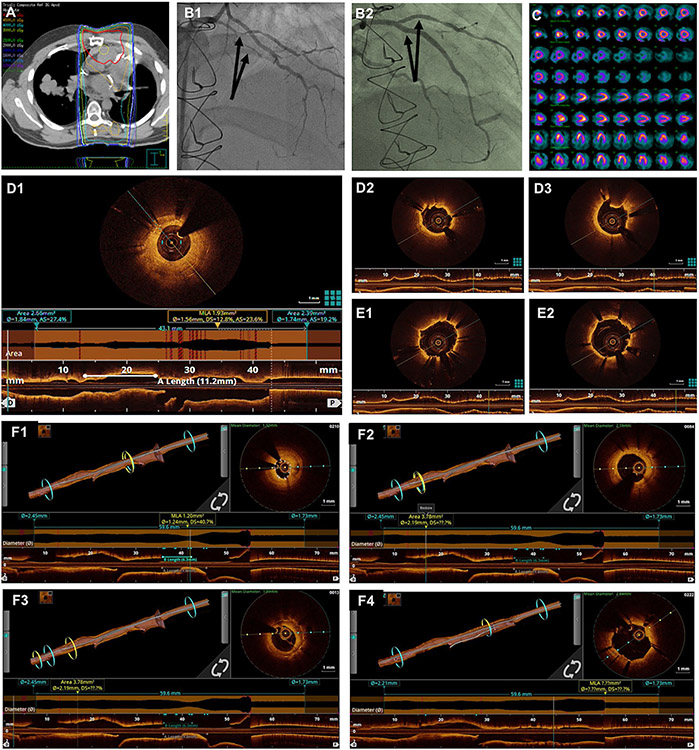
A 36-year-old male with thymic carcinoma, status post chemoradiation, presented with symptomatic systolic dysfunction (ejection fraction of 35% on transthoracic echocardiogram). He received a total dose of 50 Gy 7 years prior (Fig. 1a) and subsequent 20 Gy of palliative radiotherapy to the lower thoracic spine due to painful bone lesions. Coronary angiography revealed severe disease of the left anterior descending (LAD) artery and first diagonal, for which angioplasty with drug eluting stent (DES) was performed (Fig. 1b1, b2). Six months later, the patient returned with exertional dyspnea. Stress myocardial perfusion scan showed perfusion defects in the left circumflex (LCx) artery territory (Fig. 1c). Coronary angiography and optical coherence tomography (OCT) demonstrated severe LCx disease and in-stent restenosis of the mid-LAD. Subsequent balloon angioplasty and DES placement were performed (Fig. 1d1-d3, e1, e2). One year later, OCT revealed a new fibrofatty ostial LAD lesion and in-stent restenosis requiring angioplasty with DES implantation (Fig. 1f1-f4).
Fig. 1.
Coronary lesions in a patient with chest radiotherapy for thymic carcinoma. Dose distribution from radiation treatment plan (a). Coronary angiography revealed total mid-segment occlusion of the left anterior descending (LAD) artery and severe disease in the proximal and mid-distal first diagonal (b1, arrows). Angioplasty with drug-eluting stent (DES) in the bifurcation of the LAD and first diagonal artery was performed (b2, arrows). Stress myocardial perfusion scan 6 months later showed mild reversible defects at the basal anterolateral and mid-inferolateral left ventricular segments (c). OCT demonstrated severe in-stent restenosis of the LAD (d1). Balloon angioplasty was needed for adequate vessel preparation and plaque disruption (d2, d3), followed by DES placement; well apposed and expanded stents with appropriate coverage were observed (e1, e2). OCT with 3-Dimensional reconstruction 1 year later showed: a new fibrofatty ostial LAD lesion (f1), predominantly fibrous LAD in-stent restenosis (f2), fibrofatty in-stent restenosis (f3). Post-angioplasty OCT demonstrated material protruding through the stent struts, presumably aggressive neoatherosclerosis or intimal hyperplasia (f4)
Radiation-induced coronary artery disease (RI-CAD) appears to be more resistant to treatment than “classic” CAD and is associated with worse outcomes [1]. Surprisingly, RI-CAD presents not only with fibrous characteristics, but also with lipid and calcified components, similar to atherosclerosis [2]. A likely interaction between radiation dose, predisposition to disease, and cardiovascular risk factors results in a full spectrum of lesions. OCT can identify different lesion morphologies and guide treatment. In calcified lesions, initial atherectomy to improve stent expansion may be indicated. Fibrous lesions burden stent expansion, increasing the risk for in-stent restenosis. Fatty tissue protrudes through stent struts; in these cases, balloon angioplasty might suffice. We suggest that OCT is an important component of personalized cardio-oncology management.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Cheng YJ, Nie XY, Ji CC, Lin XX, Liu LJ, Chen XM, Yao H, Wu SH (2017) Long-term cardiovascular risk after radiotherapy in women with breast cancer. J Am Heart Assoc 6(5):e005633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caro-Codon J, Jimenez-Valero S, Galeote G, Sanchez-Recalde A, Moreno R (2016) Radiation-induced coronary artery disease: useful insights from OCT. Int J Cardiol 202:535–536 [DOI] [PubMed] [Google Scholar]