Abstract
This study was conducted to obtain data regarding the association of caregiver burden (CB) and neuropsychiatric symptoms (NPSs) in patients with Alzheimer’s disease. We conducted a series of multiple linear regressions to determine the relationship between CB and NPSs and whether the caregiver coping strategies mediated this relationship. The NPSs were assessed using the Neuropsychiatric Inventory, and caregivers were evaluated with the Caregiver Burden Interview and the Inventory and the Coping Strategies Inventory. Results show that patients with more frequent and severe NPS were more likely to be cared for by more burdened caregivers, and this was partially mediated by caregiver coping strategies. More disengagement (β = .330, P < .001) and less engagement coping (β = −.347, P < .001) were predictors for NPS after adjusting for patient and caregiver characteristics. These results may be useful with a view to designing treatment interventions that aim to modify the use of caregiver coping strategies and to reduce NPSs.
Keywords: Alzheimer’s disease, neuropsychiatric symptoms, caregiver burden, coping, anxiety, depression
Introduction
Patients with Alzheimer’s disease (AD) have high rates of neuropsychiatric symptoms (NPSs) at some point during their illness. 1,2 The presence of NPSs is associated with greater caregiver burden (CB), 3,4 greater cost of care, 5 and a shorter period of time prior to long-term institutionalization. 6 The NPSs also cause a loss of independence that in turn negatively affects the quality of life for both patients with AD and their caregivers. 7,8
The pathogenesis of NPSs has not been sufficiently defined, but recent studies have emphasized the significance of a complex interaction of neurobiological factors (eg, neurochemical, neuropathological, and genetic changes) and psychological and social factors. 9 Many studies have investigated predictors of NPSs, focusing on patient characteristics, such as demographics, cognitive impairment, dementia severity, decline in or loss of functional activities of daily living, 2,8,10 or caregiver characteristics such as age, education, relationship to the patient, hours spent caring, whether living with the patient, or low economic status. 11,12 However, only a few studies have investigated the role of CB in the presence of NPSs. 12,13 The assumption usually has been that NPSs cause CB. Although NPSs undoubtedly contribute to CB, the relationship is likely to be bidirectional. Because many NPS may represent unmet needs in the patient, or the patient's progressively reduced capacity to cope with stress, 9 it is possible that some patient-caregiver interpersonal interactions might contribute to the presence of NSP mediated by the caregiver coping strategies used.
Coping consists of constant cognitive and behavioral responses that individuals use to control or tolerate specific external and/or internal demands that are evaluated as something that exceeds their normal resources 14,15 and is recognized for its significant impact on stress-related mental and physical health problems and for its intervention potential. 16 The experience of caring for a person with AD has been analyzed within the context of transactional models of stress, and within this framework, stress is defined as an interaction between the person and the environment appraised by the person as taxing or exceeding his or her resources and as endangering well-being. 15 This definition conceptualizes coping as a dynamic process, as it consists of a series of reciprocal responses through which the individual and the environment interact and influence each other, and it incorporates a series of intentional actions, both cognitive and behavioral, meant to control the negative impact of the stressful event or situation. 14,15
There is some empirical evidence for the existence of several primary dimensions of coping: problem solving, wishful thinking, problem avoidance, social support, cognitive restructuring, self-criticism, emotional expression, or social withdrawal. 17 These primary coping strategies can be organized into 2 higher order categories: engagement or disengagement strategies. 17 Coping efforts are first categorized as to whether they represent an engagement strategy, involving approach-related actions that result in confronting stressors, often viewed as a crucial factor in limiting the long-term psychological and physiological sequelae of environmental stressors, or disengagement strategy seeking to limit exposure to noxious stimuli, often producing desirable short-term effects, but leading to longer term problems, including depressive symptoms. Within these categories, the target of the coping effort is either problem focused or emotion focused. Emotion-focused coping emphasizes the regulation of one’s affective response, whereas problem-focused coping emphasizes management of the stress-producing situation. 17,18 Engagement coping includes strategies such as problem solving, cognitive restructuring, expression of emotions, and social support, whereas disengagement coping includes strategies such as problem avoidance, wishful thinking, self-criticism, and social withdrawal (Table 1).
Table 1.
Coping Strategies Inventory by Subgroup.
| Engagement strategies |
| Problem solving |
| I worked on solving the problems in the situation |
| I made a plan of action and followed it |
| Cognitive restructuring |
| I reorganized the way I looked at the situation, so things didn’t look so bad |
| I convinced myself that things aren’t quite as bad as |
| Express emotions |
| I let my emotions out |
| I got in tough with my feelings and just let them go |
| Social support |
| I talked to someone about how I was feeling |
| I found somebody who was a good listener |
| Disengagement strategies |
| Problem avoidance |
| I avoided thinking/doing anything about the situation |
| I went along as if nothing were happening |
| Wishful thinking |
| I hoped a miracle would happen |
| I wished that the situation would go away or somehow |
| Self-criticism |
| I criticized myself for what happened |
| I blamed myself |
| Social withdrawal |
| I spent more time alone |
| I avoided being with people |
We conducted this study with a view to obtaining data regarding the association of CB and NPSs in patients with AD. We hypothesized that CB would be independently associated with NPSs after controlling for patient and caregiver characteristics and that this would be mediated by the caregiver coping strategies used. Patients with more frequent and severe NPSs were more likely to be cared for by caregivers using disengagement coping strategies.
Materials and Methods
Participants and Study Design
This is part of a larger study involving people with AD and their primary caregivers from city, town, and rural areas in Málaga and Central Spain (the MÁLAGA-AD study). Purposive recruitment was carried out with the aim of the sample being representative of people living with dementia in terms of dementia severity, gender, and care setting. 19
Participants were contacted through local health services and the voluntary sector. A total of 114 recipients and their primary caregivers were originally interviewed for the MÁLAGA-AD study, of whom 80 family caregivers agreed to take part and were included in our study. Of those not included, 20 did not complete the interview and 14 refused. All patients satisfied the criteria of the National Institute of Neurological and Communicative Disorders and the Stroke/Alzheimer’s Disease and Related Disorders Association for probable AD. 20 A further inclusion criterion was that the responsible caregiver must live with the patient, be directly involved in the patient’s care, and be a reliable source of information.
Trained researchers explained the study to the participants and requested their voluntary participation. All participants were required to sign an informed consent form. In cases where the patient did not have capacity, we asked caregivers whether they thought the patient would have agreed to participate if they could. Once they had agreed, caregivers were assessed by the research authors and data collected by the authors themselves (psychiatrist, neuropsychologist, and neurologist). During the same assessment, the interviewer compiled information on the patient’s demographics and clinical characteristics. The study was approved by the ethical committee of both the Instituto Andaluz de Neurociencia y Conducta and the University of Malaga.
Patient Data
Information was recorded on age, gender, marital status, years of education, duration of dementia from the initial diagnosis made by the specialist up to the time of evaluation, previous history of psychiatric disorders, and use of psychoactive medication (antidepressants, antipsychotics, anxiolytics or hypnotics) and antidementia drugs. Cognitive function was tested using the Mini-Mental State Examination (MMSE) 21 in its validated version in Spanish. 22 Activities of daily living (ADLs) were assessed by the Bayer Activities of Daily Living Scale (B-ADLs) 23 in its validated version in Spanish. 24 It comprises 25 items that are answered by the caregiver. The first items evaluate the patient’s ability to handle ADLs and capacity for self-care. Other items evaluate specific tasks. The last items assess cognitive functions that are important for performing activities of daily living. The score for each item ranges from 1 to 10; the lower the score, the higher the functional capacity. A mean score was obtained from 25 items.
The staging of the dementia was carried out with the Global Deterioration Scale (GDS). 25 The present study included patients in stages 4 (moderate cognitive decline), 5 (moderate to severe cognitive decline), and 6 (severe cognitive decline) of the GDS.
The study of NPSs was carried out using the Neuropsychiatric Inventory (NPI) 26 in its validated version in Spanish. 27 Cronbach α was reported to be .88. The NPI consists of a structured interview based on the answers given by the patient responsive caregiver. It is composed of 12 subscales that evaluate the most commonly occurring NPS in patients with AD: delusions, hallucinations, agitation, depression, anxiety, euphoria, apathy/indifference, disinhibition, irritability/, aberrant motor activity, sleep disorders, and eating disorders. Those who showed the symptom in each subscale, the caregiver scored it from 1 to 4 according to its frequency and from 1 to 3 in regard to its severity. A composite score for each subscale was obtained by multiplying frequency by severity, with a maximum of 12 points. Total NPI score can be obtained regarding frequency (maximum: 48 points), severity (maximum: 36 points), and composite score (maximum: 144 points).
Caregiver Data
Information on age, gender, level of education, relationship with the patient, marital status, number of hours per day spent giving care, and whether they were living with the patient was compiled. In addition, caregivers completed the following:
The Caregiver Burden Interview (CBI) 28 in its validated version in Spanish. 29 Cronbach α was reported to be .92. This consists of a 22-item self-report questionnaire that is the most consistently used measure of CB. The CBI measures caregivers’ subjective burden of caregiving in terms of health, finance, and social/interpersonal relationships. Participants’ responses were entered on a 5-point scale (0 = never to 4 = nearly always).
The Beck Depression Inventory (BDI), 30 a 21-item self-report questionnaire, used to measure the severity of depressive symptoms. Each item is composed of 4 statements, representing increasing increments of depression severity for a particular symptom. The score for each item ranges from 0 to 3, with the total score ranging from 0 to 63. The Spanish version of the BDI was used in this study. 31 Cronbach α was reported to be .90.
The State-Trait Anxiety Inventory (STAI). 32 For the purpose of this study, we used the state anxiety subscale (STAI-S) to assess caregiver anxiety. This is composed of 20 statements, which the individual answers stating how he or she usually feel. Each item score ranges from 0 to 3 points, and the total score ranges from 0 to 60 points; the higher the score, the higher the anxiety. State anxiety has been defined as an emotional state characterized by feelings of apprehension and tension with changes in the level of activity of the autonomous nervous system, which can alter over time. The Spanish version 33 of the STAI demonstrated good psychometric properties with Cronbach α = .93.
The Coping Strategies Inventory (CSI). 17 This is a self-report questionnaire with 8 subscales describing different coping strategies, with 5 items per scale. Caregivers were asked to score each strategy from 0 (not doing it at all) to 4 (doing it a lot; see Table 1). Satisfactory psychometric properties have been reported. Individual coping strategies are broadly categorized into 2 basic approaches to managing stressful situations: coping activities that engage the individual with the stressful situation and coping activities that disengage the individual from it. The Spanish version 34 of the CSI demonstrated good psychometric properties with Cronbach α ranging from 0.63 for Problem Avoidance coping strategies to 0.89 for Self-criticism coping strategies. The convergent validity was verified using intercorrelations between scales, correlations with personality dispositions and with coping efficacy.
Statistical Analysis
A retrospective power calculation revealed that a sample size of 70 caregivers was sufficient to test for a significantly moderate effect size of 0.25 when adding the coping strategies to a linear regression with the NPS as dependent variable and CB as an independent variable, using a significance level of .05 and power of 90%.
Descriptive statistics such as mean and standard deviation were obtained for all variables, including demographic and clinical characteristics of both patient and caregiver. Analysis of the distribution type was performed for continuous variables using 1 sample Kolmogorov-Smirnov test.
The relationship between caregiver and patient characteristics and NPI composite scores was assessed through 1-way analysis of variance, 2-tailed Student t tests, or correlation coefficients, when appropriate.
In order to test our main hypothesis that caregiver coping strategies mediated the relationship between CB and NPI composite scores, we used generally accepted criteria 35 to define mediation. According to these authors, first a variable functions as a mediator when it meets the following conditions: (1) variations in levels of the independent variable significantly account for variations in the dependent variable, (2) variations in levels of the independent variable significantly account for variations in the presumed mediator, (3) variations in the mediator significantly account for variations in the dependent variable; and second when a significant relationship between independent and dependent variable is reduced by adding the mediator to the model, with the strongest demonstration of mediation occurring when this relationship is zero.
We therefore conducted 4 multiple linear regressions to determine the relationship between (1) CB and NPSs, (2) CB and caregiver coping strategies, and (3) caregiver coping strategies and NPSs. A final regression was also run, which included both CB and caregiver coping strategies as predictors of NPSs. In this situation, if the relationship between CB and NPSs was no longer significant, full mediation would have occurred; if it was reduced but still significant, this would show partial mediation. In each of these models, the patient and caregiver characteristics associated with both CB and NPSs on bivariate analyses were included as covariates. In order to determine mediation significance, we conducted a Sobel test 36 and calculated the effect size of adding coping to the equation containing CB from the R2 values, using appropriate software 37 ; an effect size >0.35 is conventionally described as large, and the one >0.15 as a medium effect size. P values ≤ .05 were considered statistically significant. Analyses were performed using SPSS, version 20.
Results
There were no differences between caregivers who took part in the study and those who refused to take part or did not complete the interview in terms of gender (female 77.5% vs 75.8%, χ2 = 1.7, P = .34), mean age (62.15 ± 10.37 vs 64.12 ± 9.80, t = 1.46, P = .27), or relationship with the care recipient (χ2 = 2.3, P = .51).
Demographic and clinical characteristics of the 80 patients with AD and their caregivers and their relationship with NPI composite scores are shown in Table 2. Analysis of the results showed that the average caregiver of a patient with AD is female and approximately 60 years old. They were daughters or housewives and were personally involved in caring for patients. The majority of caregivers lived with the patient and reported good or excellent health. The mean age of the patients was 77 years, with an average level of education of 6.5 years. Nearly 62% of the patients were women. The estimated duration of dementia was 60 months. Mean overall cognitive scores (MMSE, 15.01) suggested moderate to severe dementia. Most patients (95%) had NPSs and displayed a mean number of NPSs per patient of 5.4 ± 1.87. The most prevalent symptoms in the sample were apathy (92%), followed by irritability (63%), depression (58%), and agitation (50%). The less prevalent symptoms were hallucinations (18%) and euphoria.
Table 2.
Characteristics of Sample and Their Relationship With NPS.
| Mean (SD) or number (%) | NPI composite scores | P value | |
|---|---|---|---|
| Caregiver | |||
| Age | 62.15 (10.37) | r = −.45 | <.01 |
| Gender, female | 62 (77.5%) | t = 2.98 | <.01 |
| Education, years | 6.56 (2.60) | r = −.39 | <.01 |
| Hours spent caring | 12.70 (8.31) | r = .36 | <.001 |
| Relationship | |||
| Son/daughter | 35 (43.8%) | F = 0.291 | .022 |
| Husband/wife | 31 (38.8%) | ||
| Brother/sister | 6 (7.4%) | ||
| Other relatives | 8 (10%) | ||
| Marital status | |||
| Married | 63 (78.8%) | F = 0.083 | .823 |
| Single | 9 (11.2%) | ||
| Widowed | 8 (10%) | ||
| Lives with patient | |||
| Yes | 60 (75%) | t = 3.87 | .043 |
| No | 20 (25%) | ||
| Health | |||
| Excellent | 32 (40%) | F = 0.776 | .574 |
| Good | 30 (37.5%) | ||
| Poor | 18 (22.5%) | ||
| CBI | 32.71 (11.35) | r = .54 | <.001 |
| BDI | 28.11 (8.76) | r = .42 | <.001 |
| STAI-S | 34.50 (11.61) | r = .14 | .062 |
| Engagement coping | 9.44 (3.61) | r = −.59 | <.0001 |
| Disengagement coping | 10.35 (3.55) | r = .58 | <.0001 |
| Patient | |||
| Age | 77.34 (5.74) | r = .16 | .076 |
| Gender, female | 50 (62.5%) | t = 0.38 | <.050 |
| Education, years | 6.56 ± 2.62 | r = .11 | .985 |
| Marital status | |||
| Married | 38 (47.5%) | F = 1.982 | .678 |
| Single | 8 (10%) | ||
| Widowed | 34 (42.5%) | ||
| Duration of dementia, months | 60.23 (25.15) | r = .34 | <.01 |
| History of psychiatric disorders | 35 (43.8%) | t = 1.92 | <.01 |
| Psychoactive drugs | 53 (66.3%) | t = 0.27 | .432 |
| Antidementia drugs | 65 (81.2%) | t = 0.31 | .765 |
| MMSE | 15.01 (4.80) | r = −.28 | <.01 |
| B-ADLs | 8.85 (1.28) | r = .31 | <.01 |
| NPI | 22.60 (13.91) | r = .14 | |
| GDS | |||
| 4 | 22 (27.5%) | F = 3.294 | <.001 |
| 5 | 34 (42.5%) | ||
| 6 | 24 (30%) |
Abbreviations: B-ADLs, Bayer’s Activities Daily Living; BDI, Beck Depression Inventory; CBI, Caregiver Burden Interview; GDS, Global Deterioration Scale; MMSE, Mini-Mental State Examination; NPI, Neuropsychiatric Inventory; SD, standard deviation; STAI-S, State-Trait Anxiety Inventory–State.
In bivariate analyses, mean CSI disengagement subscale scores (r = .58, P < .0001) and mean CSI engagement subscale scores (r = −.59, P < .0001) were significantly associated with NPI composite scores. In addition, other caregiver factors significantly associated with NPS on bivariate analysis were lower age, female gender, lower education, more hours spent caring, relationship with patient, living with patient, higher burden score, and higher BDI score. On the other hand, patient characteristics significantly associated with NPSs on bivariate analysis were female gender, longer duration of dementia, previous psychiatric disorders, lower MMSE score, higher B-ADL score, and higher GDS stage.
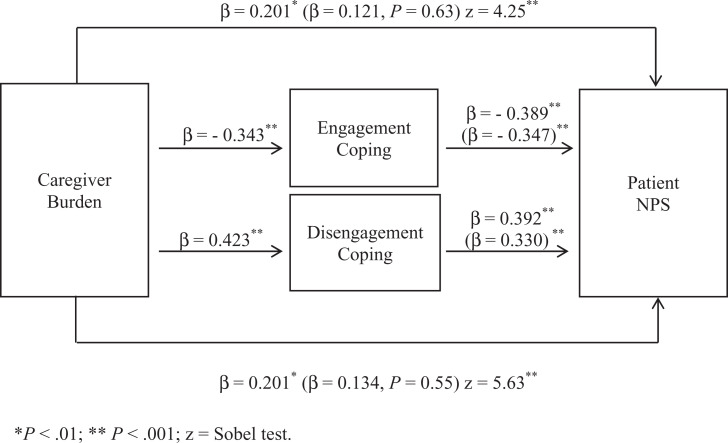
Results of our first linear regression between CB and NPSs as dependent variable indicated that CB was positively associated with NPI composite scores (β = .201, P < .01). Next, the relationship between CB and coping strategies as dependent variable was significant (β = −.343, P < .001 for use of engagement coping and β = .423, P < .001 for use of disengagement coping). Third, coping strategies were positively associated with NPI composite scores as dependent variable (β = −.389, P < .001 for use of engagement coping and β = .392, P < .001 for use of disengagement coping). In our final multiple linear regression, which included both CB and coping strategies scores, standardized β for CB was reduced by adding engagement on step 1 (β = .121, P = .63; effect size attributable to engagement 0.32) and disengagement coping scores on step 2 (β = .134, P = .55; effect size attributable to disengagement 0.34). Engagement (Sobel z-value = 4.25, P < .001) and disengagement coping strategies (Sobel z-value = 5.63, P < .001) significantly mediated the relationship between CB and NPSs. Using more disengagement (β = .330, P < .001) and less engagement coping (β = −.347, P < .001) were predictors for NPI composite scores (Figure 1).
Figure 1.
Mediational model for the association between caregiver burden (CB) and neuropsychiatric symptoms (NPSs) of patients, as mediated by caregiver coping strategies. Standardized β coefficient values outside parentheses are zero-order β. Values inside parentheses are partial regression coefficients from equations that include both CB and coping strategies as predictors of NPSs of patients.
Discussion
To our knowledge, this is the first study to investigate the relationship between caregiver engagement and disengagement coping strategies and NPSs in patients with AD in an epidemiological population.
We found evidence to support our hypothesis that caregivers who were more burdened would report higher frequency and severity of NPSs and that this relationship would be partially mediated by the use of caregiver coping strategies. Our findings suggest that those who report a higher NPI composite score were more likely to use disengagement coping strategies and that it is these strategies, rather than the burden experienced per se, that explain their greater vulnerability to NPSs. Caregivers who used more engagement coping strategies reported lower rates of NPI composite score. Moreover, our results indicate that disengagement coping strategies are associated with NPSs, irrespective of demographic and clinical characteristics of both patient and caregiver, suggesting that caregiver coping is the most important caregiver predictor of NPSs.
An interpretation of these results would be related to the fact that the use of disengagement coping strategies may revolve around a belief that NPSs are unchangeable. This might lead caregivers to believe they do not have the ability to address or emotionally process problems through direct cognitive or behavioral action. Thus, the use of disengagement coping strategies could make managing NPSs more stressful, with caregivers finding it more difficult to face the problems associated with NPSs head on. On the contrary, caregivers who use engagement coping probably have less difficulty in selecting strategies to control, solve, or minimize the consequences resulting from the presence of NPSs. Thus, they try to control the efforts that arise from managing NPSs as a form of adaptation strategy. On the other hand, we have previously shown that CB is associated with caregiver anxiety and depression and that this relationship is mediated by the use of coping strategies. 38,39 Our findings showed that caregivers who were more burdened reported higher anxiety and depression, and this relationship was partially mediated by the use of disengagement coping strategies. This could contribute toward explaining the results of the current study, as higher anxiety or depression levels may influence how caregivers perceive, think, behave, and interpret NPSs. Moreover, this situation may provoke stress-induced interaction with patients eliciting or exacerbating NPSs.
Some clinical implications are derived from this study. Perhaps, the most important implication is that identifying disengagement coping as a mediator of the relationship between CB and NPSs provides a clearly definable and specific target for clinical interventions. Thus, future interventions to reduce NPSs should focus on these coping strategies used by the caregivers themselves. Our results indicate that future studies on interventions to reduce CB that place more emphasis on reducing disengagement coping are needed. In this sense, some research 40,41 has shown that psychoeducational interventions might be useful for caregivers as these can increase their sense of competence and provide effective coping strategies to deal with caregiving. Results from these studies have shown success in reducing overall caregiver psychological morbidity that could be attributable to the modification of coping strategies, suggesting the importance of structuring specific interventions for caregivers, targeting coping strategies. Interventions that teach caregivers cognitive and behavioral skills to actively address or cognitively reframe problems may function by replacing disengagement coping strategies with more adaptative engagement coping strategies. 42 On the other hand, in our study, the patients of caregivers who used more engagement coping strategies showed less NPSs, suggesting a protective effect provided by these strategies. Therefore, future research might explore whether an increase in engagement coping mediates successful outcomes in interventions that favor positive reappraisal by caregivers to provide more positive feedback to the care recipient.
These results also raise an important issue, in that lowering NPS levels can help delay institutionalization of people with AD. Indeed, it is well known that older people in need of care such as patients with AD prefer to be cared for in their own homes. 43 Delaying institutionalization is the contemporary premise of health care policies around the world. 44 However, caregivers must be supported if they are to continue to provide such care without becoming ill themselves. Therefore, the implementation of programs aimed at reducing the levels of BPS may have economic as well as humanitarian benefits. 45
First, this was a cross-sectional design and the direction of causality cannot be determined and would be strengthened by a longitudinal study. This analysis was intended to be hypothesis generating, and it is hoped that it will stimulate larger studies with longitudinal designs might explore the temporal relationships between the constructs of CB, coping strategies, and NPSs. Second, caregivers were asked about coping strategies using a general measure of coping and not about specific situations. Also, almost all measures in this study were self-reported. The extent to which participants’ answers on coping strategy measures relate to actual behavior is debatable 46 ; anxious and depressive caregivers may be more likely to report their coping strategies negatively. However, research has shown that self-reported data collected by researchers is generally truthful, reliable, and valid in this kind of population, provided that confidentiality is ensured using anonymous reports. 47 Third, our study examined the relationship between caregiver coping and NPSs using an overall measure of NPSs. Future research may explore caregiver coping strategies and their relationship to specific NPSs. Finally, we focused on the burden produced by patients’ care, and while the relationship between burden and health problems among caregivers was not investigated, we considered caregivers affected by preexisting chronic diseases as a confounding factor, excluding them from the study as it is well known that caregivers affected by chronic diseases have higher levels of distress with the disorder being functionally impairing per se. 48
In conclusion, most patients reported high frequency and severity of NPSs, and this was partially mediated by disengagement coping strategies. These results may be useful with a view to designing treatment interventions that aim to modify use of caregiver coping strategies, thereby reducing the frequency and severity of NPSs. Our results indicate that intervention to reduce CB, which places more emphasis on engagement coping strategies, and on reducing disengagement coping strategies, associated with more NPSs, are needed.
Further longitudinal studies should be designed to identify specific NPSs related to coping in the different stages of the disease, seeking to establish which coping strategies are more effective and in which phases. Such studies may help us better meet the needs of caregivers dealing with a progressive disease. Future research might explore whether reducing disengagement coping while concurrently increasing engagement coping responses would result in decreased NPSs among patients.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Craig D, Mirakhur A, Hart DJ, McIlroy SP, Passmore AP. A cross sectional study of neuropsychiatric symptoms in 435 patients with Alzheimer’s disease. Am J Geriatr Psychiatry. 2005;13(6):460–468. [DOI] [PubMed] [Google Scholar]
- 2. García-Alberca JM, Lara JP, Berthier ML, et al. Can impairment in memory, language and executive functions predict neuropsychiatric symptoms in Alzheimer’s disease (AD)? Findings from a cross-sectional study. Arch Gerontol Geriatr. 2011; 52(3):264–269. [DOI] [PubMed] [Google Scholar]
- 3. Rocca P, Leotta D, Liffredo C, et al. Neuropsychiatric symptoms underlying caregiver stress and insight in Alzheimer’s disease. Dement Geriatr Cogn Disord. 2010;30(1):57–63. [DOI] [PubMed] [Google Scholar]
- 4. Miyamoto Y, Tachimori H, Ito H. Formal caregiver burden in dementia: impact of behavioral and psychological symptoms of dementia and activities of daily living. Geriatr Nurs. 2010;31(4):246–253. [DOI] [PubMed] [Google Scholar]
- 5. Murman DL, Chen Q, Powell MC, Kuo SB, Bradley CJ, Colenda CC. The incremental direct costs associated with behavioral symptoms in A, D. Neurology. 2002;59(11):1721–1729. [DOI] [PubMed] [Google Scholar]
- 6. Phillips VL, Diwan S. The incremental effect of dementia-related problem behaviors on the time to nursing home placement in poor, frail, demented older people. J Am Geriatr Soc. 2003;51(2):188–193. [DOI] [PubMed] [Google Scholar]
- 7. Tatsumi H, Nakaaki S, Torii K, et al. Neuropsychiatric symptoms predict change in quality of life of Alzheimer disease patients: a two-year follow-up study. Psychiatry Clin Neurosci. 2009;63(3):374–384. [DOI] [PubMed] [Google Scholar]
- 8. Karttunen K, Karppi P, Hiltunen A, et al. Neuropsychiatric symptoms and quality of life in patients with very mild and mild Alzheimer’s disease. Int J Geriatr Psychiatry. 2011;26(5):473–482. [DOI] [PubMed] [Google Scholar]
- 9. Gauthier S, Cummings J L, Ballard C, et al. Management of behavioral problems in Alzheimer’s disease. Int Psychogeriatr. 2010;22(3):346–372. [DOI] [PubMed] [Google Scholar]
- 10. Lövheim H, Sandman P O, Karlsson S, Gustafson Y. Sex differences in the prevalence of behavioral and psychological symptoms of dementia. Int Psychogeriatr. 2009;21(3):469–475. [DOI] [PubMed] [Google Scholar]
- 11. Chan DC, Kasper JD, Black BS, Rabins PV. Prevalence and correlates of behavioral and psychiatric symptoms in community-dwelling elders with dementia or mild cognitive impairment: the memory and medical care study. Int J Geriatr Psychiatry. 2003;18(2):174–182. [DOI] [PubMed] [Google Scholar]
- 12. Sink KM, Covinsky KE, Barnes D, Newcomer RJ, Yaffe K. Caregiver characteristics are associated with neuropsychiatric symptoms of dementia. J Am Geriatr Soc. 2006;54(5):796–803. [DOI] [PubMed] [Google Scholar]
- 13. Vitaliano PP, Young HM, Russo J, Romano J, Magana Amato A. Does expressed emotion in spouses predict subsequent problems among care recipients with Alzheimer’s disease? J Gerontol. 1993;48(4):202–209. [DOI] [PubMed] [Google Scholar]
- 14. Lazarus RS, Folkman S. Stress, Appraisal and Coping. New York, NY: Springer; 1984. [Google Scholar]
- 15. Lazarus RS. (1999). Stress and Emotion: A New Synthesis. New York, NY: Springer; 1984. [Google Scholar]
- 16. Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annu Rev Clin Psychol. 2007;3:377–401. [DOI] [PubMed] [Google Scholar]
- 17. Tobin DL, Holroyd KA, Reynolds RV, Wigal JK. The hierarchical factor structure of the coping strategies inventory. Cogn Ther Res. 1989;13(4):343–361. [Google Scholar]
- 18. Jones F, Bright J. Stress: Myth, Theory and Research. Edinburgh Gate: Prentice Hall; 2001. [Google Scholar]
- 19. Domenech JM. Estadísticos en Ciencias de la Salud. Barcelona: Signo; 1999. [Google Scholar]
- 20. McKhann G, Drachman D, Folstein M. Clinical diagnosis of Alzheimer’s disease: report of the NINADS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology. 1984;34(7):939–944. [DOI] [PubMed] [Google Scholar]
- 21. Folstein MF, Folstein SE, McHugh PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 22. Blesa R, Pujol M, Aguilar M, et al. Clinical validity of the “mini-mental state” for Spanish Speaking communities. Neuropsychologia. 2001;39(11):1150–1157. [DOI] [PubMed] [Google Scholar]
- 23. Hindmarch I, Lehfeld H, De Jong P. The bayer activities of daily living scale (B-ADL). Dement Geriatr Cog Disord. 1998;9(suppl 2):20–26. [DOI] [PubMed] [Google Scholar]
- 24. Erzigkeit H, Lehfeld H, Peña-Casanova J. The bayer-activities of daily living scale (B-ADL): results from a validation study in three European countries. Dement Geriatr Cogn Disord. 2001;12(5):348–358. [DOI] [PubMed] [Google Scholar]
- 25. Reisberg B, Ferris SH, De Leon MD, Crook T. The global deterioration scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136–1139. [DOI] [PubMed] [Google Scholar]
- 26. Cummings JL, Mega M, Gray K, Rosenberg Thompson S, Carusi DA, Gornbein J. The neuropsychiatric inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44(12):2308–2314. [DOI] [PubMed] [Google Scholar]
- 27. Vilalta-Franch J, Lozano-Gallego M, Hernández-Ferrándiz M, et al. Neuropsychiatric inventory. The psychometric properties of its adaptation to Spanish. Rev Neurol. 1999;29(1):15–19. [PubMed] [Google Scholar]
- 28. Zarit SH, Reever KE, Bach Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20(6):649–655. [DOI] [PubMed] [Google Scholar]
- 29. Martín Carrasco M, Salvadó I, Nadal Álava S, et al. Spanish version of the Zarit caregiver burden interview. Rev Gerontol. 1996;6:338–345. [Google Scholar]
- 30. Beck AT, Steer RA, Garbin M G. Psychometrics properties of the Beck’s depression inventory. twentyfive years of evaluation. Clin Psychol Rev. 1998;8(1):77–100. [Google Scholar]
- 31. Conde C, Useros E. Spanish version of the beck depression inventory. Rev Psiquiatr Psicol Med Eur Am Lat. 1975;12:217–236. [Google Scholar]
- 32. Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologist Press; 1970. [Google Scholar]
- 33. Seisdedos N. Spanish adaptation of the state trait anxiety inventory (STAI). Madrid: Tea Ediciones; 1982. [Google Scholar]
- 34. Cano García FJ, Rodríguez Franco L, García Martínez J. Spanish version of the coping strategies inventory. Act Esp Psiquiatr. 2007;35(1):29–39. [PubMed] [Google Scholar]
- 35. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. [DOI] [PubMed] [Google Scholar]
- 36. Sobel ME. Asymptotic confidence intervals for indirect effects in structural equations models. In: Leinhart S. (Ed), Sociological Methodology. San Francisco, CA: Jossey-Bass, 1982. [Google Scholar]
- 37. Soper D. The Free Statistics Calculators Website. Online software; 2008. [Google Scholar]
- 38. García-Alberca JM, Cruz B, Lara JP, Garrido V, Lara A, Gris E. Anxiety and depression are associated with coping strategies in caregivers of Alzheimer’s disease patients: results from the MÁLAGA-AD study. Int Psychogeriatr. 2012;24(8):1325–1334. [DOI] [PubMed] [Google Scholar]
- 39. García-Alberca JM, Cruz B, Lara JP, et al. Disengagement coping partially mediates the relationship between caregiver burden and anxiety and depression in caregivers of people with Alzheimer’s disease Results from the MÁLAGA-AD study. J Affect Disord. 2012;136(3):848–856. [DOI] [PubMed] [Google Scholar]
- 40. Gallagher-Thompson D, Coon DW, Solano N, Ambler C, Rabinowitz Y, Thompson LW. Change in indices of distress among Latino and Anglo female caregivers of elderly relatives with dementia: site specific results from the REARCH national collaborative study. Gerontologist. 2003;43(4):580–591. [DOI] [PubMed] [Google Scholar]
- 41. Marriott A, Donaldson C, Tarrier N, Burns A. Effectiveness of cognitive-behavioural family intervention in reducing the burden of care in carers of patients with Alzheimer’s disease. Br J Psychiatry. 2000;176:557–562. [DOI] [PubMed] [Google Scholar]
- 42. Gelmini G, Morabito B, Braidi G. Educational and formative training reduce stress in the caregivers of demented patients. Arch Gerontol Geriatr. 2009;49(suppl 1):119–124. [DOI] [PubMed] [Google Scholar]
- 43. Luppa M, Luck T, Weyerer S, König HH, Brähler E, Riedel-Heller SG. Prediction of institutionalization in the elderly. a systematic review. Age Ageing. 2010;39(1):31–38. [DOI] [PubMed] [Google Scholar]
- 44. Andrén S, Elmstahl S. Effective psychosocial intervention for family caregivers lengthens time elapsed before nursing home placement of individuals with dementia: a five-year follow-up study. Int Psychogeriatr. 2008;20(6):1177–1192. [DOI] [PubMed] [Google Scholar]
- 45. García-Alberca JM, Cruz B, Lara JP, et al. The experience of caregiving: the influence of coping strategies on behavioral and psychological symptoms in patients with Alzheimer’s disease. Aging Ment Health. 2013;17(5):615–622. [DOI] [PubMed] [Google Scholar]
- 46. Kneebone, Martin PR. Coping and caregivers of people with dementia. Br J Health Psychol. 2003;8(pt 1):1–17. [DOI] [PubMed] [Google Scholar]
- 47. Chou P. CH, Chao YM, Yang HJ, Yeh GL, Lee TS. Relationships between stress, coping and depressive symptoms among overseas university preparatory Chinese students: a cross-sectional study. BMC Public Health. 2011;11:352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Di Mattei VE, Prunas A, Novella L, Marcone A, Cappa SF, Sarno L. The burden of distress in caregivers of elderly demented patients and its relationship with coping strategies. Neurol Sci. 2008;29(6):383–389. [DOI] [PubMed] [Google Scholar]