Abstract
This study aimed to assess the effects of a psychoeducational intervention, designed to improve direct care workers’ stress, burnout and job satisfaction, and person-centered communicative behavior in people with dementia. A pretest–posttest control group design was conducted in 4 aged-care facilities. Two experimental facilities received a psychoeducational intervention, and 2 control facilities received an education only. Data were gathered from 53 care workers at baseline, immediately, and 6 months after the intervention, through self-administrated instruments and video-recorded morning care sessions. The experimental group showed a significant decrease in care workers’ burnout and a significant improvement in several communicative behaviors (eg, involvement). Stress levels deteriorated at 6 months, and no intervention effects were found for job satisfaction. The findings highlight the importance of providing care workers with both technical competences and tools for stress management, as this might be associated with a reduction in their levels of exhaustion and improved communicative behaviors.
Keywords: aged-care facilities, dementia, person-centered care, direct care workers, psychoeducational intervention
Introduction
People with dementia are one of the fastest growing groups of people living with long-term conditions. The number of people living with dementia worldwide in 2013 was estimated at 44.35 million, reaching 75.62 million in 2030 and 135.46 million in 2050. 1 Along with these projections, there will be an associated increase in demand for long-term care mainly provided by aged-care facilities. 1
In an aged-care facility, the bulk of care that residents receive is provided by direct care workers (DCWs). 2 These workers are responsible for helping frail and disabled older adults carry out the most basic activities of daily living, such as bathing, dressing, toileting, and eating, during which they also provide the personal interaction that is essential to residents’ quality of life and care. 2 However, stressors resulting from inadequate education and training in dementia care, high workload, interpersonal conflicts, or lack of management support have been shown to be prevalent in DCWs’ work. 3,4 Such stressors place DCWs at high risk of experiencing stress, burnout, and job dissatisfaction, which are known to create a disruption in the worker–resident relationship and hinder the delivery of quality care. 3,5
The provision of education to DCWs has been long regarded as an essential component for improving the quality of dementia care. 6,7 This is often designed to improve DCWs’ skills based on person-centered care (PCC) approaches, which have become synonymous with “best practice.” 8,9
Person-centered dementia care has its roots in the work of Kitwood 10 who was inspired by Carl Rogers and his client-centered counseling. Kitwood, 10 soon followed by Nolan et al 8 and their relationship-centered care, stressed the influence of interpersonal relationships as an essential aspect for understanding the dementia experience, theorizing that some of the deterioration seen in people with dementia was caused not only by the disease process itself but also by how the person is treated. These authors emphasized the relational nature of PCC and the need to provide workers with the skills they need to enhance positive interactions (eg, consult or validate; labeled positive person work—PPW) and reduce negative communicative behaviors (eg, ignore or infantilization) that depersonalize experiences of the person with dementia (labeled malignant social psychology—MSP), 10 thus creating an enriched environment of care. 8
In notable randomized controlled studies, DCWs were provided with PCC–based, education-only interventions designed to reduce the residents’ levels of agitation and aggression 11 -13 and to enhance residents’ engagement in daily activities. 14 Researchers have demonstrated the potential for these interventions to improve DCWs’ knowledge and enhance their willingness to encourage residents’ autonomy, independence, and communication 15 ; however, their effects on stress, burnout, or job satisfaction are modest and often neither long lasting or significant. 16,17 This suggests that interventions are mainly focused on improving DCWs’ knowledge and instrumental skills and are less concerned with their emotional and relational skills, which, despite the rhetoric of PCC, are still undervalued. Providing DCWs with both technical competences and tools for stress and emotional management holds promise as a means of driving forward benefits for DCWs and care provision. This approach may better prepare DCWs to deal with their multifaceted and emotionally demanding job, potentially improving person-centered interactions, job satisfaction, and well-being. However, to the authors’ knowledge, no studies assessing the efficacy of psychoeducational interventions in the context of formal care have been conducted.
This study aimed to examine the immediate and the 6-month effects of a PCC-based psychoeducational intervention (PCC-based Psychoeducational (PE) intervention) targeted at DCWs caring for people with dementia in aged-care facilities. It was hypothesized that, compared with an education-only intervention (control group), an intervention offering both educational and emotional support would reduce DCWs’ perceived stress, burnout, and job dissatisfaction. It was also expected that, compared to the control group, the PCC-based PE intervention would decrease the frequency and duration of DCWs’ MSP behaviors and enhance the frequency and duration of PPW behaviors.
Design
This experimental study used a pre–posttest control group design and was conducted in 4 aged-care residential facilities. The study was approved by an ethics committee (Health Sciences Research Unit: Nursing (UICISA: E), hosted by the Nursing School of Coimbra, Portugal).
Data were collected at (1) baseline assessment (T1), in all facilities 3 weeks prior to the intervention; (2) posttest (T2), 2 weeks after the end of the intervention; and (3) follow-up (T3), 6 months after the intervention.
Procedure
The facilities of the local area where the study was conducted were stratified into groups by the staff–resident ratio and residents with dementia–total of residents’ ratio. Then, 2 pairs of facilities of the same created group were approached by the research team and were given the opportunity to participate in the study. All 4 facilities agreed to participate and were randomly allocated to the experimental group—PE intervention—or control group—education-only intervention, using a random number generator. Randomization could not occur at the individual level due to possible treatment effects if the same facility functioned as both experimental and control sites. Study facilities were private, nonprofit institutions of collective accommodation with more than 30 licensed beds with a staff/resident ratio between 1:2 and 1:3.
Sample
The study sample includes DCWs (may be called under different names in different countries, for example, nursing aides or care assistants),who represent the largest component of the long-term care workforce and are responsible for helping frail and disabled older adults carry out the most intimate and basic activities of daily living. To be included in the study, DCWs had to be employed for at least 2 months (so adjustments to the residents and facility had been achieved) and provide morning personal care (ie, period of time between 7 am and 12 am that involved activities related to bathing, grooming, dressing and toileting) to people with a diagnosis of moderate to severe dementia. Temporary DCWs and trainees were excluded as it was not possible to ensure their participation until the end of the study. The identification of the eligible DCWs was supported by facility managers. Three DCWs were excluded from the study due to being temporary.
A meeting with the 58 identified DCWs was scheduled to provide detailed information about the study and invite them to participate. They were informed about the voluntary nature of their participation, and their anonymity and confidentiality were assured. All DCWs agreed to participate and their informed signed consent was obtained at the end of the meeting.
Twenty-seven DCWs received a psychoeducational intervention and 31 DCWs participated in the control group. Of these, 53 DCWs completed all 3 rounds of data collection. Two dropouts occurred in the control group and 3 in the experimental group. The dropouts were due to DCWs’ absence from work during the assessment periods, as a result of sick leave (n = 2), vacation (n = 2), or dismissal (n = 1; Figure 1).
Figure 1.
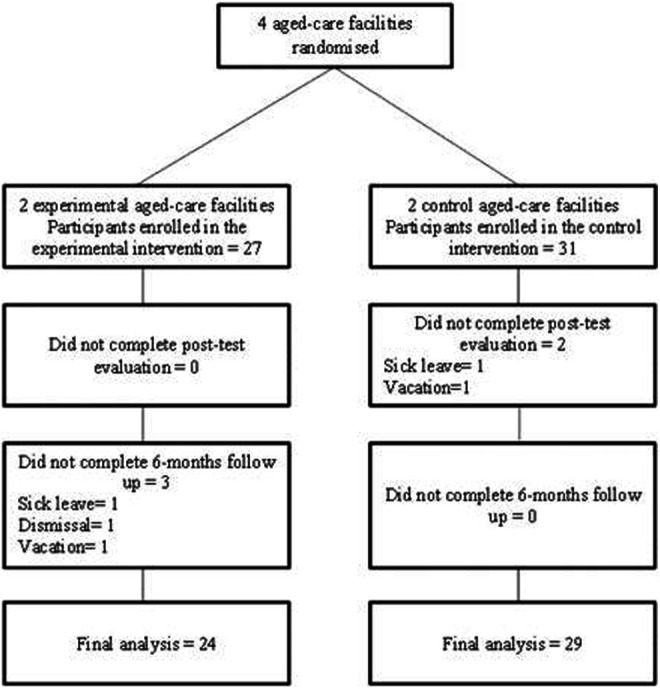
DCWs’ attrition flow chart.
The legal guardians of the identified residents were also contacted, informed about the study and asked to sign a written informed consent. From 51 residents with moderate-to-severe dementia, 47 participated (1 legal guardian refused participation, 1 resident refused permanently to be assessed by video, and 2 residents died before collecting any data).
Intervention
Person-Centered Care-Based PE Intervention
The experimental facilities received a PCC-based PE intervention informed by: (1) relevant literature on PE approaches, PCC, and dementia 11,18 ; (2) findings from a previous pilot study conducted by the authors’ research team 19 ; and (3) interviews with DCWs and managers about instrumental and emotional needs. 20 The intervention included 8 weekly 90-minute sessions, coordinated by a gerontologist and a physical therapist with training and experience in PCC approaches and psychoeducational groups. Each session followed a similar format, organized into 2 components: education and support.
The education component aimed to provide DCWs with (1) principles to integrate PCC within the care routines (eg, incorporate biographical knowledge in personal care); (2) basic knowledge about dementia; and (3) PCC-based interaction strategies, including motor stimulation (eg, encourage the person to perform one task or a part of it) and multisensory stimulation (eg, provide a gentle massage while washing resident’s hair). In the 3 days following each PE session, the gerontologist and the physical therapist assisted DCWs individually during morning care, clarifying doubts and making suggestions to help them implement a more PCC approach.
The supportive component aimed to provide DCWs with coping strategies to manage work-related stress and prevent burnout (e.g., time-management, assertiveness, and problem-solving). At the end of each supportive component, relaxation techniques, stretching, and strengthening exercises were practiced. Detailed information about the intervention can be found elsewhere 21 and is summarized in Table 1.
Table 1.
Content of the Interventions.
| Session | Component | Experimental Group | Control Group |
|---|---|---|---|
| 1 | Educative | Information about PCC and dementia: Information about the concept and principles of PCC. Basic information on dementia, its causes, symptoms, and evolution. | |
| Supportive | Emotional impact of caregiving: The positive and negative impacts of the caregiving experience on personal and professional life; abdominal breathing. | - | |
| 2 | Educative | Communication in dementia: Communicative behavioral strategies to interact with residents with dementia. (eg, give simple choices, use validation, allows time to respond, use individual’s name and eye contact). | |
| Supportive | Conflict management: Improving assertiveness through the DESC technique (Describe; Explain; Specify; Conclude) technique. 26 Stretching and strengthening exercises. | - | |
| 3 | Educative | Challenging behaviors: Information about challenging behaviors and strategies to deal with them. | |
| Supportive | Teamwork: The importance, benefits and constraints to teamwork; strategies to enhance cooperation between DCWs (eg, active listen, positive feedback). Cognitive relaxation technique. | - | |
| 4 | Educative | The environment and dementia: Strategies to enhance the physical and social environment for the person with dementia (eg, decrease background noise; post signs as reminders); information about the risk factors and strategies to prevent falls. | |
| Supportive | Dealing with emotions: Improving emotion-management strategies through the activity “six colors to think” 27 ; Stretching and strengthening exercises. | - | |
| 5 | Educative | Motor stimulation: Information about motor stimulation; strategies to enhance residents’ involvement in daily care (eg, break the small steps of an activity); and techniques for the moving and handling of residents. | |
| Supportive | Time management: The impact of poor time management on personal and professional life and tools for better time management (eg, set priorities; use a planning tool). Mental body scan. | - | |
| 6 | Educative | Multisensory stimulation—olfaction: Information about multisensory stimulation; dementia-related olfactory changes and strategies to stimulate the olfaction during the daily care (eg, use shower gel of different fragrances; place aroma diffusers in the bedroom) | |
| Supportive | Problem-solving: Using the problem-solving technique: (1) identify the problem; (2) explain the problem; (3) create solutions; (4) choose one solution; (5) plan the implementation of the solution; (6) evaluate the efficacy. Stretching and strengthening exercises | - | |
| 7 | Educative | Multi-sensory stimulation—vision and tactile stimulation: The importance of vision and touch for people with dementia, dementia-related visual and tactile changes; strategies to stimulate the vision (eg, reality orientation) and touch (eg, hand massage during bath) | |
| Supportive | Relaxation: Yoga | - | |
| 8 | Educative | Multi-sensory stimulation—audition and taste: The importance of audition and taste for people with dementia; dementia-related audition and taste changes; strategies to stimulate the audition (eg, listen to residents’ favorite song) and taste (eg, brush the person’s teeth with toothpastes of different flavors). | |
| Celebration and finalization | |||
Abbreviations: DCW, direct care worker; PCC, person-centered care.
Person-Centered Care-Based Education-Only Intervention
The control facilities received an education-only intervention. The coordination, length, order, and content of the sessions were the same as the educational component of the PE intervention. It was the absence of the supportive component that distinguished both interventions. Each participant was assisted during morning care by the same professionals who helped DCWs to deliver a more PCC and clarified doubts that emerged from sessions.
Measures
Direct Care Workers’ Perceived Stress
The DCWs’ perceived stress was measured using the Portuguese version of the Perceived Stress Scale (PSS). 22 The PSS is a 14-item self-report questionnaire rated on a 5-point Likert-type scale ranging from “never” (0) to “very often” (4). The items evaluate the degree to which individuals believe their life has been unpredictable, uncontrollable, and overloaded during the previous month. Higher scores correspond to higher degrees of perceived stress.
The Cronbach’s α coefficient of the scale showed a score of α = .8. Scores for the criterion validity ranged between 0.4 and 0.8, and the examination of the factorial validity with the 1-factor structure accounted for 43.96% of variance. Overall, the acceptable psychometric properties of the Portuguese version of the PSS are similar to those obtained in other versions. 23
Direct Care Workers’ Burnout
The 22-item Maslach Burnout Inventory (MBI) Human Services Survey was used to assess the DCWs’ experience of burnout. 24 The MBI is the most widely used instrument to assess burnout and is divided into 3 subscales: 8 items assess emotional exhaustion (EE), that is, feelings of being emotionally exhausted by one’s work; 5 items measure depersonalization (DP), that is, the negative attitudes toward recipients’ care or treatment; and 8 items assess personal accomplishment (PA), that is, feelings of competence and successful achievement in work. The respondents are asked to report the frequency with which such feelings are experienced on a 7-point Likert-type scale, ranging from “never” (0) to “every day” (6). A combination of high scores on EE and DP and a low score on PA correspond to a high level of burnout. The Cronbach’s α coefficient for the Portuguese version showed a score of α = 0.75 and reliability coefficients of 0.80 for EE, 0.71 for DP, and 0.70 for PA. The validity of the three-factor structure of the MBI was found to provide a reasonable fit to the data, explaining 43.4% of the total variance. The psychometric properties of the used version are consistent with the ones of previous studies. 25
Direct Care Workers’ Job Satisfaction
The short-form Minnesota Satisfaction Questionnaire (MSQ) 28 was used to assess DCWs’ job satisfaction. It includes 20 items rated on a 5-point Likert scale ranging from “extremely dissatisfied” (1) to “extremely satisfied” (5). Item responses are summed or averaged to create a total score—the lower the score, the lower the level of job satisfaction. Besides a total score, the MSQ can also be scored for intrinsic and extrinsic satisfaction. The intrinsic subscale includes 6 items with scores ranging between 1 and 30 and refers to how people feel about the nature of the job tasks themselves. The extrinsic satisfaction subscale contains 8 items ranging from 8 to 40 and refers to how people feel about aspects of the work situation that are external to the job tasks. The psychometric properties of the used version of the MSQ are acceptable. High internal consistency was found for the global scale (α = .93) and for the intrinsic (α = .88) and extrinsic subscales (α = .82). These values are higher than the ones found for the original scale. 26 Strong test–retest correlations were found (>.80), which denotes adequate stability coefficients and corroborates the findings obtained in previous studies. 29 The factorial analysis confirmed the adequacy of the 2-factor structure of the MSQ, which explained 62.69% of the total variance.
Direct Care Workers’ Person-Centered Communication
In order to capture both DCWs’ verbal and nonverbal communicative behaviors, video-recordings of morning care routines were used. Video-recordings were performed in the resident’s bedroom; the moment DCWs entered the room was defined as the starting point and when they left the room as the ending point. Bathing was not recorded to assure privacy to the person with dementia. Some procedures were followed to minimize participants’ or residents’ reactivity (ie, response during data collection that affects the natural course of behavior as a result of being observed): (1) prior to data collection, several video-recordings were performed in order to familiarize participants with the methodology; (2) DCWs were instructed to stop or remove the video camera if they noticed any resident’s negative reaction caused by the device presence; and (3) once the cameras were placed on a tripod and adequately positioned, the researcher left the room so that a further source of disruption could be avoided.
To prevent random DCWs’ communicative behaviors, DCWs were video-recorded thrice at each assessment point. In total, 474 morning care sessions were video-recorded. At baseline, 3 participants were only recorded twice as they were absent from work.
The DCWs’ communicative behavior was studied by analyzing the frequency and duration of a list of mutually exclusive behaviors (ethogram). The categories described in the Kitwood’s dialectical framework, 10 relevant literature on staff’s verbal and nonverbal communication 30,31 and preliminary observations of the video-recordings informed the construction of the ethogram. The final list comprised 18 verbal communicative behaviors (Table 2) and 8 nonverbal communicative behaviors (Table 3). One coder (first author) rated the DCWs’ communicative behaviors according to the ethogram using specialized software, Noldus Observer XT (version 11.0; Noldus International Technology, Wageningen, the Netherlands). The coder was previously trained to use the software.
Table 2.
Verbal Communicative Behaviors.
| Categories | Description |
|---|---|
| Consult | Consulting the person with dementia about his or her preferences, desires, and needs. Includes questions that invite resident’s judgment. Examples include:
|
| Inform | Guiding the resident in terms of what to expect and providing information about what is going to happen during the task. Examples include:
|
| Involve | Giving the resident the opportunity to take care for himself herself as much as possible and just “completing” the care task when necessary. Examples include:
|
| Reward | Rewarding the person and his or her behavior, giving compliments and using expressions of encouragement. Examples include:
|
| Validate | Acknowledging the subjective reality of a person’s emotions and feelings, and giving a response on the feeling level, without correcting the residents’ reality or frame of reference, even if it is chaotic. Using statements to interpret or recognize the emotional state of the resident during the interaction. Examples include:
|
| Assess comfort | Conveying interest and concern for the welfare and comfort of the person with dementia. Examples include:
|
| Distract | Amusing the person through humorous commentaries or distracting him or her in a positive way by guiding the conversation away from something unpleasant. |
| Sensory stimulation | Providing sensory information, without the intervention of concepts and intellectual understanding; for example through music, touch or aromas. Examples include:
|
| Conversation about the person | Showing interest in the resident’s life or background. Examples include:
|
| Social conversation | Friendly conversation that conveys an interest in the resident and is not related to instrumental care. Includes statements that acknowledge that the resident said something. Examples include:
|
| Task-oriented conversation | Communication that is related to task accomplishment or focused on nursing or therapeutic topics. Examples include:
|
| Conversation with a third person | Communication to a third person. Examples include:
|
| Ignore | Ignoring residents’ statements by responding with an unrelated statement or question, interrupting, or changing the topic of conversation. Carrying on a conversation in the presence of a person as if he or she is not present. Examples include:
|
| Infantilize | Patronizing or treating and talking to the person with dementia as if he or she was a child. Examples include:
|
| Invalidate | Failing to acknowledge the subjective reality of a person’s experience and especially what he or she is feeling. Correcting the resident on cognitive facts. Examples include:
|
| Mockery | Disdain, pointing out or making fun of residents’ behavior or actions. Placing the person toward his or her difficulties. Examples include:
|
| Criticize | Showing disapproval or criticize residents’ performance or behavior. Examples include: • That’s wrong. You are hopeless. |
| Impose | Forcing a person to do something, overriding desire or denying the possibility of choice on his or her part. Statements can be considered dominating or controlling. Examples include:
|
Table 3.
Nonverbal Communicative Behaviors.
| Affirmative Nodding | Nodding head as a sign of approval, encouragement, or interest in the resident. |
| Resident-Directed Eye Gaze | Looking at the face of the resident. |
| Smile | Expression in which the corners of the mouth are directed upwards, denoting affability toward the resident. |
| Laugh | Opening the mouth (totally or partially), making a sound commonly associated with the act of laughing. |
| Withholding | Refusing a residents’ request or question. Includes statements from the resident that the DCW does not acknowledge (eg, resident asks if she can return to her room and the DCW does not respond). |
| Affective touch | Spontaneous and affective touch that is not necessary for the completion of a task (eg, a pat on the back, a hug). |
| Guiding touch | Using touch to draw the person’s attention or guide him or her for a task. |
| Instrumental touch | Deliberate physical contact, which is necessary for the completion of a task. |
Abbreviation: DCW, direct care worker.
Data Analysis
Repeated measures ANOVA were used to determine the existence of significant differences on DCWs’ perceived stress, burnout, job satisfaction, and person-centered interactions at 3 points in time. Specifically, a series of 1 between-subjects variable (experimental vs control) and 1 within-subjects variable (pretest, posttest, and follow-up) repeated measures ANOVA was performed. This statistical technique was used to test intervention, time, and intervention by time interaction effects. Partial η2, which corresponds to the Effect Size, was interpreted as small (≥.05), medium (.05-.25), large (.25-.50), and very large (≥.50). 32 All variables were previously tested for normality. The level of significance was set at 0.05. All analyses were conducted using the SPSS v20.0 (IBM Corp., Armonk, New York).
Interobserver Reliability
Interobserver reliability with 2 independent coders was performed for 30% of the videos. This value is similar to those of previous studies. 33 The frequency and duration of each category in each moment were considered, using the intraclass correlation coefficient (ICC) equation (2.1) and the Bland and Altman method. The ICC(2,1) values were interpreted as follows: >0.75 was excellent, 0.40 to 0.75 was moderate, and <0.40 was poor. 34 The results ranged between 0.45 and 1.0, indicating a moderate to excellent reliability.
Bland and Altman 95% limits of agreement were measured, and the scatter plots were analyzed for all categories. A good agreement between the coders was found and no evidence of systematic bias was observed.
Comparison of Sample at Baseline
The experimental and control groups were compared on the basis of demographic variables and measured outcomes. Significance was set at the .05 level. The t test for independent samples was used to compare the 2 groups on the basis of age and length of service and DCWs’ outcomes; χ2 tests were used to compare the 2 groups on the basis of dichotomous variables, including gender, education, and marital status. Participants were all female with a mean age of 44.72 ± 9.02 years. The majority were married (67.2%), 46.4% had primary and middle school education, and 41.4% high school. The average length of service was 9.61 ± 3.72 years. None of the differences were statistically significant at baseline (Table 4).
Table 4.
DCWs’ Sociodemographic Characteristics.
| Outcome | Total (n = 58) | Experimental Group (n = 27) | Control Group (n = 31) | P Value |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Gender | ||||
| Female | 58 (100.0) | 27 (100.0) | 31 (100.0) | - |
| Age in years | ||||
| M (SD) | 44.72 (9.02) | 43.37 (10.00) | 45.90 (8.04) | .290a |
| Marital status | ||||
| Married | 39 (67.2) | 17 (63.0) | 22 (71.0) | .887b |
| Widowed | 3 (5.2) | 1 (3.7) | 2 (6.5) | |
| Single | 4 (6.9) | 2 (7.4) | 2 (6.5) | |
| Divorced/ separated | 9 (15.5) | 5 (15.5) | 4 (12.9) | |
| Other | 3 (5.2) | 2 (7.4) | 1 (3.2) | |
| Education | ||||
| Primary school | 15 (25.9) | 4 (14.8) | 11 (35.5) | .144b |
| Middle school | 12 (20.7) | 6 (22.2) | 6 (19.4) | |
| High school | 24 (41.4) | 11 (40.7) | 13 (41.9) | |
| College degree | 1 (1.7) | 1 (3.7) | 0 (0.0) | |
| Other | 6 (10.3) | 5 (18.5) | 1 (3.2) | |
| Length of service, years | ||||
| M (SD) | 9.61 (3.72) | 9.84 (4.86) | 9.42 (2.51) | .678a |
Abbreviations: M, mean; SD, standard deviation; DCW, direct care worker.
a t test.
bχ2.
Results
Direct Care Workers’ Perceived Stress, Burnout. and Job Satisfaction
Data concerning DCWs’ outcomes is displayed in Table 5. A negative significant time interaction effect was obtained on perceived stress, with both groups reporting higher scores at 6-month follow-up than at baseline and immediately after the intervention (P > .001). Effect sizes were large (η2 = 0.36).
Table 5.
Changes in DCWs’ Stress, Burnout, and Job Satisfaction.
| Outcome | Experimental Group (n = 24) | Control Group (n = 29) | Time Effect | ES | Group × Time Effect | ES | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 | T2 | T3 | |||||
| Mean (SD) | Mean (SD) | |||||||||
| PSS | 19.42 (5.90) | 18.79 (6.48) | 27.25 (4.59) | 20.55 (6.31) | 20.10 (4.79) | 25.55 (6.99) | F = 28.255, df(2) P = .000 | 0.36 | F = 1.346, df(2) P = .265 | 0.03 |
| MBI | ||||||||||
| Emotional Exhaustion | 17.0 (11.41) | 15.8 (8.60) | 13.82 (9.76) | 12.67 (10.59) | 15.42 (9.72) | 16.25 (10.70) | F = 0.132, df(2) P = .876 | 0.00 | F = 2.145, df(2) P = .123 | 0.05 |
| Depersonalization | 5.25 (5.05) | 6.88 (6.40) | 3.20 (3.85) | 6.07 (5.71) | 5.52 (4.01) | 6.54 (5.89) | F = 0.848; df(2) P = .431 | 0.02 | F = 3.048, df(2) P = .052 | 0.06 |
| Personal accomplishment | 40.42 (4.94) | 38.54 (8.42) | 39.50 (5.80) | 40.69 (6.20) | 37.31 (8.02) | 34.17 (8.48) | F = 4.604, df(2) P = .012 | 0.08 | F = 2.649, df(2) P = .076 | 0.05 |
| MSQ | ||||||||||
| MSQ intrinsic | 24.29 (2.31) | 24.00 (2.16) | 24.33 (2.16) | 22.55 (4.19) | 21.55 (3.53) | 20.62 (5.19) | F = 1.619, df(2) P = .203 | 0.03 | F = 1.733; df(2) P = .182 | 0.01 |
| MSQ extrinsic | 26.58 (4.67) | 26.37 (3.56) | 26.04 (4.42) | 24.62 (4.84) | 25.59 (4.15) | 26.55 (6.41) | F = 0.635, df(2); P = .532 | 0.04 | F = 2.007; df(2); P = .140 | 0.04 |
| Total | 72.96 (5.99) | 73.83 (8.48) | 72.29 (7.92) | 68.14 (9.05) | 68.55 (10.13) | 68.48 (15.38) | F = 0.209, df(2) P = .811 | 0.00 | F = 0.163, df(2) P = .849 | 0.00 |
Abbreviations: M, mean; SD, standard deviation; ES, effect sizes; df, degrees of freedom; PSS, Perceived Stress Scale; MBI, Maslach Burnout Inventory; MSQ, Minnesota Satisfaction Questionnaire.
Analyses showed a significant time interaction effect on the MBI subscale PA. After a decrease in PA scores immediately after the PE intervention, at 6 months, scores had improved in the experimental group, and the control group showed a decline over time in this variable (P > .05). Effect sizes were moderate (η2 = .08). Although no significant differences were found for the remaining MBI subscales, DCWs from the PE intervention showed improved levels of EE and DP at 6-month follow-up. In the control group, the values of all the MBI subscales deteriorated at 6-month follow-up.
No significant differences were obtained for total, intrinsic, or extrinsic job satisfaction. A modest but positive change on total job satisfaction from pre- to posttest, followed by a deterioration at 6-month follow-up, was found for both groups.
Direct Care Workers’ Person-Centered Communication
Data concerning DCWs’ person-centered communication can be found in Table 6.
Table 6.
Changes in DCWs’ Verbal and Nonverbal Communicative Behavior.
| Categories | Type | Experimental Group (n = 24) | Control Group (n = 29) | Time, P Value | Partial η2 | Group × Time, P Value | Partial η2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 Mean (SD) | T3 | T1 | T2 Mean (SD) | T3 | |||||||
| Verbal communicative behavior | ||||||||||||
| Consult | Freq | 1.02 (1.02) | 1.05 (1.13) | 0.82 (1.05) | 1.60 (1.83) | 1.24 (1.28) | 0.80 (1.18) | .097 | 0.05 | 0.412 | .02 | |
| Inform | Freq | 8.69 (4.40) | 9.45 (5.60) | 4.70 (3.68) | 8.23 (4.41) | 6.99 (3.91) | 6.98 (5.20) | .013a | 0.16 | 0.008a | .18 | |
| Involve | Freq | 3.46 (3.15) | 3.55 (3.20) | 4.85 (3.03) | 3.50 (3.28) | 6.13 (2.72) | 5.00 (2.64) | .027a | 0.07 | 0.100 | .05 | |
| Dur | 13.06 (14.92) | 17.58 (18.04) | 24.00 (14.88) | 19.14 (21.89) | 28.68 (18.94) | 21.36 (12.61) | .053 | 0.06 | 0.099 | .05 | ||
| Reward | Freq | 1.37 (1.49) | 1.81 (1.72) | 1.49 (1.70) | 0.75 (0.70) | 1.34 (1.17) | 1.38 (1.25) | .048a | 0.06 | 0.454 | .02 | |
| Validate | Freq | 0.32 (0.70) | 0.35 (0.83) | 0.02 (0.10) | 0.13 (0.34) | 0.17 (0.34) | 0.03 (0.10) | .006a | 0.37 | 0.101 | .02 | |
| Assess comfort | Freq | 0.35 (0.48) | 0.35 (0.48) | 0.19 (0.32) | 0.38 (0.58) | 0.43 (0.79) | 0.49 (0.74) | .964 | 0.00 | 0.531 | .01 | |
| Distract | Freq | 0.41 (0.84) | 0.55 (1.13) | 0.09 (0.21) | 0.25 (0.60) | 0.15 (0.34) | 0.08 (0.17) | .486 | 0.00 | 0.130 | .04 | |
| Sensory stimulation | Freq | 0.12 (0.23) | 0.33 (0.46) | 0.32 (0.42) | 0.11 (0.33) | 0.32 (0.82) | 0.44 (1.45) | .023a | 0.09 | 0.904 | .00 | |
| Dur | 0.60 (1.74) | 1.71 (2.78) | 2.06 (3.11) | 0.34 (0.98) | 3.08 (9.59) | 1.06 (3.55) | .129 | 0.44 | 0.399 | .01 | ||
| Social conversation | Freq | 4.69 (2.64) | 5.28 (2.84) | 5.19 (3.00) | 6.44 (451) | 6.95 (4.18) | 6.13 (3.09) | .306 | 0.02 | 0.993 | .00 | |
| Dur | 33.39 (30.55) | 43.79 (23.04) | 46.75 (40.92) | 37.30 (25.44) | 49.74 (33.38) | 63.40 (45.99) | .009b | 0.55 | 0.732 | .00 | ||
| Conversation about the person | Freq | 0.02 (0.11) | 0.03 (0.14) | 0.02 (0.08) | 0.12 (0.25) | 0.06 (0.16) | 0.07 (0.17) | .509 | 0.00 | 0.210 | .03 | |
| Dur | 0.09 (0.35) | 0.43 (2,09) | 0.05 (0.23) | 1.17 (2.76) | 0.80 (2.08) | 1.99 (8.08) | .907 | 0.55 | 0.09 | .01 | ||
| Instrumental conversation | Freq | 2.79 (2.10) | 2.50 (2.37) | 3.18 (2.62) | 2.10 (1.66) | 1.94 (1.15) | 2.81 (2.34) | .608 | 0.00 | 0.972 | .00 | |
| Dur | 13.41 (11.25) | 10.68 (9.81) | 19.43 (19.03) | 10.73 (9.85) | 10.73 (9.96) | 15.01 (13.96) | .040a | 0.62 | 0.082 | .01 | ||
| Conversation with others | Freq | 5.14 (4.02) | 4.86 (2.93) | 3.89 (2.84) | 5.55 (4.06) | 4.02 (2.89) | 3.89 (2.84) | .006a | 0.09 | 0.462 | .01 | |
| Dur | 21.33 (17.63) | 25.32 (14.81) | 20.52 (13.83) | 14.68 (17.90) | 20.77 (12.02) | 19.14 (12.52) | .182 | 0.04 | 0.628 | .01 | ||
| Ignore | Freq | 1.82 (1.47) | 1.70 (1.73) | 2.14 (2.07) | 2.12 (2.10) | 1.63 (1.56) | 1.65 (1.75) | .613 | 0.00 | 0.457 | .02 | |
| Infantilize | Freq | 0.02 (0.09) | 0.00 | 0.00 | 0.28 (0.51) | 0.12 (0.28) | 0.21 (0.42) | .334 | 0.02 | 0.409 | .02 | |
| Invalidate | Freq | 0.07 (0.27) | 0.00 | 0.02 (0.07) | 0.13 (0.25) | 0.17 (0.39) | 0.20 (0.10) | .909 | 0.00 | 0.418 | .02 | |
| Mockery | Freq | 0.11 (0.22) | 0.09 (0.22) | 0.34 (0.70) | 0.54 (0.69) | 0.25 (0.44) | 0.57 (1.12) | .074 | 0.05 | 0.543 | .01 | |
| Criticize | Freq | 0.47 (0.73) | 0.07 (0.25) | 0.28 (0.49) | 0.46 (0.72) | 0.57 (0.75) | 0.24 (0.53) | .386 | 0.02 | 0.051 | .06 | |
| Impose | Freq | 0.49 (0.89) | 0.16 (0.37) | 0.37 (0.60) | 0.56 (0.58) | 0.83 (1.57) | 0.22 (0.47) | .228 | 0.059 | 0.104 | .09 | |
| Nonverbal communicative behavior | ||||||||||||
| Affirmative Nodding | Freq | 0.45 (0.85) | 0.74 (1.16) | 0.22 (0.65) | 0.55 (0.84) | 0.51 (0.99) | 0.72 (1.19) | .630 | 0.02 | 0.170 | .07 | |
| Resident-directed eye gaze | Freq | 1.90 (1.99) | 2.08 (1.93) | 0.85 (0.98) | 1.91 (2.36) | 2.03 (2.26) | 1.91 (2.34) | .106 | 0.05 | 0.169 | .04 | |
| Dur | 19.18 (32.24) | 26.56 (40.08) | 4.17 (6.03) | 25.43 (56.24) | 19.68 (33.73) | 11.69 (17.92) | .032a | 0.07 | 0.461 | .02 | ||
| Smile | Freq | 0.32 (0.62) | 0.35 (0.62) | 0.33 (0.43) | 0.31 (0.86) | 0.23 (0.54) | 0.85 (1.21) | .120 | 0.08 | 0.109 | .09 | |
| Dur | 0.61 (1.25) | 0.71 (1.76) | 1.29 (3.12) | 2.65 (11.90) | 0.89 (2.11) | 5.99 (13.81) | .199 | 0.03 | 0.373 | .02 | ||
| Laugh | Freq | 1.15 (1.05) | 1.78 (1.71) | 0.94 (1.12) | 1.01 (1.01) | 0.62 (0.82) | 1.03 (1.14) | .526 | 0.01 | 0.004a | .106 | |
| Dur | 9.24 (17.38) | 7.39 (12.30) | 8.61 (19.40) | 10.28 (29.11) | 2.10 (3.03) | 3.75 (5.09) | .550 | 0.01 | 0.934 | .001 | ||
| Withholding | Freq | 0.41 (0.76) | 0.06 (0.16) | 0.00 | 0.08 (0.23) | 0.01 (0.06) | 0.07 (0.29) | .024a | 0.114 | 0.06 | .11 | |
| Affective touch | Freq | 0.69 (0.57) | 0.68 (0.62) | 0.48 (0.56) | 1.18 (1.33) | 0.75 (1.00) | 0.94 (1.28) | .324 | 0.02 | 0.393 | .02 | |
| Dur | 2.22 (3.28) | 1.69 (1.96) | 1.86 (3.61) | 3.53 (4.42) | 4.05 (9.03) | 3.68 (7.08) | .992 | 0.00 | 0.854 | .00 | ||
| Instrumental touch | Freq | 10.33 (2.61) | 10.21 (2.90) | 10.82 (2.25) | 9.82 (2.79) | 8.99 (2.34) | 10.44 (2.92) | .085 | 0.05 | 0.616 | .01 | |
| Dur | 281.06 (169.8) | 311.31 (52.67) | 296.29 (43.72) | 326.37 (251.40) | 268.9 (69.58) | 284.08 (51.45) | .849 | 0.00 | 0.27 | .03 | ||
| Awareness touch | Freq | 0.16 (0.49) | 0.56 (1.39) | 0.23 (0.38) | 0.44 (0.71) | 0.44 (0.61) | 0.43 (0.63) | .343 | 0.02 | 0.34 | .02 | |
Abbreviations: Freq, frequency; SD, standard deviation; DSW, direct care worker.
a P < 0.05.
b P < 0.001.
Within the PE group, the frequency of the majority (24 of 26 behaviors) of person-centered behaviors improved immediately after the intervention (T2). However, 22 of 26 behaviors dropped at 6-month follow-up. For 10 of these behaviors, the frequencies were lower than those found at baseline. Among these, significant time and group interaction effects were found for the frequency of “inform” (P > .01, η2 partial = .18) and “laugh” (P > .01, η2 partial = .10). In the PE group, their frequency improved from T1 to T2 and dropped at follow-up. In the control group, the frequency of inform reduced at T2, and values were sustained at follow-up, whereas laugh improved at follow-up. Also, significant time effects were obtained for the frequency of “validation” (P > .01, η2 partial = .10) and “play” (P > .05, η2 partial = .07), with both groups experiencing a decline over time in these variables. Improvements were noticed in the frequency of “involvement,” “withholding,” and “orientation.” Positive significant time effects were found for the frequency of the first 2 behaviors. The frequency of involvement (P > .05, η2 partial = 0.07) and withholding (P > .05, η2 partial = 0.11) improved over time in the experimental group and reduced at 6-month follow-up in the control group.
Concerning the duration of person-centered interactions, an improvement in 8 of 11 variables was noticed. Among these, a significant time effect was found for the duration of “social conversation” (P > .01, η2 partial = .09), with both groups reporting an improvement over time in this variable. Declines over time were found for “conversation about the person,” “instrumental conversation,” and “resident-directed eye gaze.” Significant time effects were obtained for the duration of instrumental conversation (P > .05, η2 partial = .08) and resident-directed eye gaze (P > .05, η2 partial = .07), with the experimental and control groups deteriorating over time.
Discussion
This study sought to examine the effects of a PCC-based PE intervention on DCWs’ stress, burnout, job satisfaction, and person-centered communication. Findings suggest that a PE intervention can positively impact DCWs’ burnout. Compared to DCWs in the control group, those who received the PE intervention reported a decrease in their levels of burnout (with significant findings found for the MBI subscale PA) at both postintervention and 6-month follow-up. This promising result suggests that, over time, adding a supportive component to PCC-training might enable DCWs to feel pleased about themselves and satisfied with their accomplishments on the job.
The findings did not support the hypothesis that, compared to education-only intervention, a PE intervention would improve DCWs’ job satisfaction. A modest but positive change on total job satisfaction from pre- to posttest, followed by a deterioration at 6-month follow-up, was found for both groups. One explanation for these results might be related to the measure used to assess job satisfaction. The MSQ is based on the conceptualization of job satisfaction as a multidimensional construct, considering several aspects that were not covered by the intervention (eg, managers’ support and organization conditions). Also, despite the guarantee of confidentiality, participants might have been reluctant to answer questions related to leadership’s role or policies of the organization. The individual assistance during morning care in both groups can also offer some light about the lack of significant differences between groups. By allowing workers to have immediate guidance and support to handle challenging situations, it can have an independent effect on DCWs’ job satisfaction. The extent to which individual assistance may impact DCWs’ outcomes requires further consideration.
Strongest effects were found immediately after the intervention, with diminishing strength at the 6-month follow-up, on perceived stress and on most DCWs’ person-centered communicative behaviors. Several reasons may explain these findings. First, the intervention ran for a short period of time (8 weeks). As it is important to keep DCWs under intervention long enough so they can experience lasting positive changes, maintenance strategies, such as “booster sessions” (ie, brief, periodic contacts intended to remind participants of intervention goals or encourage them to continue using the learned skills) are clearly needed. Moreover, it is possible that the results have been influenced by uncontrolled factors, such as the facility organizational culture. Contextual factors, in particular a supportive leadership and a reward culture of openness and accuracy, have been repeatedly cited in the literature as critically important to the success of interventions in terms of outcomes for DCWs. 35 According to the literature, DCWs are often not acknowledged by their managers and feel that their work is unappreciated, which negatively affects their state of well-being and care provision. 21 Therefore, efforts in improving leadership and management skills can be determinant to engender more positive impacts on DCWs. This might involve, for example, training to prepare for the challenges of leading change and support to provide adequate staff supervision and positive feedback systems. 35 However, more research is needed to determine what leadership skills can indeed be helpful. Another factor may be related to the progressive nature of dementia, which means that the symptoms gradually worsen over time increasing DCWs’ stress and reducing job satisfaction. Also, the increased perceived stress at 6-month follow-up can be the result of an enhanced DCWs’ awareness of stress on the job; the repeatedly completion of a measure on perceived stress may contribute to increase DCWs’ understanding and consciousness of stress over time. At last, the possible pressure to provide better care after the interventions could have triggered higher stress levels. Nevertheless, some person-centered behaviors were positively affected by the PE intervention and should be highlighted. Direct care worker from the experimental group experienced a significant improvement in the frequency of involvement and withholding and in the duration of social conversation. Also, positive but no significant improvements were found in the duration of multisensory stimulation and several nonverbal communicative behaviors, including smile, laugh, and affective touch. These are promising results as it is becoming increasingly acknowledged that good dementia care is underpinned by interpersonal relationships between people with dementia and DCWs that rely more on emotional, sensitive, and empathetic interactions rather than on verbal expressiveness. 9 The fact that at 6-month follow up results were more positive for the duration of behaviors suggests that DCWs spend more time communicating with fewer interruptions. Besides, these findings indicate that DCWs might have selected over time those communicative behaviors that showed to be more effective, making more use of them.
Results must be, however, interpreted with caution as DCWs were not always recorded with the same resident and this may have influenced the results. Future studies should try to create and follow the same dyads. Besides, DCWs’ performance, particularly immediately after the intervention, may have been influenced by the “Hawthorne effect,” which means that DCWs being aware of video-recording possibly behaved differently. The DCWs’ familiarization with the methodology may have minimized this effect at 6-month follow-up. 36
Other methodological limitations are also to be considered. The sample size was relatively small and might have reduced the statistical power to detect more significant changes. Hence, when cluster designs are used, there are 2 sources of variance in the observations: the variability of patients within a cluster and the variability between clusters. These 2 sources combine to produce an increase in the variance and both must be considered in the analysis. The effect of the increased variance due to a cluster design is to increase the size of the standard errors and thus to widen confidence intervals and increase P values, compared with a study of the same size using individual randomization. 37 In effect, the sample size is reduced and power is lost, and thus, sample sizes have to be inflated. Moreover, it was not possible to blind researchers to the experimental or control groups or assessments. Future studies with a double-blinded design should be conducted to clarify the findings.
Nevertheless, our findings are of interest as they provide evidence that a PE intervention may be an effective approach to reduce DCWs’ burnout levels and improve person-centered behaviors. Further research is warranted to determine the extent of the benefits of this approach on residents with dementia and on other DCWs’ outcomes such as depression, anxiety, and perceived mastery. One of the strengths of the study is the consideration of a 6-month follow-up evaluation. This is important as most studies tend to rely only on pre and immediate posttest assessments. 17 Also, the use of video-recording provided a suitable method to assess interactions. Video-recording enables replaying and reviewing the data, to control the observer’s fatigue and to achieve deeper levels of observation and analysis that are not possible to achieve by means of real-time observations. 37 The high interobserver reliability obtained for the ethogram further supports its reliability and validity to measure PCC interactions. Yet, conducting future evaluations of the ethogram in order to further develop its acceptability, utility and validity are strongly recommended.
Overall, the results suggested that providing DCWs with training and emotional support is more effective in reducing burnout and improve adequate communicative behaviors than an education-only intervention. These findings highlight the importance of interventions in dementia care settings to go beyond DCWs’ knowledge and instrumental skills to also address emotional skills. The addition of booster follow-up sessions to help maintain and extend the positive long-term effects of the intervention is highly encouraged. Also, DCWs’ outcomes are largely associated to factors within the organization, thus culture-change initiatives (eg, breaking down hierarchies, leadership commitment, and DCWs empowerment) are further encouraged, as this is determinant to achieve and sustain practice changes.
Acknowledgments
The authors gratefully acknowledge all institutions and DCWs for their participation in this study.
This article was accepted under the editorship of the former Editor-in-Chief, Carol F. Lippa.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grants (grant numbers SFRH/BD/72460/2010 and RIPD/CIF/109464/2009) from the Foundation for Science and Technology (FCT).
References
- 1. Alzheimer’s Disease International. World Alzheimer Report 2013: An Analysis of Long-Term Care for Dementia. London: Alzheimer’s Disease International; 2013. [Google Scholar]
- 2. Stone R. The Long-Term Care Workforce: From Accidental to Valued Profession. In: Wolf D, Folbre N, eds. Universal Coverage of Long-Term Care in the United States: Can We Get There from Here? New York, NY: Russell Sage Foundation; 2012:155–178. [Google Scholar]
- 3. Gray-Stanley JA, Muramatsu N. Work stress, burnout, and social and personal resources among direct care workers. Res Dev Disabil. 2011;32(3):1065–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Edberg AK, Bird M, Richards DA, Woods R, Keeley P, Davis-Quarrell V. Strain in nursing care of people with dementia: Nurses’ experience in Australia, Sweden and United Kingdom. Aging Ment Health. 2008;12(2):236–243. [DOI] [PubMed] [Google Scholar]
- 5. Edvardsson D, Sandman P, Nay R, Karlsson S. Predictors of job strain in residential dementia care nursing staff. J Nurs Manag. 2009;17(1):59–65. [DOI] [PubMed] [Google Scholar]
- 6. Menne HL, Ejaz FK, Noelker LS, Jones JA. Direct Care Workers’ Recommendations for Training and Continuing Education. Gerontol Geriatr Educ. 2007;28(2):91–108. [DOI] [PubMed] [Google Scholar]
- 7. Nolan M, Davies S, Brown J, et al. The role of education and training in achieving change in care homes: a literature review. J Res Nurs. 2008;13(5):411–433. [Google Scholar]
- 8. Nolan M, Davies S, Brown J, Keady J, Nolan J. Beyond person-centred care: a new vision for gerontological nursing. J Clin Nurs. 2004;13(3a):45–53. [DOI] [PubMed] [Google Scholar]
- 9. Brooker D. Person-Centred Dementia Care: Making Services Better. London: Jessica Kingsley Publishers; 2007. [DOI] [PubMed] [Google Scholar]
- 10. Kitwood T. Dementia Reconsidered: The Person Comes First. Buckingham: Open University Press; 1997. [Google Scholar]
- 11. Chenoweth L, King MT, Jeon YH, et al. Caring for Aged Dementia Care Resident Study (CADRES) of person-centred care, dementia-care mapping, and usual care in dementia: a cluster-randomised trial. Lancet Neurol. 2009;8(4):317–325. [DOI] [PubMed] [Google Scholar]
- 12. Fossey J. Effect of enhanced psychosocial care on antipsychotic use in nursing home residents with severe dementia: cluster randomised trial. BMJ. 2006;332(7544):756–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sloane PD, Hoeffer B, Mitchell CM, et al. Effect of person-centered showering and the towel bath on bathing-associated aggression, agitation, and discomfort in nursing home residents with dementia: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(11):1795–1804. [DOI] [PubMed] [Google Scholar]
- 14. Sidani S, Streiner D, Leclerc C. Evaluating the effectiveness of the abilities-focused approach to morning care of people with dementia. Int J Older People Nurs. 2012;7(1):37–45. [DOI] [PubMed] [Google Scholar]
- 15. Edvardsson D, Winblad B, Sandman P. Person-centred care of people with severe Alzheimer’s disease: current status and ways forward. Lancet Neurol. 2008;7(4):362–367. [DOI] [PubMed] [Google Scholar]
- 16. van den Pol-Grevelink A, Jukema JS, Smits CH. Person-centred care and job satisfaction of caregivers in nursing homes: a systematic review of the impact of different forms of person-centred care on various dimensions of job satisfaction. Int J Geriatr Psychiatry. 2012;27(3):219–229. [DOI] [PubMed] [Google Scholar]
- 17. Barbosa A, Sousa L, Nolan M, Figueiredo D. Effects of person-centered care approaches to dementia care on staff: A systematic review[published online January 20, 2014.]. Am J Alzheimers Dis Other Dement. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Van Weert J, Vandulmen A, Spreeuwenberg P, Ribbe M, Bensing J. Effects of snoezelen, integrated in 24h dementia care, on nurse–patient communication during morning care. Patient Educ Counsel. 2005;58(3):312–326. [DOI] [PubMed] [Google Scholar]
- 19. Figueiredo D, Barbosa A, Cruz J, Marques A, Sousa L. Empowering staff in dementia long-term care: Towards a more supportive approach to interventions. Educ Gerontol. 2013;39(6):413–427. [Google Scholar]
- 20. Barbosa A, Nolan M, Sousa L, Figueiredo D. Psycho-educational approaches in long-term care homes: Direct care workers and managers' perspectives. Procedia Soc Behav Sci. 2014;131:406–410. [Google Scholar]
- 21. Barbosa A, Nolan M, Sousa L, Figueiredo D. Supporting direct care workers in dementia care: effects of a psychoeducational intervention. Am J Alzheimers Dis Other Demen. 2015;30(2):130–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pais Ribeiro J, Marques T. A avaliação do stresse: a propósito de um estudo de adaptação da escala de percepção de stresse. Psicologia, Saúde & Doenças. 2009;10(2):237–248. [Google Scholar]
- 23. Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res. 2012;6(4):121–127. [DOI] [PubMed] [Google Scholar]
- 24. Melo B, Gomes A, Cruz J. Desenvolvimento e adaptação de um instrumento de avaliação psicológica do “burnout” para os profissionais de Psicologia. In: Associação dos Psicólogos Portugueses, ed. Avaliação psicologica: formas e contextos. Braga: Lusografe; 1999:596–603. [Google Scholar]
- 25. Poghosyan L, Aiken LH, Sloane DM. Factor structure of the Maslach Burnout Inventory: an analysis of data from large scale cross-sectional surveys of nurses from eight countries. Int J Nurs Stud. 2009;46(7):894–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bower S, Bower G. Asserting yourself: A practical guide for positive change. Boston, MA: Da Carpo; 2004. [Google Scholar]
- 27. Bono E. Six thinking hats. New York, NY: Little, Brown and Company; 1985. [Google Scholar]
- 28. Ferreira J, Fernandes R, Haase RF, Santos E. Minnesota Satisfaction Questionnaire - Short Form: estudo de adaptação e validação para a língua portuguesa. Psychol. 2009;51(1):251–281. [Google Scholar]
- 29. Weiss DJ, Dawis RV, England GW. Manual for the Minnesota Satisfaction Questionnaire. Minneapolis: University of Minneapolis; 1967. [Google Scholar]
- 30. Caris-Verhallen W, Kerkstra A, Bensing J. Non-verbal behaviour in nurse-elderly patient communication. J Adv Nurs. 1999;29(4):808–818. [DOI] [PubMed] [Google Scholar]
- 31. Williams K, Harris B, Lueger A, Ward K, Wassmer R, Weber A. Visual cues for person-centered communication. Clin Nurs Res. 2011;20(4):448–461. [DOI] [PubMed] [Google Scholar]
- 32. Cohen J. Statistical Power Analysis for the Behavioral Sciences 2nd ed. New Jersey: Lawrence Erbaum Associates; 1988. [Google Scholar]
- 33. Bourgeois MS, Dijkstra K, Burgio LD, Allen RS. Communication skills training for nursing aides of residents with dementia: the impact of measuring performance. Clin Gerontologist. 2004;27(1-2):119–138. [Google Scholar]
- 34. Fleiss J. The Design and Analysis of Clinical Experiments: Taylor & Francis; 1986. [Google Scholar]
- 35. Jeon YH, Merlyn T, Chenoweth L. Leadership and management in the aged care sector: a narrative synthesis. Aust J Ageing. 2010;29(2):54–60. [DOI] [PubMed] [Google Scholar]
- 36. Haidet KK, Tate J, Divirgilio-Thomas D, Kolanowski A, Happ MB. Methods to improve reliability of video-recorded behavioral data. Res Nurs Health. 2009;32(4):465–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Campbell MK, Elbourne DR, Altman DG. CONSORT statement: extension to cluster randomised trials. BMJ. 2004;328(7441):702–708. [DOI] [PMC free article] [PubMed] [Google Scholar]


