Abstract
With the aging of the population and the projected increase of dementia in the coming years, it is crucial that we understand the needs of people with dementia (PWD) in order to provide appropriate care. The aim of this study is to determine, using the best evidence possible, the care needs of PWD living in long-term care (LTC). A total of 68 studies, published between January 2000 and September 2010, were identified from six databases. From the selected studies, 19 needs of PWD were identified. The existing evidence suggests that psychosocial needs such as the need to engage in daily individualized activities and care must not be ignored in LTC. This review aims to provide a clearer picture of the needs of this growing patient population.
Keywords: Alzheimer’s disease, assisted living, responsive behaviors, psychosocial, systematic review, needs
Introduction
Over 60% of the residents living in long-term care (LTC) facilities in Canada and the United States have a diagnosis of dementia. 1,2 Dementia is “characterized by multiple cognitive deficits that include memory impairment and at least one of the following cognitive disturbances: aphasia, apraxia, agnosia, or a disturbance in executive functioning.”3(p148) According to Cohen-Mansfield and Mintzer 4 and Orrell et al, 5 the needs of people with dementia (PWD) are unmet in LTC. In fact, direct care workers feel most incapable of meeting residents’ social, psychological, and emotional needs. 6,7 Several factors contribute to the issue, such as the lack of resources. 4
Understanding and responding to the needs of PWD is of great importance, as unmet needs are both a source of reduced quality of life (QoL) and increased disruptive behaviors. 8,9 It is thought that only about 10% of the residents’ symptoms are caused by the dementia itself with the other 90% resulting from the quality of care PWD receive. 10 For instance, a problematic behavior exhibited by a resident with dementia may be a means to express discomfort or a lack of social support. Hancock et al found a higher score on the Challenging Behaviour Scale to be positively correlated with higher unmet needs among residents with dementia in residential care homes. 11 It is thus important that frontline staff understand the needs of PWD so that they can be better cared for.
Residents with dementia in LTC have a variety of complex needs. Although there exist a plethora of studies dealing with disruptive behaviors and dementia, only 2 cross-sectional studies address the question of need from the perspectives of residents themselves. Hancock et al 11 highlight the unmet needs of PWD as identified from the perspective of residents, whereas Orrell et al 5 report on the comparison of ratings of needs as assessed by the residents, the staff, and the family caregivers. Unmet needs as reported by both studies were the lack of stimulating daytime activities and social company, lack of support to help cope with psychological distress (eg, depression and anxiety) as well as poor assistance with memory, eyesight, and hearing problems. Needs that were more likely to be fulfilled were those of a basic nature such as food and appropriate accommodation. 5,11 Reed and Tilly suggest that the care fundamentals of PWD should include not only the relief of discomfort and pain but also the need for social support, the opportunity to engage in meaningful activities as well as the basic need of consuming adequate food and fluid. 12 At the end of life, care for physical symptoms (including pain) and behavioral symptoms become the focus. 13
A number of other studies have looked at the needs of PWD, but have focused on community dwellers, which often include higher functioning individuals. Bossen et al conducted a literature review looking at the needs of older adults with early stage Alzheimer’s disease. 14 Some of the needs identified were the need to be heard, the need for information and knowledge, and the need for health promotion. 14 A systematic review of the literature looking at the needs of PWD residing in the community was also conducted. 15 Studies selected for review included mostly clients from adult day programs and memory or psychogeriatric clinics. Only 3 studies from those selected included a sample of clients with severe cognitive impairment. Identified needs included the need for adequate strategies to cope with disabilities, the need to be respected and accepted as well as the need to come to terms with the condition. 15 As needs of individuals with early-stage dementia differ greatly from those with moderate to severe impairment, results from these reviews cannot be generalized to individuals living in LTC facilities. As a result of potentially unmet needs in LTC and its detrimental impact on the health of residents and no research reviews focusing on the needs of PWD in this setting specifically, this review aims to determine, using the best evidence possible, the needs of residents with dementia in LTC. More specifically, the review was designed to answer the following question: “What are the (care) needs of PWD living in long-term care facilities as supported by the best evidence”.
Methods
Searches were conducted in MEDLINE, CINAHL, HealthSTAR, EMBASE, PsycINFO, and the Cochrane Library, limited to the period of January 2000 to September 2010, and restricted to English and French publications. The following combinations of Medical Subject Headings (MeSH) terms and keywords were used: (“care needs” or “needs assessment” or “health services needs and demand” or “Camberwell assessment” or “quality of life”) and (“dementia” or “Alzheimer Disease” or “vascular dementia” or “frontotemporal dementia”) and (“long-term care” or “long term care” or “longterm care” or “nursing home” or “geriatric nursing” or “homes for the aged” or “charitable home” or “municipal home” or “aged care home” or “care home”). All types of studies (eg, thesis and book chapters) were considered for the review. Studies were first selected based on the title and abstract, and then those that were included based on title/abstract were further assessed based on the full text. The selection of the studies was evaluated by 2 independent judges by means of a data abstraction form, pilot tested by 2 individuals by means of 5 randomly selected articles, and when disagreements ensued a third judge assessed the relevance of the studies. Criteria for inclusion in this review were as follows: studies needed to relate to individuals with dementia (diagnosis or suspected dementia) and offer a description of the (care) needs of individuals with dementia living in LTC. Studies were excluded if they were anecdotal, letters to the editor, expert opinions (including “nonstudy” book chapters), and nonsystematic literature reviews. Although useful in stimulating thought processes, these types of literature were excluded, as their level of evidence is considered weak by the scientific community in providing concrete results. Studies were further excluded if the setting of focus was one of the following: community, adult day center, and/or acute care hospital.
Additional relevant studies were searched in the reference lists of the studies that met all eligibility criteria using the same filtering technique as previously described. All studies meeting the eligibility criteria were critically appraised by 2 independent judges for methodological quality with a critical review form for qualitative studies, 16 quantitative studies, 17 and the measurement tool for the “assessment of multiple systematic reviews” assessment of multiple systematic reviews (AMSTAR).
The overall quality of the studies was based on the sum of 2 variables, namely, (1) the quality rating of studies based on selected quality criteria (Table 1) such as the validity of outcome measures and the justification of sample size and (2) the level of evidence of each study. The quality rating was calculated on a scale of 1 (lowest quality) to 10 (highest quality) based on selected quality criteria taken from the assessment forms. If an article addressed a quality criterion, the criterion was marked fulfilled (+), however when an article did not address a criterion, this was marked unmet (−). When inadequate information was provided by an article for a particular item, the quality item was marked unknown (u). The levels of evidence were ranked in multiples of 10, from 10 (lowest evidence) to 50 (highest evidence). Both scores were added to obtain the overall quality for each study, with possible scores ranging from 11 (a score of 1 on quality + a score of 10 on level of evidence) to 60 (a score of 10 on quality + a score of 50 on level of evidence). Studies with higher evidence levels (eg, randomized-controlled trials) and that met a greater number of quality criteria were given more weight than studies with lower evidence levels (eg, observational studies without control groups such as case series) that met fewer quality criteria. Levels of evidence were ranked in multiples of 10 to ensure that a higher level of evidence always surpassed a lower level of evidence regardless of the quality rating of the studies.
Table 1.
Quality Criteria.
| Design Type | Criteria |
|---|---|
| Quantitative design | Design appropriate for study question |
| Sample described in detail | |
| Sample size justified | |
| Outcome measures reliable | |
| Outcome measures valid | |
| Intervention described in detail | |
| Statistical analyses reported | |
| Analysis methods appropriate | |
| Drop-outs reported | |
| Appropriate conclusions given methods and results | |
| Qualitative design | Design appropriate for study question |
| Theoretical perspective identified | |
| Purposeful selection | |
| Sampling done until redundancy reached | |
| Clear and complete description of site and participants | |
| Data analysis was inductive | |
| Findings consistent and reflective of data | |
| Decision trail developed | |
| Evidence of the 4 components of trustworthiness | |
| Appropriate conclusions given methods and results | |
| Systematic review | “Priori” design provided |
| Duplicate study selection and data extraction | |
| Comprehensive literature search performed | |
| Status of publication used as an inclusion criterion | |
| List of studies provided | |
| Characteristics of included studies provided | |
| Scientific quality of included studies assessed and documented | |
| Scientific quality of included studies used appropriately to formulate conclusions | |
| Appropriate methods used to combine the findings of studies | |
| Likelihood of publication bias assessed |
Levels of evidence were only assigned to quantitative studies, as such a system is nonexistent for qualitative studies according to the Scottish Intercollegiate Guidelines Network. 19 As a result, only the quality criteria were used for qualitative studies. For studies with mixed designs, a quality score was considered for both the quantitative and the qualitative aspects. No study was excluded on the basis of methodological quality as the identified flaws (eg, inadequate description of participants) in the studies of lower quality were unlikely to influence the findings.
Articles were also rigorously evaluated by 2 independent judges to extract specific information related to the needs of PWD living in LTC. The extracted data led to the identification of a list of needs of PWD living in LTC. The list was agreed upon by the judges and synthesized within larger, manageable categories referred to as “codes”. For example, the following extracted needs: need for satisfactory communication, need for conversation, and need for socialization were categorized within a category named social needs. Operational definitions were developed for these main categories. Three judges, including an occupational therapist, completed the matching of the needs with the newly developed categories. Disagreements were discussed by 2 other judges, and a consensus was reached among all the judges. Once the list of needs was agreed upon by the judges, the importance of each of the needs was determined based on the overall average quality and the number of studies reporting on each need.
Results
The database searches resulted in 1146 studies. Following the strategy shown in Figure 1, 68 of these studies were included in the review.
Figure 1.
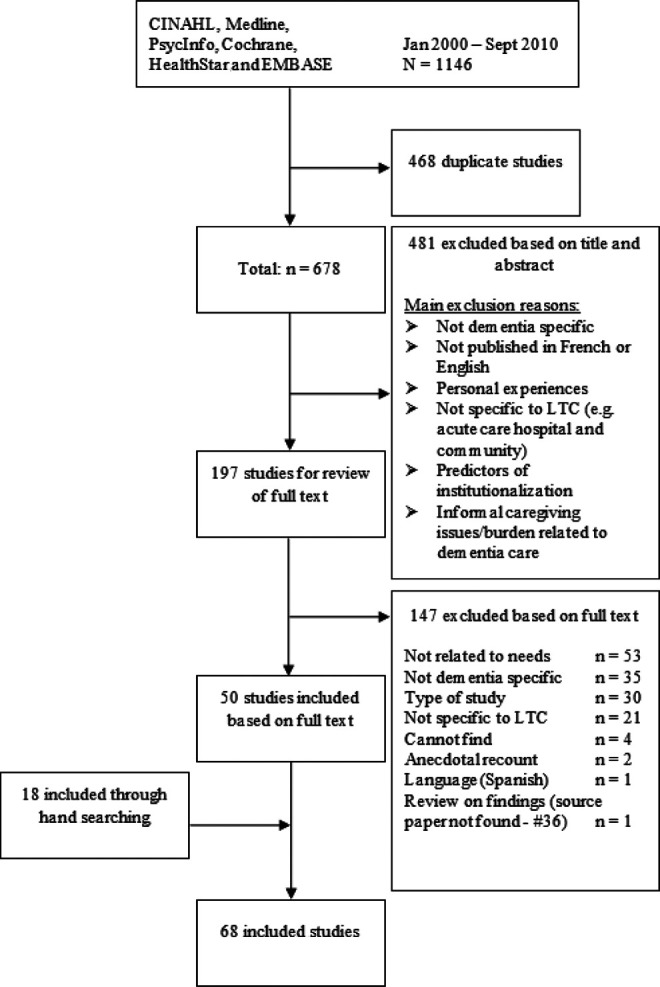
Results of search strategy.
The majority of the studies used a quantitative design (n = 50) of which 14 were randomized controlled trials. Only 15 relevant qualitative studies were identified. Three studies with mixed designs were included, and both the qualitative and the quantitative aspects of the studies were analyzed separately. The overall methodological quality of the studies is presented in Table 2. Most studies obtained a quality rating of 7 or higher (n = 54 of 68) and a lower level of evidence. Studies were conducted mainly in the United States (n = 37), the United Kingdom (n = 8), and Canada (n = 7). Half of the studies were conducted in an LTC setting with 24-hour nursing care, and the remaining included either a mix of participants from the residential setting (ie, residential care [RC]/assisted-living [AL] facilities) and the LTC setting with 24-hour nursing care (ie, NHs) or participants from the residential setting only. All study participants had a formal or “probable” diagnosis of dementia. The majority of the participants were female and had moderate to severe dementia. Most studies did not mention the severity of dementia of their participants.
Table 2.
Overall Methodological Quality of the Quantitative and Qualitative Studies.a
| Quality Rating | Qualitative Methodologies | Quantitative Methodologies | |||
|---|---|---|---|---|---|
| Level 3B (10) | Level 3A (20) | Level 2 (30) | Level 1 (40) | ||
| 2 | Tilly and Reed 20 ; Tilly and Fok 21 | ||||
| 3 | Malone and Camp 22 | Innes and Surr 23 | |||
| 4 | Van Haitsma 24 | ||||
| 5 | Cioffi et al 25 | Cohen-Mansfield et al 26 ; Kobayashi and Yamamoto 27 ; Young et al 28 | Kolanowski et al 29 | ||
| 6 | Finnema et al 30 | Blass et al 31 | Morgan et al 32 | Orsulic-Jeras et al 33 | |
| 7 | Powers and Watson34,b; Hernandez 35 ; MacDonald 36 ; Pearson and Chalmers 37 | Ballard et al 38 ; Zeisel et al 39 | Powers and Watson34,b; Buettner and Fitzsimmons 40 ; Chung 41 ; Cohen-Mansfield and Jensen 42 ; Ragneskog et al 43 ; Sloane et al 44 | ||
| 8 | Lai45,b; Bharani and Snowden 46 ; Galik et al 47 | Dobbs et al 48 ; Gill et al 49 ; Hancock et al 11 ; Milke et al 50 ; Orrell et al 5 ; Potkins et al 51 | Caserta and Lund 52 ; Gonzalez-Salvador et al 53 ; Quinn et al 54 | Mickus et al 55 | Bourgeois et al 56 ; Kovach et al 9 ; Orrell et al 57 |
| 9 | Smith58,b; Bruce et al 6 ; Dröes et al 59 ; Powers 60 ; Zingmark et al 61 | Choi 62 ; Hoe et al 63 ; Zimmerman et al 64 | Gardiner et al 65 ; Gerdner 66 ; Koch et al 67 ; Kverno et al 68 ; O’Brien and Caro 69 ; Ruka 70 | Reid and Chappell 71 | Beck et al 72 ; Finnema et al 73 ; Opie et al 74 ; Sung et al 75 |
| 10 | O’Connor et al 76 | Hicks-Moore 77 | Smith58,b; Sung et al 78 | Lai45,b; Cohen-Mansfield et al 79 ; Hicks-Moore and Robinson 80 ; Kolanowski et al 81 ; Kovach et al 82 ; Sloane et al 83 | |
a None of the studies selected for review obtained a quality rating of 1 and no quantitative studies had an evidence level of 1A (systematic review of all relevant randomized-controlled trials). Studies with a higher level of evidence are given in the lower right side of the table for quantitative methodologies and the lower left side for qualitative methodologies.
b Mixed methods.
Well-being and “QoL” are measures that reflect on the needs of PWD. Hoe et al, 63 for instance, found that PWD felt that a high QoL was strongly correlated with lower depression and anxiety levels. Care staff also felt that fewer behavior problems such as neuropsychiatric symptoms (eg, agitation and depression) were strongly correlated with a higher QoL, in addition to a lower level of physical disability. 63 End-of-life care requirements 21,34 , predictors enhancing the sense of identity of residents 6,26,79 as well as the effect of pharmacological 46,68 and/or nonpharmacological 80,76,58,78 interventions as a way to address the underlying needs expressed by disruptive behaviors were other foci of interest.
In analyzing the needs identified in each of the included studies, we were able to categorize all needs into 19 categories. The needs are listed in Table 3 by the highest to lowest number of times mentioned by a study.
Table 3.
Needs Identified in the Literature Including Their Operational Definition and Associated Studies.
| Need | Number of Studies | Overall Quality of Studiesa | Definition | |
|---|---|---|---|---|
| Quantitative | Qualitative | |||
| Management of behavioral problems 5,9,11,30,32,40,42–44, 46,50,53,55,57,58,62–66,68,70,72,73,76–78,80–83 | Total: 31 Quantitative: 27 Qualitative: 3 Mixed design: 1 | 34 | 8 | Need to receive support from staff in decreasing behavioral symptoms (general) and be provided with appropriate care measures (eg, redirection) when exhibiting disruptive behaviors |
| Need for daily individualized activities/care 5,6,11,22–24, 29,33,36,38,41,43,48,49,50,52,57,59,60,61,64–66,74,79,81 | Total: 26 Quantitative: 20 Qualitative: 6 | 30 | 8 | Need to engage in meaningful daily activities (inside or outside the facility) tailored to the resident’s interests and abilities. Activities are not limited to the individual per se; activities may be offered in a group setting. Includes the need to receive individualized care (eg, medication prescribed to meet individual symptom) |
| Social needs 5,6,11,23,30,32,34,41,45,48,49,50,51,54,56,57,59, 60–62,64,71,72,75 | Total: 24 Quantitative: 17 Qualitative: 5 Mixed design: 2 | 29 | 8 | Need for social interactions that allow the resident to connect with others on an interpersonal level; meaningful interactions and communication opportunities with staff, family members, and residents |
| Emotional needs/personhood 6,21,23,26,30,32–35, 41,42,49,50,59,60–63,70,72,73,75,79 | Total: 23 Quantitative: 15 Qualitative: 7 Mixed design: 1 | 28 | 7 | Need to retain a good emotional balance (increase positive feelings such as pleasure and decrease negative feelings such as sadness). Development of a sense of personal identity (expression of self). Feelings such as reassurance, affection, acceptance, and appreciation are of great emotional importance |
| ADLs 5,11,20,21,23,27,38,30,32,37,50,53,54,57,63,64,69,71 | Total: 18 Quantitative: 14 Qualitative: 4 | 24 | 4 | Receiving assistance with activities of daily living (ADLs). These include activities we normally perform for ourselves (eg, hair care, eating/drinking, getting in and out of bed, and toileting) |
| Need for independence/choice 6,21,24,25,32,49,50,59,60,61,72,83 | Total: 12 Quantitative: 6 Qualitative: 6 | 29 | 7 | Need to preserve a sense of agency by means of opportunities for decision-making and personal control (ie, right to refuse medications and choice of activities). In the inability to make own decisions, residents’ next of kin should be sought for decisions related to their care |
| Cognitive needs 5,6,11,32,38,50,52,54,57,71,72 , | Total: 11 Quantitative: 10 Qualitative: 1 | 29 | 9 | Need for assistance with the interpretation of messages and surroundings |
| Need to be safe/secure 5,11,25,32,39,49,50,57,59,60,72 | Total: 11 Quantitative: 8 Qualitative: 3 | 26 | 8 | Need to feel safe and be protected from self-injury as well as harm from other residents. An example of a safety feature on a dementia unit would be exit control measures (Zeisel et al 39 ) |
| General overall physical health 5,11,31,59,47,49,50,57,44,28 | Total: 10 Quantitative: 8 Qualitative: 2 | 22 | 8 | Need to retain good physical health by means of clinical care, exercise, and proper nutrition |
| Need to be in a homelike comforting environment 5,11,25,32,39,49,50,57,59,72 | Total: 10 Quantitative: 8 Qualitative: 2 | 26 | 7 | Need to reside in a “homelike” environment which may include but is not limited to having a quiet space and personalized spaces. Such an environment induces a sense of familiarity |
| Need to receive proper pain management 21,34,44,59,60,61,70,75,82,83 | Total: 10 Quantitative: 5 Qualitative: 4 Mixed design: 1 | 39 | 7 | Need to diminish the discomfort caused by physical pain |
| Sensory needs 5,11,24,32,39,49,50,57,67 | Total: 9 Quantitative: 9 | 23 | – | Need for optimal sensory stimulation from the environment (eg, proper lighting—visual stimulation). Relates to the residents 5 senses |
| Need for daily structured care 79,27,50,32,33,34 | Total: 6 Quantitative: 5 Mixed design: 1 | 29 | 7 | Need for continuous, routine, predictable care based on the resident’s needs |
| Functional needs—IADLs 5,11,54,63,80 | Total: 5 Quantitative: 5 | 20 | – | Receiving assistance in performing IADLs which include tasks that we often do to ensure our independent living (eg, taking medication, managing money, talking on the phone, and shopping) |
| Need for knowledgeable staff 5,9,21,50,64 | Total: 5 Quantitative: 4 Qualitative: 1 | 26 | 2 | Need for well trained and educated (dementia specific) staff as well as staff who have gained extensive experience in caring for people with dementia at various levels |
| Sexual needs 5,11,57,59,60 | Total: 5 Quantitative: 3 Qualitative: 2 | 28 | 9 | Need for intimate relationships |
| Need for privacy 25,32,50,59,72 | Total: 5 Quantitative: 3 Qualitative: 2 | 31 | 7 | Need for a secluded personal environment, if privacy is desired |
| Money—financial issues 5,11,59 | Total: 3 Quantitative: 2 Qualitative: 1 | 18 | 9 | Need to have a good financial situation for purchase of desired items and bill payments |
| Spiritual needs 21,59 | Total: 2 Qualitative: 2 | – | 6 | Need for spiritual support and opportunities to exercise one’s religion |
Abbreviation: IADLs, instrumental activities of daily living.
a The overall quality of the studies supporting each need is based on the sum of the level of evidence score (10-50) and the quality rating (1-10) of each study. Possible scores range from 11 to 60.
The need most discussed in the studies was the need for management of behaviors (n = 31) followed by the need for daily individualized activities/care (n = 26), social needs (n = 24), and emotional needs/personhood (n = 23). As outlined in Table 3, these needs appeared of most importance for PWD by the quantitative studies, as they were not only studied by the greatest number of studies but also by studies of highest methodological quality. Qualitative studies also suggested the importance of social needs and the need for individualized activities/care but seemed to support more strongly emotional needs/personhood. On the other hand, quantitative studies were less numerous or had fewer strong studies supporting the need to deal with financial issues or functional needs— instrumental activities of daily living. On the qualitative side, the need for knowledgeable staff did not surface among the strongest studies or the majority of studies. There were no studies indicating this was not important, but rather our study may indicate that we need more evidence in this area. The low number of studies discussing such a need does not necessarily mean that it is not a significant one but simply a one that is not adequately studied.
Discussion
This critical review looking at the needs of PWD living in LTC generated 68 studies that met all eligibility criteria. From these, a total of 19 needs were identified, of which the need to manage behavioral problems, the need for individualized activities/care, emotional needs/personhood, and social needs were found to be of most importance for PWD in LTC.
Not surprisingly, the management of behaviors was the need most mentioned by the reviewed studies and suggested as most important for PWD by quantitative studies. There is significant literature dealing with disruptive behaviors and dementia. Many studies look at the effect of interventions on behaviors. 9,80,81,78 The anxiety and aggression manifested by the residents is perceived as a signal of unease, and therefore the need to deal with these anxieties becomes a source of resource consumption. The physical environment, the presence of pain, and the lack of social stimulation are examples of needs that can trigger behavioral problems. 84 Despite the need to comprehensively understand the reason behind the behaviors, caregivers often do not have the resources available in terms of time and/or tools to assess the behavior prior to administering a treatment. Reactive responses to behaviors that refer to the administration of a treatment after a cursory assessment of the cause of the behavior was found to be the most prevalent type of response by nurses based on a sample of 112 participants from nursing homes. 9 In a prospective study examining the time used by nursing staff to manage disruptive behaviors, it was found that no nursing assessment or intervention was provided for behavioral symptoms in about 25% of the cases. 85 This may suggest that caregivers tend to opt for an immediate solution to the behaviors as a result of their distressing nature or as a result of the lack of resources to deal with these behaviors. Tilly and Fok caution that a distinction be made between managing disruptive behaviors for the sake of residents versus for the sake of staff. 21 If the resources are not sufficient to allow proper management of the behavioral issues, the behaviors might worsen leading to an escalation of unmet needs that become unmanageable. For residents with dementia, the increased levels of agitation, anxiety, and verbal outbursts can decrease their QoL and have a negative impact on their health. 42,64
The number of studies reporting on social needs, the need for daily individualized activities/care, emotional needs/personhood as well as the need for independence/choice for residents with dementia suggests that there is a need to create the notion of home for this population. As identified by Aminzadeh and colleagues, the creation of the meaning of home for PWD is of particular importance when being transferred to a collective dwelling of care. 86 According to the participants in this study, a home encompasses the following: (1) familiarity, (2) a center of socialization, (3) connectedness and affiliation, (4) a place of retreat, (5) a locus of autonomy, control, choice, and freedom of actions, (6) a site for engagement in meaningful activities of daily living, (7) a place for the expression of personal interests, values, achievements, and status, and (8) a source of memories of life histories. 86 The LTC facilities are often stigmatized as a place of “sickness” and may lack this notion of home. In a study by the same authors 87 exploring the perspectives of 16 PWD on the meanings and experiences linked with the relocation to a RC facility, the relocation signaled an inevitable downward trajectory to a more dependent, protected, and structured lifestyle.
The need for a cultural shift in LTC has been highlighted in a recent report by The Conference Board of Canada. Today’s LTC residents have different preferences (eg, independent living and need for greater autonomy) and higher expectations. Facilities that promote socialization, choice, and independence positively impact the QoL of residents, thus suggesting a need to shift from a structured to a more flexible type of care. 7 The importance of culture shift in LTC is also strongly supported by the Pioneer Network, a small group of LTC professionals formed in 1997 to advocate for person-directed care. This network, known as the culture change movement, is working on system changes for support of humane models of care “where elders live in open, diverse, and caring communities.” 88 (mission, vision and values) The aim of this emerging network is to transform the culture of aging in LTC in America as a means to provide meaningful person-centered care to residents that is independent of their age and limitations. 88
This review is not without a few limitations. First, the representation of a need in the literature does not necessarily equate to importance. Although the representation of a need in the literature is sufficient to provide evidence that this is a need, the simple fact that a need has not been studied or studied very little does not mean it is not a “real” need (eg, knowledgeable staff) for residents with dementia. Second, RC and AL were not considered as keywords or MeSH terms in the search strategy. The setting of focus in this study was initially LTC, and so only terms relevant to this setting were considered in the search process. However the term aged care home does encompass RC as well as lower levels of care in addition to 24-hour nursing care. After reviewing a considerable number of articles, it was found that the RC/AL setting is gaining popularity as a choice of care for PWD. Articles that did pertain to this setting were therefore included. Since RC and AL were not terms considered in the searching of articles, this may have limited the thoroughness of our results. Third, our search strategy focused exclusively on the needs of PWD and not on the needs of staff or family. This might have limited the types of studies we identified.
Conclusion
This research adds to the scientific evidence by providing an evidence-based rationale for identifying the overall needs of this population. The evidence on the needs of PWD in LTC supports consideration of human social needs. Many of the reviewed studies have highlighted the importance of psychosocial needs that differ from the traditional focus on physical needs and services provided by LTC facilities. The suggested importance of psychosocial needs may have been influenced by the inclusion of a QoL criterion when searching for relevant studies. Clearly, the scientific community is placing great importance on the need to consider the PWD as one with needs for personhood, choice, and well-being. The review serves as a basis toward understanding the needs of PWD, which can translate not only into better care for residents in LTC but also decreased pressures on staff and administrators due to a decrease in disruptive behaviors. This is especially important in light of the increasing prevalence of dementia among residents of LTC.
Future research is needed to validate whether the list of needs identified by this study is comprehensive. Validation should include asking frontline staff, families, and residents to comment on the list of needs identified and how they would prioritize them as well as having these stakeholders, including residents with dementia, voice their opinions in regard to the needs. Very few high-quality quantitative studies addressed the need to receive proper pain management. More evidence is needed to determine the importance of this particular need and how it might influence other needs such as social needs. Spiritual needs were considered by a few qualitative studies suggesting its importance for PWD. This presents an avenue for future research.
Many of the studies identified in this review pertained to interventions geared toward reducing behaviors resulting from unmet needs. Future studies focused on QoL concerns would contribute more significantly to the evidence as well as research focused on better understanding the behaviors.
Another avenue of interest would be to examine the list of needs identified by this study for subgroups with dementia. For example, it could be interesting to see whether differences exist between men and women as well as people from different ethnic backgrounds. This last group should be of particular interest for study, as the ethnic and linguistic diversity of LTC homes is expected to increase considerably in the coming years. Based on results from a 2006 Canadian census, 7.6% of people aged 75 years and over reported being a member of a visible minority in comparison to 12.7% for those aged between 45 and 64. 7 Other subgroups of interest to examine would be the influence of a resident’s level of income and marital status on needs.
Furthermore, it would be interesting to examine the needs of PWD living in dementia-specific units and facilities, such as assistive living and skilled nursing facilities. The results presented in this study are a general understanding of the needs of PWD in LTC. No distinctions in regard to needs have been made between nursing homes and AL facilities. It would be interesting to study this particular avenue of research from an international standpoint.
Acknowledgments
This study was completed as part of a Master’s thesis in Health Systems at the University of Ottawa. A special thanks to Rachel Blais, NRS-MDS coordinator at Bruyère Continuing Care, and a number of Health Sciences students from the University of Ottawa (Madura Sundareswaran, Farwa Malik and Emilie Meyers) for their time in helping with the filtering of articles.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Hirdes JP, Mitchell L, Maxwell CJ, White N. Beyond the ‘iron lungs of gerontology’: using evidence to shape the future of nursing homes in Canada. Can J Aging. 2011;30(3):371–390. doi:10.1017/S0714980811000304. [DOI] [PubMed] [Google Scholar]
- 2. Thies W, Bleiler L; Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):208–245. [DOI] [PubMed] [Google Scholar]
- 3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Text Revision (DSM-IV). Washington, DC: Author; 2000. [Google Scholar]
- 4. Cohen-Mansfield J, Mintzer JE. Time for change: the role of nonpharmalogical interventions in treating behavior problems in nursing home residents with dementia. Alzheimer Dis Assoc Disord. 2005;19(1):37–40. [DOI] [PubMed] [Google Scholar]
- 5. Orrell M, Hancock GA, Liyanage KC, Woods B, Challis D, Hoe J. The needs of people with dementia in care homes: the perspectives of users, staff and family caregivers. Int Psychogeriatr. 2008;20(5):941–951. doi:10.1017/S1041610208007266. [DOI] [PubMed] [Google Scholar]
- 6. Bruce E, Surr C, Tibbs MA, Downs M. Moving towards a special kind of care for people with dementia living in care homes. J Res Nurs. 2002;7(5):335–347. [Google Scholar]
- 7. The Conference Board of Canada. Elements of an Effective Innovation Strategy for Long Term Care in Ontario. Ottawa, Canada: Author; 2011. [Google Scholar]
- 8. Kolanowski A, Litaker M, Buettner L, Moeller J, Costa PT. A randomized clinical trial of theory-based activities for the behavioral symptoms of dementia in nursing home residents. J Am Geriatr Soc. 2011;59(6):1032–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kovach CR, Kelber ST, Simpson M, Wells T. Behaviors of nursing home residents with dementia: examining nurse responses. J Gerontol Nurs. 2006;32(6):13–21. [DOI] [PubMed] [Google Scholar]
- 10. Nazarko L. Providing high quality dementia care in nursing homes. Nurs Residential Care. 2009;11(6):296–300. [Google Scholar]
- 11. Hancock GA, Woods B, Challis D, Orrell M. The needs of older people with dementia in residential care. Int J Geriatr Psychiatry. 2006;21(1):43–49. doi:10.1002/gps.1421. [DOI] [PubMed] [Google Scholar]
- 12. Reed P, Tilly J. Dementia care practice recommendations for nursing homes and assisted living, phase 1: dementia care fundamentals, food and fluid consumption, pain management, and social engagement. Alzheimers Care Today. 2008;9(1):33–41. doi:10.1097/01.ALCAT.0000309013.77834.31. [Google Scholar]
- 13. Tilly J, Reed P, Gould E, Fok A. Dementia Care Practice Recommendations for Assisted Living Residences and Nursing Homes—Phase 3 End-of-Life Care. Alzheimer’s Association; 2007. http://www.alz.org/national/documents/brochure_DCPRphase3.pdf. Accessed March 10, 2013.
- 14. Bossen AL, Specht JK, McKenzie SE. Needs of people with early-stage Alzheimer’s disease: reviewing the evidence. J Gerontol Nurs. 2009;35(3):8–15. [DOI] [PubMed] [Google Scholar]
- 15. Van der Roest HG, Meiland FJ, Maroccini R, Comijs HC, Jonker C, Dröes R-M. Subjective needs of people with dementia: a review of the literature. Int Psychogeriatr. 2007;19(3):559–592. doi:10.1017/S1041610206004716. [DOI] [PubMed] [Google Scholar]
- 16. Letts L, Wilkins S, Law M, Stewart D, Bosch J, Westmorland M. Guidelines for Critical Review Form—Qualitative Studies. Version 2.0. McMaster University Occupational Therapy Evidence-Based Practice Research Group; 2007. [Google Scholar]
- 17. Law M, Stewart D, Pollock N, Letts L, Bosch J, Westmorland M. Guidelines for Critical Review Form – Quantitative Studies. McMaster University Occupational Therapy Evidence-Based Practice Research Group; 1998. [Google Scholar]
- 18. Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi:10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Scottish Intercollegiate Guidelines Network 50. Forming guideline recommendations. In: A Guideline Developer’s Handbook (section 7). http://www.sign.ac.uk/pdf/sign50.pdf. Published November 2011. Accessed February 20, 2013.
- 20. Tilly J, Reed P. Interventions that optimize quality dementia care: a comprehensive literature search selects the best evidence-based interventions to improve quality dementia care in LTC facilities. Can Nurs Home. 2005;16(3):13–21. [Google Scholar]
- 21. Tilly J, Fok A. Policy barriers to quality end-of-life care for residents with dementia in assisted living residences and nursing homes. Alzheimers Care Today. 2008;9(2):103–112. [Google Scholar]
- 22. Malone ML, Camp CJ. Montessori-based dementia programming: providing tools for engagement. Dementia. 2007;6(1):150–157. [Google Scholar]
- 23. Innes A, Surr C. Measuring the well-being of people with dementia living in formal care settings: the use of dementia care mapping. Aging Ment Health. 2001;5(3):258–268. doi:10.1080/13607860120065023. [DOI] [PubMed] [Google Scholar]
- 24. Van Haitsma K. The assessment and integration of preferences into care practices for persons with dementia residing in the nursing home. In: Rubinstein R, Moss M, Kleban MH, eds. The Many Dimensions of Aging. New York, NY: Springer Publishing Company; 2000:143–163. [Google Scholar]
- 25. Cioffi JM, Fleming A, Wilkes L, Sinfield M, Miere JL. The effect of environmental change on residents with dementia: the perceptions of relatives and staff. Dementia. 2007;6 ( 2):215–231. [Google Scholar]
- 26. Cohen-Mansfield J, Golander H, Arnheim G. Self-identity in older persons suffering from dementia: preliminary results. Soc Sci Med. 2000;51(3):381–394. [DOI] [PubMed] [Google Scholar]
- 27. Kobayashi N, Yamamoto M. Impact of the stage of dementia on the time required for bathing-related care: a pilot study in a Japanese nursing home. Int J Nurs Stud. 2004;41(7):767–774. doi:10.1016/j.ijnurstu.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 28. Young KW, Binns MA, Greenwood CE. Meal delivery practices do not meet needs of Alzheimer patients with increased cognitive and behavioral difficulties in a long-term care facility. J Gerontol A Biol Sci Med Sci. 2001;56(10):M656–M661. [DOI] [PubMed] [Google Scholar]
- 29. Kolanowski AM, Buettner L, Costa PT, Litaker MS. Capturing interests: therapeutic recreation activities for persons with dementia. Ther Recreational J. 2001;35(3):220–235. [Google Scholar]
- 30. Finnema E, Dröes RM, Ribbe M, Van Tilburg W. The effects of emotion-oriented approaches in the care for persons suffering from dementia: a review of the literature. Int J Geriatr Psychiatry. 2000;15(2):141–161. [DOI] [PubMed] [Google Scholar]
- 31. Blass DM, Black BS, Phillips H, et al. Medication use in nursing home residents with advanced dementia. Int J Geriatr Psychiatry. 2008;23(5):490–496. doi:10.1002/gps.1921. [DOI] [PubMed] [Google Scholar]
- 32. Morgan DG, Stewart NJ, D’arcy KC, Werezak LJ. Evaluating rural nursing home environments: dementia special care units versus integrated facilities. Aging Ment Health. 2004;8(3):256–265. doi:10.1080/1360786041000166796. [DOI] [PubMed] [Google Scholar]
- 33. Orsulic-Jeras S, Judge KS, Camp CJ. Montessori-based activities for long-term care residents with advanced dementia: effects on engagement and affect. Gerontologist. 2000;40(1):107–111. [DOI] [PubMed] [Google Scholar]
- 34. Powers BA, Watson NM. Meaning and practice of palliative care for nursing home residents with dementia at end of life. Am J Alzheimers Dis Other Dement. 2008;23(4):319–325. doi:10.1177/1533317508316682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hernandez RO. Effects of therapeutic gardens in special care units for people with dementia: two case studies. J Housing Elder. 2007;21(1-2):117–152. doi:10.1300/J081v21n01-07. [Google Scholar]
- 36. MacDonald KC. Family and staff perceptions of the impact of the long-term care environment on leisure. Top Geriatr Rehabil. 2006;22(4):294–308. [Google Scholar]
- 37. Pearson A, Chalmers J. Oral hygiene care for adults with dementia in residential aged care facilities. JBI Rep. 2004;2(3):65–113. [DOI] [PubMed] [Google Scholar]
- 38. Ballard C, O’Brien J, James I, et al. Quality of life for people with dementia living in residential and nursing home care: the impact of performance on activities of daily living, behavioral and psychological symptoms, language skills, and psychotropic drugs. Int Psychogeriatr. 2001;13(1):93–106. [DOI] [PubMed] [Google Scholar]
- 39. Zeisel J, Silverstein NM, Hyde J, Levkoff S, Lawton MP, Holmes W. Environmental correlates to behavioral health outcomes in Alzheimer's special care units. Gerontologist. 2003;43(5):697–711. [DOI] [PubMed] [Google Scholar]
- 40. Buettner L, Fitzsimmons S. Mixed behaviors in dementia: the need for a paradigm shift. J Gerontol Nurs. 2006;32(7):15–22. [DOI] [PubMed] [Google Scholar]
- 41. Chung JC. Activity participation and well-being of people with dementia in long-term-care settings. OTJR Occup Particip Health. 2004;24(1):22–31. [Google Scholar]
- 42. Cohen-Mansfield J, Jensen B. Do interventions bringing current self-care practices into greater correspondence with those performed premorbidly benefit the person with dementia? A pilot study. Am J Alzheimers Dis Other Dement. 2006;21(5):312–317. doi:10.1177/1533317506291135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ragneskog H, Asplund K, Kihlgren M, Norberg A. Individualized music played for agitated patients with dementia: analysis of video-recorded sessions. Int J Nurs Pract. 2001;7(3):146–155. [DOI] [PubMed] [Google Scholar]
- 44. Sloane PD, Zimmerman S, Williams CS, Hanson LC. Dying with dementia in long-term care. Gerontologist. 2008;48(6):741–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lai KY. Improving the Quality of Life for Nursing Home Residents With Dementia: A Life Story Approach [Doctoral dissertation]. ProQuest Dissertations and Theses Database; 2003. UMI Order AAI0806944. [Google Scholar]
- 46. Bharani N, Snowden M. Evidence-based interventions for nursing home residents with dementia-related behavioral symptoms. Psychiatr Clin North Am. 2005;28(4):985–1005. doi:10.1016/j.psc.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 47. Galik EM, Resnick B, Pretzer-Aboff I. 'Knowing what makes them tick': motivating cognitively impaired older adults to participate in restorative care. Int J Nurs Pract. 2009;15(1):48–55. doi:10.1111/j.1440-172X.2008.01721.x [DOI] [PubMed] [Google Scholar]
- 48. Dobbs D, Munn J, Zimmerman S, et al. Characteristics associated with lower activity involvement in long-term care residents with dementia. Gerontologist. 2005;45 Spec No 1(1):81–86. [DOI] [PubMed] [Google Scholar]
- 49. Gill KS, Williams CS, Zimmerman SP, Uman GC. Quality of long-term care as reported by residents with dementia. Alzheimers Care Today. 2007;8(4):344–359. [Google Scholar]
- 50. Milke DL, Beck CH, Danes S. Meeting the needs in continuing care of facility-based residents diagnosed with dementia: comparison of ratings by families, direct care staff, and other staff. J Appl Gerontol. 2006;25(2):103–119. doi:10.1177/0733464805284565. [Google Scholar]
- 51. Potkins D, Myint P, Bannister C, et al. Language impairment in dementia: impact on symptoms and care needs in residential homes. Int J Geriatr Psychiatry. 2003;18(11):1002–1006. doi:10.1002/gps.1002. [DOI] [PubMed] [Google Scholar]
- 52. Caserta MS, Lund DA. Video respite in an Alzheimer's care center: group versus solitary viewing. Activities Adapt Aging. 2002;27(1):13–28. [Google Scholar]
- 53. Gonzalez-Salvador T, Lyketsos CG, Baker A, et al. Quality of life in dementia patients in long-term care. Int J Geriatr Psychiatry. 2000;15(2):181–189. [DOI] [PubMed] [Google Scholar]
- 54. Quinn ME, Johnson MA, Andress EL, McGinnis P. Health characteristics of elderly residents in personal care homes. dementia, possible early dementia, and no dementia. J Gerontol Nurs. 2003;29(8):16–23. [DOI] [PubMed] [Google Scholar]
- 55. Mickus MA, Wagenaar DB, Averill M, Colenda CC, Gardiner J, Luo Z. Developing effective bathing strategies for reducing problematic behavior for residents with dementia: the PRIDE approach. J Ment Health Aging. 2002;8(1):37–43. [Google Scholar]
- 56. Bourgeois M, Dijkstra K, Burgio L, Allen-Burge R. Memory aids as an augmentative and alternative communication strategy for nursing home residents with dementia. Augmentative Altern Commun. 2001;17(3):196–209. [Google Scholar]
- 57. Orrell M, Hancock G, Hoe J, Woods B, Livingston G, Challis D. A cluster randomised controlled trial to reduce the unmet needs of people with dementia living in residential care. Int J Geriatr Psychiatry. 2007;22(11):1127–1134. doi:10.1002/gps.1801. [DOI] [PubMed] [Google Scholar]
- 58. Smith LG. Prayer as an Intervention for Agitation in Dementia Residents [Doctoral dissertation]. ProQuest Dissertations and Theses Database; 2008. UMI No. 3318989. [Google Scholar]
- 59. Dröes RM, Boelens-Van Der Knoop ECC, Bos J., et al. Quality of life in dementia in perspective: an explorative study of variations in opinions among people with dementia and their professional caregivers, and in literature. Dementia. 2006;5(4):533–558. doi:10.1177/1471301206069929 [Google Scholar]
- 60. Powers BA. Everyday ethics of dementia care in nursing homes: a definition and taxonomy. Am J Alzheimers Dis. 2000;15(3):143–151. [Google Scholar]
- 61. Zingmark K, Sandman PO, Norberg A. Promoting a good life among people with Alzheimer's disease. J Adv Nurs. 2002;38(1):50–58. [DOI] [PubMed] [Google Scholar]
- 62. Choi J. Predictors of Physically and Verbally Aggressive Behaviors in Korean Nursing Home Residents With Dementia [Doctoral dissertation]. Dissertations and Theses database; 2001. UMI No. 3008603. [Google Scholar]
- 63. Hoe J, Hancock G, Livingston G, Orrell M. Quality of life of people with dementia in residential care homes. Br J Psychiatry. 2006;188:460–464. doi:10.1192/bjp.bp.104.007658. [DOI] [PubMed] [Google Scholar]
- 64. Zimmerman S, Sloane PD, Williams CS, et al. Dementia care and quality of life in assisted living and nursing homes. Gerontologist. 2005;45 Spec No 1(1):133–146. [DOI] [PubMed] [Google Scholar]
- 65. Gardiner JC, Furois M, Tansley DP, Morgan B. Music therapy and reading as intervention strategies for disruptive behavior in dementia. Clin Gerontol. 2000;22(1):31–46. [Google Scholar]
- 66. Gerdner LA. Effects of individualized versus classical “relaxation” music on the frequency of agitation in elderly persons with Alzheimer's disease and related disorders. Int Psychogeriatr. 2000;12(1):49–65. [DOI] [PubMed] [Google Scholar]
- 67. Koch JM, Datta G, Makhdoom S, Grossberg GT. Unmet visual needs of Alzheimer's disease patients in long-term care facilities. J Am Med Dir Assoc. 2005;6(4):233–237. doi:10.1016/j.jamda.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 68. Kverno KS, Rabins PV, Blass DM, Hicks KL, Black BS. Prevalence and treatment of neuropsychiatric symptoms in advanced dementia. J Gerontol Nurs. 2008;34(12):8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. O’Brien JA, Caro JJ. Alzheimer's disease and other dementia in nursing homes: levels of management and cost. Int Psychogeriatr. 2001;13(3):347–358. doi:10.1017/S1041610201007736 [DOI] [PubMed] [Google Scholar]
- 70. Ruka SM. The effects of reminiscence on promoting a comfort zone: a single subject study of people with dementia in a nursing home (Doctoral dissertation). ProQuest Dissertations and Theses Database. 2003 (UMI No. 3122137). [Google Scholar]
- 71. Reid RC, Chappell NL. Staff ratios and resident outcomes in special care units: do activity aides make a difference? J Appl Gerontol. 2003;22(1):89–103. doi:10.1177/0733464802250047. [Google Scholar]
- 72. Beck CK, Vogelpohl TS, Rasin JH, et al. Effects of behavioral interventions on disruptive behavior and affect in demented nursing home residents. Nurs Res. 2002;51 ( 4):219–228. [DOI] [PubMed] [Google Scholar]
- 73. Finnema E, Dröes RM, Ettema T, et al. The effect of integrated emotion-oriented care versus usual care on elderly persons with dementia in the nursing home and on nursing assistants: a randomized clinical trial. Int J Geriatr Psychiatry. 2005;20(4):330–343. doi:10.1002/gps.1286. [DOI] [PubMed] [Google Scholar]
- 74. Opie J, Doyle C, O’Connor DW. Challenging behaviours in nursing home residents with dementia: a randomized controlled trial of multidisciplinary interventions. Int J Geriatr Psychiatry. 2002;17(1):6–13. doi:10.1002/gps.493. [DOI] [PubMed] [Google Scholar]
- 75. Sung HC, Chang SM, Lee WL, Lee MS. The effects of group music with movement intervention on agitated behaviours of institutionalized elders with dementia in Taiwan. Complement Ther Med. 2006;14(2):113–119. doi:10.1016/j.ctim.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 76. O’Connor DW, Ames D, Gardner B, King M. Psychosocial treatments of behavior symptoms in dementia: a systematic review of reports meeting quality standards. Int Psychogeriatr. 2009;21(2):225–240. doi:10.1017/S1041610208007588. [DOI] [PubMed] [Google Scholar]
- 77. Hicks-Moore SL. Relaxing music at mealtime in nursing homes: effects on agitated patients with dementia. J Gerontol Nurs. 2005;31(12):26–32. [DOI] [PubMed] [Google Scholar]
- 78. Sung HC, Chang AM, Lee WL. A preferred music listening intervention to reduce anxiety in older adults with dementia in nursing homes. J Clin Nurs. 2010;19(7-8):1056–1064. doi:10.1111/j.1365-2702.2009.03016.x. [DOI] [PubMed] [Google Scholar]
- 79. Cohen-Mansfield J, Parpura-Gill A, Golander H. Utilization of self-identity roles for designing interventions for persons with dementia. J Gerontol B Psychol Sci Soc Sci. 2006;61(4):P202–P212. [DOI] [PubMed] [Google Scholar]
- 80. Hicks-Moore SL, Robinson BA. Favorite music and hand massage: tow interventions to decrease agitation in residents with dementia. Dementia. 2008;7(1):95–108. doi:10.1177/1471301207085369. [Google Scholar]
- 81. Kolanowski AM, Litaker M, Buettner L. Efficacy of theory-based activities for behavioral symptoms of dementia. Nurs Res. 2005;54(4):219–228. [DOI] [PubMed] [Google Scholar]
- 82. Kovach CR, Logan BR, Noonan PE. Effects of the serial trial intervention on discomfort and behavior of nursing home residents with dementia. Am J Alzheimers Dis Other Dement. 2006;21(3):147–155. doi:10.1177/1533317506288949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Sloane PD, Hoeffer B, Mitchell CM, et al. Effect of person-centered showering and the towel bath on bathing-associated aggression, agitation, and discomfort in nursing home residents with dementia: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(11):1795–1804. [DOI] [PubMed] [Google Scholar]
- 84. Camp CJ, Cohen-Mansfield J, Capezuti EA. Use of nonpharmacologic interventions among nursing home residents with dementia. Psychiatr Serv. 2002;53(11):1397–1401. [DOI] [PubMed] [Google Scholar]
- 85. Souder E, O’Sullivan P. Disruptive behaviors of older adults in an institutional setting. J Gerontol Nurs. 2003;29(8):31–36. [DOI] [PubMed] [Google Scholar]
- 86. Aminzadeh F, Dalziel WB, Molnar FJ, Garcia LJ. Meanings, functions, and experiences of living at home for individuals with dementia at the critical point of relocation. J Gerontol Nurs. 2010;36(6):28–37. doi:10.3928/00989134-20100303-02. [DOI] [PubMed] [Google Scholar]
- 87. Aminzadeh F, Dalziel WB, Molnar FJ, Garcia LJ. Symbolic meaning of relocation to a residential care facility for persons with dementia. Aging Ment Health. 2009;13(3):487–496. doi:10.1080/13607860802607314. [DOI] [PubMed] [Google Scholar]
- 88. Pioneer Network. About us. http://www.pioneernetwork.net/AboutUs/. Accessed May 18, 2013.


