Abstract
Objectives:
To investigate the effects of using tracking technology on independent outdoor activities and psychological well-being in 3 persons with dementia (PwDs) and their spouses.
Methods:
Three experimental single-case studies with an A1B1A2B2 design. The intervention entailed access to a passive positioning alarm and technical support. Continual daily measures of independent outdoor activities among PwDs’ and spouses’ worries about these activities were made during all phases.
Results:
Access to a tracking technology consistently increased the independent outdoor activities of 2 PwDs. One of the spouses consistently reported decreased worry during B phases, another’s worry decreased only in B2, and the third showed little variability in worrying across all phases.
Conclusion:
Tracking technology may support PwDs to engage in independent outdoor activities and decrease spouses’ worries; however, randomized controlled group studies are needed to investigate whether these results can be replicated on a group level.
Keywords: Alzheimer’s, dementia, experimental single-case study, information and communication technology, outdoors, tracking technology
Introduction
The value of being outdoors for persons with dementia (PwDs) has been described, 1 –3 including how it strengthens their sense of identity, the “self.” 4,5 Some PwDs continue to spend time outdoors on their own, despite relatives’ worries that they might get lost or hurt, 6 –8 while other PwDs are restricted from going outdoors by their relatives due to such worries. 9 Locked doors are commonly used in residential homes for PwDs 10,11 and also in their own homes, although being restricted from going out has been shown to lead to decreased independence and feelings of being trapped. 12 Living with and caring for a PwD puts relatives in situations where they tend to subordinate their own activities to seeing to the PwD’s needs. 13,14 In order to support PwDs and relatives in daily life, tracking technologies based on global position system (GPS) technique have been developed, 11,15 –17 which have the potential to increase feelings of safety and security among both PwDs and their relatives. 10,18 In a recent study by Werner et al, 19 the strongest predictor of relatives’ burden was PwDs’ lower cognitive status. Notable in that study was also that, among relatives of individuals with mild dementia, a greater burden was associated with PwD spending less time outdoors. Results from Pot et al 20 showed that, while using tracking technology, PwDs experienced more freedom and were less worried while outdoors on their own and that relatives showed a trend toward being less worried. Considerable disparity of previous research regarding, for example, design, sample, and data collection methods 9,10,18 has resulted in varied outcomes concerning the effect of tracking technologies and has mostly been described from the perspective of caregivers and/or professionals. 9,16,21 Although studies 22,23 suggest that tracking technologies are reliable, there are few experimental studies evaluating the effect of using tracking technique on independent outdoor activities among PwDs and well-being among PwDs 24 and their relatives. 20 The aim of the present study was to investigate the effects of using tracking technology on independent outdoor activities and psychological well-being in 3 individual cases, that is, 3 PwDs and their spouses.
Methods
Design
Three experimental single-case studies using an A1B1A2B2 design were used, alternating nonintervention phases (A1A2) and intervention phases (B1B2). Experimental single-case designs are suitable for evaluating the effect of an intervention on behaviors and reactions in daily life. This design allows participants to be their own controls and to be studied in their natural settings, for example, their homes. The design has methodologically strong tools for showing the effects of an intervention, due to the possibility to carry out daily measures of individual-specific outcomes during different phases of the study. Daily measures assessed in structured diaries have several advantages in that they, for example, eliminate recall errors and produce consistent reporting. 25 Selected outcomes are measured daily both during a baseline period (phase A) and a period of intervention (phase B). 26 Using an A1B1A2B2 design strengthens the experiment, in that the intervention is withdrawn in A2 (return to baseline condition) and reintroduced in B2. In contrast to randomized control trial studies, where the same outcomes are measured for all participants, experimental single-case designs allow for assessment of individual-specific outcomes, taking into account that the intervention may have an impact on different aspects in different individuals. Intervention effects are demonstrated as differences in scores between phases A and B. 26
Setting and Participants
The study was conducted in the participants’ own homes and surroundings. Inclusion criteria were couples consisting of a person diagnosed with a dementia disease and his or her relative, living together in their own homes; the PwDs should have a desire and be physically able to be outdoors. Recruitment of participants was performed with the help of health care staff at the memory unit within the county council (4 couples) and the relative caregivers support center (1 couple) in a city in central Sweden. One couple was excluded due to the relative’s difficulties in carrying out the daily measures, and another couple declined participation after receiving detailed study information. Participating PwDs were all men with Alzheimer’s disease, were retired, and took medications intended to delay the progression of dementia. Participating spouses were all women and retired. Data collection was performed from May to October 2011. Characteristics of the participating couples were collected at study inclusion using individual interviews and self-administered instruments (cf. procedure and measures); participant characteristics are presented in Table 1.
Table 1.
Characteristics of Participating Couples.
| Couple 1 | Couple 2 | Couple 3 | |
|---|---|---|---|
| Persons with dementia | |||
| Age, years | 72 | 76 | 72 |
| Daytime care | 3 days/week | ||
| Spouse | |||
| Age, years | 72 | 74 | 72 |
| Descriptive measures | |||
| RUD | |||
| IADL, hours/d | 8 | 10 | |
| ADL, hours/d | 2 | 2 | |
| Supervision, hours/d | 2 | 3 | 2 |
| NPI (total score)a | 29 | 44 | 3 |
| Delusion | 0 | 1 | 0 |
| Hallucination | 0 | 1 | 0 |
| Agitation | 2 | 1 | 0 |
| Depression | 2 | 3 | 1 |
| Anxiety | 0 | 3 | 1 |
| Euphoria | 0 | 0 | 0 |
| Apathy | 8 | 4 | 1 |
| Disinhibition | 6 | 0 | 0 |
| Irritability | 6 | 3 | 0 |
| Aberrant motor behavior | 0 | 4 | 0 |
| Sleep | 4 | 12 | 0 |
| Eating | 1 | 12 | 0 |
| Caregiver Burden Scale (M) | 1.97 | 1.73 | 2.14 |
Abbreviations: RUD, Resource of Utilization in Dementia; IADLs, instrumental activities of daily living; ADLs, activities of daily living, NPI, Neuropsychiatric Inventory.
a NPI total score (range 0-144) and subarea score (range 0-12). For all instruments, high scores indicate more perceived symptoms and burden.
Couple 1
The couple lived in an apartment in an urban area with green areas/parks and several walking and bicycling paths in their neighborhood. The PwD usually took daily outdoor activities, predominantly alone. He had no mobility problems, was physically strong, and was able to take long walks. On several occasions during the month preceding study inclusion, the PwD had gotten lost while outdoors alone, causing his spouse great worry. The spouse had tried to restrict the PwD from going outdoors unaccompanied by locking the exterior door, but the PwD did not accept this and responded with irritability. According to the spouse, the PwD needed to be outdoors to avoid being irritable. The spouse also perceived the PwD to show signs of apathy, irritability, and disinhibitation (Table 1). The spouse reported that she was not engaged in her own regularly occurring activities. She had primary responsibility for the household and reported that the PwD needed some help with instrumental activities of daily living (IADLs; Table 1). The spouse perceived her level of burden due to her husband’s disease to be medium (Table 1).
Couple 2
The couple lived in an apartment with the neighborhood containing of green areas/parks along with several walking and bicycling paths; they lived in an urban area. The couple usually took daily outdoor walks together. The PwD had no history of getting lost, but due to the spouse’s fear that he would get lost, he was not allowed to take independent outdoor activities. According to the spouse, the PwD needed to be outdoors to have a feeling of well-being, and she was sad she had to restrict him from going out. The PwD participated in daytime care organized by the county council. The PwD was alone at home several hours a day when the spouse was engaged in her own activities. Because the spouse was worried that the PwD might leave the home while she was away, she locked the exterior door with an extra lock when he was at home alone. The spouse regarded this action as insulting but necessary and felt her husband accepted being locked in. The PwD had some mobility problems (not quite steady on his feet) but did not want to use any kind of aid. According to the spouse, the PwD showed signs of depression, anxiety, apathy, aberrant motor behavior changes, and severe sleep and eating disorders (Table 1). The spouse had primary responsibility for household and the PwD needed a great deal of help with IADL and some help with activities of daily living (ADLs). The spouse perceived her level of burden due to her husband’s disease to be low (Table 1).
Couple 3
The couple lived in a villa in a rural area, near wooded areas of various sizes where one could walk. In the neighborhood, there were also several walking and bicycling paths. The PwD usually took daily independent outdoor walks and bicycle rides. He had on 1 occasion been lost while outdoors alone, but this did not lead to the spouse restricting him from being outdoors. He did not have any mobility problems. The spouse was engaged in several of her own activities; she was sometimes away for the night, leaving the PwD home alone. The spouse expressed a worry that the PwD might get lost while alone outdoors. The couple did very few outdoor activities together, but during phase B1, they were on a weeklong trip to the mountains. The spouse was primarily responsible for the household, although the PwD participated. The PwD needed some help with ADL, and the spouse perceived her level of burden due to her husband’s disease to be medium (Table 1).
Intervention
The intervention (passive positioning alarm [PPA]) comprised a “service package” containing a transmitter (based on GPS technique), a cell phone, manuals for the transmitter and the cell phone, and access to a support person. When the PwDs took independent outdoor walks during phases B1 and B2, they carried the transmitter on them. When the PwD left a predefined area with a radius of 500 m, a message (short message service referred to as an alarm) with a map was sent to the spouse’s cell phone, enabling the spouse to see the location of the PwD. Further information about the PPA is reported in Olsson et al. 27
Procedures
The staff at the memory unit described the study to the couples, obtained their verbal consent, and forwarded contact information to the first author (AO), who then contacted each couple and screened them for eligibility for the study. The first author (AO) conducted an in-home interview separately with the PwDs and their spouses. This interview was done to identify individual-specific outcome variables for both the PwDs and the spouses based on perceived problems related to the PwDs’ independent outdoor activities. Detailed information was given describing the study procedure, the spouse was asked to complete self-report measures, and verbal and written informed consent was obtained from both the PwD and the spouse. In the week prior to the first baseline period (A1), the first author made a second in-home visit, during which she provided repeated information regarding study procedure, diaries covering the first 2 weeks of the study period, and stamped reply envelopes. During phase A1, the couples were instructed to make daily ratings in the diaries. On Friday at the end of phase A1, the couples participated in an instruction session regarding the PPA, provided by the support person. During the session, the couples were able to test the PPA, ask questions, and read the manuals together with the support person. The predicted time it would take for the spouses to learn to use and handle the alarm was 2 weeks. The couples received the PPA and were instructed to use the device as frequently as possible during phase B1. At the end of phase B1, the support person removed the PPA from the homes. During phase A2, the couples received no intervention. At the end of phase A2, the PPA was returned to the couples for use during phase B2.
The researcher (AO) had weekly telephone contact with the spouses during all the phases. These occasions were used to remind them to complete the dairies daily and for the researcher to answer any questions the participants might have. The participants returned their diaries by mail every week. New diaries and stamped reply envelopes were sent by mail every second week to the couples. Decisions regarding the length of each phase, for each couple, were made by 3 authors (AO, CL, and PÅ) following visual inspection of the graphs depicting the collected data; the criterion for entering the next phase was stability in the data.
Measures
Primary and secondary outcomes were assessed using daily structured ratings.
Primary Outcomes
Person with dementia independent outdoor activities (spouse rating)
The number of independent outdoor activities each day was reported by the spouses. Data are reported as the percentage of days with independent outdoor activities during each period.
Spouse’s worry concerning PwD’s independent outdoor activities (spouse rating)
The specific items concerned “worry when the husband was outdoors alone” (spouses 1 and 3) and “worry that the husband would get lost while outdoors alone” (spouse 2). Ratings were scored on numerical rating scales (0-10) with end points “not worried at all” to “extremely worried.”
Person with dementia irritability and depressive mood (proxy rating by spouse)
The specific items concerned PwD irritability (proxy PwD 1) and depressive mood (proxy PwDs 2 and 3). Spouses’ proxy ratings were scored on numerical rating scales (0-10) with end points “no irritability at all” to “extremely irritable” and “no depressive mood at all” to “extremely depressed mood,” respectively.
Secondary Outcomes
General well-being for spouses (spouse rating) and PwDs (proxy rating by spouse; PwD rating)
Ratings were scored on numerical rating scales (0-10) with end point alternatives “no well-being at all” to “extremely good.”
Worry about getting lost during independent outdoor activities (PwD 3; PwD rating)
Ratings were scored on a numerical rating scale (0-10) with end point alternatives “not worried at all” to “extremely worried.”
The diaries also contained a part in which the spouses could write whatever subjective comments they wished, for example, daily events that might have influenced use of the PPA. In addition, accompanied outdoor activities (number each day), length of independent and accompanied outdoor activities (minutes), and the number of generated alarms when the PwD was alone outdoors were assessed.
Descriptive Measures
Participant characteristics were collected at the start of phase A1 using 3 instruments completed by the spouse. The Caregiver Burden Scale (GB Scale) 28 includes 22 statements rated in terms of frequency (1 = not at all, 2 = seldom, 3 =sometimes, and 4 = often). A total burden index based on each individual’s mean scores is formed with mean scores interpreted as low burden (1.00-1.99), medium burden (2.00-2.99), and high burden (3.00-4.00). The Resource of Utilization in Dementia (RUD) 29 consists of 3 different categories, assessing how many hours are spent a day assisting the PwD with ADLs, IADLs, and supervision. The Neuropsychiatric Inventory (NPI) 30,31 includes 12 items describing symptoms that are scored regarding frequency (1 = sometimes, 2 = often, 3 = frequently, and 4 = very frequently) and severity (1 = mild, 2 = moderate, and 3 = severe); the absence of individual symptoms is assessed with a 0. Frequency scores are multiplied by severity scores, thus forming a total score that varies between 0 and 144.
Manipulation Check
The intervention was checked by documenting any events or circumstances that may have influenced the possibility for the PwDs to perform independent outdoor activities using the PPA, for example, friends visiting, doctor’s appointments, and specific weather conditions; this was achieved by inviting participants to document this in the diaries and through weekly telephone contact between the researcher (AO) and the spouses. In addition, information about instances when the transmitter was left at home, and why, was written down by participants. For couple 1, the transmitter was never forgotten at home, and for couples 2 and 3, the transmitter was left at home on 2 occasions because the spouse had forgotten to give the transmitter to the PwD.
Data Analyses
Graphs for each outcome were displayed, and medians for each outcome and phase were calculated. Visual inspections of the graphs were made so as to identify changes in level, trend, and latency. 26 Furthermore, visual inspection and calculations (percentages) of the nonoverlapping 26,32 scores between phases B1 and A1 and between B2 and A2 were made, and celeration lines 33 were drawn to “predict” the couples’ performance in later phases.
Ethical Consideration
The regional ethical review board granted permission for the study (2009/078). Participation in the study was strictly voluntary, all participants were assured of confidentiality and that they could withdraw from the study at any time without giving any explanation.
Results
Primary Outcomes: Independent Outdoor Activities, Spouse’s Worry, and PwD Irritability and Depressed Mood
Couple 1
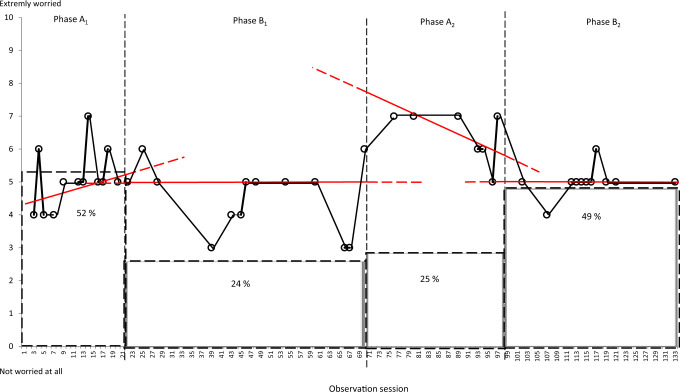
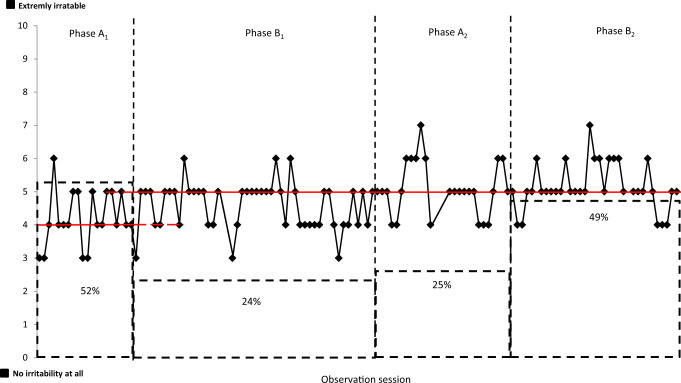
The percentage of days with independent outdoor activities for PwD 1 decreased from 52% in phase A1 to 24% in phase B1, remained stable during phase A2 (25%) and increased during phase B2 (49%; Table 2). Figure 1 shows spouse 1 worry concerning PwD 1 independent outdoor activities together with the percentage of days with PwD 1 independent outdoor activities during each phase. For spouse 1, the celeration line (red line in Figure 1) indicates a decrease in worry from A1 to B1. All except 1-point data point in phase B1 fell below the celeration line, indicating either an effect of the intervention or that the PwD 1 had fewer independent outdoor activities. The median for worry for spouse 1 increased from the first intervention phase (B1) to the second baseline phase (A2) and then decreased during the last intervention phase (B2). Person with dementia 1 irritability (proxy rating) showed little variability during all phases but increased during phase B1 (Figure 2); change in level and latency from A1 to B1 was observed, but no trend.
Table 2.
Outcome Results.
| Phase | A1 | B1 | A2 | B2 |
|---|---|---|---|---|
| Couple 1, weeks | 3 | 7 | 4 | 5 |
| Primary outcomes | ||||
| PwD independent outdoor activities, % | 11a/21 (52) | 12a/49 (24) | 7a/28 (25) | 17a/35 (49) |
| Spouse’s worry (Md, quartile) | 5, 4.5-5.5 | 5, 3.5-5 | 7, 6-7 | 5, 5-5 |
| PwD irritability (Md, quartile) | 4, 3.5-5 | 5, 4-5 | 5, 4.5-6 | 5, 5-6 |
| Secondary outcomes | ||||
| PwD well-being (proxy; Md, quartile) | 5, 5-6 | 5, 5-5 | 5, 5-5 | 5, 5-5 |
| PwD well-being (Md, quartile) | 5, 4-6 | 5, 5-5 | 5, 4-5 | 5, 4-5 |
| Spouse well-being (Md, quartile) | 5, 5-6 | 4, 4-5 | 5, 4-5 | 4, 4-5 |
| Additional outcomes | ||||
| Days with 2 or more independent outdoor activities | 0/21 | 0/49 | 1/28 | 0/35 |
| Independent outdoor activities (Md, quartile), minutes | 65, 62-70 | 60, 45-82 | 45, 27-107 | 60, 40-72 |
| Accompanied outdoor activities, n | 1 | 10 | 6 | 12 |
| Accompanied outdoor activities (Md, quartile), minutes | 45, - | 60, 39-70 | 40, 35-45 | 37, 32-41 |
| Generated alarms, n | 15 | 12 | ||
| Couple 2, weeks | 3 | 7 | 5 | 4, 3 |
| Primary outcomes | ||||
| PwD independent outdoor activities, % | 0a/21 (0) | 27a/49 (55) | 19a/35 (54) | 21a/30b (70) |
| Spouse’s worry (Md, quartile) | 0, 0-0 | 1, 0-0 | 0, 0-1 | 0, 0-0 |
| PwD depressed mood (Md, quartile) | 0, 0-2.5 | 0, 0-0 | 0, 0-0 | 0, 0-0 |
| Secondary outcomes | ||||
| PwD well-being (proxy; Md, quartile) | 10, 8-10 | 10, 10-10 | 10, 10-10 | 10, 10-10 |
| PwD well-being (Md, quartile) | 10, 10-10 | 10, 10-10 | 10, 10-10 | 10, 10-10 |
| Spouse well-being (Md, quartile) | 8, 6-10 | 10, 8-10 | 10, 10-10 | 10, 10-10 |
| Additional outcomes | ||||
| Days with 2 or more independent outdoor activities | 0/21 | 11/49 | 12/35 | 17/30b |
| Independent outdoor activities (Md, quartile), minutes | – | 40, 39-49 | 40, 30-40 | 40, 40-48 |
| Accompanied outdoor activities, n | 21 | 37 | 21 | 19 |
| Accompanied outdoor activities (Md, quartile), minutes | 75, 70-95 | 65, 40-75 | 75, 65-102 | 62, 52-67 |
| Generated alarms, n | 59 | 30 | ||
| Couple 3, weeks | 2 | 5 | 4 | 5 |
| Primary outcomes | ||||
| PwD independent outdoor activities, % | 6a/14 (43) | 31a/35 (88) | 15a/28 (54) | 27a/35 (77) |
| Spouse’s worry (Md, quartile) | 0, 0-0 | 0, 0-0 | 0, 0-0 | 0, 0-0 |
| PwD depressed mood (Md, quartile) | 0, 0-1.5 | 0, 0-0.5 | 0, 0-0 | 0, 0-0 |
| Secondary outcomes | ||||
| PwD well-being (proxy; Md, quartile) | 10, 9-10 | 9, 8.5-9 | 8, 8-9 | 9, 9-9 |
| PwD well-being (Md, quartile) | 10, 10-10 | 9, 8-9 | 8, 8-9 | 9, 9-9 |
| PwD own worry (Md, quartile) | 0, 0-0 | 0, 0-0 | 0, 0-0 | 0, 0-0 |
| Spouse well-being (Md, quartile) | 9.5, 9-10 | 9, 9-9 | 9, 8-9 | 9, 9-9 |
| Additional outcomes | ||||
| Days with 2 or more independent outdoor activities | 0/14 | 13/35 | 2/28 | 4/35 |
| Independent outdoor activities (Md, quartile), minutes | 40, 30-45 | 52, 42-55 | 40, 40-42 | 40, 40-43 |
| Accompanied outdoor activities, n | 5 | 7 | 5 | 9 |
| Accompanied outdoor activities (Md, quartile), minutes | 60, - | 35, 25-58 | 42, 38-100 | 65, 42-85 |
| Generated alarms, n | 31 | 24 | ||
Abbreviations: Md, mean deviation; PwD, person with dementia.
a Proportion of days with independent outdoor activities of the number of days on which estimations were made in the diary.
b The phases were 4 weeks and two days long.
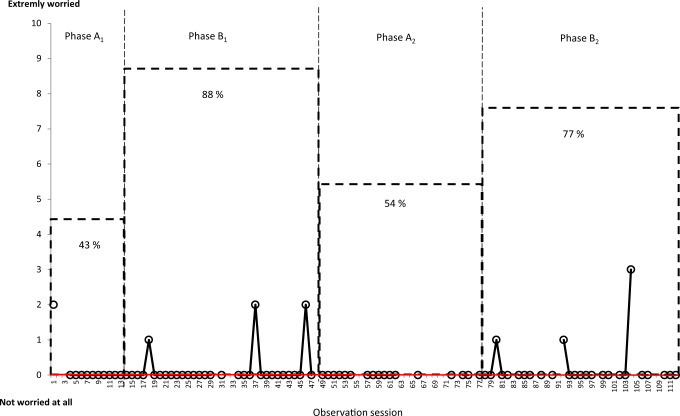
Figure 1.
Spouse 1 worry concerning PwD independent outdoor activities (O) and PwD 1 independent outdoor activities (%). PwD indicates person with dementia.
Figure 2.
Person with dementia (PwD) 1 irritability (proxy) and independent outdoor activities (%).
Couple 2
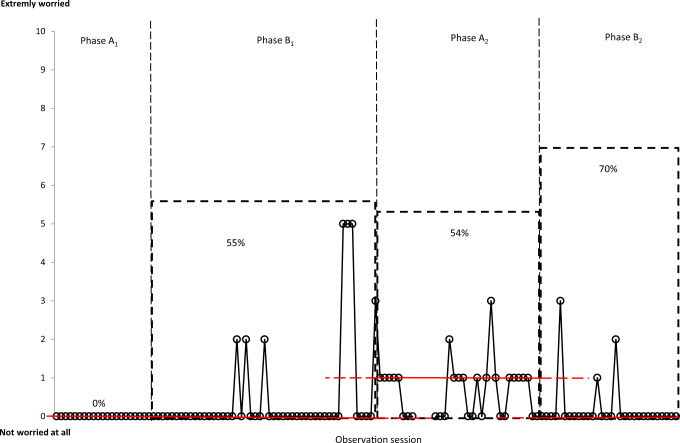
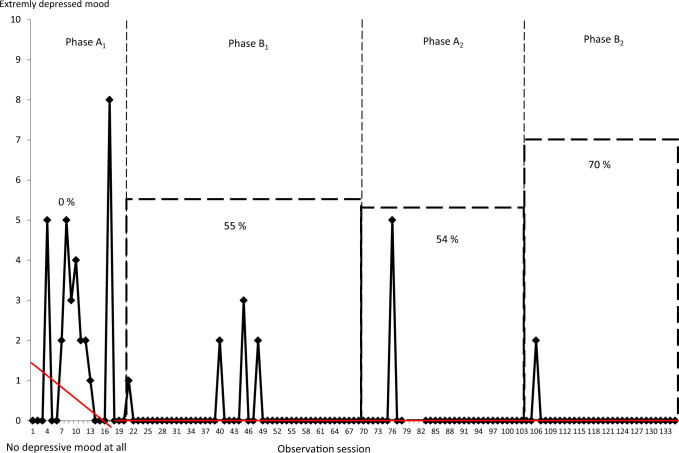
For PwD 2, the percentage of days with independent outdoor activities increased from 0% in phase A1 to 55% in phase B1. This frequency remained stable (54%) during phase A2 and further increased to 70% in phase B2 (Table 2). During phase A2, PwD 2 carried a cell phone when alone outdoors, and his walks between the home and the day care center were monitored by telephone calls between spouse 2 and center staff to communicate PwD’s departures and arrivals. Figure 3 shows data on spouse 2’s worries that her husband would get lost while alone outdoors, together with the percentage of days with PwD independent outdoor activities during each phase. In phase A1, during which PwD 2 performed no independent outdoor activities, spouse 2 reported no worry. When the intervention was introduced in phase B1, PwD 2 started performing independent outdoor activities with the support of the PPA in the third week, and spouse 2’s worries increased. In phase A2, when PwD 2’s independent outdoor activities were supported solely by the cell phone and telephone monitoring (see earlier), this was accompanied by increased spouse’s worry. Finally, a decrease in spouse’s worry was shown in phase B2, when 70% of days contained PwD independent outdoor activities. Person with dementia 2’s depressive mood (proxy) decreased over the whole study period. The celeration line (red line in Figure 4) indicates a decreasing trend of depressive mood for the PwD (proxy) from phase A1 to phase B1. Person with dementia 2 showed variability in depressive mood during phase A1; no changes in median, level, trend, or latency were observed.
Figure 3.
Spouse 2 worry concerning PwD independent outdoor activities (O) and PwD 2 independent outdoor activities (%). PwD indicates person with dementia.
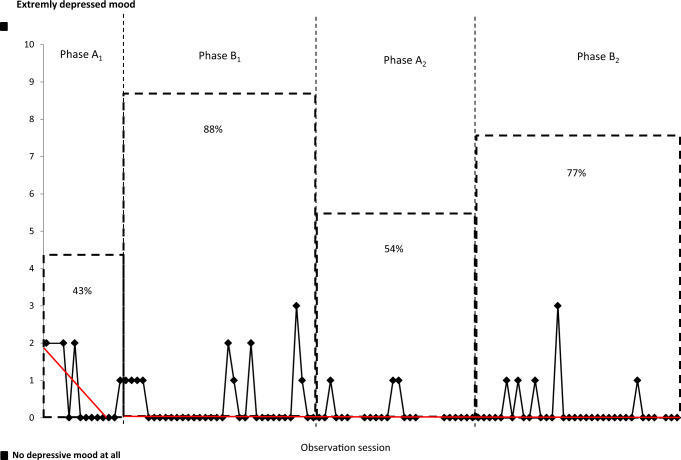
Figure 4.
Person with dementia (PwD) 2 depressive mood (proxy) and independent outdoor activities (%).
Couple 3
For PwD 3, an increased frequency of independent outdoor activities, from 43% to 88%, was shown during phase B1 (Table 2). An intervention effect was also demonstrated by a decreased percentage of days with independent outdoor activities when the intervention was withdrawn in phase A2 (54%). During phase B2, frequency of independent outdoor activities again increased to 77%. Figure 5 shows the data for spouse 3’s worries concerning PwD independent outdoor activities together with the percentage of days with independent outdoor activities for each phase. Spouse 3’s worries showed little variability during the study period (Figure 5). Depressive mood for PwD 3 (proxy) showed variability during the whole study period (Figure 6), but no changes in median, level, trend, or latency were observed.
Figure 5.
Spouse 3 worry concerning PwD independent outdoor activities (O) and PwD 3 independent outdoor activities (%). PwD indicates person with dementia.
Figure 6.
Person with dementia (PwD) 3 depressive mood (proxy) and independent outdoor activities (%).
Secondary Outcomes: Spouse and PwD Well-Being, PwD Self-Reported Outcomes, and Additional Outdoor Activity Variables
None of the PwDs performed independent outdoor activities more than once a day during the first baseline phase (A1). During the first intervention phase (B1), both PwD 2 and PwD 3 were independently outdoors 2, even 3 times a day (Table 2). The PwDs’ own ratings of well-being, depressed mood, irritability, and worry showed very little variability. The results for the primary and secondary outcomes are summarized and presented in Table 2.
Discussion
The present results show that access to a PPA consistently increased the independent outdoor activities of 2 PwDs. For 2 spouses, access to a PPA decreased the levels of worry about the PwDs’ independent outdoor activities, despite increased frequency of such activities. All couples in the present study had, in one way or another, come to a situation in which PwDs being alone outdoors was experienced by the PwDs and spouses as entailing a risk (cf 34 ). The 3 couples differed in their attitudes toward the PwDs’ possibility to continue independent outdoor activities and the couples could be seen as illustrating how these difficulties can be approached. In couple 1, the PwD was more active outdoors than the spouse was and refused to be restricted by his wife’s attempts to lock him indoors. Both spouses 2 and 3 had their own activities outside the home to a greater degree than did spouse 1 and worried that the PwD would get lost while being outdoors alone. Spouse 2 therefore locked the PwD in, which he accepted, while spouse 3 refrained from restricting her husband.
In couple 1, the interviews with the couple revealed PwD 1’s great need to be outdoors, and according to the spouse, not being allowed to go outdoors was causing him to become irritable and her to worry when the PwD was outdoors on his own. Scores on the NPI supported the spouse 1’s perception of irritability in the PwD 1. Quinn et al 35 revealed that caregivers’ perception of relationship quality was influenced negatively by the PwDs’ needs for help with ADL and by the severity of behavioral problems. Spouse 1’s worries decreased during the second intervention phase, and this might be related to the fact that the spouse had developed trust in the PPA as well as the knowledge, skills, and ability needed to use the device (cf 27 ). Previous research has shown that the intention to use and later actual use of new technology might be preceded by a stage of perceived usability. 36 Olsson et al 27 revealed that the value of a tracking technology, in terms of safety and security, was related to users’ possibility to test and evaluate the technology as well as to their own abilities, knowledge, and skills. Increased trust in the PPA during the second intervention period may also have contributed to the finding that PwDs’ independent outdoor activities increased during B2 for all 3 couples (cf 27 ).
Couple 2 took regular outdoor walks together, but spouse 2 did not want him to be alone outdoors. When spouse 2 had her own activities away from home, she felt compelled to lock PwD 2 indoors, which felt wrong but still necessary. However, PwD 2 accepted being locked in. In the present study, spouses 1 and 2 had tried to prevent the PwD from going outdoors alone in different ways, for example, by physically preventing him (standing in the way) and/or by locking the exterior door. Locked doors are commonly used in residential homes for PwDs to prevent them from leaving their homes, 37,38 and studies have also shown that relatives use this strategy in their own homes as a safety precaution for their own as well as for the PwD’s sake. 10,39 Following no independent outdoor activities for PwD 2 during the first baseline period, the couple carried the PPA with them on joint outdoor activities during the first weeks of the intervention period B1, which has been described as a way to achieve trust in the PPA. 27 During the third week of phase B1, PwD 2 engaged in his first independent outdoor activities, resulting in his wife scoring higher on worry that her husband would get lost while alone outdoors despite the PPA. During the second baseline period (A2), PwD 2 maintained the same frequency of independent outdoor activities with the support of him carrying a cell phone and telephone monitoring of his walks between the home and the day care center. Spouse 2 reported that this gave them both a feeling of safety and security (cf 27,40 ) and made it possible for her to engage in several daily independent activities outside the home, thus maintaining her freedom. Spouse 2 also reported somewhat increased worries during phase A2, which could be explained by the absence of the PPA. With use of the PPA, the door could be unlocked, improving the PwD’s depressed mood, and the spouse could be less worried and able to continue her own activities.
In couple 3, the spouse engaged in several of her own activities outside the home and on these occasions, PwD 3 was left alone at home. Spouse 3 did express worry about his safety but she did not lock him in as she felt that would be wrong. Although PwD 3’s independent outdoor activities increased during both intervention periods, no effect was found for spouse’s worry, PwD depressive mood, and PwD’s worry about getting lost. This was a surprising finding because both PwD 3 and spouse 3 had expressed being worried when the PwD was alone outdoors. Although spouse 3 reported very few neuropsychiatric symptoms for her husband and spent few hours a day supervising and supporting him in ADLs, she nevertheless reported being moderately burdened by caring for her husband. She described that she had already given up some desired activities and that her feeling of independence was limited, suggesting that her experience of care burden was related to perceived limitations in own activities. Earlier studies 13,14,41 have shown that taking care of a PwD tends to take precedence over the caregiving spouse’s own activities and hobbies, which are sacrificed.
Elderly persons and PwDs might, by the support of different kinds of technologies, have a possibility to remain living for a longer time in their own homes. However, the use of a PPA in the care of PwD needs to be introduced and used in relation to PwD’s and relatives’ problems, preferences, and needs.
Methodological Considerations
The main strengths of the present study are its structured daily measures and the A1B1A2B2 design with 2 baseline and 2 intervention phases, 26 which are believed to minimize or rule out potential threats to internal validity. The strength of the design was most obvious in couple 3, where a decrease in PwD’s independent outdoor activities was shown in phase A2 when the intervention was withdrawn. However, some limitations have been found. During some parts of the phases, the PwDs had few independent outdoor activities, thus resulting in few scores, which might have affected the results. For 2 couples (1 and 3), measures of the spouses’ worry related to the PwDs outdoor activities were missing for the days when the PwDs were not outdoors; for couple 2, the question regarding the spouse’s worry was formulated differently. The experimental single-case design is not intended to generate generalizable findings, instead this is an expressed limitation of the design. Inter-rater reliability was assessed by 2 authors (not the one who primary made the visual inspections) examining the graphs, followed by a discussion in the research group. Assessment of the PwDs’ cognitive competence using the Mini-Mental Score Examination (MMSE) was considered but rejected due to the researchers’ experienced difficulties with establishing a trustful relationship with PwDs after having examined them with MMSE (cf 42 ).
Conclusion
The present study demonstrated that the use of a PPA could provide support in daily life by allowing PwDs to engage in independent outdoor activities and decreasing their spouse’s worry related to these activities. The results from the present study may help designing a future randomized controlled group study to examine the effectiveness of a PPA for PwDs and their relatives.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the University of Gävle, Örebro University and by grants from The Dementia Association—The National Association for the Rights of the Demented as well as The Knowledge Foundation.
References
- 1. Detweiler MB, Murphy PF, Myers LC, Kim KY. Does a wander garden influence inappropriate behaviors in dementia residents? Am J Alzheimers Dis Other Demen. 2008;23(1):31–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Duggan S, Blackman T, Martyr A, Van Schaik P. The impact of early dementia on outdoor life. Dementia. 2008;7(2):191–204. [Google Scholar]
- 3. Gibson G, Chalfont GE, Clarke PD, Torrington JM, Sixsmith AJ. Housing and connection to nature for people with dementia. J Hous Elderly. 2007;21(3):55–72. [Google Scholar]
- 4. Cohen-Mansfield J, Golander H, Arnheim G. Self-identity in older persons suffering from dementia: preliminary results. Soc Sci Med. 2000;51(3):381–394. [DOI] [PubMed] [Google Scholar]
- 5. Edvardsson D, Fetherstonhaugh D, Nay R. Promoting a continuation of self and normality: person-centred care as described by people with dementia, their family members and aged care staff. J Clin Nurs. 2010;19(17-18):2611–2618. [DOI] [PubMed] [Google Scholar]
- 6. Rowe MA, Vandeveer SS, Greenblum CA, et al. Persons with dementia missing in the community: is it wandering or something unique? BMC Geriatr. 2011;11:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bowen ME, McKenzie B, Steis M, Rowe M. Prevalence of and antecedents to dementia-related missing incidents in the community. Dement Geriatr Cogn Disord. 2011;31(6):406–412. [DOI] [PubMed] [Google Scholar]
- 8. Rowe MA, Ahn H, Benito AP, Stone H, Wilson A, Kairalla J. Injuries and unattended home exits in persons with dementia: a 12-month prospective study. Am J Alzheimers Dis Other Demen. 2010;25(1):27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rasquin SMC, Willems C, de Vliger S, Geers RPJ, Soede M. The use of a technical devices to support outdoor mobility of dementia patients. Technol Disabil. 2007;19 (2/3):113–120. [Google Scholar]
- 10. Robinson L, Hutchings D, Corner L, et al. A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use. Health Technol Assess. 2006;10(26):iii, ix–108. [DOI] [PubMed] [Google Scholar]
- 11. Robinson L, Brittain K, Lindsay S, Jackson D, Olivier P. Keeping in touch everyday (KITE) project: developing assistive technologies with people with dementia and their carers to promote independence. Int Psychogeriatr. 2009;21(3):494–502. [DOI] [PubMed] [Google Scholar]
- 12. Namazi KH, Johnson BD. Pertinent autonomy for residents with dementias: modification of the physical environment to enhance independence. Am J Alzheimers Dis Other Demen. 1992;7(1):16–21. [Google Scholar]
- 13. Leong J, Madjar I, Fiveash B. Needs of family carer of elderly peoples with dementia living in the community. Australas J Ageing. 2001;20(3):133–138. [Google Scholar]
- 14. Quinn C, Clare L, Pearce A, van Dijkhuizen M. The experience of providing care in the early stages of dementia: an interpretative phenomenological analysis. Aging Ment Health. 2008;12(6):769–778. [DOI] [PubMed] [Google Scholar]
- 15. Shoval N, Auslander GK, Freytag T, et al. The use of advanced tracking technologies for the analysis of mobility in Alzheimer's disease and related cognitive diseases. BMC Geriatr. 2008;8:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bantry White E, Montgomery P, McShane R. Electronic tracking for people with dementia who get lost outside the home: a study of the experience of familial carers. Br J Occup Ther. 2010;73(4):152–159. [Google Scholar]
- 17. Landau R, Auslander GK, Werner S, Shoval N, Heinik J. Families' and professional caregivers' views of using advanced technology to track people with dementia. Qual Health Res. 2010;20(3):409–419. [DOI] [PubMed] [Google Scholar]
- 18. Lauriks S, Reinersmann A, Van der Roest HG, et al. Review of ICT-based services for identified unmet needs in people with dementia. Ageing Res Rev. 2007;6(3):223–246. [DOI] [PubMed] [Google Scholar]
- 19. Werner S, Auslander GK, Shoval N, Gitlitz T, Landau R, Heinik J. Caregiving burden and out-of-home mobility of cognitively impaired care-recipients based on GPS tracking. Int Psychogeriatr. 2012;24(11):1836–1845. [DOI] [PubMed] [Google Scholar]
- 20. Pot AM, Willemse BM, Horjus S. A pilot study on the use of tracking technology: feasibility, acceptability, and benefits for people in early stages of dementia and their informal caregivers. Aging Ment Health. 2012;16(1):127–134. [DOI] [PubMed] [Google Scholar]
- 21. Landau R, Auslander GK, Werner S, Shoval N, Heinik J. Who should make the decision on the use of GPS for people with dementia? Aging Ment Health. 2011;15(1):78–84. [DOI] [PubMed] [Google Scholar]
- 22. Miskelly F. A novel system of electronic tagging in patients with dementia and wandering. Age Ageing. 2004;33(3):304–306. [DOI] [PubMed] [Google Scholar]
- 23. Miskelly FG. Assistive technology in elderly care. Age Ageing. 2001;30(6):455–458. [DOI] [PubMed] [Google Scholar]
- 24. Oswald F, Wahl HW, Voss E, et al. The use of tracking technologies for the analysis of outdoor mobility in the face of dementia: first steps into a project and some illustrative findings from Germany. J Hous Elderly. 2010;24(1):55–73. [Google Scholar]
- 25. Aldridge D. Single case research designs for the clinician. J R Soc Med. 1991;84(5):249–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kazdin AE. Single-Case Research Designs—Methods for Clinical and Applied Settings. 2nd ed. New York: Oxford University Press, Inc.; 2011:452. [Google Scholar]
- 27. Olsson A, Engström M, Lampic C, Skovdahl K. A passive positioning alarm used by persons with dementia and their spouses—a qualitative intervention study. BMC Geriatr. 2013;13:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Elmstahl S, Malmberg B, Annerstedt L. Caregiver's burden of patients 3 years after stroke assessed by a novel caregiver burden scale. Arch Phys Med Rehabil. 1996;77(2):177–182. [DOI] [PubMed] [Google Scholar]
- 29. Wimo A, Nordberg G. Validity and reliability of assessments of time. comparisons of direct observations and estimates of time by the use of the resource utilization in dementia (RUD)-instrument. Arch Gerontol Geriatr. 2007;44(1):71–81. [DOI] [PubMed] [Google Scholar]
- 30. Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The neuropsychiatric inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44(12):2308–2314. [DOI] [PubMed] [Google Scholar]
- 31. Kaufer DI, Cummings JL, Ketchel P, et al. Validation of the NPI-Q, a brief clinical form of the neuropsychiatric inventory. J Neuropsychiatry Clin Neurosci. 2000;12(2):233–239. [DOI] [PubMed] [Google Scholar]
- 32. Parker RI, Vannest K. An improved effect size for single-case research: nonoverlap of all pairs. Behav Ther. 2009;40(4):357–367. [DOI] [PubMed] [Google Scholar]
- 33. Zhan S, Ottenbacher KJ. Single subject research designs for disability research. Disabil Rehabil. 2001;23(1):1–8. [DOI] [PubMed] [Google Scholar]
- 34. McShane R, Gedling K, Keene J, Fairburn C, Jacoby R, Hope T. Getting lost in dementia: a longitudinal study of a behavioral symptom. Int Psychogeriatr. 1998;10(3):253–260. [DOI] [PubMed] [Google Scholar]
- 35. Quinn C, Clare L, Woods B. The impact of the quality of relationship on the experiences and wellbeing of caregivers of people with dementia: a systematic review. Aging Ment Health. 2009;13(2):143–154. [DOI] [PubMed] [Google Scholar]
- 36. Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Quart. 2003;27(3):425–478. [Google Scholar]
- 37. Feng Z, Hirdes JP, Smith TF, et al. Use of physical restraints and antipsychotic medications in nursing homes: a cross-national study. Int J Geriatr Psychiatry. 2009;24(10):1110–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Meyer G, Kopke S, Haastert B, Muhlhauser I. Restraint use among nursing home residents: cross-sectional study and prospective cohort study. J Clin Nurs. 2009;18(7):981–990. [DOI] [PubMed] [Google Scholar]
- 39. Olsson A, Engstrom M, Skovdahl K, Lampic C. My, your and our needs for safety and security: relatives' reflections on using information and communication technology in dementia care. Scand J Caring Sci. 2011;26(1):104–112. [DOI] [PubMed] [Google Scholar]
- 40. Cedervall Y, Aberg AC. Physical activity and implications on well-being in mild Alzheimer's disease: a qualitative case study on two men with dementia and their spouses. Physiother Theory Pract. 2010;26(4):226–239. [DOI] [PubMed] [Google Scholar]
- 41. Vikstrom S, Josephsson S, Stigsdotter-Neely A, Nygard L. Engagement in activities: experiences of persons with dementia and their caregiving spouses. Dementia. 2008;7(2):251–270. [Google Scholar]
- 42. Bergland A, Kirkevold M. Thriving in nursing homes in Norway: contributing aspects described by residents. Int J Nurs Stud. 2006;43(6):681–691. [DOI] [PubMed] [Google Scholar]