggests that the number of persons aged 65 years and older with AD will climb from 4.7 million in 2010 to 13.8 million in 2050. Similarly, the Alzheimer’s Association estimates that the number of Americans with AD in 2014 is over 5 million and that this number may increase to 16 million by 2050. 3
Simultaneously, public awareness of AD has been growing as has recognition of its burdens 4 and its symptoms. The proportion of Americans knowing “a lot” about AD increased from 26% in 2006 to 38% in 2010. 5 A 5-country survey conducted by the Harvard University School of Public Health in collaboration with Alzheimer Europe 6 found that a majority of respondents in all 5 countries—77% in Spain, 73% in Germany and the United States, 72% in France, and 54% in Poland—reported knowing or having known someone with AD. And knowledge of the prominent symptoms of AD was very widespread among persons in the 5-country study. For instance, difficulty remembering things from the day before was seen as a common symptom of AD by 94% of the survey respondents in France, 92% in the United States, 91% in Spain, 87% in Germany, and 80% in Poland.
Coupling growing visibility with the current scientific acknowledgment that AD is inevitably fatal and that there are no behavioral or pharmaceutical agents that can slow down, stop, or reverse the course of the disease’s progression, 7 –9 it is not surprising that AD has emerged as a particularly feared condition. Data from the 5-nation survey 6 show that among persons 60 years of age and older, AD is reported as the disease they most fear getting by 47% of respondents in France, 35% in Spain, 32% in the United States, 30% in Germany, and 20% in Poland. And in 2006, a higher percentage of Americans aged 55 and older indicated that AD was the disease they most feared getting than the percentage who most feared getting cancer (31% vs 27%). 10 Recent survey data from England showed that two-thirds of respondents older than 50 years of age fear they will develop AD as compared with only 10% indicating they feared getting cancer. 11
Growth in prevalence, visibility, and fear all contribute to the phenomenon referred to as “anticipatory dementia” by Cutler and Hodgson 12 and “dementia worries” by Kessler et al. 13 Cognitive lapses (eg, forgetting someone’s name or trying to retrieve a word) prompt concern and worry as persons scrutinize their cognitive functioning for possible clues to an AD future. Research has shown that these concerns permeate the general population but are especially salient among middle age or older adults who have a first-degree relative who has been diagnosed with AD. 14,15 Indeed, 2 recent studies suggest that AD concerns and worries—if held long enough and if they are of sufficient intensity—are associated with diminished psychological well-being and poorer physical health. 16,17
Yet, studies to date on worries about developing AD have been hampered by 2 limitations. First, many have relied on small samples of limited representativeness. Cutler and Hodgson’s work, for instance, is based on a predominantly urban sample from the New England area of the United States with a T1N of 258 and a T3N of 177 eleven years later. Werner’s research, to take another example, is based on a convenience sample of 186 Jewish and Arab adults in Israel with no family history of the illness. 18 Recent research by Zeng et al in China, 19 while based on a sample of 2000, is drawn from just 5 urban areas, areas which ranged in size in 2010 from 2.8 million residents to nearly 29 million residents.
Second, even studies that are based on larger and more representative samples tend either to have a limited number of relevant predictors of worries about getting AD or they disclose inconsistent results. Recent investigations by Cantegreil-Kallen and Pin 20 in France, Wortmann et al 21 in 5 European countries, and Roberts et al 15 in the United States all show that worry is greater among persons who are familiar with someone who has had AD, but none of these studies has examined the important role played by personal assessments of cognitive functioning. 12
It is the twin shortcomings of prior work that the current study addresses. First, earlier work based on limited samples is extended by using data from a nationally representative sample of persons 50 years of age and older. Second, although the present study also examines whether worry is associated with first-hand knowledge of someone who has had AD and with relevant demographic variables, the current research extends the analysis by examining the contributions of cognitive assessments and belief factors about AD as correlates of worries about AD. Specifically, independent variables include assessments of current memory functioning and changes in memory functioning over the past 2 years, level of personal familiarity with persons who have had AD, beliefs about whether having a first-degree relative who has had AD increases one’s own chances of developing the condition, and 4 demographic variables often used in prior studies (marital status, gender, educational attainment, and age). Based on previous research, it is expected that worry about getting AD will be highest among persons:
with the poorest assessments of their memory functioning;
who indicate that their memory has become worse over the previous 2 years;
who have had a first-degree relative with AD; and
who state correctly that having a first-degree relative with AD increases one’s chance of developing AD.
Given conflicting results in prior studies, no a priori hypotheses are offered in regard to the demographic variables For instance, Werner 18 and Zeng et al 19 find nonsignificant (NS) relationships between age and concerns, Cantegriel-Kallen and Pin 20 find personal fear to be significantly higher among persons 65+ than among persons 35 to 64, and Roberts et al 15 find that worry lessens with increasing age among persons 50 and older. To take another example, although the recent work of Werner et al in Israel reports significant gender differences in worry about getting AD, 22 with women expressing greater worry, the study reported by Roberts and colleagues finds gender to be a NS predictor of worry. 15
Methods
Sample
The data used in this study are drawn from Wave 10 of the University of Michigan’s Health and Retirement Survey (HRS). HRS is a representative, ongoing longitudinal panel study of older Americans older than the age of 50. Supported by the National Institute on Aging and the Social Security Administration, HRS has reinterviewed the original sample every 2 years since 1992 and has added new cohorts of the 50+ population at each wave who are also reinterviewed at 2-year intervals. Data are routinely gathered on income and wealth, health and use of health services, employment, family relationships, biomarkers, and genetics. HRS has also served as model for the development of longitudinal surveys in other countries (eg, the Survey of Health, Aging, and Retirement in Europe [SHARE]), enabling comparative research on aging. Topical modules included in the HRS allow investigators to examine sets of specific issues with a random subsample of HRS respondents. Thus, Wave 10 of HRS in 2010 included a brief module on AD, with questions asked of a subsample of 1819 respondents. 23 Distributional characteristics of the subsample used in the analysis are provided in the “Measures” section and in the data presented in Table 1.
Table 1.
ANOVAs and MCAs for the Relationships Between Worries About Getting Alzheimer’s Disease (AD) and Independent Variables.
| Ind Var | Category | Bivariate Effects | Multivariate Effects | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Unadjusted Gross Effects | η | Unadjusted Significance | N | Adjusted Net Effects | β | Adjusted Significance | ||
| Memory rating | Excellent | 108 | 2.14 | 100 | 2.17 | ||||
| Very good | 415 | 2.23 | 397 | 2.25 | |||||
| Good | 682 | 2.47 | 661 | 2.47 | |||||
| Fair | 372 | 2.71 | 354 | 2.74 | |||||
| Poor | 78 | 2.87 | .146 | <.001 | 78 | 2.80 | .141 | <.001 | |
| Memory compared to past 2 years | Better | 43 | 2.16 | 41 | 2.12 | ||||
| Same | 1281 | 2.38 | 1206 | 2.43 | |||||
| Worse | 362 | 2.78 | .122 | <.001 | 343 | 2.65 | .077 | <.025 | |
| Familiarity with AD | Don’t know anyone | 625 | 2.31 | 594 | 2.30 | ||||
| Know someone but not first degree relative | 815 | 2.45 | 787 | 2.47 | |||||
| First degree relative has AD | 215 | 2.93 | .136 | <.001 | 209 | 2.93 | .138 | <.001 | |
| Having first degree relative with AD increases chance | False | 554 | 2.25 | 549 | 2.29 | ||||
| True | 1049 | 2.58 | .115 | <.001 | 1041 | 2.56 | .092 | <.001 | |
| Gender | Male | 726 | 2.38 | 697 | 2.41 | ||||
| Female | 930 | 2.52 | .050 | <.05 | 893 | 2.51 | .036 | NS | |
| Marital status | Married | 994 | 2.47 | 958 | 2.47 | ||||
| Unmarried | 661 | 2.44 | .010 | NS | 632 | 2.48 | .004 | NS | |
| Education | 0-8 years | 139 | 2.58 | 132 | 2.56 | ||||
| 9-11 years | 198 | 2.51 | 191 | 2.53 | |||||
| 12 years | 530 | 2.47 | 515 | 2.48 | |||||
| 13-15 years | 393 | 2.34 | 379 | 2.33 | |||||
| 16 or + years | 386 | 2.51 | .054 | NS | 373 | 2.54 | .058 | NS | |
| Age | 50-59 | 570 | 2.67 | 551 | 2.76 | ||||
| 60-69 | 440 | 2.42 | 421 | 2.40 | |||||
| 70-79 | 423 | 2.36 | 408 | 2.30 | |||||
| 80+ | 223 | 2.22 | .115 | <.001 | 210 | 2.19 | .156 | <.001 | |
| Total model | <.001 | ||||||||
| Multiple R | .288 | ||||||||
| R 2 | .083 | ||||||||
Abbreviations: Ind Var, independent variable; MCA, multiple classification analysis; NS, not significant.
Measures
Worry
The measure of worry about developing AD is based on a single item asking respondents whether they strongly disagree (scored 1), somewhat disagree (2), neither agree nor disagree (3), somewhat agree (4), or strongly agree (5) with the statement “You worry about getting Alzheimer’s someday.”
Memory assessment
In addition, respondents were asked 2 items assessing how they perceived their memory performance. First, they were asked “How would you rate your memory at the present time? Would you say it is excellent (scored 1), very good (2), good (3), fair (4), or (5) poor?” They were also asked “Compared to (the last 2 years/2 years ago), would you say your memory is better now (scored 1), about the same (2), or worse now than it was then (3)?”
Personal familiarity with AD
Respondents were asked “Do you know someone who has had Alzheimer’s disease?” and, if so, “Has your (husband/wife/partner), or a parent, sibling, or adult child of yours been diagnosed with Alzheimer’s?” A composite measure with 3 categories was constructed from the 2 questions: the respondent does not know anyone who has AD (scored 0); the respondent knows someone who has AD but it is not a spouse or partner, nor is it a parent, sibling, or adult child (1); or the respondent has had a spouse or partner, a parent, a sibling, or an adult child with AD (2).
Beliefs
Numerous studies have shown that first-degree relatives of someone with AD have a higher probability of having AD themselves. 24,25 Yet, worry may be conditioned upon whether persons believe this to be true or not. Hence, the analysis includes a variable measuring whether respondents answered true (scored 1) or false (0) to the statement “Having a parent or sibling with Alzheimer’s disease increases the chance of developing it.”
Demographics and Sample Characteristics
Marital status has been dichotomized into those Rs who are married (scored 1; 60.0%) and those who are unmarried (2; 40.0%). On gender, males are scored 1 (43.8%) and females 2 (56.2%). Educational attainment is measured by the number of years in school, recoded to 0 to 8 years (scored 0; 8.4%), 9 to 11 years (1;12.0%), 12 years (2; 32.2%), 13 to 15 years (3; 23.9%), and 16 years or more (4; 23.6%). Respondents range in age from 50 to 99, and ages have been recoded into 50 to 59 (scored 5; 34.4%), 60 to 69 (6; 26.6%), 70 to 79 (7; 25.5%), and 80 years of age and older (8; 13.5%).
Analysis
Given the different measurement levels of the independent variables, analysis of variance (ANOVA) and multiple classification analysis (MCA) have been selected as the preferred analytic techniques. The ANOVA and MCA can be used in combination to examine bivariate and multivariate effects. At the bivariate level, ANOVA produces unadjusted “gross” mean scores on a dependent variable for each category of an independent variable. At the multivariate level, MCA produces “net” mean scores for each category of an independent variable, adjusted for the effects of the remaining independent variables. ηs at the bivariate level and βs at the multivariate level are given to assess the strength of unadjusted and adjusted relationships, a multiple R and R 2 provide information about the overall fit of the multivariate model, and F tests are produced to assess the statistical significance of the gross and net effects of each independent variable as well as the significance of the model as a whole. Although the principal focus will be on the main unadjusted and adjusted effects of the independent variables, the results of MCA analyses of selected interaction effects will also be presented. Analyses were run using SPSS, V. 19, with pairwise deletion of missing cases at the bivariate level and listwise deletion at the multivariate level.
Results
Worry
The principal dependent variable—worry about getting AD someday—shows that the majority of Wave 10 HRS respondents were not particularly worried about getting AD. Considering those who strongly (36.2%) or somewhat (21.6%) disagreed that they worried about getting AD someday, more than half of the respondents expressed little or no worry. However, a substantial minority of these respondents did express some level of worry, either agreeing strongly (9.7%) with the statement about being worried or agreeing somewhat (20.5%) that they worried about getting AD someday.
Main Effects
The bivariate results presented in Table 1 show significant effects on worry for the 2 memory assessment variables. Poorer memory ratings or a perception that one’s memory has worsened over the past 2 years are both associated with greater worry about getting AD. Worry is also significantly related to familiarity with AD, with worry being highest among persons who have had a first-degree relative with AD and lowest among those who said they did not know anyone who has had AD. Again at the bivariate level, worry is significantly higher among persons who (correctly) agreed with the statement that the chance of getting AD is greater if a parent or sibling has had AD. Consistent with finding that women are more likely than men to have AD, 26 our data show a significantly (albeit marginally) higher level of worry among women. The effects of both marital status and education are statistically insignificant, while worry shows a significant decrease with increasing age among these respondents, all of whom are 50 years of age and older. Of all of the bivariate correlates, the strongest relationship as indicated by η is between worries about getting AD and memory ratings.
To take into account any suppressor or confounding effects among the independent variables (eg, educational attainment and memory ratings are negatively and significantly related, while there is a significant and positive relationship between current memory ratings and assessments of how one’s memory compares with 2 years earlier), the data in Table 1 present the MCA results for the effects of each independent variable on worry about getting AD after the effects of the remaining independent variables are removed or controlled. As seen in the columns on the right-hand side of Table 1, worry shows a significant increase with declining assessments of memory performance and with a perception that one’s memory performance is worse than it was 2 years ago. Worry about getting AD is significantly higher the closer one is to someone who has had AD. Believing that having had a first-degree relative with AD increases one’s own chance of getting AD continues to be associated with a significantly higher level of worry. The effect of gender becomes NS when other variables are controlled, while the effects of marital status and education remain NS. Finally, the effects of age continue to be significant, with levels of worry being highest among those 50 to 59 years of age and progressively decreasing as age increases. The multivariate model as a whole is clearly significant, with a multiple R of .288 and an R 2 of .083.
The multivariate results do produce changes from the bivariate findings. For example, age now emerges as the strongest predictor of worry (β = .156) with memory rating being the second strongest correlate. How respondents assess their memory compared with 2 years ago continues to exert an independent and significant effect, although the strength of the relationship is somewhat reduced when the multivariate β is compared with the bivariate η. Gender, which was a marginally significant predictor in the bivariate results, is now statistically insignificant.
Interaction Effects
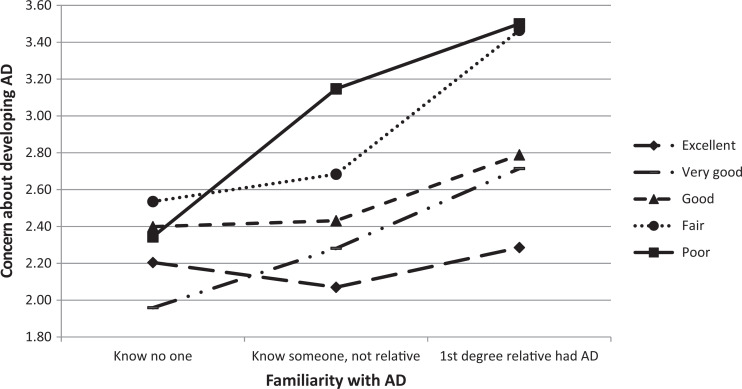
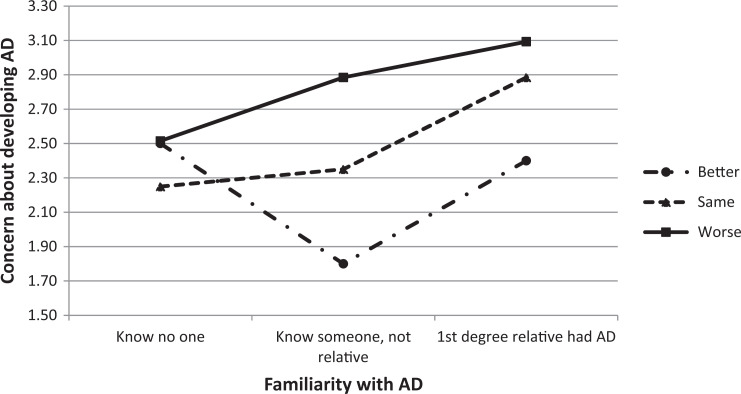
The data in Table 1 appear to indicate that memory rating and personal familiarity with AD have independent and significant effects on worry about developing AD. Likewise, the results imply that change in memory functioning over the past 2 years and personal familiarity also operate independently and significantly. Both of these tentative conclusions have been tested more explicitly and elaborated upon through an examination of interaction effects. The results of these analyses are presented in Figures 1 and 2.
Figure 1.
Worry by familiarity by memory rating.
Figure 2.
Worry by familiarity by change in memory rating.
The data in Figure 1 suggest that having had a first-degree relative with AD is associated with higher levels of worry at all levels of self-assessed memory functioning and that respondents who say that their memory functioning is poor are more worried about getting AD regardless of degree of personal familiarity with AD. That both variables operate independently is also indicated by the NS F test for the 2-way interaction between memory rating and personal familiarity (F = 1.368, df = 8, NS). Likewise, as shown in Figure 2, a perceived decline in memory functioning over the prior 2 years is associated with higher levels of worry regardless of one’s personal familiarity with AD (with the one exception of those who reported improved memory functioning and not knowing anyone with AD). Again, the nonsignificant F test (F = 1.689, df = 4, NS) for the 2-way interaction between personal familiarity with AD and changes in memory functioning points to the independence of these 2 correlates.
Discussion
Along with increasing incidence and prevalence, AD has become more visible, its symptoms increasingly recognized, and its challenges and burdens better understood and acknowledged. 4 At the same time, the promise of cures and treatment has faded in light of the extremely limited efficacy of pharmaceutical agents and behavioral interventions. Although a recent report from Alzheimer’s Disease International 27 does suggest that behavioral interventions may act to lower the risk of dementia, a consensus conference sponsored by the US National Institutes of Health 6 has concluded that neither any medications nor any lifestyle factors has been shown to be at all effective in slowing, stopping, or reversing the course of AD. Perhaps because of this pessimistic assessment, scientific efforts have been increasingly directed at discovering ways of reliably diagnosing AD at its earliest symptomatic and presymptomatic stages.
In view of the above, it is no wonder that the prospect of AD prompts fears and concerns. Among the older population, these dementia worries even eclipse the level of fear evoked by cancer. And there is some evidence that concerns about developing AD—if sufficiently intense, stressful, and held long enough—may prove to be detrimental to physical and psychological well-being and to cognitive functioning. 16,17,28 –30 Recent research has shown that persons reporting subjective memory complaints are at higher risk of developing mild cognitive impairment and dementia. 28 Thus, it is of great importance from both basic and applied perspectives to better understand the nature of the worries that persons have about developing AD and the factors that promote those worries.
Prior work on this topic has been limited by small samples of questionable representativeness. Collectively, these studies do suggest that concerns and worries about developing AD are more likely to be found among persons who perceive their memory functioning as being poorer and among those who have a higher degree of personal familiarity with persons who have had AD. Indeed, smaller scale studies also provide evidence that concerns about AD are associated with memory functioning regardless of level of personal familiarity. Research based on larger and more representative samples tends to confirm the significant effect of the level of personal familiarity on worries about getting AD, but the cumulative contribution of these larger studies is restricted by a limited range of independent variables and inconsistent findings.
The present study has drawn upon data provided by a nationally representative survey of older adults. Evidence is presented to support several conclusions. First, a substantial minority of these respondents—30.2%—indicate that they somewhat or strongly agree with the statement they “worry about getting AD someday.” Second, self-assessments of memory performance play a significantly important role in worries about getting AD. The poorer one’s assessment of one’s memory functioning and perceiving a decline in memory functioning over the previous 2 years are both independently associated with worry. Third, the greater the level of personal familiarity one has with AD, the higher the level of worry. Fourth, the correct belief that having a first-degree relative with AD increases one’s chance of having AD is also associated with a higher level of worry. Fifth, and importantly, memory assessments are associated with worry regardless of degree of personal familiarity with AD. Poorer or declining memory functioning results in higher levels of worry regardless of whether respondents know someone with AD and regardless of who that person is.
Finally, 3 of the 4 demographic variables used in the analyses—marital status, gender, and level of educational attainment—proved to be statistically insignificant predictors of worry at the multivariate level. Age did turn out to be a significant predictor at both the bivariate and the multivariate levels, and in this analysis it proved to be the strongest multivariate predictor of being worried. Of great interest, however, is the fact that the level of worry declined as age increased among this sample of persons aged 50 years and older. Given the well-known epidemiological relationship between age and AD, 31 a reasonable hypothesis would have suggested a positive relationship between age and worry about getting AD. That worry decreases steadily with increasing age perhaps suggests the presence of a threshold beyond which advancing age is accompanied by a sense of relief and a diminished level of worry about getting AD.
Despite the clarity of these findings, 3 limitations should be mentioned. First, in the nature of secondary analysis, this study is constrained by having to rely on limited indicators. In particular, it would have been valuable to be able to draw upon a more textured dependent variable that captures a wider range of dimensions of worries about getting AD. Further psychometric work along these lines is much needed. Second, this study has identified a set of theoretically and statistically meaningful correlates of worries. Yet, less than 10% of the variance in being worried about getting AD has been explained by the variables in the model. Future work should be directed at expanding the topical areas shown to be of importance in this study as well as identifying topics of relevance to worries and concerns that have not been examined in this work. Finally, although HRS is at its core a longitudinal survey of a representative sample of the older population of the United States, some items such as those on AD that were examined in this study have been asked only on a single occasion as part of a topical module. This precludes undertaking any relevant but important analyses of a processual nature. For instance, is a change in memory ratings over an interval of time—a change in the direction of perceiving a decline in memory performance—associated with an increase in worry about getting AD over that interval? Or, does increasing age along with no change in perceived memory functioning result in declining levels of worry?
For these reasons, the final word on this topic has by no means been written by the research reported in this article. But with population aging and with the growing visibility of dementia in general and AD in particular, concerns and worries about one’s cognitive status and functioning are likely to be brought with increasing frequency to the attention of health and human service providers. Those in the helping professions must recognize that these concerns and worries may be deep seated and consequential. 16,17 As Thomas observed many years ago, 32 if persons perceive a situation as real, it is real in its consequences. If people have lingering concerns about their cognitive functioning and real worries about whether AD or dementia is in their future, the consequences can be just as real. Healthcare and human service practitioners would do well, therefore, not to dismiss the cognitive worries and concerns brought to them by their patients and their clients.
Acknowledgment
The author would like to thank Corina Brăgaru for her contributions to this article.
Footnotes
Author’s Note: The data used for this study are available from the University of Michigan at http://hrsonline.isr.umich.edu/ or from the Rand Corporation at http://www.rand.org/labor/aging/dataprod.html.
The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Tejada-Vera B. Mortality from Alzheimer’s disease in the United States: data for 2000 and 2010. NCHS Data Brief. 2013(116):1–8. [PubMed] [Google Scholar]
- 2. Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology. 2013;80 (19):1778–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alzheimer’s Association. 2014 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia. 2014;10 (2):e47–e92. [DOI] [PubMed] [Google Scholar]
- 4. Takizawa C, Thompson PL, van Walsem A, Faure C, Maier WC. Epidemiological and economic burden of Alzheimer’s disease: a systematic literature review of data across Europe and the United States of America. J Alzheimer’s Dis. 2015;43 (4):1271–1284. [DOI] [PubMed] [Google Scholar]
- 5. Metlife Foundation. What America thinks: MetLife Foundation Alzheimer’s survey. https://www.metlife.com/assets/cao/foundation/alzheimers-2011.pdf. Accessed January 15, 2015.
- 6. Harvard School of Public Health/Alzheimer Europe. Five-country Alzheimer’s disease survey. http://www.hsph.harvard.edu/news/press-releases/alzheimers-international-survey/. Accessed January 15, 2015.
- 7. Daviglus ML, Bell CC, Berrettini W, et al. National Institutes of Health State-of-the-Science Conference statement: preventing Alzheimer disease and cognitive decline. Ann Intern Med. 2010;153 (3):176–181. [DOI] [PubMed] [Google Scholar]
- 8. Cummings JL, Morstorf T, Zhong K. Alzheimer’s disease drug-development pipeline: few candidates, frequent failures. Alzheimers Res Ther. 2014;6 (4):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Devanand DP. Whatever happened to new treatments for Alzheimer’s disease? J Clin Psychiatry. 2014;75 (7):775–776. [DOI] [PubMed] [Google Scholar]
- 10. MetLife Foundation. What America thinks: MetLife Foundation Alzheimer’s survey. muskrat.middlebury.edu/Lt/cr/faculty/shalpern-lt/Memory/20538296421147208330V1FAlzheimersSurvey.pdf. Accessed January 15, 2015.
- 11. Why People Fear Dementia More Than They Do Cancer. The Huffington Post UK. http://www.huffingtonpost.co.uk/2014/08/04/dementia-more-feared-than-cancer_n_5646872.html. Accessed January 15, 2015.
- 12. Cutler SJ, Hodgson LG. Anticipatory dementia: a link between memory appraisals and concerns about developing Alzheimer’s disease. Gerontologist. 1996;36 (5):657–664. [DOI] [PubMed] [Google Scholar]
- 13. Kessler E-M, Bowen C, Baer M, Froelich L, Wahl H-W. Dementia worry: a psychological examination of an unexplored phenomenon. Eur J Ageing. 2012;9 (4):275–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cutler SJ, Hodgson LG. Correlates of personal concerns about developing Alzheimer’s disease among middle-aged persons. Am J Alzheimers Dis Other Demen. 2001;16 (6):335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roberts JS, McLaughlin SJ, Connell CM. Public beliefs and knowledge about risk and protective factors for Alzheimer’s disease. Alzheimers Dement. 2014;10 (5 suppl):S381–S389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cutler SJ, Hodgson LG. Concerns about cognitive functioning, dementia worries, and psychological well-being. REVISTA DE ASISTENŢĂ SOCIALĂ (SOCIAL WORK REVIEW). 2013;XI (3):77–86. [Google Scholar]
- 17. Cutler SJ, Hodgson LG. Is health affected by dementia worries and concerns about cognitive functioning? REVISTA DE ASISTENŢĂ SOCIALĂ (SOCIAL WORK REVIEW). 2014;XII(3):7–15. [Google Scholar]
- 18. Werner P. Assessing correlates of concern about developing Alzheimer’s dementia among adults with no family history of the disease. Am J Alzheimers Dis Other Dement. 2002;17 (6):331–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zeng F, Xie WT, Wang YJ, et al. General public perceptions and attitudes toward Alzheimer’s disease from five cities in China. J Alzheimers Dis. 2015;43 (2):511–518. [DOI] [PubMed] [Google Scholar]
- 20. Cantegreil-Kallen I, Pin S. Fear of Alzheimer’s disease in the French population: impact of age and proximity to the disease. Int Psychogeriatr. 2012;24 (1):108–116. [DOI] [PubMed] [Google Scholar]
- 21. Wortmann M, Andrieu S, Mackell J, Knox S. Evolving attitudes to Alzheimer’s disease among the general public and caregivers in Europe: findings from the IMPACT survey. J Nutr Health Aging. 2010;14 (7):531–536. [DOI] [PubMed] [Google Scholar]
- 22. Werner P, Goldberg S, Mandel S, Korczyn AD. Gender differences in lay persons’ beliefs and knowledge about Alzheimer’s disease (AD): a national representative study of Israeli adults. Arch Gerontol Geriatr. 2013;56 (2):400–404. [DOI] [PubMed] [Google Scholar]
- 23. National Institute on Aging NIoH. Growing older in America: the health and retirement study. http://hrsonline.isr.umich.edu/index.php?p=dbook. Accessed January 15, 2015.
- 24. Green RC, Cupples LA, Go R, et al. Risk of dementia among white and African American relatives of patients with Alzheimer disease. JAMA. 2002;287 (3):329–336. [DOI] [PubMed] [Google Scholar]
- 25. Silverman JM, Li G, Zaccario ML, et al. Patterns of risk in first-degree relatives of patients with Alzheimer’s disease. Arch Gen Psychiatry. 1994;51 (7):577–586. [DOI] [PubMed] [Google Scholar]
- 26. Altmann A, Tian L, Henderson VW, Greicius MD. Alzheimer’s disease neuroimaging initiative I. Sex modifies the APOE-related risk of developing Alzheimer disease. Ann Neurol. 2014;75 (4):563–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Alzheimer’s Disease International. World Alzheimer Report 2014: Dementia and Risk Reduction. London: Alzheimer’s Disease International; 2014. [Google Scholar]
- 28. Kryscio RJ, Abner EL, Cooper GE, et al. Self-reported memory complaints: implications from a longitudinal cohort with autopsies. Neurology. 2014;83 (15):1359–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mizoguchi K, Yuzurihara M, Ishige A, Sasaki H, Chui DH, Tabira T. Chronic stress induces impairment of spatial working memory because of prefrontal dopaminergic dysfunction. J Neurosci. 2000;20 (4):1568–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Anderson RM, Birnie AK, Koblesky NK, Romig-Martin SA, Radley JJ. Adrenocortical status predicts the degree of age-related deficits in prefrontal structural plasticity and working memory. J Neurosci. 2014;34 (25):8387–8397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: A systematic review and metaanalysis. Alzheimers Dement. 2013;9(1):63–75.e62. [DOI] [PubMed] [Google Scholar]
- 32. Thomas WI, Thomas DST. The Child in America; Behavior Problems and Programs. New York: A. A. Knopf; 1928. [Google Scholar]