Abstract
BACKGROUND
The gender gap in physician pay is often attributed in part to women working fewer hours than men, but evidence to date is limited by self-report and a lack of detail regarding clinical revenue and gender differences in practice style.
METHODS
Using national all-payer claims and data from electronic health records, we conducted a cross-sectional analysis of 24.4 million primary care office visits in 2017 and performed comparisons between female and male physicians in the same practices. Our primary independent variable was physician gender; outcomes included visit revenue, visit counts, days worked, and observed visit time (interval between the initiation and the termination of a visit). We created multivariable regression models at the year, day, and visit level after adjustment for characteristics of the primary care physicians (PCPs), patients, and types of visit and for practice fixed effects.
RESULTS
In 2017, female PCPs generated 10.9% less revenue from office visits than their male counterparts (−$39,143.2; 95% confidence interval [CI], −53,523.0 to −24,763.4) and conducted 10.8% fewer visits (−330.5 visits; 95% CI, −406.6 to −254.3) over 2.6% fewer clinical days (−5.3 days; 95% CI, −7.7 to −3.0), after adjustment for age, academic degree, specialty, and number of sessions worked per week, yet spent 2.6% more observed time in visits that year than their male counterparts (1201.3 minutes; 95% CI, 184.7 to 2218.0). Per visit, after adjustment for PCP, patient, and visit characteristics, female PCPs generated equal revenue but spent 15.7% more time with a patient (2.4 minutes; 95% CI, 2.1 to 2.6). These results were consistent in subgroup analyses according to the gender and health status of the patients and the type and complexity of the visits.
CONCLUSIONS
Female PCPs generated less visit revenue than male colleagues in the same practices owing to a lower volume of visits, yet spent more time in direct patient care per visit, per day, and per year. (Funded in part by the Robert Wood Johnson Foundation.)
FEMALE PHYSICIANS REPRESENT A GROWING share of the medical workforce and may have better patient outcomes than male physicians,1–4 yet numerous studies have shown that they earn 8 to 29% less than their male counterparts.5–13 The magnitude of and reasons for this pay gap are still debated. There are clear roles for factors such as physician specialty, academic rank, and leadership status, all of which may be related in part to gender bias.6,14,15 Many investigators have suggested that the gap may also be explained by the possibility that female doctors on average work fewer hours than male doctors.5,6,9,11–13,16 However, this conclusion is drawn largely from survey-based studies that rely on heterogenous samples and extrapolate physician-reported estimates of hours worked, visits completed, and compensation. In addition, such previous studies have lacked sufficient details regarding patients’ characteristics, types of visits with physicians, and clinical revenue to confirm these underlying assumptions.
The relationship between physician gender and work hours deserves further scrutiny, especially given the known gender differences in practice style. Several studies have shown that female doctors may conduct longer visits,17,18 offer more counseling,17,19 and bill in less lucrative ways20 than male doctors, owing to factors such as personal characteristics, sociocultural norms, or patients’ expectations.19 Although longer visits are associated with better care,21–27 such differences may disadvantage female physicians within the still-predominant volume-based physician payment model that values visit number over quality.22,28,29 As practice leaders and policymakers experiment with new payment models that build on or disrupt the volume-based system,30 it is important to understand how the current model may contribute to the gender pay gap and, in turn, to broader population health goals. Therefore, we used a large sample of national all-payer claims and data from electronic health records (EHRs) to estimate gender differences in the time spent on primary care visits and the subsequent revenue received.
METHODS
STUDY DESIGN AND OVERVIEW
We conducted a cross-sectional analysis of primary care visits using a national sample of de-identified all-payer claims and EHR data for 2011 through 2017. The data were supplied by athenahealth, a technology company that provides Internet-based medical billing, practice management, and EHR software. The study was approved by institutional review boards at the National Bureau of Economic Research and the University of Minnesota.
Our study sample included all office visits in 2017 with physicians specializing in adult primary care (internal medicine, family practice, or general practice) who used athenahealth, were active (defined as working ≥90 days that year), and belonged to a practice with at least one male and one female primary care physician (PCP) to allow for within-practice comparisons. (Additional details regarding the study design are provided in the Methods section and Fig. S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org.)
STUDY MEASURES
The primary independent variable was physician gender. At the year level, our outcomes included the total allowed charges (i.e., revenue), number of visits, number of days worked (defined as billing ≥1 visit that day), and observed visit time (in minutes, quantified as the interval between the initiation and the termination of a visit on the basis of the EHR time stamps) aggregated across all visits in 2017.
The observed visit time measure relied on time stamps, which capture clinicians’ actions in the EHR across sequential stages of an encounter with a patient. Generally, after staff members have completed check-in (e.g., confirming insurance), a medical assistant conducts the intake assessment (e.g., vital signs and medication reconciliation). Once intake is complete, the physician clicks “Go to Exam” to start the visit (e.g., obtaining and documenting history, performing a physical examination, and placing orders). At the end of the visit, the physician closes the examination stage to advance the encounter to the checkout stage. If the time stamps for a visit were not recorded or did not meet our quality criteria, we considered the observed visit time value to be missing and used multiple imputation to impute this value.
Day-level outcomes included total allowed charges, number of visits, and observed visit time aggregated per day. Visit-level outcomes included allowed charges, number of diagnoses that were documented (according to codes of the International Classification of Diseases, Tenth Revision) to assess the number of topics discussed during the visit, number of orders that were placed (i.e., prescriptions, laboratory tests, imaging tests, and referrals), observed visit time, and difference between the observed visit time and the scheduled duration.
CHARACTERISTICS OF THE PHYSICIANS, PATIENTS, AND VISITS
We examined the characteristics of physicians, including age (continuous variable), degree (doctor of medicine or doctor of osteopathic medicine), specialty (internal medicine, family practice, or general practice), and number of scheduled sessions per day or week (defined as predetermined blocks of time in which physicians schedule visits, measured as a continuous integer variable).
The characteristics of the patients included age (categorical variable), gender, race or ethnic group, marital status, number of chronic conditions (as determined at the visit level on the basis of the previous 6 months to 3 years, according to the criteria of the Chronic Conditions Data Warehouse of the Centers for Medicare and Medicaid Services [CMS]), primary insurer (as determined at the visit level), and whether the patient was new to the physician (binary variable, determined at the visit level if the physician had billed no services for that patient since 2011).
Finally, we examined characteristics of the visit, including type (using Current Procedural Terminology Evaluation and Management billing codes from the American Medical Association, including codes for problem-based visits [99201–99215] and for preventive visits [99381–99397, G0402, and G0438–G0439]), diagnosis type (low-acuity condition vs. other), and whether the visit was scheduled in advance or as a same-day visit. Details about these determinations are provided in the Methods section and Table S1.
STATISTICAL ANALYSIS
We compared male and female physicians with respect to their characteristics and those of the patients they saw in 2017, using regression models with practices included as fixed effects. To quantify and attribute any gender differences in the outcomes of interest, we then estimated multivariable, ordinary least-squares regression models at the year, day, and visit level. For visits with missing data for the observed visit time, we used multiple imputation to impute these values.
All analyses used practice fixed effects, which means that our estimates represent gender differences within each given practice. This approach allowed us to control for unobservable differences between practices. For models at the year, day, and visit level, we also adjusted for the characteristics of the physicians, including age, academic degree, specialty, and number of sessions per week or day (for year and day models, respectively). Day-level models were further adjusted for day-of-the-week fixed effects. In addition, visit-level models included the characteristics of patients (age, gender, race or ethnic group, marital status, chronic condition count, insurer, and new-to-physician status), day-of-the-week fixed effects, diagnosis type, and whether the visit was scheduled in advance or same-day.
In addition, we conducted several sensitivity analyses to interrogate our findings. To supplement the analysis of mean gender differences as derived from regression analyses, we compared male and female PCPs according to the distribution of minutes per visit and visit revenue per minute.
We examined work Relative Value Units, the standardized unit that is used to measure physician work,31 which is then multiplied by payer-specific rates to calculate allowed charges, at the year, day, and visit level. We replicated analyses using only visits for which time-stamp data were available. We stratified year- and visit-level results according to physician age group (25 to 44 years, 45 to 64 years, and ≥65 years) and visit-level results according to patient gender. To determine whether differences persisted among medically complex patients, we performed a visit-level subgroup analysis among patients with two or more chronic conditions. Acknowledging the possibility that patients who select female PCPs may have expectations or preferences that differ from those of other patients, we performed a subgroup analysis of same-day visits, for which patients may have less choice in which clinician they see.
To examine whether results were consistent within levels of visit intensity, we repeated our analyses among visits with the same billing code for common problem-based visits (99203–99205 and 99213–99215) and preventive visits. Because these codes can be chosen on the basis of the visit complexity (as defined by documentation, which we cannot observe) or on time spent with the patient (e.g., ≥25 minutes for a 99214 code visit or ≥40 minutes for a 99215 code visit), we also explored the hypothesis that female PCPs may be more likely than male PCPs to miss opportunities to bill a higher-intensity (i.e., higher-paying) code on the basis of visit duration. Specifically, we examined the percentage of code 99213 visits that were more than 25 minutes in length and therefore might have been billed as code 99214 and the percentage of code 99214 visits that were more than 40 minutes in length and therefore might have been billed as code 99215. Details regarding the statistical methods are provided in the Supplementary Appendix.
RESULTS
STUDY POPULATION
We examined 24,391,810 primary care visits in 2017 that involved 8,513,290 patients and 8302 active PCPs across all 50 states. (These 8302 PCPs represented 5% of all PCPs in the United States.) Of the PCPs who were included in the study, 36.4% were female and 53.2% had an internal medicine specialty — results that are similar to the national distribution of PCPs in the Physician Compare database. Our sample had a larger share of PCPs in the South and fewer in the West (Table S2). Patients in our sample were older and more often enrolled in Medicare than those in a national survey-based sample of primary care visits (Table S3).
DIFFERENCES IN PCP, PATIENT, AND VISIT CHARACTERISTICS
In our sample, female PCPs were younger than their male counterparts and were more likely to specialize in family practice (Table 1). The female PCPs were scheduled for the same number of sessions per week on average as the male PCPs. Female PCPs were more likely to have visits with patients who were under the age of 65 years, female, non-White race, and covered by Medicaid or commercial insurance. Female PCPs had a slightly larger share of visits with patients who were new to them.
Table 1.
Characteristics of Male and Female PCPs and Their Visits with Patients (2017 Data).*
| Characteristic | Male PCPs | Female PCPs |
|---|---|---|
| Physicians | ||
| No. of physicians included in the analysis | 5284 | 3018 |
| Mean age (yr) | 53.2 | 46.5 |
| Specialty (%) | ||
| Internal medicine | 56.7 | 47.0 |
| Family practice | 42.5 | 52.4 |
| General practice | 0.8 | 0.6 |
| Academic degree (%) | ||
| M.D. | 87.1 | 83.3 |
| D.O. | 12.9 | 16.6 |
| Mean no. of sessions per week† | 7.9 | 7.9 |
| Patients and Visits | ||
| No. of annual visits | 16,422,457 | 7,969,353 |
| Age category %‡ | ||
| <15 yr | 2.8 | 4.0 |
| 15–24 yr | 3.9 | 5.6 |
| 25–44 yr | 14.4 | 18.8 |
| 45–64 yr | 33.9 | 35.0 |
| ≥65 yr | 44.9 | 36.5 |
| Female gender (%) | 49.7 | 70.0 |
| Married (%) | 54.9 | 51.2 |
| Race or ethnic group (%)§ | ||
| Non-Hispanic White | 76.1 | 73.0 |
| Non-White | 11.1 | 13.4 |
| Other or unknown | 12.9 | 13.6 |
| Type of payer (%) | ||
| Medicare | ||
| Traditional | 27.7 | 22.2 |
| Advantage | 13.7 | 11.7 |
| Medicaid | 7.3 | 8.7 |
| Medicare plus Medicaid | 4.8 | 4.5 |
| Commercial insurance | 43.0 | 49.6 |
| No insurance | 2.0 | 2.0 |
| Other payer | 1.5 | 1.2 |
| Mean no. of chronic conditions¶ | 1.1 | 1.0 |
| Visit for low-acuity condition (%)‖ | 4.7 | 5.4 |
| Same-day visit (%) | 22.3 | 23.4 |
| Patient new to physician (%) | 21.8 | 23.2 |
Percentages are adjusted characteristic means that were calculated with the use of a regression of the characteristic on physician gender that included practice fixed effects. Characteristics of the patients were analyzed at the patient-visit level. Percentages may not total 100 because of rounding. PCP denotes primary care physician.
To determine scheduled sessions, each physician was specified as having a session, out of a possible 10 morning (7 a.m. to noon) or afternoon (noon to 7 p.m.) weekday sessions, if they had at least one visit time-stamped during that session (e.g., Monday morning) for at least 26 weeks of the study year. We then added the number of sessions that the physician had in a given week (range, 1 to 10).
Data regarding age were missing for four patient visits, one for male PCPs and three for female PCPs.
Race or ethnic group was reported by the patients in the electronic health record.
The count of previously documented diagnoses of chronic conditions was based on the Chronic Conditions Data Warehouse criteria of the Centers for Medicare and Medicaid Services.
The classification of a condition as low acuity (e.g., conjunctivitis and sinusitis) was based on the primary diagnosis code for the visit (Table S1).
DIFFERENCES IN OUTCOMES
In 2017, in unadjusted analyses, female PCPs generated 12.4% less visit revenue than male PCPs in the same practices: $316,101.9 and $360,820.8, respectively, for a difference of −$44,718.9 (95% confidence interval [CI], −60,525.7 to −28,912.1) (Table S4). After adjustment for the physician’s age, academic degree, specialty, and number of sessions worked per week, female PCPs generated 10.9% less visit revenue than their male counterparts (−$39,143.2; 95% CI, −53,523.0 to −24,763.4) (Table 2). In adjusted analyses, female PCPs worked 2.6% fewer days per year (−5.3 days; 95% CI, −7.7 to −3.0) and provided 10.8% fewer visits (−330.5 visits; 95% CI, −406.6 to −254.3) and yet spent 2.6% more time with patients than male PCPs over the year (1201.3 minutes; 95% CI, 184.7 to 2218.0).
Table 2.
Adjusted Year-, Day-, and Visit-Level Outcomes for Male and Female PCPs.
| Outcome | Male PCPs | Female PCPs | Between-Group Difference* | |
|---|---|---|---|---|
| Absolute (95% CI) | Relative % | |||
| Per year | ||||
| No. of physicians included in analysis | 5284 | 3018 | ||
| Allowed charges (U.S. $) | 358,795.1 | 319,652.0 | −39,143.2 (−53,523.0 to −24,763.4) | −10.9 |
| No. of visits | 3058.2 | 2727.7 | −330.5 (−406.6 to −254.3) | −10.8 |
| No. of days in clinic | 203.3 | 197.9 | −5.3 (−7.7 to −3.0) | −2.6 |
| Observed time spent in patient visits (min) † | 46,709.2 | 47,910.6 | 1201.3 (184.7 to 2218.0) | 2.6 |
| Per day | ||||
| No. of physician-days included in the analysis | 1,085,623 | 585,808 | ||
| Allowed charges (U.S. $) | 1,792.3 | 1,611.6 | −180.7 (−246.8 to −114.7) | −10.1 |
| No. of visits | 15.2 | 13.6 | −1.6 (−1.9 to −1.3) | −10.5 |
| Observed time spent in patient visits (min) † | 231.5 | 239.2 | 7.7 (3.6 to 11.8) | 3.3 |
| Per visit | ||||
| No. of visits included in the analysis | 16,422,457 | 7,969,353 | ||
| Allowed charges (U.S. $) | 117.4 | 116.9 | −0.5 (−4.3 to 3.2) | −0.4 |
| No. of diagnoses documented | 3.4 | 3.7 | 0.2 (0.2 to 0.3) | 5.9 |
| No. of orders placed | 2.6 | 3.1 | 0.5 (0.4 to 0.5) | 19.2 |
| Observed visit time (min) † | 15.3 | 17.6 | 2.4 (2.1 to 2.6) | 15.7 |
| Actual visit duration vs. scheduled duration (min)‡ | −0.9 | 0.8 | 1.8 (1.5 to 2.0) | 188.9 |
The between-group difference is shown as the value among female PCPs, as compared with that among male PCPs.
For visits for which the observed visit time data were missing (i.e., time stamps were not recorded or did not meet quality standards), this value was derived by means of multiple imputation.
This value was calculated by subtracting the scheduled visit duration from the observed visit time. Data are provided for the 83.8% of visits for which information about the scheduled visit duration was available. (Details regarding this category are provided in the Supplementary Appendix.)
Per day in the clinic, female PCPs generated 10.1% less visit revenue than male PCPs (−$180.7; 95% CI, −246.8 to −114.7) and provided 10.5% fewer visits (−1.6 visits; −1.9 to −1.3). However, they spent 3.3% more time with patients (7.7 minutes; 95% CI, 3.6 to 11.8).
At the visit level, there was no significant revenue difference between female and male PCPs. Female PCPs documented 0.2 more diagnoses (5.9%) and placed 0.5 more orders (19.2%) per visit than their male counterparts. In addition, female PCPs scheduled more long (≥20 minutes) visits (26.6% vs. 23.3%), for a difference of 3.3 percentage points (95% CI, 1.6 to 5.0) among visits for which the scheduled duration was available. Female PCPs spent more time than scheduled on average and spent 15.7% more minutes with patients than male PCPs (2.4 minutes; 95% CI, 2.1 to 2.6). These estimates amounted to a revenue difference between female and male PCPs of $398.5 as compared with $460.4 per hour of direct patient care (i.e., 87% per hour relative to male PCPs).
SENSITIVITY ANALYSES
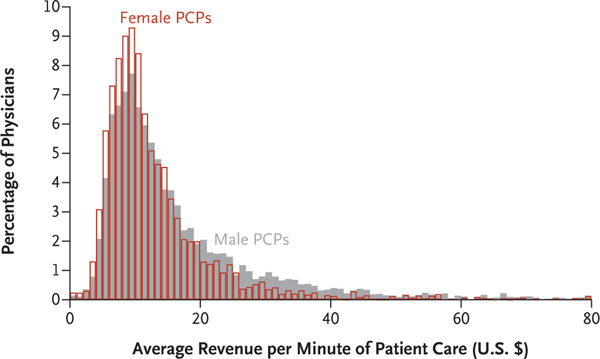
In sensitivity analyses, distributions of revenue per minute overlapped considerably between genders, although a larger share of female PCPs billed less than $10 per minute of direct patient care (Fig. 1). Differences in work Relative Value Units were consistent with revenue differences (Table S5). Results were largely consistent in an analysis that was limited to visits with nonmissing time-stamp data (Table S6). The gender gap in revenue was largest among doctors who were 65 years of age or older (Table S7A and S7B). Both male and female PCPs between the ages of 25 and 44 years worked fewer days per year than both male and female PCPs between the ages of 45 and 64 years; the gender differences in visit time per year and per visit were largest among younger PCPs.
Figure 1. Adjusted Visit Revenue per Minute of Direct Patient Care, According to Physician Gender.
Shown is the physician-level distribution of U.S. dollars earned per minute of observed visit time with patients among male and female primary care physicians (PCPs).
Female PCPs spent more time with both their male and female patients than male PCPs did. Although both male and female PCPs spent slightly more time with female patients than with male patients, these differences were not significant (Fig. S3). The gender gap in the time that PCPs spent with patients was more evident (i.e., the gap for this variable was larger than the gap among all visits) in the subset of visits with patients who had two or more chronic conditions, in which female PCPs spent 16.2% more time (adjusted difference, 2.7 minutes; 95% CI, 2.3 to 3.0) (Table S8). In a subgroup analysis of same-day visits, between-gender differences in the observed duration per visit were diminished, with female PCPs spending 12.1% more time (adjusted difference, 1.7 minutes; 95% CI, 1.4 to (Table S9).
Gender differences persisted within specific intensities of visits (Table S10). Female PCPs missed more opportunities to bill higher-intensity visit codes on the basis of time spent: among level 3 visits, 14.6% of those with female PCPs could have been billed as level 4 according to the time spent, as compared with 11.1% of those with male PCPs; among level 4 visits, 6.1% of those with female PCPs could have been billed as level 5, as compared with 4.2% with male PCPs.
DISCUSSION
Using national all-payer claims and EHR data, we found that female PCPs generated nearly 11% less annual visit revenue than otherwise similar male PCPs in the same practices, yet they spent more time with patients per visit, per day, and per year. The revenue gap was driven entirely by differences in visit volume, which were only in small part explained by the fewer days that female PCPs saw patients. Taken together, these results suggest that the differences in time spent with patients may be a contributor to the gender pay gap, with female physicians effectively generating 87% of what male physicians generate per hour of direct patient care.
We found that female PCPs spent nearly 16% more time with patients per visit than male PCPs (a difference of 2.4 minutes on average), even after we accounted for the characteristics of the PCPs, the patients, and the types of visits, including patient gender, payer, medical complexity, visit type and complexity, and previous relationship with the doctor. Our findings update previous estimates of a mean difference of 2.2 minutes in visit duration that was observed in small studies in which investigators used audio recordings and survey data from the 1980s and 1990s.18 Other studies have suggested that female PCPs may use this additional time to take a more thorough patient history, engage in shared decision making, provide more detailed explanations, and use more evidence-based, patient-centered communication approaches.17,19,32
Gender differences in how and for how long physicians communicate with patients may in turn arise from personal characteristics and from sociocultural norms. Patients may have different expectations of female doctors,33,34 and patients who desire more time may be more likely to select a female PCP. In support of this hypothesis, we found a narrower difference between female and male PCPs in the visit duration among same-day visits, for which patients may have less choice in which clinician they see. More face-to-face time is desired by clinicians and patients alike35 and is probably needed to deliver evidence-based primary care.23,24 Observational studies suggest that more time per visit is associated with higher rates of screening and counseling,21,22 better patient outcomes,21,23–25 greater patient satisfaction,22,26,27 and decreased physician burnout.36
We found that female PCPs worked slightly fewer days per year and scheduled substantially fewer visits while — and possibly in part to compensate for — spending more time with patients per visit. Our finding that this additional time spent per visit translated into more time in direct patient care per day and per year challenges conventional assumptions that female physicians work fewer hours (even if they may also choose to schedule fewer visits on the basis of this aspiration). This finding also substantiates the common critique that volume-based productivity is an imperfect measure of physician work.22,28,29 Although our study did not examine the substantial time that physicians spend on indirect patient care (e.g., telephone calls, documentation, and electronic messages),37 the duration of visits may be predictive of total work related to the visit.38 Moreover, a study performed in a large health system showed that female physicians spent more time than male physicians doing EHR-based indirect care, even on days on which they had no clinic session,39 which suggests that our findings offer a conservative estimate of differences in time worked.
We also found evidence of billing differences. Although female PCPs documented more diagnoses and placed more orders, they were more likely to miss opportunities to bill higher-paying visit codes on the basis of the time they had spent with patients, a finding that was consistent with the results of a study showing that female radiation oncologists billed fewer lucrative procedures than their male counterparts.20
This study offers several advances from previous work. Our use of a large sample of national all-payer claims and EHR data allowed us to observe clinical revenue across payers and time in visits rather than relying on physician-reported salary and work hours. We were able to compare doctors within the same practices and account for confounders at the physician, patient, and visit level.
Our study has several limitations. First, our analysis examined PCPs using one national EHR vendor, so our results may not generalize to all PCPs nationwide or to other cognitive, outpatient-based specialties. Second, we focused on visit-related revenue (the preponderance of primary care revenue) but cannot observe how this translated into physicians’ compensation. Although the vast majority of PCPs nationwide receive some form of productivity-based compensation40 and we compared doctors within practices (who are more likely to use the same compensation model), the implications of reported revenue differences would be dampened to the extent that those models attenuate the relationship between revenue generated and compensation. Third, we note that although our estimates of visit time (which were based on time stamps) match those of survey and audio-based studies,18,41 athenahealth time-stamp data have not been formally validated by direct observation. However, validation of data provided by other EHR vendors suggests that this is a reasonable approach.42 In addition, we took analytic steps to validate and refine this measure, and we confirmed that male and female physicians had the same frequency of visits with time stamps that did not meet our quality criteria (see the Methods section in the Supplementary Appendix). Fourth, even though our data set allowed for a detailed analysis of physician time, we could not ascertain how this time was used (beyond what is captured in billing codes) nor whether more time was associated with better patient outcomes.
Taken together, we found a nearly 11% gender gap in annual visit revenue among otherwise-similar physicians in the same practices. The gap was due primarily to male PCPs providing more visits, although female PCPs spent more time with patients per visit and overall. The disconnect between time spent and revenue generated may help to explain why female physicians (especially PCPs) face a greater risk of burnout than their male counterparts.33 This disconnect also presents an additional barrier to building and sustaining the increasingly female primary care workforce, given concerns that primary care is already undervalued relative to other specialties28,29 yet is important for improving population health outcomes and health care reform.43,44
More optimistically, our results suggest productivity-based payment is a modifiable structural mechanism for the gender pay gap. In the short term, clinicians could be prompted to use time-based billing when appropriate. Further research could examine ways to optimize physician time spent in visits (e.g., task sharing with clinical teams) without sacrificing patient outcomes or clinician well-being. Practice leaders and policymakers could also accelerate the development of other compensation models, such as payment for risk-adjusted panel size, and include measures of outcomes or patient experience in compensation formulas to address wage equity and to better reward time well spent.45,46
Supplementary Material
Acknowledgments
Supported in part by a grant (73623, to Dr. Sheridan) from the Robert Wood Johnson Foundation.
We thank Thomas Bodenheimer, M.D., Lydia E.W. Pace, M.D., M.P.H., Kathryn M. Rexrode, M.D., Thomas Sequist, M.D., M.P.H., Ming Tai Seale, Ph.D., M.P.H., and Julia Adler-Milstein, Ph.D., for helpful comments; Alex Everhart, B.A., for assistance with visit-time calculations; Aarti Rao, B.A., for assistance with materials included in the Supplementary Appendix; and athenahealth clients and staff for sharing their electronic-health-record user experience and knowledge with us.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
REFERENCES
- 1.Tsugawa Y, Jena AB, Figueroa JF, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med 2017;177:206–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallis CJ, Ravi B, Coburn N, Nam RK, Detsky AS, Satkunasivam R. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ 2017;359:j4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berthold HK, Gouni-Berthold I, Bestehorn KP, Böhm M, Krone W. Physician gender is associated with the quality of type 2 diabetes care. J Intern Med 2008; 264:340–50. [DOI] [PubMed] [Google Scholar]
- 4.Andersen MR, Urban N. Physician gender and screening: do patient differences account for differences in mammography use? Women Health 1997;26: 29–39. [DOI] [PubMed] [Google Scholar]
- 5.Weeks WB, Wallace AE. Race and gender differences in general internists’ annual incomes. J Gen Intern Med 2006; 21:1167–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baker LC. Differences in earnings between male and female physicians. N Engl J Med 1996;334:960–4. [DOI] [PubMed] [Google Scholar]
- 7.Ohsfeldt RL, Culler SD. Differences in income between male and female physicians. J Health Econ 1986;5:335–46. [DOI] [PubMed] [Google Scholar]
- 8.Lo Sasso AT, Richards MR, Chou CF, Gerber SE. The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood) 2011;30:193–201. [DOI] [PubMed] [Google Scholar]
- 9.Ness RB, Ukoli F, Hunt S, et al. Salary equity among male and female internists in Pennsylvania. Ann Intern Med 2000;133:104–10. [DOI] [PubMed] [Google Scholar]
- 10.Seabury SA, Chandra A, Jena AB. Trends in the earnings of male and female health care professionals in the United States, 1987 to 2010. JAMA Intern Med 2013;173:1748–50. [DOI] [PubMed] [Google Scholar]
- 11.Weeks WB, Wallace TA, Wallace AE. How do race and sex affect the earnings of primary care physicians? Health Aff (Millwood) 2009;28:557–66. [DOI] [PubMed] [Google Scholar]
- 12.Lo Sasso AT, Armstrong D, Forte G, Gerber SE. Differences in starting pay for male and female physicians persist; explanations for the gender gap remain elusive. Health Aff (Millwood) 2020;39:256–63. [DOI] [PubMed] [Google Scholar]
- 13.Ly DP, Seabury SA, Jena AB. Differences in incomes of physicians in the United States by race and sex: observational study. BMJ 2016;353:i2923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in the salaries of physician researchers. JAMA 2012;307:2410–7. [DOI] [PubMed] [Google Scholar]
- 15.Jagsi R, Griffith KA, Jones R, Perumalswami CR, Ubel P, Stewart A. Sexual harassment and discrimination experiences of academic medical faculty. JAMA 2016;315:2120–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frank E, Zhao Z, Sen S, Guille C. Gender disparities in work and parental status among early career physicians. JAMA Netw Open 2019;2(8):e198340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA 2002;288:756–64. [DOI] [PubMed] [Google Scholar]
- 18.Jefferson L, Bloor K, Birks Y, Hewitt C, Bland M. Effect of physicians’ gender on communication and consultation length: a systematic review and meta-analysis. J Health Serv Res Policy 2013;18:242–8. [DOI] [PubMed] [Google Scholar]
- 19.Roter DL, Hall JA. Physician gender and patient-centered communication: a critical review of empirical research. Annu Rev Public Health 2004;25:497–519. [DOI] [PubMed] [Google Scholar]
- 20.Valle L, Weng J, Jagsi R, et al. Assessment of differences in clinical activity and Medicare payments among female and male radiation oncologists. JAMA Netw Open 2019;2(3):e190932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen LM, Farwell WR, Jha AK. Primary care visit duration and quality: does good care take longer? Arch Intern Med 2009;169:1866–72. [DOI] [PubMed] [Google Scholar]
- 22.Zyzanski SJ, Stange KC, Langa D, Flocke SA. Trade-offs in high-volume primary care practice. J Fam Pract 1998;46: 397–402. [PubMed] [Google Scholar]
- 23.Yarnall KSH, Pollak KI, Østbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health 2003;93:635–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Østbye T, Yarnall KSH, Krause KM, Pollak KI, Gradison M, Michener JL. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med 2005;3:209–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bolen SD, Sage P, Perzynski AT, Stange KC. No moment wasted: the primary-care visit for adults with diabetes and low socio-economic status. Prim Health Care Res Dev 2016;17:18–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gross DA, Zyzanski SJ, Borawski EA, Cebul RD, Stange KC. Patient satisfaction with time spent with their physician. J Fam Pract 1998;47:133–7. [PubMed] [Google Scholar]
- 27.Lin CT, Albertson GA, Schilling LM, et al. Is patients’ perception of time spent with the physician a determinant of ambulatory patient satisfaction? Arch Intern Med 2001;161:1437–42. [DOI] [PubMed] [Google Scholar]
- 28.Goodson JD. Unintended consequences of resource-based relative value scale reimbursement. JAMA 2007;298:2308–10. [DOI] [PubMed] [Google Scholar]
- 29.Bodenheimer T, Berenson RA, Rudolf P. The primary care-specialty income gap: why it matters. Ann Intern Med 2007;146: 301–6. [DOI] [PubMed] [Google Scholar]
- 30.Ginsburg PB, Patel KK. Physician payment reform — progress to date. N Engl J Med 2017;377:285–92. [DOI] [PubMed] [Google Scholar]
- 31.MedPAC. Physician and other health professional payment system. Payment Basics. October 2019. (http://medpac.gov/docs/default-source/payment-basics/medpac_payment_basics_19_physician_final_sec.pdf?sfvrsn=0).
- 32.Roter DL, Hall JA. Why physician gender matters in shaping the physician-patient relationship. J Womens Health 1998;7:1093–7. [DOI] [PubMed] [Google Scholar]
- 33.Linzer M, Harwood E. Gendered expectations: do they contribute to high burnout among female physicians? J Gen Intern Med 2018;33:963–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schmid Mast M, Hall JA, Roter DL. Disentangling physician sex and physician communication style: their effects on patient satisfaction in a virtual medical visit. Patient Educ Couns 2007;68:16–22. [DOI] [PubMed] [Google Scholar]
- 35.Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. J Gen Intern Med 1999;14:Suppl 1: S34–S40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Linzer M, Manwell LB, Williams ES, et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med 2009;151:28–36. [DOI] [PubMed] [Google Scholar]
- 37.Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med 2017;15:419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lasker RD, Marquis MS. The intensity of physicians’ work in patient visits — implications for the coding of patient evaluation and management services. N Engl J Med 1999;341:337–41. [DOI] [PubMed] [Google Scholar]
- 39.Gupta K, Murray SG, Sarkar U, Mourad M, Adler-Milstein J. Differences in ambulatory EHR use patterns for male vs. female physicians. NEJM Catalyst. November 13, 2019. (https://catalyst.nejm.org/ambulatory-ehr-patterns-physician-gender/). [Google Scholar]
- 40.Rama A Policy research perspectives: how are physicians paid? A detailed look at the methods used to compensate physicians in different practice types and specialties. Chicago: American Medical Association, 2018. (https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/member/health-policy/prp-how-physicians-paid.pdf). [Google Scholar]
- 41.Rao A, Shi Z, Ray KN, Mehrotra A, Ganguli I. National trends in primary care visit use and practice capabilities, 2008–2015. Ann Fam Med 2019;17:538–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rule A, Chiang MF, Hribar MR. Using electronic health record audit logs to study clinical activity: a systematic review of aims, measures, and methods. J Am Med Inform Assoc 2020;27:480–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Friedberg MW, Hussey PS, Schneider EC. Primary care: a critical review of the evidence on quality and costs of health care. Health Aff (Millwood) 2010;29:766–72. [DOI] [PubMed] [Google Scholar]
- 44.Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care — two essential elements of delivery-system reform. N Engl J Med 2009;361:2301–3. [DOI] [PubMed] [Google Scholar]
- 45.Trowbridge E, Bartels CM, Koslov S, Kamnetz S, Pandhi N. Development and impact of a novel academic primary care compensation model. J Gen Intern Med 2015;30:1865–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rajkomar A, Yim JWL, Grumbach K, Parekh A. Weighting primary care patient panel size: a novel electronic health record-derived measure using machine learning. JMIR Med Inform 2016;4(4):e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.