Neurofibromatosis type I (NF-1) is associated with skeletal deformities, with spinal deformities being the most common1-3). Patients with NF-1 with intracanal rib head (IRH) are often young4). Herein, we report the case of an adult with IRH-induced myelopathy treated with rib head resection and posterior spinal fusion.
The patient was a 55-year-old woman whose chief complaint was gait disturbance. She was diagnosed with syndromic scoliosis due to NF-1 as an elementary school student. At the age of 54, brace treatment of back pain was initiated. After a year, she gradually felt her knees giving way during walking without any trauma, and she could not walk well. She exhibited no painful rib hump or Lhermitte's sign (Fig. 1). Manual muscle tests revealed weakness below the psoas level. Deep tendon reflexes demonstrated hyperactivity in the patellar and Achilles tendon reflexes; she also had urinary incontinence. The Japanese Orthopedic Association (JOA) score of thoracic myelopathy was 2.5/11, the Japanese Orthopedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) score of the lower extremity was 9, and X-ray imaging revealed left convex rigid scoliosis (Fig. 2). Preoperative magnetic resonance imaging and computed tomography (CT) revealed a flattened spinal cord at the 11th rib caused by IRH (Fig. 3).
Figure 1.
Patient’s clinical photographs.
Café-au-lait spots and lumbar humps are present due to severe scoliosis.
Figure 2.
Preoperative radiographs.
X-ray depicting left convex scoliosis with a Cobb angle of 72° from the T11 to L2 level (A), and a lateral view showing 60° kyphosis from the T10 to L2 level (B). Regarding sagittal modifiers, the pelvic incidence-lumbar lordosis is 16°, the sagittal vertebral axis is 84 mm, and the pelvic tilt is 56° (B). Side bending and manual traction evaluations revealed rigid scoliosis (C, D, and E).
Figure 3.
Preoperative computed tomography and magnetic resonance imaging.
Computed tomography depicting IRH at the 11th rib (A and B). Magnetic resonance imaging showing the dural canal compressed by IRH (C). Intraoperation picture shows the dural tube (asterisk) and 11th rib head (arrow) after resection of left articular process invaginated into the spinal canal (D).
She was diagnosed with scoliosis associated with NF-1 and thoracic myelopathy due to IRH and underwent surgery. Initially, laminectomy and facetectomy were performed. Invagination of the upper facet of T12 and entrapped 11th rib head severely compressed the spinal cord. It was difficult to resect them; however, complete resection using intraoperative CT navigation (O-armⓇ, StealthStation8Ⓡ) was performed. Finally, T5-L4 posterior corrective fusion and bone grafting with local and allogeneic bone were performed. Intraoperative blood loss was 2300 g. Her gait and urinary disturbance improved and corrections were maintained two years after surgery (Fig. 4), with a JOA and JOACMEQ lower extremity scores of 4.5/11 and 32, respectively.
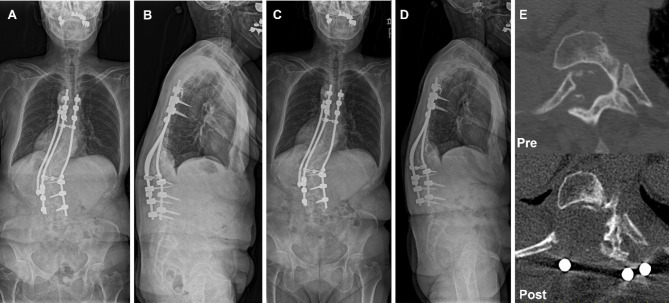
Figure 4.
Radiographs and computed tomography after surgery.
Radiographs 2 years after surgery show the thoracolumbar Cobb angle of 59° and the kyphosis 16° (C and D). The pelvic incidence-lumbar lordosis is 16°, sagittal vertebral axis is 73 mm, and pelvic tilt is 38° (D). There is unremarkable correction loss compared to immediately after surgery (A and B). Computed tomography showing complete resection of the IRH compared with pre operation (E).
IRH were observed in 16 to 25 % in patients with dystrophic type scoliosis secondary to NF-1, with an age range of 8.8-14.2 years5,6). Treatment in these patients was determined based on the presence of preoperative neurological symptoms5). If patients have mild or no spinal cord injury, correcting spinal deformities could lead to IRH decompression5,7). Since it may lead to severe neurological deficit, high-grade osteotomy should be performed carefully in selected patients with dystrophic scoliosis8). Based on the clinical course of our patient, direct decompression by resecting the IRH before correcting the spinal deformity using grade 1 and 2 osteotomies was recommended as a safe treatment method for adult rigid scoliosis. If IRH remains unresectable due to cord adherence, neurological damage might be prevented by making IRH floating via osteotomy of rib shaft on the proximal side and avoiding remarkable translational correction.
IRH primarily occurs on the convex side of the main thoracic curve5-7,9). Half of the IRH cases were located on the convex side of the apical vertebra of the main thoracic curve, 29% were on 1 above the apical vertebra, and 21% were below the apical vertebra. In this case, IRH occurred at the lower-end vertebra of the thoracolumbar curve. As dystrophic kyphoscoliosis gradually progresses, the upper facet of T12 might have severely entered the spinal canal. Furthermore, this dystrophic condition could have caused expansion of the foramen and costotransverse joint dislocation at T11, resulting in IRH. IRH mainly occurs in young patients. However, some adult cases could not be treated using the same strategy as in young patients showing flexibility of spinal deformity. Even if patients with spinal deformities associated with NF-1 exhibit no other symptoms, they should be carefully observed over a long period of time.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: None
Author Contributions: TY, YN, and KW designed the study; GK, TA, and KA revised the manuscript; KW and YI supervised the study; and TY and KW wrote the manuscript.
Ethical Approval: This study entitled “A Case of Neurofibromatosis 1 with Myelopathy Due to Intracanal Rib Head and Kyphoscoliosis in an Adult” was approved by the Ethics Committee of Hirosaki University Graduate School of Medicine, on March 9th, 2023. Approval document is attached for this report as a supplementary file in this submission, because approval codes have not been issued by the institutional review board for case reports.
Informed Consent: Informed consent for publication was obtained by the patient in this study.
References
- 1.Akbarnia BA, Gabriel KR, Beckman E, et al. Prevalence of scoliosis in neurofibromatosis. Spine. 1992;17(8 Suppl):S244-8. [DOI] [PubMed] [Google Scholar]
- 2.Vitale MG, Guha A, Skaggs DL. Orthopaedic manifestations of neurofibromatosis in children: an update. Clin Orthop Relat Res. 2002;(401):107-18. [DOI] [PubMed] [Google Scholar]
- 3.Curtis-Lopez CM, Soh C, Ealing J, et al. Clinical and neuroradiological characterisation of spinal lesions in adults with neurofibromatosis type 1. J Clin Neurosci. 2020;77:98-105. [DOI] [PubMed] [Google Scholar]
- 4.Mataliotakis GI, Bounakis N, Garrido-Stratenwerth E. Surgical management of intracanal rib head dislocation in neurofibromatosis type 1 dystrophic kyphoscoliosis: report of two cases and literature review. Case Rep Orthop. 2016;2016:2908915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gao R, Guo D, Zhang X, et al. Surgical treatment of the intraspinal rib head dislocation in children with dystrophic scoliosis secondary to type 1 neurofibromatosis. J Pediatr Orthop. 2022;42(3):e242-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mao S, Shi B, Wang S, et al. Migration of the penetrated rib head following deformity correction surgery without rib head excision in dystrophic scoliosis secondary to type 1 neurofibromatosis. Eur Spine J. 2015;24(7):1502-9. [DOI] [PubMed] [Google Scholar]
- 7.Yalcin N, Bar-on E, Yazici M. Impingement of spinal cord by dislocated rib in dystrophic scoliosis secondary to neurofibromatosis type 1: radiological signs and management strategies. Spine. 2008;33(23):E881-6. [DOI] [PubMed] [Google Scholar]
- 8.Neifert SN, Khan HA, Kurland DB, et al. Management and surgical outcomes of dystrophic scoliosis in neurofibromatosis type 1: a systematic review. Neurosurg Focus. 2022;52(5):E7. [DOI] [PubMed] [Google Scholar]
- 9.Khoshhal KI, Ellis RD. Paraparesis after posterior spinal fusion in neurofibromatosis secondary to rib displacement: case report and literature review. J Pediatr Orthop. 2000;20(6):799-801. [DOI] [PubMed] [Google Scholar]