Abstract
Simple Summary
This study focused on identifying and evaluating the use of selected potential biomarkers in predicting the treatment response of mast cell tumours (MCT) in dogs using a combination of electrochemotherapy (ECT) and interleukin 12 gene electrotransfer (IL-12 GET). In the study of 48 patients with 86 MCTs, blood samples were taken before, one month and six months after treatment to identify reliable biomarkers that predict response to treatment. An increased plasma nucleosome concentration and increased serum lactate dehydrogenase (LDH) activity one month after treatment correlated with a more effective local response, such as necrosis and swelling. These biomarkers proved to be potential early indicators of treatment success. However, the serum ferritin concentration did not prove to be meaningful. The results of this study provide crucial insights into the use of the plasma nucleosome concentration and serum LDH activity as potential indicators of treatment efficacy in veterinary oncology. Ultimately, this study emphasises the need to identify and validate predictive biomarkers to improve treatment outcomes in dogs with MCT and other malignancies treated similarly.
Abstract
Electrochemotherapy (ECT) in combination with the gene electrotransfer of interleukin 12 (IL-12 GET) has been successfully used in veterinary medicine for the treatment of mast cell tumours (MCT), but the biomarkers that could predict response to this treatment have not yet been investigated. The aim of this study was to determine the plasma nucleosome and serum ferritin concentrations, as well as the lactate dehydrogenase (LDH) activity, in the serum of treated patients before and one and six months after treatment to evaluate their utility as potential biomarkers that could predict response to the combined treatment. The study was conducted in 48 patients with a total of 86 MCTs that we treated with the combined treatment. The blood samples used for analysing the potential predictive biomarkers were taken before treatment and one and six months after treatment, when the response to treatment was also assessed. The Nu. Q® Vet Cancer Test, the Canine Ferritin ELISA Kit, and the RX Daytona+ automated biochemical analyser were used to analyse the blood samples. The results showed that the plasma nucleosome concentration (before treatment (BT): 32.84 ng/mL (median); one month after treatment (1 M AT): 58.89 ng/mL (median); p = 0.010) and serum LDH activity (BT: 59.75 U/L (median); 1 M AT: 107.5 U/L (median); p = 0.012) increased significantly one month after treatment and that the increase correlated significantly with the presence of a more pronounced local reaction (necrosis, swelling, etc.) at that time point for both markers (nucleosome: BT (necrosis): 21.61 ng/mL (median); 1 M AT (necrosis): 69.92 ng/mL (median), p = 0.030; LDH: BT (necrosis): 54.75 U/L (median); 1 M AT (necrosis): 100.3 U/L (median), p = 0.048). Therefore, both the plasma nucleosome concentration and serum LDH activity could serve as early indicators of the effect of the treatment. In this context, the serum ferritin concentration showed no significant predictive potential for treatment response (p > 0.999 for all comparisons). In conclusion, this study provides some new and important observations on the use of predictive biomarkers in veterinary oncology. Furthermore, it emphasises the need for the continued identification and validation of potential predictive biomarkers in dogs with MCT and other malignancies undergoing ECT treatment in combination with IL-12 GET to ultimately improve treatment outcomes.
Keywords: electrochemotherapy, gene electrotransfer, interleukin 12, mast cell tumour, biomarkers, nucleosomes, ferritin, lactate dehydrogenase
1. Introduction
Several studies have been published in which electrochemotherapy (ECT) or a combination of ECT with the gene electrotransfer of interleukin 12 (IL-12 GET) has been successfully used to treat various canine neoplasms such as mast cell tumours (MCT), squamous cell carcinomas, acanthomatous ameloblastomas, perianal tumours and oral malignant melanomas [1,2,3,4,5,6,7]. In human medicine, ECT has proven to be an effective treatment method for various primary malignancies and metastatic diseases. Its application goes beyond the treatment of skin and subcutaneous lesions when combined with imaging and endoscopic procedures, or when used in the treatment of vascular malformations [8,9,10,11].
The basic mechanism of ECT is electroporation, which uses high-voltage pulses to temporarily and reversibly break the cell membrane barrier. This allows larger molecules, such as DNA, to be introduced into the cells. When electroporation is used for the local treatment of tumours by enhancing the toxicity of chemotherapeutic agents, it is called electrochemotherapy. This is an ablative technique that causes the reversible permeability of the cell membrane so that chemotherapeutic agents such as cisplatin and bleomycin can penetrate the tumour cells and cause immunogenic cell death and the activation of the immune cell response [1,6,9,10,12,13]. Recent studies indicate that ECT also has a systemic remote effect on untreated tumours [10,13,14,15,16]. It induces immunogenic cell death, leading to the release of tumour antigens and educating immune cells, resulting in a systemic effect. When ECT is combined with IL-12 GET immunotherapy, which has also shown a systemic remote effect, the overall effect can be enhanced. This enhancement has been demonstrated in preclinical studies in mice, as well as in clinical studies in veterinary and human oncology [1,3,6,15,17,18,19].
Mast cell tumours are the abnormal growth of mast cells. In dogs, MCTs account for 16–21% of all skin neoplasms and can occur in various parts of the body, with cutaneous and subcutaneous sites being the most common [12,20]. Several clinical studies in veterinary oncology have shown that the treatment of various canine cutaneous, subcutaneous and oral tumours, including MCTs, with ECT alone or in combination with IL-12 GET results in a high percentage of long-lasting objective responders (i.e., animals that had a complete or partial response to treatment, according to RECIST criteria [21]) [1,3,6,22]. Currently, decision making regarding treatment in ECT practice is guided by clinical factors such as the tumour histiotype, tumour size and previous treatments, while there are no known biomarkers that could predict the response to treatment [23].
Biomarkers are defined as indicators of normal biological processes, pathogenic processes or responses to an exposure or intervention, including therapeutic interventions. Based on their clinical use, biomarkers can be categorised as susceptibility or risk, diagnostic, monitoring, prognostic, predictive, pharmacodynamic or response and safety biomarkers [24]. Currently, the most commonly used method for the identification and analysis of biomarkers in oncology is tumour biopsy [23]. As biopsies can be invasive and expensive, and can increase the risk of adverse events, the search for biomarkers in peripheral blood for clinical utility is the next logical step [25]. Biomarkers that could predict the response to treatment of different tumours with ECT or the combination of ECT with IL-12 GET have not yet been investigated in veterinary oncology. Nucleosome and ferritin concentrations and the LDH activity in blood have been shown to be valuable diagnostic biomarkers for various malignancies in animals [26,27,28,29,30,31,32,33,34,35].
Nucleosomes are important components of chromosomes and consist of DNA wrapped around nuclear histones. They perform several functions, including condensing chromatin, protecting DNA, and regulating genes by restricting the binding of transcription factors. While nucleosomes are present in all mammalian cells, they can also be found in the bloodstream and are normally released by activated or dying white blood cells [36]. Severe inflammation or trauma results in the significant release of nucleosomes [37,38,39]. Elevated nucleosome concentrations have been observed in humans and dogs in different malignancies, suggesting that nucleosomes may serve as biomarkers for the early detection of the disease [35,36,40,41,42]. In addition, nucleosomes, their core components histones, and other proteins are the integral constituents of liquid biopsies, a new approach to cancer detection and monitoring [43,44].
Ferritin, a protein involved in intracellular iron storage and cell protection, is found in high concentrations in the liver, spleen, and bone marrow of mammals [45,46,47]. High serum ferritin levels are influenced by conditions such as iron overload, inflammatory diseases, liver damage and malignant tumours [48]. Malignant tumours have been shown to produce and release ferritin, leading to an increase in serum ferritin levels [26,49]. Elevated serum ferritin levels have also been observed in clinical studies in tumour patients and have been attributed to reduced iron utilisation during tumour development [29,50]. In veterinary medicine, elevated serum ferritin concentrations are observed in dogs with lymphomas, histiocytic sarcomas, mammary tumours, immune-mediated haemolytic anaemia (IMHA) and liver disease [26,27,28,29].
Lactate dehydrogenase (LDH), present in five isoenzymes, is a ubiquitous glycolytic enzyme involved in the metabolism of glucose and the production of lactate [51]. The production of lactate plays a significant role in the malignant progression of cancer by facilitating tumour cell migration and invasion, promoting angiogenesis, and causing the suppression of immunity [52]. Elevated serum LDH activity is thought to reflect high metabolic activity in the hypoxic and highly active cellular environment of malignant tumours [30,31]. Studies in human and veterinary medicine have shown a significant increase in serum LDH activity in patients with lymphomas, leukaemias, mammary gland tumours and oral cavity tumours, especially oral malignant melanoma [30,31,32,33,34].
As far as the authors are aware, the relationship between the effectiveness of treatment with ECT and IL-12 GET and the levels of nucleosomes, ferritin or LDH has not yet been studied in veterinary medicine. The aim of this study was therefore to investigate the possible changes in the plasma nucleosome and serum ferritin concentrations, as well as in the serum LDH activity, before and after the combined treatment of MCT with ECT and IL-12 GET in dogs in relation to the clinical response.
2. Materials and Methods
This study included 48 dogs (Table 1) that presented to the Small Animal Clinic of the Veterinary Faculty in Ljubljana with 86 MCTs and were enrolled in a clinical study entitled “Monitoring of clinical and immune response to improve the outcome of combined ECT and IL-12 GET in dogs with spontaneous peripheral tumours” between April 2021 and July 2023. The clinical trial was approved by the Ethics Committee of the Ministry of Agriculture, Forestry, and Food of the Republic of Slovenia (approval no. 254-20/2015/7, and permit for the deliberate release of genetically modified organisms 35419/2021-2550-8). All dogs included in this study met the inclusion criteria, i.e., they had to have at least one cytologically or histopathologically diagnosed peripheral (cutaneous, subcutaneous or mucosal) MCT and an anticipated life expectancy of more than three months. Patients who had received systemic chemotherapy or tyrosine kinase inhibitors (masitinib or toceranib) in the previous 14 days and patients with evidence of other systemic disease (renal insufficiency, cardiovascular disease) at the time of inclusion were excluded. Pregnancy or lactation were also excluding criteria. The determination of whether other systemic diseases were present was based on a comprehensive assessment that included the patients’ medical history, clinical examination findings, haematological and biochemical analysis results and, if indicated, diagnostic imaging. Written informed consent was obtained from the owner of each animal prior to participation in the clinical trial.
Disease staging was performed at inclusion and consisted of a clinical examination of the patient, a basic haematological and biochemical examination, and an assessment of the size and growth pattern of each MCT and the number of MCTs present. In addition, the regional lymph nodes were palpated, and a fine needle biopsy and cytology were performed on the liver and spleen and on suspicious lymph nodes if clinically indicated. The samples for cytological and pathohistological analysis were forwarded to the Laboratory for Pathoanatomical Diagnostics and Pathohistology of the Veterinary faculty in Ljubljana. The samples were analysed by one of the non-board-certified experienced pathologists on duty.
Based on this information, animals were categorised into five stages, in accordance with the proposed amendment to the WHO clinical staging for canine MCT [53]. In patients where tumour biopsy and histopathology were performed, MCT was graded according to both the Kiupel and Patnaik schemes [54,55]. The sample used for pathohistological grading was a four-millimetre punch biopsy (MedGyn Disposable Punch 4 mm. MedGyn, Addison, IL, USA) that was performed prior to treatment. In cases where an animal had several tumours, only one tumour was preferably sampled, with the largest tumour usually selected for sampling and grading. Furthermore, blood samples were taken from the included dogs at various time points to determine the plasma nucleosome and serum ferritin concentrations, as well as the serum LDH activity.
Table 1.
Demographic data for included patients.
| Patient Number | Breed | Sex | Age [Years] | Site of the Tumours | Histopathological Grade * | Clinical Stage ** | Longest Diameter of the Tumour [cm] (Tumor Volume) |
|---|---|---|---|---|---|---|---|
| 1 | Boxer | F | 6.3 | Left hind leg | ND | I | 2.2 (3.63 cm3) |
| 2 | Miniature Schnauzer | F | 11.3 | Left front leg | ND | I | 2.1 (2.78 cm3) |
| 3 | Crossbreed | F | 7.7 | Left front leg | ND | I | 2.3 (4.12 cm3) |
| 4 | Boxer | F | 9.8 | Right inguinal region | II (low) | I | 4.0 (17.42 cm3) |
| 5 | Boston Terrier | M | 10.4 | Right hind leg | ND | II | 1.5 (0.78 cm3) |
| Right scapula | 0.7 (0.11 cm3) | ||||||
| Left hind leg | 1.9 (3.40 cm3) | ||||||
| Left inguinal region | 0.5 (0.07 cm3) | ||||||
| 6 | French Bulldog | F | 10.0 | Right hind leg | II (low) | I | 1.6 (1.09 cm3) |
| 7 | Golden Retriever | F | 3.4 | Left scapula | ND | I | 1.2 (0.76 cm3) |
| 8 | Crossbreed | F | 11.1 | Right dorsum | ND | I | 1.7 (1.49 cm3) |
| 9 | Crossbreed | F | 9.9 | Left hind leg | ND | I | 2.0 (2.93 cm3) |
| 10 | Dogo Argentino | F | 6.8 | Right front leg | ND | I | 3.8 (13.72 cm3) |
| 11 | Dachshund | M | 11.0 | Left ear | ND | II | 0.5 (0.07 cm3) |
| Dorsal part of the neck | 0.5 (0.07 cm3) | ||||||
| Right abdominal region | 0.5 (0.07 cm3) | ||||||
| Perianal region | 0.8 (0.17 cm3) | ||||||
| 12 | Crossbreed | M | 10.2 | Prepuce | I (low) | I | 0.5 (0.07 cm3) |
| 13 | Jack Russell Terrier | M | 7.8 | Left front leg | II (low) | I | 5.0 (0.05 cm3) |
| Right lip commissure | 0.8 (0.27 cm3) | ||||||
| 14 | Crossbreed | F | 6.6 | Dorsum | ND | II | 0.4 (0.33 cm3) |
| Left abdominal region | 0.4 (0.33 cm3) | ||||||
| Left hind leg | 0.5 (0.07 cm3) | ||||||
| Left hind leg | 0.5 (0.07 cm3) | ||||||
| Tail base | 1.1 (0.70 cm3) | ||||||
| Vulva | 0.4 (0.33 cm3) | ||||||
| 15 | Boston Terrier | F | 7.2 | Left elbow | ND | I | 1.2 (0.53 cm3) |
| 16 | Manchester Terrier | F | 8.2 | Right inguinal region | ND | I | 2.8 (3.62 cm3) |
| 17 | Golden Retriever | F | 7.7 | Chin | II (low) | II | 1.5 (0.78 cm3) |
| Right thoracic region | 1.0 (0.52 cm3) | ||||||
| Right hind leg | 0.5 (0.04 cm3) | ||||||
| Right hind leg | 0.6 (0.09 cm3) | ||||||
| 18 | English Greyhound | M | 4.7 | Perianal region | II (low) | I | 1.4 (0.88 cm3) |
| 19 | Greater Swiss Mountain Dog | F | 3.3 | Left hind leg | II (low) | I | 2.3 (3.71 cm3) |
| 20 | Boston Terrier | M | 8.9 | Left abdominal region | ND | II | 2.4 (1.32 cm3) |
| Left front leg | 0.5 (0.07 cm3) | ||||||
| Right hind leg | 2.2 (0.69 cm3) | ||||||
| 21 | Shih Tzu | M | 6.5 | Right hind leg | II (low) | I | 2.0 (1.63 cm3) |
| 22 | French Bulldog | M | 6.0 | Right orbital region | II (low) | II | 0.8 (0.20 cm3) |
| Perianal region | 0.7 (0.07 cm3) | ||||||
| Perianal region | 1.3 (0.12 cm3) | ||||||
| Right hind leg | 0.3 (0.01 cm3) | ||||||
| 23 | Boston Terrier | M | 6.1 | Right front leg | ND | II | 1.0 (0.42 cm3) |
| Left front leg | 0.5 (0.07 cm3) | ||||||
| Sternal region | 0.5 (0.07 cm3) | ||||||
| Right orbital region | 0.5 (0.07 cm3) | ||||||
| 24 | Newfoundland | M | 8.6 | Right hind leg | ND | I | 1.3 (0.60 cm3) |
| 25 | Boston Terrier | M | 8.4 | Prepuce | II (low) | II | 1.1 (0.06 cm3) |
| Right hind leg | 1.1 (0.02 cm3) | ||||||
| Perianal region | 1.2 (0.28 cm3) | ||||||
| Right abdominal region | 1.1 (0.23 cm3) | ||||||
| 26 | French Bulldog | M | 6.2 | Prepuce | II (low) | I | 1.5 (1.12 cm3) |
| 27 | Hungarian Vizsla | F | 9.9 | Right ear | II (low) | I | 1.2 (0.28 cm3) |
| 28 | Boxer | M | 5.8 | Left ear | II (low) | I | 1.1 (0.29 cm3) |
| 29 | Pit bull | M | 8.3 | Left abdominal region | II (low) | I | 1.5 (0.55 cm3) |
| 30 | Crossbreed | F | 12.2 | Left thoracic region | ND | II | 0.5 (0.07 cm3) |
| Left thoracic region | 0.5 (0.07 cm3) | ||||||
| Left hind leg | 0.5 (0.07 cm3) | ||||||
| Right ear | 0.2 (0.004 cm3) | ||||||
| Right thoracic region | 0.5 (0.07 cm3) | ||||||
| Left inguinal region | 0.5 (0.07 cm3) | ||||||
| 31 | Havanese | F | 9.3 | Left hind leg | II (low) | I | 1.0 (0.25 cm3) |
| 32 | Maltese | F | 10.8 | Tail | ND | I | 0.9 (0.20 cm3) |
| 33 | Boston Terrier | F | 8.4 | Right front leg | ND | I | 1.8 (1.60 cm3) |
| 34 | French Bulldog | M | 8.7 | Left hind leg | II (low) | II | 1.7 (1.99 cm3) |
| Left hind leg | 0.7 (0.18 cm3) | ||||||
| Scrotum | 0.9 (0.38 cm3) | ||||||
| Prepuce | 0.9 (0.38 cm3) | ||||||
| Left front leg | 0.7 (0.18 cm3) | ||||||
| 35 | French Bulldog | M | 5.5 | Prepuce | II (low) | I | 1.0 (0.37 cm3) |
| Right hind leg | 0.8 (0.27 cm3) | ||||||
| 36 | Boxer | M | 8.3 | Right front leg | II (low) | I | 4.0 (8.29 cm3) |
| 37 | Boxer | M | 7.6 | Right abdominal region | II (low) | I | 1.5 (1.53 cm3) |
| Perianal region | 2.0 (3.77 cm3) | ||||||
| 38 | Boxer | F | 8.8 | Right lip corner | Subcutaneous | I | 1.5 (1.12 cm3) |
| 39 | Yorkshire Terrier | F | 13.6 | Left front leg | ND | I | 1.1 (0.06 cm3) |
| Left front leg | 1.1 (0.02 cm3) | ||||||
| 40 | Crossbreed | F | 10.7 | Frontal region | ND | III | 2.5 (3.14 cm3) |
| 41 | Boxer | M | 5.2 | Left ear | II (low) | I | 1.0 (0.33 cm3) |
| 42 | Boxer | F | 6.4 | Left hind leg | Subcutaneous | I | 2.2 (3.29 cm3) |
| 43 | French Bulldog | F | 2.5 | Perianal region | II (low) | I | 1.0 (0.42 cm3) |
| 44 | Boxer | M | 4.1 | Right hind leg | II (low) | I | 1.0 (0.42 cm3) |
| 45 | Crossbreed | F | 11.5 | Left axillary region | II (high) | III | 3.7 (14.33 cm3) |
| 46 | Crossbreed | F | 7.0 | Right hind leg | Subcutaneous | III | 2.0 (2.35 cm3) |
| 47 | Maltese | F | 7.4 | Right lip commissure | MCT mucosae labie | I | 1.5 (0.47 cm3) |
| 48 | Boston Terrier | F | 7.4 | Right hind leg | II (high) | I | 1.8 (1.27 cm3) |
2.1. Blood Sampling and Processing
The blood samples to be used for serum and plasma preparation were collected from the included patients before the start of therapy and four weeks after therapy. The collection of samples at six months post treatment depended on the treatment response and possible re-treatment, owner compliance and the time of inclusion in this study. At each sampling, we collected five millilitres of venous blood into two micro sample tubes containing the anticoagulant sodium citrate (Sarstedt AG & Co. KG, Nümbrecht, Germany) and one serum separation tube (Jørgen Kruuse A/S, Langeskov, Denmark). After centrifugation, the serum and plasma were harvested and aliquoted. The serum samples were stored at −20 °C and the plasma samples at −80 °C until later batch analyses.
2.2. Treatment Protocol
All dogs were treated with a combination of ECT and IL-12 GET using the previously described plasmid for canine IL-12 without the antibiotic resistance gene (pORFcaIL-12-ORT, COBIK, Ajdovscina, Slovenia) [56]. On the day of treatment, they were examined by an anaesthesiologist and placed under general anaesthesia as previously described [3]. An abdominal ultrasound with an ultrasound-guided fine needle biopsy of the spleen and liver was performed as part of the staging of the disease. The cytostatic drug used in the treatment protocol was either cisplatin (Cisplatin Accord, Accord Health Care, London, UK) or bleomycin (Bleomycin Medac, Medac GmbH, Hamburg, Germany). Cisplatin was the first-line cytostatic drug, but replaced by bleomycin if multiple tumours were present, if the tumour was ulcerated or bleeding, or if the animal had been previously treated with cisplatin and did not respond adequately [6]. The treated tumours were measured in three dimensions using a calliper and the tumour volume was calculated using the following formula: V = a × b × c × π/6 [3]. When cisplatin (1 mg/mL) was used, the drug was administered intratumorally (i.t.) one minute before electroporation at a dose of 1 mg/cm3 for tumours smaller than 1 cm3 and 0.5 mg/cm3 for tumours larger than 1 cm3. When bleomycin was used, the drug was dissolved at a concentration of 3 mg/mL and administered intravenously at a dose of 0.3 mg/kg eight minutes before electroporation [6]. Plasmid DNA with IL-12 was administered intratumorally five minutes before electroporation, regardless of the cytostatic drug chosen. An electroporation protocol with eight electrical pulses, a 100 µs duration, a 1300 V/cm ratio and a 5 kHz frequency, was performed using the Cliniporator™ pulse generator (IGEA s.r.l., Carpi, Italy). Depending on the tumour size, stainless steel plate electrodes (6 mm spacing), needle electrodes (4 mm spacing) or hexagonal electrodes were used. The delivery of a sequential pulse from the tumour edge towards the centre reduced the blood flow, resulting in vascular lock and the better retention of the chemotherapeutic agent in the tumour nodule [57].
2.3. Evaluation of Treatment Outcome
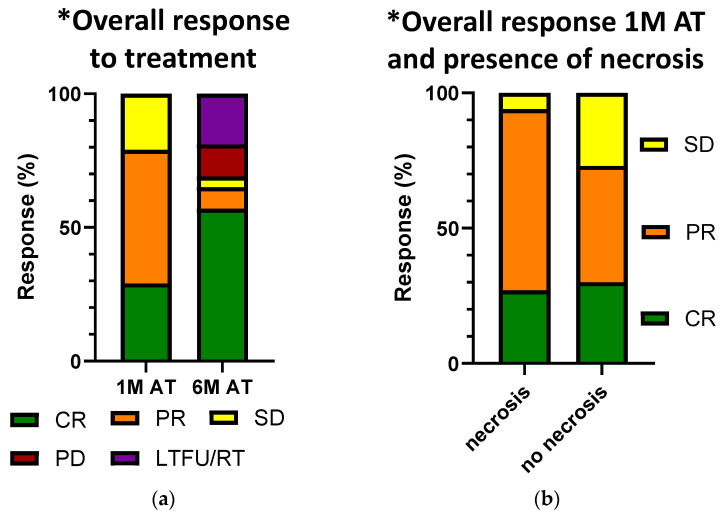
After the treatment, the follow-up visits were scheduled at one week, four weeks, two months, three months, and six months after the treatment, based on previously described operating procedures [57]. At each visit, the dogs were clinically examined, the treatment site was thoroughly inspected, any residual tumours were measured with a calliper and the treatment site was photographed. The owners were interviewed about the dog’s general well-being and response to therapy. In line with the protocol described above, blood was drawn again four weeks after therapy, in some patients also six months after therapy (Table 2), and stored accordingly. However, patients who did not respond satisfactorily to their initial treatment and required re-treatment during the observation period were excluded from sampling at the six-month follow up. In some cases, owners declined the six-month follow-up due to a positive response to treatment and considered the appointment unnecessary. In addition, patients enrolled in the study after February 2023 were not sampled at the six-month follow-up because the batch and statistical analyses were completed in July 2023, which was prior to their scheduled six-month follow-up. The patients’ response to therapy was determined according to the RECIST criteria (Table 3): complete response (CR), i.e., disappearance of the tumour; partial response (PR), i.e., reduction in the tumour by at least 30%; stable disease (SD), i.e., reduction in the tumour by less than 30% or enlargement by less than 20%; and progressive disease (PD), i.e., enlargement of the tumour by at least 20% [21]. Some of the patients (15/48) reacted more conspicuously to the treatment than others, with the occurrence of tissue swelling, redness, an open wound or enhanced tumour necrosis in the treated area, which may have been due to the inflammatory process triggered by the combined treatment. This response was observed and visually assessed by one of three veterinarians that were conducting the clinical examination of the treated animals in this study. When assessing the response to treatment in patients with multiple treated tumours, the response was recorded for each individual tumour site. The least favourable response was considered to determine the overall response for the assessment of potential biomarkers that may correlate with the presence of disease (Figure 1a). This approach is based on the consideration that if one of the treated sites still shows signs of the disease, this could have a systemic impact on the potential biomarkers tested in the blood.
Table 2.
List of patients in whom the nucleosome and ferritin concentrations and LDH activity were determined.
| Patient Number | Nucleosomes | Ferritin | LDH | Patient Number | Nucleosomes | Ferritin | LDH | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 and 1 M | 6 M | 0 and 1 M | 6 M | 0 and 1 M | 6 M | 0 and 1 M | 6 M | 0 and 1 M | 6 M | 0 and 1 M | 6 M | ||
| 1 | ✓ | ✓ | ✓ | ✓ | ✓ | 25 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 2 | ✓ | ✓ | ✓ | 26 | ✓ | ✓ | ✓ | ||||||
| 3 | ✓ | ✓ | ✓ | 27 | ✓ | ✓ | ✓ | ||||||
| 4 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 28 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 5 | ✓ | ✓ | ✓ | 29 | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| 6 | ✓ | ✓ | ✓ | 30 | ✓ | ✓ | ✓ | ||||||
| 7 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 31 | ✓ | ✓ | ✓ | |||
| 8 | ✓ | ✓ | ✓ | 32 | ✓ | ✓ | |||||||
| 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 33 | ✓ | ✓ | ✓ | |||
| 10 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 34 | ✓ | ✓ | ||||
| 11 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 35 | ✓ | ✓ | ✓ | |||
| 12 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 36 | ✓ | ✓ | ✓ | |||
| 13 | ✓ | ✓ | ✓ | ✓ | 37 | ✓ | ✓ | ✓ | |||||
| 14 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 38 | ✓ | ✓ | ✓ | |||
| 15 | ✓ | ✓ | ✓ | ✓ | ✓ | 39 | ✓ | ✓ | |||||
| 16 | ✓ | ✓ | ✓ | ✓ | 40 | ✓ | ✓ | ||||||
| 17 | ✓ | ✓ | 41 | ✓ | ✓ | ||||||||
| 18 | ✓ | ✓ | 42 | ✓ | |||||||||
| 19 | ✓ | ✓ | ✓ | ✓ | 43 | ✓ | ✓ | ||||||
| 20 | ✓ | ✓ | ✓ | ✓ | 44 | ✓ | ✓ | ||||||
| 21 | ✓ | ✓ | ✓ | 45 | ✓ | ||||||||
| 22 | ✓ | ✓ | ✓ | 46 | ✓ | ||||||||
| 23 | ✓ | ✓ | ✓ | ✓ | 47 | ✓ | |||||||
| 24 | ✓ | ✓ | ✓ | ✓ | ✓ | 48 | ✓ | ||||||
LDH, lactate dehydrogenase; 0 and 1 M, the day of treatment and one month after treatment; 6 M, six months after treatment; ✓, blood sampling and determination of potential biomarker.
Table 3.
Tumour response one- and six-months post treatment and overall response one- and six-months post treatment.
| Patient Number |
Site of the Tumours | Tumour Response One Month Post Treatment | Tumour Response Six Months Post Treatment | Overall Response One Month Post Treatment | Overall Response Six Months Post Treatment | Necrosis Observed at One Month Post Treatment |
|---|---|---|---|---|---|---|
| 1 | Left hind leg | SD | PR | SD | PR | ✓ |
| 2 | Left front leg | PR | PD | PR | PD | ✓ |
| 3 | Left front leg | PR | PD | PR | PD | ✓ |
| 4 | Right inguinal region | CR | CR | CR | CR | ✓ |
| 5 | Right hind leg | PR | CR | PR | SD | |
| Right scapula | PR | CR | ||||
| Left hind leg | PR | RT | ||||
| Left inguinal region | PR | CR | ||||
| 6 | Right hind leg | SD | RT | SD | RT | |
| 7 | Left scapula | CR | CR | CR | CR | |
| 8 | Right dorsum | PR | RT | PR | RT | |
| 9 | Left hind leg | PR | CR | PR | CR | |
| 10 | Right front leg | CR | CR | CR | CR | ✓ |
| 11 | Left ear | CR | CR | CR | CR | |
| Dorsal part of the neck | CR | CR | ||||
| Right abdominal region | CR | CR | ||||
| Perianal region | CR | CR | ||||
| 12 | Prepuce | CR | CR | CR | CR | |
| 13 | Left front leg | CR | CR | CR | CR | ✓ |
| Right lip commissure | CR | CR | ||||
| 14 | Dorsum | CR | CR | CR | CR | |
| Left abdominal region | CR | CR | ||||
| Left hind leg | CR | CR | ||||
| Left hind leg | CR | CR | ||||
| Tail base | CR | CR | ||||
| Vulva | CR | CR | ||||
| 15 | Left elbow | CR | CR | CR | CR | |
| 16 | Right inguinal region | PR | CR | PR | CR | ✓ |
| 17 | Chin | SD | RT | SD | RT | |
| Right thoracic region | CR | CR | ||||
| Right hind leg | SD | RT | ||||
| Right hind leg | CR | CR | ||||
| 18 | Perianal region | CR | PD | CR | PD | |
| 19 | Left hind leg | PR | CR | PR | CR | |
| 20 | Left abdominal region | PR | PR | PR | PR | |
| Left front leg | PR | PR | ||||
| Right hind leg | PR | PR | ||||
| 21 | Right hind leg | CR | CR | CR | CR | |
| 22 | Right orbital region | PR | LTFU | PR | LTFU | |
| Perianal region | CR | LTFU | ||||
| Perianal region | CR | LTFU | ||||
| Right hind leg | CR | LTFU | ||||
| 23 | Right front leg | PR | PR | SD | PD | |
| Left front leg | PR | CR | ||||
| Sternal region | SD | SD | ||||
| Right orbital region | PR | CR | ||||
| 24 | Right hind leg | PR | CR | PR | CR | |
| 25 | Prepuce | CR | CR | PR | CR | |
| Right hind leg | CR | CR | ||||
| Perianal region | CR | CR | ||||
| Right abdominal region | CR | CR | ||||
| 26 | Prepuce | SD | PD | SD | PD | |
| 27 | Right ear | PR | CR | PR | CR | |
| 28 | Left ear | PR | CR | PR | CR | |
| 29 | Left abdominal region | PR | CR | PR | CR | |
| 30 | Left thoracic region | CR | CR | CR | RT | |
| Left thoracic region | CR | CR | ||||
| Left hind leg | CR | CR | ||||
| Right ear | CR | CR | ||||
| Right thoracic region | CR | CR | ||||
| Left inguinal region | CR | CR | ||||
| 31 | Left hind leg | PR | CR | PR | CR | |
| 32 | Tail | CR | CR | CR | CR | |
| 33 | Right front leg | PR | CR | PR | CR | ✓ |
| 34 | Left hind leg | SD | RT | SD | RT | |
| Left hind leg | SD | RT | ||||
| Scrotum | SD | RT | ||||
| Prepuce | SD | RT | ||||
| Left front leg | SD | RT | ||||
| 35 | Prepuce | PR | CR | SD | RT | |
| Right hind leg | PR | CR | ||||
| 36 | Right front leg | PR | CR | PR | CR | ✓ |
| 37 | Right abdominal region | PR | PR | PR | PR | ✓ |
| Perianal region | PR | PR | ||||
| 38 | Right lip corner | PR | CR | PR | CR | |
| 39 | Left front leg | PR | LTFU | PR | LTFU | ✓ |
| Left front leg | PR | LTFU | ||||
| 40 | Frontal region | CR | CR | CR | CR | ✓ |
| 41 | Left ear | SD | RT | SD | RT | |
| 42 | Left hind leg | SD | SD | SD | SD | |
| 43 | Perianal region | PR | PR | PR | PR | |
| 44 | Right hind leg | PR | CR | PR | CR | |
| 45 | Left axillary region | PR | CR | PR | CR | ✓ |
| 46 | Right hind leg | PR | CR | PR | CR | ✓ |
| 47 | Right lip commissure | CR | CR | CR | CR | |
| 48 | Right hind leg | SD | PD | SD | PD |
CR, complete response; PR, partial response; SD, stable disease; PD, progressive disease; RT, re-treatment prior to response evaluation; LTFU, lost to follow-up; ✓, necrosis observed. Evaluation of response to treatment is based on the RECIST criteria [21].
Figure 1.
(a) Comparison of overall responses to treatment one month post treatment and six months post treatment. Responses were evaluated according to the RECIST criteria [21]. The graph shows a high overall response rate (CR and PR combined) one month after treatment. At six months after treatment, this rate further increases, as well as the percentage of CR, when excluding the LTFU/RT patients. CR, complete response; PR, partial response; SD, stable disease; PD, progressive disease; LTFU/RT, lost to follow-up/re-treatment; 1 M AT, one month after treatment; 6 M AT, six months after treatment. * In patients with more than one MCT, we only recorded the least favourable response to treatment; (b) correlation of overall response to treatment and presence of necrosis one month post treatment. The graph shows a higher percentage for the overall response rate (CR and PR combined) in patients where necrosis was seen at one month post treatment. CR, complete response; PR, partial response; SD, stable disease; PD, progressive disease; LTFU/RT, lost to follow-up/re-treatment; 1 M AT, one month after treatment. * In patients with more than one MCT, we only recorded the least favourable response to treatment.
2.4. Sample Analysis
2.4.1. Nucleosomes and Ferritin
The concentrations of nucleosomes and ferritin were determined from the plasma (nucleosomes) and serum (ferritin) samples using the Nu. Q® Vet Cancer Test (Belgian Volition SRL, Isnes, Belgium), a sandwich format assay for the determination of nucleosomes, and the Canine Ferritin ELISA Kit (MyBioSource, Inc., San Diego, CA, USA) for ferritin determination, according to the manufacturer’s instructions. In brief, samples were placed in wells coated with anti-H3.1 nucleosome monoclonal antibody or anti-Canine FE monoclonal antibody. The horseradish peroxidase (HRP) system was used for detection. Absorbance measurements were used to determine the concentration of H3.1 nucleosomes and ferritin in the samples.
2.4.2. Lactate Dehydrogenase
The lactate dehydrogenase activity was measured spectrophotometrically using an RX Daytona+ automated biochemical analyser (Randox, Crumlin, UK) and the Randox lactate dehydrogenase L-lactate–Pyruvate reagent kit (Randox). A brief description of the assay principle is as follows: Nicotinamide adenine dinucleotide (NAD+) and lactate are converted to pyruvate and NADH (reduced form of NAD+) at the same rate in equimolar amounts. The rate at which NADH is formed is determined by an increase in the absorbance and is directly proportional to the LDH activity. The normal range for LDH at the laboratory in which analysis was preformed is 21–217 U/L.
2.5. Statistical Analysis
Statistical analysis was performed using GraphPad Prism 10 (Systat software, London, UK). A Shapiro–Wilk test was performed to determine the distribution of the data. The data were not normally distributed; therefore, significance was determined using a Kruskal–Wallis or Wilcoxon test; p < 0.05 values were considered statistically significant. The values were expressed as medians with quartile 1 and quartile 3. The groups that were compared in the statistical analysis for ferritin, nucleosomes and LDH were marked as before treatment (BT), one month after treatment (1 M AT) and six months after treatment (6 M AT).
3. Results
In this study, we included 48 dogs with 86 MCTs treated with a combination of ECT and GET with pORFcaIL-12-ORT. We followed the patients for six months after treatment and analysed the levels of plasma and serum biomarkers.
3.1. The Percentage of Complete Responses (CR) after the Combination of ECT and IL-12 GET Increased after 6 Months
The antitumour effectiveness was evaluated one and six months after treatment (Figure 1a). The results showed that one month after treatment, the overall response rate (ORR) was 83.7%, of which 43.0% was CR and 40.7% was PR. Six months after treatment, the percentage of CR increased to 76.8% and PR changed to 11.6%, with an ORR of 88.4%, similar to observations in previously published results [6,58,59]. Seventeen tumours in eight patients could not be evaluated at six months after treatment because they had undergone repeated treatment or another treatment or were lost to follow-up (Table 3). Therefore, they were excluded from the six-month statistics. No PD was observed one month after treatment, but six months after treatment, PD was seen in five tumours (7.2%).
3.2. The Nucleosome Concentration Significantly Increased One Month after Treatment. Enhanced Tumour Necrosis Was Positively Associated with Elevations in Nucleosome Concentration One Month after Treatment
Plasma for the measurement of the nucleosome concentration was collected from 43 dogs in this study. The Nu. Q® Vet Cancer Test has a standardised reference range for plasma H3.1 nucleosome concentrations. It categorises the concentrations as high range (>67.4 ng/mL), grey zone (>30.4 and ≤67.4 ng/mL) or low range (≤30.4 ng/mL). In our study, we observed that before treatment, 23.3% of the included patients (10/43) had high concentrations of nucleosomes, 27.9% (12/43) were in the grey zone and 48.8% (21/43) were in the low range.
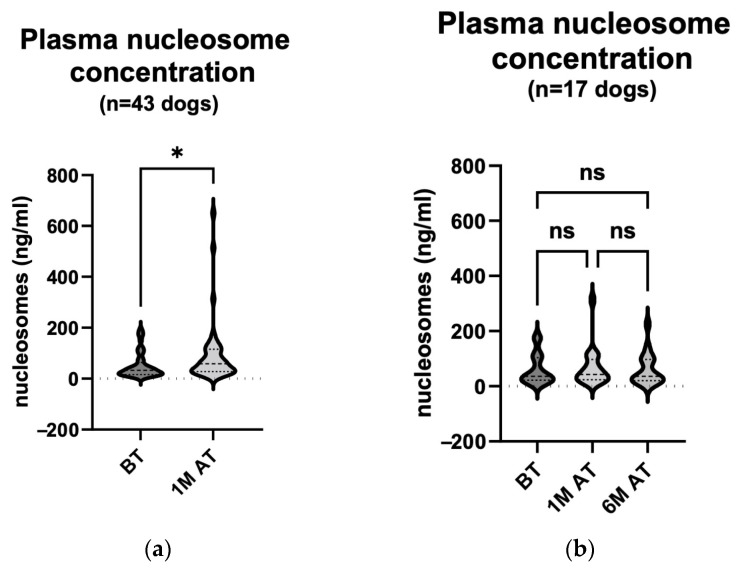
We then compared the results of the samples collected before and one month after treatment (Figure 2a). The results showed a statistically significant increase (p = 0.010) in the plasma nucleosome concentration one month after the treatment (median value 32.84 ng/mL (15.87–64.07 ng/mL) before treatment and 58.89 ng/mL (28.24–115.2 ng/mL) one month after treatment) of the tumours with a combination of ECT and IL-12 GET. Six months after treatment, only 17 patients were re-sampled for analysis (Table 2). When we compared the results before treatment (median 36.64 ng/mL (21.89–103.6 ng/mL)), one month after treatment (median 42.54 ng/mL (23.97–97.39 ng/mL)) and six months after treatment (median 36.07 ng/mL (20.00–96.90 ng/mL)), there were no statistically significant changes (p > 0.999) in the relevant comparisons (Figure 2b). When comparing only the results of the 17 dogs that were also sampled six months after treatment, the statistically significant increase in the plasma nucleosome concentration previously observed was no longer significant in a smaller number of patients.
Figure 2.
(a) Plasma nucleosome concentration comparison: pre-treatment and one-month post-treatment in 43 dogs. The concentration was measured using the Nu. Q® Vet Cancer Test on the day of the treatment and four weeks later. The analysis showed a statistically significant rise in the plasma nucleosome concentration one month following the treatment (p = 0.010). BT, before treatment; 1 M AT, one month after treatment * p < 0.05. (b) Plasma nucleosome concentration comparison: pre-treatment, one month post treatment and six months post treatment in 17 dogs. The concentration was measured using the Nu. Q® Vet Cancer Test on the day of the treatment, four weeks later and at the end of the observation period. The analysis showed no statistically notable changes in the plasma nucleosome concentration. BT, before treatment; 1 M AT, one month after treatment; 6 M AT, six months after treatment; ns, not significant (p > 0.999 for all three comparisons).
One month after the treatment of the MCTs, 12 of the 43 dogs in which the plasma nucleosome level was determined had a CR (median 21.89 ng/mL (15.00–33.17 ng/mL) before treatment and median 38.34 ng/mL (24.13–57.00 ng/mL) one month after treatment). In the remaining 31 animals, the response was either PR, SD, or PD (median 38.23 ng/mL (20.14–76.16 ng/mL) before treatment and median 67.83 ng/mL (30.00–117.2 ng/mL) one month after treatment). The latter three responses were grouped as a non-complete response (nCR) for comparison with the CR group. We found no statistically significant changes between the respective groups (Figure 3a; p: BT (CR) vs. BT (nCR) = 0.624; BT (CR) vs. 1 M AT (CR) = 0.965; BT (CR) vs. 1 M AT (nCR) = 0.008; BT (nCR) vs. 1 M AT (CR) > 0.999; BT (nCR) vs. 1 M AT (nCR) = 0.195; 1 M AT (CR) vs. 1 M AT (nCR) = 0.741).
Figure 3.
(a) Plasma nucleosome concentration comparison: pre-treatment and one month post treatment in correlation with response to treatment in 43 dogs. The concentration was measured using the Nu. Q® Vet Cancer Test on the day of treatment and four weeks later. The analysis showed no statistically remarkable changes in the plasma nucleosome concentration (p: BT (CR) vs. BT (nCR) = 0.624; BT (CR) vs. 1 M AT (CR) = 0.965; BT (CR) vs. 1 M AT (nCR) = 0.008; BT (nCR) vs. 1 M AT (CR) > 0.999; BT (nCR) vs. 1 M AT (nCR) = 0.195; 1 M AT (CR) vs. 1 M AT (nCR) = 0.741). BT, before treatment; 1 M AT, one month after treatment; CR, complete response; nCR, non-complete response (comprising of PR, SD, and PD); ns, not significant ** p < 0.01. (b) Plasma nucleosome concentration comparison: pre-treatment and one month post treatment in correlation with treatment-related enhanced tumour necrosis in 43 dogs. The concentration was measured using the Nu. Q® Vet Cancer Test on the day of treatment and four weeks later. The analysis showed a statistically remarkable rise in the plasma nucleosome concentration one month after treatment in patients where tumour necrosis was seen. BT, before treatment; 1 M AT, one month after treatment; ns, not significant (p: BT (necrosis) vs. BT (no necrosis) = 0.275; BT (necrosis) vs. 1 M AT (necrosis) = 0.030; BT (necrosis) vs. 1 M AT (no necrosis) = 0.055; BT (no necrosis) vs. 1 M AT (necrosis) > 0.999; BT (no necrosis) vs. 1 M AT (no necrosis) > 0.999; 1 M AT (necrosis) vs. 1 M AT (no necrosis) > 0.999); * p < 0.05.
Similarly, we compared the plasma nucleosome levels before and one month after treatment in the 12 dogs that responded with the enhanced necrosis of tumour tissue (median 21.61 ng/mL (15.12–45.86 ng/mL) before treatment and 69.92 ng/mL (31.94–127.2 ng/mL) one month after treatment) and in the 31 that showed no signs of necrosis (median 38.23 ng/mL (23.82–104.2 ng/mL) before treatment and 52.64 ng/mL (27.44–115.2 ng/mL) one month after treatment). In the first group, the nucleosome levels were statistically significantly elevated one month after treatment (Figure 3b; p: BT (necrosis) vs. BT (no necrosis) = 0.275; BT (necrosis) vs. 1 M AT (necrosis) = 0.030; BT (necrosis) vs. 1 M AT (no necrosis) = 0.055; BT (no necrosis) vs. 1 M AT (necrosis) > 0.999; BT (no necrosis) vs. 1 M AT (no necrosis) > 0.999; 1 M AT (necrosis) vs. 1 M AT (no necrosis) > 0.999).
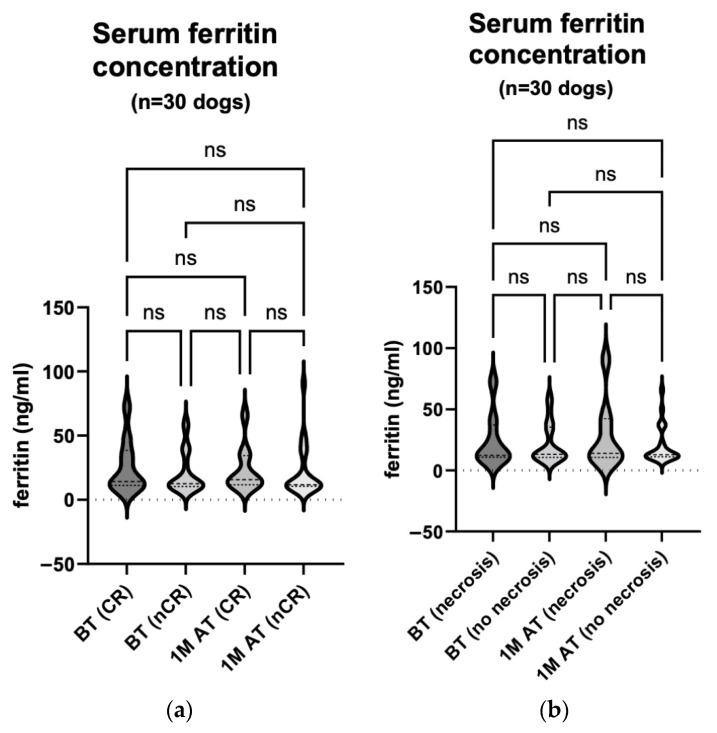
3.3. Ferritin Concentrations Did Not Correlate with Time before or after Treatment, nor with Treatment Efficacy
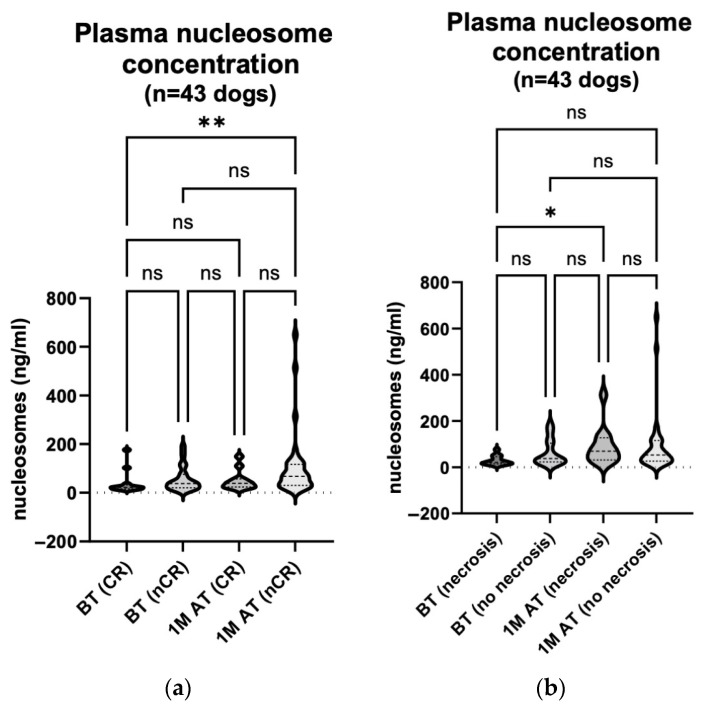
The serum ferritin concentration was measured in 30 dogs before and one month after treatment. Samples were also taken from 10 of the 30 dogs six months after treatment (Table 2). We compared the serum ferritin concentration before treatment (median 12.75 ng/mL (10.59–35.46 ng/mL)) and one month after treatment (median 12.70 ng/mL (11.13–34.39 ng/mL)) in all 30 dogs, regardless of the treatment response (Figure 4a; p = 0.667). We also compared 10 of the 30 animals before treatment (median 13.37 ng/mL (10.43–41.33 ng/mL)), one month (median 15.78 ng/mL (11.74–34.39 ng/mL)) and six months after treatment (median 12.24 ng/mL (10.26–13.95 ng/mL)). Neither comparison showed statistically significant changes in the serum ferritin concentrations (Figure 4b; p: BT vs. 1 M AT > 0.999; BT vs. 6 M AT = 0.221; 1 M AT vs. 6 M AT = 0.076).
Figure 4.
(a) Serum ferritin concentration comparison: pre-treatment and one month post treatment in 30 dogs. The concentration was measured using the Canine Ferritin ELISA Kit on the day of the treatment and four weeks later. The analysis showed no statistically significant change in the serum ferritin concentration one month following the treatment (p = 0.667). BT, before treatment; 1 M AT, one month after treatment; ns, not significant. (b) Serum ferritin concentration comparison: pre-treatment, one month post treatment and six months post treatment in 10 dogs. The concentration was measured using the Canine Ferritin ELISA Kit on the day of the treatment, four weeks later and at the end of the observation period. The analyses showed no statistically significant changes in the serum ferritin concentrations (p: BT vs. 1 M AT > 0.999; BT vs. 6 M AT = 0.221; 1 M AT vs. 6 M AT = 0.076). BT, before treatment; 1 M AT, one month after treatment; 6 M AT, six months after treatment; ns, not significant.
In addition, we compared the serum ferritin concentrations measured before treatment and one month after treatment between the animals with CR (median 14.33 ng/mL (11.19–38.44 ng/mL) before treatment and median 15.78 ng/mL (11.68–34.39 ng/mL) one month after) and the animals whose response to treatment was classified as PR, SD or PD (median 12.52 ng/mL (10.46–33.55 ng/mL) before treatment and median 11.71 ng/mL (10.65–33.40 ng/mL) one month after treatment). The latter three responses were grouped as a non-complete response (nCR) for comparison with the CR group. These comparisons did not yield statistically significant results (Figure 5a; p > 0.999 for all comparisons).
Figure 5.
(a) Serum ferritin concentration comparison: pre-treatment and one month post treatment in correlation with response to treatment in 30 dogs. The concentration was measured using the Canine Ferritin ELISA Kit on the day of treatment and four weeks later. The analyses showed no statistically remarkable changes in the serum ferritin concentrations (p > 0.999 for all comparisons). BT, before treatment; 1 M AT, one month after treatment; CR, complete response; nCR, non-complete response (comprising of PR, SD, and PD); ns, not significant. (b) Serum ferritin concentration comparison: pre-treatment and one month post treatment in correlation with treatment- related enhanced tumour necrosis in 30 dogs. The concentration was measured using the Canine Ferritin ELISA Kit on the day of treatment and four weeks later. The analyses showed no statistically remarkable changes in the serum ferritin concentrations (p > 0.999 for all comparisons). BT, before treatment; 1 M AT, one month after treatment; ns, not significant.
The enhanced necrosis of tumour tissue at the treatment site was noted in eight of the 30 dogs. We compared the serum ferritin concentrations of these 8 dogs before treatment (median 12.32 ng/mL (10.70–37.22 ng/mL)) and one month after treatment (median 13.94 ng/mL (10.56–42.34 ng/mL)) with those of the remaining 22 dogs before treatment (median 13.13 ng/mL (10.59–35.46 ng/mL)) and one month after treatment (median 12.70 ng/mL (11.13–25.85 ng/mL)); this was in order to determine whether enhanced necrosis affected the release of serum ferritin. These comparisons also revealed no statistically significant changes (Figure 5b; p > 0.999 for all comparisons).
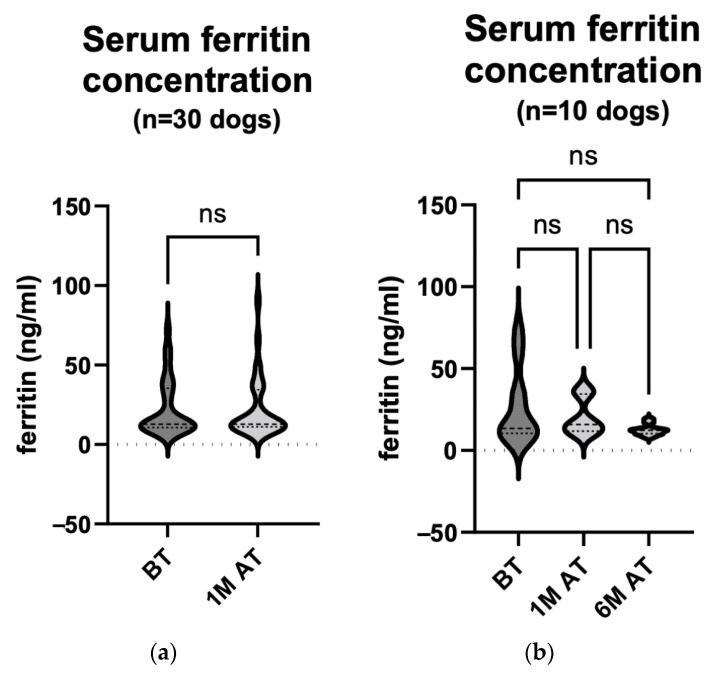
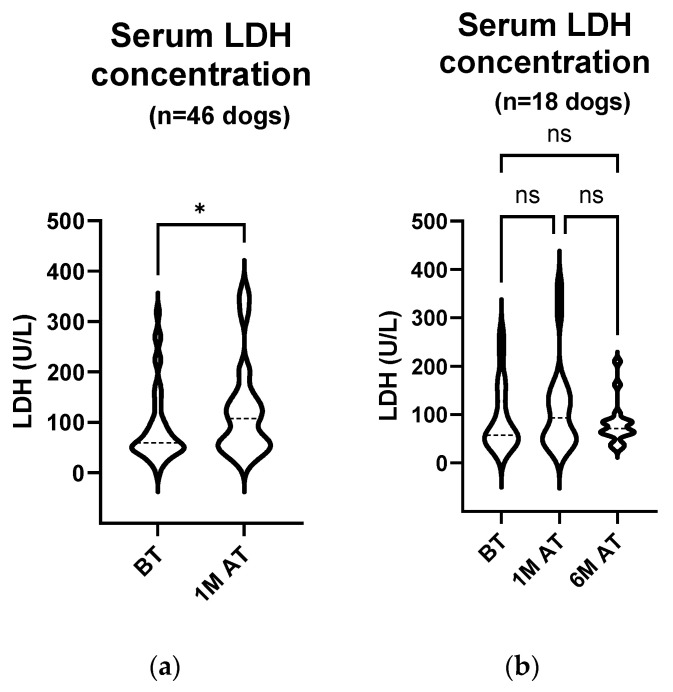
3.4. LDH Activity Increased Significantly Four Weeks after Treatment in All Patients and in Those with Treatment-Related Enhanced Tumour Necrosis
Serum from 46 dogs that participated in the study was collected before and one month after treatment to measure the LDH activity (Figure 6a). In total, 5 out of 46 dogs or 10.8% had elevated serum LDH activity before treatment. A comparison of the two groups showed a statistically significant increase in the serum LDH activity one month after treatment (median 59.75 U/L (45.75–105.0 U/L) before treatment and median 107.5 U/L (54.38–145.9 U/L) one month after treatment; p = 0.012). Samples were taken again from 18 of the 46 dogs six months after treatment (Table 2). When comparing the LDH concentrations of only these 18 animals before treatment (median 57.75 U/L (47.25–143.0 U/L)), one month (median 93.25 U/L (48.38–145.9 U/L)) and six months after treatment (median 71.00 U/L (61.63–86.63 U/L)), no statistically significant change was observed (Figure 6b; p > 0.999 for all comparisons).
Figure 6.
(a) Serum LDH activity comparison: pre-treatment and one month post treatment in 46 dogs. The enzyme activity was measured with an automated biochemical analyser on the day of treatment and four weeks later. The analyses showed a statistically significant increase in the serum LDH activity one month after treatment (p = 0.012). BT, before treatment; 1 M AT, one month after treatment; * p < 0.05. (b) Serum LDH activity comparison: pre-treatment, one month post treatment and six months post treatment in 18 dogs. The enzyme activity was measured on the day of treatment, four weeks later and at the end of the observation period using an automated biochemical analyser. The analyses showed no statistically remarkable changes in the serum LDH activity (p > 0.999 for all comparisons). BT, before treatment; 1 M AT, one month after treatment; 6 M AT, six months after treatment; ns, not significant.
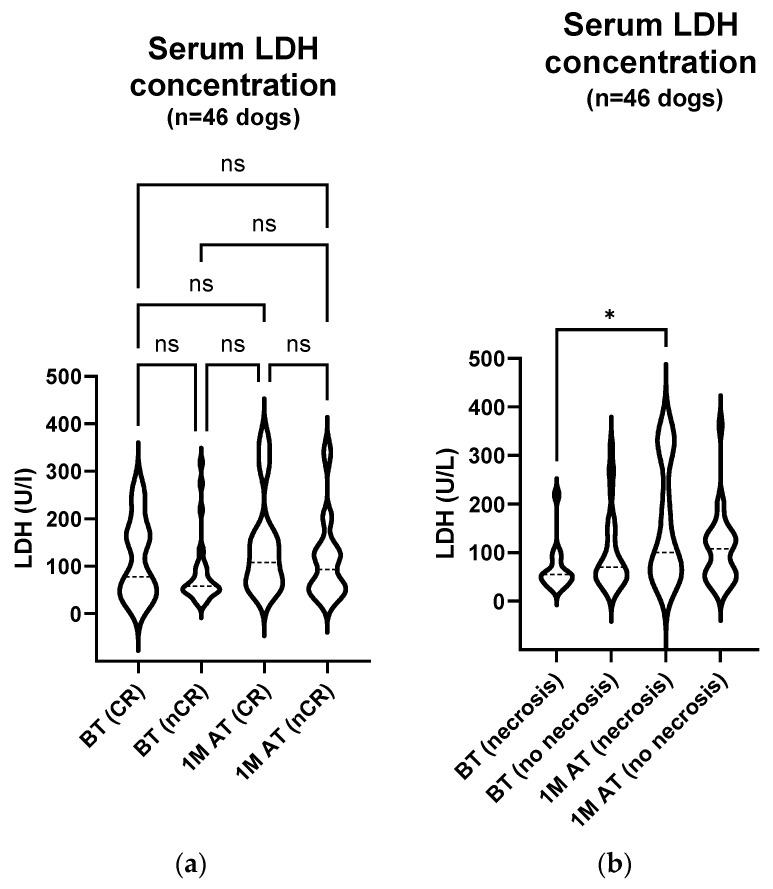
Also, the serum LDH activity before and one month post treatment was compared between the 11 dogs with CR (median 77.50 U/L (44.00–174.5 U/L) before treatment and median 108.0 U/L (65.00–171.0 U/L) one month after treatment) and the remaining 35 dogs with nCR (either PR, SD or PD) at that time point (median 58.00 U/L (46.00–91.50 U/L) before treatment and median 93.00 U/L (48.50–137.0 U/L) one month after treatment); no statistically significant changes were observed between the respective groups (Figure 7a; p: BT (CR) vs. BT (nCR) > 0.999; BT (CR) vs. 1 M AT (CR) > 0.999; BT (CR) vs. 1 M AT (nCR) > 0.999; BT (nCR) vs. 1 M AT (CR) = 0.117; BT (nCR) vs. 1 M AT (nCR) = 0.370; 1 M AT (CR) vs. 1 M AT (nCR) > 0.999).
Figure 7.
(a) Serum LDH activity comparison: pre-treatment and one month post treatment in correlation with treatment response in 46 dogs. The enzyme activity was measured with an automated biochemical analyser on the day of treatment and four weeks later. The analysis showed no statistically remarkable changes in the serum LDH activity (p: BT (CR) vs. BT (nCR) > 0.999; BT (CR) vs. 1 M AT (CR) > 0.999; BT (CR) vs. 1 M AT (nCR) > 0.999; BT (nCR) vs. 1 M AT (CR) = 0.117; BT (nCR) vs. 1 M AT (nCR) = 0.370; 1 M AT (CR) vs. 1 M AT (nCR) > 0.999). BT, before treatment; 1 M AT, one month after treatment; CR, complete response; nCR, non–complete response (comprising of PR, SD, and PD); ns, not significant. (b) Serum LDH activity comparison: pre-treatment and one month post treatment in correlation with treatment-related enhanced tumour necrosis in 46 dogs. The enzyme activity was measured with an automated biochemical analyser on the day of treatment and four weeks later. The analyses showed a statistically significant increase in the serum LDH activity one month after treatment (p: BT (necrosis) vs. BT (no necrosis) > 0.999; BT (necrosis) vs. 1 M AT (necrosis) = 0.048; BT (necrosis) vs. 1 M AT (no necrosis) = 0.284; BT (no necrosis) vs. 1 M AT (necrosis) = 0.628; BT (no necrosis) vs. 1 M AT (no necrosis) > 0.999; 1 M AT (necrosis) vs. 1 M AT (no necrosis) > 0.999). BT, before treatment; 1 M AT, one month after treatment; * p < 0.05.
One month after treatment, the enhanced necrosis of tumour tissue was observed in 14 of the 46 dogs. We compared the serum LDH activity between these 14 animals before and one month after treatment (median 54.75 U/L (39.88–81.00 U/L) before treatment and median 100.3 U/L (56.50–313.8 U/L) one month after treatment) and the remaining 32 animals at the same time points (median 70.25 U/L (46.75–134.3 U/L) before treatment and median 107.8 U/L (48.13–136.5 U/L) one month after treatment). A statistically significant increase in the serum LDH activity was observed in the dogs in which treatment caused the necrosis of tumour tissue (Figure 7b; (p: BT (necrosis) vs. BT (no necrosis) > 0.999; BT (necrosis) vs. 1 M AT (necrosis) = 0.048; BT (necrosis) vs. 1 M AT (no necrosis) = 0.284; BT (no necrosis) vs. 1 M AT (necrosis) = 0.628; BT (no necrosis) vs. 1 M AT (no necrosis) > 0.999; 1 M AT (necrosis) vs. 1 M AT (no necrosis) > 0.999).
4. Discussion
The efficacy of ECT has been proven not only in the treatment of canine MCT, but also in various other tumour types [58,59,60]. In combination with IL-12 GET, this treatment approach is further improved and leads to better treatment results, as previous studies have shown [1,2,3,4,5,6]. Although the evaluation of its antitumour effectiveness was not the primary aim of this study, we examined the treatment outcomes at both one- and six-months post treatment. The findings of our study are consistent with previously published results and emphasise the treatment efficacy [6]. However, the focus of this study was on investigating possible changes in selected biomarkers and their clinical utility as predictive indicators of treatment success. Therefore, a long-term follow-up was not conducted.
To begin with, one of the possible biomarkers observed in this study was serum ferritin, in part because elevated serum ferritin levels have been observed in dogs with various malignancies, including lymphomas, histiocytic sarcomas, mammary tumours, IMHA and liver disease [26,27,28,29]. The aetiology of hyperferritinaemia is not fully known. It is likely to be complex in both neoplastic and non-neoplastic diseases. The proposed mechanisms include factors such as erythrocyte degradation, alterations in erythropoietic processes, release due to tissue damage and hepatocyte injury. It has already been demonstrated that malignant cells are able to synthesise ferritin [61].
There is a publication describing that mast cells in human skin store ferritin in their secretory granules and release it rapidly when activated by various mediators [62]. However, to the authors’ knowledge, changes in the serum ferritin concentrations in dogs have not been associated with the presence of MCT or with the assessment of the response to treatment using an ablative technique, such as ECT alone or in combination with IL-12 GET.
In our study, we did not detect significant changes in the serum ferritin concentration before and after treatment, regardless of the response to treatment or the presence of enhanced tumour necrosis. This suggests that the serum ferritin concentration may not be a reliable biomarker for assessing the response to ECT and IL-12 GET treatment in dogs with MCT. Nevertheless, we cannot exclude ferritin as a biomarker in dogs with MCT, as we did not compare the serum ferritin levels with a group of healthy dogs.
Furthermore, the nucleosome concentration was also analysed in the treated patients. Plasma nucleosome concentrations have been evaluated as a potential diagnostic or predictive biomarker because elevated nucleosome concentrations have previously been observed in various malignancies in humans and in certain malignancies in dogs, including lymphomas, haemangiosarcomas, histiocytic sarcomas and malignant melanomas, suggesting their utility as a diagnostic biomarker for early detection in dogs [35,36,40,41,42]. However, in a recent study, the serum nucleosome concentration did not prove to be a reliable diagnostic biomarker for MCT, accurately predicting only 19% of MCT cases. Interestingly, the study showed that high-grade MCTs had a significantly higher mean nucleosome concentration than low-grade MCTs and healthy dogs [35]. In our study, we measured the nucleosome concentration in 43 patients with confirmed mast cell neoplasia before treatment and found that the assay used accurately predicted the presence of the disease in 23.3% of patients (high concentrations), while 27.9% were in the grey zone. This study showed that the assay was more sensitive compared to previous reports; however, the number of patients observed in our study was lower. The specificity of the assay could not be evaluated in comparison to previous studies, as there was no healthy control group.
However, we refrained from comparing the nucleosome concentrations between different tumour grades as several tumours in our study were subcutaneous, and therefore such a classification is not possible, or were cutaneous, but no histopathology was performed. Most cutaneous MCTs in our study that were histopathologically graded were classified as grade II (Patnaik) and low grade (Kiupel). It is worth noting that, in this study, accurate grading was less reliable in animals with multiple MCTs, as in these animals only one tumour was sampled for grading. In addition, a previous study has shown that grading based on punch biopsy, as we performed, compared to excisional biopsy has 100% agreement with the Patnaik grading but only 95% agreement with the Kiupel grading [63]. Consequently, there is a possibility that the grade is underestimated when relying on punch biopsy to estimate the grade of the tumour, especially using the Kiupel grading standards.
On the other hand, we did observe a significant increase in Patnaik grading plasma nucleosome concentrations in 43 MCT patients one month after treatment with ECT and IL-12 GET. Looking at the measured values six months after treatment, they were not significantly changed in 17 out of 43 dogs. But at the same time, the values in the same 17 patients one month after treatment were no longer significant. This can be explained by the fact that a much smaller number of animals were included in the latter comparison. This raises the question of whether the change in the serum nucleosome concentration six months after treatment could be statistically significant if more patients were included.
A comparison between the response to treatment one month after treatment and changes in the plasma nucleosome concentrations showed no correlation. On the other hand, the presence of enhanced tumour necrosis at the same time point correlated significantly positively with the plasma nucleosome concentrations. Nucleosomes are predominantly located within cells and are released into the bloodstream, particularly upon activation or cell death [36]. This may explain the increase in the plasma nucleosome concentrations in patients where ablative techniques such as ECT with IL-12 GET were used for treatment, resulting in tissue inflammation and the necrosis of the tumour. In a recent study, Wilson-Robles et al. examined the nucleosome levels in 528 dogs with various common malignancies and compared them to 134 healthy dogs. Although elevated nucleosome levels have been found least frequently in soft tissue sarcomas, osteosarcomas and MCT [35], we could hypothesize that the increase in the plasma nucleosome concentration is due to tumour tissue degradation, regardless of the tumour type. Very similar changes in the nucleosome concentration during treatment with either radiotherapy or chemotherapy have been observed in human medicine in various malignancies [64,65,66]. The fluctuation in the plasma nucleosome concentration should be further investigated in different tumour types in dogs.
Overall, the results suggest that nucleosomes may be useful in assessing early treatment effects, particularly in the context of enhanced tumour necrosis. Their use as reliable biomarkers for predicting the long-term response to treatment needs further investigation. Since nucleosomes are part of the emerging concept of liquid biopsy, measuring circulating tumour DNA, circulating tumour cells and tumour extracellular vesicles in the blood of these animals could also provide further insight into disease progression or the treatment outcome [67].
Further on, the serum LDH activity was measured. Elevated serum LDH levels are associated with various cancers and are considered an indicator of high metabolic activity in malignant tumours [30,31]. In veterinary medicine, LDH has been studied in lymphomas, mammary gland tumours and oral cavity tumours, especially oral malignant melanoma [30,31,32,33,34].
In our study, a significant increase in the serum LDH activity was observed in 46 patients one month after treatment. We also observed changes in the LDH activity six months after treatment, albeit in a smaller group of 18 dogs examined at this time. However, in these 18 dogs, there was no significant change in the serum LDH activity six months after treatment, either compared to the pre-treatment values or compared to the period one month after treatment. Furthermore, a comparison of the LDH activity between the day of treatment and one month after treatment also showed no significant difference in these 18 dogs. As mentioned with regard to the plasma nucleosome concentration, it is important to consider the potential impact of the small sample size on these observations.
The serum LDH activity did not differ significantly between patients who responded to treatment and those who did not, as observed for the plasma nucleosome concentrations. When comparing the presence of enhanced tumour necrosis one month after treatment and the serum LDH activity, a significant increase was observed. In a study by Marconato et al., they found no association between significantly elevated LDH levels and the presence of MCT or MCT metastases in dogs when comparing healthy animals, animals with non-neoplastic disease and dogs with cancer [31]. A similar observation was made in our study, where only 10.8% of our patients with cytologically or histopathologically confirmed MCT had increased serum LDH activity before treatment. Therefore, the increase in LDH activity after one month of treatment and in the presence of enhanced tumour necrosis could be due to tissue breakdown, which is specifically greatest in the period up to one month after treatment with ECT and IL-12 GET. This suggests that the serum LDH activity may reflect short-term treatment effects but may not serve as a reliable long-term predictive biomarker for assessing the treatment response in dogs with MCT treated with ECT and IL-12 GET. Furthermore, the lack of correlation between the increased serum LDH activity and the presence of MCT suggests that the measurement of the serum LDH activity is not a useful diagnostic biomarker for determining the presence of MCT.
Finally, during the observation period, it was often detected that a higher number of PR and SD treatment responses occurred one month after treatment, accompanied by general signs of inflammation in the treated area. However, as healing progressed, the treatment responses generally became satisfactory. Similar observations were also made in a recent study, suggesting that the assessment of the treatment response after one month may be premature for the ECT combined with GET treatment approach, as the immune response is still active at this time, as evidenced by persistent swelling [6]. In light of this consideration, the comparison between the CR and nCR groups one month after treatment is less meaningful, as persistent swelling may interfere with the accurate assessment of treatment outcomes (based on RECIST criteria) and a comparison at a later date may be more meaningful.
Study Limitations
A major limitation of this study is the lack of samples six months after treatment in patients with disease progression. For a more meaningful comparison, it would be beneficial to have a larger number of samples from patients with stable or progressive disease six months after treatment to observe possible trends or differences in the measured biomarkers between patients with different long-term treatment outcomes.
Limitations also arise from the practise of sampling only one tumour for grading in animals with multiple tumours. This approach may underestimate the grade of the other present tumours, considering that different mast cell tumours may have different grades in the same animal.
A further limitation results from the inconsistent and incomplete clinical staging of the regional lymph nodes and the incomplete tumour grading. Tumour biopsy and histopathological grading were not performed in all patients. When tumours were assessed cytologically, no grading criteria were applied [68]. The surgical removal of regional lymph nodes or their sampling for the cytological determination of the presence of metastases were also not consistently performed, and the cytological grading criteria for lymph nodes were not applied [69]. Therefore, the possible influence of the tumour grade or metastatic disease on the measured biomarkers cannot be definitively excluded.
The lack of a healthy patient group for comparison is another important limitation of this study. Given the fact that markers were not monitored in patients with stable or progressive disease, and the lack of sufficient patient numbers, especially in the groups where trends were observed, further studies in larger patient groups are warranted.
Finally, the comparison of the selected biomarkers before and one month after treatment, based on the response to treatment according to the RECIST criteria, may not be meaningful in this study. The ongoing immune response within the tumour remains active and directly influences the assessment of the response to treatment and therefore represents a limitation of this study.
5. Conclusions
In summary, this study investigated the potential of plasma nucleosome and serum ferritin concentrations, as well as serum LDH activity, to be used as biomarkers for predicting the response to treatment of dogs with MCT using a combination of ECT and IL-12 GET. The plasma nucleosome concentration and serum LDH activity were found to be promising early indicators of treatment effects, especially in animals with enhanced tumour necrosis (Figure 1b), but their long-term predictive value needs further investigation. The serum ferritin concentration showed no significant predictive potential for the treatment response in this context.
Overall, this study contributes valuable insights into the use of biomarkers in veterinary oncology and highlights the need for further research to identify reliable predictors of the treatment response in dogs with MCT or other malignancies undergoing ECT and IL-12 GET therapy. The further investigation and validation of potential predictive biomarkers, as well as research into additional markers, could ultimately improve decision making in the treatment of canine cancer patients and improve treatment outcomes.
Author Contributions
Conceptualization, N.T., U.L.T., M.Č. and G.S.; methodology, U.L.T., N.T., M.Č., G.S. and N.M.; validation, U.L.T. and A.N.S.; formal analysis M.V., U.L.T. and A.N.S.; investigation, M.V., U.L.T., N.T. and N.M.; resources, U.L.T., N.T., A.N.S., M.Č. and G.S.; data curation, U.L.T., M.V. and A.N.S.; writing—original draft preparation, M.V.; writing—review and editing, U.L.T., N.T., N.M., M.Č., G.S. and A.N.S.; visualization, M.V. and U.L.T.; supervision, N.T., U.L.T., M.Č. and G.S.; project administration, U.L.T. and N.T.; funding acquisition, N.T., M.Č. and G.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The clinical trial was approved by the Ethics Committee of the Ministry of Agriculture, Forestry, and Food of the Republic of Slovenia (approval no. 254-20/2015/7 and permit for deliberate release of genetically modified organisms 35419/2021-2550-8).
Informed Consent Statement
Informed consent is obtained from the owner of the animals.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was supported by Slovenian Research and Innovation Agency (ARIS), grant numbers P3–0003, P4–0053, and J4–2546.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Cemazar M., Ambrozic Avgustin J., Pavlin D., Sersa G., Poli A., Krhac Levacic A., Tesic N., Lampreht Tratar U., Rak M., Tozon N. Efficacy and safety of electrochemotherapy combined with peritumoral IL-12 gene electrotransfer of canine mast cell tumours. Veter. Comp. Oncol. 2017;15:641–654. doi: 10.1111/vco.12208. [DOI] [PubMed] [Google Scholar]
- 2.Cutrera J., King G., Jones P., Kicenuik K., Gumpel E., Xia X., Li S. Safe and effective treatment of spontaneous neoplasms with interleukin 12 electro-chemo-gene therapy. J. Cell. Mol. Med. 2015;19:664–675. doi: 10.1111/jcmm.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Milevoj N., Tratar U.L., Nemec A., Brožič A., Žnidar K., Serša G., Čemažar M., Tozon N. A combination of electrochemotherapy, gene electrotransfer of plasmid encoding canine IL-12 and cytoreductive surgery in the treatment of canine oral malignant melanoma. Res. Veter. Sci. 2019;122:40–49. doi: 10.1016/j.rvsc.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Salvadori C., Svara T., Rocchigiani G., Millanta F., Pavlin D., Cemazar M., Lampreht Tratar U., Sersa G., Tozon N., Poli A. Effects of Electrochemotherapy with Cisplatin and Peritumoral IL-12 Gene Electrotransfer on Canine Mast Cell Tumors: A Histopathologic and Immunohistochemical Study. Radiol. Oncol. 2017;51:286–294. doi: 10.1515/raon-2017-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reed S.D., Fulmer A., Buckholz J., Zhang B., Cutrera J., Shiomitsu K., Li S. Bleomycin/interleukin-12 electrochemogenetherapy for treating naturally occurring spontaneous neoplasms in dogs. Cancer Gene Ther. 2010;17:571–578. doi: 10.1038/cgt.2010.13. [DOI] [PubMed] [Google Scholar]
- 6.Lampreht Tratar U., Milevoj N., Cemazar M., Znidar K., Ursic Valentinuzzi K., Brozic A., Tomsic K., Sersa G., Tozon N. Treatment of spontaneous canine mast cell tumors by electrochemotherapy combined with IL-12 gene electrotransfer: Comparison of intratumoral and peritumoral application of IL-12. Int. Immunopharmacol. 2023;120:110274. doi: 10.1016/j.intimp.2023.110274. [DOI] [PubMed] [Google Scholar]
- 7.Tozon N., Kodre V., Sersa G., Cemazar M. Effective treatment of perianal tumors in dogs with electrochemotherapy. Anticancer. Res. 2005;25:839–845. [PubMed] [Google Scholar]
- 8.Muir T., Bertino G., Groselj A., Ratnam L., Kis E., Odili J., McCafferty I., Wohlgemuth W.A., Cemazar M., Krt A., et al. Bleomycin electrosclerotherapy (BEST) for the treatment of vascular malformations. An International Network for Sharing Practices on Electrochemotherapy (InspECT) study group report. Radiol. Oncol. 2023;57:141–149. doi: 10.2478/raon-2023-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gothelf A., Mir L.M., Gehl J. Electrochemotherapy: Results of cancer treatment using enhanced delivery of bleomycin by electroporation. Cancer Treat. Rev. 2003;29:371–387. doi: 10.1016/S0305-7372(03)00073-2. [DOI] [PubMed] [Google Scholar]
- 10.Gehl J., Geertsen P.F. Efficient palliation of haemorrhaging malignant melanoma skin metastases by electrochemotherapy. Melanoma Res. 2000;10:585–589. doi: 10.1097/00008390-200012000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Djokic M., Dezman R., Cemazar M., Stabuc M., Petric M., Smid L.M., Jansa R., Plesnik B., Bosnjak M., Tratar U.L., et al. Percutaneous image guided electrochemotherapy of hepatocellular carcinoma: Technological advancement. Radiol. Oncol. 2020;54:347–352. doi: 10.2478/raon-2020-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Withrow S.J., Vail D.M., Page R.L., editors. Withrow and MacEwen’s Small Animal Clinical Oncology. Elsevier; Amsterdam, The Netherlands: 2020. [Google Scholar]
- 13.Calvet C.Y., Famin D., André F.M., Mir L.M. Electrochemotherapy with bleomycin induces hallmarks of immunogenic cell death in murine colon cancer cells. OncoImmunology. 2014;3:e28131. doi: 10.4161/onci.28131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tremble L.F., O’Brien M.A., Soden D.M., Forde P.F. Electrochemotherapy with cisplatin increases survival and induces immunogenic responses in murine models of lung cancer and colorectal cancer. Cancer Lett. 2019;442:475–482. doi: 10.1016/j.canlet.2018.11.015. [DOI] [PubMed] [Google Scholar]
- 15.Ursic K., Kos S., Kamensek U., Cemazar M., Miceska S., Markelc B., Bucek S., Staresinic B., Kloboves Prevodnik V., Heller R., et al. Potentiation of electrochemotherapy effectiveness by immunostimulation with IL-12 gene electrotransfer in mice is dependent on tumor immune status. J. Control. Release. 2021;332:623–635. doi: 10.1016/j.jconrel.2021.03.009. [DOI] [PubMed] [Google Scholar]
- 16.Snoj M., Cemazar M., Slekovec Kolar B., Sersa G. Effective treatment of multiple unresectable skin melanoma metastases by electrochemotherapy. Croat. Med. J. 2007;48:391–395. [PMC free article] [PubMed] [Google Scholar]
- 17.Lampreht Tratar U., Loiacono L., Cemazar M., Kamensek U., Fazio V.M., Sersa G., Signori E. Gene Electrotransfer of Plasmid-Encoding IL-12 Recruits the M1 Macrophages and Antigen-Presenting Cells Inducing the Eradication of Aggressive B16F10 Murine Melanoma. Mediat. Inflamm. 2017;2017:5285890. doi: 10.1155/2017/5285890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Groselj A., Bosnjak M., Jesenko T., Cemazar M., Markelc B., Strojan P., Sersa G. Treatment of skin tumors with intratumoral interleukin 12 gene electrotransfer in the head and neck region: A first-in-human clinical trial protocol. Radiol. Oncol. 2022;56:398–408. doi: 10.2478/raon-2022-0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daud A.I., DeConti R.C., Andrews S., Urbas P., Riker A.I., Sondak V.K., Munster P.N., Sullivan D.M., Ugen K.E., Messina J.L., et al. Phase I trial of interleukin-12 plasmid electroporation in patients with metastatic melanoma. J. Clin. Oncol. 2008;26:5896–5903. doi: 10.1200/JCO.2007.15.6794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blackwood L., Murphy S., Buracco P., De Vos J.P., De Fornel-Thibaud P., Hirschberger J., Kessler M., Pastor J., Ponce F., Savary-Bataille K., et al. European consensus document on mast cell tumours in dogs and cats. Veter. Comp. Oncol. 2012;10:e1–e29. doi: 10.1111/j.1476-5829.2012.00341.x. [DOI] [PubMed] [Google Scholar]
- 21.Nguyen S.M., Thamm D.H., Vail D.M., London C.A. Response evaluation criteria for solid tumours in dogs (v1.0): A Veterinary Cooperative Oncology Group (VCOG) consensus document. Veter. Comp. Oncol. 2015;13:176–183. doi: 10.1111/vco.12032. [DOI] [PubMed] [Google Scholar]
- 22.Kodre V., Cemazar M., Pecar J., Sersa G., Cor A., Tozon N. Electrochemotherapy compared to surgery for treatment of canine mast cell tumours. Vivo. 2009;23:55–62. [PubMed] [Google Scholar]
- 23.Sersa G., Ursic K., Cemazar M., Heller R., Bosnjak M., Campana L.G. Biological factors of the tumour response to electrochemotherapy: Review of the evidence and a research roadmap. Eur. J. Surg. Oncol. 2021;47:1836–1846. doi: 10.1016/j.ejso.2021.03.229. [DOI] [PubMed] [Google Scholar]
- 24.Myers M.J., Smith E.R., Turfle P.G. Biomarkers in Veterinary Medicine. Annu. Rev. Anim. Biosci. 2017;5:65–87. doi: 10.1146/annurev-animal-021815-111431. [DOI] [PubMed] [Google Scholar]
- 25.Nixon A.B., Schalper K.A., Jacobs I., Potluri S., Wang I.-M., Fleener C. Peripheral immune-based biomarkers in cancer immunotherapy: Can we realize their predictive potential? J. Immunother. Cancer. 2019;7:325. doi: 10.1186/s40425-019-0799-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friedrichs K., Thomas C., Plier M., Andrews G., Chavey P., Young K. Evaluation of serum ferritin as a tumor marker for canine histiocytic sarcoma. J. Veter. Intern. Med. 2010;24:904–911. doi: 10.1111/j.1939-1676.2010.0543.x. [DOI] [PubMed] [Google Scholar]
- 27.Kazmierski K.J., Ogilvie G.K., Fettman M.J., Lana S.E., Walton J.A., Hansen R.A., Richardson K.L., Hamar D.W., Bedwell C.L., Andrews G., et al. Serum zinc, chromium, and iron concentrations in dogs with lymphoma and osteosarcoma. J. Vet. Intern. Med. 2001;15:585–588. doi: 10.1111/j.1939-1676.2001.tb01595.x. [DOI] [PubMed] [Google Scholar]
- 28.Newlands C.E., Houston D.M., Vasconcelos D.Y. Hyperferritinemia associated with malignant histiocytosis in a dog. J. Am. Vet. Med. Assoc. 1994;205:849–851. doi: 10.2460/javma.1994.205.06.849. [DOI] [PubMed] [Google Scholar]
- 29.Fan Y., Ren X., Liu X., Shi D., Xu E., Wang S., Liu Y. Combined detection of CA15-3, CEA, and SF in serum and tissue of canine mammary gland tumor patients. Sci. Rep. 2021;11:6651. doi: 10.1038/s41598-021-85029-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Campos L., Lavalle G., Estrela-Lima A., Melgaço de Faria J., Guimarães J., Dutra Á.P., Ferreira E., de Sousa L.P., Rabelo É.M., Vieira da Costa A.F., et al. CA15.3, CEA and LDH in Dogs with Malignant Mammary Tumors. J. Veter. Intern. Med. 2012;26:1383–1388. doi: 10.1111/j.1939-1676.2012.01014.x. [DOI] [PubMed] [Google Scholar]
- 31.Marconato L., Crispino G., Finotello R., Mazzotti S., Salerni F., Zini E. Serum lactate dehydrogenase activity in canine malignancies. Veter. Comp. Oncol. 2009;7:236–243. doi: 10.1111/j.1476-5829.2009.00196.x. [DOI] [PubMed] [Google Scholar]
- 32.Zanatta R., Abate O., D’Angelo A., Miniscalco B., Mannelli A. Diagnostic and prognostic value of serum lactate dehydrogenase (LDH) and LDH isoenzymes in canine lymphoma. Veter. Res. Commun. 2003;27:449–452. doi: 10.1023/B:VERC.0000014201.82393.67. [DOI] [PubMed] [Google Scholar]
- 33.Choisunirachon N., Klansnoh U., Phoomvuthisarn P., Pisamai S., Thanaboonnipat C., Rungsipipat A. The expression of serum lactate dehydrogenase in canine oral tumors. Thai J. Veter. Med. 2019;49:283–288. doi: 10.56808/2985-1130.2993. [DOI] [Google Scholar]
- 34.Murray B., Blacklock K.L.B. Pilot Study: Assessing the Expression of Serum Lactate Dehydrogenase and Peripheral Leukocyte Ratios in Canine Oral Malignant Melanoma. Veter. Sci. 2022;9:421. doi: 10.3390/vetsci9080421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilson-Robles H.M., Bygott T., Kelly T.K., Miller T.M., Miller P., Matsushita M., Terrell J., Bougoussa M., Butera T. Evaluation of plasma nucleosome concentrations in dogs with a variety of common cancers and in healthy dogs. BMC Veter. Res. 2022;18:329. doi: 10.1186/s12917-022-03429-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilson-Robles H., Miller T., Jarvis J., Terrell J., Dewsbury N., Kelly T., Herzog M., Bygott T., Hardat N., Michel G. Evaluation of nucleosome concentrations in healthy dogs and dogs with cancer. PLoS ONE. 2020;15:e0236228. doi: 10.1371/journal.pone.0236228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martiny P., Goggs R. Biomarker Guided Diagnosis of Septic Peritonitis in Dogs. Front. Veter. Sci. 2019;6:208. doi: 10.3389/fvets.2019.00208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Letendre J.-A., Goggs R. Determining prognosis in canine sepsis by bedside measurement of cell-free DNA and nucleosomes. J. Veter. Emerg. Crit. Care. 2018;28:503–511. doi: 10.1111/vec.12773. [DOI] [PubMed] [Google Scholar]
- 39.Letendre J.-A., Goggs R. Concentrations of Plasma Nucleosomes but Not Cell-Free DNA Are Prognostic in Dogs Following Trauma. Front. Veter. Sci. 2018;5:180. doi: 10.3389/fvets.2018.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dolan C., Miller T., Jill J., Terrell J., Kelly T.K., Bygott T., Wilson-Robles H. Characterizing circulating nucleosomes in the plasma of dogs with lymphoma. BMC Veter. Res. 2021;17:276. doi: 10.1186/s12917-021-02991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rasmussen L., Christensen I.J., Herzog M., Micallef J., Nielsen H.J. For the Danish Collaborative Group on Early Detection of Colorectal Cancer Circulating cell-free nucleosomes as biomarkers for early detection of colorectal cancer. Oncotarget. 2018;9:10247–10258. doi: 10.18632/oncotarget.21908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kumar S., Guleria R., Singh V., Bharti A.C., Mohan A., Das B.C. Plasma Nucleosome Levels Might Predict Response to Therapy in Patients with Advanced Non–Small-Cell Lung Cancer. Clin. Lung Cancer. 2010;11:36–44. doi: 10.3816/CLC.2010.n.006. [DOI] [PubMed] [Google Scholar]
- 43.Tsoneva D.K., Ivanov M.N., Conev N.V., Manev R., Stoyanov D.S., Vinciguerra M. Circulating Histones to Detect and Monitor the Progression of Cancer. Int. J. Mol. Sci. 2023;24:942. doi: 10.3390/ijms24020942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cruz C., Pedro A.Q., Carvalho J., Santos T., Talhada D., Paiva A., Queiroz J.A., Andrade M., Pinto M., Montenegro L., et al. Nucleolin as a potential biomarker for canine malignant neoplasia. Res. Veter. Sci. 2021;135:297–303. doi: 10.1016/j.rvsc.2020.10.004. [DOI] [PubMed] [Google Scholar]
- 45.Hintze K., Theil E.C. Cellular regulation and molecular interactions of the ferritins. Cell. Mol. Life Sci. 2006;63:591–600. doi: 10.1007/s00018-005-5285-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cullis J.O., Fitzsimons E.J., Griffiths W.J., Tsochatzis E., Thomas D.W., Haematology T.B.S.F. Investigation and management of a raised serum ferritin. Br. J. Haematol. 2018;181:331–340. doi: 10.1111/bjh.15166. [DOI] [PubMed] [Google Scholar]
- 47.Jacobs A., Worwood M. Ferritin in serum: Clinical and biochemical implications. N. Engl. J. Med. 1975;292:951–956. doi: 10.1056/NEJM197505012921805. [DOI] [PubMed] [Google Scholar]
- 48.Worwood M. Ferritin. Blood Rev. 1990;4:259–269. doi: 10.1016/0268-960X(90)90006-E. [DOI] [PubMed] [Google Scholar]
- 49.Hu Z., Wang L., Han Y., Li F., Zheng A., Xu Y., Wang F., Xiao B., Chen C., Tao Z. Ferritin: A potential serum marker for lymph node metastasis in head and neck squamous cell carcinoma. Oncol. Lett. 2018;17:314–322. doi: 10.3892/ol.2018.9642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jung M., Mertens C., Tomat E., Brüne B. Iron as a Central Player and Promising Target in Cancer Progression. Int. J. Mol. Sci. 2019;20:273. doi: 10.3390/ijms20020273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim J.-W., Dang C.V. Multifaceted roles of glycolytic enzymes. Trends Biochem. Sci. 2005;30:142–150. doi: 10.1016/j.tibs.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 52.Feng Y., Xiong Y., Qiao T., Li X., Jia L., Han Y. Lactate dehydrogenase A: A key player in carcinogenesis and potential target in cancer therapy. Cancer Med. 2018;7:6124–6136. doi: 10.1002/cam4.1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Horta R.S., Lavalle G.E., Monteiro L.N., Souza M.C.C., Cassali G.D., Araújo R.B. Assessment of Canine Mast Cell Tumor Mortality Risk Based on Clinical, Histologic, Immunohistochemical, and Molecular Features. Veter. Pathol. 2018;55:212–223. doi: 10.1177/0300985817747325. [DOI] [PubMed] [Google Scholar]
- 54.Kiupel M., Webster J.D., Bailey K.L., Best S., DeLay J., Detrisac C.J., Fitzgerald S.D., Gamble D., Ginn P.E., Goldschmidt M.H., et al. Proposal of a 2-Tier Histologic Grading System for Canine Cutaneous Mast Cell Tumors to More Accurately Predict Biological Behavior. Veter. Pathol. 2011;48:147–155. doi: 10.1177/0300985810386469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Patnaik A.K., Ehler W.J., MacEwen E.G. Canine Cutaneous Mast Cell Tumor: Morphologic Grading and Survival Time in 83 Dogs. Veter. Pathol. 1984;21:469–474. doi: 10.1177/030098588402100503. [DOI] [PubMed] [Google Scholar]
- 56.Lampreht Tratar U., Kos S., Kamensek U., Ota M., Tozon N., Sersa G., Cemazar M. Antitumor effect of antibiotic resistance gene-free plasmids encoding interleukin-12 in canine melanoma model. Cancer Gene Ther. 2018;25:260–273. doi: 10.1038/s41417-018-0014-5. [DOI] [PubMed] [Google Scholar]
- 57.Tozon N., Lampreht Tratar U., Znidar K., Sersa G., Teissie J., Cemazar M. Operating Procedures of the Electrochemotherapy for Treatment of Tumor in Dogs and Cats. J. Vis. Exp. 2016;2016:e54760. doi: 10.3791/54760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lowe R., Gavazza A., Impellizeri J.A., Soden D.M., Lubas G. The treatment of canine mast cell tumours with electrochemotherapy with or without surgical excision. Veter. Comp. Oncol. 2017;15:775–784. doi: 10.1111/vco.12217. [DOI] [PubMed] [Google Scholar]
- 59.Spugnini E.P., Vincenzi B., Amadio B., Baldi A. Adjuvant electrochemotherapy with bleomycin and cisplatin combination for canine soft tissue sarcomas: A study of 30 cases. Open Veter. J. 2019;9:88–93. doi: 10.4314/ovj.v9i1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Torrigiani F., Pierini A., Lowe R., Simčič P., Lubas G. Soft tissue sarcoma in dogs: A treatment review and a novel approach using electrochemotherapy in a case series. Veter. Comp. Oncol. 2019;17:234–241. doi: 10.1111/vco.12462. [DOI] [PubMed] [Google Scholar]
- 61.Sarcione E.J., Smalley J.R., Lema M.J., Stutzman L. Increased ferritin synthesis and release by Hodgkin’s disease peripheral blood lymphocytes. Int. J. Cancer. 1977;20:339–346. doi: 10.1002/ijc.2910200304. [DOI] [PubMed] [Google Scholar]
- 62.Ward B.R., Hicks M., Johnson J.-M., Myo Y.P.A. Ferritin Particles Accumulate in Human Mast Cell Secretory Granules and Are Released upon FcεRI-mediated Activation. J. Allergy Clin. Immunol. 2018;141:AB229. doi: 10.1016/j.jaci.2017.12.722. [DOI] [Google Scholar]
- 63.Shaw T., Kudnig S.T., Firestone S.M. Diagnostic accuracy of pre-treatment biopsy for grading cutaneous mast cell tumours in dogs. Veter. Comp. Oncol. 2018;16:214–219. doi: 10.1111/vco.12346. [DOI] [PubMed] [Google Scholar]
- 64.Kremer A., Holdenrieder S., Stieber P., Wilkowski R., Nagel D., Seidel D. Nucleosomes in Colorectal Cancer Patients during Radiochemotherapy. Tumor Biol. 2006;27:235–242. doi: 10.1159/000094694. [DOI] [PubMed] [Google Scholar]
- 65.Holdenrieder S., Stieber P. Therapy Control in Oncology by Circulating Nucleosomes. Ann. N. Y. Acad. Sci. 2004;1022:211–216. doi: 10.1196/annals.1318.032. [DOI] [PubMed] [Google Scholar]
- 66.Holdenrieder S., Stieber P., Bodenmüller H., Busch M., Fertig G., Fürst H., Schalhorn A., Schmeller N., Untch M., Seidel D. Nucleosomes in serum of patients with benign and malignant diseases. Int. J. Cancer. 2001;95:114–120. doi: 10.1002/1097-0215(20010320)95:2<114::AID-IJC1020>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 67.Yee N.S. Liquid Biopsy: A Biomarker-Driven Tool towards Precision Oncology. J. Clin. Med. 2020;9:2556. doi: 10.3390/jcm9082556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Camus M.S., Priest H.L., Koehler J.W., Driskell E.A., Rakich P.M., Ilha M.R., Krimer P.M. Cytologic Criteria for Mast Cell Tumor Grading in Dogs with Evaluation of Clinical Outcome. Veter. Pathol. 2016;53:1117–1123. doi: 10.1177/0300985816638721. [DOI] [PubMed] [Google Scholar]
- 69.Krick E.L., Billings A.P., Shofer F.S., Watanabe S., Sorenmo K.U. Cytological lymph node evaluation in dogs with mast cell tumours: Association with grade and survival. Veter. Comp. Oncol. 2009;7:130–138. doi: 10.1111/j.1476-5829.2009.00185.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.