Abstract
This study aimed to determine the specific correlation between indoor air temperature and agitation of nursing home residents with dementia. Agitated behaviors of 21 residents, living in 1 nursing home, were assessed for a 10-month period using the Cohen-Mansfield Agitation Inventory (CMAI). The CMAI Total Frequency scores were found to increase significantly when indoor average temperatures deviated from 22.6°C. In addition, cumulative exposure to temperatures higher than 26°C and lower than 20°C was linearly correlated with CMAI Total Frequency scores. Results showed that agitated behaviors not only affected the person manifesting them but were found to be disruptive for other residents and the delivery of care. Agitation can, therefore, be potentially reduced by limiting the range of indoor air temperature variations, and aged care providers should ensure that a thermally comfortable environment is provided in nursing homes to enhance comfort and well-being of all occupants.
Keywords: thermal environment, supportive living environment, nonpharmacological management of behavioral symptoms, behavioral and psychological symptoms of dementia, residential aged care facility, agitation
Introduction
Australia is experiencing a major demographic shift toward an older population. In 2015, over 3 569 000 people (15% of the entire population) were aged 65 years or more, and this number is projected to rapidly increase over the coming decades. 1 Although dementia is not seen as a normal part of aging, it does primarily affect older people, 2 and recent demographic projections indicate that the number of people with dementia in Australia will more than double in the coming 30 years. 3 In 2014, approximately 270 600 Australians lived in nursing homes, with over 50% of them diagnosed with dementia. 4 Dementia is one of the leading causes of institutionalization among older adults, 5,6 consequently, the demand for nursing home care is also projected to rise markedly. 7 However, the relocation of a person with the condition to a nursing home often do not help in reducing agitation. 8
It is commonly believed that on average the adult population spends between 80% and 90% of their day indoors. 9 This percentage is likely to be even higher among residents of nursing homes who depend heavily on the indoor environment to compensate for their decreasing vitality and sensory abilities. 10 People with dementia are very sensitive to indoor environmental conditions, 11 may be unable to filter out irrelevant sensory or cognitive information, 12 and may have difficulties in recognizing their needs or know how to actively adjust or interpret the environment around them. 13 Agitation may be a form of communication that they employ to express themselves or be an outcome of unaddressed needs. 14,15 Agitation not only affects the person who is manifesting such symptoms, but it also interferes with the provision of care and impacts on well-being of other residents 8 ; therefore, it is crucial to determine the causes of the behavior and what can be done to prevent it. 16
Over the recent decades, evidence from previous studies indicates that indoor environmental quality has a significant impact on quality of life (QOL) of residents. 14,17 -22 Hence, numerous design guidelines and recommendations have been published to help designers and aged care providers to upgrade and build better nursing homes. 21 As a result, many facilities accommodating people with dementia are now designed to provide appropriate levels of stimulation while reducing possible sources of confusion or distress for residents. Environmental factors such as acoustic and lighting comfort, home-like atmosphere, and architectural dementia-friendly design have all been found to be linked to a decrease in levels of agitation. 8,11,19,23 -27 Studies have also been conducted into the effect of indoor air contaminants on the well-being of nursing home residents, 9,28 while others have investigated the thermal comfort requirements of elderly people 29,30 and differences in perceptions of thermal comfort between young adults and the aged population. 17,31,32 It is widely believed that older people are more affected than younger adults when exposed to extreme indoor air temperatures. 22 However, to date uncertainty remains as to how people with dementia perceive their thermal environment and how thermal discomfort affects their health and well-being. 18,28 Garre-Olmo et al 33 provided empirical evidence that high indoor temperatures in nursing homes were associated with lower levels of QOL. In addition, Wong et al 18 found that cases of dysphoria and insomnia were more frequent with high indoor temperatures and anorexia with low indoor temperatures. Nevertheless, the specific impacts of thermal comfort on agitation in nursing homes is currently largely unknown. 34,35
As a result of the lack of knowledge on the link between thermal comfort and agitation, practical guidelines to help building designers optimize environmental conditions in dementia care facilities often do not address the provision of thermally comfortable conditions. 24 Consequently, it would appear that many nursing homes across Australia are not providing optimal comfort conditions for all occupants, 36 most likely because thermal comfort was often not considered to be a priority when the facilities were designed and built. Residents with dementia, in comparison to other occupants, are among those who are affected the most when their needs are ignored in the building design process. 14
This study, using an exploratory approach, aimed to gather quantitative evidence regarding the possible correlation between indoor air temperature and agitation of people with dementia. The hypothesis that exposure to excessively warm and/or cold indoor air temperatures was associated with high levels of frequency and disruptiveness of agitated behaviors raised the following research questions: (a) What were the spatial and temporal variations in indoor temperatures within the case study nursing home? and (b) Was cumulative exposure to warm and/or cold indoor air conditions correlated with an increase in agitation and agitated behaviors that are likely to be disruptive to other occupants?
Materials and Methods
The study was approved by the University of Wollongong human research ethics committee (HE14/478). Proxy consent was obtained in writing from caregivers and from the legal guardian of each resident.
Sample
In the present longitudinal prospective cohort study, people with dementia living in a particular facility were observed for a 10-month period. The inclusion criteria for the study were (a) the participant had been resident in the nursing home for at least 3 months, (b) the participant scored higher than 4 on the cognitive decline subject of the Psychogeriatric Assessment Scales (PAS), 37 and (c) a signed consent form was obtained from the legal guardian.
People moving to nursing homes may experience stress triggered by relocation, and this is likely to be higher in the first 3 months. 38 Hence, the period of residency criterion was included to reduce the probability that agitation was caused by relocation. The PAS is a cognitive screening tool routinely used in Australian nursing homes to assess the level of cognitive functioning; total scores range from 0 to 21 and higher total scores indicate higher cognitive impairment. A PAS score higher than 4 was necessary for inclusion since Jorm et al 37 found that 80% of people who score higher than 4 in the PAS had dementia. The PAS assessments were administered by registered nurses prior to beginning of data collection and all participants in this study scored 10 or higher. Since residents were unable to give informed consent for their inclusion in the study, consent was obtained from their legal guardian. We obtained 21 signed consent forms, and all consented residents met the other 2 selection criteria.
Case Study Facility
The study was conducted in a nursing home located in the Illawarra region, New South Wales, Australia. The external walls of the facility were double brick and were not insulated. The building had a tiled hip roof with a 10-cm cellulose insulation layer that was installed immediately above the ceilings. Windows were single glazed, without draught seals, with metallic frames, and a substantial fraction of the windows were openable by occupants. There were 10 rooms with 4 beds each, 5 double bedrooms, and 4 single bedrooms. Only the dining room and the physiotherapy room were equipped with reverse cycle air-conditioning units (providing both cooling and heating), while other rooms were heated in cooler months by hydronic wall radiators. The hydronic gas-fired central heating system, which was manually turned on and off by the maintenance team, did not include local thermostat control that could regulate the heating output delivered to individual rooms.
Data Collection
Data were collected on (a) agitated behaviors, (b) indoor air temperature, and (c) time spent by each resident in various locations throughout the nursing home. Data collection started in March 2015 and ended in December 2015.
Agitated behaviors
The Cohen-Mansfield Agitation Inventory (CMAI) was used to assess agitated behaviors. 39 The CMAI is an informant rating questionnaire used to score frequency and disruptiveness of 29 agitated behaviors over a 14-day period. The CMAI has a 9-point frequency scale and a 6-point disruptiveness scale. Frequency scores range from 1 to 9, with 1 denoting never to 7 denoting several times an hour; 8 and 9 denote would occur if not prevented and not applicable, respectively. Disruptiveness scores range from 1 to 5, with 1 denoting not at all to 5 denoting extremely; a score of 9 denotes not applicable. Personal care assistants, blinded to the study aim, were trained individually by a psychologist for approximately an hour and they were provided with a copy of the CMAI prior to completing the questionnaires. The CMAI were administered face-to-face, in a quite area of the facility, by a trained research assistant who ensured that caregivers were completing each questionnaire with sufficient attention. One CMAI per resident was collected every fortnight. When a score equal to 8 or 9 was recorded, it was substituted with the average score that the resident received for that specific behavior during the whole research period. 40
Indoor air temperature
Indoor air temperature (dry-bulb) was measured and logged using 24 iButton. 41 The iButtons (Maxim Integrated) were small, cylindrical data logging devices 17.5 mm in diameter and 6 mm deep. These devices were able to measure and store dry-bulb air temperature at 15-minute intervals with an accuracy of ±0.5°C, ranging from −40°C up to 85°C, complying with the requirements of the International Organization for Standardization (ISO) 7726:1998 standard. 42 The devices were installed on internal walls using thick adhesive tape at the approximate chest height of occupants (0.6 m sitting/reclining, 1.1 m standing) where possible, as suggested by ISO 7726:1998. The specific height of the device in each room was selected based on the most common type of activity and body position of the participants therein. The temperature sensor in the iButton was encased in a polished metal capsule to reduce the effects of thermal radiation, they were not exposed to solar radiation, or radiation from neighboring heat sources, and were not installed above radiators or under air conditioners.
Location of the resident
After completing each CMAI, caregivers were asked to complete a 24-hour time chart in which they reported the location where the resident had spent the majority of time during each hour of a typical day during a given fortnightly observation period.
Analytical Strategy
Temperature data analysis
Two indices were developed to characterize the thermal environment experienced by participants by combining temperature data with the reported location of each resident throughout the nursing home, that is, (a) the average indoor air temperature to which each resident was exposed over each fortnightly observation period and (b) the cumulative percentage of time that each resident was exposed to temperatures outside a comfort range from 20°C to 26°C, as recommended in Annex A of the ISO 7730:2005 standard. 43 It should be noted that guidelines from ISO 7730:2005 were used since at the time of writing the Australian residential aged care Accreditation Standards did not specify indoor temperature requirements for nursing homes.
Agitation data
The CMAI data were highly correlated since repeated observations were made of each resident. A multilevel analysis (also known as mixed model or hierarchical model) was used because of its suitability for the analysis of correlated data which have a hierarchical structure, and multilevel models can handle different numbers of observations within and between participants. 44 Observations were clustered by residents, and residents were clustered by observers. Data analysis was carried out using the Mixed Model procedure in IBM SPSS Statistics (version 21.0). 45
The CMAI data were postprocessed to provide an overall characterization of each participant’s behavior, for a given 2-week observation period, through the following 2 derived indices: (a) the “CMAI Total Frequency” score, a measure of the overall frequency of observed manifestations of agitation, defined as the sum of all 29 individual frequency scores and (b) the “CMAI Overall Disruptiveness” score, a combined measure of frequency and intensity of disruptive behaviors, defined as the sum of the individual products of frequency and respective disruptiveness scores for each of the 29 items for each participant.
Three separate statistical models were used to answer the research questions. The first model examined the correlation between average indoor air temperature and CMAI Total Frequency scores. The second model examined the specific impact that cumulative exposure to temperatures outside the comfort temperature range had on agitated behaviors. The third model examined how disruptive agitation was for other occupants. The goodness of fit achieved by adding 1 parameter at a time to the model was determined by testing the difference in 2 log-likelihood values against a χ2 distribution. A 2-tailed P value of .05 was adopted as the standard for significance testing. The maximum likelihood method was selected as the estimation method since this is claimed to produce more accurate estimates of fixed regression parameters. 44 Data were examined to check that the assumptions of normality of the residuals and homoscedasticity were met for each model. The CMAI data were positively skewed and the assumption of normality of the residuals was not met. We therefore decided to transform the dependent variable in all 3 models. 44 In the first 2 statistical models, the dependent variable was transformed using the negative reciprocal function, −1/y. The reciprocal transformation changes the order among values, making the largest value the smallest. Thus, the negative reciprocal function was used to preserve the order among the values. While in the third model the dependent variable was transformed using the natural logarithmic function. By transforming the dependent variable, we were able to demonstrate that each model met the test assumptions.
Results
Indoor air temperature varied significantly as a function of both space and time during the research period. The highest indoor dry-bulb air temperature recorded was 33.6°C in a bedroom during a period of hot weather on November 18, 2015, when the outdoor temperature reached 37.3°C. The main causes of such high indoor air temperatures were thought to be the relatively low thermal resistance of the building envelope (wall, windows, floor, and ceiling/roof) and the absence of air-conditioning systems in some rooms. Occupant also affected indoor air temperatures to some extent; for example, during the warm weather in some occasions windows were found to be open even in unoccupied rooms, allowing hot outdoor air to enter and overheat the interior of the building.
The lowest indoor temperature recorded was 16.2°C in a corridor for 3 consecutive mornings in May 2015. The main cause of the low temperatures at these times was the absence of a localized control system to regulate the heating provided to individual rooms. This was also the main cause of overly warm indoor temperatures during the heating season, for example, on June 9 the outdoor temperature reached 22.4°C but the unregulated heating system led to indoor temperatures as high as 26.6°C. Figure 1 shows the percentage of time that each temperature range occurred in the facility for different room types.
Figure 1.

Percentage of time that each temperature range occurred in the facility. Locations are grouped by room type and temperature data are grouped by season.
Characteristics of the Sample of Participants
A total of 330 CMAI forms were collected. Five participants passed away during the research project and agitation data from the fortnight prior to their passing away were not included in the present analysis; therefore, not all the participants were observed the same number of times. Table 1 shows the characteristics of the sample, including the number of times agitation was assessed for each participant and mean, minimum, and maximum CMAI Total Frequency scores.
Table 1.
Characteristics of the Sample of Participants.
| PAS Score | Clinical Characteristic | Age | CMAI Total Frequency Scores | |||
|---|---|---|---|---|---|---|
| Number of Observations | Mean (SD) | Min | Max | |||
| Females | ||||||
| 16-21 | Alzheimer’s disease/depression | 88 | 15 | 49.1 (19.7) | 31 | 94 |
| 10-15 | Alzheimer’s disease | 67 | 18 | 78.8 (27.5) | 38 | 131 |
| 10-15 | Alzheimer’s disease/depression | 88 | 19 | 40.4 (5.4) | 34 | 57 |
| 16-21 | Alzheimer’s disease/depression | 88 | 19 | 47.9 (5.3) | 41 | 61 |
| 16-21 | Other dementia | 61 | 19 | 36.1 (5.6) | 29 | 47 |
| 16-21 | Alzheimer’s disease/depression | 86 | 20 | 36.7 (10.1) | 29 | 72 |
| 10-15 | Alzheimer’s disease | 86 | 20 | 50.7 (11.3) | 33 | 76 |
| Males | ||||||
| 16-21 | Alzheimer’s disease/depression | 75 | 3 | 35.7 (0.6) | 35 | 36 |
| 10-15 | Other dementia | 92 | 5 | 46.8 (8.0) | 38 | 57 |
| 16-21 | Alzheimer’s disease | 82 | 7 | 78.6 (25.7) | 50 | 111 |
| 16-21 | Alzheimer’s disease/depression | 88 | 7 | 41.1 (6.7) | 35 | 53 |
| 16-21 | Other dementia | 77 | 13 | 46.1 (4.5) | 36 | 54 |
| 10-15 | Alzheimer’s disease/depression | 81 | 15 | 42.5 (8.4) | 29 | 64 |
| 16-21 | Alzheimer’s disease | 86 | 17 | 39.4 (5.7) | 34 | 58 |
| 16-21 | Vascular dementia/depression | 82 | 18 | 62.5 (27.8) | 29 | 125 |
| 16-21 | Other dementia | 70 | 18 | 71.9 (27.5) | 29 | 132 |
| 16-21 | Vascular dementia | 82 | 18 | 80.7 (27.7) | 47 | 134 |
| 16-21 | Alzheimer’s disease | 88 | 19 | 44.5 (10.5) | 34 | 70 |
| 16-21 | Alzheimer’s disease/depression | 82 | 20 | 41.7 (11.1) | 31 | 72 |
| 16-21 | Other dementia | 73 | 20 | 40.7 (8.6) | 31 | 67 |
| 16-21 | Vascular dementia | 82 | 20 | 36.7 (4.7) | 33 | 49 |
Abbreviations: PAS, Psychogeriatric Assessment Scales; CMAI, Cohen-Mansfield Agitation Inventory.
Agitated Behaviors and Indoor Average Temperatures
A multilevel model was used to analyze the relationship between indoor average temperatures at which each resident was exposed over each fortnight and CMAI Total Frequency scores, and results are presented in Table 2. The trends in the data were best described by a second-order polynomial regression equation, and CMAI Total Frequency scores were found to significantly (P < .01) increase when average indoor air temperature deviated from 22.6°C. The dependent variable (y) was transformed using the negative reciprocal function, −1/y. It should be noted that to facilitate the interpretation of the intercept coefficient in the results the independent variable was centered on the overall average mean temperature for all observations, that is, 23.5°C.
Table 2.
Estimated Fixed Effects and Covariance Parameters for the Statistical Model of the Impact of Average Temperatures to Which Each Resident Was Exposed Over Each Fortnight on CMAI Total Frequency Scores.
| Estimates of Fixed Effectsa | |||||||
|---|---|---|---|---|---|---|---|
| Parameter | Estimate | Std. Error | df | t | Sig. | 95% Confidence Interval | |
| Lower Bound | Upper Bound | ||||||
| Intercept | −0.0214 | 0.00144 | 17.82 | −14.9 | 0.000 | −0.024440 | −0.0184 |
| Average temperature (centered) | 0.000709 | 0.000230 | 313.01 | 3.09 | 0.002 | 0.000257 | 0.00116 |
| [Average temperature (centered)]2 | 0.000380 | 0.000114 | 306.98 | 3.33 | 0.001 | 0.000155 | 0.000604 |
| Estimates of Covariance Parametersa | |||||||
| Parameter | Estimate | Std. Error | Wald Z | Sig. | 95% Confidence Interval | ||
| Lower Bound | Upper Bound | ||||||
| Residual | 0.0000133 | 0.00 | 12.22 | 0.000 | 0.0000113 | 0.0000156 | |
| Intercept (paricipant = resident) | Variance | 0.00000670 | 0.00 | 2.49 | 0.013 | 0.00000305 | 0.0000147 |
| Intercept (participant = caregiver) | Variance | 0.0000203 | 0.00 | 2.28 | 0.022 | 0.00000860 | 0.0000479 |
Abbreviation: CMAI, Cohen-Mansfield Agitation Inventory.
aDependent variable: −1/(CMAI Total Frequency score).
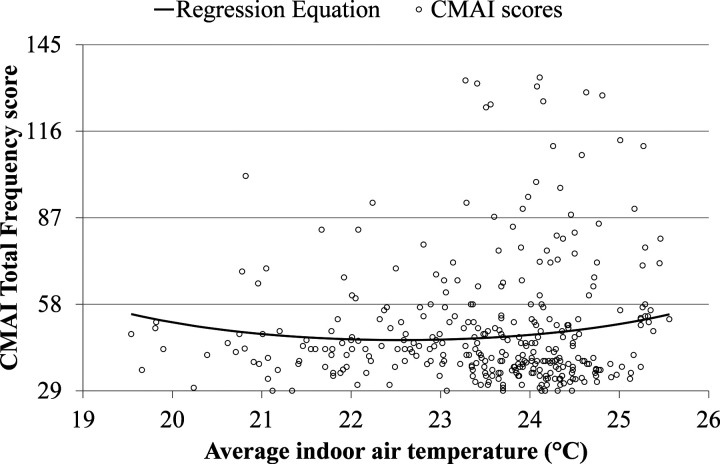
Figure 2 shows the CMAI Total Frequency scores plotted against the average indoor air temperature experience by each participant. (The best fit regression curves in Figures 2, 3, and 4 were plotted using the coefficients estimated by the multilevel models).
Figure 2.
CMAI Total Frequency scores determined for each resident plotted against the average temperature that the resident was likely to be exposed to over a given 2-week observation period. CMAI indicates Cohen-Mansfield Agitation Inventory.
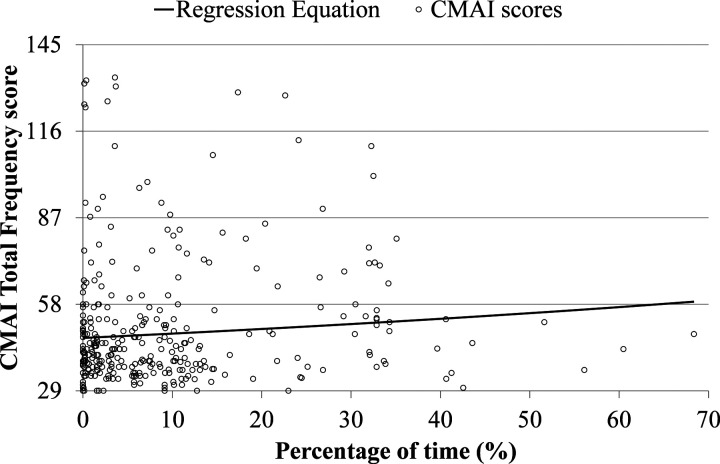
Figure 3.
CMAI Total Frequency scores plotted against the cumulative percentage of time that temperatures were outside the comfort range during each fortnight of observations for each participant. CMAI indicates Cohen-Mansfield Agitation Inventory.
Cumulative Exposure to Temperatures Lower Than 20°C and Higher Than 26°C
A second analysis was carried out to determine the specific relationship between the CMAI Total Frequency scores and the cumulative percentage of time that residents were exposed to temperatures lower than 20°C and higher than 26°C. As in the previous model, the dependent variable (y) was transformed using the negative reciprocal function, −1/y.
A linear best fit of the data to the model was determined. The cumulative percentage of time at which residents were exposed to temperatures outside the comfort temperature range significantly predicted CMAI Total Frequency scores. Table 3 provides a summary of the outputs from the multilevel analysis.
Table 3.
Estimated Fixed Effects and Covariance Parameters for the Statistical Model of the Impact of Cumulative Exposure to Temperatures Lower Than 20°C and Higher Than 26°C During Each Fortnight on CMAI Total Frequency Scores.
| Estimates of Fixed Effectsa | |||||||
|---|---|---|---|---|---|---|---|
| Parameter | Estimate | Std. Error | df | t | Sig. | 95% Confidence Interval | |
| Lower Bound | Upper Bound | ||||||
| Intercept | −0.0214 | 0.00144 | 17.59 | −14.9 | 0.000 | −0.0245 | −0.0184 |
| %Time outside comfort temperature range | 0.0000646 | 0.0000182 | 305.09 | 3.55 | 0.000 | 0.000029 | 0.000100 |
| Estimates of Covariance Parametersa | |||||||
| Parameter | Estimate | Std. Error | Wald Z | Sig. | 95% Confidence Interval | ||
| Lower Bound | Upper Bound | ||||||
| Residual | 0.0000134 | 0.00000109 | 12.22 | 0.000 | 0.0000114 | 0.0000157 | |
| Intercept (participant = resident) | Variance | 0.00000655 | 0.00000264 | 2.48 | 0.013 | 0.00000297 | 0.00001444 |
| Intercept (participant = caregiver) | Variance | 0.0000204 | 0.00000894 | 2.28 | 0.023 | 0.00000863 | 0.00004817 |
Abbreviation: CMAI, Cohen-Mansfield Agitation Inventory.
aDependent variable: −1/(CMAI Total Frequency score).
Figure 3 shows the CMAI Total Frequency scores plotted against the cumulative percentage of time at which temperatures outside the comfort range were recorded over each fortnight.
Relationship Between Behaviors Disruptiveness and Indoor Average Temperatures
A third multilevel model was used to determine how disruptive were agitated behaviors, caused specifically by thermal discomfort, for other occupants. The CMAI Overall Disruptiveness score was transformed using natural logarithmic function and was entered in the model as the dependent variable. The independent variable was centered using the average temperature mean value (23.5°C). The trend in the data was best described by a second-order polynomial regression equation. The CMAI Overall Disruptiveness scores were found to increase significantly when average temperatures deviated from 22.5°C, leading to similar results as those obtained via the first analysis. Table 4 shows the outputs from the multilevel analysis.
Table 4.
Estimated Fixed Effects and Covariance Parameters for the Statistical Model of the Impact of Average Indoor Air Temperatures on CMAI Overall Disruptiveness Scores.
| Estimates of Fixed Effectsa | |||||||
|---|---|---|---|---|---|---|---|
| Parameter | Estimate | Std. Error | df | t | Sig. | 95% Confidence Interval | |
| Lower Bound | Upper Bound | ||||||
| Intercept | 4.58 | 0.16 | 17.96 | 28.24 | 0.000 | 4.24 | 4.92 |
| Average temperature (centered) | 0.0839 | 0.0246 | 311.92 | 3.41 | 0.001 | 0.0354 | 0.1324 |
| [Average temperature (centered)]2 | 0.0415 | 0.0122 | 306.09 | 3.39 | 0.001 | 0.0174 | 0.0656 |
| Estimates of Covariance Parametersa | |||||||
| Parameter | Estimate | Std. Error | Wald Z | Sig. | 95% Confidence Interval | ||
| Lower Bound | Upper Bound | ||||||
| Residual | 0.153 | 0.013 | 12.21 | 0.000 | 0.130 | 0.180 | |
| Intercept (participant = resident) | Variance | 0.087 | 0.034 | 2.56 | 0.011 | 0.040 | 0.187 |
| Intercept (participant = caregiver) | Variance | 0.257 | 0.112 | 2.31 | 0.021 | 0.110 | 0.602 |
Abbreviation: CMAI, Cohen-Mansfield Agitation Inventory.
aDependent variable: ln(CMAI Overall Disruptiveness score).
Figure 4 shows the CMAI Overall Disruptiveness scores plotted against the average indoor air temperature that each resident was estimated to have been exposed to during each fortnight.
Figure 4.
Total CMAI Overall Disruptiveness scores plotted against the cumulative percentage of time that temperatures were outside the comfort range during each fortnight of observations for each participant. CMAI indicates Cohen-Mansfield Agitation Inventory.
Discussion
Agitated behaviors are frequently observed in residents, especially in those with dementia, and are one of the most challenging management problems in nursing homes. 20 Data on the care needs of permanent residents in subsidized Australian residential aged care places indicate that 87% of the residents with dementia needed a high level of care and that about 62% of them scored the highest possible rating in the “behavior characteristic” domain of the Aged Care Funding Instrument 3 ; which is a tool used to assess the status of people living in nursing homes. Residents with dementia were scoring almost 3 times higher in the behavior characteristic domain than other residents. 3 Therefore, to improve the quality of care delivered and the QOL of residents, it is essential to control environmental factors that may be the cause of agitated behaviors. 24 Agitation not only affects the person manifesting the behaviors, but it has also been found to be disruptive to other buildings occupants. 46
Results of the present study showed that the heating and cooling systems in the case study facility were not able to fully control indoor air temperature throughout the facility, and temperatures as low as 16.2°C and as high as 33.6°C were recorded during the study period. In nursing homes generally, both cold and hot indoor temperatures should be avoided because they may impact health and well-being of residents, potentially leading to hypothermia, hyperthermia, and an increasing the risk of illness and death. 47 -52
The CMAI Total Frequency scores increased when residents were exposed to either relatively cold or warm indoor temperatures at a statistically significant level. The best fit of the model was obtained using a quadratic function with a global minimum at 22.6°C. The estimated CMAI Total Frequency score was 6.0 points higher when the average indoor temperature was 20.0°C and 5.3 points higher when the average indoor temperature was 25.0°C. These results may be compared with the effects of medication used for the treatment of behavioral disturbance in dementia. For example, a study conducted on agitated nursing home residents with dementia showed that across 3 randomized controlled trials risperidone significantly decreased the average CMAI score of the treatment group versus the control group: weighted mean difference = −3.00 points, 95% CI (−4.22 to −1.78), P < .00001. 53 At the time of the study, risperidone was among the most frequently prescribed antipsychotic drugs in Sydney for treatment of behavioral disturbances in patients with dementia. 54 Enhancing the thermal comfort conditions for such patients may therefore have a comparable or greater effect than risperidone in decreasing agitation. Thus, the provision of good “thermal care” 28 could be classified as an effective nonpharmacological approach to the reduction of behavioral disturbances.
Agitation in the present study was also significantly correlated with the amount of hours that residents were exposed to temperatures higher than 26°C and lower than 20°C and disruptiveness significantly decreased when the average indoor air temperature was approximately 22.5°C.
Exposure of residents to temperatures outside the comfort temperature range not only has an impact on the manifestation and disruptiveness of agitated behaviors, it also potentially affects their health. Dementia can impair people’s perception of their environment, suffering threshold, and physiological defense mechanisms. 55 People with dementia are more vulnerable to heat stress because of the potential for dysfunctional thermoregulatory mechanisms, chronic dehydration, and the use of medications. 28,49 The World Health Organization suggests that a minimum air temperature of at least 20°C be maintained in indoor environments for people with special requirements, to avoid the possibility of their body temperature decreasing, potentially leading to hypothermia. 52 Therefore, the heating and cooling systems in nursing homes should be designed to accurately control temperature within the appropriate comfort temperature range and imply that caregivers should be trained to provide thermal care. Caregivers should not only be responsible for controlling the temperature in the building but also help residents, who may not have the ability to do so, to perform behavioral thermal adjustments (e.g. consuming hot or cold drinks, adjusting clothing insulation throughout the day, opening and closing windows, turning ceiling fans on and off).
Moreover, when hot and cold temperatures occur at the facility, it is likely that caregivers would have to deal with an increasing level of agitation in residents while themselves working in a potentially uncomfortable environment, which would likely have a negative impact on their productivity. 34 Thus, enhancing thermal comfort conditions may improve both staff productivity and the quality of care that residents receive.
Limitations
Firstly, perception of thermal comfort is influenced by 6 main factors: metabolic rate, clothing insulation, air temperature, mean radiant temperature, air speed, and relative humidity. 56 However, only the influence of air temperature was studied in the present work. Secondly, the number of participants involved in the research was limited and they were all living in the same nursing home. Thirdly, residents positions indoor were determined by asking caregivers to recollect where each resident had spent the majority of time during each hour of a typical day during a given fortnightly observation period and were not precisely determined using an indoor positioning system.
Conclusions
Indoor air temperatures recorded in the case study nursing home during the present study were found to range between 16.2°C and 33.6°C, exposing residents and caregivers to temperatures that could potentially affect not only their behaviors but also their health. The main causes of such significant temperature variations were thought to be the relatively poor thermal performance of the building envelope (e.g. wall, windows, floor, and ceiling/roof), the absence of air-conditioning systems in some areas, and the absence of an adequate control system, including localized control to regulate the heating output delivered to individual rooms. Occupants also influenced indoor air temperatures through their control of openable windows. For example, during warmer weather occupants sometimes opened windows to ventilate the building with fresh air, but on occasion this led to overheating if outdoors temperatures were high. On the other hand, the air-conditioning systems, when present and properly operated, were capable of maintaining indoor temperatures within recommended limits.
The present study also provided quantitative evidence regarding the specific impact that the thermal environment had on the manifestation of agitated behaviors in residents with dementia. This new research has contributed to a better understanding of the way in which the indoor thermal environment influences behavioral and psychological symptoms of patients with dementia. Results from the present study have highlighted that the exposure of residents to temperatures outside the comfort range did not only have a negative impact on their comfort but also negatively affected their behaviors. The manifestation and disruptiveness of agitated behaviors increased when residents were exposed to either relatively cold or warm indoor temperatures at a statistically significant level. Manifestation of agitated behaviors was also statistically significantly correlated with the amount of hours that residents were exposed to temperatures higher than 26°C and lower than 20°C.
The provision of good thermal care could be classified as an effective nonpharmacological approach to the reduction of behavioral disturbances in people with dementia living in nursing homes.
For policy makers, aged care providers, and building designers, this study has clear and important implications. Nursing homes should be built and operated so as to focus on the needs of occupants and should provide comfortable indoor thermal conditions each day and throughout the year. Minimum prerequisites regarding thermal comfort in nursing homes should be set and specific guidelines developed to help aged care providers to better understand how to operate their buildings. Staff members should also be trained in how to provide good thermal care, for example, to maintain a comfortable indoor environment at all times and to help those residents who cannot carry out their own thermally adaptive strategies.
More research in this area is needed to determine the optimal temperature range to be maintained in nursing homes and to investigate the impacts that other thermal comfort factors have on behavioral and psychological symptoms of dementia. It is also hoped that future work might involve a larger sample of participants from nursing homes of different types, in a range of different climatic conditions, so as to provide more statistically robust and widely applicable conclusions.
Acknowledgments
We would like to thank the University of Wollongong and Warrigal for financially supporting this research, the University of Wollongong statistical consulting service for the provision of advice on the analysis of the data, and the Warrigal caregivers who actively participated in this research project.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a joint partnership scholarship to the first author by the University of Wollongong (UOW), and the aged care provider Warrigal.
References
- 1. Australian Bureau of Statistics. Australian demographic statistics. Aust Demogr Stat. Canberra: Australian Bureau of Statistics; 2015:1–64. [Google Scholar]
- 2. World Health Organization. WHO|Dementia. http://www.who.int/mediacentre/factsheets/fs362/en/. Updated 2015. Accessed March 23, 2015.
- 3. Australian Institute of Health and Welfare. Dementia in Australia. Canberra: Australian Institute of Health and Welfare; 2012. [Google Scholar]
- 4. Australian Institute of Health and Welfare. Dementia. 2015. http://www.aihw.gov.au/dementia/. Updated 2015. Accessed January 11, 2016.
- 5. Sommer OH. Agitation in Patients With Dementia—Challenges in Diagnosis and Treatment. Oslo, Norway: Faculty of Medicine, University of Oslo; 2010. [Google Scholar]
- 6. Allen-Burge R, Stevens A, Burgio LD. Effective behavioural interventions for decreasing dementia-related challenging behaviour in nursing homes. J Geriatr Psychiatry. 1999;14(3):213–228. doi:10.1002/(SICI)1099-1166(199903)14. [PubMed] [Google Scholar]
- 7. Aged Care Financing Authority. Fourth Report on the Funding and Financing of the Aged Care Sector. Aged Care Financing Authority; 2016. [Google Scholar]
- 8. Joosse LL. Do sound levels and space contribute to agitation in nursing home residents with dementia? Res Gerontol Nurs. 2012;5(3):174–184. doi:10.3928/19404921-20120605-02. [DOI] [PubMed] [Google Scholar]
- 9. Mendes A, Bonassi S, Aguiar L, et al. Indoor air quality and thermal comfort in elderly care centers. Urban Clim. 2015;14(3):486–501. doi:10.1016/j.uclim.2014.07.005. [Google Scholar]
- 10. van Hoof J, Kort HSM. Supportive living environments: a first concept of a dwelling designed for older adults with dementia. Dementia. 2009;8(2):293–316. doi:10.1177/1471301209103276. [Google Scholar]
- 11. van Hoof J, Kort HSM, Duijnstee MSH, Rutten PGS, Hensen JLM. The indoor environment and the integrated design of homes for older people with dementia. Build Environ. 2010;45(5):1244–1261. doi:10.1016/j.buildenv.2009.11.008. [Google Scholar]
- 12. Perriol MP, Dujardin K, Derambure P, et al. Disturbance of sensory filtering in dementia with Lewy bodies: comparison with Parkinson’s disease dementia and Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2005;76(1):106–108. doi:10.1136/jnnp.2003.035022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cohen-Mansfield J. Conceptualization of agitation: results based on the Cohen-Mansfield Agitation Inventory and the Agitation Behavior Mapping Instrument. Int Psychogeriatr. 1996;8(suppl 3):309–315; discussion 351-354. doi:10.1017/S1041610297003530. [DOI] [PubMed] [Google Scholar]
- 14. van Hoof J, Kort HSM, Hensen JLM, Duijnstee MSH, Rutten PGS. Thermal comfort and the integrated design of homes for older people with dementia. Build Environ. 2010;45(2):358–370. doi:10.1016/j.buildenv.2009.06.013. [Google Scholar]
- 15. Hayne MJ, Fleming R. Acoustic design guidelines for dementia care facilities. In: Proceedings of 43rd International Congress on Noise Control Engineering: Internoise2014. Australia: Australian Acoustical Society; 2014:1–10. http://ro.uow.edu.au/smhpapers/2640 [Google Scholar]
- 16. Cohen-Mansfield J, Martin LS. Assessment of agitation in older adults. In: Lichtenberg PA, ed. Handbook of Assessment in Clinical Gerontology. 2nd ed, San Diego, CA: Academic Press; 2010:381–403. doi:10.1016/B978-0-12-374961-1.10015-6. [Google Scholar]
- 17. van Hoof J, Hensen JLM. Thermal comfort and older adults. Gerontechnol J. 2006;4(4):223–228. [Google Scholar]
- 18. Wong JKW, Skitmore M, Buys L, Wang K. The effects of the indoor environment of residential care homes on dementia suffers in Hong Kong: a critical incident technique approach. Build Environ. 2014;73:32–39. doi:10.1016/j.buildenv.2013.12.001. [Google Scholar]
- 19. Fleming R, Goodenough B, Low LF, Chenoweth L, Brodaty H. The relationship between the quality of the built environment and the quality of life of people with dementia in residential care. Dementia. 2016;15(4):1–18. doi:10.1177/1471301214532460. [DOI] [PubMed] [Google Scholar]
- 20. Cohen-Mansfield J, Werner P. Environmental influences on agitation: an integrative summary of an observational study. Am J Alzheimers Dis Other Demen. 1995;10(1):32–39. doi:10.1177/153331759501000108. [Google Scholar]
- 21. van Hoof J, Kort HSM, van Waarde H, Blom MM. Environmental interventions and the design of homes for older adults with dementia: an overview. Am J Alzheimers Dis Other Demen. 2010;25(3):202–232. doi:10.1177/1533317509358885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brawley E. Alzheirner’s disease: designing the physical environment. Am J Alzheimer’s Care Relat Disord Res. 1992;7(1):3–8. [Google Scholar]
- 23. Fleming R, Forbes I, Bennett K. Adapting the ward for people with dementia. Sydney: NSW Department of Health; 2003:1–124. [Google Scholar]
- 24. van Hoof J, Kort HSM, Duijnstee MSH, Schoutens AMC, Hensen JLM, Begemann SHA. The indoor environment in relation to people with dementia. In: Strom-Tejsen P, et al., eds. Proceedings of the 11th International Conference on Indoor Air Quality and Climate, Indoor Air; 2008:17–22. [Google Scholar]
- 25. Riemersma-van der Lek RF, Swaab DF, Twisk J, Hol EM, Hoogendijk WJ, Van Someren EJW. Effect of bright light and melatonin on cognitive and concognitive function in elderly residents of group care facilities. JAMA. 2008;299(22):2642. doi:10.1001/jama.299.22.2642. [DOI] [PubMed] [Google Scholar]
- 26. Plitnick BA, Lok A, Jones GE, Higgins P, Hornick TR, Rea MS. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clin Interv Aging. 2014;9:1527–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Marquardt G, Schmieg P. Dementia-friendly architecture: environments that facilitate wayfinding in nursing homes. Am J Alzheimers Dis Other Demen. 2009;24(4):333–340. doi:10.1177/1533317509334959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Walker G, Brown S, Neven L. Thermal comfort in care homes: vulnerability, responsibility and thermal care. Build Res Inf. 2015:37–41. doi:10.1080/09613218.2014.998552. [Google Scholar]
- 29. Wong LT, Fong KNK, Mui KW, Wong WWY, Lee LW. A field survey of the expected desirable thermal environment for older people. Indoor Built Environ. 2009;18(4):336–345. doi:10.1177/1420326X09337044. [Google Scholar]
- 30. Hwang RL, Chen CP. Field study on behaviors and adaptation of elderly people and their thermal comfort requirements in residential environments. Indoor Air. 2010;20(3):235–245. doi:10.1111/j.1600-0668.2010.00649.x. [DOI] [PubMed] [Google Scholar]
- 31. Schellen L, van Marken Lichtenbelt WD, Loomans MGLC, Toftum J, de Wit MH. Differences between young adults and elderly in thermal comfort, productivity, and thermal physiology in response to a moderate temperature drift and a steady-state condition. Indoor Air. 2010;20(4):273–283. doi:10.1111/j.1600-0668.2010.00657.x. [DOI] [PubMed] [Google Scholar]
- 32. Van Someren EJW. Age-related changes in thermoreception and thermoregulation. In: Masoro E, Austad S, eds. Handbook of the Biology of Aging. 7th ed. San Diego, CA: Elsevier; 2011:463–478. doi:10.1016/B978-0-12-378638-8.00022-1. [Google Scholar]
- 33. Garre-Olmo J, Lopez-Pousa S, Turon-Estrada A, Juvinya D, Ballester D, Vilalta-Franch J. Environmental determinants of quality of life in nursing home residents with severe dementia. J Am Geriatr Soc. 2012;60(7):1230–1236. doi:10.1111/j.1532-5415.2012.04040.x. [DOI] [PubMed] [Google Scholar]
- 34. van Hoof J. Forty years of Fanger’s model of thermal comfort: comfort for all? Indoor Air. 2008;18(3):182–201. doi:10.1111/j.1600-0668.2007.00516.x. [DOI] [PubMed] [Google Scholar]
- 35. van Hoof J, Kort HSM. Healthy living environments for older adults with dementia. In: de Oliveira Fernandes E, Gameiro da Silva M, Rosado Pinto J, eds. Proceedings of the 8th International Conference Healthy Buildings. Lissabon; 2006:88–93. [Google Scholar]
- 36. Australian Office of Environment and Heritage. Aged-Care Toolkit. Sydney, Australia: Australian Office of Environment and Heritage; 2014. [Google Scholar]
- 37. Jorm A, Mackinnon AJ, Henderson AS, et al. The Psychogeriatric Assessment Scales: a multi-dimensional alternative to categorical diagnoses of dementia and depression in the elderly. Psychol Med. 1995;25(3):447–460. [DOI] [PubMed] [Google Scholar]
- 38. Melrose S. Reducing relocation stress syndrome in long-term care facilities. J Pract Nurs. 2004;54(4):15–17. [PubMed] [Google Scholar]
- 39. Cohen-Mansfield J, Marx MS, Rosenthal AS. A description of agitation in a nursing home. J Gerontol. 1989;44(3):M77–M84. [DOI] [PubMed] [Google Scholar]
- 40. Cohen-Mansfield J. Instruction manual for the Cohen-Mansfield Agitation Inventory (CMAI); 1991:1–37. [Google Scholar]
- 41. Maxim Integrated. Data Loggers—Maxim. 2015. https://www.maximintegrated.com/en/products/digital/data-loggers.html. Updated 2015. Accessed September 28, 2015.
- 42. International Organization for Standardization. Ergonomics of the Thermal Environment: Instruments for Measuring Physical Quantities Physiques. Geneva, Switzerland: International Organization for Standardization; 1998. [Google Scholar]
- 43. International Organization for Standardization. Ergonomics of the Thermal Environment – Analytical Determination and Interpretation of Thermal Comfort Using Calculation of the PMV and PPD Indices and Local Thermal Comfort Criteria. Geneva: International Organization for Standardization; 2005:52. [Google Scholar]
- 44. Twisk JWR. Applied Multilevel Analysis: A Practical Guide. Cambridge: Cambridge University Press; 2006. [Google Scholar]
- 45. IBM Corp. Released. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp; 2012. [Google Scholar]
- 46. Ritchie K, Lovestone S. The dementias. Lancet. 2002;360(9347):1759–1766. doi:10.1016/S0140-6736(02)11667-9. [DOI] [PubMed] [Google Scholar]
- 47. Black D, Veitch C, Wilson L, Hansen A. Heat-Ready: Heatwave Awareness , Preparedness and Adaptive Capacity in Aged Care Facilities in Three Australian States: New South Wales, Queensland and South Australia. Gold Coast: National Climate Change Adaptation Research Facility, 2013. [Google Scholar]
- 48. Loughnan M, Carroll M, Tapper NJ. The relationship between housing and heat wave resilience in older people. Int J Biometeorol. 2015;59(9):1291–1298. doi:10.1007/s00484-014-0939-9. [DOI] [PubMed] [Google Scholar]
- 49. Worfolk JB. Heat waves: their impact on the health of elders. Geriatr Nurs (Minneap). 2000;21(2):70–77. [DOI] [PubMed] [Google Scholar]
- 50. Anderson M, Carmichael C, Murray V, Dengel A, Swainson M. Defining indoor heat thresholds for health in the UK. Perspect Public Health. 2013;133(3):158–164. doi:10.1177/1757913912453411. [DOI] [PubMed] [Google Scholar]
- 51. Aminoff BZ. Not calm and aminoff suffering syndrome in advanced Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2016;31(2):169–180. doi:10.1177/1533317515598858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. WHO, UNEP. Indoor Environment: Health Aspects of Air Quality, Thermal Environment, Light and Noise. Geneva: World Health Organization; United Nations Environmental Programme; 1990. [Google Scholar]
- 53. Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr psychiatry. 2006;14(3):191–210. doi:10.1097/01.JGP.0000200589.01396.6d. [DOI] [PubMed] [Google Scholar]
- 54. Snowdon J, Galanos D, Vaswani D. Patterns of psychotropic medication use in nursing homes: surveys in Sydney, allowing comparisons over time and between countries. Int psychogeriatr. 2011;23(9):1520–1525. doi:10.1017/S1041610211000445. [DOI] [PubMed] [Google Scholar]
- 55. Conti S, Masocco M, Meli P, et al. General and specific mortality among the elderly during the 2003 heat wave in Genoa (Italy). Environ Res. 2007;103(2):267–274. doi:10.1016/j.envres.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 56. ANSI, ASHRAE. Thermal Environmental Conditions for Human Occupancy. Atlanta: American Society of Heating Refrigerating and Air-Conditioning Engineers; American National Standards Institute; 2013. [Google Scholar]