Abstract
Intergenerational programs are an authentic way to engage elders in meaningful activity and report benefits to both elders and youth. The Avondale Intergenerational Design Challenge (AVID) randomly assigned small teams of technology students aged 13 to 15 years (total N = 59) to 1 of 24 aged care residents with a range of cognitive impairment. Students met with the resident 4 times over 15 weeks and ultimately crafted a personalized item for them. Students showed no change in self-reported attitudes to elders, empathy, or self-esteem post-AVID or at 3-month follow-up, compared to a 3-month within-subject control period pre-AVID. Compared to usual lifestyle activities, residents showed significant improvements in self-reported positive affect and negative affect after student visits and were observed to be significantly more engaged during visits, especially residents with greater cognitive impairment. The personal and guided nature of intergenerational programs may be especially effective in engaging elders with cognitive impairment in meaningful activity.
Keywords: intergenerational, dementia, engagement, affect
Introduction
Participation in meaningful social, leisure, and productive activity is reliably associated with quality of life and well-being in older adults. 1,2 This evidence base is recognized in government documents citing opportunities for social and community contacts and participation in leisure interests as the national minimum standard for residential aged care facilities (RACFs). 3,4 While the corresponding increase in lifestyle and psychosocial interventions in residential aged care has been encouraging, 5 recent papers continue to reiterate old findings that residents spend the majority of their time sleeping, doing nothing, or watching TV and only 13% of the time communicating or participating in hobbies. 6 -8 For this reason, how to engage aged care residents in meaningful and purposeful activities continues to be an important research question and perhaps more so for residents with cognitive impairment where deficits in memory, attention, language, and so forth present unique challenges in engaging this population. 9
Intergenerational programs, whereby older people and youths participate in a shared activity, such as art, dance, reading, or music, have been observed to be engaging for residents with and without dementia. 10 -16 Other reported quantitative benefits for residents include improved quality of life, as well as decreased levels of depression 17 and anxiety. 18 Qualitative studies report an increase in residents’ sense of connectedness, 14,19 “youthfulness,” acceptance, and reciprocity 18 and a decrease in resident fatigue 14 and loneliness. 20
While research indicates that intergenerational programs have positive effects on residents’ well-being, evaluations of the benefits for youth have focused primarily on their attitudes toward older adults or aging. Moreover, the findings have been mixed. Some studies show improved attitudes and behaviors toward elders and people with dementia, 18,21 -24 whereas some show no significant change in perception. 13,25,26 It has been argued that intergenerational programs with a clear purpose and structured visits may be more successful in cultivating positive attitudes toward elders in the younger generation. 22,27
The aim of this study was to evaluate the outcomes of the Avondale Intergenerational Design Challenge (AVID), a good-quality well-defined program that has been recognized by the Australian Aged Care Quality Agency as an example of better practice.23 The program connects 13- to 15-year-old technology students with aged care residents who have a range of cognitive impairment, for whom the students ultimately craft a personalized item based on the resident’s needs and preferences. Previous intergenerational studies indicate improved resident outcomes relating to sense of self and mood. 14,17 -19 The studies typically used self-report measures such as the Quality of Life–Alzheimer’s Disease Scale, Geriatric Depression Scale, 17 and Beck Anxiety Inventory. 18 These scales demand a modest amount of cognitive ability. Using less demanding single-item questions, the present study explored whether these reported benefits could be replicated with residents with a full range of cognitive impairment representative of a standard RACF. Further, resident affect is typically measured through observation and is a consistent feature of observed engagement scales. However, how someone says they are feeling (ie, their subjective perception) has been posited to be the more meaningful indicator of quality of life. 28 Thus, the present study aimed to measure self-reported positive affect and negative affect, independent, as well as part, of exhibited engagement behavior.
In terms of student benefits, the study explored the impact of AVID on students’ attitudes toward elders. The study also aimed to quantify anecdotal and parent reports that by exposing children to people who are different from them, intergenerational programs develop children’s empathy for others. 22,29 The AVID primes students to think about the resident’s needs and behavior, and thus, it was hypothesized that the program may be especially placed to develop children’s empathy. Finally, the study hypothesized that AVID may have a positive impact on students’ self-esteem.
Method
Setting
The study was run concurrently in 2 RACFs, in collaboration with a local independent high school in regional New South Wales, Australia. The study was approved by the University’s Human Research Ethics Committee (HC15171).
Participants
Thirty-seven residents (and/or their family members) were invited to participate by RACF staff. Residents were required to understand spoken English and be well enough to participate in AVID visits. Residents unable to provide their own written consent and who were under public guardianship with no person responsible to consent on their behalf were ineligible to participate. Twenty-six residents (and/or their family members; 70%) provided written consent to participate. Reasons for nonparticipation included health problems (n = 4), too busy/disinterested (n = 2), too anxious (n = 2), or no reason was provided (n = 1). Two residents died between obtaining consent and the study start; thus, the final resident sample was 24.
All technology students in the selected school year (ie, 13-15 years of age; n = 67) identified to participate in AVID were invited to partake in its evaluation, via an information sheet and consent form sent home to their parents. Fifty-nine (88%) students returned written parental consent and completed participation. All students were fluent in English.
Intervention
The AVID intervention took the following structure
Introductory education seminar (40 minutes)
Prior to visiting the RACF, students participated in an orientation seminar with a diversional therapist from the participating RACF (author L.W.). Students learnt about aging, aged care, what to expect during their resident visits, and how to communicate with residents with sensory and cognitive impairments. Students were briefed on the objective to get to know the resident through conversation and reminiscence and to use their technology skills to create something meaningful for the resident based on individual needs and preferences. There was emphasis on the personhood of the resident and students learning about the rich lives of the resident.
Visit 1: “Getting to know the resident” (40 minutes)
Teams of 2 or 3 technology students were each randomly assigned to 1 resident and introduced to their resident at the RACF within a relaxed atmosphere with food and drink. Students came with a pro forma “hint sheet” of questions to ask the residents. At each visit, extra RACF staff were rostered to support the students in their interactions.
Visit 2: “Establishing a need” (40 minutes)
This visit was 3 weeks after the initial visit. Resident hobbies, interests (past and present), and daily routines were typically discussed. Students identified a resident need and used this to establish a design brief. Between visits 2 and 3, students were encouraged to e-mail the diversional therapist at the RACF (author L.W.) for feedback and assistance on their brief.
Visit 3: “Confirming the final design” (40 minutes)
This visit was 4 weeks after the second visit. Students presented their design plans to the resident. As designers, the students were encouraged to include their resident in their plan modifications and give the resident ownership over the design. Over the next 8 weeks before the final visit, students had 3 hours a week in the school workshop to create their product using digital fabrication (computer-controlled machine use, for example, laser cutter), timber, metal, textiles, polymer, and information and communications technologies.
Visit 4: “Presenting the product” (90 minutes)
Each team gave a formal speech that described their resident, their need, and how the product met this need and then presented the product to the resident. Innovations included a timber box to hold knitting wool (to stop the wool from getting tangled), a customized stable table for a resident’s wheelchair, a tactile handmade quilt, and a personalized jewelry box. Clinical registered nurses at the RACF judged how well the product met the resident’s need, and the winning team was awarded a small cash prize. Family members of both residents and students were invited to attend. No student family members attended, but a few resident family members attended. Students did not return to the RACF to see the product being used.
Design
A repeated-measures within-subject design was used. Resident data were collected during the second, third, and fourth student visits only. The day after each of these visits, comparable data were collected for each resident during a typical RACF lifestyle activity (eg, concert), and this was utilized as a within-subject control. Students completed questionnaires 3 months pre-AVID (May 2015), immediately before the start of AVID (August 2015), immediately after AVID ended (November 2015), and at 3-month follow-up (February 2016). The change in outcome measures from pre-AVID to the start of AVID (ie, May to August 2015) was utilized as a within-subject control.
Measures
Resident measures
Resident engagement
Trained RACF staff observed each resident for 5 minutes during the second, third, and fourth student visits (ie, 15 minutes total) and recorded their engagement using the Homecare Measure of Engagement–Staff report, 30 adapted for use in the residential setting. The 6-item scale measures the rate of refusal (ie, how often the resident declined student interactions such as conversation or activity), the average amount of time that the resident was occupied in conversation or activity with the students, the degree of resident attention to the interaction, the resident’s attitude toward the interaction (ie, positive and negative), and the nature of the interaction (ie, passive and active). The 6 weighted scores are summed to create a total score ranging from 1 to 6, where a higher total score reflects higher engagement. The measure has demonstrated good test–retest reliability and convergent validity, 30 and inter-rater reliability for the current sample (based on a sample of 5) indicated very good agreement (κ = .87). The day after each observed student visit, each resident was observed by RACF staff for 5 minutes during a usual RACF lifestyle activity (eg, concert) and their engagement recorded using the Homecare Measure of Engagement–Staff questionnaire. The student visits and lifestyle activity took place in a communal area, and staff observed discreetly from a distance.
Resident affect
Before and after the second, third, and fourth student visits, residents were assisted by staff to rate their present moment affect, that is, how sad, anxious, happy, calm, and valued they felt, using a numbered smiley face scale and the following prompt: “On this scale from 0 to 8, how XXXX are you feeling right now, in this present moment, with 8 being extremely XXXX, and 0 being not at all.” Prescores were subtracted from the postscores to create a change in affect score. The resident affect scale was based on a similar measure used in patients with Alzheimer’s disease. 31 The day after each student visit in which this was recorded, each resident completed the same affect measure before and after a typical RACF lifestyle activity.
Baseline resident demographics, dementia and mental health diagnoses, and sensory impairment data were obtained from resident case notes. Cognitive skills were based on the Psychogeriatric Assessment Scales–Cognitive Impairment Scale (PAS-CIS). Scores range from 0 to 14, with a score of 4 or more indicative of cognitive impairment. 32,33 Chart diagnoses of dementia were also recorded, however, these were not included in covariate analyses as the reliability and timeframe of the diagnoses could not be confirmed.
Student measures
Students completed a basic demographic questionnaire as well as 3 self-report measures.
Rosenberg Self-Esteem Scale. 34
A well-established 10-item measure of global self-esteem (eg, “I feel that I have a number of good qualities”) rated on a 4-point Likert scale from 0 “strongly disagree” to 3 “strongly agree.” Among college students, the scale has strong internal consistency (α = .88) and construct validity. 35 Scores are summed to derive a total score ranging from 0 to 30. A higher score indicates higher self-esteem. Cronbach α for the current study ranged from .85 to .92 across the 4 student data points.
Toronto Empathy Questionnaire. 36
A widely used 16-item measure of empathy (eg, “I can tell when others are sad even when they do not say anything”) scored on a 5-point Likert scale from 0 “never” to 4 “always.” The questionnaire has demonstrated strong internal consistency (α = .87), test–retest reliability (r = .81, P < .001), as well as strong convergent and divergent validity among university students. 36 Scores are summed to derive a total score ranging from 0 to 64. A higher score indicates higher empathy. Cronbach α for the current study ranged from .70 to .78 across the 4 student data points.
Children’s Perceptions of Aging and Elderly. 37
A 20-item measure of children’s attitudes toward older persons (eg, “I like visiting old people”) rated on a 4-point scale from 1 “strongly disagree,” to 4 “strongly agree.” Among children, the measure has shown good test–retest reliability 37 and high internal consistency 38 (α = .86). Scores are summed to derive a total score ranging from 20 to 80. Higher scores indicate more favorable (ie, positive) attitudes toward older persons. Cronbach α for the current study ranged between .82 and .88 across the 4 student data points.
Process evaluation
Attendance of student and resident at each of the AVID sessions was recorded.
Power Analyses
A priori power calculations were conducted using GPower(Version 3). A sample size of 20 residents was sufficient to achieve 80% power to detect a medium effect size (d = .45) between AVID sessions and usual activities on the engagement and present moment affect measures using a 2-tailed test with α for significance set at .05. We recruited 26 residents to allow for missing data/attrition, such as residents not being well enough to attend a student visit.
For student outcomes, power analysis was based on 1 group comparing pre- and postmeasures. A sample size of 60 students would achieve over 80% power to detect a medium effect size (Cohen d = .05) for attitudes to aging and over 70% power to detect a small-to-medium effect size (Cohen d = .03) for self-esteem and empathy, at a significance level of 2-sided .05, assuming a median intraclass correlation (ρ = .5) between pre- and postintervention measures.
Statistical Analyses
For scales missing ≤20% of items, mean substitution was used. Scales with >20% of missing items were excluded. Statistical analyses were conducted using IBM SPSS 22. Tests were 2 tailed, and to correct for the multiple analyses, α was set at .01. Differences in resident engagement and affect change scores between activity conditions over time were analyzed using linear mixed models. Key sample characteristics such as resident gender and cognition were entered as covariates. Nonsignificant covariates and interactions were removed. Linear multilevel models were also utilized to examine changes in student outcomes over time. Linear multilevel models take into account correlations between repeated measurements, as well as inclusion of participants with incomplete data.
Results
Sample Characteristics
Resident demographics are presented in Table 1. The average age of the residents was 87 years and the majority of them were women (67%). Over 79% of residents had chart diagnosis of depression, anxiety, or both. Over 50% or 65% of residents were indicated to have dementia, based on PAS-CIS score or chart diagnosis, respectively. Trimmed means for the sample characteristics did not differ (ie, nothing over 0.2 of a difference) from the original mean, therefore, the extreme scores did not have a strong influence on the mean. The Kolmogorov-Smirnov statistic was significant for the PAS-CIS score, indicating that the assumption of normality was violated. This was rectified using a square root transformation, and this square root PAS-CIS score was used in all analyses.
Table 1.
Baseline Resident Demographics and Other Characteristics.
| Resident Characteristic (n) | n (%) or Mean (SD [Range]) |
|---|---|
| Gender—Female (24) | 16 (66.7) |
| Age in years (24) | 87.13 (7.56 [65-99]) |
| Country of birth—Australia (24) | 16 (66.7) |
| Length of stay, years | 2.47 (2.45 [0.08-10]) |
| Marital status (24) | |
| Widow/divorced | 18 (75) |
| Married/partner | 5 (20.8) |
| Single | 1 (4.2) |
| Sensory impairment (24) | |
| Visual | 14 (58.3) |
| Hearing | 2 (8.3) |
| Visual and hearing | 6 (25) |
| No sensory impairment | 2 (8.3) |
| Mental health (24) | |
| Depression | 11 (45.8) |
| Anxiety | 3 (12.5) |
| Depression and anxiety | 5 (20.8) |
| No mental health difficulties | 5 (20.8) |
| Chart diagnosis of dementia (24) | 16 (66.7) |
| Alzheimer’s disease | 5 (20.8) |
| Vascular dementia | 1 (4.2) |
| Unspecified | 10 (41.7) |
| PAS-CIS score (22) | 5.61 (5.0 [0-14]) |
| Cognitively impaired on PAS-CIS (>5) | 12 (50) |
| Cornell Depression score (23) | 14.44 (6.86 [2-24]) |
Abbreviations: PAS-CIS, Psychogeriatric Assessment Scales–Cognitive Impairment Scale; SD, standard deviation.
The average age of student participants was 14 years (standard deviation [SD] = 0.45, range: 13-15 years), 47.3% were female (n = 28), and the majority were born in Australia (84.7%; n = 50).
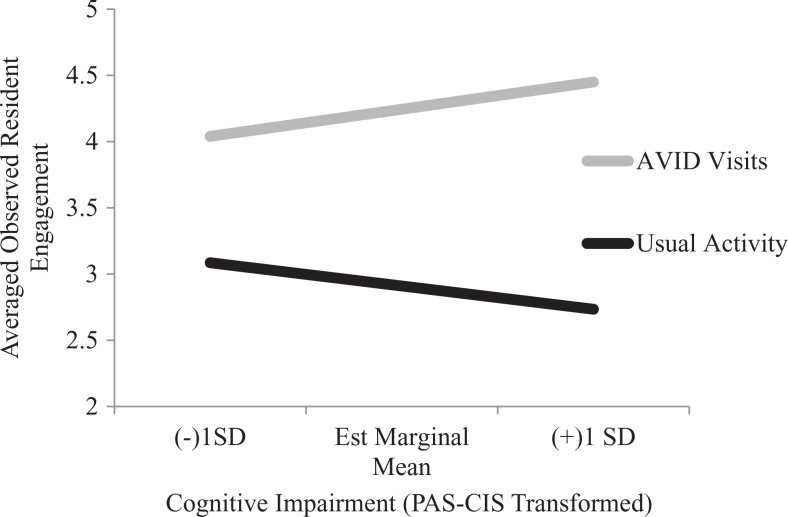
Resident Engagement
There was a significant main effect of activity, in that resident engagement was higher during the AVID student visits compared to usual RACF activities averaged across all 4 time points (see Table 2). Further, there was a significant interaction effect between activity and resident cognition. Specifically, during AVID visits, greater cognitive impairment was associated with increased resident engagement, whereas during usual activities, greater cognitive impairment was associated with decreased resident engagement. Thus, as resident cognitive impairment increased, the difference in engagement between AVID visits and usual activities increased (see Figure 1). Pairwise comparisons revealed that the mean difference between activities, that is, higher engagement during AVID compared to usual activities, was significant across all 3 estimated levels of cognitive impairment, P < .001 (ie, mean level and 1 SD above and below the mean).
Table 2.
Resident Engagement During AVID Student Visits and Usual RACF Lifestyle Activities.
| HoME score | First Observation (n = 23) | Second Observation (n = 23) | Third Observation (n = 24) | Statistical Tests | |||
|---|---|---|---|---|---|---|---|
| AVID Visit Mean (SD) | Usual Activity Mean (SD) | AVID Visit Mean (SD) | Usual Activity Mean (SD) | AVID Visit Mean (SD) | Usual Activity Mean (SD) | ||
| Total | 4.45 ± 0.60 | 3.13 ± 1.07 | 4.42 ± 0.56 | 2.73 ± 0.68 | 3.86 ± 0.92 | 2.80 ± 0.94 | P act = F 1, 124 = 8.73, P = .004; P t = F 2, 124 = 2.52, P = .09; Pcog = F 1, 124 = .044, P = 834; P actxcog = F 1, 124 = 6.86, P = .010 |
Abbreviations: AVID, Avondale Intergenerational Design Challenge; RACF, residential aged care facilities; HoME, Homecare Measure of Engagement-Staff report; Pact , main effect of activity; Pactxcog , the interaction of activity by cognition; Pcog , main effect of cognition; Pt , main effect of time.
Figure 1.
Resident engagement averaged across time, during Avondale Intergenerational Design Challenge (AVID) student visits and usual residential aged care facilities (RACFs) activities as a function of resident cognitive impairment.
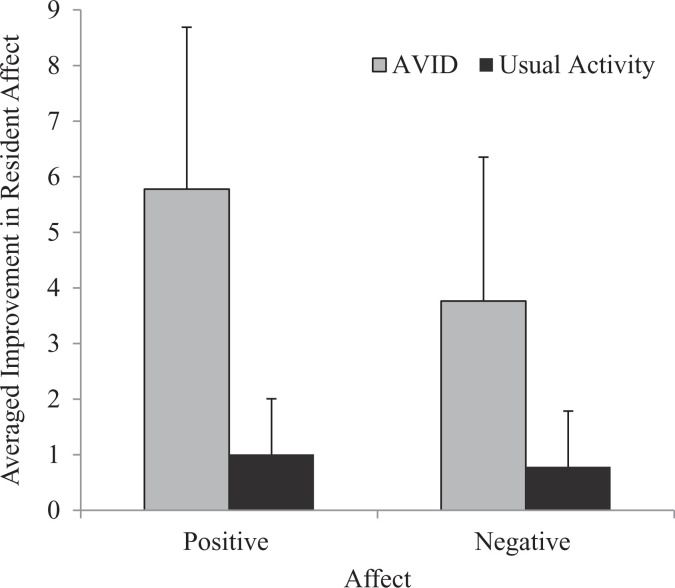
Resident Affect
Residents scores on the affect scale items “happy,” “calm,” and “valued” were collapsed together to create a total positive affect score. Likewise, resident scores on the items “sad” and “anxious” were collapsed together to create a total negative affect score. The scores were collapsed due to significant correlations between the positive affect items, P < .005, and negative affect items, P < .001, and consistent significant change trends across the group of items. There was a significant main effect of activity (ie, AVID vs usual RACF activity). Residents felt more positive (F 1, 133 = 52.22, P < .001) and less negative (F 1, 133 = 30.80, P < .001) from pre- and post-AVID visits relative to pre- and post-usual activities (see Table 3 for scores at each time point and Figure 2 for the total score across time). There were no significant interactions or main effect of time for resident affect.
Table 3.
Positive Affect and Negative Affect of Resident Before and After AVID Student Visits and Usual RACF Lifestyle Activities.
| Feelings | Second Visit | Third Visit | Fourth Visit | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AVID Visit (n = 23) | Usual Activity (n = 23) | AVID Visit (n = 23) | Usual Activity (n = 22) | AVID Visit (n = 24) | Usual Activity (n = 24) | |||||||||||||
| Pre Mean (SD) | Post Mean (SD) | M Ch. | Pre Mean (SD) | Post Mean (SD) | M Ch. | Pre Mean (SD) | Post Mean (SD) | M Ch. | Pre Mean (SD) | Post Mean (SD) | M Ch. | Pre Mean (SD) | Post Mean (SD) | M Ch. | Pre Mean (SD) | Post Mean (SD) | M Ch. | |
| Positive emotion | 13.26 ± 4.14 | 19.78 ± 4.08 | 6.52 ± 3.89 | 15.17 ± 4.91 | 15.13 ± 6.31 | −0.04 ± 4.93 | 14.77 ± 4.25 | 19.32 ± 4.20 | 4.55 ± 4.11 | 14.76 ± 4.16 | 16.17 ± 4.12 | 1.41 ± 3.37 | 14.73 ± 3.35 | 21.46 ± 3.06 | 6.68 ± 4.86 | 15.62 ± 4.00 | 17.13 ± 3.52 | 1.50 ± 2.27 |
| Negative emotion | 5.04 ± 3.67 | 1.87 ± 2.63 | −3.17 ± 2.92 | 5.65 ± 3.86 | 4.61 ± 4.46 | −1.04 ± 3.40 | 5.45 ± 4.19 | 1.82 ± 2.30 | −3.63 ± 3.79 | 5.74 ± 2.86 | 4.83 ± 2.87 | −0.91 ± 2.60 | 6.45 ± 3.26 | 1.83 ± 2.20 | −4.55 ± 3.63 | 5.63 ± 3.68 | 5.17 ± 3.68 | −0.46 ± 2.30 |
Abbreviations: AVID, Avondale Intergenerational Design Challenge; M Ch., mean change.
Figure 2.
Improvement in resident affect averaged across time, from pre- and post-Avondale Intergenerational Design Challenge (AVID) student visits and usual residential aged care facilities (RACFs) activities.
Student Attitudes to Older Adults, Self-Esteem, and Empathy
There was no significant change in students’ attitudes to older adults, self-esteem, or empathy, at any time point, P > .005 (see Table 4).
Table 4.
Student Self-Reports of Self-Esteem, Attitudes to Older Adults, and Empathy, Across the 4 Study Time Points.
| Student Measure | Pre (−3 Months; n = 55), Mean (SD) | Baseline (0; n = 59), Mean (SD) | Post (+3 Months; n = 58), Mean (SD) | Follow-Up (+6 Months; n = 56), Mean (SD) |
|---|---|---|---|---|
| RSES | 16.98 (5.78) | 16.52 (5.60) | 16.66 (5.72) | 19.39 (6.47) |
| CPAE | 55.83 (6.38) | 56.29 (6.36) | 55.44 (6.79) | 54.70 (6.85) |
| TEQ | 20.85 (6.09) | 21.96 (6.46) | 20.60 (6.33) | 22.59 (6.85) |
Abbreviations: CPAE, Children’s Perceptions of Aging and Elderly; RSE, Rosenberg Self-Esteem Scale; TEQ, Toronto Empathy Questionnaire.
Process Evaluation
All residents were present for at least 3 of the 4 student visits. Over 79% of residents (n = 19) were present for all 4 student visits. Regarding the “usual activity,” 87.5% of residents (n = 21) attended all 3 activity points. Further information regarding attendance can be observed in Table 5. Reasons for nonattendance were typically ill health.
Table 5.
Attendance of Resident and Student at Each AVID Visit.
| AVID Visit | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Residents | ||||
| Student visit | 21 | 23 | 23 | 24 |
| Other activity | NA | 23 | 22 | 24 |
| Studentsp a | 54 | 53 | 54 | 55 |
| StudentsTot b | 61 | 58 | 60 | 60 |
Abbreviation: AVID, Avondale Intergenerational Design Challenge.
aIncludes students who participated in the research component of AVID.
bIncludes all students who participated in AVID independent of the research component.
Discussion
Residents felt more positive (ie, happier, calmer, and more valued) and less negative (ie, sad or anxious) after AVID student visits relative to after usual RACF lifestyle activities. Residents were also more engaged during student visits relative to usual activities. These benefits are consistent with the outcomes of other intergenerational programs. 10 -16 Moreover, engagement was shown to be particularly enhanced during AVID for residents with greater cognitive impairment. Although past studies have revealed that cognitive impairment is not prohibitive of participation or engagement in intergenerational programs, and that intergenerational programs may be equally beneficial for residents with and without dementia, 15 this study is distinctive in its finding that intergenerational programs could be especially beneficial for residents with cognitive impairment. In the context of reported low levels of meaningful or engaging activity in RACFs, 6,8 and findings relating cognitive impairment to lower engagement in RACF activities, 9 this finding has important implications for aged care providers. Indeed, the current study also showed that as cognitive impairment increased, observed engagement in usual RACF activities decreased.
The AVID program involved personal, 2- or 3-on-1, “guided” interactions or conversations. For example, students were able to lead or direct the interaction, by asking questions, offering information or inviting the resident to engage with an item they had brought in. For residents with cognitive impairment with possible challenges in attention and self-initiation and so forth, it makes sense that this type of activity may be more engaging than typically less personalized, group-led RACF activities. This idea is corroborated by the finding that guided, as opposed to unguided, interactions lead to longer engagement durations in residents with dementia. 39 For residents with minimal or mild cognitive impairment, who may be more able to attend or self-initiate, for example, activity type may have a reduced impact on engagement. It would be interesting to ascertain whether there was something special about the AVID visits being with students or whether similar results could be obtained with adult visits, for example. In other words, is it the age of the visitors that is important, or rather having someone, of any age, engage personably one-on-one with the resident that is important? Future controlled comparisons of youth visits versus adult visits would be fruitful in answering this question.
Another tentative conjecture as to why AVID may have been especially engaging for residents with cognitive impairment is the novel and social nature of the program. Both original and social stimuli are more attention-grabbing than familiar or nonsocial stimuli. 40 In a typically routine-driven RACF, AVID may have crossed a higher threshold in obtaining and maintaining the interest and attention of residents with cognitive impairment. Future research looking into how the interactions differ between students and residents depending upon on the resident’s level of cognitive impairment would assist this discussion.
We deliberately chose common lifestyle activities as a control because they are representative of most RACFs. However, this means that the observed benefits of AVID could simply be a function of reducing the “boredom” of the residents’ routine in the RACF. For example, residents’ rather flat emotional responses after the usual RACF activity could be indicative of boredom. We did not ask residents how bored they felt nor did we collect data on frequency of outside visitors (distinct to the student visits). However, post hoc analyses indicated that when controlling for length of stay at the RACF (an assumed correlate of boredom to routine), the interaction between activity and cognitive impairment for engagement remained, as did the main effects of activity for positive and negative mood (and engagement), P < .001 (see note 1). This suggests that there is still something about AVID, beyond potential boredom effects, that is, engaging and mood enhancing. In a qualitative study exploring perspective of people with dementia on what makes an activity meaningful when living in an RACF, themes comprised feeling valued and included via quality social interactions, talking about the past, and having visitors who took an interest. 41 Such concepts parallel the activities involved in AVID. The AVID also invited residents to contribute to students’ technology projects, which was congruent with another reported theme of being able to make a contribution. 41 The mechanism by which AVID (and other intergenerational initiatives) benefits residents, and especially residents with dementia, is an endeavor for future research. In addition to resident benefits, if intergenerational programs show mutual benefits to youths, this is valid evidence for implementing such programs. Past literature endorses improvements in children’s attitudes and behaviors toward elders 18,21 -24 and, to a less-established extent, empathy. 22,29 The current study showed no benefits to students, in terms of positive attitudes toward elders, empathy, or self-esteem. In fact, students’ scores remained relatively static across all time points. Students only had 3.5 hours of face-to-face time with residents, thus, it is likely that the contact was too minimal for AVID to have an effect, especially for quite stable constructs such as self-esteem and empathy. Where studies have reported a beneficial (qualitative) effect on youths’ empathy, intergenerational contact was regular and sustained over several months. 22,29 The study endeavor to explore youth benefits beyond attitude change was an important attempt to progress research into the youth benefits of intergenerational programs. However, it seems that we do not yet have the optimal measures by which to quantifiably capture the wealth of self- and informant anecdotal reports of the benefits (such as the noticeable involvement of students otherwise typically reserved) to participating youths.
The strength of the study was the controlled design. A significant limitation to the interpretation of the engagement finding is that engagement was rated by RACF staff, nonblinded to the study purpose and of course activity. Single-item affect measures are less reliable than multi-item measures, yet in the current study, they had the worthy purpose of enabling residents of all cognitive abilities to contribute to the evaluation of their participation in AVID. The sample size was adequate relative to other evaluation studies of intergenerational programs, wherein resident numbers typically range from 10 to 25. While the in-the-moment benefits of improved engagement and mood during AVID may be sufficient justification to implement the program, 42 future research assessing whether there are any carryover effects, for example, asking the affect items once more 20 minutes after the students departure, would make a valuable contribution to the psychosocial literature. In summary, AVID is more engaging and mood enhancing to residents than usual activities in RACFs. Moreover, AVID may be an especially effective way of providing meaningful activity for residents with cognitive impairment.
Note
We thank an anonymous reviewer for this suggestion.
Footnotes
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: L.W. and J.R. are staff (diversional therapist and physiotherapist, respectively) at the participating residential aged care facilities. N.L. is technologies coordinator at the participating school.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Adams KB, Leibbrandt S, Moon H. A critical review of the literature on social and leisure activity and wellbeing in later life. Ageing Soc. 2011;31(4):683–712. [Google Scholar]
- 2. Moyle W, O’Dwyer S. Quality of life in people living with dementia in nursing homes. Curr Opin Psychiatry. 2012;25(6):480–484. [DOI] [PubMed] [Google Scholar]
- 3. Australian Aged Care Quality Agency. Accreditation Standards. Canberra, Australia: Government of Australia; 2014. [Google Scholar]
- 4. Department of Health. Care Homes for Older People: National Minimum Standards. London, United Kingdom: STO; 2003. [Google Scholar]
- 5. Trahan MA, Kuo J, Carlson MC, Gitlin LN. A systematic review of strategies to foster activity engagement in persons with dementia. Health Educ Behav. 2014;41(suppl 1):70S–83S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. den Ouden M, Bleijlevens MHC, Meijers JMM, et al. Daily (in)activities of nursing home residents in their wards: an observation study. J Am Med Dir Assoc. 2015;16(11):963–968. [DOI] [PubMed] [Google Scholar]
- 7. Harper Ice G. Daily life in a nursing home. Has it changed in 25 years? J Aging Stud. 2002;16(4):345–359. [Google Scholar]
- 8. Casey AN, Low LF, Goodenough B, Fletcher J, Brodaty H. Computer-assisted direct observation of behavioral agitation, engagement, and affect in long-term care residents. J Am Med Dir Assoc. 2014;15(7):514–520. [DOI] [PubMed] [Google Scholar]
- 9. Kolanowski A, Buettner L, Litaker M, Yu F. Factors that relate to activity engagement in nursing home residents. Am J Alzheimers Dis Other Demen. 2006;21(1):15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Low LF, Russell F, McDonald T, Kauffman A. Grandfriends, an intergenerational program for nursing-home residents and preschoolers: a randomized trial. J Intergener Relatsh. 2015;13(3):227–240. [Google Scholar]
- 11. Camp CJ, Judge KS, Bye CA, et al. An intergenerational program for persons with dementia using Montessori methods. Gerontologist. 1997;37(5):688–692. [DOI] [PubMed] [Google Scholar]
- 12. Lee MM, Camp CJ, Malone ML. Effects of intergenerational Montessori-based activities programming on engagement of nursing home residents with dementia. Clin Interv Aging. 2007;2(3):477–483. [PMC free article] [PubMed] [Google Scholar]
- 13. Xaverius PK, Mathews RM. Evaluating the impact of intergenerational activities on elders’ engagement and expressiveness levels in two settings. J Intergener Relatsh. 2004;1(4):53–69. [Google Scholar]
- 14. Skropeta CM, Colvin A, Sladen S. An evaluative study of the benefits of participating in intergenerational playgroups in aged care for older people. BMC Geriatr. 2014;14(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jarrott SE, Bruno K. Intergenerational activities involving persons with dementia: an observational assessment. Am J Alzheimers Dis Other Demen. 2003;18(1):31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Short-DeGraff MA, Diamond K. Intergenerational program effects on social responses of elderly adult day care members. Educ Gerontol. 1996;22(5):467–482. [Google Scholar]
- 17. Chung JCC. An intergenerational reminiscence programme for older adults with early dementia and youth volunteers: values and challenges. Scand J Caring Sci. 2009;23(2):259–264. [DOI] [PubMed] [Google Scholar]
- 18. George DR. Intergenerational volunteering and quality of life: mixed methods evaluation of a randomized control trial involving persons with mild to moderate dementia. Qual Life Res. 2011;20(7):987–995. [DOI] [PubMed] [Google Scholar]
- 19. Teater B. Intergenerational programs to promote active aging: the experiences and perspectives of older adults. Act Adapt Aging. 2016;40(1):1–19. [Google Scholar]
- 20. Harris PB, Caporella CA. An intergenerational choir formed to lessen Alzheimer’s disease stigma in college students and decrease the social isolation of people with Alzheimer’s disease and their family members: a pilot study. Am J Alzheimers Dis Other Demen. 2014;29(3):270–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Heyman JC, Gutheil IA, White-Ryan L. Preschool children’s attitudes toward older adults: comparison of intergenerational and traditional day care. J Intergener Relatsh. 2011;9(4):435–444. [Google Scholar]
- 22. Femia EE, Zarit SH, Blair C, Jarrott SE, Bruno K. Intergenerational preschool experiences and the young child: potential benefits to development. Early Child Res Q. 2008;23(2):272–287. [Google Scholar]
- 23. Lokon E, Kinney JM, Kunkel S. Building bridges across age and cognitive barriers through art: college students’ reflections on an intergenerational program with elders who have dementia. J Intergener Relatsh. 2012;10(4):337–354. [Google Scholar]
- 24. Powers M, Gray M, Garver K. Attitudes toward older adults: results from a fitness-based intergenerational learning experience. J Intergener Relatsh. 2013;11(1):50–61. [Google Scholar]
- 25. Middlecamp M, Gross D. Intergenerational daycare and preschoolers’ attitudes about aging. Educ Gerontol. 2002;28(4):271–288. [Google Scholar]
- 26. Belgrave M. The effect of a music therapy intergenerational program on children and older adults’ intergenerational interactions, cross-age attitudes, and older adults’ psychosocial well-being. J Music Ther. 2011;48(4):486–508. [DOI] [PubMed] [Google Scholar]
- 27. Cook G, Bailey C. Older care home residents’ views of intergenerational practice. J Intergener Relatsh. 2013;11(4):410–424. [Google Scholar]
- 28. Logsdon RG, Gibbons LE, McCurry SM, Teri L. Assessing quality of life in older adults with cognitive impairment. Psychosom Med. 2002;64(3):510–519. [DOI] [PubMed] [Google Scholar]
- 29. Schwalbach E, Kiernan S. Effects of an intergenerational friendly visit program on the attitudes of fourth graders toward elders. Educ Gerontol. 2002;28(3):175–187. [Google Scholar]
- 30. Baker JR, Harrison F, Low LF. Development of two measures of client engagement for use in home aged care. Health Soc Care Community. 2016;24(3):363–374. [DOI] [PubMed] [Google Scholar]
- 31. Guzmán-Vélez E, Feinstein JS, Tranel D. Feelings without memory in Alzheimer disease. Cogn Behav Neurol. 2014;27(3):117–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Robinson JA, Crawford GB. Do palliative patients and carers agree about patients’ psychological functioning? Palliat Support Care. 2010;8(1):69–74. [DOI] [PubMed] [Google Scholar]
- 33. Department of Health and Ageing. Aged Care Funding Instrument: User Guide. Australia: Commonwealth of Australia; 2009. [Google Scholar]
- 34. Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University; 2015. [Google Scholar]
- 35. Robins RW, Hendin HM, Trzesniewski KH. Measuring global self-esteem: construct validation of a single-item measure and the Rosenberg Self-Esteem Scale. Pers Soc Psychol Bull. 2001;27(2):151–161. [Google Scholar]
- 36. Spreng RN, McKinnon MC, Mar RA, Levine B. The Toronto Empathy Questionnaire: scale development and initial validation of a factor-analytic solution to multiple empathy measures. J Pers Assess. 2009;91(1):62–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rich PE, Myrick RD, Campbell C. Changing children’s perceptions of the elderly. Educ Gerontol. 1983;9(5-6):483–491. [Google Scholar]
- 38. Aday RH, Sims CR, Evans E. Youth’s attitudes toward the elderly: the impact of intergenerational partners. J Appl Gerontol. 1991;10(3):372–384. [Google Scholar]
- 39. Leone E, Deudon A, Piano J, Robert P, Dechamps A. Are dementia patients engagement using tailored stimuli the same? The apathy dilemma in nursing home residents. Curr Gerontol Geriatr Res. 2012;2012:942640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Strack F, Förster J. Social Cognition: The Basis of Human Interaction. New York: Psychology Press; 2009. [Google Scholar]
- 41. Harmer BJ, Orrell M. What is meaningful activity for people with dementia living in care homes? A comparison of the views of older people with dementia, staff and family carers. Aging Ment Health. 2008;12(5):548–558. [DOI] [PubMed] [Google Scholar]
- 42. MacPherson S, Bird M, Anderson K, Davis T, Blair A. An Art Gallery Access Programme for people with dementia: ‘You do it for the moment’. Aging Ment Health. 2009;13(5):744–752. [DOI] [PubMed] [Google Scholar]