Abstract
It is somewhat unexpected to have headaches in patients with idiopathic normal pressure hydrocephalus (INPH) for which the treatment is drainage of cerebrospinal fluid (CSF) using shunt. Moreover, intracranial hypotension syndrome (IHS) can be a challenging diagnosis, as CSF leak may be difficult to confirm as imaging findings can be normal. This report describes a woman with INPH who developed symptoms of IHS after a spinal tap test. There might be cases with IHS, like our case, who do not completely fulfill the current diagnostic criteria in terms of not having any objective evidence of intracranial hypotension but who also could not be explained by other conditions and recovered totally after classical IHS treatment. Current diagnostic criteria for IHS might be revised for those having normal neuroimaging and not accepting lumbar puncture. Nevertheless, when the history, signs, and symptoms strongly suggest IHS even with normal imaging, treatment should be started immediately.
Keywords: normal pressure hydrocephalus, intracranial hypotension, tap test, headache
Introduction
Idiopathic normal pressure hydrocephalus (INPH) is an increasingly recognized disorder which is characterized by a slowly progressive impairment of gait and balance, cognitive deterioration, and urinary incontinence. These symptoms can be relieved by the insertion of a ventriculoperitoneal shunt. The challenge for the clinician is to predict which patient with INPH would benefit from shunt surgery. The diagnosis of INPH is based on clinical examination, brain imaging, and supplementary tests on circulation of cerebrospinal fluid (CSF). 1,2 One of the most common supplementary tests is CSF tap test which is used as prognostic tool to select patients for shunt surgery. 2 The specificity of the tap test is as high as 100%, whereas the sensitivity only ranged from 26% to 62% in some studies. 2,3 Up to 50 mL CSF is removed through a lumbar puncture, and assessments of functions, mainly gait functions, are performed before and after the CSF withdrawal. 2,4 Postdural puncture headache might be seen in the clinical setting not related to the volume of the CSF sample. Orthostatic headache usually starts within 48 hours after lumbar puncture and disappears in 50% to 80% of patients after 5 days. 5 It is the typical manifestation of intracranial hypotension syndrome (IHS). In addition to the headache, other symptoms have been reported in IHS including neck pain or stiffness, nausea, and emesis. In total, these symptoms have been reported to be present in up to 50% of patients. 6 Cranial nerve abnormalities are rare and patients may also complain of facial numbness, dizziness, and interscapular, neck, low back pain, diplopia, blurring of vision, or visual field change. 7 In 2013, the Headache Classification Committee of the International Headache Society proposed revised diagnostic criteria for IHS, reporting the necessity of showing low CSF pressure (<60 mm CSF) and/or evidence of CSF leakage on imaging. 8 However, some patients have the syndrome without pachymeningeal enhancement. 9
We present a patient who had INPH initially but after spinal tap developed symptoms of IHS. This situation is interesting because an orthostatic headache was seen in a patient with a disease in which the main treatment is drainage of CSF.
Case Report
A 83-year-old woman was admitted to our Department of Geriatrics due to gait and walking difficulty, recurrent falls, urgency incontinence, and mild memory problems approximately for 1 year. She had known spinal stenosis since 2009 and osteoporosis, for which she had been treated with alendronate sodium. Her examination revealed a “magnetic” gait, turning en bloc, and postural instability. No muscle weakness, no spasticity or other pyramidal signs, and no proprioceptive sensory disturbance or Romberg’s sign suggestive of sensory ataxia or spinal cord dysfunction were present. Signs of cerebellar ataxia, those of extrapyramidal rigidity, and resting tremor were also absent.
Her neuropsychological evaluation is shown in Table 1. She was hospitalized and subjected to brain computed tomography (CT) which showed enlargement of the ventricular system not entirely attributable to diffuse cerebral atrophy and showed no macroscopic obstruction to CSF flow (Figure 1 A and B). To confirm the suspicion of idiopathic normal pressure hydrocephalus (INPH), a spinal tap test was performed using a 20-gauge atraumatic needle in the lateral recumbent position, and 30 mL CSF was withdrawn. Lumbar puncture showed normal opening pressure (80 mm H2O) of CSF (normal, 70-180 mm H2O), which showed a normal protein, glucose, and cell count and no organisms (Gram’s stain or culture). The stylet was replaced before withdrawing the needle as always done. After tap test, her gait improved dramatically as shown by her gait reexamination which was made 2 hours after the tap test (Table 1), and based on these results she was diagnosed with INPH. She was scheduled to see a neurosurgeon and was discharged the following day.
Table 1.
Neuropsychological and Laboratory Evaluation of the Patient: Comprehensive Geriatric Assessment.
| Before Tap Test | After Tap Test (2 hours later) | |
|---|---|---|
| CDR | 1 | − |
| COST 12 | 23/30 | 25/30 |
| POMA balance | 5 | 8 |
| POMA gait | 4 | 9 |
| POMA total | 9 | 17 |
| Up & go test, sec | 42 | 30 |
| MNA tool | 11 | − |
| Luria’s drawings | NMa | − |
| Clock drawing | NMa | − |
| Stroop test | NMa | − |
| VFT | 6 animals/60 s; 9 fruits/60 s with 2 perseverations | − |
| BI | 71 | − |
| IADL scale | 2 | − |
| CSDD | 8 | − |
| Laboratory evaluation | ||
| WBC, cell/mm3 | 7200 | |
| Hemoglobin, g/dL | 12.4 | |
| ESR, mm/h | 10 | |
| CRP | 2.2 | |
| AST, U/L | 9 | |
| Vitamin D, ng/mL | 35.2 | |
| Vitamin B12, pg/mL | 1036 | |
| Folic Acid, ng/mL | 6.4 | |
| TSH, IU/mL | 1.5 | |
Abbreviations: BI, Barthel Index (0 [worst]-100 [best]); CDR, Clinical Dementia Rating scale; CSDD, The Cornell Scale for Depression in Dementia (0 [worst]-38 [best]); COST, cognitive state test (0 [worst]-30 [best]); IADL, Lawton Broady Instrumental Activities of Daily Living Scale (0 [worst]-17 [best]); MNA, mini-nutritional assessment tool (0 [worst]-14 [best]); POMA: Tinetti Performance Oriented Mobility Assessment, POMA-Gait (0 [worst]-12 [best]), and POMA-Balance (0 [worst]-16 [best]); VFT, verbal fluency test; AST, aspartate aminotransferase; CPR; C-reactive protein; ESR, erythrocyte sedimentation rate; Hb, hemoglobin; TSH, thyroid-stimulating hormone; WBC, white blood cell.
a The patient was not able to do some tests such as Luria’s drawings, Clock drawings, and stroop test before tap test, shortened as NM (not managed). The minus sign means that the tests have not been applied to the patient after the tap test.
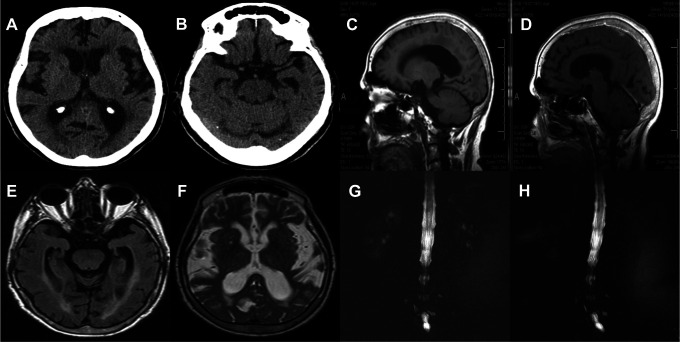
Figure 1.
A, A brain computed tomography (CT) revealed ventricular enlargement out of proportion to sulcal enlargement and cerebral atrophy with an Evan’s index of 0.31. Also, the image revealed periventricular signal changes as the evidence of altered brain water content in the patient who has no ischemic risk factors. B, The CT scan shows enlargement of the temporal horns of the lateral ventricles not entirely attributable to hippocampus atrophy. C and D, Sagittal views of T1-weighted and gadolinum-enhanced T1-weighted magnetic resonance imaging (MRI) revealed normal in terms of intracranial hypotension syndrome (IHS). E, Flair T2 axial image showed lateral ventricular enlargement and presence of an aqueductal flow void. F, T2-weighted axial image showed periventricular signal changes as in (A). G and H, Magnetic resonance myelography proved no evidence of cerebrospinal fluid leak.
At the 1-month visit, she reported that 2 days after the discharge she had started to have headache and dizziness. Her headache was postural headache mainly in the whole head. She also reported that she had severe nausea, vomiting, photophobia, and transient blurring of vision since 2 days after her discharge. She felt worse when sitting up or walking and better in a lying down position. The patient was completely conscious, oriented, and cooperative. Fundus examination was normal. Mild neck stiffness was present. Convergence was slightly weaker in the right eye. The remaining neurological examination and laboratory evaluation revealed normal. She had no fever. She was rehospitalized due to the development of these symptoms by being considered to have intracranial hypotension based on her medical background, current complaints, and findings. For this reason, she had a brain magnetic resonance imaging (MRI) with contrast which showed neither pachymeningeal enhancement suggestive of IHS nor any other findings that could be compatible with intracranial hypotension (Figure 1 C-F). Magnetic resonance (MR) myelography of the lumbar spine revealed no proof of site of CSF leak (Figure 1 G and H). In addition, her upper gastrointestinal endoscopy and abdominal ultrasonography were normal. Unfortunately, she rejected to have a lumbar puncture again. In this situation, when her typical headache with orthostatic symptoms and no antecedent medical conditions other than the spinal tap test were taken into consideration, it was likely considered as IHS without neuroimaging findings. She was given bed rest and during that time infusion of saline solution was immediately started. Conventional analgesics like caffeine and paracetamol relieved her headache. She was discharged home within 3 days with a favorable improvement prior to her admission. She had totally recovered when she was assessed 10 days later at the control visit.
Discussion
The patient presented with severe gait disturbance, mild cognitive decline in approximately 1 year’s duration with a reportedly progressive course, and urgency. She had falls due to impaired postural instability. Her cognitive pattern of performance revealed moderate frontal subcortical dysfunction, which was interpreted as consistent with INPH. Her brain imaging revealed ventriculomegaly out of proportion to cerebral atrophy. And there was no communicative obstruction. With the suspicion of INPH, a tap test was performed for measuring the CSF opening pressure and for observing her responsiveness to the test. The condition of the patient with gait disturbance as the prominent symptom improved. Unfortunately, soon after the tap test, she had symptoms of headache, severe nausea, vomiting, dizziness, photophobia, and transient blurring of vision that worsened when sitting up or walking.
One of the most common adverse effects of tap test is postlumbar puncture headache. It usually starts within 48 hours after lumbar puncture and disappears within 2 weeks. 10 However, in this case, different from the literature, 10 the duration of the headache was more than 4 weeks with accompanying other symptoms that made us to consider intracranial hypotension. As headache is the most prominent symptom in patients with IHS after spinal tap test, some elderly patients, in particular those having very severe cognitive deficit, could not disclose their headaches but live with anxiety or restlessness. 11
Diagnostic criteria for IHS require low CSF pressure (<60 mm CSF) and/or evidence of CSF leakage on imaging. 8 But, we could not show imaging findings compatible with IHS in the clinical setting to support the diagnosis. The CSF leakage was not confirmed either using contrast-enhanced MRI or using MR myelography. Additionally, we could not be able to measure the opening pressure, since the patient did not accept to have a lumbar puncture once again. However, there was no antecedent medical condition other than the spinal tap test sufficient to explain in the presentation. Also, hydration, caffeine, and conventional analgesics relieved her symptoms. With all these findings, she was diagnosed with intracranial hypotension-like syndrome. We might interpret that her CSF leakage was not active or was small and possibly stopped during her hospitalization. On the other hand, as many as 20% to 30% of patients with IHS have a normal cranial MRI. 7 There might be cases with IHS who do not completely fulfill the current diagnostic criteria in terms of not having any objective evidence of intracranial hypotension but who also could not be explained by other conditions and recovered totally after classical IHS treatment. Therefore, we have thought that it would be better to review the diagnostic criteria for IHS in the patients whose CSF pressure cannot be measured and cranial MRI is nondiagnostic.
It is somewhat unexpected to have headaches in patients with INPH for which the treatment is drainage of CSF using shunt. Moreover, those patients could have prolonged typical orthostatic symptoms. Finally, when clinically IHS is strongly thought, the patients should be considered to have IHS and as traditionally done, it is initiallymanaged by conservative treatment as soon as possible. Current diagnostic criteria for IHS might be revised for those having normal neuroimaging and not accepting lumbar puncture.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM. Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005;57 (3 suppl):S4–S16. [DOI] [PubMed] [Google Scholar]
- 2. Marmarou A, Bergsneider M, Klinge P, Relkin N, Black PM. The value of supplemental prognostic tests for the preoperative assessment of idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005;57 (3 suppl):S17–S28. [DOI] [PubMed] [Google Scholar]
- 3. Malm J, Kristensen B, Karlsson T, Fagerlund M, Elfverson J, Ekstedt J. The predictive value of cerebrospinal fluid dynamic tests in patients with th idiopathic adult hydrocephalus syndrome. Arch Neurol. 1995;52 (8):783–789. [DOI] [PubMed] [Google Scholar]
- 4. Ghosh S, Lippa C. Diagnosis and prognosis in Idiopathic Normal Pressure Hydrocephalus. Am J Alzheimers Dis Other Demen. 2014;29 (7):583–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lybecker H, Djernes M, Schmidt JF. Postdural puncture headache (PDPH): onset, duration, severity, and associated symptoms. An analysis of 75 consecutive patients with PDPH. Acta Anaesthesiol Scand. 1995;39 (5):605–612. [DOI] [PubMed] [Google Scholar]
- 6. Schievink WI. Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol. 2003;60 (12):1713–1718. [DOI] [PubMed] [Google Scholar]
- 7. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295 (19):2286–2296. [DOI] [PubMed] [Google Scholar]
- 8. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33 (9):629–808. [DOI] [PubMed] [Google Scholar]
- 9. Mokri B, Atkinson JLD, Dodick DW, Miller GM, Piepgras DG. Absent pachymeningeal gadolinium enhancement on cranial MRI despite symptomatic CSF leak. Neurology. 1999;53 (2):402–404. [DOI] [PubMed] [Google Scholar]
- 10. Web site. http://www.uptodate.com/contents/lumbar-puncture-technique-indications-contraindications-and-complications-in-adults?. Updated September 18, 2013; Published August 27, 2014.
- 11. Moretti R, Torre P, Antonello RM, Cazzato G. Headache in dementia. Eur J Neurol. 2001;8 (1):93–94. [DOI] [PubMed] [Google Scholar]
- 12. Babacan-Yildiz G, Isik AT, Ur E, et al. COST: Cognitive state test, a brief screening battery for Alzheimer disease in illiterate and literate patients. Int Psychogeriatr. 2013;25 (3):403–412. [DOI] [PubMed] [Google Scholar]