Abstract
Introduction
In this study, we aim to estimate the natural standing sagittal alignment in patients with adult spinal deformity (ASD), firstly by investigating the normative values of anatomical pelvic parameters based on the anterior pelvic plane (APP) in a healthy population, and to clarify the relationships between the anatomical and positional pelvic parameters in standing position.
Methods
The images of biplanar slot-scanning full-body stereoradiography in 140 healthy Japanese volunteers (mean age, 39.5 years; 59.3% female) were examined. In addition to three-dimensional measurements including pelvic incidence (PI), sacral slope (SS), and pelvic tilt (PT), the APP angle (APPA; anterior tilting=positive) was measured as the angle between the APP and the vertical line using the two-dimensional lateral image. Anatomical SS and PT (aSS and aPT) were calculated as the angles of SS and PT in reference to APP.
Results
The mean (range) values of APPA, aSS, and aPT were determined to be 0.7° (−16.8°/15.5°), 36.8° (18.3°/64.9°), and 13.2° (−0.6°/28.7°), respectively. Moreover, SS was found to be significantly correlated with PI and aSS, while PT was significantly correlated with PI, aSS, aPT, and body weight. Also, PT was significantly larger in females than in males. Multiple linear regression analysis deduced the following equations: SS=0.404×aSS+0.203×PI+12.463, PT=−0.391×aSS+0.774×PI+1.950×sex (male=0, female=1)−12.971, wherein aSS had the greatest effect for predicting SS among the included factors and PI had the greatest effect for predicting PT. In addition, no significant differences were noted between PT/PI and aPT/PI.
Conclusions
As per the results of this study, significant correlations were noted among parameters and predicting models for positional parameters (SS and PT) using anatomical parameters (aSS and aPT) in a healthy population. This novel measurement concept based on the APP has been considered to be useful in estimating natural SS and PT in standing position using the anatomical pelvic parameters in patients with ASD.
Keywords: sacral slope, pelvic tilt, pelvic incidence, anterior pelvic plane, anatomical parameter, standing sagittal alignment
Introduction
Standing upright with a horizontal gaze can be achieved with a chain of balance beginning at the feet; extending to the lower limbs, pelvis, and spinal segments; and ending at the cranium1,2). In a study by Duval-Beaupère et al., the pelvis has been identified as the keystone of standing alignment and balance3,4), and pelvic incidence (PI) has been proposed as a representative parameter of pelvic morphology5) or an anatomical parameter that determines the appropriate lumbar lordosis (LL)4). Degenerative loss of the LL, which is the main driver of the deterioration of standing sagittal alignment in adult spinal deformity (ASD), can result in a spinopelvic mismatch (PI-LL mismatch) and trigger compensatory mechanisms to maintain a standing posture. The primary mechanism of compensation is the posterior tilt of the pelvis, which is represented by changes in positional pelvic parameters, including an increase in pelvic tilt (PT) and a decrease in sacral slope (SS)6-8). Therefore, in surgical planning for ASD, it is deemed necessary to predict patient-specific natural sagittal alignment or estimate the grade of compensation by pelvic retroversion, using anatomical pelvic parameters, which have been assumed to be constant. Moreover, predicting natural SS and PT would help estimate the natural sagittal profile represented by the Roussouly classification9,10), making the surgical goal more appropriate. Although PI has been the most commonly used anatomical parameter for those prediction processes11,12), the PI can change with age13), positioning14,15), and corrective spinal surgery16,17), even in healthy adults7,18,19). Pelvic retroversion generally increases acetabular anteversion and inclination20), decreasing anterior coverage of the femoral head by the acetabulum and leading to hip osteoarthritis21,22). Hip osteoarthritis may have negative impacts on the precise determination of the hip axis and PI measurements because of the degeneration and incongruity of both hip joints (Fig. 1). Therefore, to compensate for these shortcomings of PI, multiple anatomical parameters of the pelvis other than the PI are necessary to predict patient-specific natural sagittal alignment more precisely.
Figure 1.
Standing biplanar slot-scanning full-body stereoradiography images of a 74-year-old female patient with adult spinal deformity.
Anteroposterior images show bilateral severe hip osteoarthritis and mild lumbar scoliosis (A). The lateral images demonstrate the mismatch between pelvic incidence (PI, 80°) and lumbar lordosis (LL, 44°) (PI-LL=36°), which is compensated by pelvic retroversion (pelvic tilt=35°) (B).
Lewinnek et al.23) have described the anterior pelvic plane (APP), defined by the bilateral anterior superior iliac spines and the anterior surface of the pubis symphysis, which is commonly used as a reference for positioning and postoperative evaluation of the acetabular cup in total hip arthroplasty. To analyze the morphological characteristics in patients with dysplasia of the hip, Imai et al. have proposed novel anatomical pelvic parameters, i.e., anatomical SS and PT (aSS and aPT), which are measured as the SS and PT related to the APP24). They are considered promising anatomical parameters that can represent the characteristics of pelvic morphology even in patients with hip pathologies because they do not require a horizontal line, vertical line, and the center of the femoral head for measurements. Hence, in this study, we hypothesized that aSS and aPT can be used to speculate the original standing sagittal spine alignment in patients with ASD and that clarifying the normative values and relationships between anatomical and positional parameters in healthy populations would be useful.
Suzuki et al. measured radiographic parameters, including aSS, in a healthy population. However, because their cohort consisted of Japanese women with a limited age range (mean, 64.3 years; range, 47-84 years)25), there seems to be a paucity of normative data in young and middle-aged adults. Moreover, they used conventional whole-spine radiographs25). In contrast to conventional X-ray devices, two-dimensional (2D) measurements based on biplanar slot-scanning full-body stereoradiography (EOS) images can be performed without vertical distortion or magnification, because the X-ray tube and detector move together longitudinally through the imaging area. Therefore, the EOS system allows for more precise bone reconstruction in orthopedics, especially at the level of the spine, pelvis, and lower limbs26).
In this study, we aimed to reveal the normative values of the APP angle (APPA), aSS, and aPT measured using EOS images, which allow for precise measurements, and to clarify the relationships between the anatomical and positional pelvic parameters in healthy Japanese adults with a wide age range.
Materials and Methods
Study design and subjects
We have retrospectively analyzed prospectively collected data from EOS imaging in healthy volunteers, as has been reported previously27). In brief, healthy adult volunteers aged ≥20 years without a history of treatment for a spinal disease were enrolled in this study and underwent an EOS system (EOS imaging, Paris, France) from the head to the feet. During the EOS examination, participants were asked to stand comfortably with their hands on their cheeks and maintain a horizontal gaze, aided by a mirror placed at eye level on the inner wall of the EOS cabin. Participants were then scanned within 30 s from the skull to the feet at a speed of 7.6 cm/s7). The average dose of radiation was 23.3 mGy・cm2 including the front and side surfaces. Participants with an Oswestry Disability Index of >20%, scoliosis (Cobb angle >20°), abnormal vertebral counts, or transitional vertebrae were excluded. In total, 140 participants (57 males and 83 females) were included in this analysis. This study was approved by the Institutional Review Boards of the authors' affiliated institutions, and all participants provided written informed consent.
Radiographic measurements
Radiographic measurements were performed automatically using commercially available 2D/three-dimensional (3D) sterEOSⓇ modeling software, including PI, PT, and SS. We have previously reported that inter- and intra-observer reproducibilities were very high for 3D measurements of these parameters with the intraclass correlation coefficient (ICC) of ≥0.9526). In addition, the APPA was measured on 2D images using ImageJ software (Fig. 2). The APPA was defined as the angle between the line connecting the midpoint of both the anterior superior iliac spines (ASISs) to the anterior surface of the pubic symphysis, which was the APP, and the vertical line of the 2D lateral image. A positive value indicates the anterior tilt of the APP, whereas a negative value indicates the posterior tilt of the APP. The aSS was defined as the angle between the superior endplate of S1 and the line perpendicular to the APP in the sagittal plane (Fig. 3)24). aPT was defined as the angle between the line connecting the midpoint of the sacral plate to the hip axis and the line parallel to the APP in the sagittal plane (Fig. 3)24). The aSS and aPT represent the pelvis morphology, which does not change with posture, and are fundamentally different from the SS and PT, which are dependent on posture.
Figure 2.

Anterior pelvic plane angle (APPA) measurement using two-dimensional lateral images of EOS imaging. APPA is the angle between the line connecting the midpoint of both anterior superior iliac spines (ASIS) and the pubic symphysis.
Figure 3.

Anatomical sagittal parameters of the pelvis based on the anterior pelvic plane.
The anatomical sacral slope (aSS) is defined as the angle between the sacral plate and the line perpendicular to the anterior pelvic plane (APP). The anatomical pelvic tilt (aPT) is the angle between the line connecting the midpoint of the sacral plate to the hip axis and the line parallel to the APP.
Two observers [the first author (observer A) and another orthopedic surgeon (observer B)] measured the APPA twice at 1-month intervals in order to determine intra- and inter-observer reliabilities. Using the second measurement data of the first author (observer A), anatomical SS (aSS) and PT (aPT) were calculated using the following formulas; aSS=SS−APPA, aPT=PT+APPA. In addition, aPT/PI and PT/PI ratios were calculated as parameters that reflect the amount of compensation by pelvic retroversion in the standing position.
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences software (version 19; IBM Corp., Armonk, NY, USA). Continuous data were expressed as mean±standard deviation or median (interquartile range), as deemed appropriate. The Shapiro-Wilk test was used to evaluate data normality. Nonparametric tests were used when data were not normally distributed. Group differences were evaluated using the unpaired t-test or Mann-Whitney U test. The difference between the PT/PI and aPT/PI ratios was analyzed using the paired t-test. Bivariate associations were evaluated using the Pearson correlation coefficient (r) or Spearman rank correlation coefficient (rs). Additionally, multivariate regression with a forward stepwise procedure was performed to estimate the SS and PT using anatomical pelvic parameters and participant characteristics including age, sex, and anthropometric parameters. Factors with a p-value of <0.10 in the univariate analyses were included in this multivariate analysis. To evaluate variation, we calculated the mean absolute difference (MAD) and variability (standard deviation, SD). Intra- and inter-observer reliabilities were examined using ICCs and two-sided 95% confidence intervals. Statistical significance was set at p-value of <0.05.
Results
Demographic and radiographic parameters are shown in Table 1. All parameters except age, body weight, body mass index, and aSS were normally distributed. The females were noted to have significantly smaller anthropometric parameters and a significantly larger PT as compared to the males (Table 2).
Table 1.
Demographic and Pelvic Alignment Data.
| Mean | SD | Range (min/max) | Median | IQR (25%/75%) | Shapiro-Wilk test | ||
|---|---|---|---|---|---|---|---|
| W (df=140) | P value | ||||||
| Age (years) | 40.2 | 10.9 | 20/76 | 39.5 | 32/47 | 0.978 | 0.021 |
| BH (cm) | 164.1 | 8.7 | 144.6/188.4 | 164.2 | 157.8/170.2 | 0.993 | 0.756 |
| BW (kg) | 60.0 | 12.1 | 41.1/113.6 | 58.4 | 51.1/67.4 | 0.947 | <0.001 |
| BMI (kg/m2) | 22.1 | 3.3 | 17.4/39 | 21.6 | 19.8/24.1 | 0.916 | <0.001 |
| APPA (°) | 0.7 | 6.4 | −16.8/15.5 | 1.4 | −2.9/5.6 | 0.988 | 0.247 |
| PI (°) | 50 | 9.4 | 28.8/74.2 | 49.3 | 43.4/55.6 | 0.989 | 0.306 |
| SS (°) | 37.5 | 7.2 | 17.6/56.4 | 37.9 | 33.3/41.8 | 0.989 | 0.340 |
| PT (°) | 12.5 | 7.4 | −7.7/31.6 | 11.8 | 7.4/17.4 | 0.991 | 0.464 |
| aSS (°) | 36.8 | 8.3 | 18.3/64.9 | 36.4 | 31.7/41.2 | 0.972 | 0.006 |
| aPT (°) | 13.2 | 6.0 | −0.6/28.7 | 12.5 | 9.3/17.3 | 0.985 | 0.145 |
BH, body height; BW, body weight; BMI, body mass index; APPA, anterior pelvic plane angle; PI, pelvis incidence; SS, sacral slope; PT, pelvic tilt; aSS, anatomical sacral slope; aPT, anatomical pelvic tilt; SD, standard deviation; IQR, interquartile range
Table 2.
Differences in Terms of Participant Characteristics and Radiographic Parameters between Males and Females.
| Males (n=57) | Females (n=83) | P value | |
|---|---|---|---|
| Age (years) [median (IQR)] | 38.0 (14.5) | 41.0 (14.0) | 0.509 |
| BH (cm) [mean (SD)] | 151.4 (6.4) | 159.1 (6.2) | <0.001 |
| BW (kg) [median (IQR)] | 68.4 (14.8) | 52.1 (9.6) | <0.001 |
| BMI (kg/m2) [median (IQR)] | 23.2 (3.9) | 20.7 (3.4) | <0.001 |
| APPA (°) [mean (SD)] | 1.9 (5.7) | −0.1 (6.7) | 0.067 |
| PI (°) [mean (SD)] | 48.5 (8.6) | 51.0 (9.8) | 0.114 |
| SS (°) [mean (SD)] | 38.1 (7.1) | 37.1 (7.3) | 0.428 |
| PT (°) [mean (SD)] | 10.4 (6.1) | 14.0 (7.9) | 0.003 |
| aSS (°) [median (IQR)] | 36.1 (11.0) | 36.6 (8.9) | 0.671 |
| aPT (°) [mean (SD)] | 12.3 (5.3) | 13.9 (7.9) | 0.142 |
BH, body height; BW, body weight; BMI, body mass index; APPA, anterior pelvic plane angle; PI, pelvis incidence; SS, sacral slope; PT, pelvic tilt; aSS, anatomical sacral slope; aPT, anatomical pelvic tilt; SD, standard deviation; IQR, interquartile range
Radiographic parameters
The mean APPA was 0.7°±6.4°, indicating that the pelvis was tilted anteriorly by an average of 0.7°. The APPA tended to tilt anteriorly more frequently in males (1.9°±5.7°) than in females (−0.1°±6.7°) (p=0.067).
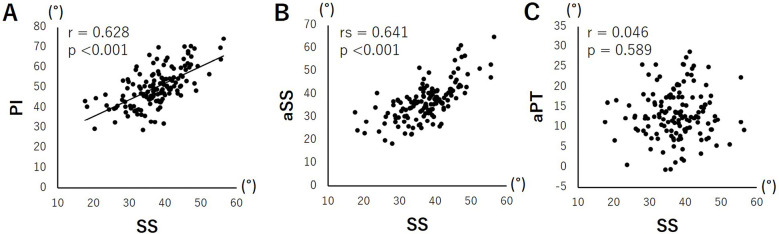
With regard to the correlations among the pelvic parameters (Table 3), SS was moderately and positively correlated with PI (Fig. 4A) and aSS (Fig. 4B), whereas SS was not correlated with aPT (Fig. 4C). In contrast, PT was moderately and positively correlated with PI (Fig. 5A) and aPT (Fig. 5C), while PT was weakly and positively correlated with aSS (Fig. 5B). In the correlation analysis with age and anthropometric parameters, statistically significant, negative correlations were determined between PI and body weight, between PT and body height, and between PT and body weight (Table 3).
Table 3.
Correlation Coefficients among Radiographic Parameters and Age.
| APPA | PI | SS | PT | aSS* | aPT | |
|---|---|---|---|---|---|---|
| PI | −0.305 | |||||
| SS | 0.246 | 0.628 | ||||
| PT | −0.624 | 0.657 | −0.173 | |||
| aSS* | −0.504 | 0.729 | 0.641 | 0.294 | ||
| aPT | 0.286 | 0.486 | 0.046 | 0.571 | −0.155 | |
| age* | −0.112 | 0.050 | 0.065 | 0.010 | 0.151 | −0.064 |
| BH | 0.124 | −0.127 | 0.007 | −0.167 | −0.088 | −0.075 |
| BW* | 0.071 | −0.190 | −0.089 | −0.181 | −0.101 | −0.112 |
| BMI* | 0.010 | −0.153 | −0.080 | −0.137 | −0.037 | −0.122 |
Correlations among parameters, except aSS, were analyzed using Pearson correlation coefficients (r).
*Correlations with aSS, age, BW, and BMI were analyzed using the Spearman rank correlation coefficient (rs).
Correlation coefficients with p<0.05 in underlined.
APPA, anterior pelvic plane angle; PI, pelvis incidence; SS, sacral slope; PT, pelvic tilt; aSS, anatomical sacral slope; aPT, anatomical pelvic tilt; BH, body height; BW, body weight; BMI, body mass index
Figure 4.
Correlations between sacral slope (SS) and anatomical pelvic parameters.
SS was determined to be significantly, positively correlated with PI (A) and aSS (B) but not with aPT (C).
Figure 5.
Correlations between pelvic tilt (PT) and anatomical pelvic parameters.
PT was noted to be significantly, positively correlated with PI (A), aSS (B), and aPT (C).
Multiple linear regression for predicting SS and PT
To estimate SS and PT from anatomical pelvic parameters and participants' characteristics, we performed stepwise multiple linear regression analysis, in which PI and aSS were included for SS and PI, aSS, aPT, sex (male=0, female=1), body height, and body weight were included for PT. These analyses resulted in the following formulas: SS=0.404×aSS+0.203×PI+12.463 (R=0.695, R2=0.483), PT=−0.391×aSS+0.774×PI+1.950×sex (male=0, female=1)−12.971 (R=0.729, R2=0.531). In addition, the standardized partial regression coefficients in the SS equation were 0.468 for aSS and 0.266 for PI, whereas those in the PT equation were −0.440 for aSS, 0.980 for PI, and 0.130 for sex.
Differences and relationship between PT/PI and aPT/PI
To estimate the amount of compensation by the pelvis for each patient, we have evaluated the differences and relationships between the PT/PI and aPT/PI ratios. The mean PT/PI was 0.24±0.13, while the mean aPT/PI was 0.26±0.11. No significant differences were noted between the two ratios, where the mean difference was −0.02±0.13 (95% confidence interval, −0.04 to 0.0002; p=0.053). Moreover, PT/PI was significantly, moderately correlated with aPT/PI (r=0.418, p<0.001; Fig. 6).
Figure 6.

Correlations between aPT/PI and PI/PT ratios.
The aPT/PI ratio is significantly, positively correlated with the PT/PI ratio.
aPT, anatomical pelvic tilt; PT, pelvic tilt; PI, pelvic incidence
Reliability of APPA measurements
The APPA data measured twice by the two observers are summarized in Table 4, in which all sets of data were normally distributed. The intra-observer MAD was <1.3°, while the ICC was >0.95. With regard to inter-observer reliability, which was evaluated using the second measurement data of observers, the MAD and ICC were determined to be 1.3° and 0.962, respectively.
Table 4.
Reliability of the APPA Measurement.
| Observer A | Observer B | |||
|---|---|---|---|---|
| Measurements | 1st | 2nd | 1st | 2nd |
| Mean | 0.6 | 0.7 | −0.2 | 0.1 |
| SD | 6.4 | 6.4 | 6.4 | 6.4 |
| Range (min/max) | −18.0/16.8 | −16.8/15.5 | −16.2/13.4 | −17.0/15.6 |
| Shapiro-Wilk test | ||||
| W (df=140) | 0.993 | 0.988 | 0.983 | 0.983 |
| P | 0.671 | 0.247 | 0.079 | 0.078 |
| Absolute difference between 1st and 2nd measurements | ||||
| MAD | 1.1 | 1.3 | ||
| SD | 1.1 | 1.4 | ||
| Range (min/max) | 0/5.2 | 0/7.7 | ||
| Intraobserver ICC | 0.958 | 0.973 | ||
| 95% CI | 0.942–0.970 | 0.962–0.980 | ||
| P | <0.001 | <0.001 | ||
| Absolute difference of 2nd measurements between observers A and B | ||||
| MAD | 1.3 | |||
| SD | 1.2 | |||
| Range (min/max) | 0/6.5 | |||
| Interobserver ICC | 0.962 | |||
| 95% CI | 0.936–0.976 | |||
| P | <0.001 | |||
MAD, mean absolute difference; SD, standard deviation; ICC, interclass correlation coefficient; CI, confidence interval
Discussion
In this study, we have analyzed a cohort of healthy Japanese volunteers of both sexes with a wide age distribution from their 20s to 70s using EOS imaging and revealed the correlations among the anatomical and positional pelvic parameters to predict the positional parameters, SS and PT, based on the anatomical parameters and participant characteristics. APPA measurements using lateral 2D EOS images demonstrated excellent intra- and inter-observer reliabilities, and the mean value of APPA was 0.7°±6.0° (range, −16.8° to 15.5°) in a healthy Japanese population. Concerning the correlations between the anatomical and positional pelvic parameters, SS was found to be moderately correlated with PI and aSS, which is consistent with Suzuki et al.'s finding25). Moreover, we found that PT was moderately correlated with PI and aPT and weakly correlated with aSS.
Deterioration of standing sagittal alignment in ASD, which substantially debilitates patients' function and general health28,29), is compensated by pelvic retroversion quantified by the increase in PT6,7). Therefore, to predict the natural PT for each patient with ASD, it is deemed essential to determine the relationship between the anatomical and positional pelvic parameters in a healthy population. In contrast, in corrective spinal surgery for ASD, the target LL angle is usually determined based on the PI for each patient29). However, LL is the sagittal radiographic parameter most strongly correlated with SS7,30,31). Moreover, Roussouly et al. evaluated the variation in sagittal spinal alignment among healthy young adults and classified the sagittal spinal profile according to SS10). Therefore, estimation of the natural SS and PT for each patient with ASD is necessary to determine not only the natural LL but also the sagittal profile of the spine. To precisely predict the positional pelvic parameters (SS and PT), we performed a multiple linear regression analysis with a forward stepwise procedure using anatomical parameters (PI, aSS, and aPT) and participant characteristics. Consequently, we have deduced the following equations: SS=0.404×aSS+0.203×PI+12.463, PT=−0.391×aSS+0.774×PI+1.950×sex (male=0, female=1)−12.971. These results indicate that SS and PT were more precisely predicted by considering not only PI but also aSS and sex. Notably, unlike PI and aPT, aSS does not use the center of the femoral head in the measurements. Therefore, aSS may be able to represent the characteristics of SS that PI and aPT cannot. This hypothesis is consistent with the result that the effect of aSS was the greatest among the factors in the regression model for SS, whereas the effect of PI was the greatest for PT, as per the analysis of standardized partial regression coefficients in the regression models. However, the PT/PI ratio, which reflects the amount of compensation via pelvic retroversion in the standing position, has demonstrated no significant difference and a significant, positive correlation with the aPT/PI ratio in our cohort. Therefore, the difference between aPT/PI and PT/PI in patients with ASD may be used to estimate the amount of compensation in the standing position.
The complex anatomy of the sacroiliac (SI) joint with a strong network of ligaments restricts the movement of the SI joint32,33); therefore, the PI has been assumed to be constant in each individual. However, previous studies have demonstrated a positive correlation between PI and age in both healthy adults and patients with scoliosis7,13,18,19). Additionally, Hasegawa et al. investigated the factors affecting PI, including pelvic thickness (PTh), which is the distance between the hip axis and the center of the sacral endplate18), a representative parameter for pelvic size, and demonstrated a positive correlation between PI and age, a negative correlation between PTh and age, and the highest contribution of PTh to the PI value among the affecting factors. Based on these results, they hypothesized that aging or SI joint osteoarthrosis with concomitant hypermobility may result in a posteroinferior shift of the sacral endplate, leading to an increase in PI18). The effects of the posteroinferior shift of the sacral endplate should be smaller on the angle between the APP and the sacral endplate, or aSS, than on the angle between the perpendicular line from the sacral plate and the line connecting the midpoint of the sacral plate to the hip axis, or PI. Therefore, as compared to PI, aSS is a less susceptible anatomical parameter to aging and SI joint degeneration.
This study has some limitations. For one, this was a cross-sectional study with a small sample size of healthy Japanese participants. Therefore, definitive conclusions with regard to age-related changes and the effects of ethnicity on pelvic parameters could not be drawn. In addition, age distribution in our cohort was young; 96.4% of subjects were younger than 60 years, which might be due to the inclusion criteria of ODI ≤20%. Moreover, the age distribution in our study might have caused the PI to be insignificantly correlated with age. Therefore, further studies with a larger sample size and a wide age range comprising a multiethnic cohort are deemed necessary. Moreover, there are certain limitations in adapting our results to patients with ASD. First, because this current study was conducted on healthy volunteers, it remains unclear if the APP is reliable as a reference plane and if anatomical pelvic parameters measured based on the APP are constant in patients with ASD. Second, all measurements in this study were performed using radiographs acquired using an EOS system, which provides excellent intra- and inter-observer reliabilities. Therefore, it is unclear if radiographs acquired using commonly used conventional X-ray devices yield similar results, especially in patients with ASD.
In conclusion, we were able to establish normative APPA, aSS, and aPT values in a cohort of healthy adult Japanese volunteers. SS has been significantly and positively correlated with aSS and PI, whereas PT has been significantly and positively correlated with aSS, aPT, and PI. Multiple linear regression analysis deduced the formulas for predicting SS and PT from the anatomical pelvic parameters and participant characteristics, in which aSS was determined to have the greatest effect on SS and PI for PT. Therefore, anatomical pelvic parameters measured based on the APP, especially aSS, are novel fundamental parameters for predicting standing sagittal alignment of the pelvis in a healthy population. As these parameters might be useful in estimating compensation by pelvic retroversion and in setting a target alignment for correction surgery in patients with ASD, validation of the estimation method on the natural sagittal spinopelvic alignment using aSS and aPT in patients with ASD is currently underway.
Disclaimer: Kei Watanabe is one of the Editors of Spine Surgery and Related Research and on the journal's Editorial Committee. Kazuhiro Hasegawa is one of the advisors of Spine Surgery and Related Research and on the journal's Editorial Committee. They were not involved in the editorial evaluation or decision to accept this article for publication at all.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: None.
Author Contributions: M.O., K.H., S.H., and N.I. designed the study. M.O. and N.I. performed data acquisition, analysis, and interpretation of the results. M.O. and K.H. wrote the manuscript. M.O., K.H., S.H., N.I., H.T., T.M., K.M., M.S., and K.W. drafted and substantively revised the manuscript.
Ethical Approval: This study was approved by the Ethics Committee of Medical Corporation Aijinkai (IRB approval #6 [R1]-2019, on May 16, 2019) and Niigata University Graduate School of Medical and Dental Sciences (No. 2022-0048).
Informed Consent: Written informed consent was obtained from all participants.
References
- 1.Dubousset J. Three-dimensional analysis of the scoliotic deformity. Pediatr Spine Princ Pract. 1994. [Google Scholar]
- 2.Hasegawa K, Dubousset JF. Cone of economy with the chain of balance-historical perspective and proof of concept. Spine Surg Relat Res. 2022;6(4):337-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duval-Beaupère G, Robain G. Visualization on full spine radiographs of the anatomical connections of the centres of the segmental body mass supported by each vertebra and measured in vivo. Int Orthop. 1987;11(3):261-9. [DOI] [PubMed] [Google Scholar]
- 4.Duval-Beaupère G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20(4):451-62. [DOI] [PubMed] [Google Scholar]
- 5.Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diebo BG, Ferrero E, Lafage R, et al. Recruitment of compensatory mechanisms in sagittal spinal malalignment is age and regional deformity dependent: a full-standing axis analysis of key radiographical parameters. Spine. 2015;40(9):642-9. [DOI] [PubMed] [Google Scholar]
- 7.Hasegawa K, Okamoto M, Hatsushikano S, et al. Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur Spine J. 2016;25(11):3675-86. [DOI] [PubMed] [Google Scholar]
- 8.Hasegawa K, Okamoto M, Hatsushikano S, et al. Compensation for standing posture by whole-body sagittal alignment in relation to health-related quality of life. Bone Joint J. 2020;102-B(10):1359-67. [DOI] [PubMed] [Google Scholar]
- 9.Laouissat F, Sebaaly A, Gehrchen M, et al. Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur Spine J. 2018;27(8):2002-11. [DOI] [PubMed] [Google Scholar]
- 10.Roussouly P, Gollogly S, Berthonnaud E, et al. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30(3):346-53. [DOI] [PubMed] [Google Scholar]
- 11.Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine. 2012;37(12):1077-82. [DOI] [PubMed] [Google Scholar]
- 12.Yilgor C, Sogunmez N, Boissiere L, et al. Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am. 2017;99(19):1661-72. [DOI] [PubMed] [Google Scholar]
- 13.Vrtovec T, Janssen MM, Likar B, et al. A review of methods for evaluating the quantitative parameters of sagittal pelvic alignment. Spine J. 2012;12(5):433-46. [DOI] [PubMed] [Google Scholar]
- 14.Hasegawa K, Okamoto M, Hatsushikano S, et al. Difference in whole spinal alignment between supine and standing positions in patients with adult spinal deformity using a new comparison method with slot-scanning three-dimensional X-ray imager and computed tomography through digital reconstructed radiography. BMC Musculoskelet Disord. 2018;19(1):437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohya J, Kawamura N, Takasawa E, et al. Pelvic incidence change on the operating table. Eur Spine J. 2021;30(9):2473-9. [DOI] [PubMed] [Google Scholar]
- 16.Wei C, Zuckerman SL, Cerpa M, et al. Can pelvic incidence change after spinal deformity correction to the pelvis with S2-alar-iliac screws? Eur Spine J. 2021;30(9):2486-94. [DOI] [PubMed] [Google Scholar]
- 17.Oba H, Ebata S, Takahashi J, et al. Loss of pelvic incidence correction after long fusion using iliac screws for adult spinal deformity: cause and effect on clinical outcome. Spine. 2019;44(3):195-202. [DOI] [PubMed] [Google Scholar]
- 18.Hasegawa K, Hatsushikano S, Le Huec JC, et al. Pelvic thickness, sex, ethnicity, and age affect pelvic incidence in healthy volunteers of Multi-ethnic Alignment Normative Study (MEANS) database. Eur Spine J. 2022;31(6):1421-30. [DOI] [PubMed] [Google Scholar]
- 19.Sardar ZM, Cerpa M, Kelly M, et al. Age and gender based spinopelvic and regional spinal alignment in asymptomatic adult volunteers: results of the Multi-ethnic Alignment Normative Study (MEANS). Spine. 2022;47(19):1382-90. [DOI] [PubMed] [Google Scholar]
- 20.Pizones J, García-Rey E. Pelvic motion the key to understanding spine-hip interaction. EFORT Open Rev. 2020;5(9):522-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85(2):278-86. [DOI] [PubMed] [Google Scholar]
- 22.Tiziani S, Gautier L, Farei-Campagna J, et al. Correlation of pelvic incidence with radiographical parameters for acetabular retroversion: a retrospective radiological study. BMC Med Imaging. 2015;15:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217-20. [PubMed] [Google Scholar]
- 24.Imai N, Miyasaka D, Tsuchiya K, et al. Evaluation of pelvic morphology in female patients with developmental dysplasia of the hip using three-dimensional computed tomography: a cross-sectional study. J Orthop Sci. 2018;23(5):788-92. [DOI] [PubMed] [Google Scholar]
- 25.Suzuki H, Imai N, Nozaki A, et al. Anatomical sacral slope, a new pelvic parameter, is associated with lumbar lordosis and pelvic incidence in healthy Japanese women: a retrospective cross-sectional study. J Orthop Surg (Hong Kong). 2020;28(1):2309499019888809. [DOI] [PubMed] [Google Scholar]
- 26.Okamoto M, Jabour F, Sakai K, et al. Sagittal balance measures are more reproducible when measured in 3D vs in 2D using full-body EOSⓇ images. Eur Radiol. 2018;28(11):4570-7. [DOI] [PubMed] [Google Scholar]
- 27.Hasegawa K, Hatsushikano S, Watanabe K, et al. Scoliosis Research Society-22r score is affected by standing whole body sagittal alignment, age, and sex, but not by standing balance or skeletal muscle mass in healthy volunteers. Eur Spine J. 2022;31(11):3000-12. [DOI] [PubMed] [Google Scholar]
- 28.Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine. 2009;34(17):E599-606. [DOI] [PubMed] [Google Scholar]
- 29.Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine. 2013;38(13):E803-12. [DOI] [PubMed] [Google Scholar]
- 30.Vialle R, Levassor N, Rillardon L, et al. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87(2):260-7. [DOI] [PubMed] [Google Scholar]
- 31.Vaz G, Roussouly P, Berthonnaud E, et al. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11(1):80-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vleeming A, Pool-Goudzwaard AL, Hammudoghlu D, et al. The function of the long dorsal sacroiliac ligament: its implication for understanding low back pain. Spine. 1996;21(5):556-62. [DOI] [PubMed] [Google Scholar]
- 33.Eichenseer PH, Sybert DR, Cotton JR. A finite element analysis of sacroiliac joint ligaments in response to different loading conditions. Spine. 2011;36(22):E1446-52. [DOI] [PubMed] [Google Scholar]