Abstract
Background/Aim:
Two studies assessed the effectiveness of video prompting as a strategy to support persons with mild and moderate Alzheimer’s disease in performing daily activities.
Methods:
In study I, video prompting was compared to an existing strategy relying on verbal instructions. In study II, video prompting was compared to another existing strategy relying on static pictorial cues. Video prompting and the other strategies were counterbalanced across tasks and participants and compared within alternating treatments designs.
Results:
Video prompting was effective in all participants. Similarly effective were the other 2 strategies, and only occasional differences between the strategies were reported. Two social validation assessments showed that university psychology students and graduates rated the patients’ performance with video prompting more favorably than their performance with the other strategies.
Conclusion:
Video prompting may be considered a valuable alternative to the other strategies to support daily activities in persons with Alzheimer's disease.
Keywords: Alzheimer’s disease, video prompting, verbal instructions, pictorial instructions, daily activities
Introduction
Alzheimer’s disease is an irreversible neurodegenerative condition characterized by a progressive and significant decline in cognitive and physical functioning and is a leading cause of disability (dementia) in old age. 1 –7 The disease is also frequently associated with increasing spatial disorientation, even in indoor contexts, 8 –11 memory impairment, and negative social–emotional effects (eg, apathy, withdrawal, and depression), making the situation of the persons affected very complex and seriously compromised. 12 -17 One of the key clinical features associated with Alzheimer’s disease is the progressive decline in the patient’s ability to perform daily activities (ie, the ability to remember the steps involved in the activities and their sequential order). 18 -26
Behavioral research efforts aimed at devising strategies to support the performance (recovery) of daily activities are based on the assumption that the patients’ ability to carry out daily activities is a way to (1) counter their decline, frustration/depression, and withdrawal, 3,17,27 -32 (2) promote their self-determination, alertness, and social image, 3,7,17,30,31 and (3) enhance their overall quality of life and reduce their demand on caregivers. 33,34
Recently, several efforts have been directed at setting up and evaluating technology-based instruction strategies to promote independent daily activity in patients with Alzheimer’s disease. 35 -41 These technology-aided strategies were designed to provide the patients one instruction at a time, in relation to the single steps of the activities that they were to perform, in order to help them circumvent their memory problems. 22,23,25,42 The view was that the patients could learn to use those instructions successfully and, hence, manage the activities independently regardless of their memory conditions. 29,35 -40 The more widely used strategy involved verbal instructions. 29,35 -40 A second strategy assessed with these patients involved pictorial instructions. 41
The positive results obtained with both those strategies are very encouraging and also suggest the desirability or need of devising additional strategies so as to have multiple alternatives allowing one to reach a wider range of patients. For example, the pictorial instructions involved in the second strategy mentioned above were static visual cues. Recent research with persons having developmental disabilities and autism seems to indicate that dynamic visual cues (ie, video clips representing the actions involved in the single activity steps) may be more effective forms of instruction than static pictorial images. 43 -47 Such a dynamic approach, known as video prompting, 44 -46 might represent a more informative/transparent form of instruction than static pictorial representations and verbal instructions (whose messages need to be translated into step actions) for persons with Alzheimer’s disease as well. 41,45,46,48
The present 2 studies served to (1) develop and assess a technology-aided intervention strategy involving video prompting for persons with Alzheimer’s disease and (2) compare the effects of such a strategy with those of a verbal instruction strategy (study I) and those of a strategy based on static pictorial cues (study II). The expectation was that the new strategy could be more effective than, or as effective as, the previously developed strategies (ie, based on the presumably high transparency of video prompting). 45,48 In the former case, the data would point to a new approach that could become an instrument of choice in the daily work with persons with Alzheimer’s disease. In the latter case, the data would point to an alternative that could be used profitably whenever staff or patients preferred it to the previous ones. A second objective of the studies was to carry out social validation assessments of the video prompting strategy in comparison with each of the existing strategies. University psychology students and graduates served as social raters within those assessments.
Study I
Method
Participants
The participants (Holly, Wendy, Louise, and Rhonda) were between 72 and 91 (mean [M] = 78) years of age and attended a nursing home for persons with Alzheimer’s disease and other dementias, in which they were involved in various forms of supervised occupational and leisure activity (eg, craft projects, games, and music) and mild physical and cognitive exercises. They were not reported to have specific pharmacological treatment for their disease. Their selection for the study was based on 3 general criteria. First, they were functioning within the mild or moderate range of Alzheimer’s disease. Their scores on the Mini-Mental State Examination 49 were between 11 and 22, with a mean of 18. The scores on the Hamilton Depression Rating Scale (17-item version) 50 were below 6, suggesting that all participants were within the normal range. Second, they presented serious problems in carrying out daily activities (ie, showed step substitution, omission, or sequence errors that psychological reports attributed to their fading memory). However, they possessed a good control of the upper limbs, which was required for carrying out the activity steps. They were also reported to have typical hearing and visual functioning skills that allowed them to understand (respond to) verbal instructions as well as videos aimed at guiding them through the activity steps. Third, their families and staff personnel were highly interested in an evaluation and possible application of technology-based intervention strategies to support their daily activities. Their families had also signed a formal consent authorizing their involvement in this study, which had been approved by a scientific and ethics committee.
Setting, Activities, and Data Recording
The study was carried out in a quiet room of the nursing home that the participants attended. Two activities were available for each participant. One activity used the video prompting strategy and the other activity used the verbal instructions strategy. One or two trials per activity occurred each day. The activities were similar to those used by Lancioni et al 40 and practically relevant for the participants. They consisted of coffee preparation and table setting and included 18 steps. Table 1 reports the list of steps used for coffee preparation and the general verbal instructions that were available for them. When this activity was used with the video prompting strategy, the step instructions consisted of video clips portraying the actions required to complete the single steps from the performer’s perspective. 44,45 The participants used 2 contiguous desks for the activity. One desk (ie, items’ desk) contained all the items required for the activity scheduled; the other desk (ie, implementation desk) served for using/arranging those items and thus completing the activity. 37 Data recording concerned the participants’ performance of the activity steps. A step was recorded as “correct” if it matched the description of that step and occurred independent of guidance by research assistants. Interrater agreement was checked over 20% of the baseline and intervention trials. The percentages of interrater agreement were computed by dividing the number of activity steps with agreement by the total number of steps and multiplying by 100. The percentages were within the 85 to 100 range, with means above 95.
Table 1.
List of Steps (and General Verbal Instructions) for Coffee Preparation Activity.
| 1. Take the tablecloth |
| 2. Put tablecloth on the table |
| 3. Take the coffee machine |
| 4. Put coffee machine on the table |
| 5. Take the filter |
| 6. Put filter in the machine |
| 7. Take the coffee can |
| 8. Put coffee can on the table |
| 9. Take the spoon |
| 10. Put coffee in the filter |
| 11. Take the bottle of water |
| 12. Put water in the machine |
| 13. Take the rag |
| 14. Clean the table |
| 15. Take the tray |
| 16. Put tray on the table |
| 17. Take 2 cups |
| 18. Put the cups on the tray |
Technology With Verbal Instructions
The technology with verbal instructions included (1) a computer with specific software containing the recording of the verbal instructions related to the activity to be performed, (2) 2 speakers, (3) optic sensors (photocells), and (4) light-reflecting paper. Two contiguous desks were used for the activities, namely, an items’ desk and an implementation desk (discussed previously). The photocells and light-reflecting paper were arranged in front (at the opposite sides) of the first desk, that is, the one containing the activity items, so that the participant broke the photocell light beams every time she reached for the items. Activity trials started with the computer presenting the first instruction (eg, take the tablecloth). In taking the item, the participant activated the photocells. This started a programmed, brief interval (eg, 4 seconds) at the end of which the computer presented the next instruction (eg, put tablecloth on table). After a programmed, longer interval (eg, 20 seconds), the third instruction occurred. Such a procedure continued for each step of the sequence. Brief intervals were programmed after the responses of taking objects from the items’ desk and longer intervals after the instructions of using/arranging those objects at the implementation desk. The length of the intervals was programmed, for each participant individually, by the research assistants involved in the study. 35 -40 Such programming was based on observations of the participants during the activity. 35 -40 In essence, the technology ensured that the participants received 1 verbal instruction at a time, in relation to the single steps of the activities that they were to perform. 28,29,35,36,44,45
Technology With Video Prompting
The technology with video prompting included (1) a computer with specific software regulating the video clips related to the activity steps to be performed, (2) 2 speakers, (3) 1 screen located on a base between the items’ desk and the implementation desk, (4) optic sensors (photocells), and (5) light-reflecting paper. Video prompting consisted of the presentation of video clips (ie, separate film segments), which represented the activity steps. Each video clip (ie, step representation) lasted 6 to 18 seconds, with an average duration of about 9 seconds. The clips were filmed from the performer’s perspective (ie, the perspective of the person who had to carry out the activity) and involved the same material as used during the intervention trials. 45 In addition to demonstrating the actions required for completing a step, each video clip included a voice-over cue alerting/encouraging the participant to watch. Each video clip ended with a static image (ie, the last frame of the clip) that remained on view. Activity trials started with the computer presenting the first video clip/prompt. The procedure followed for the presentation of the video clips/prompts of the following steps was the same as that described for the verbal instructions. In essence, the participant was presented 1 video clip at a time, and the technology was arranged in such a way that it would allow the participant the possibility of completing the step on hand before the next clip was shown. 41,47
Experimental Conditions
The study was carried out according to an alternating treatments design, in which each of the 2 strategies was used for 1 of the activities available. 51 For Louise and Wendy, the first activity (ie, coffee preparation) was used with the verbal instructions strategy, and the second activity (ie, table setting) was used with the video prompting strategy. Rhonda and Holly had the opposite activity–strategy combination. When the participants’ performance showed stability over trials, a crossover phase reversing the activity–strategy combinations was introduced. This served to verify whether the percentages of correct responses/steps obtained for the activities were due to the strategies or the activities per se. 51,52 Guidance by a research assistant occurred if the participants failed to respond to a verbal instruction or video prompt for 10 to 20 seconds (during intervention) or performed a step incorrectly (during both baseline and intervention). At the end of the sequence, the research assistant expressed social appreciation (ie, 2 or 3 sentences underlining the participants’ good effort). Following the end of the study, a social validation assessment was carried out, in which university psychology students were asked to rate the participants’ performance with the video prompting strategy and the verbal instructions strategy on a 5-item questionnaire.
Baseline
Four or 8 baseline trials were carried out on each of the 2 activities available for the participants. During baseline trials, the participants did not have the support of the technology. The research assistant simply asked the participants to carry out the activity scheduled for the trial. The baseline ended only if the percentage of correct steps at the last trial was lower than or equal to that recorded in one or more of the previous trials. 41
Intervention
Intervention on each activity was preceded by 6 or 7 familiarization (practice) trials during which the research assistant used the necessary guidance to ensure that the participants responded to the technology-based instructions (verbal instructions or video prompts) and avoided errors. These trials were followed by 40 to 50 regular intervention trials per activity (ie, a number of trials ensuring performance consolidation/stability). Each activity was combined with 1 of the strategies (see Experimental conditions), and the trials on them occurred in an alternating fashion. 51 Guidance by the research assistant occurred as described above (see Experimental Conditions).
Crossover
Thirty crossover trials were carried out for each activity (ie, to be able to identify any immediate or delayed difference between strategies). During the crossover trials, the activity previously matched with video prompting was combined with verbal instructions and vice versa.
Social Validation Assessment
The social validation assessment of the participants’ performance with the 2 instruction strategies relied on the ratings of 4 groups of 10 university psychology students with a mean age of about 22 years. These groups represented convenience samples selected among students who had an interest in the field of disabilities and rehabilitation. 53 Each group was employed to rate the performance of 1 of the 4 participants by watching two 3-minute video clips of that participant. One video contained part of a trial with the verbal strategy and the other video part of a trial with video prompting. The order of the 2 parts varied across the students. Those parts were selected by the research assistants in charge of the study who had agreed in considering them representative of the participant's performance with the 2 strategies. The rating was carried out through a 5-item questionnaire (see Table 2). For each item, the students provided a score of 1 to 5, which indicated least and most positive ratings, respectively.
Table 2.
Questionnaire Items of the Social Validation Assessment.
| 1. Do you think that the participant is comfortable with this strategy? |
| 2. Do you think that this strategy is easily compatible with the daily context? |
| 3. Do you think that the participant can benefit from this strategy? |
| 4. Do you think that caregivers and family would support this strategy? |
| 5. Would you like to be involved in the use of this strategy? |
Results
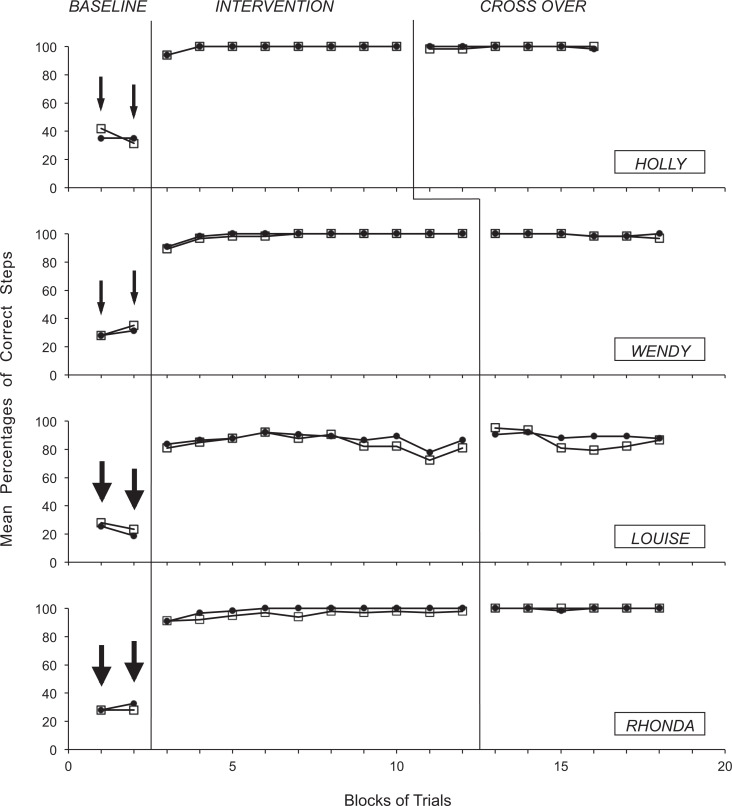
The 4 graphs of Figure 1 summarize the data for Holly, Wendy, Louise, and Rhonda, respectively. The black circles and empty squares represent mean percentages of correct steps over blocks of baseline, intervention, and crossover trials for the activity assigned to video prompting and the activity assigned to verbal instructions, respectively. Blocks include 5 trials except when arrows are present. In those cases, they include 2 or 4 trials, depending on whether a smaller or a larger arrow is present. During baseline, the participants’ mean percentages of activity steps carried out correctly varied from below 20 to about 40. During the intervention with video prompting, the participants’ mean percentages of correct steps increased to levels exceeding 90, except in the case of Louise who had a level of about 85. During the intervention with the verbal instructions, their mean percentages were similarly high. During the crossover phase, the percentages remained largely similar regardless of the change in the activity–strategy combinations. The Kolmogorov-Smirnov test (a standard nonparametric procedure to compare data distributions) 54 showed no significant difference between the levels of correct steps obtained with the 2 strategies. The study was completed in about 3 months for all the participants.
Figure 1.
The 4 graphs summarize the data for Holly, Wendy, Louise, and Rhonda. The black circles and empty squares represent mean percentages of correct steps over blocks of baseline, intervention, and crossover trials for the activity assigned to video prompting and the activity assigned to verbal instructions, respectively. Blocks include 5 trials except when a smaller or a larger arrow is present. In those cases, they include 2 and 4 trials, respectively.
Table 3 shows the raters’ mean scores, standard deviations, and P values computed on the single questionnaire items for both the strategies. The computation was based on the data of all 4 participants. The mean scores for the 5 items of the questionnaire varied between 3.45 and 3.63 in relation to the video prompting strategy and between 2.78 and 3.45 in relation to the verbal instructions strategy. The score differences between the 2 strategies, assessed with paired t tests (standard parametric procedures to compare data distributions), 55 were statistically significant for 3 items of the questionnaire. Those items were the second, fourth, and fifth and concerned the compatibility of the strategy with the daily context, caregivers’ and family’s support for the strategy, and raters’ personal interest in using it (see Table 3).
Table 3.
Raters’ Mean Scores (M) and Standard Deviations (SD) on the Questionnaire Items for the 2 Strategies.a
| Strategies | |||||
|---|---|---|---|---|---|
| Video Prompting | Verbal Instructions | ||||
| Items | M | SD | M | SD | Paired t test P Value |
| 1 | 3.58 | 0.89 | 3.45 | 0.77 | ns |
| 2 | 3.45 | 1.09 | 2.78 | 0.91 | P < .001 |
| 3 | 3.53 | 0.97 | 3.10 | 0.99 | ns |
| 4 | 3.63 | 0.89 | 3.20 | 0.90 | P < .05 |
| 5 | 3.53 | 0.87 | 3.00 | 0.87 | P < .001 |
Abbreviations: M, mean; SD, standard deviation; ns, not significant.
a Rating scale used anchors of 1 = very low and 5 = very high.
Study II
Method
Participants
The participants (Peggy, Page, Tory, and Scarlett) were between 75 and 91 (M = 80) years of age and attended a day center for persons with Alzheimer’s disease, where they were provided with some supervised activity involvement and mild movement opportunities. Pharmacological treatment for the Alzheimer’s condition was available for Tory and Scarlett and consisted of memantine. Like in study I, the participants’ selection was based on 3 general criteria. First, they were functioning within the mild or moderate range of the disease. Their scores on the Mini-Mental State Examination 49 were 20, 17, 22, and 22, respectively. The scores on the Hamilton Depression Rating Scale (17-item version) 50 were between 7 and 23, suggesting that 1 participant (Peggy) was in the severe and another 1 (Page) in the mild range of depression, whereas the other 2 did not have depression. Second, all 4 participants had problems in carrying out daily activities (with step and sequence errors attributed to fading memory; ie, as in study I). However, they were known to possess and control the motor schemes required for the activity steps and understand and respond to verbal and pictorial instructions. Third, their families and staff personnel were highly interested in the use of technology-based intervention strategies to support their daily activities. Their families had also signed a formal consent for this study, which had been approved by a scientific and ethics committee.
Setting, Activities, and Data Recording
The setting for this study was an activity room of the day center that the participants attended. The 2 activities selected for the study were practically relevant for the participants and consisted of preparing vegetables and dressing vegetables. The activities included 20 steps. Table 4 reports the list of steps for the dressing activity. When an activity was used with the pictorial cues strategy, the step instructions consisted of static picture cues. When the activity was used with the video prompting strategy, the step instructions consisted of video clips portraying the step actions from the performer’s perspective (see study I). Use of instructions, data recording, and interrater reliability matched those of study I.
Table 4.
List of Steps for Dressing Vegetables Activity.
| 1. Take the apron |
| 2. Put the apron on |
| 3. Take the tablecloth |
| 4. Put the tablecloth on the table |
| 5. Take the baking tin with vegetables |
| 6. Put the baking tin on the table |
| 7. Take olive oil |
| 8. Pour oil on vegetables |
| 9. Take salt |
| 10. Put salt on vegetables |
| 11. Take spices |
| 12. Put spices on vegetables |
| 13. Take pieces of cheese |
| 14. Put pieces on vegetables |
| 15. Take a large spoon |
| 16. Mix the vegetables |
| 17. Take grained bread |
| 18. Spread bread on vegetables |
| 19. Take a rag |
| 20. Clean the table |
Technology With Pictorial Cues
The technology with pictorial cues included (1) a computer with specific software regulating the pictorial (photographic) images/cues related to the activity steps to be performed, (2) 2 speakers, (3) 1 screen located on a base between the items’ desk and the implementation desk, (4) optic sensors (photocells), and (5) light-reflecting paper. At the start of an activity trial, the screen showed a pictorial cue. This represented the first instruction (eg, the image of the apron that the participant was to take from the items’ desk). In taking the apron, the participant activated the optic sensors and caused the appearance of a new pictorial cue (marked by an alerting sound) on the screen. This cue, which replaced the previous one on the screen, represented the second step of the task (eg, put the apron on). After a programmed interval (eg, 20 seconds), a new pictorial cue signaled by an alerting sound appeared on the screen. This cue represented the third instruction (ie, an item that the participant was to take from the items’ desk). The procedure continued the same way through the different steps of the activity. This technology/strategy was a simplified version of the strategy with pictorial cues used by Lancioni et al. 41
Technology With Video Prompting
The technology with video prompting was as described in study I.
Experimental Conditions
The study was carried out according to an alternating treatments design that allowed comparison of the video prompting strategy with the pictorial cues strategy. 51 Baseline, preintervention familiarization, and intervention conditions were comparable to those reported in study I. Similarly, a crossover phase followed the regular intervention period. The number of intervention and crossover trials varied between 27 and 37 and 10 and 15, respectively. Smaller numbers of trials were used compared to study I due to (1) a somewhat reduced availability of the participants and (2) the assumption that even a smaller data set could be fairly informative.
Social Validation Assessment
Four groups of 14 university psychology graduates, with a mean age of about 25 years, were involved (as raters) in a social validation assessment of the participants’ performance with the 2 strategies. Each group rated the performance of 1 participant after watching two 3-minute video clips of the participant. The clips covered part of the trial with the video prompting strategy and part of the trial with pictorial cues and were selected as in study I. The order of the parts varied across the raters. The rating was carried out through the same questionnaire used in study I (see Table 2).
Results
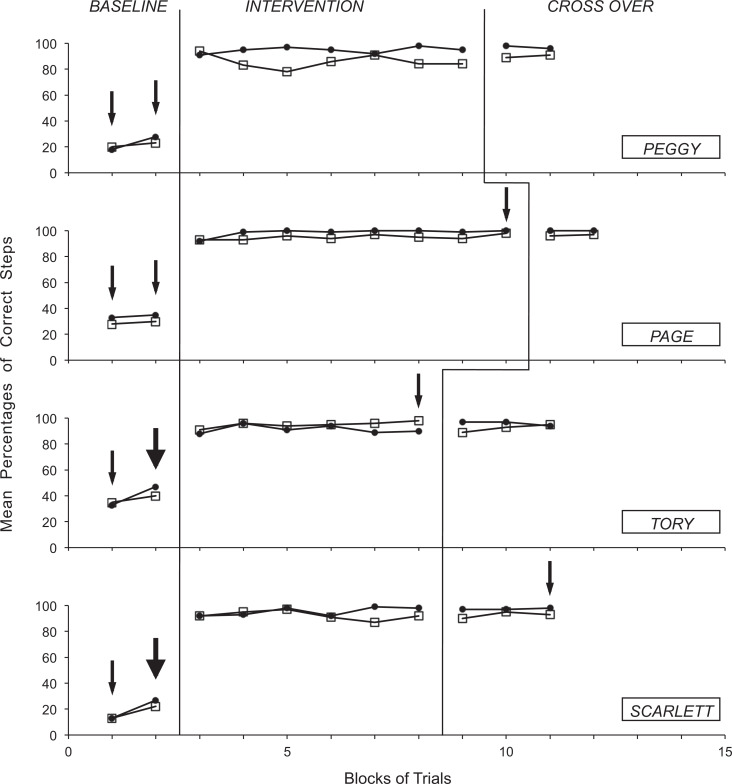
The 4 graphs of Figure 2 summarize the data for Peggy, Page, Tory, and Scarlett, respectively. The black circles and empty squares represent mean percentages of correct steps over blocks of baseline, intervention, and crossover trials for the activity assigned to video prompting and the activity assigned to pictorial cues, respectively. The blocks are as in Figure 1. During baseline, the participants’ mean percentages of activity steps carried out correctly were always below 40. Like in study I, the intervention produced high levels of correct steps with both strategies. These levels remained high during the crossover phase also. The percentages were above 90 for all the participants with video prompting and 3 of them (Peggy, Tory, and Scarlett) with pictorial cues. The Kolmogorov-Smirnov test 54 showed that the levels of correct steps obtained with video prompting were significantly higher (P < .01) than those obtained with pictorial cues during both intervention and crossover phases (for Peggy) or during the intervention phase (for Page). The study lasted less than 3 months for all the participants.
Figure 2.
The 4 graphs summarize the data for Peggy, Page, Tory, and Scarlett. The black circles and empty squares represent mean percentages of correct steps over blocks of baseline, intervention, and crossover trials for the activity assigned to video prompting and the activity assigned to pictorial cues, respectively. The blocks are portrayed as in Figure 1.
Table 5 shows that the raters’ M scores for the 5 items of the questionnaire varied between 3.38 and 4.02 in relation to the video prompting strategy and between 3.07 and 3.27 in relation to the pictorial cues strategy. The score differences between the 2 approaches, assessed with paired t tests, 55 were statistically significant for all the items of the questionnaire in favor of video prompting.
Table 5.
Raters’ Mean Scores (M) and Standard Deviations (SD) on the Questionnaire Items for the 2 Strategies.a
| Strategies | |||||
|---|---|---|---|---|---|
| Video Prompting | Pictorial Cues | ||||
| Items | M | SD | M | SD | Paired t test P Value |
| 1 | 3.88 | 0.78 | 3.09 | 0.89 | P < .001 |
| 2 | 3.38 | 0.90 | 3.11 | 0.86 | P < .05 |
| 3 | 4.02 | 0.69 | 3.23 | 0.94 | P < .001 |
| 4 | 3.98 | 0.79 | 3.27 | 0.92 | P < .001 |
| 5 | 3.64 | 0.87 | 3.07 | 1.02 | P < .001 |
Abbreviations: M, mean; SD, standard deviation; ns, not significant.
a Rating scale used anchors of 1 = very low and 5 = very high.
General Discussion
The results of these studies indicate that the new computer-aided video prompting strategy was effective in all the participants. Each participant obtained rapid and large increases in the percentage of correct steps, showing overall levels of performance comparable to or higher than those obtained with existing verbal and pictorial strategies (ie, strategies serving as relevant practical criteria). 51,56 The results of the social validation assessments indicated that the video prompting strategy was rated as (1) equivalent to the verbal instructions strategy from the standpoint of being comfortable and practically beneficial for the participant and better than the verbal instructions strategy in terms of compatibility with the daily context, caregivers’ and family’s support, and raters’ personal interest in using it (study I), and (2) better than the pictorial cues strategy on all items (study II).
In light of these results, a number of considerations can be put forward. First, the primary goal of the study, that is, developing an effective alternative to the verbal and pictorial instructions strategies for supporting daily activities in people with mild and moderate Alzheimer’s disease, appears to have been achieved. Indeed, the video prompting strategy seemed to be at least as effective as the other 2 strategies when applied with persons functioning within the mild or moderate range of the disease. 45 -48,57 Obviously, some caution may be needed in making general statements given (1) the limited number of participants and activities involved in the study and (2) the use of familiarization/practice trials at the start of the intervention. Those trials might have concealed possible differences between strategies in level of instruction transparency/efficacy (and their early effects on correct performance). 48,57
Second, the video prompting strategy may need to be analyzed not only in relation to its efficacy but also in terms of its possible advantages over the other strategies. Indeed, it may have an advantage over the verbal strategy in terms of compatibility with other activities and patients present in the same environment in which it is employed (ie, its use may occur without producing much disturbance, particularly if the screen is in a room corner). It may also have an advantage over the verbal strategy as well as the pictorial instructions strategy in terms of its impact on the opinion of social raters (ie, as indicated by the social validation assessments). Its compatibility with other activities and other people may be practically relevant and facilitate (promote) its employment over time in daily contexts. 5,28,35,36,43,46,47,58 Its positive impact on social raters and, potentially, service managers could be another factor in favor of its daily employment. 41
Third, the video prompting strategy does not largely differ from the other strategies in terms of costs. It requires a computer-aided system (like the other 2 strategies) and a screen (like the strategy relying on static pictorial cues). One could argue that the preparation of the video prompts is more laborious and time consuming than the preparation of static pictorial cues or of verbal instructions, and this might direct the choice of some staff personnel away from the first strategy. 41,58 In contrast to that mentioned previously, one could also underline the fact that the preparation of the instructions is only carried out (and for a fairly brief time period) at the beginning of the intervention program and whenever a new activity is introduced in the program. In other words, the additional time cost might be seen only as marginally relevant in relation to the overall time investment that any program requires. 59
Fourth, although the social raters considered the video prompting strategy the preferred alternative of the 3 being used, the studies failed to assess the participants’ direct preference. Knowing their preference would be important, given that they would be expected to be more consistently (lastingly) successful and at ease with the strategy that they prefer. 46,60 This would be relevant in terms of their engagement perspectives as well as their level of satisfaction. 4,6,15 Personal satisfaction could represent a most meaningful target of any intervention with these participants. 13,37,40,61,62
Fifth, new research in this area could address various issues. One issue could be the investigation of the aforementioned participants’ preference to determine whether this aspect can be used to guide the intervention choice that families and care/rehabilitation centers are required to make. 63 A second issue could concern an extension in the use of the strategies to determine whether the present findings can be replicated across patients and contexts and with multiple activities for each strategy. 51 A third issue could concern upgrades of the technology solutions at the basis of the different strategies so as to facilitate their use by staff and families. 45 A fourth issue could concern an investigation of possible ways of combining video prompting and verbal instructions to determine whether such a combination might increase the patients’ instruction benefit as opposed to the use of only verbal instructions or video prompts. 59 A fifth issue could concern new initiatives to search for possible alternatives to the present strategies in the attempt to successfully reach and help an increasingly large number of patients. 51,64
Footnotes
Authors' Note: The authors alone are responsible for the content and writing of the article.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Arkin S. Language-enriched exercise plus socialization slows cognitive decline in Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2007;22(1):62–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fernandez AL, Mainoiloff LM, Monti AA. Long-term cognitive treatment of Alzheimer’s disease: a single case study. Neuropsychol Rehabil. 2006;16(1):96–109. [DOI] [PubMed] [Google Scholar]
- 3. Giovannetti T, Bettcher BM, Libon DJ, Brennan L, Sestito N, Kessler RK. Environmental adaptations improve everyday action performance in Alzheimer’s disease: empirical support from performance-based assessment. Neuropsychol. 2007;21(4):448–457. [DOI] [PubMed] [Google Scholar]
- 4. Gitlin LN, Winter L, Burke J, Chernett N, Dennis MP, Hauck WW. Tailored activities to manage neuropsychiatric behaviors in persons with dementia and reduce caregiver burden: a randomized pilot study. Am J Geriatr Psychiatry. 2008;16(3):229–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Graff MJL, Adang EMM, Vernooij-Dassen MJM, et al. Community occupational therapy for older patients with dementia and their care givers: cost effectiveness study. BMJ. 2008;336(7636):134–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Raggi A, Iannacone S, Marcone A, et al. The effects of a comprehensive rehabilitation program of Alzheimer’s disease in a hospital setting. Behav Neurol. 2007;18(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gure TR, Kabeto MU, Plassman BL, Piette JD, Langa KM. Differences in functional impairment across subtypes of dementia. J Gerontol A Biol Sci Med Sci. 2010;65(4):434–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lancioni GE, Perilli V, Singh NN, et al. Persons with mild or moderate Alzheimer’s disease use a basic orientation technology to travel to different rooms within a day center. Res Dev Disabil. 2011;32(5):1895–1901. [DOI] [PubMed] [Google Scholar]
- 9. Lancioni GE, Perilli V, O'Reilly MF, et al. Technology-based orientation programs to support indoor travel by persons with moderate Alzheimer’s disease: Impact assessment and social validation. Res Dev Disabil. 2013;34(1):286–293. [DOI] [PubMed] [Google Scholar]
- 10. Caffò AO, De Caro MF, Picucci L, et al. Reorientation deficits are associated with amnestic mild cognitive impairment. Am J Alzheimers Dis Other Demen. 2012;27(5):321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Picucci L, Caffò AO, Bosco A. Age and sex differences in a virtual version of the reorientation task. Cogn Process. 2009;10(suppl 2):S272–S275. [DOI] [PubMed] [Google Scholar]
- 12. Appleby BS, Roy P, Valenti A, Lee HB. Diagnosis and treatment of depression in Alzheimer’s disease: impact on mood and cognition. Panminerva Med. 2007;49(3):139–149. [PubMed] [Google Scholar]
- 13. Onor ML, Trevisiol M, Negro C, Signorini A, Saina M, Aguglia E. Impact of a multimodal rehabilitative intervention on demented patients and their caregivers. Am J Alzheimers Dis Other Demen. 2007;22(4):261–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tsuno N, Homma A. What is the association between depression and Alzheimer’s disease? Expert Rev Neurother. 2009;9(11):1667–1676. [DOI] [PubMed] [Google Scholar]
- 15. Williams CL, Tappen RM. Effect of exercise on mood in nursing home residents with Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2007;22(5):389–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Williams CL, Tappen RM. Exercise training for depressed older adults with Alzheimer’s disease. Aging Ment Health. 2008;12(1):72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wood W, Womack J, Hooper B. Dying of boredom: An exploratory case study of time use, apparent affect, and routine activity situations on two Alzheimer’s special care units. Am J Occup Ther. 2009;63(3):337–350. [DOI] [PubMed] [Google Scholar]
- 18. Brown PJ, Devanand DP, Liu X, Caccappolo E. Functional impairment in elderly patients with mild cognitive impairment and mild Alzheimer disease. Arch Gen Psychiatry. 2011;68(6):617–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Galasko D. An integrated approach to the management of Alzheimer’s disease: Assessing cognition, function and behaviour. Eur J Neurol. 1998;5:S9–S17. [Google Scholar]
- 20. Green CR, Mohs RC, Schmeidler J, Aryan M, Davis KL. Functional decline in Alzheimer’s disease: a longitudinal study. J Am Geriatr Soc. 1993;41(6):654–661. [DOI] [PubMed] [Google Scholar]
- 21. Jefferson AL, Paul RH, Ozonoff A, Cohen RA. Evaluating elements of executive functioning as predictors of instrumental activities of daily living (IADLs). Arch Clin Neuropsychol. 2006;21(4):311–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Razani J, Bayan S, Funes C, et al. Patterns of deficits in daily functioning and cognitive performance of patients with Alzheimer disease. J Geriatr Psychiatry Neurol. 2011;24(1):23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rusted J, Sheppard L. Action-based memory in Alzheimer’s disease: a longitudinal look at tea making. Neurocase. 2002;8(1-2):111–126. [DOI] [PubMed] [Google Scholar]
- 24. Stern Y, Hesdorffer D, Sano M, Mayeux R. Measurement and prediction of functional capacity in Alzheimer’s disease. Neurology. 1990;40(1):8–14. [DOI] [PubMed] [Google Scholar]
- 25. Wojtasik V, Olivier C, Lekeu F, Quittre A, Adam S, Salmon E. A grid for a precise analysis of daily activities. Neuropsychol Rehabil. 2010;20(1):120–136. [DOI] [PubMed] [Google Scholar]
- 26. Zanetti O, Zanieri G, Di Giovanni G, et al. Effectiveness of procedural memory stimulation in mild Alzheimer’s disease patients: a controlled study. Neuropsychol Rehabil. 2001;11(3-4):263–272. [Google Scholar]
- 27. Boger J, Hoey J, Poupart P, Boutilier C, Fernie G, Mihailidis A. A planning system based on Markov decision processes to guide people with dementia through activities of daily living. IEEE Trans Inf Technol Biomed. 2006;10(2):323–333. [DOI] [PubMed] [Google Scholar]
- 28. Labelle KL, Mihailidis A. The use of automated prompting to facilitate handwashing in persons with dementia. Am J Occup Ther. 2006;60(4):442–450. [DOI] [PubMed] [Google Scholar]
- 29. Mihailidis A, Boger J, Canido M, Hoey J. The use of an intelligent prompting system for people with dementia. ACM Interactions. 2007;14(4):34–37. [Google Scholar]
- 30. Phinney A, Chaufhury H, O’Connor DL. Doing as much as I can do: The meaning of activity for people with dementia. Aging Ment Health. 2007;11(4):384–393. [DOI] [PubMed] [Google Scholar]
- 31. Vernooij-Dassen M. Meaningful activities for people with dementia. Aging Ment Health. 2007;11(4):359–360. [DOI] [PubMed] [Google Scholar]
- 32. Wood W, Harris S, Snider M, Patchel SA. Activity situations on an Alzheimer’s disease special care unit and resident environmental interaction, time, use, and affect. Am J Alzheimers Dis Other Demen. 2005;20(2):105–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Parmenter TR. Quality of life as a concept and measurable entity. Soc Indic Res. 1994;33(1-3):9–46. [Google Scholar]
- 34. Haveman M, van Berkum G, Rejinders R, Heller T. Differences in service needs, time demands, and caregiving burden among parents of persons with mental retardation across the life cycle. Fam Relat. 1997;46(4):417–525. [Google Scholar]
- 35. Lancioni GE, La Martire ML, Singh NN, et al. Persons with mild or moderate Alzheimer's disease managing daily activities via verbal instruction technology. Am J Alzheimers Dis Other Demen. 2008;23(6):552–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lancioni GE, Pinto K, La Martire ML, et al. Helping persons with mild or moderate Alzheimer’s disease recapture basic daily activities through the use of an instruction strategy. Disabil Rehabil. 2009;31(3):211–219. [DOI] [PubMed] [Google Scholar]
- 37. Lancioni GE, Singh NN, O’Reilly MF, et al. Persons with moderate Alzheimer’s disease improve activities and mood via instruction technology. Am J Alzheimers Dis Other Demen. 2009;24(3):246–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lancioni G, Singh N, O’Reilly M, et al. Persons with mild and moderate Alzheimer’s disease use verbal-instruction technology to manage daily activities: Effects on performance and mood. Dev Neurorehabil. 2009;12(4):181–190. [DOI] [PubMed] [Google Scholar]
- 39. Lancioni G, Singh N, O'Reilly M, et al. Persons with Alzheimer's disease perform daily activities using verbal-instruction technology: a maintenance assessment. Dev Neurorehabil. 2010;13(2):103–113. [DOI] [PubMed] [Google Scholar]
- 40. Lancioni GE, Singh NN, O'Reilly MF, et al. Technology-aided verbal instructions to help persons with mild or moderate Alzheimer's disease perform daily activities. Res Dev Disabil. 2010;31(6):1240–1250. [DOI] [PubMed] [Google Scholar]
- 41. Lancioni GE, Perilli V, Singh NN, et al. Technology-aided pictorial cues to support the performance of daily activities by persons with moderate Alzheimer's disease. Res Dev Disabil. 2012;33(1):265–273. [DOI] [PubMed] [Google Scholar]
- 42. Wattmo C, Wallin ÅK, Londos E, Minthon L. Long-term outcome and prediction models of activities of daily living in Alzheimer disease with cholinesterase inhibitor treatment. Alzheimer Dis Assoc Disord. 2011;25(1):63–72. [DOI] [PubMed] [Google Scholar]
- 43. Mechling LC, Gustafson M. Comparison of the effects of static picture and video prompting on completion of cooking related tasks by students with moderate intellectual disabilities. Exceptionality: Spec Educ J. 2009;17(2):103–116. [Google Scholar]
- 44. Cannella-Malone H, Sigafoos J, O’Reilly M, De La Cruz B, Edrisinha C, Lancioni GE. Comparing video prompting to video modeling for teaching daily living skills to six adults with developmental disabilities. Educ Train Dev Disabil. 2006;41(4):344–356. [Google Scholar]
- 45. Cannella-Malone HI, Fleming C, Chung Y, Wheeler GM, Basbagill AR, Singh AH. Teaching daily living skills to seven individuals with severe intellectual disabilities: a comparison of video prompting to video modeling. J Posit Behav Interv. 2011;13(3):144–153. [Google Scholar]
- 46. Cihak D, Alberto PA, Taber-Doughty T, Gama RI. A comparison of static picture prompting and video prompting simulation strategies using group instructional procedures. Focus on Autism and Other Developmental Disabilities. 2006;21(2):89–99. [Google Scholar]
- 47. Sigafoos J, O’Reilly M, Cannella H, et al. Evaluation of a video prompting and fading procedure for teaching dish washing skills to adults with developmental disabilities. J Behav Educ. 2007;16(2):93–109. [Google Scholar]
- 48. Chang YJ, Wang TY. Comparing picture and video prompting in autonomous indoor wayfinding for individuals with cognitive impairments. Pers Ubiquit Comput. 2010;14(8):737–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Folstein M, Folstein SE, McHugh PR. “Mini-mental state”. a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. [DOI] [PubMed] [Google Scholar]
- 50. Bagby RM, Ryder AG, Schuller DR, Marshall MB. The Hamilton Depression Rating Scale: has the golden standard become a lead weight? Am J Psychiatry. 2004;161(12):2163–2177. [DOI] [PubMed] [Google Scholar]
- 51. Barlow DH, Nock MK, Hersen M. Single Case Experimental Designs: Strategies for Studying Behavior Change. 3rd ed. New York, NY: Pergamon; 2009. [Google Scholar]
- 52. Lancioni GE, Singh NN, O'Reilly MF, Sigafoos J, Oliva D. A Verbal-instruction system to help a woman with intellectual disability and blindness manage food- and drink-preparation tasks. Clin Case Studies. 2011;10:79–90. [Google Scholar]
- 53. Pedhazur E, Schmelkin L. Measurement Design and Analysis: An Integrated Approach. New York, NY: Psychology Press; 1991. [Google Scholar]
- 54. Siegel S, Castellan NJ. Nonparametric Statistics for the Behavioral Sciences. 2nd ed. London, UK: McGraw-Hill; 1988. [Google Scholar]
- 55. Hastie T, Tibshirani R, Friedman J. The Elements of Statistical Learning: Data Mining, Inference, and Prediction. 2nd ed. New York, NY: Springer; 2009. [Google Scholar]
- 56. Kennedy C. Single Case Designs for Educational Research. New York, NY: Allyn & Bacon; 2005. [Google Scholar]
- 57. Van Laarhoven T, Kraus E, Karpman K, Nizzi R, Valentino J. A comparison of picture and video prompts to teach daily living skills to individuals with autism. Focus Autism Other Dev Disabil. 2010;25(4):195–208. [Google Scholar]
- 58. Kazdin AE. Behavior Modification in Applied Settings. 6th ed. London, UK: Wadsworth; 2001. [Google Scholar]
- 59. Sigafoos J, O’Reilly M, Cannella H, et al. Computer-presented video prompting for teaching microwave oven use to three adults with developmental disabilities. J Behav Educ. 2005;14(3):189–201. [Google Scholar]
- 60. Scherer MJ, Craddock G, Mackeogh T. The relationship of personal factors and subjective well-being to the use of assistive technology devices. Disabil Rehabil. 2011;33(10):811–817. [DOI] [PubMed] [Google Scholar]
- 61. Lancioni GE, Singh NN, O’Reilly MF, Oliva D, Basili G. An overview of research on increasing indices of happiness of people with severe/profound intellectual and multiple disabilities. Disabil Rehabil. 2005;27(3):83–93. [DOI] [PubMed] [Google Scholar]
- 62. Mausbach BT, Coon DW, Patterson TL, Grant I. Engagement in activities is associated with affective arousal in Alzheimer’s caregivers: a preliminary examination of the temporal relations between activity and affect. Behav Ther. 2008;39(4):366–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Feliciano L, Steers ME, Elite-Marcandonatou A, McLane M, Arean PA. Applications of preference assessment procedures in depression and agitation management in elders with dementia. Clin Gerontol. 2009;32(3):239–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Malinowsky C, Almkvist O, Nygård L, Kottorp A. Individual variability and environmental characteristics influence older adults’ abilities to manage everyday technology. Int Psychogeriatr. 2012;24(3):484–495. [DOI] [PubMed] [Google Scholar]