Abstract
There is a growing body of research on Alzheimer’s disease and driving, but much less is known about less common dementias, such as frontotemporal dementia (FTD). The purpose of this study was to review the empirical literature about FTD and driving. A study was included if it met the following criteria: published from 1992 to 2013 in English, research involving humans, and included both FTD and driving data. We searched the following electronic databases: EBSCOhost, PubMed, Google Scholar, Proquest, Web of Knowledge, and Publishing Connect. A total of 367 abstracts were reviewed; however, only 4 articles satisfied the inclusion criteria. Results showed that drivers with FTD had more problems than control groups. Specific driving issues were related to antisocial behaviors common among people with FTD (eg, hit and run crashes, failure to stop at red lights, speeding infractions, and failure to recognize pedestrians at intersections). More research on FTD and driving is needed.
Keywords: frontotemporal dementia, dementia, driving, crash, older drivers
Introduction
Research exploring how Alzheimer’s disease (AD) impacts driving is making rapid progress. Unfortunately, frontotemporal dementia (FTD) and driving remain quite understudied. This is likely because FTD is much less common than AD and is often misdiagnosed as another disease or disorder. FTD is a degenerative condition of the frontal and anterior temporal lobes that impairs thinking and reasoning, personality, movement, speech and language, sociability, and some aspects of memory. 1 FTD tends to develop earlier than AD, with the average age onset of FTD between 2 40 and 65, whereas in AD, the age of onset is usually after 65 years.
Three different subtypes of FTD have been identified: behavioral variant FTD formerly known as Pick’s disease, progressive nonfluent aphasia, and semantic dementia. Although all variants of FTD impair executive function, the presentation of behavioral symptoms vary by subtype. 3 Frontotemporal dementia used to be considered rare, but it may account for up to 10% to 15% of all patients with dementia and prevalence is likely underestimated because FTD is easily misdiagnosed as other conditions and is also underdiagnosed. 4 There is not a test or any group of tests that conclusively diagnose FTD; thus, diagnosis is clinical based on a physicians’ best opinion of symptomology. 4 However, brain imaging is improving dramatically, and more cases of FTD will likely be documented as the population ages.
Given the impact of FTD on executive function, clear consequences on cognitively demanding tasks like driving are expected. Further, the degeneration caused by FTD affects planning ability, multitasking ability, motivation, and decision making as well as causing distractibility and lack of insight. 5 All these abilities impact the ability to drive safely. For example, a person with FTD may not be able to plan and follow a route or attend to traffic cues due to these impairments. Similarly, reacting to multiple different stimuli while driving (eg, other cars and pedestrians) is difficult and sometimes impossible for people who have FTD. Yet, FTD is vastly understudied in comparison to AD and the other dementias. The purpose of this study was to review the literature related to FTD and driving to determine the impact on driving status, driving outcomes, and identify gaps in the literature warranting further research.
Methods
A review of the literature and state of science on FTD and driving was conducted in order to better understand the scope of the problem of FTD and driving. Further, this review was conducted to bring attention to the issue of FTD and driving, so that other researchers can become attuned to the issue.
Literature Search
The following strategy was used to identify usable articles for the literature review. First relevant electronic databases were searched including Academic Search Premier, AgeLine, CINAHL, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Cochrane Methodology Register, ERIC, Health and Psychosocial Instruments, Health Technology Assessments, MEDLINE, Primary Search, PsycARTICLES, PsycINFO, SocINDEX, Pubmed, Google Scholar, Proquest, Web of Knowledge, and Publishing Connect. The following search terms were used: Frontotemporal dementia and driving automobile, Frontotemporal dementia and driving vehicle, Frontotemporal dementia and driving car, Frontotemporal dementia and driving accidents, driving cessation and Frontotemporal dementia, Frontotemporal dementia and automobile crashes, Frontotemporal dementia and crashes, Frontotemporal dementia and automobile, Frontotemporal dementia and car, Neurodegenerative diseases and driving, Frontotemporal dementia and caregiver. Further, we followed the suggestion of a professional librarian and ran another search using the same databases listed earlier and with these terms: “FTD, car and drive” “Frontotemporal dementia, drive, and car” and “driving car and Frontotemporal dementia.” This new search did not produce any further articles for the review. In addition, key journals were electronically searched, including The Journal of Geriatric Psychiatry and Neurology and The American Journal of Neurology. A higher order search term approach was used to ensure that studies with both FTD and driving were located and included in the review. A hand search of relevant articles (ie, “Driving Abilities in Frontotemporal Dementia Patients” by V. de Simone et al) was also conducted. Three clinical research leaders in FTD were consulted regarding study aims and asked to identify relevant studies (ie, a coauthor of the de Simone article; a member of the Frisoni research team; and a neurologist leading a FTD clinic at an academic medical center).
Inclusion/Exclusion Criteria
A study was included in the literature review if it met the following criteria: published from 1992 to 2013, published in English, were based solely on human research not animal research, included both FTD and driving, frontal temporal lobar degeneration and driving, neurodegenerative diseases and driving or Pick’s disease, and driving within the same article. Studies were excluded if they were not in English, were based on animal research, and did not make a connection between FTD and driving within the same article. The authors’ primary language proficiency was English, thus studies only in English were used for the review.
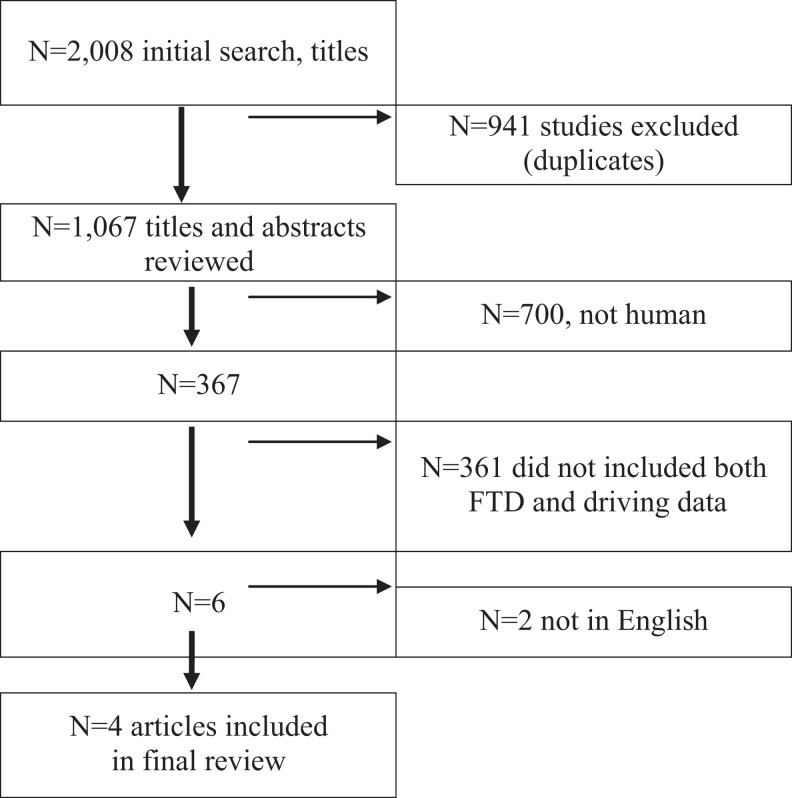
Flow of Studies
A total of 2008 titles and abstracts were reviewed. As seen in Figure 1, the flow diagram shows that duplicate articles were excluded (941), bringing the total for review to 1067. A total of 700 studies were excluded due to not involving humans, leaving the total at 367. A total of 361 articles were excluded for not reporting FTD and driving leaving the total to 6. Of the last 6 studies, 2 had to be left out of the review because they were not available in English. The final number of studies used for this literature review was 4 studies.
Figure 1.
Flow diagram.
Results
Results of this comprehensive literature search showed that drivers with FTD had more problems behind the wheel than control groups and fitness to drive should be questioned (Table 1). Specific driving issues were related to antisocial behaviors common among people with FTD. The most common antisocial driving behaviors exhibited by individuals with FTD cited in the literature were hit and run car accidents, running red lights, speeding infractions, driving impulsively, and lack of ability to recognize pedestrians at intersections. These abnormal driving behaviors are heavily cited in the literature and thought to be a result of the impact FTD has on brain function.
Table 1.
Descriptive Characteristics of Included Studies.
| Author | Study Design | Number of Patients | Settings | FTD | Driving | Notes | FTD |
|---|---|---|---|---|---|---|---|
| de Simone, 2007 | Case control | 15 patients with FTD (10 male, 5 female), 15 controls | Cognitive Neuroscience Section, NIH, Bethesda, MD | Disease duration 4.2 years | 67% cases still driving Driving simulation: 60% of cases had collisions, 47% off-road accidents, and 33% ran stop signs (P = .003); speeding tickets | Speed variability and number of billboards recalled after simulation correctly classified 90% of patients | Behavioral changes (aggressive, agitated) lead to inappropriate driving |
| Zuin et al, 2002 | Case control | 56 with dementia (17 male, 39 female)—2 patients with FTD 31 controls—(19 male and 12 female) | Neuropsych. Research Program, Pittsburgh, PA | Neurological examination, psychiatric evaluation | Interview regarding motor vehicle crashes and abnormal driving behaviors 20% with dementia exhibited abnormal driving behaviors, 11% reported motor vehicle crashes, 6% reported multiple motor vehicle crashes | Results did not differentiate between patients with FTD and AD | N/A |
| Miller et al, 1997 | Case study—patients with AD and FTD | 22 patients with FTD (11 male and 11 female), 22 people with AD (14 female, 8 male) | Harbor-UCLA Medical Center Torrance, CA | MMSE, previous neuropsych. tests, neuroimaging with MRI and SPECT | Of the 22 patients with FTD, 10 presented history of socially disrupted behavior Of the 22 patients with AD, 1 presented this history | Hit and run accidents were problematic with FTD not AD | Antisocial |
| Frisoni et al, 1995 | Case control | 19 with FTD, 11 patients with FTD having complete data, 16 with AD, 7 Controls | Alzheimer’s Disease Unit, University of Padua, Italy | CT scan, SPET scan, neuropsych. testing | Proxy (family) report of cases indicated impulsivity when driving occurred in FTD | FTD drivers have poor impulse control, causing minor accidents and distracted driving | Impulse control |
Abbreviations: AD, Alzheimer’s disease; FTD, frontotemporal dementia.
Results also indicate that other abnormal and socially disruptive behaviors such as assault, indecent exposure, shoplifting, and agitation often occur within people with FTD. These socially disruptive behaviors can impact driving, namely, agitation. Agitation while driving can lead to traffic accidents, excessive speeding and erratic lane changes, and other dangerous driving behaviors. The research on FTD and driving is sparse. Due to the severity of the behaviors associated with FTD and driving, it is imperative that further research is conducted.
Discussion
To our knowledge, this is the first literature review of FTD and driving and it encompassed the last 21 years of research. The results of this study showed that there is a paucity of research on FTD and driving. Results highlight the different behavioral actions among drivers with AD and drivers with FTD, as many drivers with AD can continue to drive after diagnosis. 7 Possible driving manifestations of FTD behavioral problems (eg, poor impulse control) may include running red lights, speeding, and not stopping when involved in crashes. This impaired impulse control is a threat to safety for the driver and others on the road including pedestrians. Other possible driving problems related to FTD are due to the inability to plan, solve problems correctly, and make proper judgments. Each of these behaviors is essential to driving safety and driving fitness. Although research suggests that some patients with AD may continue to drive for a short time after diagnosis, 7,8 our review suggests this is not the case for drivers with FTD. Because persons with FTD tend to get diagnosed later in the course of illness and the behavioral and judgment issues that inevitably arise, we believe the risk of adverse driving events is heightened.
Driving problems are not restricted to the behavioral or judgment problems prominent in FTD. Problems also arise due to the aggressive antisocial behaviors (eg, agitation, assault, and indecent exposure) if these occur while operating a vehicle. Driving in the best circumstances presents many instances where rapid decisions and reactions are necessary to maintain safety. Drivers exhibiting antisocial or aggressive behaviors may react in ways that are not safe. Finally, withdrawal from social contact and connectedness, personality rigidity, inattention, and emotional directness are all common behavioral symptoms among people with FTD. As driving skills decay, very often drivers rely on a navigator or copilot to prolong driving. However, the social impairments associated with FTD progression may limit the availability of helpers. Due to the young age of onset and position in the life course, many individuals with FTD are still getting behind the wheel on a regular basis; thus, these predominant behaviors of people with FTD impact driving status and safety.
There is no scientific literature about licensing and renewal for people with FTD, and there are no specific screening procedures for those with FTD. Policy solutions for FTD are not in place. Driving is regulated at the state level using license renewal and medical reporting procedures. 9 In terms of license renewal, given the current policies, drivers with early FTD could likely pass. People with FTD do not usually exhibit memory problems, thus it can be hypothesized that an individual with FTD could pass a written license renewal examination. Based on what we do know about FTD and driving, we suggest that driving examinations contain specific items that target people with FTD, such as items that get at aggressive and antisocial behaviors behind the wheel. Additionally, because individuals with FTD are much younger than the average person with dementia, they may not be required to complete an in-person driving evaluation like those in their 70s and 80s. One suggestion should perhaps be that anyone diagnosed with FTD should be required to take an in-person driving fitness test. Moreover, examination of licensing and renewal policies specific to people with FTD must be undertaken to help deter drivers with FTD from driving.
Mandatory medical reporting for cognitive impairment to the State Department of Motor Vehicles exists in about 6 states, and it does not yet adequately address FTD and driving. Some other states encourage physicians to report individuals who may be unsafe behind the wheel, but it is voluntary, not mandatory. There are also some state regulations that encourage self-reporting as well as family reporting to the DMV. 6 Consequently, these systems are not prepared to handle FTD because a person with FTD would not be able to provide a self-report of their inappropriate behavior behind the wheel because they may be unaware of their actions. Moreover, in many cases, the inappropriate driver must be reported via postal mail causing a major time delay in actually revoking the individual’s driving privileges. 6
There is also a lack of scientific research on alternative transportation options for people with FTD. Due to the outward antisocial behaviors people with FTD display, busses, trains, and communal transportation may not be viable options as modes of transportation for people with FTD. Moreover, because FTD strikes at such a young age, some may not be eligible for senior transportation rides. If there are senior transportation services in the geographic region where the person resides, one suggestion could be to make exception allowing them to use ride services if a person diagnosed with FTD is below the age of 60. Volunteer drivers may be a viable option that will help drivers with FTD stay off the roads but may not be available in all areas. Further research is necessary to determine what alternative transportation options are best for people with FTD deemed no longer able to drive.
Caregiving for persons with FTD is especially emotionally demanding due to the distressing behavioral issues associated with FTD. Moreover, due to the drastic personality changes associated with FTD, communication about driving can be difficult. Our results showed that studies have not explicitly addressed implications for family members caring for someone with FTD who is still driving. Further study of family support options related to FTD and driving should be undertaken due to the distinct behavioral profile that affects driving ability in patients with FTD. It is advisable that family members begin to watch for antisocial behaviors related to FTD and begin to facilitate discussions about limiting driving or complete cessation of driving. However, this may be an ineffective way to accomplish the goal of driving cessation for the patient with FTD because of their inability to make proper judgment.
One major limitation of this study is that some of the studies reviewed use the case control methodology that is considered a weak methodology. Specifically, the studies are at a descriptive level, use only small clinical samples, and there is somewhat of a lack of scientific rigor in terms of reporting findings due to the lack of research associated with this topic.
Future scientific research related to FTD and driving is imperative for understanding this population. Future studies are important so that researchers, practitioners, and families can gain quality insight into the complicated relationship between someone with FTD and their driving behavior.
Footnotes
Authors’ Note: An earlier version of this article was presented at the Alzheimer’s Association International Conference in Boston MA on July 16, 2013.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Braaten A, Parsons T, McCue R, Sellers A, Burns W. Neurocognitive differential diagnosis of dementing diseases: Alzheimer's dementia, vascular dementia, frontotemporal dementia, and major depressive disorder. Int J Neurosci. 2006;116(11):1271–1293. http://www.ncbi.nlm.nih.gov/pubmed/17000529. Accessed March 6, 2012. [DOI] [PubMed] [Google Scholar]
- 2. Passant U, Rosén I, Gustafson L, Englund E. The heterogeneity of frontotemporal dementia with regard to initial symptoms, qEEG and neuropathology. Int J Geriatr Psychiatry. 2005;20(10):983–988. Accessed March 9, 2012. [DOI] [PubMed] [Google Scholar]
- 3. Frontotemporal dementia. http://memory.ucsf.edu/ftd/. Accessed November 11, 2012.
- 4. Frontotemporal dementia. http://www.alz.org/dementia/fronto-temporal-dementia-ftd-symptoms.asp. Accessed October 24, 2013.
- 5. Hunt L, Murphy C, Carr D, Duchek J, Buckles V, Morris J. Reliability of the Washington university road test. A performance-based assessment for drivers with dementia of the Alzheimer type. Arch Neurol. 1997;54(6):707–712. http://www.ncbi.nlm.nih.gov/pubmed/9193205. Accessed August 29, 2013. [DOI] [PubMed] [Google Scholar]
- 6. Miller B, Darby A, Benson D, Cummings J, Miller M. Aggressive, socially disruptive and antisocial behaviour associated with fronto-temporal dementia. Br J Psychiatry. 1997;170(2):150–154. http://www.ncbi.nlm.nih.gov/pubmed/9093504. Accessed March 2, 2012. [DOI] [PubMed] [Google Scholar]
- 7. State Policy Affecting Community Mobility. http://www.nhtsa.gov/people/injury/olddrive/CommMobilityDementia/pages/CurrentScr-StatePolicy.htm. Accessed August 6, 2013.
- 8. Dugan E, Barton K, Coyle C, Lee C. U.S. Policies to Enhance Older Driver Safety: A systematic review of the literature. J Aging Social Policy. 2013;25(4):335–352. Accessed November 8, 2013. [DOI] [PubMed] [Google Scholar]
- 9. de Simone V, Kaplan L, Patronas N, Wassermann E, Grafman J. Driving abilities in frontotemporal dementia patients. Dement Geriatr Cogn Disord. 2007;23(1):1–7. http://www.ncbi.nlm.nih.gov/pubmed/17047327. Accessed March 1, 2012. [DOI] [PubMed] [Google Scholar]
- 10. Frisoni G, Pizzolato G, Geroldi C, Rossato A, Bianchetti A, Trabucchi M. Dementia of the frontal type: neuropsychological and [99Tc]-HM-PAO SPET features. J Geriatr Psychiatry Neurol. 1995;8(1):42–48. http://www.ncbi.nlm.nih.gov/pubmed/7710647. Accessed February 16, 2012. [PubMed] [Google Scholar]
- 11. Zuin D, Ortiz H, Boromei D, Lopez O. Motor vehicle crashes and abnormal driving behaviours in patients with dementia in Mendoza, Argentina. Eur J Neurol. 2002;9(1):29–34. http://www.ncbi.nlm.nih.gov/pubmed/11784373. Accessed February 4, 2012. [DOI] [PubMed] [Google Scholar]