Abstract
The purpose of this study was to assess the effects of multisensory stimulation in a multisensory stimulation environment (MSSE) such as a Snoezelen room versus one-to-one activity sessions with regard to mood, behavior, and biomedical parameters (heart rate and blood oxygen saturation). The MSSE group and activity group (one-to-one activities) of patients with dementia participated in 2 weekly individualized intervention sessions over 16 weeks, where mood and behavior before, during, and after the sessions, and biomedical parameters immediately before and after, were recorded. Immediately after the sessions, patients spoke more spontaneously, related better to others, were more attentive to their environments, more active/alert, less bored/inactive, and more relaxed/content. Both groups exhibited decreases in heart rate and increases in oxygen saturation (Spo 2) values from before to after the sessions. The MSSE sessions in a Snoezelen room were found to be as effective as activity sessions, highlighting the importance of the one-to-one interaction with the therapist.
Keywords: multisensory stimulation, snoezelen, activity, dementia, elderly
Introduction
Institutionalized elderly people with dementia are exposed to either sensory deprivation or excessive sensory stimulation. Both cases favor psychic discomfort and agitated behaviors, 1 hence it is important to optimize the levels of stimulation. 1,2 One of the most suitable interventions for this purpose is Snoezelen, based on multisensory stimulation environment (MSSE), which provides a stress-free, entertaining environment designed both to stimulate or to relax. 3
Snoezelen was developed in the Netherlands in the 1970s and was first introduced to people with learning difficulties. Subsequently, its clinical application was extended to the care of people with dementia. 4 –6 The term Snoezelen is a contraction of 2 Dutch words, the equivalent in English being “sniffing and dozing.” 5 Snoezelen usually occurs in a room specifically designed for that purpose known as Snoezelen room, which includes many objects that pertain to the 5 senses, including fiber-optic cables, water columns, aroma therapy, different music/sounds, tactile objects, and screen projectors, among others. 7 One of the distinguishing elements of the Snoezelen compared to other therapies is the one-to-one attention and the adoption of a nondirective approach, which encourages patients to engage with sensory stimuli of their choice. 8
In a recent review, 9 evidence supported the claim that MSSE in Snoezelen rooms seems to provide immediate positive effects on the mood and behavior of people with dementia. Also, it has also been observed that a more structured approach of multisensory stimulation has effective outcomes in the functional performance of people with dementia. 10,11 However, many of the scientific studies analyzed in that review 9 had several methodological shortcomings, such as a limited number of intervention sessions 12 –14 or the lack of a control group against which to compare the results. 12,15 –17
There is limited evidence demonstrating that MSSE has higher effectiveness than other one-to-one activities that are frequently used in patients with dementia and that have a clear aim and focus, for example, playing cards, looking at photographs, playing games, or doing puzzles. 8,18 It is therefore necessary to develop studies of longer duration, including one-to-one control groups, to distinguish between the potential benefits of multisensory stimulation and those benefits that stem from receiving individualized therapy.
On the other hand, few studies 12,13 include the assessment of biomedical parameters such as heart rate or blood hemoglobin Spo 2. In older people, these vital signs are objective measures of physiological function which are used to monitor acute and chronic disease and thus serve as a basic communication tool for patient status. 19
Therefore, the main objective of the current study was to assess whether MSSE in a Snoezelen room is more effective than one-to-one activity sessions in regard to the mood, behavior, and biomedical parameters of institutionalized elderly individuals with dementia.
Methods
Design
We conducted a controlled longitudinal study in which participants were stratified according to their cognitive and functional status on activities of daily living (ADLs) and were then randomly assigned to 1 of 3 groups (MSSE, activity, and control).
Participants
The sample was selected among the residents of a specialized elderly center in A Coruña (Spain).
The inclusion criterion was a dementia diagnosis (ie, a neurologist’s dementia diagnosis as recorded in the patient’s medical register and corroborated by the psychologist researcher using the Global Deterioration Scale [GDS], 20 which categorized dementia as mild, moderate, or severe—levels 4-7), and the exclusion criterion was the presence of a sensory disorder that would adversely affect interactions with the multisensory stimulation objects.
After a clinical psychologist checked the eligibility of the participants according to the inclusion and exclusion criteria, the sample consisted of 30 participants. A computer-based random number generator was used to randomly divide the sample into 3 groups of 10 participants. 21
The study protocol was approved by the Ethics Committee at the University of A Coruña (Spain). Before beginning data collection, all participants’ proxies were informed about the study. Proxies were used as legally authorized representatives to provide informed consent for the elderly individuals having dementia to participate in the research.
Procedure
The MSSE group participated in multisensory sessions in a Snoezelen room which included various elements stimulating the senses, including fiber-optic cables, water columns, a vibrating water bed, a mirror ball, screen projectors, video, an interactive projecting system, musical selections, aroma therapy equipment, and a tactile board with various textures, among others.
The activity group participated in a series of one-to-one activity sessions, in which intellectual or physical demands were placed on the individual and in which the approach was directive. These participants were asked to take part in activities such as playing cards, quizzes, or viewing photographs. This group was included in the study to differentiate the specific benefits of the multisensory stimulation from those derived from attending one-to-one therapy sessions. 8
The control group did not participate in any of the aforementioned activities being not included in the results analysis; rather, this group continued with the daily routines of the center, including cognitive stimulation group sessions—consisting of themed activities to orientate and actively stimulate cognition (focused on patients with GDS 4-6); training on ADLs—which consists of guided performance providing the minimal required assistance to complete target ADLs (GDS 4-6); education and training of nursing assistants in dementia knowledge; acknowledgment of resident’s experiences; and communication techniques and behavior management (GDS 4-7). The control group was involved in the study to assess the long-term effects of MSSE in a Snoezelen room. 21
The design of the sessions 21 followed by the MSSE and the activity groups was based on the protocol suggested by Baker et al. 22 Nonspecific variables, such as the 1:1 therapist–patient ratio and the number, frequency, and length of sessions, were equivalent for the MSSE and activity groups. All participants from both the groups took part in 2 weekly sessions for 16 weeks. These sessions lasted 30 minutes, unless the participant expressed a desire to leave. Sessions in both the groups followed an internal structure that involved introducing the session, moving through the session, and ending the session. Nevertheless, in the MSSE group, there was flexibility within the standardization, in keeping with the traditional philosophy of multisensory stimulation.
All sessions were conducted by professionals (ie, an occupational therapist or a psychologist) with equivalent education and training in the methodology used. To avoid the creation of positive or negative expectations, the MSSE and the activity sessions were presented to the staff and caregivers as 2 equally valid therapies.
As a result of this design, any differences found between the 2 conditions could be specifically attributed to multisensory stimulation rather than to more general therapeutic effects, such as the one-to-one attention given to the patients.
The difference between the 2 types of intervention was caused by the characteristics that define the MSSE. The MSSE group used multisensory unpatterned stimuli; its therapist followed a nondirective approach, and the therapy required few intellectual or physical demands, thereby being suitable for people with severe or very severe dementia and with limited verbal and psychomotor capabilities. In contrast, during the activity sessions, no intentional special multisensory experiences were introduced, the therapist followed a directive approach, and intellectual and/or physical demands were placed on the individual.
Data on the participants’ sensorial preferences and interests were previously collected to design the content of the sessions and minimize the behavioral problems that some participants could present within the MSSE and the activity contexts. In the MSSE group, sensorial preferences in the Snoezelen room were assessed based on the procedure suggested by Pace et al. 23 Furthermore, relatives of the participants of both groups were interviewed with the aim of identifying the participants’ hobbies, interests, and tastes.
Mood and Behavior
The participants’ mood and behavior were rated before, during, and after the MSSE and activity sessions using the Interact scale. 24 Interact is a rating scale developed specifically for evaluating the effects of MSSE in dementia care. An interrater reliability of r = .99 was found on a small sample. 25 In this study, “Interact during” and “Interact short” scales were used.
Interact during had a total of 22 items measured on a Likert-type scale and was scored according to the frequency of occurrence of each behavior, ranging from 1 (not at all) to 5 (nearly all the time). These data give an indication of the processes that occur within sessions.
Interact short, a 12-item version of Interact, was used to record mood and behavior during the 10 minutes immediately before sessions and the 10 minutes immediately after sessions to measure any observable changes. This gives an indication of the amount of change that each session produces in the short term.
The therapists who administered the sessions rated the participants’ behavior before, during (immediately after finishing the session), and after each session. Therapists received training in the use of the Interact scale, rated the same participants, and discussed discrepancies. In order to avoid behavioral changes due to social desirability effect, Interact short was administered by therapists who work with the participants daily.
Biomedical Parameters
Two biomedical parameters, heart rate (beats per minute) and Spo 2, were recorded immediately before and after sessions in the MSSE and activity groups using mobile finger pulse oximeters (Riester, Germany).
Statistical Analysis
The sample characteristics were summarized as frequencies and percentages for the categorical variables and as the means and standard deviations (SDs) for the continuous variables. Differences in the mood and behavior of patients during the MSSE and activity sessions as measured by ‘nteract during were analyzed using unpaired t-tests.
The immediate effects of the MSSE and activity sessions on patients’ mood and behavior as measured by Interact short were analyzed using paired t-tests to compare the means of scores from before sessions to the means of scores after sessions for each of the 12 outcome measurements. Within each group, an effect size was estimated as the mean change in the score for each variable before and after sessions divided by the SD of the scores.
To determine whether there were any differences in the Interact short scores from before to after a session between the groups, a repeated-measure analysis of variance (ANOVA) was conducted. The within-participants variable was the difference in measurements over time (before versus after), and the between-participants variable was the group (namely, MSSE vs activity).
In addition, a repeated-measure ANOVA was used to determine whether there were any differences between the groups in the number of changes in biomedical parameters (heart rate and Spo 2) from before to after the sessions. The within-participants variable was the measure over time (before and after), and the between-participants variable was the group (MSSE and activity).
In both cases, differences between the groups were tested by a group–time interaction. Statistical significance was set at a P value of less than .05. Statistical analysis was performed using 26 PASW Statistics 18.
Results
Table 1 shows the sociodemographic characteristics of the participants in the MSSE and activity groups at baseline. We found no significant differences between the groups in age, gender, marital status, educational level, and dementia severity. The mean age of the sample was 87.6 years (SD: ±5.7). Women made up 95.0% (n = 19) of the sample; 5.0% (n = 1) were men. With respect to marital status, 80.0% (n = 16) of the participants were widowed and 20.0% (n = 4) were single. Furthermore, 20.0% (n = 4) had no formal education and 25.0% (n = 5) had only primary education.
Table 1.
Characteristics of the Residents With Dementia at Baseline.
| MSSE (n = 10) | Act (n = 10) | Total (n = 20) | |
|---|---|---|---|
| Age, years | |||
| Mean (SD) | 87.2 (6.8) | 87.9 (4.7) | 87.55 (5.7) |
| Minimum–maximum | 77–96 | 79–94 | 77–96 |
| Gender, n (%) | |||
| Female | 10 (100.0) | 9 (90.0) | 19 (95.0) |
| Male | 0 (0.0) | 1 (10.0) | 1 (5.0) |
| Marital status, n (%) | |||
| Single | 3 (30.0) | 1 (10.0) | 4 (20.0) |
| Married or partner | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Widowed | 7 (70.0) | 9 (90.0) | 16 (80.0) |
| Separated or divorced | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Educational level, n (%) | |||
| No formal education | 2 (20.0) | 2 (20.0) | 4 (20.0) |
| Primary | 2 (20.0) | 3 (30.0) | 5 (25.0) |
| Secondary | 6 (60.0) | 3 (30.0) | 9 (45.0) |
| College or higher degree | 0 (0.0) | 2 (20.0) | 2 (10.0) |
| GDS level, n (%) | |||
| GDS 4 | 2 (20.0) | 1 (10.0) | 3 (15.0) |
| GDS 5 | 3 (20.0) | 3 (30.0) | 6 (30.0) |
| GDS 6 | 4 (40.0) | 4 (40.0) | 8 (40.0) |
| GDS 7 | 1 (10.0) | 2 (20.0) | 3 (15.0) |
Abbreviations: GDS, Global Deterioration Scale; MSSE, multisensory stimulation group in a Snoezelen room; Act, activity group; SD, standard deviation.
Effects on Mood and Behavior
Table 2 shows the means and SDs for each group on each item of Interact short and the results of paired t-tests. Significant improvements were observed from before sessions to after sessions in the MSSE group in the following items: more spontaneous speech (P = .006), relating to people better (P = .014), more attentive to/focused on their environment (P = .022), enjoying themselves, more active or alert (P = .004), and more relaxed/content (P = .000). The activity group showed significant improvements from before sessions to after sessions in the following items: more happy/content (P = .012), less confused (P = .043), more spontaneous speech (P = .016), relating to people better (P = .005), more attentive to/focused on their environment (P = .002), enjoying themselves, more active or alert (P = .024), less bored/inactive (P = .002), and more relaxed/content (P = .000).
Table 2.
Means Scores (SDs) for Each Group on Interact Short (Before and After Sessions).a
| Construct | Item | Group | Before | After | P Value | d |
|---|---|---|---|---|---|---|
| Mood | Tearful/sad | MSSE | 1.44 (1.22) | 1.09 (0.14) | 0.341 | 0.40 |
| Activity | 1.10 (0.12) | 1.06 (0.07) | 0.059 | 0.41 | ||
| Happy/content | MSSE | 2.42 (1.35) | 2.35 (1.05) | 0.846 | 0.06 | |
| Activity | 1.84 (0.48) | 2.32 (0.89) | 0.012 | −0.67 | ||
| Fearful/anxious | MSSE | 1.32 (0.62) | 1.09 (0.10) | 0.279 | 0.52 | |
| Activity | 1.19 (0.28) | 1.07 (0.10) | 0.097 | 0.57 | ||
| Confused | MSSE | 1.48 (0.72) | 1.25 (0.22) | 0.237 | 0.43 | |
| Activity | 1.31 (0.31) | 1.22 (0.22) | 0.043 | 0.33 | ||
| Speech | Talked spontaneously | MSSE | 1.70 (0.59) | 2.09 (0.89) | 0.006 | −0.52 |
| Activity | 1.60 (0.60) | 1.84 (0.64) | 0.016 | −0.39 | ||
| Relating to people | Related well | MSSE | 2.50 (0.96) | 2.86 (1.18) | 0.014 | −0.33 |
| Activity | 2.29 (0.64) | 2.76 (0.96) | 0.005 | −0.58 | ||
| Relating to environment | Attentive/focused on environment/objects | MSSE | 2.63 (0.90) | 2.97 (1.00) | 0.022 | −0.36 |
| Activity | 2.35 (0.46) | 3.01 (0.65) | 0.002 | −1.17 | ||
| Need for prompting | Did things from own initiative | MSSE | 1.69 (0.74) | 1.52 (0.42) | 0.338 | 0.28 |
| Activity | 1.48 (0.49) | 1.41 (0.34) | 0.633 | 0.17 | ||
| Stimulation level | Wandering, restless, or aggressive | MSSE | 1.21 (0.32) | 1.17 (0.34) | 0.461 | 0.12 |
| Activity | 1.41 (0.65) | 1.32 (0.61) | 0.212 | 0.14 | ||
| Enjoying self, active, or alert | MSSE | 2.23 (0.93) | 2.79 (1.19) | 0.004 | −0.52 | |
| Activity | 2.02 (0.49) | 2.59 (1.02) | 0.024 | −0.71 | ||
| Bored, inactive, or sleeping inappropriately | MSSE | 2.18 (0.81) | 1.79 (0.54) | 0.097 | 0.57 | |
| Activity | 2.63 (0.76) | 1.83 (0.71) | 0.002 | 1.09 | ||
| Relaxed, content, or sleeping appropriately | MSSE | 2.86 (0.78) | 3.53 (0.61) | 0.000 | −0.96 | |
| Activity | 2.37 (0.66) | 3.21 (0.66) | 0.000 | −1.27 |
Abbreviations: MSSE, multisensory stimulation group in a Snoezelen room; Act, activity group; d, effect size; SD, standard deviation.
a Significant (P value) < .05.
With regard to the repeated-measure ANOVA results, there were no significant differences between the groups from before to after sessions (group–time interactions). There were significant time effects in 6 of the 12 outcome measures: talked spontaneously; related well to others; attentive to/focused on their environment; enjoying self, active/alert; bored/inactive; and relaxed/content.
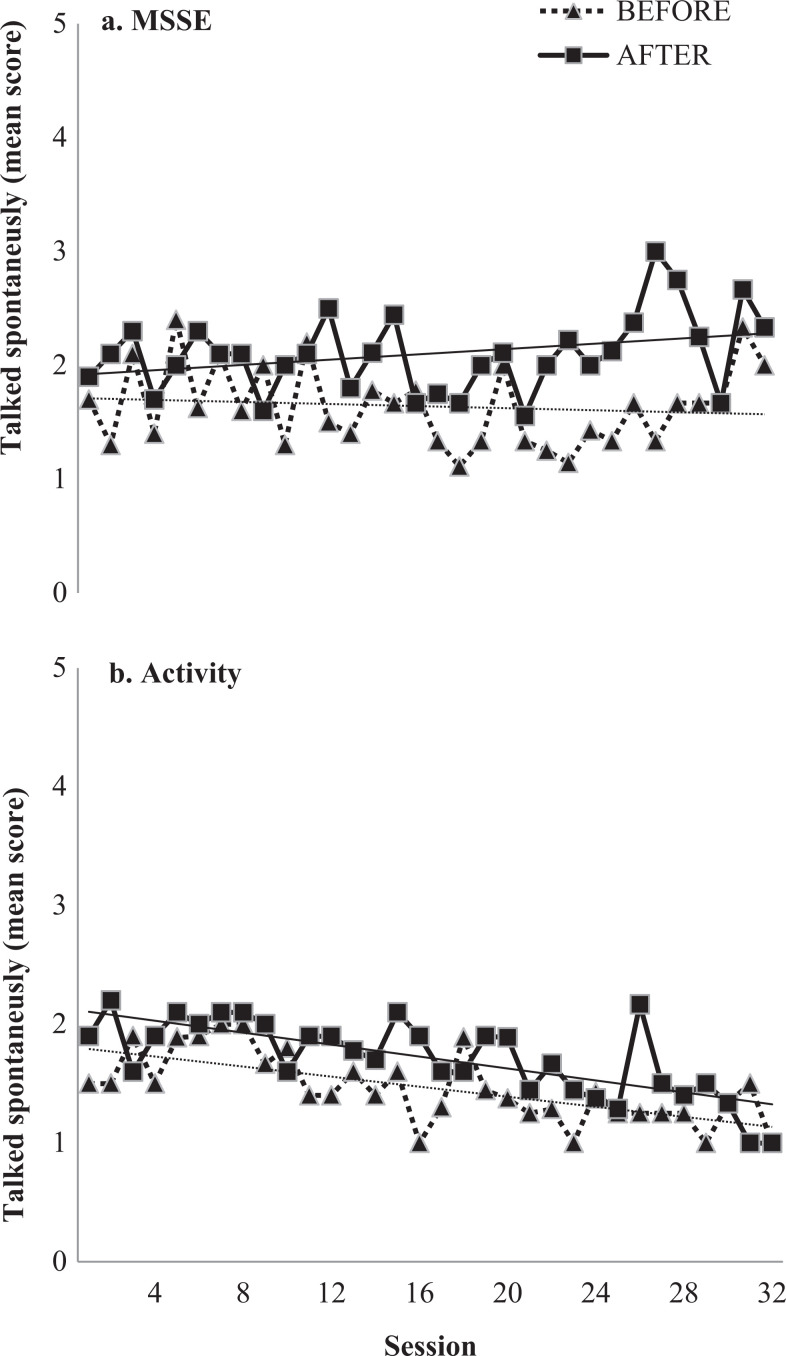
Participants in both the groups talked more spontaneously in the 10 minutes after the sessions compared to the 10 minutes before the sessions (F 1, 18 = 21.184, P < .001). Figure 1 shows the proportion of time in which participants talked spontaneously before and after the sessions across the 32 intervention sessions. It is noteworthy that, in the MSSE group, the before- and after-session differences for this item increased over the course of the study.
Figure 1.
The ability to speak spontaneously. Interact short measurements before and 10 minutes immediately after each session in 2 types of interventions—(A) multisensory stimulation environment (MSSE) in a Snoezelen room and (B) activity—at sessions 0 (baseline) and 32 (posttrial). 1 indicates not at all; 2 = a bit of the time; 3 = some of the time; 4 = most of the time; 5 = nearly all of the time.
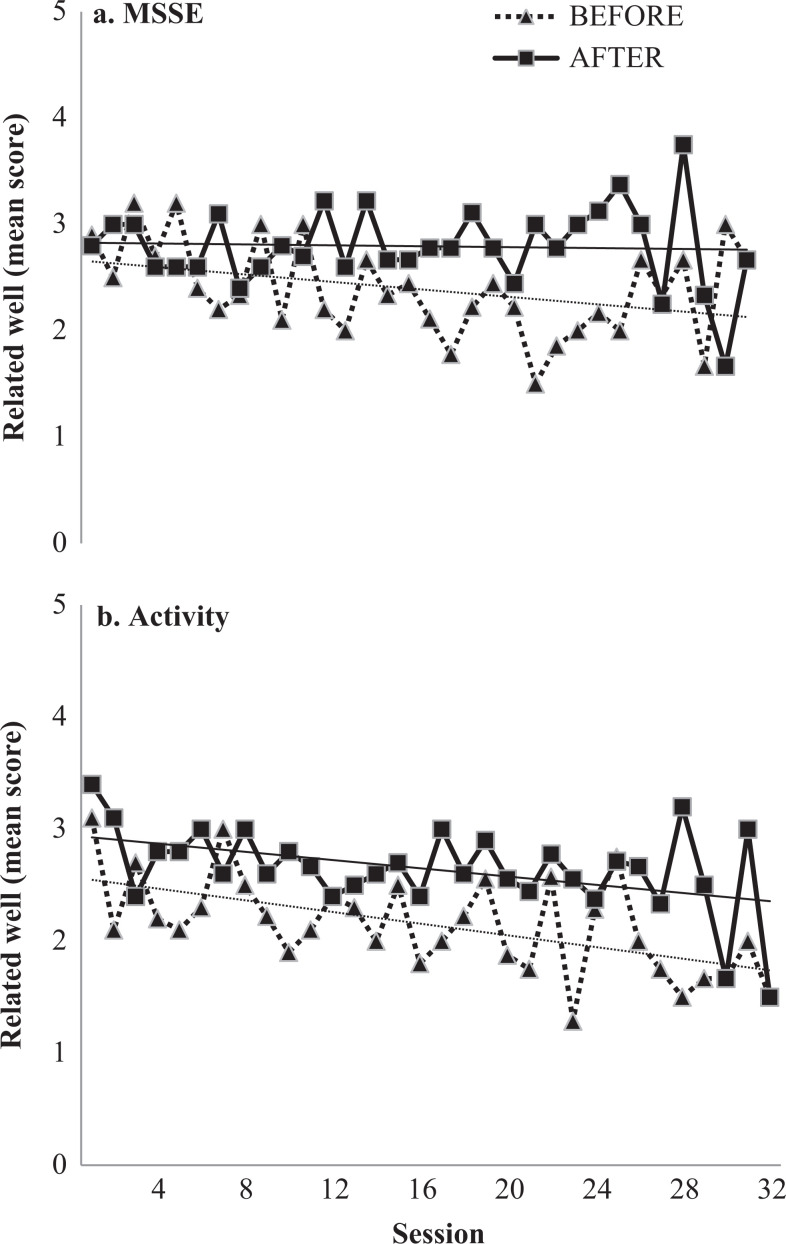
In both the groups, participants related better to others in the 10 minutes after the sessions than 10 minutes before the sessions (F 1, 18 = 22.977 P < .001). In the MSSE group, the before- and after-session differences on this item increased as the study progressed (Figure 2).
Figure 2.
Related well to other staff/patients. Interact short measurements before and 10 minutes immediately after each session in 2 types of interventions—(A) multisensory stimulation environment (MSSE) in a Snoezelen room and (B) activity—at sessions 0 (baseline) and 32 (posttrial). 1 indicates not at all; 2 = a bit of the time, 3 = Some of the time; 4= most of the time; 5 = nearly all of the time.
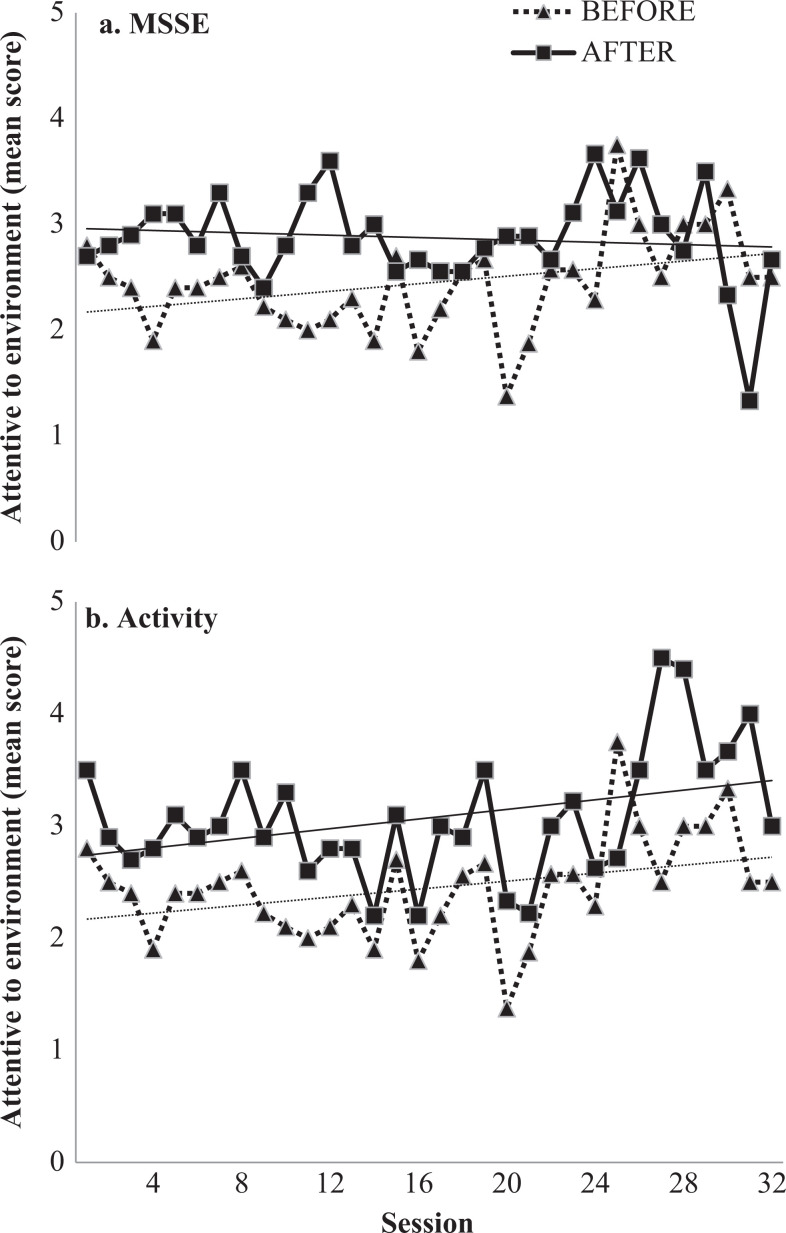
After the sessions, participants of both the groups spent more time attentive to/focused on their environment (F 1, 18 = 25.607, P < .001) compared to the 10 minutes before the sessions. In the activity group, the proportion of time in which the participants were attentive to their environment, both during the 10 minutes before and after the sessions, increased across the course of the study (Figure 3).
Figure 3.
Relating to environment/attentive to environment. Interact short measurements before and 10 minutes immediately after each session in 2 types of intervention—(A) multisensory stimulation environment (MSSE) in a Snoezelen room and (B) activity—at sessions 0 (baseline) and 32 (posttrial). 1 indicates not at all; 2 = a bit of the time; 3 = some of the time; 4 = most of the time; 5 = nearly all of the time.
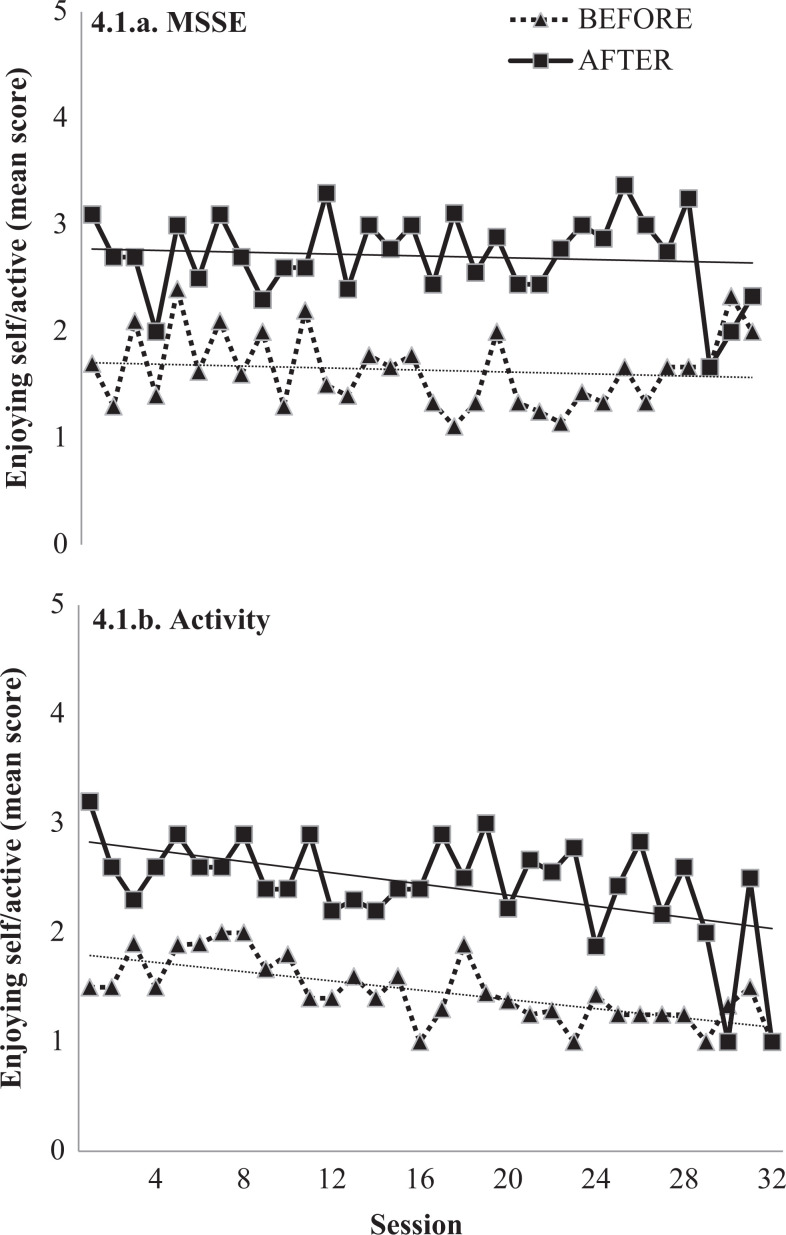
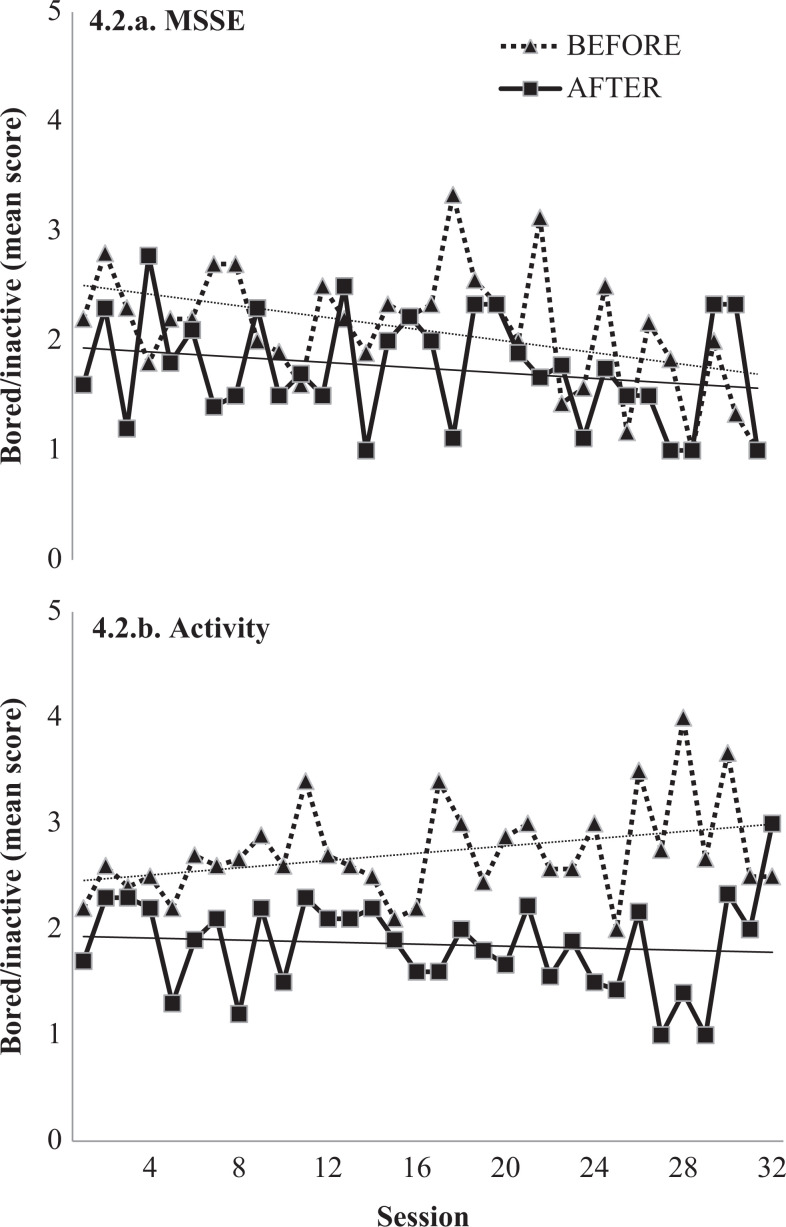
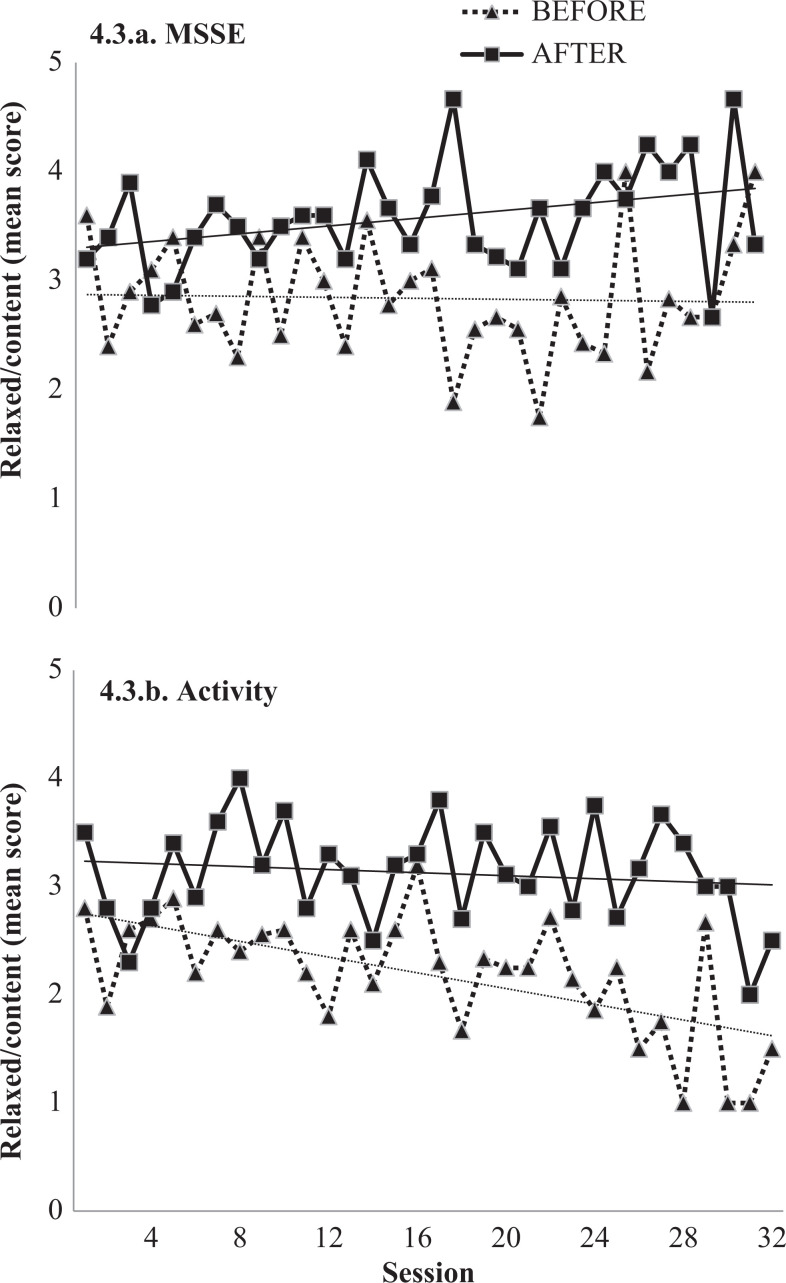
With regard to stimulation levels, at the end of the sessions, participants of both the groups were more active/alert (F 1, 18 = 19.195, P < .001), were less bored/inactive (F 1, 18 = 17.912, P = .001), and were more relaxed/content (F 1, 18 = 71.031, P < .001) than before the sessions. Figure 4 shows the mean scores before and after the sessions on these 3 items. In the activity group, the proportion of time in which participants were active/alert decreased from the beginning to the end of the study, whereas in the MSSE group, it remained more or less stable (Figure 4.1). As regards the bored/inactive item, the before- and after-session differences in the activity group increased across the course of the study (Figure 4.2). Finally, for the relaxed/content item, the before- and after-session differences increased in both the groups as the study progressed (Figure 4.3). With regard to Interact during, there were no significant differences between the mean scores of MSSE and the activity groups on any of the 22 items that were tested.
Figure 4.
Stimulation level, measured by 3 items (namely, 4.1, enjoying self, active, or alert; 4.2, bored, inactive, or sleeping inappropriately; 4.3, relaxed, content of sleeping appropriately). Interact short measurements before and 10 minutes immediately after each session in 2 types of intervention—(a) multisensory stimulation environment (MSSE) in a Snoezelen room and (b) activity—at sessions 0 (baseline) and 32 (posttrial). 1 indicates not at all; 2 = a bit of the time; 3 = some of the time; 4 = most of the time; 5 = nearly all of the time.
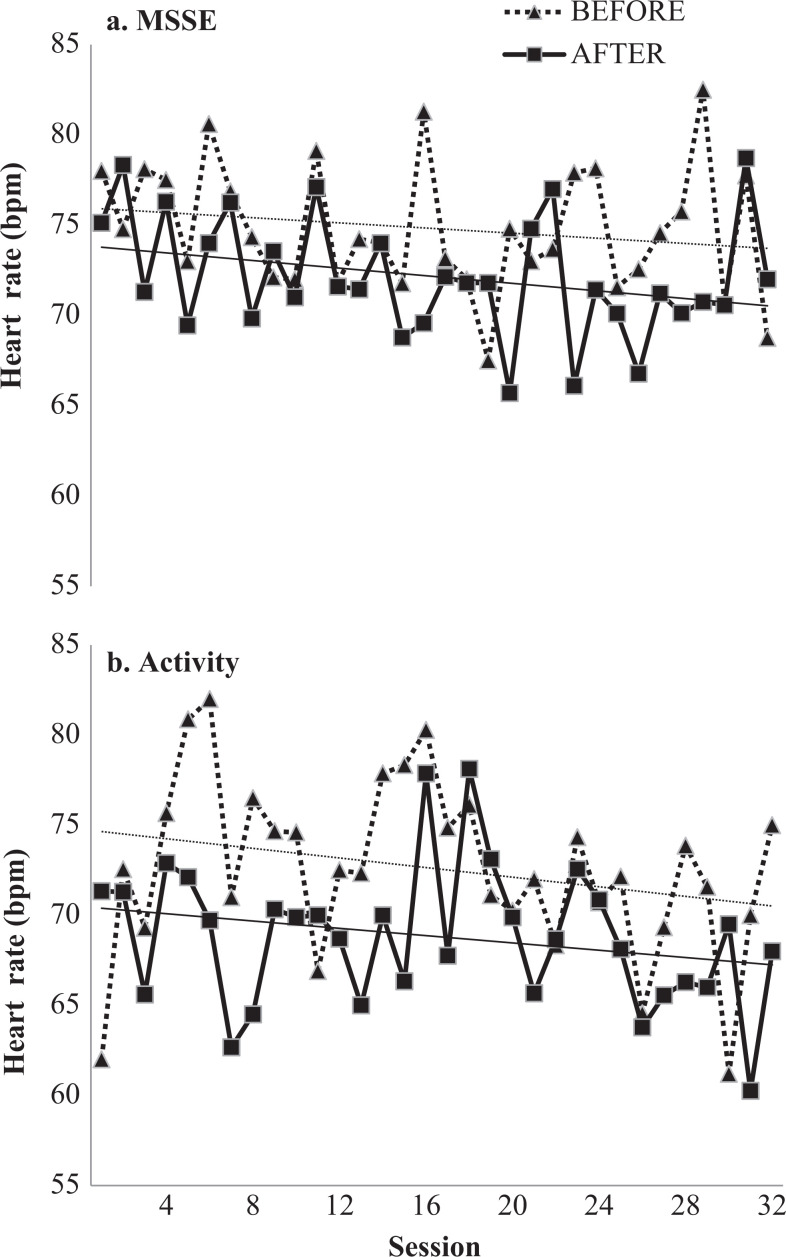
Effects on Biomedical Parameters
Regarding biomedical parameters, there were significant time effects on heart rate. Both groups reflected a decrease in heart rate from before to after sessions (F 1, 18 = 10.60, P = .004), although no significant differences were found between the groups. Figure 5 shows the participants’ heart rates in the 10 minutes before and after the MSSE and the activity sessions across the 32 sessions of intervention. Both groups reported a decrease in heart rate from the beginning to the end of the study in the 10 minutes before and after the sessions.
Figure 5.
Heart rate (beats per minute, bpm) before and after completion of 2 types of intervention—(a) multisensory stimulation environment (MSSE) in a Snoezelen room and (b) activity—at sessions 0 (baseline) and 32 (8-week follow-up).
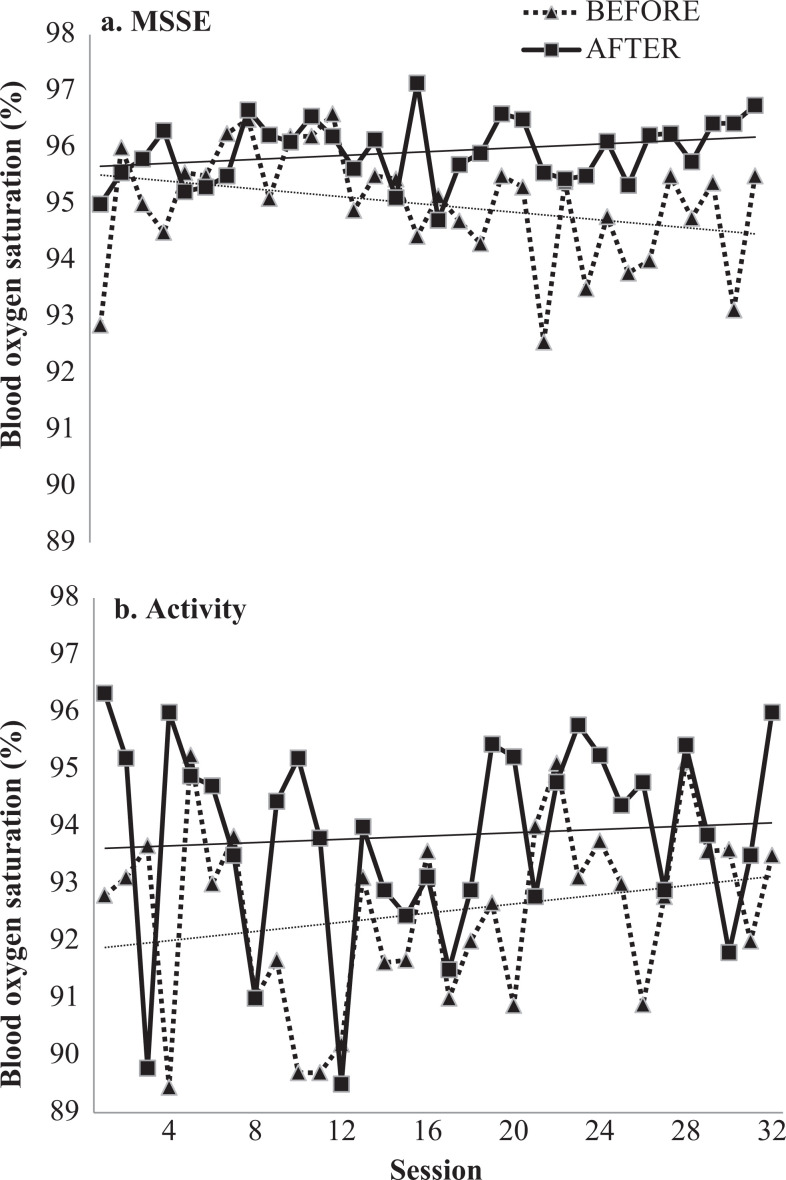
Significant time effects were also found in Spo 2. There was an increase in the mean values of both groups from before to after the sessions (F 1, 18 = 11.143, P = .004), with no significant differences between the groups. Figure 6 shows the participants’ Spo 2 levels before and after the sessions across the 32 sessions. It can be observed that the before- and after-session differences in the MSSE group increased from the beginning to the end of the intervention, whereas these differences decreased in the activity group.
Figure 6.
Blood hemoglobin oxygen saturation (%) before and after completion of 2 types of intervention—(a) multisensory stimulation environment (MSSE) in a Snoezelen room and (b) activity—at sessions 0 (baseline) and 32 (8-week follow-up).
Discussion
Effects on Mood and Behavior
Our research did not find significant differences between the groups on any of the analyzed items. This result indicates that both therapies seem to be effective at stimulating patients, albeit for a limited time. 8 Positive aspects of one-to-one therapies, as MSSE or activity sessions, can be attributed to the higher time and effort being spent with the person with dementia, the perceived qualitative shift in the relationship between the patient and the staff, and, as a result, elderly care improvement. A systematic review 27 suggested the use of psychosocial treatments in people with dementia, concluding that the benefits cannot be attributed confidently to a unique therapeutic modality, and in some instances, the benefits in the symptoms can be attributed to the empathic human interaction with the staff. The MSSE, like other one-to-one interventions, may be a useful method of managing the psychological symptoms of dementia; however, as there is currently limited evidence to support the efficacy of MSSE, in most instances the efficacy of using these for residents need to be determined on an individual basis. 28
We found that both MSSE and the activity sessions have immediate positive effects on behavior measured with the Interact short. At the end of the sessions, participants of both the groups spoke spontaneously, related better to others, and were more attentive to/focused on their environment. With regard to stimulation levels, we found that participants were more active/alert, were less bored/inactive, and were more relaxed/content.
Concerning mood and behavior during the sessions, we did not find significant differences between the MSSE and the activity groups on any of the 22 items queried in the Interact during scale.
In previous studies, interventions in a Snoezelen room have reported positive effects on the mood and behavior of patients with dementia during and after the sessions. 12 –16 The immediate effects of MSSE in a Snoezelen room were studied in 29 older people with dementia diagnoses and found that some items on the Interact during scale (eg, happy/content, held eye contact, active/alert, and relaxed/content) showed desirable changes during the session. 12
However, studies comparing the effect of a Snoezelen room intervention with a one-to-one control condition have not found significant differences between the 2 groups—if they exist, they are quite limited. 13,18 In a 4-week randomized controlled trial, the effectiveness and extent of the benefits of MSSE were compared with a control group receiving one-to-one activity sessions. 18 Consistent with our results, the authors did not find significant differences between both the groups from before to after sessions in the Interact short; as in our case, they found that, at the end of the sessions, participants of both groups related better to others and were less bored/inactive. Contrary to our findings, the authors 18 found significant differences between both the groups on the Interact during. During the sessions, participants in the MSSE group recalled significantly more memories than those from the activity group, whereas participants from this last group touched objects/equipment more appropriately and were more attentive to activities/objects. In a randomized controlled trial, the effect of the MSSE was compared to reminiscence therapy on the mood and behavior of people with dementia using a revised version of the Interact scale. 13 The authors found that both interventions had an immediate positive effect on mood and behavior and did not find differences between the groups. The effect of the MSSE on the mood of people with dementia was compared with 2 one-to-one interventions (namely, a landscaped garden and a normal living room activity). 14 The authors concluded that the 3 interventions improved mood, but what created the positive effect was the one-to-one attention.
Effects on Biomedical Parameters
In regard to the physiological rates, our study found a heart rate decrease and a Spo 2 increase in both groups from before to after sessions, with no significant differences between the 2 groups. This decline may be partly due to the fact that the participants were usually seated during the session and/or that they were less agitated. 13
Previous studies that analyzed the relaxing effect of MSSE measuring heart rate do not provide conclusive data on its effectiveness. Heart rates immediately before and after the MSSE sessions were recorded and significant differences were not found. 12 A decrease in heart rate during and immediately after the MSSE sessions was observed, but no significant differences were found compared to a control group that had received one-to-one reminiscence therapy. 13
Importance of One-to-One Intervention
The results of our study suggest that although the multisensory stimulation was experienced positively, what really improves the behavioral symptoms of people with dementia is one-to-one intervention from the therapists. This would be consistent with the empirical evidence showing that different types of one-to-one interventions (eg, behavior therapy, music therapy, reminiscence therapy, and Montessori therapy) have a positive effect on the behavioral symptoms of people with dementia. 29 –32 Additionally, in a systematic review examining the use of different psychosocial treatments in people with dementia, 27 the authors concluded that symptom improvements cannot be attributed confidently to a unique therapeutic modality; in some instances, benefits can instead be attributed to empathic human interactions with staff.
The importance of one-to-one intervention in dementia lies largely in the fact that the communication with these patients is normally complicated, particularly as the disease progresses. Therefore, therapists should devote time and effort to the relationship with the patient. The MSSE is one of the interventions that offer the potential to increase meaningful communication with patients with dementia. 33
Despite limited evidence supporting a higher efficacy of MSSE compared to other type of one-to-one interventions, its growing popularity in recent times may be due to the move to a more holistic and person-centered approach to the care of older people in residential aged care settings. 28 In line with this approach, the MSSE puts special emphasis on recognizing the personality of the patient with dementia, toward the goals of personalizing care and fostering shared decision making.34,35 Moreover, the MSSE creates a sense of calm and well-being in caregivers, 14 positively affects their behavior toward patients and the quality of their working lives, and affects the adoption of a more person-centered approach. 36,37
A possible hypothesis is that patients with very low levels of functioning may differentially benefit from MSSE in comparison to more cognitively demanding one-to-one interventions. It may be argued that each intervention is appropriate at different stages and levels of dementia. 8,18
Regardless of such details, when carrying out individualized sessions for MSSE or other types of one-to-one activities, it is very important to take into account personal circumstances, such as lifestyle, preferences, residual abilities, desires, and cultural diversity, to adjust the stimulation for each person. 38 –40 Also, a more standardized approach of MSSE, wherein the presentation of the equipment and the structure and timing of the intervention were standardized according to sensory preferences and individual need of each participants, has also effective outcomes. 10,11 In this sense, nonpharmacological interventions for people with dementia have proved more effective when they are tailored to individuals’ backgrounds and preferences. 27,41
Limitations and Recommendations for Future Research
One limitation from the present study is the sample sizes of each group. The small samples may account for the nonsignificant results found in some of the outcome measures. Future empirical studies with larger samples are necessary to confirm our results.
Another factor to take into account is that people in advanced stages of dementia, with very low levels of functioning, may benefit more from MSSE than from more cognitively demanding one-to-one activities. Activity sessions may only be viable if the patient is able to understand simple instructions to carry out simple tasks, whereas MSSE stimuli are unpatterned and not highly demanding on attention. 8,18 Therefore, future research should conduct specific studies on people in advanced stages of dementia, using tools that allow more discriminative measurements for this group.
An MSSE using a Snoezelen room requires the investment of economic resources greater than those required in other one-to-one therapies for people with dementia. Therefore, it is especially necessary to demonstrate in an empirical way that its benefits on symptoms of people with dementia are better than those provided by one-to-one attention. Resources such as the man power and the costs of setting up an MSSE cannot be justified without such evidence. 6
Conclusions
Our results support the idea that both MSSE and activity sessions seem to be appropriate therapies for people with dementia. Immediately after the sessions, patients spoke more spontaneously, related better to others, were more attentive to their environments, more active/alert, less bored/inactive, and more relaxed/content. Also, both groups exhibited an improvement in the physiological rates from before to after the sessions. The MSSE was not found to be more effective than the activity sessions for any of the parameters analyzed, and this nonsignificant finding might be explained by a one-to-one interaction with the therapist being the therapeutically active factor on behavior and physiology.
Acknowledgments
We thank the users and staff of the Gerontology Complex La Milagrosa without whom the study would not have been possible. We are truly grateful to Prof Roger Baker for providing us information to design a randomized control trial of the snoezelen multisensory environment for patients with dementia.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Kovach CR. Sensoristasis and imbalance in persons with dementia. J Nurs Scholarsh. 2000;32(4):379–384. [DOI] [PubMed] [Google Scholar]
- 2. Fleming R, Purandare N. Long-term care for people with dementia: environmental design guidelines. Int Psychogeriatr. 2010;22(7):1084–1096. [DOI] [PubMed] [Google Scholar]
- 3. Chitsey AM, Haight BK, Jones MM. Snoezelen: a multisensory environmental intervention. J Gerontol Nurs. 2002;28(3):41–49. [DOI] [PubMed] [Google Scholar]
- 4. Moffat N, Barker P, Pinkney L. Snoezelen: An Experience for People with Dementia. Chesterfield, MO: Rompa; 1993. [Google Scholar]
- 5. Burns I, Cox H, Plant H. Leisure or therapeutics? Snoezelen and the care of older persons with dementia. Int J Nurs Pract. 2000;6(3):118–126. [DOI] [PubMed] [Google Scholar]
- 6. Chung JC, Lai CK. Snoezelen for dementia. The Cochrane Library. 2002;(4):CD003152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Milev RV, Kellar T, McLean M, et al. Multisensory stimulation for elderly with dementia: A 24-week single-blind randomized controlled pilot study. Am J Alzheimers Dis Other Demen. 2008;23(4):372–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baker R, Bell S, Baker E, et al. A randomized controlled trial of the effects of multi-sensory stimulation (MSS) for people with dementia. Br J Clin Psychol. 2001;40(pt 1):81–96. [DOI] [PubMed] [Google Scholar]
- 9. Sánchez A, Millán-Calenti JC, Lorenzo-López L, Maseda A. Multisensory stimulation for people with dementia: a review of the literature. Am J Alzheimers Dis Other Demen. 2013:28(1):7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Collier L, McPherson K, Ellis-Hill C, Staal J, Bucks R. Multisensory stimulation to improve functional performance in moderate to severe dementia–interim results. Am J Alzheimers Dis Other Demen. 2010;25(8):698–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Staal JA. Functional analytic multisensory environmental therapy for people with dementia. Int J Alzheimers Dis. 2012;2012:294801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hope KW. The effects of multisensory environments on older people with dementia. J Psychiatr Ment Health Nurs. 1998;5(5):377–385. [DOI] [PubMed] [Google Scholar]
- 13. Baillon S, Van Diepen E, Prettyman R, Redman J, Rooke N, Campbell R. A comparison of the effects of Snoezelen and reminiscence therapy on the agitated behaviour of patients with dementia. Int J Geriatr Psychiatry. 2004;19(11):1047–1052. [DOI] [PubMed] [Google Scholar]
- 14. Cox H, Burns I, Savage S. Multisensory environments for leisure: promoting well-being in nursing home residents with dementia. J Gerontol Nurs. 2004;30(2):37–45. [DOI] [PubMed] [Google Scholar]
- 15. Cornell A. Evaluating the effectiveness of Snoezelen on women who have a dementing illness. Int J Psychiatr Nurs Res. 2004;9(2):1045–1062. [PubMed] [Google Scholar]
- 16. Minner D, Hoffstetter P, Casey L, Jones D. Snoezelen activity: the Good Shepherd Nursing Home experience. J Nurs Care Qual. 2004;19(4):343–348. [DOI] [PubMed] [Google Scholar]
- 17. Riley-Doucet CK. Use of multisensory environments in the home for people with dementia. J Gerontol Nurs. 2009;35(5):42–52. [DOI] [PubMed] [Google Scholar]
- 18. Baker R, Holloway J, Holtkamp CC, et al. Effects of multi-sensory stimulation for people with dementia. J Adv Nurs. 2003;43(5):465–477. [DOI] [PubMed] [Google Scholar]
- 19. Chester JG, Rudolph JL. Vital signs in older patients: age-related changes. J Am Med Dir Assoc. 2011;12(5):337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reisberg B, Ferris SH, de León MJ, Crook T. Global Deterioration Scale (GDS). Psychofarmacol Bull. 1988;24(4):661–663. [PubMed] [Google Scholar]
- 21. Maseda A, Sánchez A, Marante MP, González-Abraldes I, Buján A, Millán-Calenti JC. Effects of multisensory stimulation in a simple of institutionalized elderly people with dementia diagnosis: a controlled longitudinal trial. Am J Alzheimers Dis Other Demen. published online 6 March 2014; DOI: 10.1177/1533317514522540. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Baker R, Bell S, Assey J, et al. A Randomized Controlled Trial of the Snoezelen Multi-Sensory Environment for Patients With Dementia. Dorset: Research and Development Support Unit, Poole Hospital; 1998. [Google Scholar]
- 23. Pace GM, Ivancic MT, Edwards GL, Iwata BA, Page TJ. Assessment of stimulus preference and reinforcer value with profoundly retarded individuals. J Appl Behav Anal. 1985;18(3):249–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Baker R, Dowling Z. INTERACT. Bournemouth: King’s Park Community Hospital, Dorset Healthcare NHS Trust; 1995. [Google Scholar]
- 25. Wareing L, Coleman P, Baker R. Multisensory environments and older people with dementia. Br J Ther Rehabil. 1998;5(2):624–629. [Google Scholar]
- 26. SPSS PASW®. Statistics 18 Core System User’s Guide. Chicago: SPSS Inc; 2009. [Google Scholar]
- 27. O'Connor DW, Ames D, Gardner B, King M. Psychosocial treatments of behavior symptoms in dementia: a systematic review of reports meeting quality standards. Int Psychogeriatr. 2009;21(2):225–240. [DOI] [PubMed] [Google Scholar]
- 28. Bauer M, Rayner JA, Koch S, Chenco C. The use of multi-sensory interventions to manage dementia-related behaviours in the residential aged care setting: a survey of one Australian state. J Clin Nurs. 2012;21(21-22):3061–3069. [DOI] [PubMed] [Google Scholar]
- 29. Politis AM, Vozzella S, Mayer LS, Onyike CU, Baker AS, Lyketsos CG. A randomized, controlled, clinical trial of activity therapy for apathy in patients with dementia residing in long-term care. Int J Geriatr Psychiatry. 2004;19(11):1087–1094. [DOI] [PubMed] [Google Scholar]
- 30. Davison TE, Hudgson C, McCabe MP, George K, Buchanan G. An individualized psychosocial approach for “treatment resistant” behavioral symptoms of dementia among aged care residents. Int Psychogeriatr. 2007;19(5):859–873. [DOI] [PubMed] [Google Scholar]
- 31. Sakamoto M, Ando H, Tsutou A. Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. Int Psychogeriatr. 2013;25(5):775–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. van der Ploeg ES, Eppingstall B, Camp CJ, Runci SJ, Taffe J, O'Connor DW. A randomized crossover trial to study the effect of personalized, one-to-one interaction using Montessori-based activities on agitation, affect, and engagement in nursing home residents with Dementia. Int Psychogeriatr. 2013;25(4):565–575. [DOI] [PubMed] [Google Scholar]
- 33. Hope KW, Easby R, Waterman H. Finding the person the disease has'-the case for multisensory environments. J Psychiatr Ment Health Nurs. 2004;11(5):554–561. [DOI] [PubMed] [Google Scholar]
- 34. Buron B. Levels of personhood: a model for dementia care. Geriatr Nurs. 2008;29(5):324–332. [DOI] [PubMed] [Google Scholar]
- 34. Edvardsson D, Winblad B, Sandman PO. Person-centred care of people with severe Alzheimer's disease: current status and ways forward. Lancet Neurol. 2008;7(4):362–367. [DOI] [PubMed] [Google Scholar]
- 36. van Weert JC, van Dulmen AM, Spreeuwenberg PM, Bensing JM, Ribbe MW. The effects of the implementation of snoezelen on the quality of working life in psychogeriatric care. Int Psychogeriatr. 2005;17(3):407–428. [DOI] [PubMed] [Google Scholar]
- 37. Van Weert JC, Janssen BM, Van Dulmen AM, Spreeuwenberg PM, Bensing JM, Ribbe MW. Nursing assistants’ behavior during morning care: effects of the implementation of snoezelen, integrated in 24-hour dementia care. J Adv Nurs. 2006;53(6):656–668. [DOI] [PubMed] [Google Scholar]
- 38. Lancioni GE, Cuvo AJ, O’Reilly MF. Snoezelen: an overview of research with people with developmental disabilities and dementia. Disabil Rehabil. 2002;24(4):175–184. [DOI] [PubMed] [Google Scholar]
- 39. Feliciano L, Steers ME, Elite-Marcandonatou A, McLane M, Areán PA. Applications of preference assessment procedures in depression and agitation management in elders with dementia. Clin Gerontologist. 2009;32(3):239–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cruz J, Marques A, Barbosa AL, Figueiredo D, Sousa L. Effects of a motor and multisensory-based approach on residents with moderate-to-severe dementia. Am J Alzheimers Dis Other Demen. 2011;26(4):282–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sung HC, Chang AM. Use of preferred music to decrease agitated behaviors in older people with dementia: a review of the literature. J Clin Nurs. 2005;14(9):1133–1140. [DOI] [PubMed] [Google Scholar]