Key Clinical Message
Type V gastric ulcer is an unusual etiology of gastrosplenic fistula (GSF). Prompt diagnosis and early embolization of splenic vessels prior to esophagogastroduodenoscopy and surgical resection is crucial.
Keywords: embolization, endoscopy, gastric ulcers, gastrointestinal bleeding, gastrosplenic fistula, NSAIDs
1. INTRODUCTION
Gastrosplenic fistula (GSF) is a rare entity characterized by an abnormal communication between the gastric cavity and the spleen. Reported etiologies of GSF are splenic or gastric malignancies, splenic abscess, crohn's disease, peptic ulcers disease, sickle cell disease, sleeve gastrectomy, and abdominal trauma. 1 , 2 Diffuse large B‐cell lymphoma (DLBCL) is the most common malignancy resulting in GSF. 1 , 2 Predominant symptoms at clinical presentation are abdominal pain, hematemesis, melena, and constitutional symptoms such as generalized weakness, fever, and weight loss. Imaging findings of air bubbles and leakage of oral contrast from gastric cavity into the spleen is diagnostic of GSF. 3 Prognosis and short‐term survival in patients with GSF are good (up to 82%) in patients presented without gastrointestinal bleeding (GIB). 4 Some patients with GSF may present with life‐threatening GIB. We present a case of GSF secondary to type V gastric ulcer associated with upper GIB.
2. CASE HISTORY
A 41‐year‐old man with a history of oculodentodigital dysplasia, spastic paraplegia, and sacral decubitus ulcers with diverting sigmoid colostomy, chronic back pain presented with malaise and melena through colostomy. His home medications include intrathecal baclofen pump 300 mcg daily, gabapentin 800 mg four times daily, topiramate 25 mg daily, metoprolol succinate 25 mg daily, trazadone 50 mg daily, and oxybutynin 5 mg daily. He admitted intermittent use of NSAIDs for chronic back pain. On arrival to ER, he was tachycardic (113/min), with a BP of 126/82 mmHg and pale appearing. His Hgb was 4.9 g/dL (baseline Hgb 12.1 g/dL).
3. METHODS
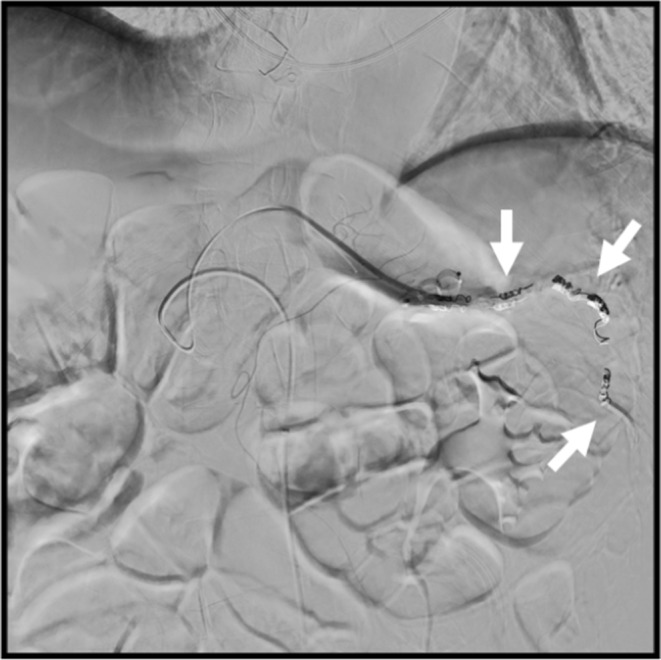
CT angiogram of the abdomen/pelvis was negative for active contrast extravasation, however, revealed direct contiguity between the gastric fundus and spleen indicating GSF (Figure 1). The patient was resuscitated with IV fluid and required multiple blood transfusions. Splenic artery (SA) angiogram showed hyperemia along the posterior wall of the stomach corresponding to CT findings of GSF (Figure 2). Embolization of the main SA, right gastroepiploic, and left omental artery was performed (Figure 3). An esophagogastroduodenoscopy (EGD) showed a benign inflammatory mass in the gastric fundus with the invasion of splenic tissue into the gastric mucosa (Figure 4). A gastric biopsy was negative for H. pylori and malignancy, however, revealed mild chronic inflammation and reactive gastropathy. Patient was managed with partial gastrectomy and splenectomy. Operative findings were consistent with a large type V gastric ulcer at the fundus with direct extension into the spleen (gastro‐splenic fistula) and a necrotic spleen. Pathology of operative specimen demonstrated transmural granulation tissue and acute inflammation with acute serositis and mucosal ulceration without evidence of ischemia.
FIGURE 1.
CT angiogram shows wedge‐shaped defect between gastric fundus and spleen indicating gastrosplenic fistula (arrow).
FIGURE 2.
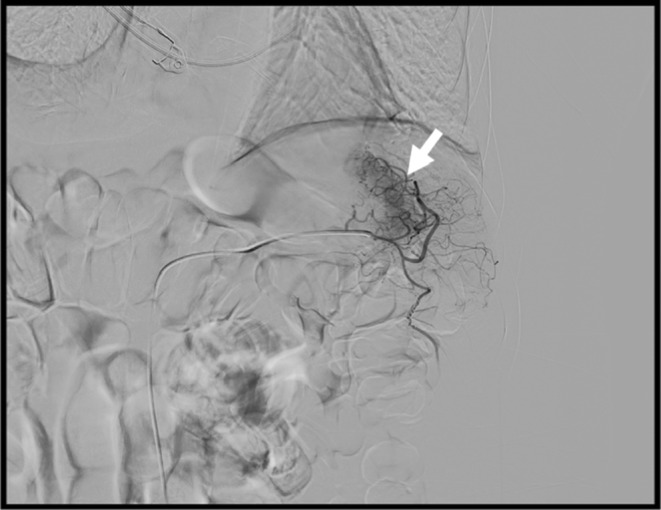
Catheter angiography of the splenic artery shows extravasation of blood along the posterior wall of the stomach corresponding to the site of gastric ulceration on the CT scan.
FIGURE 3.

Splenic artery angiogram after Gelfoam slurry, coil, and Amplatzer embolization. There is no contrast extravasation after embolization.
FIGURE 4.
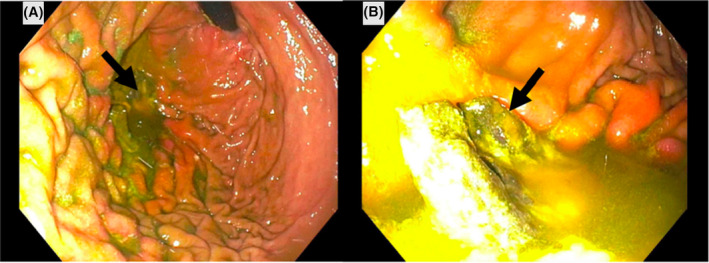
Esophagogastroduodenoscopy shows a large benign gastric ulcerated mass in the gastric fundus, consistent with splenic tissue invading through gastric wall ulcer.
4. CONCLUSION AND RESULTS
The peritoneal fluid culture grew Enterococcus fecalis. Post‐operatively, the patient was managed with broad spectrum antibiotics vancomycin and meropenem along with micafungin. The post‐operative course was complicated by wound dehiscence and the patient underwent debridement and closure of abdominal wall. He was discharged to rehab after a prolonged hospital course.
5. DISCUSSION
Gastrosplenic fistula due to type V gastric ulcer complicated by massive GIB is rare. There are five types of benign gastric ulcers including true gastric ulcers at incisura angularis (type I), combined gastric and duodenal ulcers (type II), Pyloric and pre‐pyloric ulcers (type III), ulcers high along lesser curvature within 1–2 cm of gastroesophageal junction (type IV), and gastric ulcers anywhere secondary to medications (type V). 5 The incidence of type V ulcers is <5%. The proposed pathogenic mechanism of GSF is progressive infiltrative, erosive, and penetrating lesions of spleen and/or adjacent gastric wall. A subset of patients with GSF, present with GIB due to necrosis of underlying blood vessel in splenic parenchyma, gastric wall and gastrosplenic ligament that contain short gastric, and left gastroepiploic vessels. 6
In our case, the patient had significant drop in hemoglobin from his baseline and evidence of GSF on cross‐sectional radiologic images that was the source of GIB. Abdominal CT was negative for splenic abscess, ischemia, lymphadenopathy, or mass concerning for malignancy. Although patient was hemodynamically stable on admission and there was no active bleeding on CT scan, an embolization of the main splenic artery, right gastroepiploic, and left omental artery was performed by interventional radiology prior to EGD to prevent procedural‐related risks of iatrogenic bleeding as biopsy of gastric ulcer was essential to rule out malignancy and other etiologies of GSF. 7 Gastric biopsies were negative for H‐pylori, malignancy, however, demonstrated non‐specific findings of mild chronic inflammation and reactive gastropathy that may be seen in patients with GSF and its sequalae. Operative findings and pathology of operative specimen demonstrated transmural granulation tissue and acute inflammation with acute serositis and mucosal ulceration consistent with type V gastric ulcer. The risk factor of type V gastric ulcer in our patient was chronic NSAID's use intermittently for back pain, which may results in fistulation due to chronic inflammation involving transmural gastric wall ulceration.
Prior to definitive surgical management of GSF, an EGD evaluation of other causes of upper GIB is crucial to establish etiology by obtaining tissue diagnosis. Surgical resection of GSF is curative treatment. The choice of surgical resection depends on patient's hemodynamic stability, extension of underlying disease, and surgeons' preferences. Laparoscopic partial gastrectomy with or without splenectomy is common method of surgical resection with favorable outcomes. 1 , 2 , 8 Non‐surgical management of GSF with chemotherapy has also been reported effective in several cases of DLBCL. 8 , 9 , 10
AUTHOR CONTRIBUTIONS
Muhammad Nadeem Yousaf: Conceptualization; data curation; validation; writing – original draft; writing – review and editing. Riyasha Dahal: Data curation; validation; writing – review and editing. Subeena Phull: Data curation; validation; writing – original draft; writing – review and editing. Vinayak Aryal: Data curation; writing – original draft; writing – review and editing. Karun Neupane: Data curation; writing – review and editing. Hamza Ertugrul: Data curation; writing – review and editing. Ebubekir Daglilar: Conceptualization; supervision; writing – review and editing.
FUNDING INFORMATION
The authors declare that there is no financial support and competing conflict of interests in this study.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no competing interests.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
PRIOR PRESENTATIONS
Poster of this case was presented at the ACG annual meeting 2022 held at Charlotte NC in October 2022.
INFORMED CONSENT
Informed consent was obtained from the patient for the publication of this case.
ACKNOWLEDGMENTS
There is no acknowledgment.
Yousaf MN, Dahal R, Phull S, et al. Type V gastric ulcer: An unusual etiology of gastrosplenic fistula associated with upper gastrointestinal bleeding. Clin Case Rep. 2024;12:e8518. doi: 10.1002/ccr3.8518
DATA AVAILABILITY STATEMENT
All the relevant data have been included in the manuscript.
REFERENCES
- 1. Borgharia S, Juneja P, Hazrah P, Lal R, Kapur N, Chaudhary P. Gastrosplenic fistula: a systematic review. Indian J Surg Oncol. 2022;13(3):652‐660. doi: 10.1007/s13193-022-01551-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kang DH, Huh J, Lee JH, Jeong YK, Cha HJ. Gastrosplenic fistula occurring in lymphoma patients: systematic review with a new case of extranodal NK/T‐cell lymphoma. World J Gastroenterol. 2017;23(35):6491‐6499. doi: 10.3748/wjg.v23.i35.6491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ali HA, Scherer PM. Gastrosplenic fistula secondary to simultaneous gastric and splenic diffuse large B cell lymphoma. J Nucl Med Technol. 2023;51:160‐161. doi: 10.2967/jnmt.122.264789 [DOI] [PubMed] [Google Scholar]
- 4. Frenkel A, Bichovsky Y, Perry ZH, et al. Management of gastrosplenic fistula in the emergency setting‐a case report and review of the literature. Ann Med Surg (Lond). 2018;29:26‐29. doi: 10.1016/j.amsu.2018.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chernyshev VN, Aleksandrov IK. Classification of stomach ulcers and choice of the surgery method. Khirurgiia (Mosk). 1992;9(10):3‐8. [PubMed] [Google Scholar]
- 6. Jain V, Pauli E, Sharzehi K, Moyer M. Spontaneous gastrosplenic fistula secondary to diffuse large B‐cell lymphoma. Gastrointest Endosc. 2011;73(3):608‐609. doi: 10.1016/j.gie.2010.09.015 [DOI] [PubMed] [Google Scholar]
- 7. Bird MA, Amjadi D, Behrns KE. Primary splenic lymphoma complicated by hematemesis and gastric erosion. South Med J. 2002;95(8):941‐942. [PubMed] [Google Scholar]
- 8. Wang TP, Doss M, Tokar JL, Reddy S, Barta SK, Yu JQ. Lymphoma causing gastrosplenic fistula revealed by FDG PET/CT. Clin Nucl Med. 2017;42(11):890‐892. doi: 10.1097/rlu.0000000000001801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saito M, Miyashita K, Miura Y, et al. Successful treatment of gastrosplenic fistula arising from diffuse large B‐cell lymphoma with chemotherapy: two case reports. Case Rep Oncol. 2019;12(2):376‐383. doi: 10.1159/000500505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Khan F, Vessal S, McKimm E, D'Souza R. Spontaneous gastrosplenic fistula secondary to primary splenic lymphoma. BMJ Case Rep. 2010;2010:bcr0420102932. doi: 10.1136/bcr.04.2010.2932 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the relevant data have been included in the manuscript.


